Abstract
Background
The development of valid parent-report measures of symptom change in pediatric bipolar disorder (PBD) is imperative to evaluating the effectiveness of different treatment approaches; yet, few studies have tested the sensitivity of symptom measures. The current study evaluated the sensitivity of the Child Mania Rating Scale (CMRS-P) to detect symptom change over time in a treatment study for PBD.
Methods
Data on symptom change was drawn from a prospective six-week, double-blind, placebo-controlled, randomized outpatient medication treatment trial of risperidone versus divalproex. The sample included 66 children with Bipolar type I disorder. Measures were administered every week for six weeks of treatment.
Results
The CMRS-P demonstrated statistically (p<.05) and clinically significant change in symptom report from pre to post-test. Growth curve modeling indicated that the CMRS-P demonstrated overall similarity to the YMRS in the magnitude and trajectory of change over time. Finally, results indicate that the CMRS-P is able to detect response rates with moderate levels of agreement with other measures.
Limitations
Limitations of this study include a relatively small sample size and uncertain generalizability beyond treatment trials.
Conclusions
The CMRS-P is short, easy to administer, and represents parent's report of symptoms, all strengths which make it a compelling treatment outcome tool. This preliminary evidence of its validity as a treatment outcome measure makes it applicable in other research settings and suggests its potential use in clinical settings.
Keywords: Bipolar Disorder, Pediatric, Treatment, Measure Sensitivity, Mania
Introduction
Pediatric bipolar disorder (PBD) is a serious psychiatric disorder, and is associated with debilitating symptoms and functional impairment (American Psychiatric Association, 1994). The symptom presentation of PBD is characterized by significant episodic mood lability, mixed mood states, high rates of comorbidity, and rapid cycling, which distinguish the early-onset pediatric phenotype from its adult-onset counterpart (Pavuluri, Birmaher & Naylor, 2005). PBD is also characterized by a chronic and refractory course, low recovery, and high relapse rates (Geller, Craney, Bolhofner, DelBello, Axelson, Luby, et, al, 2003), which places a significant strain on parents and providers alike. Even with the highest quality evidence-based approaches, response to treatment is notoriously poor. As promising interventions continue to be developed and tested, the valid measurement of degree of change becomes critical. In particular, measuring symptom change from a parents' perspective is essential, as they have the primary caretaking responsibility for their child and are optimally positioned to observe changes over time with treatment. Currently, there are no studies examining the psychometric properties of current symptom measures in evaluating symptom change associated with treatment in PBD.
Pharmacotherapy is the cornerstone of treatment for pediatric mania. The development of valid and sensitive pharmacotherapy treatment outcome measures for manic symptoms is imperative in evaluating the effectiveness of any specific medication. However, there are various barriers to accurately assessing symptom changes in PBD. First, a core feature of PBD is rapidly fluctuating mood states. Children with PBD fluctuate frequently between being irritable, sad, excitable, and elated in mood. Second, mood states tend to vary by environmental context and the presence or absence of key triggers for mood variation. These triggers are often better understood and observed by parents who see the child across multiple contexts. Third, PBD is a chronic and refractory disorder. Even when children's symptoms are effectively addressed initially, breakthrough and residual symptoms can occur with some frequency over the course of treatment. It becomes important to have accurate measures of the extent of symptoms over time to differentiate residual symptoms from acute episodes meeting full criteria. Finally, children with PBD have high rates of comorbid disorders, including Attention Deficit Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD), and anxiety disorders. Comorbid symptoms, particularly those associated with ADHD, can be difficult to distinguish from PBD. This complex clinical presentation of PBD indicates the importance of developing measures that can effectively discriminate the profiles of PBD and ADHD.
These barriers to assessing symptom change associated with treatment in pediatric mania indicate that optimal treatment outcome measurement would incorporate multiple informants who could capture the child's functioning over time and across various contexts, would accurately distinguish gradations of severity in symptom experience, and would differentiate mania symptoms from co-occurring symptoms, especially ADHD. In particular, parent reports are essential as parents observe their children for extended time periods and across many contexts, which may enable them to integrate data pertinent to the child's overall level of functioning.
In addition, research evidence suggests that parent-report measures may be the most accurate in assessing pediatric mania. Youngstrom and colleagues (2005) conducted a review of the current screening measures for pediatric mania and concluded that parent reports (which are most often mother reports) have higher diagnostic accuracy than either child or teacher reports, and that additional reporters add little utility beyond parent report. However, the authors noted that the overall predictive validity of parent-rated instruments was still modest, and thus, these measures continue to need improvement (Youngstrom, Findling, Youngstrom, & Calabrese, 2005). Currently, the commonly used parent measures include the Child Mania Rating Scale – Parent Version (CMRS-P; Pavuluri, Henry, Devineni, Carbray, & Birmaher, 2006), the Parent Young Mania Rating Scale (P-YMRS; Gracious, Youngstrom, Findling, & Calabrese, 2002), and the Parent – General Behavior Inventory (P-GBI; Youngstrom, Findling, Youngstrom, & Calabrese, 2005). Although many of these scales have been used in treatment outcome research, none of them have been specifically tested for efficacy in measuring treatment outcomes.
Of all three measures, only the CMRS-P (Pavuluri et al., 2006) was specifically developed to address the need for a short, easily administered, comprehensive, parent-report screening and outcome measure for pediatric mania. The CMRS-P is a 21-item parent-rating scale for pediatric mania that exhibits excellent psychometric properties and accuracy in differentiating pediatric mania from ADHD. In the preliminary investigation of this measure (Pavuluri et al., 2006), the CMRS-P demonstrated excellent internal consistency reliability, high correlations with clinician-administered interview measures for diagnosing pediatric mania (rs = .78–.83), and an ability to accurately differentiate PBD from ADHD and healthy controls greater than 90% of the time. A brief form of the CMRS-P (10 items) was also developed and showed comparable accuracy in differentiating children with PBD from children with ADHD and healthy controls, compared to the long form (Brief CMRS-P; Henry, Pavuluri, Youngstrom, & Birmaher, 2008). While the CMRS-P is widely used as a diagnostic screening tool in clinical work and research, neither the long form nor the brief form has been evaluated as to its validity as a measure of symptom change with treatment.
Therefore, the current study evaluated the sensitivity of the CMRS-P (both full and brief forms) to symptom change over time with treatment. The hypotheses tested were that: (1) the CMRS-P would demonstrate sensitivity to symptom change through statistically significant change from pre-treatment to post-treatment assessment; (2) change on the CMRS-P would correlate with change on the “gold standard” YMRS suggesting concurrent validity for measuring symptoms changes; and (3) changes in symptoms over the course of treatment captured by the CMRS-P would converge with response rates from other measures. If the CMRS-P proves to be a sensitive and valid instrument to measure symptom change, its broad use as an outcome measure in PBD treatment studies would be warranted and, because of its brevity and easy administration, it could be effectively incorporated into clinical practice and research as a treatment outcome indicator. Further, if both the brief and long forms are found to be sensitive to symptom change with treatment, then providers or researchers using the scale could choose the form based on their priorities (e.g. to reduce reporting burden on parents vs. acquire comprehensive symptom assessment).
Methods
Design
Data for this study were collected as part of a prospective six-week double-blind, placebo-controlled, randomized outpatient medication treatment trial of risperidone vs. divalproex for manic episodes in children with PBD. The CMRS-P was administered weekly for six weeks of treatment so that both the magnitude and trajectory of symptom change over time could be examined. In addition, changes noted on the CMRS-P were compared with changes on the gold-standard clinician-rated Young Mania Rating Scale (YMRS) and the Clinical Global Impressions Severity Scale for Bipolar Disorder (CGI-BP) to assess correspondence between the measures of symptom change. Finally, we examined the convergence of the three mania measures in predicting treatment response. This study was approved by the University of Illinois at Chicago (UIC) Institutional Review Board.
Sample
Participants in this study were recruited from our Pediatric Mood Disorders Program. All participants included in the study had a DSM-IV diagnosis of Bipolar disorder Type I (mixed or manic episode); were 8 to 18 years of age at baseline; and were medication-free or clinically unstable on medication. Parents of participants consented for their children to be washed out of their current medications at study entry. Potential participants were excluded if they demonstrated active substance abuse measured by a urine drug screen, had serious medical problems, had a history of allergy to risperidone or divalproex, or if they had autism or non-affective psychotic disorders.
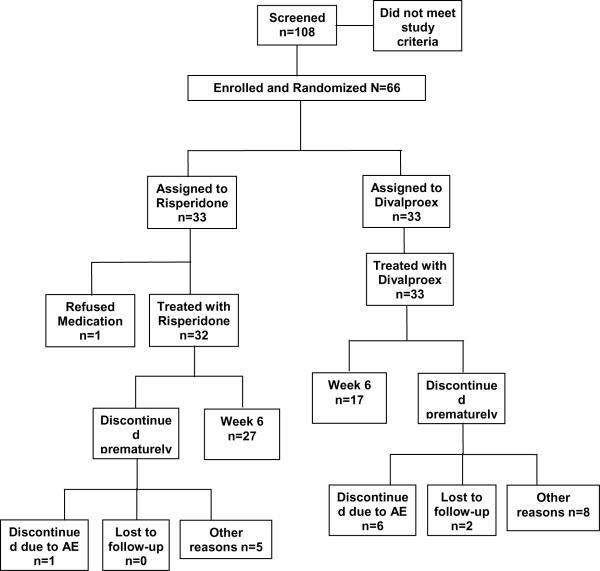
One-hundred and eight potential subjects were initially screened to obtain a sample of 66 participants who were randomized to treatment conditions. Sixty-five participants received at least one week of treatment and 43 completed 6 weeks (see Chart 1 for details). Details about the effect of missing data on outcomes are summarized elsewhere (Pavuluri, Henry, Findling, Parnes, Carbray, Mohammed, et al., in press), but in sum, the ITT sample was comparable to those who completed the study. The mean age of the participants was 10.85 years old (SD=3.34) and 40 (60.6%) were male. The ethnic composition of the sample was 58% Caucasian, 14% African-American, 2% Hispanic, and 26% other or unknown. Thirty-five percent had a mixed episode at baseline and 65% had a manic episode at baseline. Fifty-two (79%) had rapid cycling, 12 (18%) had comorbid ADHD, and 5 (8%) had comorbid anxiety disorders.
Chart 1.
CONSORT Chart of the Patient Flow in the Randomized Trial of Risperidone Versus Divalproex in Pediatric Bipolar Disorder
Treatment
The study medications were administered in a double-blind, double-dummy (placebo and active medication were made to look identical) randomized manner by our investigational pharmacist. Investigational staff involved in rating efficacy and safety measures, parents, caregivers and subjects were blind to the medication received. A full description of the study including medication dosing can be obtained from the original article (Pavuluri, et al, in press).
Assessment Procedures
All patients underwent a standard diagnostic evaluation. Each child and the parent or legal guardian were interviewed using the Washington University in St. Louis Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS; Geller, Zimerman, Williams, & Frazier, 1994, revised 1996) and episodes are defined using the Kiddie-Sads-Present and Lifetime Version (K-SADS-PL; Kaufman, et. al, 1997). Both WASH-U-KSADS and parts of KSADS-PL on episodes interviews were completed by trained physicians or other doctoral-levels clinicians and high inter-rater reliability was established (Cohen's kappa = .94).
Treatment Outcome Measurement
Mania symptom severity was assessed at pre-test, post-test, and weekly during the six weeks of treatment. Three scales were used to assess mania symptoms and severity.
Young Mania Rating Scale
The YMRS is a clinician-rated measure (Young, Biggs, Ziegler, & Meyer, 1978). It is intended to measure symptoms during a manic state. The YMRS consists of 11 items, each with either 5 levels (scored 0–4) or in some cases 9 defined levels of severity (scored 0–8). The scale is designed to be administered by a trained clinician during a 15 to 20 minute interview. Severity ratings are based on the patient's subjective experience during the past 48 hours and the clinician's observations during the interview. Inter-rater reliability is .93 and concurrent validity with other mania rating scales is .77 to .89. This instrument has been validated for use with children (Youngstrom, Danielson, Findling, Gracious, & Calabrese, 2002). Scores of ≤ 12 on the Young Mania Rating Scale (YMRS) are used to define remission (Tohen, Jacobs, Grundy, McElroy, Banov, Janicak et al., 2000).
Clinical Global Impression Severity Scale for Bipolar Disorder (CGI-BP)
The CGI-BP (Spearing, Post, Leverich, Brandt, & Nolen 1997) allows the clinician to rate the severity of symptoms on dimensions of mania, depression, attention deficit/hyperactivity disorder, psychosis, and sleep difficulties, as well as overall illness severity. Scores are calculated by summing across the six subscales, each of which is rated on a Likert-type scale of 1 (not at all ill) to 7 (extremely ill). The mania rating scale from the CGI-BP was used for analyses in this study. The cutoff for remission is a CGI-BP score ≤3.
Child Mania Rating Scale (CMRS-P)
The CMRS-P is a parent mania rating scale (Henry et al., 2008; Pavuluri et al., 2006). It includes 21 items reflecting the DSM-IV criteria for a manic episode (American Psychiatric Association, 1994). Items are age-specific; each item is considered to be a problem only if it is causing impairment, a deviation from what is normative for that child's age, and has been causing a problem in the last month. Each item is answered on a four-point Likert-type scale anchored by 0 (Never/Rare), 1 (Sometimes), 2 (Often), and 3 (Very Often). Items are written at a third grade reading level and the scale takes approximately 10 to 15 minutes to complete. The CMRS-P has an internal consistency reliability of .96, has proved to be a valid assessment of mania when compared to clinician-rated scales and shows sensitivity and specificity for differentiating pediatric mania from other disorders and no disorder (Pavuluri et al., 2006). A score of 20 is considered to differentiate children with PBD from children with ADHD and healthy controls and to indicate remission from mania symptoms.
The brief form of the CMRS-P is comprised of 10 of the 21 items on the long form of the CMRS-P. The 10 items correlate strongly with the 11 unused items in the full form of the CMRS-P. Logistic analysis of the ROC curves found strong sensitivity and specificity for differentiating mania from youth with ADHD and mania from healthy controls. The validation study for the Brief CMRS-P found that a cut score of 10 had high sensitivity and specificity for differentiating pediatric mania from ADHD (Henry et al., 2008).
For the purpose of this study and in order to establish the reliability and validity of CMRS-P as an outcome measure we instructed parents to rate their children's symptoms based on the preceding week in the clinical trial.
Statistical Analysis
All the statistics presented in this study were derived from intent-to-treat analyses, that is, data from all subjects who were randomized and had at least one assessment after baseline were analyzed (Fisher, Dixon, Herson, Frankowski, Hearron, & Peace, 1990). The sensitivity of the CMRS-P to detect change over time was assessed using three different analyses. First, to assess the overall sensitivity of the CMRS-P to detect symptom change over the course of treatment, a paired samples t-test was used to test whether there was statistically significant change from pre-treatment to post-treatment on the CMRS-P, compared to the other mania measures on which significant change was found. From this analysis we computed effect sizes (Cohen's d coefficients; Cohen, 1977) for pre-post change on all mania measures, allowing a comparison of the magnitude of change on the CMRS-P and Brief CMRS-P and the other mania measures (i.e. YMRS, CGI-BP). Second, we fit joint growth curve models using all waves of data to determine how closely change as measured by the CMRS-P and Brief CMRS-P and the YMRS correlated, reasoning that closer correspondence would indicate greater sensitivity to change. The YMRS was chosen as the measure for comparison in these analyses, as it currently represents the “gold-standard” measure to assess mania symptoms. A joint growth model has significant advantages for assessing sensitivity to change. Such a model can use all waves of data in assessing sensitivity to change, yet it does not assume that the variables are measured without error. Third, we calculated the proportion of patients showing evidence of response to treatment on each measure and the association between response on the full and brief CMRS-P and response on the validity measures.
Results
Comparison of Pre- and Posttest Change
Table 1 shows the sample's mean pre- and posttest scores on each of the three mania measures. Whereas the pretest means all fell in the clinical range for mania, the post-test means for all the measures indicated remission, as evidenced by scores falling below the clinical cut-off for mania on all three measures (YMRS ≤ 12; CGI-BP Severity ≤ 3; CMRS-P ≤ 20; Brief CMRS-P ≤ 12). Repeated measure t tests (also in Table 1) were used to determine if changes from pre to posttest were statistically significant. All pre to posttest contrasts were significant.
Table 1.
Pre and Posttest Mean Scores for Patients with Pediatric Bipolar Disorder Treated with Medication
| Pretest M (SD) | Posttest M (SD) | df | t | |
|---|---|---|---|---|
| CGI-BP | 4.74(1.02) | 2.40(1.20) | 65 | 12.00* |
| CMRS-P | 29.77 (9.20) | 15.24(10.93) | 65 | 8.40** |
| Brief CMRS-P | 14.65 (5.04) | 7.87 (5.36) | 60 | 9.70** |
| YMRS | 28.89 (6.80) | 9.70(8.53) | 65 | 12.38* |
p<0.01
p<.001
To compare the magnitude of symptom change as assessed by different outcome measures, changes from pre to posttest on each scale were converted to Cohen's (1977) d, a standardized measure of effect size. Cohen (1977) stated that effect sizes of 0.2, 0.5, and 0.8 correspond to small, medium and large effects, respectively. The effect size derived from the CMRS-P (d = 1.44) and brief CMRS-P (d = 1.43) were lower than those calculated from the clinician-rated YMRS (d = 2.49) and CGI-BP (d = 2.10), but still indicated large effect sizes.
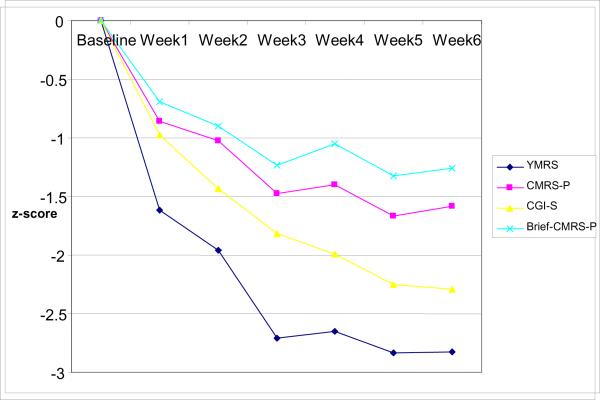
We plotted trajectories of change for all measures by calculating z-score means for each time point using the baseline mean and standard deviation as anchors. The change over the six weeks was plotted with each line representing a different measure. As demonstrated in Figure 1, the trajectory of change for each measure was roughly comparable. The YMRS showed a steep decline after treatment was initiated, which continued until the 4th session and then flattened out, while the CGI-BP showed a steadier curvilinear decline over the six sessions. Interestingly, the CMRS-P showed the most variability between sessions, with the mean scores for weeks 2, 4, and 6 increasing slightly over the previous weeks. However, similar to the other measures, the overall trajectory over time for the CMRS-P demonstrated improvement in mania symptoms with treatment. Although more modest in its demonstration, the Brief CMRS-P also indicated a similar improvement trajectory over time.
Figure 1.
Z-score comparisons for YMRS, CMRS-P, CGI-S and Brief CMRS-P over treatment
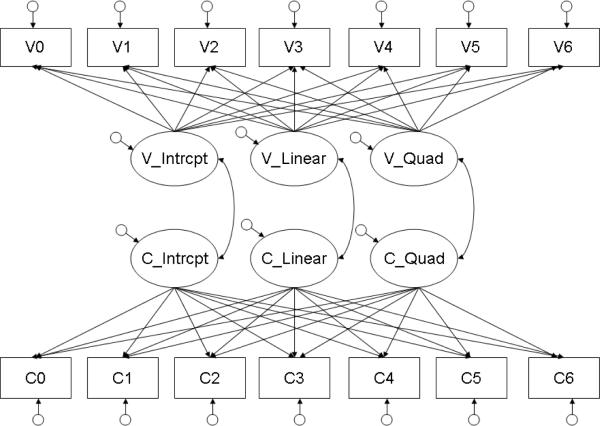
Correlations between Different Measures of Change
Our second approach was to fit joint growth curve models of change in the CMRS-P and Brief CMRS-P and change in the YMRS. The model included a growth curve for each measure, consisting of intercept, linear slope, and quadratic slope terms, and estimated the correlations between linear slopes and quadratic slopes. Figure 2 illustrates the joint growth curve models. For each growth model the indicators were the measure (CMRS-P or Brief CMRS-P and YMRS) at each of 7 waves of data collection (baseline and Waves 1–6). Factor loadings for the intercepts were fixed at 1.0 at each wave. Loadings for the linear slope were fixed at 0 for the baseline assessment, 1.0 at Wave 1, 2.0 at Wave 2, continuing to 6.0 at Wave 6. Factor loadings for the quadratic component of change were fixed at the square of the linear slope: 0 at baseline, 1.0 at Wave 1, 4.0 at Wave 2, 9.0 at Wave 3, continuing to 36.0 at Wave 6, in order to model acceleration or deceleration of change. Variances of the indicators and growth components (intercept, linear change, quadratic change) were estimated as were correlations among the growth parameters within measures. Most important for our purposes, these models estimated correlations between the latent linear and quadratic components of change across measures. Thus, these models provided direct assessment of the correlation between change as measured by the CMRS-P or Brief CMRS-P and change on the YMRS.
Figure 2.
Structure of the Joint growth curve models of CMRS-P change and change in YMRS measures. Note: * p < .05. ** p < .01. Variables C0 through C6 are CMRS-P measures, and variables V0 through V6 is the validity measure (YMRS). Similarly, “C” latent variables represent growth in the CMRS-P, and “V” latent variables represent growth in the validity measure.
The joint growth curve models fit the data reasonably well. On the full CMRS-P model this was indicated by a non-significant goodness of fit test (χ2(75, N=65) = 93.03, ns), a Comparative Fit Index of .96, and an RMSEA of .06. The Brief CMRS-Pmodel also had a non-significant goodness of fit test (χ2(75, N=65) = 93.7, ns), a Comparative Fit Index of .96, and an RMSEA of .06.
Table 2 reports the results of the two joint growth models. The top panels for the full CMRS-P and the bottom panels for the Brief CMRS-P report values, standard errors and 95% confidence intervals of three components of change for each measure: Intercept, Linear slope, and Quadratic slope. They also report the correlations between the growth components as measured on the CMRS-P and growth components measured on the YMRS, as well as their standard errors and 95% confidence intervals. Asterisks report the results of tests of the null hypothesis that the growth parameter or correlation between growth parameters is equal to zero.
Table 2.
Estimates from the Joint Growth Curve Analysis of Full and Brief CMRS-P and YMRS
| Estimate | SE | 95% CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Full CMRS-P | ||||
| CMRS-P | ||||
| Intercept | 4.62** | 1.11 | 2.44 | 6.80 |
| Linear | −1.62** | 0.45 | −2.50 | −0.74 |
| Quadratic | 0.93** | 0.26 | 0.41 | 1.44 |
| YMRS | ||||
| Intercept | 4.86** | 1.04 | 2.82 | 6.89 |
| Linear | −1.89** | 0.39 | −2.63 | −1.13 |
| Quadratic | ^ 73** | 0.53 | 0.70 | 2.76 |
| Correlations | ||||
| Intercept | 0.41 | 0.23 | −0.03 | 0.86 |
| Linear | 0.74** | 0.21 | 0.32 | 1.00 |
| Quadratic | 0.67** | 0.25 | 0.18 | 1.00 |
|
| ||||
| Brief CMRS-P | ||||
| Brief CMRS-P | ||||
| Intercept | 4.74* | 1.92 | 0.55 | 8.92 |
| Linear | −1.89* | 0.73 | −3.64 | −0.15 |
| Quadratic | 1.20* | 0.39 | 0.12 | 2.29 |
| YMRS | ||||
| Intercept | 5.96** | 1.25 | 1.86 | 10.06 |
| Linear | −1.2** | 0.42 | −2.79 | −1.05 |
| Quadratic | 1.68** | 0.51 | 0.56 | 2.80 |
| Correlations | ||||
| Intercept | 0.01 | 0.36 | −0.70 | 0.71 |
| Linear | 0.87* | 0.37 | 0.15 | 1.00 |
| Quadratic | 0.80* | 0.32 | 0.18 | 1.00 |
p<.05.
p<.01
Note: Estimates are standardized.
As can be seen in the top panel of Table 2, for the full CMRS-P the intercepts, linear and quadratic components of change all were significantly different from zero for both the full CMRS-P and the YMRS. Although the intercepts did not correlate significantly between the CMRS-P and the YMRS, the linear and quadratic components of change did correlate significantly and strongly (.74 for linear and .67 for quadratic).
The lower panel of Table 2 reports the joint growth curve model of the Brief CMRS-P and the YMRS. As can be seen there, all of the growth parameters were significant for the Brief CMRS-P and the YMRS as before. Tests of the correlations between change on the Brief CMRS-P and change on the YMRS were both significant, r = .87, p < .05 for linear change and, r = .80, p < .05 for quadratic change.
Agreement in Response to Treatment Across Measures
As reported above, the CMRS-P indicated an average reduction in symptoms from the clinical to non-clinical range from pre to post-test. The number of patients achieving response on the CMRS-P (using a cut score of 20) and the Brief CMRS-P (using a cut score of 10) was compared to the number of patients achieving response on the YMRS and CGI-BP. The results, reported in Table 3, indicate that all the measures demonstrated similar rates of remission (67–84%). These response rates indicate strong convergence across measures in detecting response to treatment.
Table 3.
Response Status
| Measure | Response rates n (%) |
|---|---|
| CMRS-P | 48 (73) |
| Brief CMRS-P | 42 (69) |
| YMRS | 44 (67) |
| CGI-BP | 55 (84) |
Further analyses examined more precisely the degree of agreement between the CMRS-P and the two other measures. Kappas indicate level of agreement between two measures, and, generally, 0.0–0.20 is slight, 0.21–0.4 is fair, 0.41–0.6 is moderate, 0.61 to 0.8 is substantial and 0.81 –1.0 is perfect (Landis & Koch, 1977). The CMRS-P and the YMRS indicated a moderate agreement, with a κ = .55 (p<.01), and the Brief CMRS-P and YMRS also demonstrated moderate agreement with the YMRS (κ = .45, p<.01). The CMRS-P demonstrated a sensitivity of .82 and a specificity of .80 for predicting recovery on the YMRS, and the Brief CMRS-P had sensitivity of .85 and specificity of .68. On the full CMRS-P, the predictive value of a positive test was .68 and the predictive value of a negative test was .32. The Brief CMRS-P had a positive predictive value of .79 and a negative predictive value of 0.32 with the YMRS. For recovery on the CGI-BP, the CMRS-P had a sensitivity of .63 and a specificity of .73. For the CGI-BP, and the CMRS-P, κ = 0.43 (p<.01), indicating moderate agreement. The score had a sensitivity of .63 and a specificity of .73. The predictive value of a positive test was .55 and the predictive value of a negative test was .45. In comparison, the CGI-BP and the YMRS indicated a moderate agreement, with a κ = .52 (p<.01). For predicting recovery on the CGI-BP, the Brief CMRS-P (κ = 0.36, p<.01), had sensitivity of .81, specificity of .45, positive predictive value of .79, and negative predictive value of .42.
Discussion
The CMRS-P is a concise, easy-to-administer parent-report instrument to measure symptoms of pediatric mania that has good psychometric properties. It is a complement to alternative measures of pediatric mania, which are limited by their focus on clinician report, length, complexity, and inability to assess variability in symptom presentation. The CMRS-P has proven to be a reliable and valid screening measure for mania symptoms and to differentiate pediatric mania from ADHD symptoms. However, to show promise as a treatment outcome measure, the CMRS-P must demonstrate sensitivity in detecting symptom change over the course of treatment. The present study is the first to examine the sensitivity of the CMRS-P to detect changes in symptoms due to pharmacological treatment and the specificity of response when compared to other gold-standard clinician-rated instruments of pediatric mania.
Our findings suggest that the CMRS-P is sensitive to symptom changes that occur as a result of pharmacological treatment for PBD. Similar to the YMRS and the CGI-BP, the CMRSP demonstrated statistically and clinically significant change in symptom report from pre to post-test. While the average score for all three measures fell in the severely manic range at pre-test, after 6 weeks of treatment, the average score on all three measures indicated that most patients fell in the sub-clinical range of symptoms and were in remission.
Interestingly, the magnitude of difference or effect size from pre to post scores, although still large, was not quite as large for the CMRS-P as the other clinician-rated measures. One possible explanation for this is that, while the YMRS and CGI-BP are clinician report measures, the CMRS-P is a parent report measure. It may be that clinician in-session ratings of symptoms are artificially inflated due to the fact that they rely on a provider's observation at a single time point during a clinical appointment when this child is likely to be on his or her best behavior. Indeed, in our clinical experience working with children with PBD, parents often report frustration that their children are so well-behaved during appointments and that we as providers are not getting a representative version of what the parents have to cope with at home and in other settings. The CMRS-P, in representing the parent's perspectives, may actually be a more comprehensive and accurate version of the child's functioning across time and various settings. A parent's version of the child's functioning is likely to be more variable than a clinician's ratings during a single 30 minute session, and therefore may result in lower, yet potentially more representative ratings of the child's global symptomatic functioning. Therefore, parent reports may represent an important aspect of outcome measurement, alongside expert clinician ratings of symptomatic functioning. This notion is consistent with previous research indicating that parents are the most accurate reporters of their child's mania symptoms and that other reports do not add much in the way of incremental validity (Youngstrom, et al, 2005).
Despite a significant difference in effect size from pre to posttest, growth modeling analyses indicated that both the CMRS-P and Brief CMRS-P demonstrated overall similarity to the YMRS in the magnitude and trajectory of change from pre to post-test. This finding suggests that both long and short forms of the CMRS-P are sensitive to detect linear and nonlinear treatment change comparable to a clinician-rated “gold standard” measure. Estimating the correlation between the linear and quadratic slopes of the CMRS-P and the validity measures using the joint growth curve models provides a direct measure of the sensitivity of the CMRS-P to change. The correlation indexes the similarity between individual linear and quadratic slopes on two measures. The association between change as measured by the parent-rated CMRS-P and the clinician-rated YMRS was strong and positive for both measures. There also was a significant association between nonlinear change on the CMRS-P and the YMRS.
Finally, there is great clinical utility in a measure's ability to detect clinically significant changes in symptoms over the course of treatment and discriminate responders from nonresponders, usually measured by rates of remission. Findings from this study indicate that the CMRS-P is able to detect clinically significant changes in symptoms as measured by response rates, and has moderate agreement with the YMRS and CGI-BP in detecting response rates. Moderate agreement with the YMRS and CGI-BP is noteworthy because the CMRS-P incorporates the parent perspective on symptoms to a much larger degree than the alternative clinician report measures. There is a solid conceptual argument for the importance of parent's reports on symptoms, without a clinician mediating parent's input, in that parents have the most comprehensive access to their child's daily functioning across various settings and in the context of different relationships and stressors. Therefore, the fact that the CMRS-P is still able to discriminate children who respond or achieve recovery in a comparable manner to a clinical “expert” provides further support for the CMRS-P as a valid and sensitive outcome measure capturing response to treatment. Once again, the brief version of the CMRS-P showed strong validity as a measure of treatment response, both on the YMRS and CGI-BP.
There are several considerations that are important to note when interpreting these results. First, the sample size was relatively small. We do not consider the small sample a limitation as it was sufficient to provide adequate power to detect correspondence in multiple measures of change and is comparable in size to other published PBD treatment studies. However, it is possible that with a larger sample, results would not have been as strong. Second, the study was conducted within the context of a “head to head” medication trial in which reduction in symptoms after the first assessment was substantial for most participants. In one sense this is a strength of the study, as there was enough reliable change to evaluate the ability of different scales to measure change. In another sense, however, the dramatic amount of change experienced by subjects did not provide an opportunity for detection of variation in the ability to assess more subtle degrees of change. Thus, we cannot claim that the CMRS-P will be able to detect change under more naturalistic circumstances or to detect worsening of symptoms among children who are stable on medication. Third, although this was a double-blind study, the validity of the blind was not explicitly tested by asking raters or patients if they thought they knew condition assignments. Therefore, some families may have guessed their condition and symptom changes may be associated with expectancy effects. Finally, although we examined agreement across measures in identifying treatment responders, there are more in depth methods of assessing clinical significance that will be important to address in future research.
This study represents an important preliminary investigation of the CMRS-P as a treatment outcome measure. These results suggest the CMRS-P may be a valid and sensitive measure for assessing symptom change over the course of treatment. This finding represents a significant contribution to the field because the CMRS-P is shorter and easier to administer as compared to other measures. Additionally, as a parent-report measure, the CMRS-P likely captures a broader and more accurate representation of the child's functioning across contexts than an in-session clinician rating. Parent report measures are a valuable complement to expert ratings of symptom functioning and outcomes. Based on this preliminary evidence of its validity and sensitivity to change over time compared to gold-standard expert ratings, the CMRS-P may now be applied in research settings as a measure of treatment-related symptom change, and shows potential for use to track symptom change in clinical settings.
Acknowledgement
The authors would also like to acknowledge all of the investigators who participated in the trial and the original study that this manuscript was based on: Robert L. Findling, M.D., Stephanie Parnes, B.A., Julie A. Carbray, Ph.D., Tahseen Mohammed, M.D., Philip G. Janicak, M.D., and John H. Sweeney, Ph.D. The authors would like to thank Tasneem Hussein for her assistance in preparation of this manuscript.
Role of Funding Source This research was funded by NIH 1 K23 RR018638-01 and NIH-MO1-RR-13987. Study drugs and matching placebo were provided by Johnson and Johnson and Abbott Pharmaceuticals. The NIH, Johnson and Johnson, and Abbott Pharmaceuticals had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Dr. Pavuluri received study drugs and matching placebo from Janssen and Abbott Pharmaceuticals. She was speaker for Astrazeneca and Bristol Myer Squibbs. All other authors declare that they have no conflicts of interest.
This statement is for editorial purposes only and will not be published with the article.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders : DSM-IV. 4rth edn Washington DC: 1994. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Academic Press; New York: 1977. Rev. ed. edn. [Google Scholar]
- Fisher LD, Dixon DO, Herson J, Frankowski RK, Hearron MS, Peace KE. Intention-to-Treat in clinical trials. In: Peace KE, editor. Statistical Issues in Drug Research and Development. Marcel Dekker; 1990. pp. 331–350. [Google Scholar]
- Geller B, Craney JL, Bolhofner K, DelBello MP, Axelson D, Luby J, Williams M, Zimerman B, Nickelsburg MJ, Frazier J, Beringer L. Phenomenology and longitudinal course of children with a prepubertal and early adolescent bipolar disorder phenotype. In: Geller B, DelBello MP, editors. Bipolar disorder in childhood and early adolescence. Guilford Press; New York, NY, US: 2003. pp. 25–50. [Google Scholar]
- Geller B, Zimerman B, Williams M, Frazier J. WASH-U-KSADS (Washington University at St. Louis Kiddie and Young Adult Schedule for Affective Disorders and Schizophrenia—Lifetime and Present Episode Version-DSM-IV) Washington University School of Medicine; St. Louis, MO: 1994. revised 1996. [Google Scholar]
- Gracious BL, Youngstrom E, Findling RL, Calabrese JR. Discriminative validity of a parent version of the young mania rating scale. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1350–1359. doi: 10.1097/00004583-200211000-00017. [DOI] [PubMed] [Google Scholar]
- Henry DB, Pavuluri MN, Youngstrom E, Birmaher B. Accuracy of brief and full forms of the Child Mania Rating Scale. Journal of clinical psychology. 2008;64(no. 4):368–381. doi: 10.1002/jclp.20464. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(no. 7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(no. 1):159–174. [PubMed] [Google Scholar]
- Pavuluri MN, Birmaher B, Naylor MW. Pediatric Bipolar Disorder: A Review of the Past 10 Years. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(no. 9):846–871. doi: 10.1097/01.chi.0000170554.23422.c1. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Henry DB, Devineni B, Carbray JA, Birmaher B. Child Mania Rating Scale: Development, Reliability, and Validity. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(no. 5):550–560. doi: 10.1097/01.chi.0000205700.40700.50. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Henry DB, Findling RL, Parnes S, Carbray JA, Mohammed T, Janicak PG, Sweeney JA. Double-Blind Randomized Trial of Risperidone versus Divalproex in Pediatric Bipolar Disorder. Bipolar Disorders. doi: 10.1111/j.1399-5618.2010.00850.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry research. 1997;73(no. 3):159–171. doi: 10.1016/s0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- Tohen M, Jacobs TG, Grundy SL, McElroy SL, Banov MC, Janicak PG, Sanger T, Risser R, Zhang F, Toma V, Francis J, Tollefson GD, Breier A. Efficacy of Olanzapine in Acute Bipolar Mania: A Double-blind, Placebo-Controlled Study. Archives of General Psychiatry. 2000;57(no. 9):841–849. doi: 10.1001/archpsyc.57.9.841. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Danielson CK, Findling RL, Gracious BL, Calabrese JR. Factor structure of the Young Mania Rating Scale for use with youths ages 5 to 17 years. Journal of Clinical Child and Adolescent Psychology. 2002;31(no. 4):567–572. doi: 10.1207/S15374424JCCP3104_15. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Findling RL, Youngstrom JK, Calabrese JR. Toward an evidence-based assessment of pediatric bipolar disorder. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):433–448. doi: 10.1207/s15374424jccp3403_4. [DOI] [PubMed] [Google Scholar]