Abstract
Background
Traditional perinatal practices may protect against postnatal common mental disorders (CMD) in non-Western societies.
Aims
To evaluate the association between perinatal practices and postnatal CMD in rural Ethiopia.
Method
A population-based sample of 1065 women was followed up from pregnancy until 2 months postpartum. Qualitative investigation informed the development of scales measuring attitudes towards and adherence to perinatal practices. Postnatal CMD was measured using the Self-Reporting Questionnaire.
Results
Endorsement of sociocultural perinatal practices was associated with lower odds of antenatal CMD persisting into the postnatal period (adjusted odds ratio (OR) = 0.66, 95% CI 0.45–0.95). Women who endorsed protective and celebratory perinatal practices but were unable to complete them had increased odds of incident (adjusted OR = 7.26, 95% CI 1.38–38.04) and persistent postnatal CMD (adjusted OR = 2.16, 95% CI 1.11–4.23) respectively.
Conclusions
There is evidence for an independent role of sociocultural practices in maintaining perinatal mental health in this Ethiopian community.
The extensive sociocultural elaboration of the perinatal period in non-Western societies has been hypothesised to protect against the onset of postnatal common mental disorders (CMD: characterised by significant levels of depressive, anxiety and somatic symptoms).1 Epidemiological studies from non-Western countries challenge this view,2 finding the prevalence of postnatal CMD to be largely comparable with that seen in Western countries.3 Specific postnatal practices have been variably associated with postnatal CMD in non-Western countries,4–8 highlighting the need for a contextualised understanding of the meanings associated with perinatal practices in a particular sociocultural setting. We are aware of only one previous study (from Hong Kong) that used ethnographically informed epidemiological methods to explore the relationship between traditional postnatal practices and postnatal mental health.5,9 No such studies have been published from sub-Saharan Africa.
The Perinatal Maternal Mental health in Ethiopia (P-MaMiE) study is a mixed method study that was undertaken to evaluate the impact of sociocultural practices on risk of postnatal CMD in rural Ethiopia. On the basis of initial qualitative work10 and the literature, the following hypotheses were generated: antenatal women who endorse adherence towards traditional sociocultural perinatal practices will be protected against incident postnatal CMD and in these women, non-completion of postnatal practices will be associated with increased risk of incident and persistent postnatal CMD.
Method
Ethical approval was obtained from the research ethics committees of the participating institutions in Ethiopia and the UK.
Setting
The P-MaMiE study was located within the demographic surveillance site in Butajira, which forms part of the Butajira Rural Health Programme.11 Butajira is a predominantly rural area of Ethiopia located 130 km south of the capital city Addis Ababa. Around Butajira, the livelihood of residents is based on mixed farming, with khat (an amphetamine-like psychostimulant) and chilli pepper as the main cash crops and maize as the predominant subsistence grain. Maternal mortality rates are estimated at 400–850/100 000 births.12 Fewer than 10% of women attend for delivery in a health facility or receive any formal postnatal care.13
Developing measures of sociocultural perinatal practices
Identifying perinatal practices
In our previous qualitative study, sociocultural patterning of the perinatal period was explored in relation to women’s perinatal mental health.10 In brief, a total of 25 in-depth interviews and 5 focus-group discussions, involving 78 informants, were conducted with community stakeholders in the Butajira area. Open questions were used to probe systematically about perinatal practices and the potential impact on the mother if she was unable to fulfil them. Perinatal women in rural Ethiopia are commonly expected to adhere to a series of prohibitions and prescribed practices that serve to protect them against harm and restore health following childbirth. Certain celebratory practices that recognise the woman’s role transition are also culturally endorsed. We used these data to operationalise measures of women’s attitudes towards and adherence to perinatal practices. Those perinatal practices that recurred across accounts and whose non-performance was considered by participants to result in adverse consequences, were selected for inclusion in the quantitative study. This resulted in selection of 13 perinatal practices, 8 protective and 5 celebratory (Table 1).
Table 1.
Frequency distribution of endorsed and non-completed perinatal sociocultural practices
| Items included in scales
|
|||||
|---|---|---|---|---|---|
| Perinatal practice | Endorsing practice antenatally, n (%) | Not carrying out practice if endorsed, n (%) | Antenatal sociocultural attitudes scale | Discordant protective practices scale | Discordant celebratory practices scale |
| Pregnancy practices | |||||
| Should cover abdomen (to conceal the pregnancy) | 548 (57.5) | – | Yes | – | – |
| Should restrict diet | 563 (59.3) | – | Yes | – | – |
| Should carry pot on back | 573 (60.1) | – | Yes | – | – |
| Should prepare for postnatal period | 925 (97.1) | – | – | – | – |
| Should perform dua/deremaa |
600 (63.0)
|
–
|
Yes
|
–
|
–
|
| Postnatal practices | |||||
| Should slaughter animal | 761 (79.9) | 398 (41.8) | – | – | Yes |
| Should receive gifts | 803 (84.4) | 153 (16.1) | – | – | Yes |
| Should bury placenta | 879 (92.2) | 101 (10.6) | Yes | – | – |
| Should carry metal | 785 (82.4) | 129 (13.5) | Yes | Yes | – |
| Should speak softly | 856 (89.8) | 102 (10.7) | Yes | Yes | – |
| Should avoid cold air/draughts | 935 (98.1) | 62 (6.5) | Yes | Yes | – |
| Should do bathing ceremony | 938 (98.4) | 25 (2.6) | Yes | – | – |
| Should perform dang mergetb | 710 (74.5) | – | Yes | – | – |
a. Dua/derema refers to a prayer ceremony.
b. Dang merget describes the ritualistic crossing of the home boundary to celebrate completion of the postnatal period.
Attitudes and adherence to perinatal practices
Sociocultural perinatal attitudes. Perinatal practices were turned into a series of statements (Table 1). At the antenatal time point, participants were asked to indicate their level of agreement on a five-point Likert scale (not at all, not much, neither agree nor disagree, somewhat, very much). Antenatal attitudes towards perinatal sociocultural practices were dichotomised (item endorsed – agree somewhat or very much).
Discordance between attitudes and adherence. At the 2-month postnatal time point, women were asked whether they had completed specific postnatal practices. New variables were defined for women who endorsed specific postnatal practices antenatally and then did not carry them out postnatally (Table 1).
Mokken scaling
Responses to the perinatal attitudes and adherence questions were analysed using Mokken analysis.14 This approach has been used widely in psychology, education and social science research, and more recently has been applied within psychiatric research.15 Mokken analysis utilises non-parametric item-response theory to evaluate the presence of a hierarchical scale within a set of responses.15 In Mokken scales, the relative ordering of items is assumed to reflect ordering along an underlying latent trait. The presence of a Mokken scale justifies summing item scores.
Following standard procedure, item-pair Loevinger coefficients for both perinatal attitudes and discordance between attitudes and adherence were inspected and the highest were sequentially added to the scale, retained if the Loevinger H item-scale coefficient for the individual item was ≥0.30. The conditions of monotone homogeneity and double monotonicity were assessed and items leading to violations were removed. The Loevinger H for each final scale was evaluated. A scale is considered dimensionally weak for Loevinger coefficients between 0.30 and 0.39, moderate for coefficients between 0.40 and 0.49 and strong for coefficients of 0.50 or higher.14
Population-based cohort study
Sample
Eligible women were between the ages of 15 and 49 years, able to speak Amharic (the official language of Ethiopia), living in the demographic surveillance site area and in the third trimester of pregnancy during the study recruitment period (July 2005 to February 2006). Women were identified by the Butajira Rural Health Programme enumerators in the course of their 3-monthly surveillance interviews and, after giving informed consent, were interviewed by the project data collectors. Of eligible pregnant women, 1065 (86.3%) were successfully recruited. Non-recruited women did not differ significantly from participating women in terms of age, religion, ethnicity, level of literacy or location of residence. All women were reimbursed for healthcare costs for themselves and the project child for the duration of the project. Any women suffering from severe mental disturbance were given money for transport and referred for assessment to the local psychiatric unit in Butajira town, staffed by two psychiatric nurses and a general practitioner.
Data collection
The project data collectors were local women with completed high-school education who worked exclusively on the P-MaMiE project and had been trained for a minimum of 1 week in questionnaire administration and anthropometric measurement. They interviewed participating women during their pregnancy and 2 months after delivery. The Butajira Rural Health Programme enumerators and traditional birth attendants obtained additional information shortly after birth.
Measures
All questionnaires were translated into Amharic and administered to the project women in their homes or surrounding area, with every attempt made to ensure privacy. Primary exposures were scales of sociocultural perinatal attitudes and discordance between attitudes and adherence. The outcome measure was the incident and persistent postnatal CMD. Symptoms of CMD were measured using the Self-Reporting Questionnaire (SRQ–20).16 This 20-item scale asks about depressive, anxiety and somatic symptoms present in the preceding month and generates a continuously distributed scale score indicating level of overall psychological morbidity. The SRQ–20 has been used in previous Ethiopian community-based studies,17 but was extensively prevalidated for use in a mixed sample of pregnant and postnatal women in the Butajira population.18 High levels of CMD symptoms were defined as a score of ≥6 on the SRQ–20.
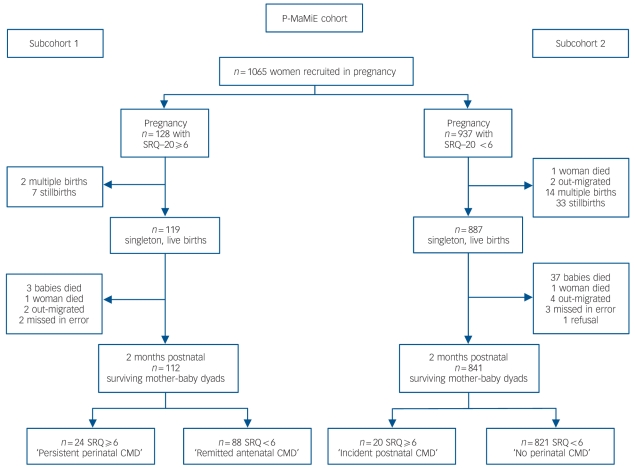
The importance of disaggregating the effects of risk factors on new-onset postnatal CMD compared with CMD persisting from the antenatal period is increasingly recognised.19 Therefore, two subcohorts of women were defined according to the number of CMD symptoms at the pregnancy time point: subcohort 1 with high antenatal CMD (SRQ–20 ≥6) and subcohort 2 with low antenatal CMD (SRQ–20 <6) (Fig. 1). High postnatal CMD symptoms were therefore divided into incident (occurring in subcohort 2; low antenatal CMD) and persistent (occurring in subcohort 1; high antenatal CMD).
Fig. 1.
Flow diagram of follow-up between pregnancy and 2-month postnatal time point for subcohorts 1 and 2 of the Perinatal Maternal Mental health in Ethiopia (P-MaMiE) cohort.
CMD, common mental disorder.
Subcohort 1: antenatal Self-Reporting Questionnaire (SRQ–20) ≥6;
Subcohort 2: antenatal SRQ–20 <6. CMD, common mental disorders.
Potential confounders
Domains of potential confounders were defined as below. All except infant gender and maternal postnatal ill health were measured at the antenatal time point. Items (h), (i) and (j) were only considered confounders for discordance between attitudes and adherence to perinatal practices.
Maternal age and parity.
Parental education.
Socioeconomic status: level of household wealth relative to others (lower v. the same or greater), experience of hunger in the preceding month due to lack of money, indebtedness, lacking the resources to survive for 1 month in the event of an emergency. Living standard was indicated with the following variables: ownership of a business, bed and radio, availability of a latrine and sanitary means for disposal of rubbish, having a window within the home. A hierarchical living standard scale of these six items was confirmed using Mokken analysis (Loevinger H coefficient 0.45).
Residence: living in Butajira town v. one of the nine rural subdistricts.
Gender disadvantage: polygamous marriage, non-consenting marriage, experiencing violence and degree of household autonomy. The latter was assessed by asking whether the woman had to ask her husband before she was able to sell crops, spend household money, attend meetings, purchase medications for herself or her children, attend a health facility. Responses to the five categories were summed and recategorised as follows: always has to ask, sometimes asks, never asks.
Antenatal CMD: SRQ–20 score.
Social support: frequency of contact with family and friends (dichotomised as monthly or less v. at least weekly), received insufficient help from family and with housework.
Marital discord: husband not providing enough help, relationship ‘average, bad or very bad’ (compared with good or very good), sometimes or often quarrel and perceiving that the husband drank too much alcohol. A marital discord scale of these four items was confirmed using Mokken analysis (Loevinger H coefficient 0.35).
Maternal nutritional status: body mass index (kg/m2) was calculated from anthropometric measurements in antenatal women, adjusted for gestational age at recruitment.
Maternal ill health: episodes of diarrhoea or malaria in 2 months since birth. For obstetric complications, a composite variable was created by summing responses to the following: instrumental or operative delivery, duration of labour greater than 24 h, bleeding after delivery and fever after delivery. The resulting scale was then categorised according to number of complications: zero, one, two or more.
Data analysis
Analyses were conducted using Stata/SE version 10.1 for Windows. Association with the potential confounding variables was evaluated for each perinatal practices scale: proportional odds ordinal regression for discordant attitudes and adherence scales, linear regression for the sociocultural perinatal attitudes scale. Chi-squared test-for-trend was reported for ordered categories. Exploratory multiple linear regression was conducted to identify variables independently associated with sociocultural attitudes score.
Multivariable logistic regression analysis was hypothesis-driven, presenting the association between (a) sociocultural attitudes scale, (b) discordant attitudes and adherence scales and the outcomes of incident and persistent postnatal CMD, adjusted for separate groups of confounders as defined above and, finally, with all potential confounders added simultaneously into the fully adjusted model.
The sample size was determined to address objectives of the P-MaMiE project other than those addressed within this paper.
Results
Hierarchical scales of attitudes and adherence
Sociocultural perinatal practices were endorsed by the majority of project women (Table 1). Analyses were conducted on the 954 women with singleton babies surviving to the 2-month time point. Mokken analysis indicated that 10 of the 13 items measuring antenatal attitudes towards different perinatal practices formed an acceptable hierarchical scale with a Loevinger H coefficient of 0.38 (sociocultural attitudes scale). Summing the items gave a scale with a median score of 8 (25th centile 6, 75th centile 10).
Discordance between a woman’s antenatal endorsement of a practice and whether she had actually carried out the practice postnatally is shown in Table 1. Mokken analysis for these discordant items supported two hierarchical scales, discordant protective (three item; Loevinger H coefficient 0.35) and discordant celebratory (two item; Loevinger H coefficient 0.31). For the discordant protective scale, 742 (77.8%) of women reported no discordance, 147 (15.4%) were discordant for one protective practice, 49 (5.1%) for two and 16 (1.7%) disordant for all three. Considering the discordant celebratory scale, 493 (51.7%) of women reported no discordance, 369 (38.7%) were discordant for one celebratory practice and 91 (9.6%) for both.
Incident and persistent perinatal CMD
When considering all women with singleton babies surviving to the 2-month time point, follow-up rates were 96.6% (112/116) in subcohort 1 and 98.8% (842/852) in subcohort 2. High levels of prevalent postnatal CMD symptoms (SRQ ≥6) were found in 44 (4.6%) women. The proportion of women with low antenatal CMD scores (subcohort 1) having an onset of postnatal CMD (incident postnatal CMD) was 20/841 (2.4%), and the proportion of those with high antenatal CMD scores (subcohort 2) with persistent postnatal CMD was 24/112 (21.4%) (Fig. 1).
Variables associated with perinatal practices
In the multiple regression analysis, women who expressed positive attitudes towards perinatal practices (high scores on the sociocultural attitudes scale) were more likely to be Muslim and multiparous, and to have no formal education, a poorer living standard, to have been hungry in the preceding month and to have less autonomy in the home (online Table DS1). However, positive attitudes towards perinatal practices were also less likely to be associated with poor social support, being in debt or non-consenting marriage. Protestant women were significantly less likely to endorse the perinatal sociocultural practices.
Being discordant for celebratory practices was associated with worse socioeconomic status and living standards, older maternal age, higher parity, neither parent having received formal education, higher levels of antenatal CMD symptoms, higher levels of marital discord, being more likely to have been married without consent, and having had a malarial episode since giving birth. However, discordance for protective practices was not associated with any of the potential confounders (Table 2).
Table 2.
Univariate proportional odds regression analysis of associations between potential confounders and score on the discordant protective and discordant celebratory scales
| Proportional odds ratio (95% CI)
|
|||||
|---|---|---|---|---|---|
| Potential confounders | n (%) | Mean (s.d.) | Median (IQR) | Discordant protective scale (0–3) | Discordant celebratory scale (0–2) |
| Maternal age, years
|
26.9 (6.3)
|
0.98 (0.95–1.00)
|
1.03 (1.01–1.06)
|
||
| Parity | |||||
| Primiparous | 138 (14.5) | Referencea | Referencea | ||
| 2–4 births | 423 (44.4) | 1.03 (0.66–1.61) | 1.91 (1.28–2.84) | ||
| 5 or more
|
392 (41.1)
|
0.83 (0.52–1.32)
|
2.44 (1.64–3.64)
|
||
| No maternal education
|
762 (80.0)
|
0.94 (0.65–1.37)
|
1.67 (1.22–2.29)
|
||
| No paternal education
|
349 (36.9)
|
0.87 (0.63–1.20)
|
1.40 (1.09–1.81)
|
||
| Living standard scale (0–6)
|
1.85 (1.4)
|
1.04 (0.93–1.16)
|
0.81 (0.74–0.89)
|
||
| Lower relative wealth
|
539 (56.7)
|
1.02 (0.75–1.39)
|
1.28 (1.00–1.65)
|
||
| Indebted
|
79 (8.3)
|
1.37 (0.83– 2.27)
|
1.16 (0.74–1.81)
|
||
| Hungry in last month
|
152 (16.0)
|
0.75 (0.48–1.17)
|
1.62 (1.17–2.25)
|
||
| No emergency resources
|
528 (55.5)
|
1.01 (0.75–1.38)
|
1.57 (1.22–2.01)
|
||
| Rural
|
818 (85.8)
|
0.87 (0.56–1.33)
|
1.41 (0.98–2.03)
|
||
| Autonomy level | |||||
| Lowest | 613 (64.8) | Referenceb | Referenceb | ||
| Middle | 188 (19.9) | 1.03 (0.70–1.53) | 0.81 (0.59–1.11) | ||
| Highest
|
145 (15.3)
|
1.23 (0.81–1.87)
|
1.07 (0.76–1.52)
|
||
| Polygamous marriage
|
173 (18.3)
|
0.99 (0.66–1.47)
|
1.28 (0.93–1.76)
|
||
| Antenatal violence
|
22 (2.3)
|
0.33 (0.08–1.44)
|
1.34 (0.59–3.01)
|
||
| Marriage without consent
|
176 (18.6)
|
1.17 (0.80–1.70)
|
1.48 (1.09–2.02)
|
||
| Self-Reporting Questionnaire (SRQ–20) score
|
2 (4)
|
0.97 (0.92–1.02)
|
1.07 (1.03–1.11)
|
||
| Sees family ≤monthly
|
282 (29.6)
|
1.07 (0.77–1.49)
|
1.73 (1.33–2.26)
|
||
| Sees friends ≤monthly
|
230 (24.1)
|
1.04 (0.73–1.48)
|
0.92 (0.69–1.23)
|
||
| Not enough help from family
|
189 (19.8)
|
0.59 (0.39–0.90)
|
1.48 (1.09–2.01)
|
||
| Not enough help at home
|
578 (60.7)
|
1.01 (0.74–1.38)
|
1.03 (0.80–1.33)
|
||
| Scale (0–4)
|
271 (28.7)
|
0.96 (0.79–1.16)
|
1.28 (1.10–1.49)
|
||
| Body mass index in pregnancy, kg/m2 |
21.7 (2.3)
|
0.99 (0.92–1.05)
|
0.96 (0.91–1.02)
|
||
| Obstetric complications | |||||
| 0 | 330 (35.9) | Referencec | Referencec | ||
| 1 | 319 (34.7) | 1.15 (0.80–1.65) | 1.08 (0.81–1.46) | ||
| ≥2
|
270 (29.4)
|
1.00 (0.68–1.46)
|
0.98 (0.72–1.34)
|
||
| Diarrhoeal episodes
|
55 (5.8)
|
1.31 (0.71–2.40)
|
1.35 (0.79–2.29)
|
||
| Malarial episodes
|
125 (13.2)
|
1.21 (0.79–1.86)
|
1.60 (1.11–2.29)
|
||
| Girl | 468 (49.1) | 0.85 (0.63–1.16) | 0.85 (0.66–1.09) | ||
IQR, interquartile range.
a. Parity: test for trend (a) discordant protective χ21 = 1.21, P = 0.2712; (b) discordant celebratory χ21 = 17.79, P<0.0001.
b. Autonomy: test for trend (a) discordant protective χ21 = 0.80, P = 0.3702; (b) discordant celebratory χ21 = 0.01, P = 0.9258.
c. Obstetric complications: test for trend (a) discordant protective χ21 = 0.00, P = 0.9697; (b) discordant celebratory χ21 = 0.01, P = 0.9286.
Perinatal traditions and postnatal CMD
Sociocultural attitudes scale
In the univariate analysis, scores on the sociocultural attitudes scale were not associated with incident postnatal CMD (OR = 1.11, 95% CI 0.87–1.40; Table 3). When adjusting for groups of confounders, there was evidence of negative confounding by socioeconomic status, gender disadvantage and antenatal CMD symptoms but the association remained marginally non-significant (adjusted OR = 1.36, 95% CI 0.99–1.86). In contrast, higher sociocultural attitudes scores were protective against persistence of antenatal CMD into the postnatal period in both the crude (OR = 0.81, 95% CI 0.64–1.02) and fully adjusted (adjusted OR = 0.66, 95% CI 0.45–0.95) analyses (Table 4).
Table 3.
Adjusted odds ratio for association between (a) antenatal sociocultural attitudes scale, (b) discordant protective and (c) discordant celebratory perinatal practice scales, and incident postnatal common mental disorder (CMD)
| Odds ratio (95%CI)
|
|||
|---|---|---|---|
| Odds ratio for incident postnatal CMD | Sociocultural attitudes scale | Discordant protective scale | Discordant celebratory scale |
| Crude odds ratio
|
1.11 (0.87–1.40)
|
1.84 (1.15–2.96)
|
0.87 (0.43–1.75)
|
| Adjusted separately for each set of potential confounders | |||
| Maternal characteristics | 1.10 (0.87–1.40) | 1.85 (1.15–2.98) | 0.84 (0.41–1.71) |
| No parental formal education | 1.11 (0.87–1.41) | 1.84 (1.15–2.96) | 0.86 (0.42–1.75) |
| Poor socioeconomic status | 1.16 (0.91–1.48) | 1.83 (1.11–3.02) | 0.79 (0.38–1.63) |
| Gender disadvantage | 1.17 (0.91–1.51) | 1.98 (1.21–3.25) | 0.84 (0.41–1.72) |
| Antenatal CMD score | 1.14 (0.90–1.45) | 2.00 (1.22–3.26) | 0.83 (0.41–1.67) |
| Poor social support | 1.12 (0.88–1.43) | 2.00 (1.21–3.30) | 0.94 (0.46–1.89) |
| Poorer marital relationship | – | 1.86 (1.16–2.98) | 0.86 (0.42–1.74) |
| Antenatal maternal body mass index, kg/m2 | – | 1.91 (1.18–3.09) | 0.90 (0.45–1.82) |
| Maternal ill health | – | 1.81 (1.10–2.98) | 0.78 (0.38–1.59) |
| Baby's gender
|
–
|
1.84 (1.14–2.95)
|
0.86 (0.43–1.74)
|
| Fully adjusted odds ratioa | 1.36 (0.99–1.86) | 2.16 (1.11–4.23) | 0.78 (0.35–1.76) |
a. Sociocultural attitudes scale: n = 813; discordant protective scale: n = 791; discordant celebratory scale: n = 791.
Table 4.
Adjusted odds ratios for association between (a) antenatal sociocultural attitudes scale, (b) discordant protective and (c) discordant celebratory perinatal practice scales, and persistent perinatal common mental disorder (CMD)
| Odds ratio (95%CI)
|
|||
|---|---|---|---|
| Odds ratio for persistent postnatal CMD | Sociocultural attitudes scale | Discordant protective scale | Discordant celebratory scale |
| Crude odds ratio | 0.81 (0.64–1.02) | 2.08 (1.02–4.24) | 2.42 (1.20–4.88) |
| Adjusted separately for each set of potential confounders | |||
| Maternal characteristics | 0.81 (0.64–1.02) | 2.01 (0.97–4.14) | 2.41 (1.16–4.99) |
| No parental formal education | 0.80 (0.63–1.02) | 2.21 (1.07–4.57) | 2.56 (1.26–5.22) |
| Poor socioeconomic status | 0.76 (0.58–0.99) | 3.09 (1.30–7.33) | 2.80 (1.31–6.00) |
| Gender disadvantage | 0.81 (0.63–1.04) | 1.82 (0.87–3.84) | 2.37 (1.10–5.09) |
| Antenatal CMD score | 0.81 (0.63–1.03) | 1.83 (0.86–3.88) | 2.22 (1.08–4.56) |
| Poor social support | 0.80 (0.62–1.02) | 2.44 (1.09–5.45) | 2.32 (1.13–4.78) |
| Poor marital relationship | – | 2.08 (1.01–4.26) | 2.48 (1.20–5.15) |
| Antenatal maternal body mass index, kg/m2 | – | 1.89 (0.92–3.89) | 2.56 (1.25–5.25) |
| Maternal ill health | – | 2.06 (0.98–4.32) | 2.70 (1.25–5.82) |
| Baby's gender
|
–
|
1.82 (0.87–3.81)
|
2.60 (1.23–5.50)
|
| Fully adjusted odds ratioa | 0.66 (0.45–0.95) | 4.26 (0.80–22.67) | 7.26 (1.38–38.04) |
a. Sociocultural attitudes scale: n = 103; discordant protective scale: n = 104; discordant celebratory scale: n = 104.
Discordant protective scale
Women with higher scores on the discordant protective scale, indicating that they were unable to complete protective practices that had been endorsed antenatally, were more likely to have both incident (OR = 1.84, 95% CI 1.15–2.96) and persistent (OR = 2.08, 95% CI 1.02–4.24) postnatal CMD in the univariate analyses. In the final fully adjusted model, higher levels of discordance for protective practices remained significantly associated with incident CMD (adjusted OR = 2.16, 95% CI 1.11–4.23) but not persistent (adjusted OR = 4.26, 95% CI 0.80–22.67) postnatal CMD. The latter appeared to be negatively confounded by gender disadvantage, maternal ill health and obstetric complications.
Discordant celebratory scale
Higher levels of discordance for celebratory practices were associated with persistent perinatal CMD in both the crude (OR = 2.42, 95% CI 1.20–4.88) and fully adjusted (adjusted OR = 7.26, 95% CI 1.38–38.04) analyses. There was no association with incident postnatal CMD.
Discussion
Building on findings from our qualitative study, we set out to investigate the relationship between perinatal sociocultural practices and onset or persistence of postnatal CMD in a large, population-based cohort in rural Ethiopia. With regard to our first hypothesis, more positive antenatal attitudes towards perinatal practices were not associated with a lower incidence of postnatal CMD. Expressing more traditional sociocultural attitudes was, however, associated with lower odds of antenatal CMD persisting into the postnatal period. In keeping with the second hypothesis, women who endorsed protective practices antenatally but did not complete them postnatally had a twofold increase in the odds of incident postnatal CMD. Likewise, women who endorsed celebratory practices but did not carry them out had a sevenfold increase in the odds of antenatal CMD persisting into the postnatal period.
Sociocultural attitudes and discordant practices
Not all of the maternal characteristics associated with endorsement of traditional attitudes were as expected. Higher scores on the sociocultural attitudes scale were associated with lower perception of poor social support. The inverse association between high traditional attitude and indebtedness might be as a result of a prohibition against borrowing money among more traditional women, although it could also reflect the relative lack of opportunity for poorer women to borrow money. The negative association with non-consenting marriage might indicate that traditional structures have a role to play in protecting women, although an alternative explanation is reporting bias because of the reluctance of more traditional women to discuss their marital status. Even though the qualitative study included stakeholders from all the major religions present in Butajira, the sociocultural practices chosen for inclusion in our questionnaire may have biased towards those favoured by the majority religion: Islam.
Discordance between antenatal attitudes towards celebratory postnatal practices, namely receiving gifts and the husband slaughtering an animal, were associated with a number of indicators of poor socioeconomic status, marital discord and gender disadvantage. As these postnatal practices depend on wealth and the cooperation of the woman’s husband this is perhaps not surprising. Likewise the absence of any association between discordance for protective postnatal practices and the variables under consideration is understandable. Even without the support of her husband or the need for expenditure, most postnatal women would have been able to complete the practices of carrying metal, speaking softly and avoiding draughts of air, if minded to do so.
Hypothesis 1: sociocultural attitudes and postnatal CMD
Contrary to our hypothesis, there was no protective effect of traditional attitudes on incident postnatal CMD. Indeed, the trend was in the opposite direction (OR = 1.36, 95% CI 0.99–1.86). From our previous qualitative work,10 participants identified that adhering to postnatal confinement and other sociocultural practices might be associated with mental ill health if coupled with poverty and gender disadvantage, for example, by confining a woman to an abusive home and separating her from potential sources of support. In pregnancy, women have more freedom to meet with others and earn small amounts of money, whereas postnatally they become dependent on their husband and immediate family (usually in-laws) to meet their needs. Any mental health benefits of a more traditional outlook expressed in pregnancy might therefore be offset by the negative impact of postnatal restrictions.
The small number of postnatal cases of CMD may have limited the power of the study to find a true association with incident postnatal CMD. An alternative explanation for the difference in associations with incident and persistent postnatal CMD could relate to the nature of antenatal CMD. In our previous qualitative work, threats to mental health in pregnancy were reported by participants as largely relating to fear of childbirth and the physical burden of pregnancy in women weakened by poverty and ill health.20 This may explain our observation that most women with high antenatal CMD symptoms remitted postnatally (78.6%). This high remission rate for antenatal CMD is very similar to that identified in Nigeria21 and Uganda.22 Having safely negotiated childbirth, more traditionally minded women who had experienced high levels of CMD symptoms in pregnancy may have better psychological adjustment to the demands of the postnatal period, leading to remission of symptoms. The perception of better social support in more traditional women may be an important factor.
Hypothesis 2: discordant perinatal practices and postnatal CMD
Discordance between endorsing protective practices antenatally and carrying them out postnatally was associated with increased odds of both incident and persistent postnatal CMD, but for persistent CMD the association was only seen in the univariate analysis. In the fully adjusted model, the size of the adjusted odds ratio actually increased but the confidence interval became very wide, indicating that we were underpowered to detect an effect. Discordance for celebratory practices was only associated with persistent postnatal CMD. Negative recall bias cannot be excluded as an explanation for the association with postnatal CMD. Furthermore, we cannot rule out reverse causality, that women with postnatal CMD were less likely to complete postnatal practices and not vice versa.
Few studies have previously attempted to take into account women’s attitudes towards postnatal practices,23,24 and we were unable to find any other studies that had prospectively explored this issue. Chee et al24 reported that Singaporean women who reported a negative confinement experience were more likely to be postnatally depressed, but this may have been because of negative recall bias in the women with depression. In Chinese migrants to Australia, 18% of women expressed ambivalence about carrying out postnatal practices but the sample size was too small to meaningfully examine the association with postnatal depression.23
Our measure of discordance approximates to Dressler’s concept of cultural dissonance. Individuals are said to be culturally consonant if their own behaviours approximate widely shared cultural models.25 When the individual is unable to adhere to these cultural values, for whatever reason, cultural dissonance results and has been shown to be associated with poorer health outcomes, including depression.26 The greater the consensus in a cultural domain, the more strongly cultural dissonance is said to favour development of depression.25 This may partly explain the less robust association with postnatal CMD arising from discordance for celebratory rather than protective practices. The celebratory practice scale included slaughtering an animal in celebration. This item was, however, the most commonly non-completed postnatal practice (41.8%), probably because of the prohibitive cost for this population. Women’s expectations of an animal actually being slaughtered in celebration of birth may therefore have been lower, even though they endorsed this as a desirable tradition. An ethnographic study from Fiji suggests another possible interpretation.27 The postnatal sociosomatic syndrome of na tadoka ni vasucu is conceptualised as embodying any affront to the social and moral order that holds dear the need for extra care for vulnerable postnatal women. In Fiji, identification of the disorder provoked a social reaction, with, for example, additional support and care mobilised in order to rectify the breach. The latter was not evident in Ethiopia. Further qualitative work has been carried out with the purpose of understanding conceptualisations of postnatal CMD in Ethiopia and will hopefully shed light on these findings.
In our study it was not just those postnatal rituals that mobilise care and support that seemed important for mental health in the Butajira setting. Even after adjusting for women’s perceptions of poor social support from family, friends (and neighbours) and their husband, discordance for protective practices that relied on individual actions alone and for celebrations of her role transition remained associated with poorer postnatal mental health. This is in contrast to the findings in Hong Kong women5 where the association between completing the traditional period of confinement, peiyue, and postnatal depression became non-significant after adjusting for relationship difficulties with the mother-in-law.
Prevalence of perinatal CMD
The SRQ–20 has been shown to be a valid measure of postnatal CMD in Ghana,28 Malawi29 and Ethiopia.18 Although the moderate sensitivity and specificity of the SRQ–20 for detection of postnatal CMD raise the possibility of misclassification, the cut-off of 6 or more was lower than that used in most previous Ethiopian studies making under-ascertainment less likely.17
Although our prevalence estimate for postnatal CMD was lower than anticipated, it is difficult to know whether this is atypical for a rural African setting because of the dearth of comparable studies. We were only able to identify one population-based rural study, from Ghana, where the prevalence of postnatal CMD was 9.6%.28 Two other community-based studies were conducted in urban South Africa: in a settlement characterised by high levels of violence, the prevalence of DSM–IV-defined depressive disorder was 34.7%;30 in another urban setting using a CMD symptom scale, the prevalence was 16.4%.31 Among clinic-based studies of postnatal CMD in sub-Saharan Africa, three studies give comparable estimates of prevalence to our study: 6.1% in Nigeria,32 3.5% in Zambia33 and 6.1% in Uganda.34 The low prevalence of postnatal CMD in rural Ethiopia may reflect the high level of endorsement and adherence to sociocultural perinatal practices observed in our study.
Implications
Butajira is a rural Ethiopian society in transition, with increasing out-migration of the labour force, changing economic opportunities and improving connections to the capital city.35 The ability of women to adhere to widely endorsed sociocultural practices could be being undermined by socioeconomic exigencies and gender disadvantage.35,36 Our study indicates that such changes may be detrimental to women’s postnatal mental health.
Funding
This study was funded through a Wellcome Trust research training fellowship for C.H. (GR071643).
Acknowledgments
The authors gratefully acknowledge all the women who gave up their time to participate in this study, and for all assistance received from the staff of the Butajira Rural Health Programme.
Declaration of interest
None.
References
- 1.Stern G, Kruckman L. Multi-disciplinary perspectives on post-partum depression: an anthropological critique. Soc Sci Med 1983; 17: 1027–41. [DOI] [PubMed] [Google Scholar]
- 2.Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord 2006; 91: 97–111. [DOI] [PubMed] [Google Scholar]
- 3.O’Hara MW, Swain AM. Rates and risk of postpartum degression – a meta-analysis. Int Rev Psychiatry 1996; 8: 37–54. [Google Scholar]
- 4.Ho-Yen SD, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Factors associated with depressive symptoms among postnatal women in Nepal. Acta Obstet Gynaecol Scand 2007; 86: 291–7. [DOI] [PubMed] [Google Scholar]
- 5.Lee DTS, Yip ASK, Leung TYS, Chung TKH. Ethnoepidemiology of postnatal depression. Prospective multivariate study of sociocultural risk factors in a Chinese population in Hong Kong. Br J Psychiatry 2004; 184: 34–40. [DOI] [PubMed] [Google Scholar]
- 6.Teng H-W, Hsu C-S, Shih S-M, Lu M-L, Pan J-J, Shen WW. Screening postpartum depression with the Taiwanese version of the Edinburgh Postnatal Depression Scale. Compr Psychiatry 2005; 46: 261–5. [DOI] [PubMed] [Google Scholar]
- 7.Fisher JRW, Morrow MM, Ngoc NTN, Anh LTH. Prevalence, nature, severity and correlates of postpartum depressive symptoms in Vietnam. Br J Obstet Gynaecol 2004; 111: 1353–60. [DOI] [PubMed] [Google Scholar]
- 8.Grace J, Lee KK, Ballard C, Herbert M. The relationship between post-natal depression, somatization and behaviour in Malaysian women. Transcult Psychiatry 2001; 38: 27–34. [Google Scholar]
- 9.Chan SW, Levy V, Chung TK, Lee D. A qualitative study of the experiences of a group of Hong Kong Chinese women diagnosed with postnatal depression. J Adv Nurs 2002; 39: 571–9. [DOI] [PubMed] [Google Scholar]
- 10.Hanlon C, Whitley R, Wondimagegn D, Alem A, Prince M. Postnatal mental distress in relation to the sociocultural practices of childbirth: an exploratory qualitative study from Ethiopia. Soc Sci Med 2009; 69: 1211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berhane Y, Wall S, Kebede D, Emmelin A, Enqueselassie F, Byass P, et al. Establishing an epidemiological field laboratory in rural areas – potentials for public health research and interventions. The Butajira Rural Health Programme 1987–99. (Special Issue). Ethiopian J Health Dev 1999; 13: 1–47. [Google Scholar]
- 12.Berhane Y, Andersson T, Wall S, Byass P, Hogberg U. Aims, options and outcomes in measuring maternal mortality in developing societies. Acta Obstet Gynaecol Scand 2000; 79: 968–72. [PubMed] [Google Scholar]
- 13.Central Statistical Authority (Ethiopia) and ORC Macro. Ethiopia Demographic and Health Survey 2005. Central Statistical Authority and ORC Macro, 2006.
- 14.Mokken RJ. A Theory and Procedure of Scale Analysis. Mouton, 1971.
- 15.Watson R, Deary IJ, Shipley B. A hierarchy of distress: Mokken scaling of the GHQ-30. Psychol Med 2008; 38: 575–9. [DOI] [PubMed] [Google Scholar]
- 16.Beusenberg M, Orley J. A User’s Guide to the Self-Reporting Questionnaire (SRQ). World Health Organization, 1994.
- 17.Alem A, Kebede D, Woldesemiat G, Jacobsson L, Kullgren G. The prevalence and socio-demographic correlates of mental distress in Butajira, Ethiopia. Acta Psychiatr Scand Suppl 1999; 397: 48–55. [DOI] [PubMed] [Google Scholar]
- 18.Hanlon C, Medhin G, Alem A, Araya M, Abdulahi A, Hughes M, et al. Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J Affect Disord 2008; 108: 251–62. [DOI] [PubMed] [Google Scholar]
- 19.Chandran M, Tharyan P, Muliyil J, Abraham S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry 2002; 181: 499–504. [DOI] [PubMed] [Google Scholar]
- 20.Hanlon C, Whitley R, Wondimagegn D, Alem A, Prince M. Between life and death: exploring the sociocultural context of antenatal mental distress in rural Ethiopia. Arch Women Ment Health 2010; February 11 (Epub ahead of print). [DOI] [PMC free article] [PubMed]
- 21.Aderibigbe YA, Gureje O, Omigbodun O. Postnatal emotional disorders in Nigerian women. A study of antecedents and associations. Br J Psychiatry 1993; 163: 645–50. [DOI] [PubMed] [Google Scholar]
- 22.Cox JL. Postnatal depression: a comparison of African and Scottish women. Soc Psychiatry 1983; 18: 25–8. [DOI] [PubMed] [Google Scholar]
- 23.Matthey S, Panasetis P, Barnett B. Adherence to cultural practices following childbirth in migrant Chinese women and relation to postpartum mood. Health Care Women Int 2002; 23: 567–75. [DOI] [PubMed] [Google Scholar]
- 24.Chee CYI, Lee DTS, Chong YS, Tan LK, Ng TP, Fones CSL. Confinement and other psychosocial factors in preinatal depression: a transcultural study in Singapore. J Affect Disord 2005; 89: 157–66. [DOI] [PubMed] [Google Scholar]
- 25.Dressler WW, Baleiro MC, Ribeiro RP, dos Santos JE. Cultural consonance and psychological distress: examining the associations in multiple cultural domains. Cult Med Psychiatry 2007; 31: 195–224. [DOI] [PubMed] [Google Scholar]
- 26.Dressler WW, Balieiro MC, Ribeiro RP, dos Santos JE. A prospective study of cultural consonance and depressive symptoms in urban Brazil. Soc Sci Med 2007; 65: 2058–69. [DOI] [PubMed] [Google Scholar]
- 27.Becker AE. Postpartum illness in Fiji: a sociosomatic perspective. Psychosom Med 1998; 60: 431–8. [DOI] [PubMed] [Google Scholar]
- 28.Weobong B, Akpalu B, Doku V, Owusu-Agyei S, Hurt L, Kirkwood B, et al. The comparative validity of screening scales for postnatal common mental disorder in Kintampo, Ghana. J Affect Disord 2008; 113: 109–17. [DOI] [PubMed] [Google Scholar]
- 29.Stewart RC, Kauye F, Umar E, Vokhiwa M, Bunn J, Fitzgerald M, et al. Validation of a Chichewa version of the Self-Reporting Questionnaire (SRQ) as a brief screening measure for maternal depressive disorder in Malawi, Africa. J Affect Disord 2008; 112: 126–34. [DOI] [PubMed] [Google Scholar]
- 30.Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Post-partum depression and the mother–infant relationship in a South African peri-urban settlement. Br J Psychiatry 1999; 175: 554–8. [DOI] [PubMed] [Google Scholar]
- 31.Ramchandani PG, Richter LM, Stein A, Norris SA. Predictors of postnatal depression in an urban South African cohort. J Affect Disord 2009; 113: 279–84. [DOI] [PubMed] [Google Scholar]
- 32.Adewunmi AB. Psychiatric morbidity in mothers attending maternal and child health clinics in Abeokuta, Nigeria. West Afr J Med 1991; 10: 383–9. [PubMed] [Google Scholar]
- 33.Collin SM, Chisegna MM, Kasonka L, Haworth A, Young C, Filteu S, et al. Factors associated with postpartum physical and mental morbidity among women with known HIV status in Lusaka, Zambia. AIDS Care 2006; 18: 812–20. [DOI] [PubMed] [Google Scholar]
- 34.Nakku JEM, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. Afr Health Sci 2006; 6: 207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berhane Y, Gossaye Y, Emmelin M, Hogberg U. Women’s health in a rural setting in societal transition in Ethiopia. Soc Sci Med 2001; 53: 1525–39. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi–country study on women’s health and domestic violence. Lancet 2006; 368: 1260–9. [DOI] [PubMed] [Google Scholar]