Congestive heart failure (CHF) continues to account for 3% of admissions to hospitals in the United States, and the diagnosis carries a mortality rate of 20% at one year and 80% at eight years.1,2 There have been numerous advances in the chronic medical management of CHF, including angiotensin antagonists, beta blockers, and aldosterone antagonists, all of which have shown significant mortality reductions in clinical trial populations with varying degrees of CHF severity.2–4 Evidence from clinical trials, however, does not always readily translate to community practice.5,6 Previous studies in outpatient populations in the late 1990s and the early 2000s observed suboptimal use of evidence-based therapy for CHF. Using nationally representative data, we evaluated whether patterns of medication use have improved over time.
Methods
We used data from the National Disease and Therapeutic Index (NDTI) physician survey produced by IMS Health (Plymouth Meeting PA) to characterize contemporary trends in the outpatient use of recommended medications for CHF from January 1994 through March 2009. The NDTI is an ongoing physician survey that provides nationally representative diagnostic and medication use information on patients treated by office-based, private practice physicians in the continental United States.
We employed descriptive statistical analysis to determine the proportion of use of each drug class in various cohorts. The outcome measure was proportion of visits where the use of the selected medications was reported. For the NDTI estimates, 95% confidence intervals (CIs) were calculated using tables of relative standard errors that accounted for the complex NDTI sampling design.
Results
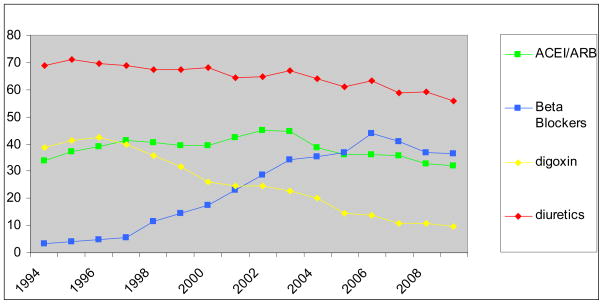
A gradual decline in the number of patient visits for CHF occurred over the 15 year study period: from 10.9 million non-hospital visits in 1994 to 8.5 in 2000 to 5.7 million visits in 2008. Physician reported degree of CHF severity for patient visits did not change appreciably over time. ACEI or angiotensin II receptor blocker (ARB) use gradually increased from 34% in 1994 to 45% in 2002. However, after 2002 there was a steady decline in ACEI or ARB use, decreasing to 32% in 2009. Because ARB use remained steady after 1998, fluctuating between 4–9%, the trend in ACEI/ARB use was entirely due to the rise and fall in ACEI use for CHF. We observed a gradual increase in BB use for outpatient CHF visits from 11% in 1998 to a peak of 44% in 2006. After 2006, there was a decline in BB use to 37% in 2009.
There was a slow increase in aldosterone antagonist use in CHF from 1% in 1998 to 11%in 2003, maintaining a fluctuating plateau through 2009(8%–12%). We also noted a stable proportion of patients with CHF reported to be on digoxin from 1994 to 1997 at 39–43%, with a sudden, precipitous decline after 1997 to 32% in 1999 to 10% in 2008. The use of diuretics in our cohort declined slowly over fifteen years from 69% in 1994 to 56% in 2008.
Discussion
While our analysis shows initial adoption of evidence-based therapies for CHF through the 1990s and mid 2000s, uptake of these therapies has been modest. What we observe after the mid-2000s is troubling, however. Some therapies that previously were increasing slowly have reached a plateau. Other recommended therapies have declined. The persistence of this trend could lead to a regression in the beneficial outcomes purchased by the increasing use of these therapies. The current framework used to promulgate evidence-based therapy for CHF does not appear to be sufficient to maintain appropriate levels of therapy. Our results suggest that further improvements are needed; these could perhaps be attained by targeting at-risk patient subgroups and increasing utilization among providers with lower rates of recommended medication use. These measures alone may not be sufficient and given the saturation of providers with clinical guidelines, innovative approaches to facilitating evidence-based prescribing practices may be required.
Figure 1.
Reported use of medications in patients with congestive heart failure, January 1994 through March 2009, IMS Health, National Disease and Therapeutic Index (NDTI).
Acknowledgments
Dr. Banerjee is supported by an Institutional Training Award from the National Heart, Lung and Blood Institute (T32-HL07034). Dr. Stafford’s contribution to this work was supported by a mid-career development award from the National Heart, Lung and Blood Institute (K24-HL086703). The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health Incorporated information service: National Disease and Therapeutic Indextm (1994–2009), IMS Health Incorporated. All Rights Reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities. The funding source and IMS Health had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation or approval of the manuscript for publication.
Abbreviations
- CHF
congestive heart failure
- BB
beta-blocker
- ACEI
angiotensin converting enzyme inhibitors
- ARB
angiotensin receptor blockers
- NDTI
National disease and therapeutic index
- ICD-9
International Classification of Disease Codes, 9th revision, Clinical Modification
- ACC
American College of Cardiology
- AHA
American Heart Association
- CI
confidence interval
References
- 1. [accessed 1/15/10]; http://www.cdc.gov/nchs/data/series/sr_13/sr13_165.pdf#table12.
- 2.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009 Jan 27;119(3):480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 3.Packer M, Fowler MB, Roecker EB, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002 Oct 22;106(17):2194–2199. doi: 10.1161/01.cir.0000035653.72855.bf. [DOI] [PubMed] [Google Scholar]
- 4.Jhund PS, Macintyre K, Simpson CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009 Feb 3;119(4):515–523. doi: 10.1161/CIRCULATIONAHA.108.812172. [DOI] [PubMed] [Google Scholar]
- 5.Putnam W, Burge FI, Lawson B, et al. Evidence-based cardiovascular care in the community: a population-based cross-sectional study. BMC Fam Pract. 2004 Apr 1;5:6. doi: 10.1186/1471-2296-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gheorghiade M, Gattis WA, O’Connor CM. Treatment gaps in the pharmacologic management of heart failure. Rev Cardiovasc Med. 2002;3( Suppl 3):S11–19. [PubMed] [Google Scholar]