Abstract
Tuberculosis (TB) services in China are provided through a large network of TB dispensaries. Even though hospitals are not as well placed to follow recommended standards of TB care, a significant proportion of people with TB symptoms seek care from hospitals. In spite of having a policy and mandate in place, the Ministry of Health had little success in encouraging hospitals to refer suspected TB cases to dispensaries. Following the epidemic of severe acute respiratory syndrome in 2003, the government set up a nationwide Internet-based communicable diseases reporting system. This achieved productive collaboration between hospitals and TB dispensaries. From 2004 to 2007, the percentage of TB suspects and patients needing referral from hospitals who arrived in TB dispensaries increased substantially from 58.7% to 77.8% and the contribution of hospitals to diagnosing sputum smear-positive TB cases doubled from 16.3% to 32.9%. Using the Internet-based reporting system, hospitals in China contributed to finding about one third of all sputum smear-positive TB cases and helped meet the global TB control target of detecting 70% of such cases. Based on the data available from routine surveillance facilitated by this Internet-based system, this paper details the process and outcomes of strengthening collaboration between hospitals and TB dispensaries using the Internet as a tool and its potential application to other country settings.
Resumé
En Chine, les services de traitement de la tuberculose (TB) sont fournis par un large réseau de dispensaires de TB. Même si les hôpitaux ne sont pas bien placés pour suivre les normes recommandées en matière de soins de la TB, une part importante de personnes présentant les symptômes de la TB cherche à se faire soigner dans les hôpitaux. Bien que le ministère de la Santé dispose d’une politique et d’un mandat, il n’a que très peu réussi à encourager les hôpitaux à signaler les suspicions de TB aux dispensaires. Suite à l’épidémie du syndrome respiratoire aigu sévère (SRAS) en 2003, le gouvernement a mis en place un système de notification des maladies par Internet à l'échelle nationale. Ce système a permis d’obtenir une collaboration productive entre les hôpitaux et les dispensaires de TB. De 2004 à 2007, le pourcentage de suspicions et de cas avérés de TB nécessitant une orientation des patients des hôpitaux vers les dispensaires de TB a considérablement augmenté de 58,7 à 77,8%. De plus, la contribution des hôpitaux dans le diagnostic des cas de TB à frottis d’expectoration positifs a doublé, passant de 16,3 à 32,9%. En utilisant un système de notification par Internet, les hôpitaux chinois ont contribué à détecter environ un tiers de tous les cas de TB à frottis d’expectoration positifs et ont permis de répondre à l'objectif de contrôle de la TB global, qui est d’identifier 70% de ces cas. Reposant sur les données disponibles de la surveillance continue facilitée par ce système Internet, cet article décrit en détail le processus et les résultats d’une collaboration renforcée entre les hôpitaux et les dispensaires de TB qui utilisent Internet comme un outil ainsi que son application potentielle aux situations des autres pays.
Resumen
Los servicios de atención sanitaria de la tuberculosis (TB) en China se proporcionan a través de una amplia red de dispensarios especializados. Aunque los hospitales no están incluidos en las normas asistenciales recomendadas para la tuberculosis, una proporción considerable de personas con síntomas de tuberculosis acuden a ellos. A pesar de haber dispuesto una normativa y una orden al respecto, el Ministerio de Sanidad no había conseguido que los hospitales remitieran los casos sospechosos de tuberculosis a los dispensarios. A raíz de la epidemia de síndrome respiratorio agudo y grave de 2003, el gobierno creó un sistema nacional de notificación de enfermedades transmisibles a través de Internet, que consiguió que los hospitales y los dispensarios de atención de la tuberculosis desarrollaran una colaboración fructífera. Entre 2004 y 2007, el porcentaje de casos posibles o confirmados de tuberculosis derivados de los hospitales que accedieron a los dispensarios de tuberculosis aumentó considerablemente, del 58,7% al 77,8%, y la contribución de los hospitales para el diagnóstico de los casos de TB con baciloscopias positivas se duplicó del 16,3% al 32,9%. Gracias a la utilización del sistema de notificación a través de Internet, los hospitales de China han contribuido en la detección de aproximadamente un tercio de todos los casos de TB con baciloscopias positivas y han ayudado a cumplir el objetivo mundial de control de la tuberculosis, esto es, detectar el 70% de los casos. Basándose en los datos disponibles de vigilancia sistemática facilitados por este sistema basado en Internet, este artículo detalla el proceso y los resultados de la consolidación de la colaboración entre los hospitales y los dispensarios de tuberculosis que utilizan Internet como herramienta fundamental, así como su posible aplicación a otros países.
ملخص
تُقدَم خدمات مرض السل في الصين من خلال شبكة واسعة من المستوصفات المعنية بهذا المرض. وبالرغم من أن المستشفيات لا تتمكن من متابعة المعايير الموصى بها لرعاية حالات السل، إلا أن هناك نسبة كبيرة يعتد بها إحصائيا من المرضى الذين يعانون من أعراض السل يلتمسون الرعاية من المستشفيات. وبالرغم من أن وزارة الصحة تمتلك سياسات ومهام واضحة لهذا الأمر، إلا أنها لم تنجح كثيراً في تشجيع المستشفيات على إحالة المشتبه في إصابتهم بالسل إلى المستوصفات المتخصصة. وعقب جائحة المتلازمة التنفسية الحادة الوخيمة التي حدثت في 2003، وضعت الحكومة نظاماً قطرياً، للتبليغ عن الأمراض السارية بالارتكاز على شبكة الإنترنت. ومنذ عام 2004 وحتى عام 2007، ارتفعت النسبة المئوية لإحالة المشتبه في إصابتهم بالسل ومرضاه من المستشفيات إلى المستوصفات، من 58.7% إلى 77.8%، وتضاعفت مساهمة المستشفيات في تشخيص حالات السل الإيجابي للطاخة البلغم من 16.3% إلى 32.9%. وباستخدام النظام المرتكز على شبكة الإنترنت، ساهمت المستشفيات في الصين على اكتشاف ثلث إجمالي الحالات الإيجابية من مرضى السل، وساعدت على تحقيق الهدف العالمي لمكافحة السل المتمثل في الكشف عن 70% من هذه الحالات. وطبقا للمعطيات المتوافرة من الترصد الروتيني الذي يتم من خلال النظام المرتكز على شبكة الإنترنت، فإن هذه الورقة البحثية تقدم بالتفصيل عملية ونتائج تعزيز التعاون بين المستشفيات والمستوصفات المعنية بحالات السل باستخدام الإنترنت، وإمكانية تطبيق ذلك في سائر المواقع بالقطر.
Резюме
Услуги в области профилактики и лечения туберкулеза (ТБ) в Китае предоставляются широкой сетью ТБ-диспансеров. Однако значительная доля населения с симптомами ТБ обращается за помощью в больницы, хотя условия в больницах не слишком соответствуют рекомендуемым стандартам медицинской помощи при ТБ,. Министерству здравоохранения, которое осуществляет соответствующую политику и обладает необходимыми полномочиями, не удалось побудить больницы направлять лиц с подозрением на ТБ в диспансеры. После эпидемии тяжелого острого респираторного синдрома (ТОРС) в 2003 г. правительство cоздало общенациональную систему отчетности об инфекционных ,болезнях на базе Интернета. В результате этого было налажено плодотворное сотрудничество между больницами и ТБ-диспансерами. В период с 2004 по 2007 г. процентная доля обратившихся в ТБ-диспансеры больных с подозрением на ТБ и пациентов, которым требовалось направление из больницы, значительно возросло – с 58,7 до 77,8%, – а вклад больниц в диагностирование случаев заболевания ТБ с положительным мазком мокроты удвоился с16,3 до 32,9%. Используя систему отчетности на базе Интернета, больницы в Китае содействовали выявлению почти 1/3 всех случаев заболевания ТБ с положительным мазком мокроты и помогли достигнуть глобальной цели в области профилактики и лечения – выявить 70% таких случаев. Настоящая статья, основанная на данных рутинного наблюдения, которое облегчается с помощью этой Интернет-системы, подробно освещает процесс и результаты укрепления сотрудничества между больницами и ТБ-диспансерами путем использования Интернета и рассматривает возможности ее применения в условиях других стран.
摘要
中国通过大型的结核病防治机构网络向结核病患者提供相关的治疗服务。在中国,遵守结核病治疗的推荐标准不是放在综合性医疗机构执行,但仍有相当大比例的结核病患者前往综合性医疗机构寻求相关的治疗。尽管中国有转院政策,并且政府要求落实该政策,卫生部却没有成功地鼓励医院将疑似肺结核病例转入肺结核防治机构进行治疗。在2003年发生非典型肺炎疫情之后,中国政府建立了一个以网络为基础的全国传染病报告系统。在该系统的帮助下,综合性医疗机构和肺结核防治机构进行了有效的合作。从2004年至2007年,被转入肺结核防治机构的疑似肺结核病例和有必要转院的肺结核患者的比例得到了大幅地提高,从58.7%提高至77.8%,综合性医疗机构诊断出的痰涂片呈阳性的肺结核病例数翻了一番,从16.3%增至32.9%。利用以网络为基础的报告系统,中国各医院发现了大约三分之一的痰涂片呈阳性的肺结核病例,帮助实现了全球结核病控制目标,即新发涂阳肺结核病人发现率达到70%。依据这个以网络为基础的系统的日常监测得到的数据,本论文详细阐述了利用网络报告加强综合性医疗机构和肺结核防治机构间的合作过程和成果,以及在其他国家网络报告的潜在应用价值。
Introduction
Engaging all relevant health-care providers in tuberculosis (TB) care and control through public–private and public–public mix approaches is an essential component of the World Health Organization's (WHO's) Stop TB Strategy.1 Public–private mix implies collaboration between the public sector and private care providers for delivery of TB care and control while a public–public mix means collaboration among different public sector entities within and outside the scope of ministries of health. China has used a public–public partnership between public hospitals and TB dispensaries as one of the strategies to reach the global TB control targets.2
According to the 2000 National TB Prevalence Survey in China, 94% of TB suspects reportedly went to “non-TB facilities”: 34% to general hospitals, 29% to township/village clinics, 22% to private clinics and 9% to traditional health clinics and other providers.3 Only 4.3% and 1.3% consulted a TB dispensary or a TB hospital. This finding was also corroborated subsequently by a social assessment study in four provinces.4 In 2003, the TB case detection rate in China was below the global TB control target of 70%. Two of the main strategies pursued by the Ministry of Health to improve the case detection rate were geographical expansion of DOTS (Directly Observed Treatment, Short course) strategy implementation and strengthening of the hospital–TB dispensary collaboration.
A window of opportunity opened in 2003 when China encountered a serious epidemic of severe acute respiratory syndrome. After this epidemic was brought under control, the Chinese government implemented a series of measures to strengthen its public health system.5 One of these measures was strengthening the surveillance of communicable diseases. The law on the control of infectious diseases was also revised, making it mandatory to report communicable diseases, including TB.
The National Centre for Tuberculosis Control and Prevention used this new tool to accelerate nationwide scale-up of hospital involvement in TB control. It carried out a pilot project of the Internet-based TB reporting and referral system with the cooperation of the China country office of WHO. This project demonstrated that collaboration between hospitals and TB dispensaries was feasible and that it enhanced TB case finding.6 Based on the evidence from the pilot project, the Ministry of Health issued an updated policy of collaboration between hospitals and TB dispensaries. The new policy stipulated that all pulmonary TB cases and suspects detected in general hospitals should be reported through the Internet and referred to TB dispensaries. The dispensaries must also trace the reported cases that fail to come to the dispensaries.
Based on data emerging from routine surveillance reports, this paper describes the processes and outcomes of collaboration between hospitals and TB dispensaries in China facilitated by the Internet-based TB reporting and management system.
Setting
The Chinese Ministry of Health has 17 departments. While control of communicable diseases is the responsibility of the Department for Disease Control, all hospitals fall under the Department of Medical Administration. The National Centre for Tuberculosis Control and Prevention under the Chinese Centre for Disease Control and Prevention provides technical support and routine management for national TB control programme implementation. This structure is replicated at provincial and prefecture levels. At the county level, most dispensaries that provide TB services are under the Centre for Disease Control and Prevention. Hospitals are required to report and refer TB suspects and cases to TB dispensaries.
Internet-based reporting
In January 2004, China launched the world's largest Internet-based National Communicable Disease Information System. The purpose of the system was to provide a common platform for health facilities including general public hospitals to use the Internet to notify 37 communicable diseases, including TB, in real-time.7
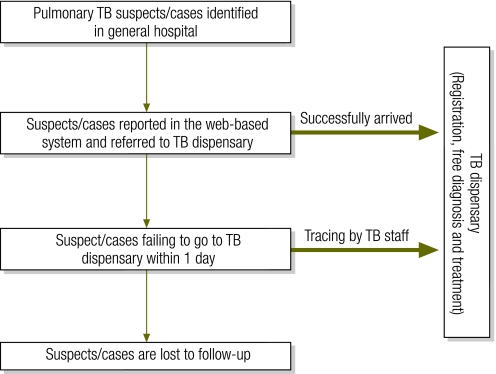
As Fig. 1 shows, doctors in all health facilities, including hospitals, report information on TB suspects and cases through the Internet and refer them to the TB dispensary in the area. This information includes essential contact details and diagnostic status of each reported suspect and cases. It is available to authorized individuals and institutions as soon as it is entered into the system. TB dispensaries are required to record the arrival and confirmed diagnosis of all reported TB suspects and cases. If the referred suspects/cases do not arrive at the dispensary within one day, authorized staff members retrieve the relevant information from the system and trace the cases. Data quality is checked at different levels. Designated hospital staff members check the completeness and quality of reporting by different departments every day.
Fig. 1.
Flowchart showing the policy on hospital–tuberculosis dispensary collaboration
TB, tuberculosis.
At the TB dispensary, an assigned staff member checks the system every day for TB suspects/cases reported by hospitals. Steps in tracing non-reporting suspects/cases include telephoning the patient, tracking town or village doctors and, if required, visiting the patient at home. For each successful referral, the TB dispensary pays US$ 3 to the referring hospital. Township and village doctors are paid US$ 2 for every successfully retrieved patient while dispensary staff members earn US$ 1 for the same. A local “coordinating group” comprising officials from the local health bureau, hospitals and the TB dispensary guides, supports and supervises the implementation of the policy.
The financial resources for implementing this policy are provided by the government and international agencies. A central fund provides resources to all provinces to cover financial incentives for reporting and field-tracing. Expenses towards training, coordination meetings and telephone-tracing fees in 24 provinces are covered through a grant from The Global Fund to Fight AIDS, Tuberculosis and Malaria.
Data collection and analysis
The data for the analysis presented in this paper were collected from monthly and quarterly reports drawn from the routine TB surveillance system in China. Monthly reports are used specifically to monitor collaboration between hospitals and TB dispensaries on reporting, referring and tracing TB suspects/cases. The monthly reports submitted by all provinces from 2004–2007 were compiled and reviewed. These reports provide information on the number of TB suspects and cases reported, the number referred by hospitals, as well as the number arriving at the dispensaries on their own, by referral or after tracing. Since the monthly report data was limited, the quarterly reporting system was used to determine the number of confirmed TB patients among referred arrivals and the number of notified TB cases.
The following set of indicators was used to evaluate the process and the outcome of the collaboration: (i) proportion of hospitals participating in the Internet-based system; (ii) number of TB suspects/cases reported by the hospitals on the Internet and referred; (iii) proportion of TB suspects/cases whose sputum examination was reported by the referring hospitals; (iv) proportion of referred TB suspects/cases arriving at the TB dispensary without requiring tracing (referred arrival rate); (v) proportion of TB suspects/cases arriving at the TB dispensary after tracing (traced arrival rate); (vi) percentage of TB suspects/cases needing referral from hospitals who arrived in TB dispensaries with or without tracing (overall arrival rate); (vii) contribution of hospitals to case finding, i.e. proportion of TB cases from general hospitals among all TB cases registered in the national tuberculosis programme.
The reporting formats used routinely by provinces to send TB-related data to the central unit do not allow disaggregation of TB suspects and cases referred by hospitals. Similarly, disaggregating treatment outcomes of patients referred by hospitals and those presenting to dispensaries was not possible.
Results
Combined data from the monthly and quarterly surveillance system was used to measure the outcome of each of the steps involved in improving the referral of TB suspects/cases to TB dispensaries. These included: participation of hospitals in the Internet-based reporting system; hospitals reporting TB suspects/cases through the Internet-based system and referring them to the TB dispensaries; the referred suspects/cases arriving at the dispensaries; dispensaries tracing those suspects/cases that fail to present; the traced and retrieved patients arriving at the dispensaries; and, as an outcome of all these steps, the overall contribution of hospitals to TB case finding in the country.
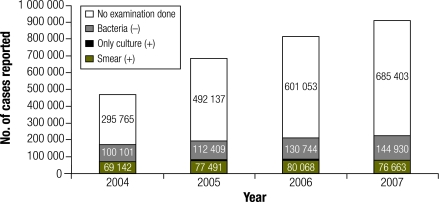
An increasing number of hospitals participated in the Internet-based reporting and referring system over the years, from 93.2% in 2004 to 96.0% in 2007. By 2007, 96% of the 9044 county hospitals and all 3007 TB dispensaries in the country were part of the Internet-based system. From 2004 to 2007, about 2.9 million TB suspects/cases were reported by hospitals through the Internet. In 2007 alone, hospitals reported about a million TB suspects/cases, more than twice the number reported in 2004 (Fig. 2).
Fig. 2.
Cases of tuberculosis reported by hospitals in China, 2004–2007
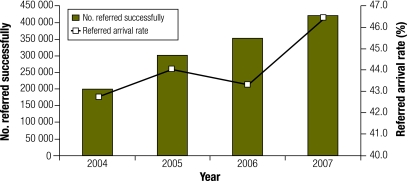
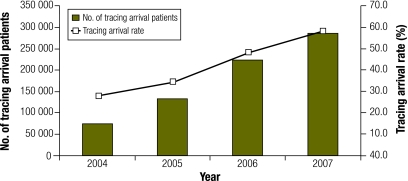
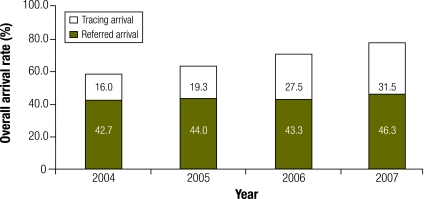
Among the cases reported by hospitals, the number of smear-positive cases remained stable and the number of smear-negative cases rose slightly. However, the number of cases without sputum examination more than doubled. Importantly, the cases reported without sputum examination accounted for about 75% of all reported cases in 2007. The total number of referred TB suspects/cases who arrived at the TB dispensary also doubled from 2004 to 2007. However, the referred arrival rate remained almost constant (from 42.7% to 46.4%), (Fig. 3). The number of suspects/cases that needed to be traced by the TB dispensaries increased about fourfold over the period with a doubling of the tracing arrival rate (Fig. 4).
Fig. 3.
Patients referred by hospitals to tuberculosis dispensaries in China, 2004–2007
Fig. 4.
Patients arriving at dispensaries after tracing, China, 2004–2007
By 2007, the total number of suspects/cases arriving at and evaluated by TB dispensaries increased by more than 150% (from 273 582 to 707 284). The percentage of TB suspects/cases needing referral from the hospitals who arrived in TB dispensaries increased by over 33%, from 58.7% in 2004 to 77.8% in 2007 (Fig. 5). This increase was mainly due to improved tracing of referred patients who did not report to the dispensaries when first referred.
Fig. 5.
Patients arriving at dispensaries after referral with or without tracing, China, 2004–2007
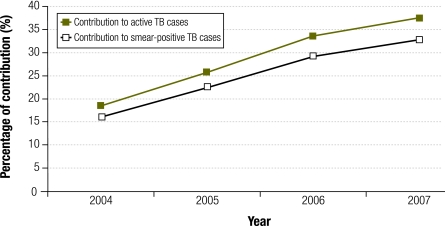
The collaboration between hospitals and TB dispensaries, enhanced by the Internet-based system, contributed substantially to the overall case finding. In 2007, about one third of all smear-positive TB cases notified were contributed by hospitals (Fig. 6).
Fig. 6.
Contribution of hospitals to tuberculosis case detection in China, 2004–2007
TB, tuberculosis.
As mentioned previously, data available from routine surveillance did not allow the disaggregation of treatment outcomes of patients referred by hospitals and those presenting to dispensaries. It was however reasonable to assume that the treatment success rates among patients referred by hospitals were unlikely to be inferior since the overall treatment success rates across the country remained consistently high before and after hospital involvement.
Discussion
TB control and hospitals
The global target for tuberculosis control of detecting 70% of the estimated new sputum smear-positive cases was postponed in the year 2000 and not achieved in 2005.8 A major barrier to achieving the target in many countries has been limited engagement of large hospitals, both public and private, in TB care and control. In China and many other countries, most TB suspects, i.e. patients with a cough of long duration, first seek care at general public hospitals.
TB patients are not always managed well in hospitals. Typically, hospitals and hospital-based clinicians do not follow the recommended methods of TB management and they treat TB as any other medical condition rather than an important public health problem. There is a clinical–public health divide between the medical treatment of TB in hospitals and DOTS-based, patient-centred management in a health centre or dispensary. In China, as in most countries with a high burden of TB, the divide is vertical: at the top, the department or directorate responsible for hospitals is separate from that responsible for health centres or dispensaries and at the bottom there are few formal linkages between hospitals and health centres.9
Against this backdrop, the success of China's national tuberculosis programme is noteworthy. Since 2005, the collaboration between hospitals and TB dispensaries has been the main contributor to meeting and maintaining the global TB control targets of detecting at least 70% of new sputum-smear positive cases and curing 85% of them.10 One limitation has been the inability of the Internet-based system to determine the precise contribution of hospitals to the national TB case-detection rate.
Shifting workload
The Internet-based system allowed monitoring of the process as well as the outcome of the hospital-dispensary collaboration. While increasing numbers of hospitals participated and TB suspects and cases referred by hospitals to TB dispensaries increased substantially, the number of patients acting on the hospital clinicians' advice and reporting to the dispensaries (referred arrivals) hardly increased (Fig. 3). The gains made in referrals (total arrivals) were all due to effective tracing of referred patients by the dispensary staff (traced arrivals) (Fig. 4 and Fig. 5). This remains a source of concern to the TB programme. Tracing so many patients results in an additional burden on the field staff, requires additional resources and, importantly, delays diagnosis and continues transmission of TB in the community. In the pilot period, we found that good health education provided to TB suspects and cases in hospitals contributes to a significant reduction in delay of diagnosis from 8.6 days in the pre-intervention period to 3.9 days after intervention.11 Increased workload of sputum smear microscopy on the laboratory staff due to a rapid and substantial increase in the number of suspects and a high proportion of smear-negative suspects have also been a matter of concern to the TB programme, with implications for supply of both human and financial resources.
Enablers and incentives
The Internet-based system required diverse inputs from the central and lower levels of government: enhanced government commitment and a conducive regulatory environment in the wake of the epidemic of severe acute respiratory syndrome, funding provision including financial incentives for hospital and dispensary staff, systematic training of hospital and dispensary staff, administrative commitment at the provincial level and a steering mechanism in the form of a local coordinating group. This paper based largely on the output from the routine surveillance system did not assess relative contribution of the varied interventions to the productive engagement of hospitals in TB control.
The issue of sustaining financial incentives to staff is important. The two functions for which financial incentives were provided – referral by the hospital staff and tracing by the field staff – produced impressive results.
Unresolved issues
The analysis presented here demonstrates successful adaptation of an Internet-based communicable disease reporting system to facilitate collaboration between hospitals and dispensaries for TB control. It also raises important questions that the national TB programme plans to address through further research and interventions. For any such system to work well on a sustainable basis, it has to be acceptable to all concerned – hospitals, dispensaries and patients. Some of the issues may need to be systematically addressed: do hospitals refer all TB suspects/cases to dispensaries? Why do hospitals increasingly send patients without giving sputum examinations? Why do a significant proportion of patients not report to dispensaries after referral? Will the dispensaries be able to bear the increasing burden of patient tracing? What happens to a large proportion of referred suspects that do not turn out to be TB?
Alternative strategies
Alternative strategies in setting up hospital–health centre collaboration for proper TB care and control could be either to strip hospitals of functions they do not traditionally perform well or to build their capacities to take on new tasks. In relieving hospitals of managing TB suspects and cases, the Internet-based system follows the former strategy. A middle path could be to compel hospitals to take on limited “clinical” tasks that they are well placed to carry out. For example, making a proper diagnosis, providing a correct drug prescription and supporting diagnosed patients with “public health” tasks such as notifying, counselling, record keeping, contact tracing, follow up and default retrieval. This seemed to have worked in large-scale projects in India and Indonesia.12,13 China's national TB programme has also been trying out a scheme of “designated hospitals” with encouraging results. In this scheme, a limited number of hospitals have been identified and strengthened to undertake high-quality TB management.
Strengthening health systems
The strength of China's Internet-based communicable disease reporting system is its integrated approach that combines reporting requirements of 37 important conditions. The TB programme has exploited the opportunity and the system to its own advantage. This successful example could well be adapted and applied in many countries. Other countries, including India,14 Republic of Korea15and Thailand, also have Internet-based systems that have helped improve TB surveillance and monitoring. It would be worthwhile to investigate additional benefits these systems may offer in detecting more cases earlier. Drawing lessons from this initiative in China, there is enormous scope to use advances in digital technology to adapt and set up new Internet-based systems, strengthen existing monitoring systems, integrate TB monitoring and surveillance into general disease surveillance and use Internet-based platforms to involve public and private care providers outside the TB control programmes.
Over the past decade, TB programmes worldwide have focused their attention on strengthening DOTS-based care at health centres in the hope that TB suspects and cases will not need to visit hospitals. Evidence that significant proportions of TB patients still continue to seek care from hospitals and other care providers requires that national TB programmes should cast their net wider and adopt a much broader “systems” approach that seeks to “engage all care providers”, as recommended by WHO's Stop TB Strategy.
Funding:
Government of China.
Competing interests:
None declared.
References
- 1.Raviglione MC, Uplekar MW. WHO’s new Stop TB Strategy. Lancet. 2006;367:952–5. doi: 10.1016/S0140-6736(06)68392-X. [DOI] [PubMed] [Google Scholar]
- 2.Engaging all health-care providers in TB control. Geneva: World Health Organization; 2006. [Google Scholar]
- 3.Report on the nationwide random survey for the epidemiology of tuberculosis in 2000. Beijing: Ministry of Health of the People's Republic of China; 2002.
- 4.Social assessment support to WB/DFID-Funded TB Control Project in China. Liverpool: Liverpool Associates in Tropical Health; 2005.
- 5.Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet. 2007;369:691–6. doi: 10.1016/S0140-6736(07)60316-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L, Cheng S, Xu M, Huang F, Xu W, Li R, et al. Model collaboration between hospitals and public health system to improve tuberculosis control in China. Int J Tuberc Lung Dis. 2009;13:1486–92. [PubMed] [Google Scholar]
- 7.Ma JQ, Yang GH, Shi XM. Information technology platform in China's disease surveillance system. Dis Surveill. 2006;21:1–3. [Google Scholar]
- 8.Global tuberculosis control: surveillance, planning, financing. Geneva: World Health Organization; 2005 (WHO/HTM/TB/2005.349).
- 9.Uplekar M. Stopping tuberculosis: time to turn urgent attention to hospitals. Int J Tuberc Lung Dis. 2008;12:986. [Editorial] [PubMed] [Google Scholar]
- 10.Global tuberculosis control: a short update to the 2009 report. Geneva: World Health Organization; 2009 (WHO/HTM/TB/2009.426).
- 11.Wang L, Cheng S, Xu M, Xu W, Liren Z, Chen S, et al. Report of the pilot project on public–public mix DOTS in China: cooperation of general hospitals and TB dispensaries on reporting, referring and tracing TB patients. The Journal of the Chinese Antituberculosis Association. 2007;29:479. [Google Scholar]
- 12.Pantoja A, Lönnroth K, Lal SS, Chauhan LS, Uplekar M, Padma MR, et al. Economic evaluation of public-private mix for tuberculosis care and control, India. Part II. Cost and cost-effectiveness. Int J Tuberc Lung Dis. 2009;13:705–12. [PubMed] [Google Scholar]
- 13.Irawati SR, Basri C, Arias MS, Prihatini S, Rintiswati N, Voskens J, et al. Hospital DOTS linkage in Indonesia: a model for DOTS expansion into government and private hospitals. Int J Tuberc Lung Dis. 2007;11:33–9. [PubMed] [Google Scholar]
- 14.Tuberculosis control India [Internet site]. Available from: http://www.tbcindia.org/ [accessed 7 September 2010].
- 15.Lew WJ, Lee EG, Bai JY, Kim HJ, Bai GH, Ahn DI, et al. An Internet-based surveillance system for tuberculosis in Korea. Int J Tuberc Lung Dis. 2006;10:1241–7. [PubMed] [Google Scholar]