Abstract
Duodenal varices are a rare complication in patients with portal hypertension. Bleeding from duodenal varices often results in a severe prognosis. Diagnosis of the disease is usually based on findings obtained by endoscopy or angiography. However, it occasionally fails to detect the lesion and demonstrate its porto-systemic shunt vessels which are necessary information to decide an appropriate treatment. Recent advances in CT may make it possible for us to reveal duodenal varices with complicated porto-systemic shunt vessels. We report the case of a 58-year-old man with liver cirrhosis with repeated bleeding from duodenal varices. Esophagogastroduodenoscopy (EGD) revealed multinodular varices in the third portion of the duodenum. Then we conducted a capsule endoscopy (CE) and found fresh blood in the duodenum, suggesting duodenal variceal hemorrhage. Angiography depicted the varices with one afferent and two efferent vessels. Abdominal CT examination was conducted using a four-channel multi-detector row CT scanner. The multiplanar reconstructed images revealed not only the varices, but also three afferent and two efferent vessels. The patient was treated by surgical ligation and sclerotherapy, because of its complicated porto-systemic shunt and reserved liver function. No gastrointestinal bleeding has been seen after the surgery. Our case suggests the usefulness of multi-detector CT with multiplanar reconstruction (MPR) for the diagnosis and therapeutic decision of duodenal varices.
Keywords: Varices, Computed tomography, Duodenum, Surgical hemostasis
Introduction
Duodenal varices are a rare complication in patients with portal hypertension. Bleeding from duodenal varices often results in a severe prognosis. Duodenal varices mainly develop in the bulbar portion, but the varices are also found in further sites of the duodenum. Diagnosis of the disease is usually based on findings obtained by endoscopy or angiography. However, conventional endoscopy cannot reach the distal site of the duodenum and angiography occasionally fails to depict duodenal varices due to inappropriate catheter cannulation to collateral vessels [1]. CT angiography has been reported as efficient in detecting duodenal varices [2]. Recent advances in CT may make it possible for us to reveal duodenal varices with complicated porto-systemic shunt vessels [3].
Case report
A 58-year-old man with liver cirrhosis due to hepatitis C virus infection was referred to our hospital with continuing melena. The patient had experienced the same clinical episodes and received blood transfusion for eight times before he was admitted to our hospital. Several imaging examinations including esophagogastroduodenoscopy (EGD), colonoscopy, and abdominal CT without contrast agent had been performed since the first bleeding episode appeared. However, the origin of bleeding remained unknown.
The hemoglobin level was 6.9 g/dl [normal range (NR) 11.3–15.5 g/dl]. EGD revealed multinodular varices in the third portion of the duodenum. However, no blood was seen in the upper GI tract when examined by EGD. Then we conducted a capsule endoscopy (CE) and found fresh blood in the duodenum, suggesting duodenal variceal hemorrhage.
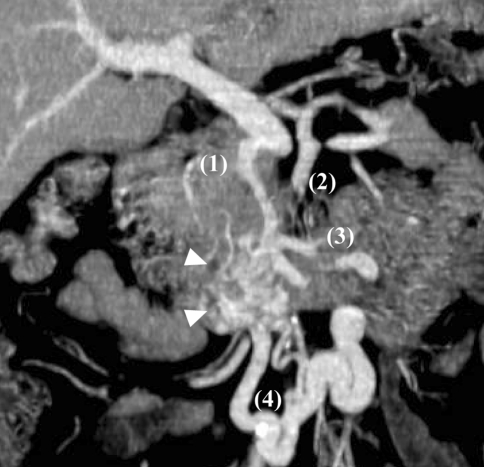
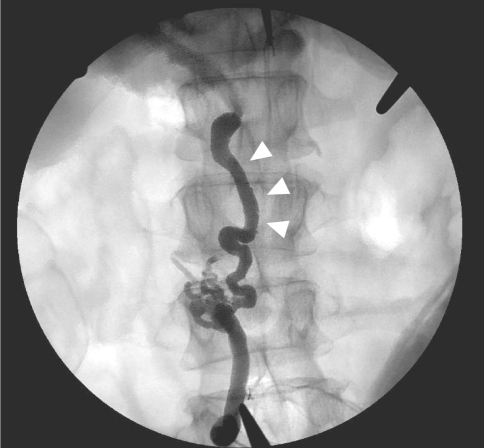
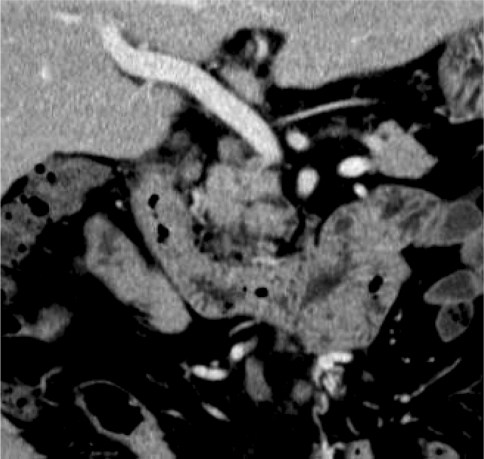
In order to investigate the hemodynamics of the varices, an abdominal CT examination was conducted using a four-channel multi-detector row CT scanner (Robusto®, Hitachi Medical Corporation, Tokyo, Japan). Images were reconstructed with a slice width of 2.5 mm and a reconstruction interval of 1.5 mm. The abdomen was dynamically scanned during administration of 100 ml of nonionic iodinated contrast material (Iomeprol®, Iomeron 350 mg I/ml; Eisai, Tokyo, Japan) with duration of 60 s. The scan was started 90 s after the contrast material injection was initiated. The axial view of the CT showed the duodenal wall thickness with high-density contrast, suggesting the presence of the duodenal varices. The multiplanar reconstruction (MPR) image clearly revealed the varices with multiple porto-systemic shunt vessels: three afferent vessels (the posterior superior pancreaticoduodenal vein, dorsal pancreatic vein, and superior mesenteric vein via jejunal vein) and at least two efferent vessels (the lumbar vein and left renal vein via the veins of Retzius) (Fig. 1). An angiography also showed the varices, however, it depicted only one afferent (the posterior superior pancreaticoduodenal vein) and two efferent vessels. Endovascular obliteration therapy was considered inappropriate for the patient, because of the multiple porto-systemic shunt vessels in the varices and inaccessibility to the veins of Retzius. We did not consider performing percutaneous transhepatic obliteration (PTO), because of its relatively high recurrence rate [4]. Finally, we decided the patient was to receive surgical ligation and sclerotherapy. An angiography during surgery which injected a contrast agent from veins of Retzius showed one afferent vessel (dorsal pancreatic vein, Fig. 2). An angiography with manual occlusion of dorsal pancreatic vein to portal vein showed the three afferent vessels and one efferent vessel draining to the veins of Retzius (Fig. 3). 10% ethanolamine oleate (Oldamin®, Mochida Phamaceutical, Tokyo, Japan) and the same amount of iopamidol (300 mg iodine; Iopamiron®, Schring, Osaka, Japan) were injected in the varices. The residual communications between the varices and collateral shunt vessels were ligated and detached (Fig. 4). CT with MPR revealed that the duodenal varices disappeared after the treatment (Fig. 5). No gastrointestinal bleeding has been seen after the surgery.
Fig. 1.
CT scan image by multiplanar reconstruction CT. The image revealed the duodenal varices (arrowhead) with three afferent vessels: posterior superior pancreaticoduodenal vein (1), dorsal pancreatic vein (2), and superior mesenteric vein via jejunal vein (3). Two efferent vessels draining through the veins of Retzius (4) were also depicted
Fig. 2.
Angiography without manual occlusion of a connecting vessel to portal vein during surgery. The angiography revealed one afferent vessel (dorsal pancreatic vein, arrowhead) and the veins of Retzius
Fig. 3.
Angiography with manual occlusion of a connecting vessel to portal vein during the surgery. The angiography revealed three afferent vessels (posterior superior pancreaticoduodenal vein (1), dorsal pancreatic vein (2), and superior mesenteric vein via jejunal vein (3) and the veins of Retzius (4)
Fig. 4.
Angiography with manual occlusion after the sclerotherapy. The residual communications between the varices and collateral shunt vessels were ligated and detached
Fig. 5.
Multiplanar reconstruction CT after the surgery. The varices and its connecting vessels completely disappeared
Discussion
Our case suggests the usefulness of multi-detector CT with MPR for the diagnosis of duodenal varices. Multi-detector CT with intravenous contrast agent depicted the duodenal varices with complicated porto-systemic shunt vessels. The importance of CT during arterial portography for revealing paraumbilical varices has been reported [2, 5]. Usefulness of CT-maximum intensity projection (CT-MIP) for depicting gastric varices with collateral vessels has been reported [6]. However, there have been few papers suggesting the efficacy of multislice CT with reconstruction on the diagnosis of duodenal varices [3]. Scanning speed and imaging quality of CT have been improving and the role of CT in the diagnosis of duodenal varices should become more important.
Capsule endoscopy is a novel procedure which makes it possible for us to see small intestinal mucosa. In our case, CE revealed the presence of fresh blood in the duodenum, which indicates the bleeding site precisely. Pennazio et al. [7] reported that sensitivity of CE for obscure gastrointestinal bleeding is 88.9%. However, it is impossible to access the collateral porto-systemic shunt vessels outside of the intestine, which are necessary to decide treatment options.
Our case received surgical treatment and took a good clinical course after the procedure. There have been many treatment procedures for duodenal varices: endoscopic injection sclerotherapy (EIS), endoscopic variceal ligation (EVL), transjuglar intrahepatic porto-systemic shunt (TIPS), endovascular obliteration including PTO and balloon-occluded retrograde transvenous obliteration (BRTO), and surgery. Endoscopic treatment is one of the most plausible options, because it is easier and less invasive than others. However, the efficacy of EVL is of short term and limited to small varices [8]. EIS has a risk of perforation after the procedure [9]. TIPS has been widely preformed, especially in patients with gastrointestinal varices which are difficult to access by endovascular intervention procedure. However, TIPS decreases hepatic function by reducing blood flow in portal vein and promotes hepatic encephalopathy by increasing porto-systemic shunt blood flow [10]. Endovascular obliteration should be effective for duodenal varices, likewise for gastric varices. However, it is very difficult to perform endovascular obliteration in patients with multiple afferent vessels. In addition, occlusion of the efferent vein is indispensable for endovascular obliteration [11]. Although surgical treatment is more invasive than other procedures, the treatment achieves curative effects on duodenal varices especially in patients with reserved liver function. Our case suggests that surgical ligation and sclerotherapy are worthy of consideration for patients with complicated shunt vessels and reserved liver function.
In conclusion, we have reported that multi-detector dynamic CT is an effective modality to demonstrate duodenal varices with complicated porto-systemic shunt vessels, all of which is necessary information in deciding the best treatment. Multi-detector dynamic CT is a quick, simple and safe procedure and should be performed in patients with duodenal varices.
References
- 1.Perchik L, Max T. Massive hemorrhage from varices of the duodenal loop in a cirrhotic patient. Radiology. 1963;80:641–645. [Google Scholar]
- 2.Ibukuro K, Tsukiyama T, Mori K, Inoue Y. Veins of Retzius at CT during arterial portography: anatomy and clinical importance. Radiology. 1998;209:793–800. doi: 10.1148/radiology.209.3.9844676. [DOI] [PubMed] [Google Scholar]
- 3.Weishaupt D, Pfammatter T, Hilfiker PR, Wolfensberger U, Marincek B. Detecting bleeding duodenal varices with multislice helical CT. AJR Am J Roentgenol. 2002;178:399–401. doi: 10.2214/ajr.178.2.1780399. [DOI] [PubMed] [Google Scholar]
- 4.Kameda N, Higuchi K, Shiba M, Kadouchi K, Machida H, Okazaki H, Tanigawa T, Watanabe T, Tominaga K, Fujiwara Y, Nakamura K, Arakawa T. Management of gastric fundal varices without gastro-renal shunt in 15 patients. World J Gastroenterol. 2008;14:448–453. doi: 10.3748/wjg.14.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seo YS, Kwon YD, Park S, Keum B, Park BJ, Kim YS, Jeen YT, Chun HJ, Kim CD, Ryu HS, Um SH. Complete eradication of duodenal varices after endoscopic injection sclerotherapy with ethanolamine oleate: a case report. Gastrointest Endosc. 2008;67:759–762. doi: 10.1016/j.gie.2007.08.027. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa T, Ushiki T, Mizuno K, Togashi T, Watanabe K, Seki K, Ohta H, Yoshida T, Takeda K, Kamimura T. CT-maximum intensity projection is a clinically useful modality for the detection of gastric varices. World J Gastroenterol. 2005;11:7515–7519. doi: 10.3748/wjg.v11.i47.7515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, Franchis R. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology. 2004;126:643–653. doi: 10.1053/j.gastro.2003.11.057. [DOI] [PubMed] [Google Scholar]
- 8.Yoshida Y, Imai Y, Nishikawa M, Nakatukasa M, Kurokawa M, Shibata K, Shimomukai H, Shimano T, Tokunaga K, Yonezawa T. Successful endoscopic injection sclerotherapy with n-butyl-2-cyanoacrylate following the recurrence of bleeding soon after endoscopic ligation for ruptured duodenal varices. Am J Gastroenterol. 1997;92:1227–1229. [PubMed] [Google Scholar]
- 9.Tsuji H, Okano H, Fujino H, Satoh T, Kodama T, Takino T, Yoshimura N, Aikawa I, Oka T, Tsuchihashi Y. A case of endoscopic injection sclerotherapy for a bleeding duodenal varix. Gastroenterol Jpn. 1989;24:60–64. doi: 10.1007/BF02774872. [DOI] [PubMed] [Google Scholar]
- 10.Sahagun G, Benner KG, Saxon R, Barton RE, Rabkin J, Keller FS, Rosch J. Outcome of 100 patients after transjugular intrahepatic porto-systemic shunt for variceal hemorrhage. Am J Gastroenterol. 1997;92:1444–1452. [PubMed] [Google Scholar]
- 11.Takao H, Ohtomo K. Balloon-occluded retrograde transvenous obliteration of gastric varices using three-dimensional rotational angiography. Br J Radiol. 2009;82:e55–e57. doi: 10.1259/bjr/23922063. [DOI] [PubMed] [Google Scholar]