Abstract
Objective
To systematically review the Chinese-language literature on acupuncture-related adverse events.
Methods
We searched three Chinese databases (the Chinese Biomedical Literature Database, 1980–2009; the Chinese Journal Full-Text Database, 1980–2009; and the Weipu Journal Database, 1989–2009) to identify Chinese-language articles about the safety of traditional needle acupuncture. Case reports, case series, surveys and other observational studies were included if they reported factual data, but review articles, translations and clinical trials were excluded.
Findings
The inclusion criteria were met by 115 articles (98 case reports and 17 case series) that in total reported on 479 cases of adverse events after acupuncture. Fourteen patients died. Acupuncture-related adverse events were classified into three categories: traumatic, infectious and “other”. The most frequent adverse events were pneumothorax, fainting, subarachnoid haemorrhage and infection, while the most serious ones were cardiovascular injuries, subarachnoid haemorrhage, pneumothorax and recurrent cerebral haemorrhage.
Conclusion
Many acupuncture-related adverse events, most of them owing to improper technique, have been described in the published Chinese literature. Efforts should be made to find effective ways of monitoring and minimizing the risks related to acupuncture.
Resumé
Objectif
Évaluer systématiquement la documentation en langue chinoise sur les événements indésirables liés à l’acupuncture.
Méthodes
Nous avons fait des recherches dans trois bases de données chinoises (la base de données sur la documentation biomédicale chinoise, 1980–2009, la base de données en texte intégral du Journal chinois, 1980–2009 et la base de données de la revue Weipu, 1989–2009) afin d’identifier les articles en langue chinoise qui abordent le thème de la sécurité de l’acupuncture traditionnelle pratiquée avec des aiguilles. Les observations, les séries de cas, les enquêtes et d’autres études d’observation ont été prises en compte lorsqu’elles rapportaient des données factuelles, mais les articles, les traductions et les essais cliniques ont été exclus.
Résultats
Les critères d’inclusion concernaient 115 articles (98 observations et 17 séries de cas) qui signalaient au total 479 cas d’événements indésirables après acupuncture. Quatorze patients étaient décédés. Les événements indésirables liés à l’acupuncture étaient classés en trois catégories : traumatiques, infectieux et «autres». Les événements indésirables les plus fréquents étaient le pneumothorax, l’évanouissement, l’hémorragie méningée et l’infection, les plus graves étant les lésions cardiovasculaires, l’hémorragie méningée, le pneumothorax et l’hémorragie cérébrale récurrente.
Conclusion
De nombreux événements indésirables liés à l’acupuncture, dont la majorité était due à une technique incorrecte, ont été décrits dans la documentation chinoise publiée. Des efforts sont indispensables afin de trouver des moyens efficaces de contrôler et de réduire les risques liés à l’acupuncture.
Resumen
Objetivo
Realizar una revisión sistemática de la bibliografía en chino sobre los acontecimientos adversos relacionados con la acupuntura.
Métodos
Se realizaron búsquedas en tres bases de datos chinas (Biomedical Literature Database, 1980–2009; Chinese Journal Full-Text Database, 1980–2009 y Weipu Journal Database, 1989–2009) con el fin de identificar los artículos en lengua china sobre la seguridad de la acupuntura tradicional con agujas. Se incluyeron casos clínicos, series de casos, encuestas y otros estudios de observación que presentaran datos documentados, pero se excluyeron los artículos de revisión, las traducciones y los ensayos clínicos.
Resultados
Los criterios de inclusión se cumplieron en 115 artículos (98 casos clínicos y 17 series de casos) que, en total, informaron sobre 479 casos de efectos adversos tras la acupuntura. Catorce pacientes fallecieron. Los acontecimientos adversos relacionados con la acupuntura fueron clasificaron en tres categorías: traumáticos, infecciosos y «otros». Los acontecimientos adversos más frecuentes fueron: neumotórax, desmayo, hemorragia subaracnoidea e infección; mientras que los más graves fueron: lesiones cardiovasculares, hemorragia subaracnoidea, neumotórax y hemorragia cerebral recurrente.
Conclusión
En la bibliografía china publicada se han descrito muchas reacciones adversas relacionadas con la acupuntura, debidas en su mayor parte a una técnica inadecuada. Debemos esforzarnos para encontrar formas eficaces de controlar y reducir al mínimo los riesgos relacionados con la acupuntura.
ملخص
الغرض مراجعة أدبيات اللغة الصينية حول الآثار الضائرة المرتبطة بالوخز الإبري مراجعة نظامية
الطريقة قام الباحثون بالبحث في ثلاث قواعد بيانات صينية وهي (قاعدة بيانات الأدبيات الطبية البيولوجية الصينية، 1980-2009؛ وقاعدة بيانات النصوص الكاملة للمجلات الصينية، 1980-2009؛ وقاعدة بيانات جريدة ويبو Weipu، 1989-2009)، من أجل تحديد المقالات الواردة فيها باللغة الصينية حول سلامة الوخز الإبري التقليدي. ولقد تضمن البحث تقارير حالة، وسلسلة للحالات، مع مسوحات وسائر الدراسات القائمة على المراقبة، حال احتوائها على معطيات واقعية، وقد استبعدت مقالات المراجعة، والمقالات المترجمة والتجارب السريرية.
المجودات لبت 115 مقالة معايير الإدراج في الدراسة (98 تقارير حالة، و17 سلسلة من الحالات) واشتملت على إجمالي 479 حالة تعرضت للآثار الضائرة بعد استخدام الوخز الإبري، وتوفي 14 مريضا. ولقد صنفت الآثار الضائرة المرتبطة بالوخز الإبري إلى ثلاث فئات: رضحي، ومعدٍ، وأخرى. وكانت أكثر الآثار الضائرة تكراراً على الإطلاق استرواح الصدر، والإغماء، والنزف تحت العنكوبتية، والعدوى، بينما كانت الآثار الأكثر تفاقما هي تلك التي ارتبطت بالإصابات القلبية الوعائية، والنزف تحت العنكوبتية، واسترواح الصدر، وتكرار النزف الدماغي.
الاستنتاج احتوت الأدبيات الصينية المنشورة على العديد من الأحداث الخاصة بالآثار الضائرة المرتبطة بالوخز الإبري، وكان أكثرها يعود إلى استخدام التقنية الخاطئة. ومن ثم، يتوجب بذل الجهود من أجل إيجاد طرق فعالة للمراقبة والرصد وتقليص المخاطر المرتبطة بالوخز الإبري.
Резюме
Цель
Провести систематический обзор литературы на китайском языке о нежелательных явлениях, связанных с иглоукалыванием.
Методы
Мы провели поиск в трех китайских базах данных (База данных китайской медико-биологической литературы за 1980–2009 гг., База данных полных текстов китайских журналов за 1980–2009 гг. и база данных журнальных статей Weipu за 1989–2009 гг.) для выявления статей на китайском языке о безопасности иглоукалывания – традиционного метода китайской медицины. В обзор включались описания клинических случаев, описания серии клинических случаев, отчеты об опросах и других обсервационных исследованиях, если в них приводились фактические данные. Обзоры, переводы и отчеты о клинических испытаниях исключались из обзора.
Результаты
Критериям включения в обзор соответствовали 115 статей (98 описаний клинических случаев и 17 описаний серии клинических случаев), в которых в общей сложности сообщалось о 479 случаях нежелательных явлений, развившихся после лечения иглоукалыванием. Четырнадцать пациентов умерли. Неблагоприятные явления, связанные с лечением иглоукалыванием были разделены на три категории: травматические, инфекционные и «прочие». Наиболее распространенными нежелательными явлениями были пневмоторакс, потеря сознания, субарахноидальное кровоизлияние и инфекция, а наиболее серьезными – повреждения сердечно-сосудистой системы, субарахноидальное кровоизлияние, пневмоторакс и рецидивирующие внутримозговые кровоизлияния.
Вывод
В китайских публикациях описано множество неблагоприятных явлений, связанных с лечением иглоукалыванием. Большинство из них было вызвано применением неправильной техники. Необходимо предпринять усилия для нахождения эффективных способов мониторинга и минимизации рисков, связанных с лечением иглоукалыванием.
摘要
目的
旨在系统综述与针灸相关的不良事件的中文文献。
方法
我们调查了三个中文数据库(中国生物医学文献数据库,1980-2009;中国期刊全文数据库;1980-2009;维普期刊数据库,1989-2009)从而确定关于传统针灸安全性的中文文章。报告真实资料的个案报告、病例分析、调查和其他观察性研究均包括在内,然而评论文章、译文和临床试验均未包括在内。
发现
115篇文章满足入选标准(98份个案报告和17份病例分析),共计报告了479例针灸后不良事件。十四位患者死亡。与针灸相关的不良事件分为三类:外伤、感染和“其他”。最常见的不良事件是气胸、昏厥、蛛网膜下腔出血和感染,而最严重的是心血管损伤、蛛网膜下腔出血、气胸和复发性脑出血。
结论
许多主要因技术不当造成的针灸相关不良事件在已经出版的中文文献中均有描述。应努力寻找监控并尽量减少针灸相关风险的有效途径。
Introduction
Acupuncture is popular in most countries, but nowhere more than in China. Because its use is so widespread, safety is an important issue that deserves close attention. Serious adverse events resulting from acupuncture, including pneumothorax, cardiac tamponade, spinal cord injury and viral hepatitis, have been identified in previous literature reviews.1–4 Prospective surveys to determine the frequency of acupuncture-related adverse events have been conducted in Germany,5,6 Norway7 and the United Kingdom of Great Britain and Northern Ireland.8,9 These studies have shown an incidence of mild, transient acupuncture-related adverse events that ranges from 6.71% to 15%. The most common adverse events of this type were local pain from needling (range: 1.1–2.9%) and slight bleeding or haematoma (range: 2.1–6.1%). In a prospective observational study of 190 924 patients, the incidence of serious adverse events (death, organ trauma or hospital admission) was about 0.024%.5 Another large-scale observational study showed a rate of adverse events requiring specific treatment of 2.2% (4963 incidents among 229 230 subjects).6 Studies such as these have shown that in extremely rare cases acupuncture can lead to serious, sometimes life-threatening complications, in addition to mild and transient adverse events.
Because most reports on the safety of acupuncture have been published outside China, the objective of this article was to summarize the Chinese literature on the subject of acupuncture-related adverse events and determine the possible reasons that such events occur.
Methods
Inclusion/exclusion criteria
In December 2009 we searched the following electronic databases: Chinese Biomedical Literature Database (1980–2009), Chinese Journal Full-Text Database (1980–2009) and Weipu Journal Database (1989–2009). The search terms were: (acupuncture OR needle) AND (induce OR cause OR adverse event OR adverse reaction OR side effect OR complication OR harm OR risk OR mistake OR infection OR injury OR fainting OR haemorrhage OR bleeding OR death OR pneumothorax OR pain). We searched for these terms (in Chinese) as free text in the title or abstract, and we also hand-searched the reference lists of all reports located through the electronic searches.
Case reports, case series, surveys and other observational studies were included in the review if they reported factual data on complications related to acupuncture. Review articles, translations and clinical trials were excluded. The search was limited to Chinese-language papers.
Different types of acupuncture can lead to different adverse events. To present clear results, we only included reports on traditional needle acupuncture, defined as a procedure in which stainless steel filiform needles are inserted into acupoints – acupuncture points located throughout the body that are associated with specific therapeutic effects – and manipulated in place. Other types of acupuncture, such as electroacupuncture, laser acupuncture and auricular acupuncture, were excluded.
Two authors (Zhang and Shang) independently examined the titles and abstracts of all papers found through the search to determine if they fulfilled the inclusion criteria outlined above. The full texts of potentially relevant articles were retrieved for detailed assessment. Disagreements between the two authors were resolved by discussion.
Information on author, patient, acupuncturist, acupuncture site, adverse event, treatment and outcome was extracted from the primary articles and entered into a pre-formulated spreadsheet. Acupoints were described by pinyin name (i.e. the Latinized spelling of traditional Mandarin Chinese names) and code according to a standard nomenclature developed by the World Health Organization.10,11 These data have been summarized in three tables according to the type of adverse event.
Results
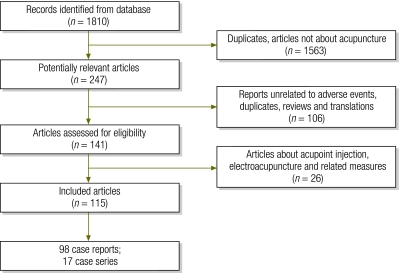
Our inclusion criteria were met by 115 articles (98 case reports and 17 case series) (Fig. 1). We noted no clear trend in the frequency of reports of acupuncture-related adverse events over the past 30 years.
Fig. 1.
Flow diagram for systematic review of the Chinese-language literature on adverse events related to traditional needle acupuncture, 1980–2009
In total, 479 cases of acupuncture-related adverse events were reported. Patients ranged in age from 2 to 73 years. The first authors of the papers were members of medical departments, court jurisdictions and police departments. Only 20% of these authors were the acupuncturists who performed the procedure that caused the adverse event. The reported acupuncture-related adverse events were classified into three categories: traumatic (Table 1, available at: http://www.who.int/bulletin/volumes/88/12/10-076737), infectious (Table 2) and “other” (Table 3).
Table 1. Traumatic events after acupuncture, as identified through a systematic review of the Chinese-language literature, 1980–2009.
| Body site and referencea | Adverse event (no. of casesb) | Acupoint (codec or site) | Outcome |
|---|---|---|---|
| Spinal cord and neighbouring tissues | |||
| Bao LP, Gao CT. Subarachnoid haemorrhage after acupuncture at Fengchi and Yamen points in 3 cases. Jilin Med J 1983;4:45–6. | Subarachnoid haemorrhage (35 cases) | GB20, GV15, GV16, GV14, BL10 | 3 deaths; 32 recoveries |
| Bian F, Zhang XL, Tian SP. Acupuncture at Fengchi point caused subarachnoid haemorrhage. J Zhangjiakou Med College 1997;14:73. | |||
| Chen YZ, Huang WC. Acupuncture at neck points caused subarachnoid haemorrhage. Shanxi Trad Chin Med J 1985;1:47–8. | |||
| Chen MX. Acupuncture at Yamen point caused subarachnoid haemorrhage. J Pract Int Med 1987;7:355. | |||
| Jiang TZ, Chen WD, Zhang B, et al. Subarachnoid haemorrhage in 2 cases after acupuncture at the nape. J Anhui Trad Chin Med Coll 1996;15:48. | |||
| Li LF, Cong X, Jin QW. Acupuncture at Fengfu point caused subarachnoid haemorrhage. Chin Acu Moxibustion 2008;28:292. | |||
| Liu SX. Acupuncture at Fengchi point caused subarachnoid haemorrhage. Shanxi Med J 1980;9:53. | |||
| Liu ZH, Xiao HP, Liu JS, et al. Subarachnoid haemorrhage in 12 cases after acupuncture at nape. People’s Mil Surg 1984;12:51–2. | |||
| Liu FY. Acupuncture at Fengchi point caused subdural haematoma. Med J Liaoning 1992;6:25. | |||
| Mi XH, Li SK, Jia SK. Acupuncture at Yamen point caused subarachnoid haemorrhage. Shandong J Trad Chin Med 1989;8:22. | |||
| Niu LJ, Zhang RW. Acupuncture-induced haemorrhage in the cisterna magna. Prac J Med Pharm 2006;23:932. | |||
| Su Y, Chen HX, Chen CC, et al. Acupuncture at Yamen point caused subarachnoid haemorrhage. Shanghai J Acu Moxibustion 1985;3:22. | |||
| Wu BS, Xu QZ. One death from spinal cord injury after acupuncture at Ash acupoints in third cervical vertebra. ChinJ Forensic Med 1990;5:32–3. | |||
| Yang YD, Shi R, Ge SH. Subarachnoid haemorrhage caused by acupuncture. Liaoning J Trad Chin Med 1985;8:37. | |||
| Yu BR. Acupuncture at nape points caused subarachnoid haemorrhage in 7 cases. J Apoplexy Nerv Dis 1986;3:74–5. | |||
| Zhou JW. Acupuncture at Fengchi point caused one death. J Sichuan Trad Chin Med 1988;10:52. | |||
| Li YQ, Chen GW. Acupuncture caused epidural haemorrhage in cervical spine. Chin Comm Doctors 2003;19:46–7. | Spinal epidural haematoma (9 cases) | – | 9 recoveries |
| Liu FY. Acupuncture at Fengchi point caused subdural haematoma. Med J Liaoning 1992;6:25. | |||
| Zhang J. Diagnosis and treatment of spinal epidural haematoma caused by acupuncture. Mod Med Health 2006;22:2924–5. | |||
| Thoracic organs and tissues | |||
| Chang JY. Acupuncture at back acupoints caused haemopneumothorax. Hebei J Trad Chin Med 1984;3:48. | Pneumothorax (201 cases) | GB21, BL13, BL18, BL23, LI17, ST12, CV22, CV15, CV14, SI9, SI13 | 4 deaths; 197 recoveries |
| Ding WY. Acupuncture at chest and back points caused 10 cases of traumatic pneumothorax. Central Plains Med J 1986;4:39. | |||
| Du JY. Report of 10 cases of pneumothorax caused by acupuncture. Central Plains Med J 1981;2:22. | |||
| Duan QL, Wang SR. Lessons from 3 cases of severe complications of acupuncture. Hebei J Trad Chin Med 1984;1:36–7. | |||
| Gao CG. Two cases of bilateral pneumothorax caused by acupuncture. J Pract Med 1984;3:38–9. | |||
| Hu DR. Traumatic pneumothorax caused by acupuncture in 7 cases. Jiangxi J Trad Chin Med 1981;4:29–30. | |||
| Hu QX, Zhang HY. Acupuncture caused 9 cases of traumatic pneumothorax. Clin Med (Northfield, IL) 1987;7:331–3. | |||
| Hu YA. Acupuncture at chest acupoints caused 13 cases of pneumothorax: X-ray diagnosis and analysis. Nei Mongol J Trad Chin Med 1995;S1:51. | |||
| Jiang DG. Acupuncture at Jiuwei point caused pneumothorax. Chongqi Med J 1980;6:47. | |||
| Jin BR. Acupuncture at Quyuani point caused pneumothorax. Shanghai J Acu Moxibustion 1987;3:45. | |||
| Jin PL. Acupuncture-related accidents and their prevention. Chin J Pract Chin Mod Med 2005;8:765. | |||
| Li YC. Clinical analysis of 25 cases of acupuncture-induced pneumothorax. Chin Comm Doctors 1995;12:37–8. | |||
| Li YY, Cheng XL. One case of pneumothorax caused by acupuncture. J Handan Med Coll 1997;10:72–3. | |||
| Liu LY. One case of haemopneumothorax caused by acupuncture. J Changchun Univ Trad Chin Med 2007;23:58. | |||
| Lu B, Tian XH. One case of traumatic tension pneumothorax caused by excessively deep acupuncture. Guizhou Med J 1993;17:125. | |||
| Ma WT. Analyses of 14 cases of traumatic pneumothorax induced by acupuncture. Anhui Med J 1993;14:41. | |||
| Ma L, Zhang CJ. Clinical analysis of acupuncture-induced pneumothorax. J Clin Acu Moxibustion 1997;13:40. | |||
| Ma BZ. Acupuncture-induced traumatic pneumothorax in one case. Qinghai Med J 2007;37:41. | |||
| Ou Q, Ji JC. Acupuncture at shoulder acupoints caused 5 cases of pneumothorax. J Trad Chin Orthop Traumatol 1997;9:54. | |||
| Qin MX, Ao WH. Improper acupuncture caused pneumothorax. Clin Misdiag Misther 2003;16:76. | |||
| Ruan KY, Qi KJ, Mou ZC. Acupuncture at points in supraclavicular fossa caused hydropneumothorax. New J Trad Chin Med 1992;4:33. | |||
| Shi YK. Lessons from 38 cases of pneumothorax caused by acupuncture. People’s. Mil Surg 1980;10:53. | |||
| Song BZ, Xu JS. One case haemopneumothorax caused by acupuncture at left Jianjin point. J Anhui Trad Chin Med Coll 1987;6:45. | |||
| Song QL, Wu TY. Three therapeutic errors of acupuncture. Clin Misdiag Misther 2001;14:73. | |||
| Wang DS. Acupuncture at epigastrium caused pleural effusion. People’s. Mil Surg 1982;10:73. | |||
| Wang YL. One death from pneumothorax caused by acupuncture at bilateral Tianding points. J Forensic Med 1999;15:47–8. | |||
| Xia C. Treating acupuncture-induced accidents. J Clin Acu Moxibustion 1993;2:75–6. | |||
| Yan ZC. Acupuncture at Tiantu point caused severe pneumothorax. New Chin Med 1985;16:655. | |||
| Zha CH. Identification of haemopneumothorax after acupuncture from piercing of the left lung. Chin J Forensic Med 2006;21:75–6. | |||
| Zhang SP. Acupuncture caused haemopneumothorax. Shanghai J Acu Moxibustion 1986;4:21. | |||
| Zhang CY, Zheng SM, Pei YF. Five cases of accidental injury of internal organs caused by improper acupuncture. Heilongjiang J Trad Chin Med 1992;1:38. | |||
| Zhao DY, Zhang GL. Clinical analysis of 38 cases of pneumothorax induced by acupuncture or injection at acupoint. Chin Acu Moxibustion 2009;29:239–42. | |||
| Zheng PD, Pang SH. Acupuncture caused severe haemopneumothorax. J Trad Chin Med 1983;5:32. | |||
| Zhu ZH, Shen H. Accidental pneumothorax caused by acupuncture therapy. Int J Emerg Crit Care Med 2005;2:992–5. | |||
| Zong WJ. Pneumothorax caused by acupuncture in 5 cases. Shanghai J Acu Moxibustion 1984;1:24. | |||
| Yang ST. Acupuncture at Feishu point caused chylothorax. J Clin Acu Moxibustion 1991;4:19. | Chylothorax (1 case) | BL13 | Recovery |
| Huo SH, Tian YP, Ma QL, et al. Acupuncture caused cardiac injury with pneumothorax. Chin J Crit Care Med 2007;27:908. | Right ventricular puncture (4 cases) | CV15, 2nd–3th ICR near sternal edge; precordial region; under right breast | 2 deaths; 2 recoveries |
| Luo YZ, Dong L, Yuan HS, et al. Acupuncture caused pulsus tardus and cardiac tamponade. Chin J Clin Thorac Cardiovasc Surg 2006;13:343. | |||
| Zhu WT, Li XS, Zhang YT, et al. Acupuncture caused death from cardiac rupture. J Forensic Med 2008;24:312. | |||
| Xie JZ, Lin WZ. Acupuncture causes death from cardiac injury. Chin J Integr Trad West Med Int Crit Care 2003;1:51. | |||
| Zhu J. Acupuncture at Qimen point induced death from aortic haemorrhage. Shanghai J Acu Moxibustion 1990;2:31. | Aortic artery rupture (1 case) | LR14 | Death |
| Gen JQ. Successful management of acupuncture-induced coronary artery injury with acute cardiac tamponade. J Clin Cardiol 2005;21:392. | Coronary artery puncture with cardiac tamponade (1 case) | LU1 | Recovery |
| Abdominal organs and tissues | |||
| Zhang JH. Acupuncture at abdominal acupoints caused 4 cases of peritonitis. Chin Rural Doctor 1997;4:20–1. | Peritonitis (2 cases) | – | Recovery |
| Zheng BS, Zhao ML. Lessons from 2 cases of gallbladder perforation complicated with bile peritonitis caused by acupuncture. Chin J Clin 1983;3:44. | |||
| Wu DP, He RL. Gallbladder perforation complicated with bile peritonitis, 2 cases caused by acupuncture. Shanxi J Trad Chin Med 1981;S1:44. | |||
| Bai XF. Acupuncture-induced gallbladder perforation with bile peritonitis. Inner Mongolia Med J 1991;11:80. | |||
| Liu JC, Liu HY. Gallbladder perforation, 2 cases caused by acupuncture. Chin J Bases Clin Gen Surg 2001;8:226. | Perforated gallbladder (7 cases, 5 with peritonitis) | ST25, CV12 | Recovery |
| Duan QL, Wang SR. Severe complications caused by acupuncture in 3 cases. Hebei J Trad Chin Med 1984;1:36–7. | Intestinal perforation (5 cases, all with peritonitis) | – | Recovery |
| Wang MY. Serious consequences of acupuncture at abdominal acupoints in 2 cases. People’s. Mil Surg 1985;6:61–2. | |||
| Zhang JH. Acupuncture at abdominal acupoints caused 2 cases of peritonitis. Chin Rural Doctor 1997;4:20–1. | |||
| Xiao XT. Gastric perforation caused by acupuncture. Chin J Clin 1985;1:9. | Gastric perforation (1 case, with peritonitis) | CV12 | Recovery |
| Liu WG, Duan LJ, Sun DT. Acupuncture at Tianshu point caused intestinal obstruction. Chin J Int Trad West Med 1992;3:147. | Intestinal wall haematoma with obstruction (1 case) | ST25 | Recovery |
| Neck area | |||
| Zhu J. Acupuncture at Tiantu point caused one death. Jiangsu J Trad Chin Med 1986;2:28. | Injury of inferior laryngeal nerve and trachea (1 case) | CV22 | Death |
| Gao LW. Acupuncture at Futu point caused dyspnoea. Chin J Trad Chin Med Pharm 1989;2:50. | Vocal cord paralysis; subcutaneous emphysema (1 case) | LI18 | Recovery |
| Zhou LZ, Zhao DG, Peng L. Opinions regarding acupuncture-induced hoarseness. Shanghai J Acu Moxibustion 2005;27:27. | Hoarseness (1 case) | Nape area | Recovery |
| Yan BX. Acupuncture at brachial plexus caused phrenic nerve injury. Shaanxi J Trad Chin Med 1994;15:513. | Injury of phrenic nerve (1 case) | Bicong | Recovery |
| Cai XJ. Acupuncture caused thyroid capsule haemorrhage with asphyxia. Med J Chin People's Liberation Army 1991;6:494. | Thyroid haemorrhage; infection (1 case) | Neck area | Recovery |
| Chen SM. Acupuncture caused traumatic carotid artery aneurysm. J Trad Chin Med 1980;7:49. | False aneurysm of carotid artery (1 case) | Neck area | Recovery |
| Eye area | |||
| Jin PL. A discussion of acupuncture-related accidents and their prevention. Chin J Pract Chin Mod Med 2005;8:765. | Orbital haemorrhage (3 cases) | SL1, EX-HN7 | 2 recoveries; 1 Visual impairment |
| Xu RZ. Acupuncture at Jingming point caused exophthalmos: prevention and countermeasures. J Clin Acu Moxibustion 2003;19:22. | |||
| Yang G, Wang SL. Blindness caused by acupuncture. Tianjin J Trad Chin Med 1996;13:6. | |||
| Yang G, Wang SL. Blindness caused by acupuncture. Tianjin J Trad Chin Med 1996;13:6. | Traumatic cataract (1 case) | Superciliary acupoints | Visual impairment |
| Xu LH, Liu AH. Oculomotor nerve injury caused by acupuncture. Chin J Ocular Trauma Occup Eye Dis 1997;19:226. | Injury of oculomotor nerve (1 case) | ST1 | Recovery |
| Liu BS, Li ZX, Lei F. Acupuncture-induced retinal detachment. Chin J Ocular Trauma Occup Eye Dis 1988;1:43–4. | Retinal injury (1 case) | Eyelid | Recovery |
| Peripheral nerves and blood vessels | |||
| Ding XY, Liu SY. Accident due to clinical acupuncture. Chin Acu Moxibustion 2008;28:817–8. | Leg, haemorrhage; diabetic foot (1 case) | ST38, BL57 | – |
| Xia C. Treating acupuncture-induced accident. J Clin Acu Moxibustion 1993;2:75–6. | Cheeks, haematoma (1 case) | ST5 | Recovery |
| Han LX. Acupuncture at Lianquan point caused sublingual fold haematoma. Shanghai J Acu Moxibustion 1994;13:107. | Hypoglottis, haematoma (2 cases) | CV23 | Recovery |
| Wang NR. Acupuncture at Lianquan point caused sublingual haematoma. J Clin Acu Moxibustion 1996;7:89. | |||
| Ou LS, Liu DC, Tian LY, et al. Acupuncture at Hegu point caused thumb adduction deformity in 12 children. J Anhui Trad Chin Med Coll 1989;8:40. | Adduction deformity of thumb (3 cases) | LI4 | Recovery |
| Wang SF. Acupuncture at Taiyang point caused adverse reactions from improper manipulation in 2 cases. Central Plains Med J 1982;3:135. | Inability to close eye (1 case) | EX-HN5 | Recovery |
| Wang SF. Acupuncture at Taiyang point caused adverse reactions from improper manipulation in 2 cases. Central Plains Med J 1982;3:185. | Inability to shut mouth (1 case) | EX-HN5 | Recovery |
| Wang L. Acupuncture at Neiguan point induced hand muscle contracture. Shanghai J Acu Moxibustion 1991;2:45. | Palmar muscle contracture (2 cases) | PC6 | Recovery |
| Needling site | |||
| Feng B, Huang YX. Adverse events caused by improper acupuncture. J Clin Acu Moxibustion 1996;12:42. | Pain (4 cases) | SI3, LI11, hand acupoints | Recovery |
| Shi GP, Chen ZM. Analysis of 3 accidents caused by acupuncture. J Clin Acu Moxibustion 1994;10:38. | |||
| Li SL, Cui XM. Fractured acupuncture needle caused intra-abdominal lump. Shanghai J Acu Moxibustion 1992;3:32. | Broken needle (1 case) | – | Recovery |
a All references in this table are in Chinese. The English-language paper and journal titles are free translations. The original Chinese-language titles can be obtained from the corresponding author.
b Only cases of traditional needle acupuncture are included. This explains any discrepancy between the number of cases in this column and the title of the corresponding reference.
Table 2. Case reports of infection after traditional needle acupuncture, as identified through a systematic review of the Chinese-language literature, 1980–2009.
| Referencea | Casesb (age in years and sex) | Reason for acupuncture | Acupoint (codec or site) | Adverse event | Outcome | Caused by acupuncture? |
|---|---|---|---|---|---|---|
| Zhang JG. Acupuncture caused buccal space abscess. Med J Chin People's Armed Police Forces 2007;18:778. | 23, male | Toothache | Buccal region | Buccal space abscess | Recovery | Probably |
| Zhao YJ. Acupuncture induced temporal space abscess. Chin J Med Today 2003;3:71. | 52, male | Toothache | Buccal region | Temporal space abscess | Recovery | Probably |
| Ma JF, Wang KK, Tian ZC. Acupuncture-induced infection in buttocks with extensive subcutaneous tissue necrosis. Chin Pract J Rural Doctor 1990;2:30–1. | 45, male | Gluteal numbness | Gluteal region | Gluteal abscess | Recovery | Certainly |
| Chen YS, Gao L. Brain abscess after acupuncture in the head. People’s Mil Surg 1995;4:58. | 30, male | Insomnia, dizziness | Cephalic region | Abscess of scalp, intracranial abscess | Recovery | Certainly |
| Xu CZ. Intracranial infection caused by acupuncture. Nei Mongol J Trad Chin Med 1990;1:12. | 19, male | Headache | Cephalic region | Abscess of scalp, intracranial abscess | Recovery | Certainly |
| Song QL, Wu TY. Three therapeutic acupuncture errors. Clin Misdiag Misther 2001;14:73. | 38, male | Arthritis | EX-LE5 | Suppurative arthritis | Recovery | Certainly |
| Zhou Z. Superficial tuberculous abscess caused by acupuncture in 3 cases. Jiujiang Med J 1999;1:47. | 22–28, 1 male & 2 females | Psoatic strain | Lower back | Tuberculous abscess | Recovery | Probably |
| Liu CR. Acupuncture-induced tetanus. Chin Pract J Rural Doctor 1992;4:30. | 52, female | Leg pain | – | Tetanus | Recovery | Probably |
| Liu GX. Acupuncture caused tetanus. J Med Theor Pract 1991;4:30. | 52, female | Headache | Cephalic region | Tetanus | Recovery | Probably |
a All references in this table are in Chinese. The English-language paper and journal titles are free translations. The original Chinese-language titles can be obtained from the corresponding author.
b Only cases of traditional needle acupuncture are included. This explains any discrepancy between the number of cases in this column and the title of the corresponding reference.
Table 3. Acupuncture-related adverse events other than trauma and infection, as identified through a systematic review of the Chinese-language literature, 1980–2009.
| Referencea | Casesb (age in years and sex, or no. of cases) | Reason for acupuncture | Acupoint (codec or site) | Adverse event | Outcome | Caused by acupuncture? |
|---|---|---|---|---|---|---|
| Liu CB. Acupuncture-related syncope in 4 cases. J Clin Acu Moxibustion 2001;17:51. | 34, 45 & 56, females | Low back pain; shoulder pain | Fainting | Recovery | Certainly | |
| Liu YZ. Improper posture caused by acupuncture in 2 cases. Lishizhen Med Materia Med Res 2007;18:1756. | 42, female | Shoulder pain | Shoulder site | Fainting | Recovery | Certainly |
| Shi GP, Chen ZM. Accidents caused by acupuncture in 3 cases. J Clin Acu Moxibustion 1994;10:38. | 57, female | Stomach ache | – | Fainting | Recovery | Certainly |
| Xu GP, Yuan YM. First aid and care of 82 fainting episodes during acupuncture. China Health care Innov 2007;2:125. | 82 cases | – | – | Fainting | Recovery | Certainly |
| You Y. Fainting during acupuncture in 60 flight personnel. Chin J Misdiag 2007;7:5668–9. | 60 cases | – | – | Fainting | Recovery | Certainly |
| Zhang H, Sun S. Fainting during acupuncture and its management in 3 cases. China. Pract Med (Barc) 2008;13:137–8. | 35 & 45, males 30, female | Cervical spondylosis | Cervical site | Fainting | Recovery | Certainly |
| Kang YH. Stroke after acupuncture: first-aid care and lesson. Jilin Med Inf 1994;7:29. | 72, female | Arm pain, rheumatoid arthritis | LI4, LI10, LI11, SJ3 | Stroke | Recovery | Probably |
| Feng B, Huang YX. Adverse events after improper acupuncture. J Clin Acu Moxibustion 1996;12:42. | 65, male | Stroke-related hemiplegia | GB20, CV23 | Stroke | Recovery | Probably |
| Mi J. Recurrent cerebral haemorrhage caused by acupuncture. Heilongjiang J Trad Chin Med 1993;2:34. | 73, male | Sequela of cerebral haemorrhage | LI4, LI11, ST36, etc. | Cerebral haemorrhage | Death | Probably |
| Song QL, Wu TY. Three therapeutic acupuncture errors. Clin Misdiag Misther 2001;14:73. | 58, male | Sequela of cerebral haemorrhage | KI1 | Cerebral haemorrhage | Death | Probably |
| Zhou TQ, Zhang HY. Acupuncture-induced fatal haemorrhagic stroke. Xinjiang J Trad Chin Med 1985;4:24–5. | 59, male | Sequela of stroke | EX-HN5, GV20, GB20 | Cerebral haemorrhage | Death | Probably |
| Ma ZH. Acupuncture-induced cardiac arrest. Hebei J Trad Chin Med 2005;27:589. | 28, male | Tic douloureu | EX-HN5, LI4, SJ5 | Cardiac arrest | Recovery | Probably |
| Zhang CY, Zheng SM, Pei YF. Accidental injury to internal organs caused by improper acupuncture in 5 cases. Heilongjiang J Trad Chin Med 1992;1:38. | 39, male | Asthma | BL13 | Shock | Recovery | Certainly |
| Wang L. Acupuncture-induced petit mal epilepsy. Chin Acu Moxibustion 2004;S1:96. | 35, male | Cheiralgia | Painful spot | Pyknolepsy | Recovery | Probably |
| Gan ZZ. Acupuncture at Taiyang point caused severe orbital haemorrhage. Chin J Ocular Trauma Occup Eye Dis 2000;22:246. | 46, female | Cold, headache | EX-HN5 | Orbital haemorrhage | Recovery | Probably |
| Li JS. Acupuncture-induced fever. Chin Acu Moxibustion 2000;10:639. | 52, male | Sequela of brain concussion | GV20, GB20, LI11, LI4, etc. | Fever | Recovery | Probably |
| Shang YT. Adverse events caused by acupuncture in 2 cases. New J Trad Chin Med 2006;38:76. | 65, female | Facioplegia | GB14, LI4 | Cough | Recovery | Probably |
| 46, female | Obesity | ST25, SP15 | Thirst | Recovery | Certainly | |
| Wang SF, Lan YH. Acupuncture at Neiguan point caused sudden aphonia. New Chin Med 1980;11:587–8. | 36, female 46, male | Hiccups | PC6 | Aphonia | Recovery | Probably |
| Li M. Acupuncture at Houxi point caused left lower extremity numbness. J Shanxi Trad Chin Med Coll 1994;1:37. | 47, female | Sciatica | SI3 | Leg numbness | – | Probably |
| Yang XH, Zhang GS. Long-term acupuncture at Guanyuan point caused sexual dysfunction in 2 men with obesity. Chin J Hum Sex 2009;18:19–20. | 52, male 41, female | Simple obesity | CV4 | Sexual dysfunction | Recovery | Probably |
| Zhang RM. Misuse of acupuncture in 2 cases. Jiangxi J Trad Chin Med 1992;23:47. | 20, male | Headache | KI1 | Spermatorrhea | Recovery | Probably |
| Lan XL, Du XH. Allergic skin rash induced by acupuncture. J Yunyang Med Coll 2004;23:378. | 50, male | Cervical spondylosis | GB20, etc | Skin rash | Recovery | Certainly |
| Cheng C. Acupuncture caused widespread allergic erythema. Jiangxi J Trad Chin Med 1988;2:52. | 11, female | Coxarthritis | BL57, BL40 | Metal allergy | Recovery | Certainly |
| Guo YJ. Allergy to metal needles in 2 cases. Chin Acu Moxibustion 2006;26:307–8. | 33 & 52, females | Abdominal pain | – | Metal allergy | Recovery | Certainly |
a All references in this table are in Chinese. The English-language paper and journal titles are free translations. The original Chinese-language titles can be obtained from the corresponding author.
b Only cases of traditional needle acupuncture are included. This explains any discrepancy between the number of cases in this column and the title of the corresponding reference.
Traumatic events
Traumatic injuries were reported in 87 articles (73 case reports and 14 case series) and totalled 296 cases. The events were classified into seven subgroups according to the type and site of the injury.
Arachnoid and spinal dura mater
Nine cases of spinal epidural haematoma (in the cervical, thoracic and lumbar spine) were reported. No further information was provided.
Subarachnoid haemorrhage was reported in 35 patients, 3 of whom died. The others recovered after 1 to 8 weeks of treatment. One of the deceased patients had a history of hypertension and cerebral haemorrhage and died 10 days after the acupuncture. The other two patients died within 30 minutes of having undergone the acupuncture, perhaps as a result of injury to the medulla oblongata.
The acupoints most frequently involved in cases of subarachnoid haemorrhage and spinal epidural haematoma were Fengchi (GB20), Yamen (GV15), Fengfu (GV16), Dazhui (GV14) and Tianzhu (BL10). In several cases, the needles were inserted to a depth of 4 to 5 cm below the skin’s surface, and such deep insertion is suspected to have led to injury.
Thoracic organs and tissues
With a total of 201 cases, pneumothorax was the most frequently reported acupuncture-related adverse event. Four patients died from it and the others recovered after 2 to 30 days of treatment. One patient was a 70-year-old woman with a history of chronic bronchitis, emphysema, cor pulmonale and heart failure who died from pulmonary infection, heart failure and pneumothorax. Two more women died after not receiving timely treatment for pneumothorax caused by needling at the Jianjing (GB21) and Tianding (LI17) acupoints. The fourth patient died from tension pneumothorax but no further information was provided.
The acupuncture sites in these cases were primarily in the shoulder and scapular regions (64%) and in the chest (24%). In two cases, the Tianding (LI17) point in the neck area had been needled. The most frequently used acupoints were Jianjing (GB21; 30%), Feishu (BL13; 15%), Quepen (ST12; 10%) and Tiantu (CV22; 10%). Other acupoints were Ganshu (BL18), Shenshu (BL23), Tianding (LI17), Jiuwei (CV15), Juque (CV14), Jianzhen (SI9), Quyuan (SI13) and Dingchuan (EX-B1).
Chylothorax was reported after needling at the Feishu (BL13) point in a 21-year-old man with a malformed thoracic duct. Right ventricular injury was reported in four cases, two of which recovered after surgical treatment. The other two patients died from right ventricular puncture complicated by cardiac tamponade and multiorgan dysfunction syndrome. One case of aortic artery rupture was reported after needling at the Qimen point (LR14) at a depth of 4 cm; the patient died within 15 minutes. Coronary artery injury with cardiac tamponade was reported in a man who treated himself for chronic bronchitis and lost the needle at the Zhongfu point (LU1).
Abdominal organs and tissues
Injuries of abdominal organs and tissues were reported in 16 patients, all of whom recovered after surgery. These instances included perforations of the gallbladder, of the bowels and of the stomach, frequently complicated by peritonitis. A 2-year-old boy suffered intestinal wall haematoma with intestinal obstruction after acupuncture treatment for diarrhoea.
The acupoints associated with such adverse events were Tianshu (ST25), Zhongwan (CV12) and Qimen (LR14). Most of the patients underwent acupuncture for abdominal pain, attributable mainly to appendicitis or cholecystitis. Deep needling accounted for most of the abdominal injuries.
Neck area
Six cases of injuries in the neck region were reported, including neural injuries (4), a false aneurysm of the carotid artery (1) and thyroid haemorrhage (1). One patient died after acupuncture at the Tiantu point (CV22); the needle had been inserted to a depth of 6 cm.
Eyes
Five articles reported injuries to the eyes, including orbital haemorrhage (3), traumatic cataract (1), injury of the oculomotor nerve (1) and retinal puncture (1). One case of optic atrophy accompanied by haemorrhage and traumatic cataract resulted in visual impairment.
The acupoints in the above cases were Jingming (SL1), Qiuhou (EX-HN7) and Chengqi (ST1). When needling acupoints in the area of the orbital cavity, bleeding is difficult to avoid, even for the experienced acupuncturist. Deep needling can also injure the oculomotor nerve, the retina and neighbouring tissues.
Peripheral nerves, vessels and other tissues
Three cases of haemorrhage were reported after acupuncture on the cheeks and the hypoglottis. One case of calf haematoma complicated by diabetic foot was caused by needling at the Tiaokou (ST38) and Chengshan (BL57) acupoints.
Four cases of peripheral motor nerve injuries and subsequent motor dysfunction were reported. Three children suffered adductor muscle fibrosis and adduction deformity of the thumb as a result of local vascular and muscular injuries from needling at the Hegu point (LI4).
The acupoints most frequently involved in the injuries were Taiyang (EX-HN5), Neiguan (PC6) and Hegu (LI4). Forceful needle manipulation at these points, which are quite superficial, can cause injury to peripheral nerves, capillaries and muscle fibres.
Needling site pain and broken needle
Four cases of pain at the needling site were reported in two articles. An intra-abdominal lump turned out to be caused by an acupuncture needle fragment that had broken off 15 years earlier.
Infectious events
Nine cases of bacterial infection and two cases of viral infection were reported. All patients recovered after appropriate treatment.
Infections were mainly due to poor sterilization of acupuncture needles. Acupoints on the head became infected most often, perhaps because hair makes it difficult to implement aseptic technique. Two cases of facial abscess may have been caused by acupuncture to relieve toothache.
Other adverse events
A total of 172 acupuncture-related adverse events that were neither due to trauma nor to infection were reported. Local allergic reactions occurred after acupuncture in four patients with an allergy to metal needles.
In our review, fainting was the most common adverse event associated with acupuncture, and it occurred primarily in patients receiving acupuncture for the first time. In total, 150 cases of fainting were reported. In one report of 82 cases, 60% (49) of the patients fainted during the first treatment. Of these 49 fainting spells, 83% occurred when acupuncture was being applied to the head or neck.
Stroke after acupuncture was reported in five patients (aged from 58 to 73 years). One case of stroke occurred in a 72-year-old woman who received acupuncture on her arm. The other four patients had a history of stroke and hypertension. Three patients died from cerebral haemorrhage that was considered to be causally related to the acupuncture.
Other adverse effects included cardiac arrest, pyknolepsy (epileptiform attacks resembling petit mal), shock, fever, cough, thirst, aphonia, leg numbness and sexual dysfunction. However, the existence of a causal link between acupuncture and these adverse events is uncertain.
Discussion
Many types of acupuncture-related adverse events have been identified in the Chinese literature. Injuries and infections appear to be related to inappropriate technique, whereas other types of adverse events are not. Fainting is vasovagal in origin and minor bleeding is sometimes inevitable.
Infections result primarily from poor aseptic procedure and insufficient knowledge on the part of acupuncturists, who often disinfect reusable acupuncture needles with alcohol instead of sterilizing them. The use of disposable sterile acupuncture needles and guide tubes is strongly recommended.12
Most traumatic events are caused by improper manipulation in high-risk acupoints. The depth of needle insertion is crucial. The lung surface is about 10 to 20 mm beneath the skin in the region of the medial scapular or midclavicular line.2 This may explain the high incidence of pneumothorax during needling in this area. Other traumatic complications, such as subarachnoid haemorrhage, cardiovascular injuries or perforation of the gallbladder, can also be caused by excessively deep needle insertion.
The patient’s condition also needs to be considered. Cardiovascular trauma occurred most frequently in patients with cardiomegaly. Patients with abdominal pain that has no clear diagnosis are at increased risk of trauma or infection from acupuncture at abdominal acupoints. Symptomatic treatment of abdominal pain with acupuncture can also delay effective therapy. During needling at peripheral acupoints on the legs, arms and face, manipulation should be carefully executed to avoid damaging nerves and blood vessels.
Some adverse events are inevitable but could be minimized through preventive measures. Fainting, which is a reflex caused by vagal excitation, is the most common adverse event during acupuncture.13 Its incidence can be reduced by preparing patients and positioning them properly; the patient should not be hungry or tired and should preferably be placed in the supine, lateral or prone position.
Of the 87 articles reporting traumatic events, 59 (70%) provided information about the acupuncturists. Of these 59 articles, 68% (40) indicated that the acupuncturists were practising in village clinics or rural hospitals when they performed the procedures that caused the traumatic events. All infections reported were caused by acupuncturists in rural areas. In China, acupuncturists in rural and urban hospitals have a great disparity in clinical skills. Acupuncturists practising in rural hospitals, township health centres or village clinics rarely receive formal education in medical colleges. It follows that training for the practice of acupuncture needs to be unified and improved.
Several serious adverse events were identified through a review of case reports,14 but very few were found in surveys7–9 or prospective observational studies.5,6 This suggests that serious acupuncture-related adverse events are rare. Bleeding and pain during needling are reported less often in the Chinese-language than in the English-language literature, perhaps because practitioners in China consider such events too trivial to report. Infections (primarily hepatitis) after acupuncture are reported frequently in the English-language literature1 but relatively rarely in the Chinese-language literature, even though non-disposable acupuncture needles are still used in China. It is possible that in China acupuncture-related infections are underreported.
Of the 87 articles reporting traumatic injuries, 72 (about 70%) were authored not by the acupuncturists themselves, but by the physicians who treated the adverse events. None of the articles reporting infections were authored by the acupuncturists, as opposed to 16 of the 20 (80%) reports of adverse events other than trauma or infection. Again, we suspect that underreporting of such events in the Chinese-language literature is much higher than in the English-language literature.
Our review has several limitations. Although our search strategy was comprehensive, we cannot guarantee that all relevant articles were identified. Many of the reports lacked detail, so that cause–effect relationships are often uncertain. In the absence of a denominator (i.e. the total number of acupuncture treatments practised over the study period), the reported adverse events do not lend themselves to generating incidence figures. There are 2688 hospitals of traditional Chinese medicine in China.15 If we assume, for instance, that each hospital receives 50 to 100 visits for acupuncture per day (a conservative figure), the annual number of acupuncture treatments would total from 50 to 100 million. This would suggest that the incidence of acupuncture-related adverse events is negligible. However, the true incidence remains unknown and cannot be accurately estimated. Collectively these factors limit the conclusiveness of our findings.
Conclusion
Various types of acupuncture-related adverse events have been reported in China. Similar events have been reported by other countries,1–9 usually as a result of inappropriate technique. Acupuncture can be considered inherently safe in the hands of well trained practitioners. However, there is a need to find effective ways to improve the practice of acupuncture and to monitor and minimize the health risks involved.
Acknowledgements
The authors thank YY Xu, X Zhang and WK Zheng for their help with the literature search.
Competing interests:
None declared.
References
- 1.Norheim AJ. Adverse effects of acupuncture: a study of the literature for the years 1981–1994. J Altern Complement Med. 1996;2:291–7. doi: 10.1089/acm.1996.2.291. [DOI] [PubMed] [Google Scholar]
- 2.Peuker ET, White A, Ernst E, Pera F, Filler TJ. Traumatic complications of acupuncture. Therapists need to know human anatomy. Arch Fam Med. 1999;8:553–8. doi: 10.1001/archfami.8.6.553. [DOI] [PubMed] [Google Scholar]
- 3.Yamashita H, Tsukayama H, White AR, Tanno Y, Sugishita C, Ernst E. Systematic review of adverse events following acupuncture: the Japanese literature. Complement Ther Med. 2001;9:98–104. doi: 10.1054/ctim.2001.0446. [DOI] [PubMed] [Google Scholar]
- 4.Ernst E, Sherman KJ. Is acupuncture a risk factor for hepatitis? Systematic review of epidemiological studies. J Gastroenterol Hepatol. 2003;18:1231–6. doi: 10.1046/j.1440-1746.2003.03135.x. [DOI] [PubMed] [Google Scholar]
- 5.Endres HG, Molsberger A, Lungenhausen M, Trampisch HJ. An internal standard for verifying the accuracy of serious adverse event reporting: the example of an acupuncture study of 190,924 patients. Eur J Med Res. 2004;9:545–51. [PubMed] [Google Scholar]
- 6.Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16:91–7. doi: 10.1159/000209315. [DOI] [PubMed] [Google Scholar]
- 7.Norheim AJ, Fønnebø V. Acupuncture adverse effects are more than occasional case reports: Results from questionnaires among 1135 randomly selected doctors, and 197 acupuncturists. Complement Ther Med. 1996;4:8–13. doi: 10.1016/S0965-2299(96)80049-5. [DOI] [Google Scholar]
- 8.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001;323:485–6. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macpherson H, Scullion A, Thomas KJ, Walters S. Patient reports of adverse events associated with acupuncture treatment: a prospective national survey. Qual Saf Health Care. 2004;13:349–55. doi: 10.1136/qshc.2003.009134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.A proposed standard international acupuncture nomenclature: report of a WHO scientific group. Geneva: World Health Organization; 1991. [Google Scholar]
- 11.WHO standard acupuncture point locations in the Western Pacific Region. Geneva: World Health Organization; 2008. [Google Scholar]
- 12.Guidelines on basic training and safety in acupuncture. Geneva: World Health Organization; 1999. [Google Scholar]
- 13.He J, Tang QF, Zhuang LX. Clinical analysis of the therapeutic effect of fainting during acupuncture and preliminary study of the mechanism. Chin Acu Moxibustion. 2004;24:553–5. [Google Scholar]
- 14.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72–83. [PubMed] [Google Scholar]
- 15.Ministry of Health of the People’s Republic of China [Internet]. Beijing: Ministry of Health; 2010. Available from: http://www.moh.gov.cn [accessed 11 August 2010]. Chinese.