Abstract
Healthy aging is accompanied by limitations in performance of activities of daily living and personal independence. Recent reports demonstrated improvements in motor function induced by non-invasive anodal direct current stimulation (tDCS) of the primary motor cortex (M1) in young healthy adults. Here we tested the hypothesis that a single session of anodal tDCS over left M1 could facilitate performance of right upper extremity tasks required for activities of daily living (Jebsen-Taylor Hand function Test, JTT) in older subjects relative to sham in a double-blind crossover study design. We found (a) significant improvement in JTT function with tDCS relative to sham that outlasted the stimulation period by at least 30 minutes, (b) that the older the subjects the more prominent this improvement appeared and (c) that consistent with previous results in younger subjects, these effects were not accompanied by any overt undesired side effect. We conclude that anodal tDCS applied over M1 can facilitate performance of skilled hand functions required for activities of daily living in older subjects.
Introduction
Functional independence in performance of activities of daily life requires skilled hand motor control. Healthy aging is associated with slowing of movements (Bennett and Castiello, 1994), increased variability in grip and lift force production (Cole and Rotella, 2001; Cole et al., 1999), diminished accuracy of force release (Erim et al., 1999; Voelcker-Rehage and Alberts, 2005), and dexterity (Cole and Katifi, 1991), and reduced coordination in reach to grasp movements (Brown et al., 1996; Pratt et al., 1994; Sarlegna, 2006). Some of these deficits are evident for example during performance of choice-reaction times or in dualtask conditions (Ketcham et al., 2002). Ageing also leads to reorganization of neural networks engaged in performance of various sensorimotor tasks (Heuninckx et al., 2008; Talelli, Ewas et al., 2008) and to some extent to a decrease of neuronal activity in circuits involved in performance of cognitive tasks (for review Burke and Barnes, 2006; Chapman, 2005; Disterhoft and Oh, 2007; Ward et al., 2008). In the motor system, ageing is associated with changes in the excitability of the primary motor cortex (M1) (Oliviero et al., 2006; Yordanova et al., 2004), with reduced ability to encode an elementary motor memory within M1 with motor training (Sawaki et al., 2003), and possibly with reduced efficiency of training-based exercise programs relative to younger individuals. The significance of these deficits in relation to performance of activities of daily living has been explored only partially. What is known is that deficits in the motor domain appear to have more significant consequences on independent living than declines in visual or auditory functions (Anstey et al., 2005; Teasdale et al., 1991).
It has been reported that noninvasive transcranial stimulation of M1 results in improvements in motor performance (Carey et al., 2006; Fecteau et al., 2006; Kobayashi et al., 2004; Vines et al., 2006; Voss et al., 2007) and facilitates the response to motor training protocols (Butefisch et al., 2004) as well as motor learning (Nitsche, Schauenburg et al., 2003; Reis et al., 2008) in healthy younger adults. There is however a gap in knowledge on the ability of noninvasive stimulation of M1 to facilitate motor function in older subjects, in an age group characterized by declining motor function and higher susceptibility to brain lesions with subsequent invalidating motor impairment. Here, we tested the hypothesis that application of anodal tDCS over M1 would facilitate performance of a set of skilled hand motor functions required for activities of daily life (measured in the setting of the Jebsen-Taylor Hand function Test [JTT](Jebsen et al., 1969)) relative to sham stimulation in a double blind, sham-controlled cross-over experimental design.
Methods
Subjects
Ten healthy subjects (age range 56-87 years, mean 69±9.24 SD; five women) participated in the study. All of them were right-handed as assessed by the Edinburgh Handedness Inventory (Oldfield, 1971) with a score of 97.0±3.4. None reported a history of neurological disease or musculoskeletal dysfunction. In all subjects, the Mini Mental Status was within normal limits (> 29/30) (Folstein et al., 1975). Subjects were informed about the experimental procedures and gave their written informed consent according to the declaration of Helsinki. The study protocol was approved by the NINDS Institutional Review Board.
Experimental procedures
Subjects participated in three experimental sessions. In the first session, they familiarized with the Jebsen Taylor Task (JTT) task (Jebsen et al., 1969), the experimental environment and with tDCS (Fregni et al., 2005; Hummel, Celnik, Giraux et al., 2005). In this first session, they also practiced the JTT task until a plateau was reached and they could not improve further. The primary endpoint measure of the study was the time required to complete the JTT, a widely used well validated test for functional motor assessment that reflects activities of daily living (Jebsen et al., 1969), that has good validity and reliability, and for which normative data are available for different ages and genders (Hackel et al., 1992; Jebsen et al., 1969). Anodal tDCS or Sham were applied in a pseudo-randomized, counterbalanced order in separate sessions (2 and 3) separated by 5 days to the left (dominant) M1 of each subject in a double-blind, crossover order. The site for positioning the electrode for application of anodal tDCS over M1 (hand knob (Yousry et al., 1997)) was determined separately in each subject using a frameless stereotactic device (Brainsight®). In each of these two sessions, the JTT (primary outcome measure) was evaluated preceding (Baseline: JTT1-3) and following (Testing: JTT4-6) each intervention (tDCS or Sham). Four times in each session, subjects were asked to report their level of attention towards the task and perception of fatigue (before and after Baseline determination of the JTT and before and after each intervention, Fig. 1). The degree of discomfort with tDCS and Sham was evaluated one time at the end of the session using a separate visual-analogue scale (Fig. 1). Participating subjects and investigator performing motor testing and data analysis were blinded towards the type of intervention (tDCS or Sham).
Figure 1. Experimental design.
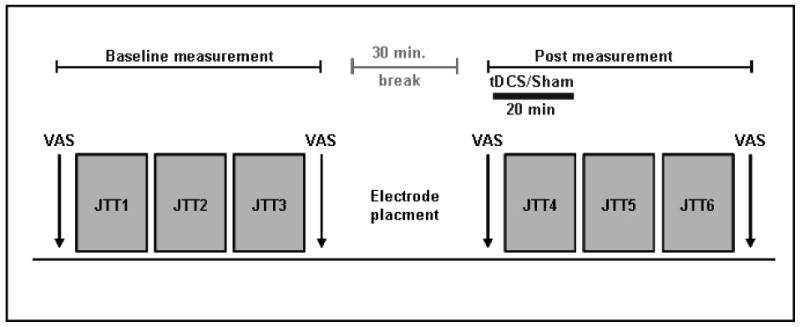
Patients participated in three sessions. In the first session, they familiarized themselves with the JTT and reached a stable level of performance. The second and third sessions started with questionnaires followed by baseline determinations of JTT (JTT1–3), cortical stimulation (tDCS) or Sham in a counterbalanced double-blind design and later by post-intervention JTT (JTT4-6), with JTT4 determined during stimulation and JTT5-6 after stimulation. Questionnaires (VAS) in which subjects characterized level of attention and fatigue during the experiment were given at four different times in each session.
Transcranial DC stimulation
Anodal tDCS (Floel and Cohen, 2007; Hummel and Cohen, 2005; Nitsche et al., 2005) was delivered for 20 minutes in the tDCS session using a Phoresor® II Auto (Model No. PM850, IOMED®, Salt Lake City, Utah 84120 USA) through two saline-soaked gel-sponge electrodes (TransQE, IOMED®, 25cm2 surface area). The anode was positioned over the hand knob area of the left M1 as determined using a frameless stereotactic device. The cathode was placed on the skin overlying the contralateral supraorbital region (Nitsche and Paulus, 2000). Anodal tDCS applied in this way results in an increase in excitability of the underlying M1 that outlasts the period of stimulation (Jeffery et al., 2007; Kwon et al., 2008; Lang et al., 2004; Lang et al., 2005; Power et al., 2006). Sham was administered according to a welldescribed protocol (Fregni et al., 2006; Gandiga et al., 2006; Hummel, Celnik, Floel et al., 2005; Hummel et al., 2006; Nitsche, Schauenburg et al., 2003). At the onset of both interventions (tDCS and sham), current (1mA) was increased in a ramp-like fashion eliciting a transient tingling sensation on the scalp that faded over seconds and that elicited comparable perceptions (Gandiga et al., 2006; Nitsche et al., in press; Nitsche, Liebetanz et al., 2003). Current remained at the 1mA level for 20 minutes in the tDCS session and for up to 30 seconds in the Sham session. In both sessions, currents were turned off slowly over a few seconds, a procedure that does not elicit perceptions and that was implemented out of the field of view of the subjects (Gandiga et al., 2006; Nitsche et al., in press; Nitsche, Liebetanz et al., 2003).
Testing of motor performance
Jebsen Taylor Hand function Test
The JTT is a measurement commonly used in neurorehabilitative settings that mimics activities of daily living (Jebsen et al., 1969). It has been well validated and is reliable in populations of different ages (Hackel et al., 1992). The 6 subtests evaluate turning cards, grasping small objects, lifting small objects with a spoon, stacking checkers, lifting light and heavy cans. Subjects were instructed to perform the tasks sequentially as quickly and accurately as possible according to standardized instructions (Jebsen et al., 1969; Stern, 1992). Feedback on task performance was not provided. Total JTT time and partial subtest times were recorded for analysis. The total JTT time is calculated as the sum of the performance time of each subtest. Dropping of an object was counted as an accuracy error and analyzed off-line.
Data analysis
Total time for JTT and time for JTT subtests were normally distributed as evaluated by Kolmogorov-Smirnov goodness of fit test. Repeated measures ANOVARM was used to evaluate the effects of TIME(base, post) and INTERVENTION(tDCS, Sham) on total JTT time. JTT subtests involving skilled distal fine hand and finger function (1. turning cards, 2. grasping small objects, 3. lifting small objects with spoon) and gross motor upper limb function (4. checkers, 5. light and 6. heavy cans) also analyzed separately. Correlations were calculated using the Pearson, 2-tailed test. Paired t-tests were used to evaluate reports of discomfort/pain. Non-parametric tests were used to evaluate the effects of INTERVENTION(tDCS, Sham) on attention fatigue, pain and discomfort, which were not normally distributed (for details see Table1). All calculations with ANOVA were Greenhouse-Geisser corrected. Conditioned on significant p-values (p<0.05), post-hoc testing was performed and corrected for multiple comparisons where necessary.
Table 1.
| A Absolute JTT time, averaged over all subjects for pre/post and sham/tDCS | |||
|---|---|---|---|
| a.) Absolute total JTT time (mean ± SEM) | |||
| pre | post | ||
| tDCS | 29.89 ± 1.42 | 28.00 ± 1.29 | |
| Sham | 28.53 ± 1.39 | 29.16 ± 1.60 | |
| b.) Absolute JTT time for gross versus fine motor tasks (mean ± SEM) | |||
| FINE MOTOR TASK | GROSS MOTOR TASK | ||
| tDCS | |||
| pre | 6.60 ± 0.41 | 3.37 ± 0.13 | |
| post | 6.11 ± 0.35 | 3.22 ± 0.12 | |
| Sham | |||
| pre | 6.16 ± 0.38 | 3.35 ± 0.12 | |
| post | 6.45 ± 0.42 | 3.27 ± 0.12 | |
| B Summary of statistical results regarding tDCS versus Sham stimulation | ||||||||
|---|---|---|---|---|---|---|---|---|
| a.) ANOVA | ||||||||
| Factor | Time (baseline vs post stimulation) | Intervention (tDCS vs Sham) | Intervention × Time | |||||
| F ratio | P value | F ratio | P value | F ratio | P value | |||
| JTT (in sec) | F = 1.638; | P = 0.233 | F = 0.053; | P = 0.824 | F = 8.068; | P = 0.019* | ||
| b) ANOVA | ||||||||
| Factor | Task (fine vs gross motor) | Intervention (tDCS vs Sham) | Intervention × Task | |||||
| F ratio | P value | F ratio | P value | F ratio | P value | |||
| JTT (in sec) | F = 2.610; | P = 0.141 | F = 6.290; | P = 0.033* | F = 6.200; | P = 0.034* | ||
| c) ANOVA | ||||||||
| Factor | Time (baseline vs post stimulation) | Run (1,2,3) | Intervention (tDCS vs Sham) | |||||
| F ratio | P value | F ratio | P value | F ratio | P value | |||
| JTT (in sec) | F = 1.743; | P = 0.203 | F = 7.436; | P = 0.002* | F = 0.008; | P = 0.929 | ||
| Factor | Time × Run | Intervention × Time | Intervention × Run | Time × Run × Intervention | ||||
| F ratio | P value | F ratio | P value | F ratio | P value | F ratio | P value | |
| JTT (in sec) | F = 1.004; | P = 0.375 | F = 7.514; | P = 0.013* | F = 0.537; | P = 0.585 | F = 0.467; | P = 0.629 |
| ANOVARM with factors (a) TIME(base, post) and INTERVENTION(tDCS, Sham) and (b) TASK(fine, gross) and INTERVENTION(tDCS, Sham) and (c) TIME(base, post), RUN(1,2,3), and INTERVENTION(tDCS, Sham) was applied to analyse the data,. P < 0.05 is defined as statistical significant (*). | ||||||||
| C Summarized data for perceived levels of attention, fatigue, pain, and discomfort during the experiment | ||||||||
|---|---|---|---|---|---|---|---|---|
| a) Absolute scores in VAS averaged for all subjects (mean ± SD) | ||||||||
| tDCS | SHAM | |||||||
| pre | post | pre | post | pre | post | pre | post | |
| Baseline | Stimulation | Baseline | Stimulation | |||||
| Attention1 | 8.7 ± 1.1 | 8.9 ± 1.4 | 8.7 ± 1.5 | 8.7 ± 1.8 | 8.2 ± 1.5 | 8.6 ± 1.3 | 8.6 ± 1.5 | 8.8 ± 1.6 |
| Fatigue2 | 8.9 ± 1.2 | 8.6 ± 1.4 | 8.4 ± 1.5 | 8.7 ± 1.8 | 8.4 ± 1.2 | 8.6 ± 1.3 | 8.4 ± 1.9 | 8.6 ± 1.5 |
| Pain3 | 1.4 ± 0.5 | 0.8 ± 0.8 | ||||||
| Discomfort3 | 1.5 ± 0.6 | 1.3 ± 1.2 | ||||||
| b) statistical analysis for change in perceived level of attention and fatigue at the four time points evaluated between interventions (tDCS versus Sham) (Kruskal-Wallis one-way analysis of variance) | ||||||||
| pre Baseline | post Baseline | pre Stimulation | post Stimulation | |||||
| Attention1 | p = 0.476 | p = 0.487 | p = 0.798 | p = 1.0 | ||||
| Fatigue2 | p = 0.386 | p = 0.958 | p = 0.840 | p = 0.679 | ||||
| statistical analysis for differences in perceived level of attention and fatigue between different time points for tDCS and Sham (Friedman Test for related samples) | ||||||||
| tDCS | Sham | |||||||
| Attention1 | p = 0.855 | p = 0.866 | ||||||
| Fatigue2 | p = 0.281 | p = 0.866 | ||||||
| c) statistical analysis for differences in perceived level of pain, and discomfort between interventions (Wilcoxon signed rank test) | ||||||||
| Pain3 | Z = -1.342; p = 0.180 | |||||||
| Discomfort3 | Z = -0.816; p = 0.414 | |||||||
VAS attention. 0=no attention at all, 10=very high level of attention.
VAS fatigue; 0= very tired, 10 not tired at all.
VAS pain and discomfort. 0 = no pain/discomfort, 10 = highest imaginable level of pain/discomfort. Evaluated only at post Stimulation.
Results
Jebsen-Taylor test
During the familiarization session, JTT performance reached a stable level, consistent with previous studies (Fregni et al., 2005; Hummel, Celnik, Giraux et al., 2005), that was comparable to the baseline JTT in sessions 2 (T=-0.19, ns) and 3 (T=-1.50, ns). Baseline JTT in sessions 2 and 3 did not show significant differences (T=-1.98, ns).
Total JTT time improved significantly with tDCS but not with Sham. ANOVARM revealed a significant TIME(base, post) × INTERVENTION(tDCS, Sham) interaction on total JTT time (F[1,1]=8.07, p<0.05, Table 1).
Post-hoc testing showed that anodal tDCS elicited a significant improvement in total JTT time (from 29.89±4.50 sec at baseline to 28.00±4.08 sec post-stimulation, p<0.05) in the absence of changes (except a trend to slowing) with sham (28.53±4.39 sec to 29.16±5.05 sec; ns). The net change in total JTT with tDCS relative to Sham (% JTT change with tDCS - % JTT change with Sham + 100) was on average 7.98±8.33%. The improvement in total JTT time with a single session of anodal tDCS over M1 remained identifiable for at least 32.6±5.2 min following the end of tDCS. Error rates were comparable in the tDCS and Sham sessions. At baseline, the older the subject, the longer the time required to complete the JTT (R = 0.79; p < 0.01). After tDCS, the older the subject, the more prominent was the improvement in JTT relative to baseline (R= 0.65, p < 0.05; Fig. 1A). It is of note that the only subject above 80yo was the one showing the most pronounced effect of tDCS.
Figure 2. Effect of anodal tDCS administered to the primary motor cortex on Jebsen Taylor Handfunction Test performance.
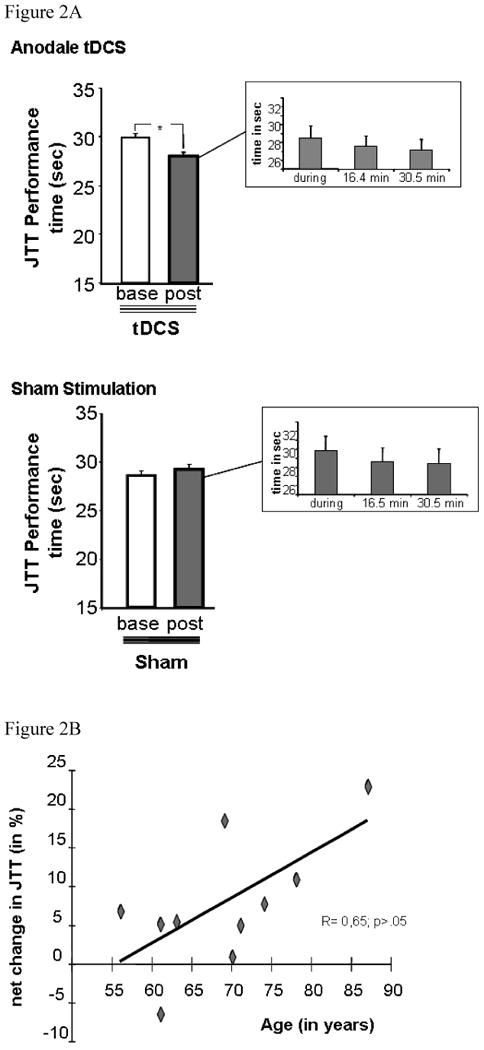
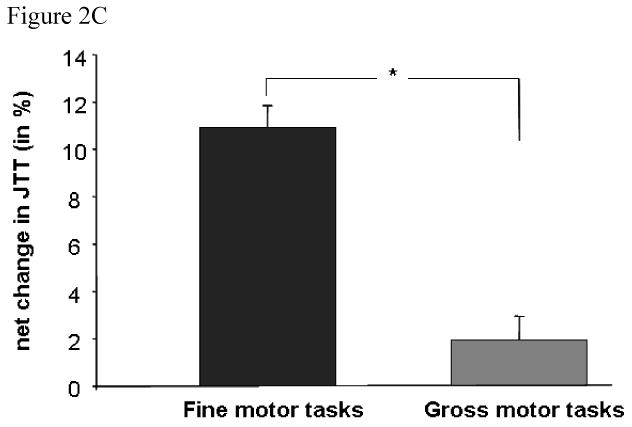
(A) JTT total time at baseline (corresponding to the average of JTT1–3), during and following (corresponding to the average of JTT4–6) tDCS (upper row) or Sham (lower row). Please note that tDCS (upper row, asterisk) but not Sham (lower row) resulted in shorter total times. Performance improvements that appeared during tDCS, persisted beyond the stimulation period for at least 30 min (upper row, inset). (B) Correlation analysis between age (x-axis) and tDCS-induced behavioural improvement in JTT performance (y-axis). Note the significant correlation with the more tDCS-induced improvement the older the subjects. (C) Effect of tDCS on fine motor versus gross motor tasks. Y-axis displays the averaged improvements for JTT subtests 1-3 and 4-6 (in % of improvement). Note the significantly larger effect of tDCS on tasks requiring more dexterous, fine motor function. * indicates p<0.05.
Additionally, there was a significant effect of INTERVENTION(tDCS, Sham) (F=6.29, p<0.05) and TASK(fine, gross) × INTERVENTION(tDCS, Sham) interaction on JTT (F=6.20, p<0.05). Post hoc paired t-test showed a more prominent net-effect of anodal tDCS on fine finger tasks than on gross tasks (p<0.05 level, Fig. 1B) (Hummel, Celnik, Giraux et al., 2005).
There were no significant differences between tDCS and Sham on attention to task, fatigue, and/or discomfort. Subjects were not able to identify the intervention administered in each session (2 and 3).
Discussion
The main findings of the present study were that a single session of anodal tDCS over M1 of aged healthy subjects led to significant improvement in performance of skilled motor tasks included in the Jebsen Taylor Hand function Test (Jebsen et al., 1969) relative to Sham stimulation. This effect outlasted the stimulation period by approximately 30 minutes, appeared more prominent in older individuals, and more evident in tasks engaging more dexterous and fine motor skills than in gross more proximal arm functions.
Accuracy and skill in performance of motor tasks diminish with age (Allum et al., 2002; Enoka et al., 2003; Olafsdottir et al., 2007; Wu and Hallett, 2005) resulting in substantial disability in otherwise healthy aged humans (Amirjani et al., 2007; Bischoff et al., 2003; Nutt et al., 2000; Ruiz et al., 2007), impact personal care and activities of daily living, balance and locomotion and may cause invalidating falls (Allum et al., 2002; Kannus et al., 2005; Maki and McIlroy, 2006). While the neural substrates for these age-related declines remain under investigation (for Review Burke and Barnes, 2006) the diminished ability of older subjects to respond to motor training protocols identified in clinical settings (Celnik et al., 2006; Floel et al., 2005; Howard et al., 2004; Sawaki et al., 2003; Shea et al., 2006) emphasize the need to develop rationale adjuvant interventional strategies to compensate these deficits (Holtzer et al., 2007; Scuteri et al., 2005).
Here, we tested the overall hypothesis that application of anodal tDCS over left M1 would facilitate motor function in the contralateral hand in older healthy humans. The main finding was that anodal tDCS resulted in significant improvements in performance of the JTT task relative to sham and that these effects outlasted the stimulation period by approximately 30 minutes in the absence of differences in scales of attention, fatigue and other psychometric tests.
The present results are consistent with previous findings in younger individuals that documented that this form of stimulation can facilitate motor function (Nitsche, Schauenburg et al., 2003; Vines et al., 2006) and motor cortical excitability of the stimulated M1 (Nitsche et al., 2005). The magnitude of the behavioural improvements reported here in older subjects (in the range of 10%) are quantitatively comparable to the improvements elicited by anodal tDCS in healthy young subjects (Nitsche, Schauenburg et al., 2003; Vines et al., 2006) and in chronic stroke patients (Fregni et al., 2005; Hummel, Celnik, Giraux et al., 2005; Hummel et al., 2006), indicating that older subjects have room for improvement in performance of these motor tasks and that we are not facing a ceiling effect. While the quantitative improvement of approximately 10 % might seem unimpressive, it should be kept in mind that subjects received only one session of tDCS and that it was not applied in direct association with a motor training protocol. Data from younger individuals point to the existence of additive effects when tDCS is applied multiple times and in synchrony with motor training or motor learning protocols, an issue we are presently investigating (Reis et al., 2008). One possible mechanism underlying the beneficial effects of anodal tDCS in this study could be restoration of the ability of older subjects to modulate activity in the primary motor cortex (Talelli, Ewas et al., 2008; Talelli, Waddingham et al., 2008; Ward et al., 2008), a hypothesis for future investigation.
The finding that tDCS-induced improvements were more prominent for distal skilled hand tasks than for proximal synergies could point to some degree of task specificity in the effects of tDCS in older subjects. Performance of these tasks require accurate visuomotor integration that relies on activity in primary motor and premotor cortical areas (Chouinard et al., 2006). Given the spatial resolution of tDCS (Nitsche et al., 2007; Wagner et al., 2007) and relatively large effect size reported in a previous study (Lang et al., 2005), we can not rule out the possibility that stimulation applied over M1 could have spread to nearby premotor areas.
Conclusion
Ageing is associated with a general decline in motor function that critically interferes with activities of daily living (Francis and Spirduso, 2000; Giampaoli et al., 1999; Kannus et al., 2005). The present results suggest that noninvasive cortical stimulation applied over the primary motor cortex might facilitate motor function of older subjects, an effect that was more pronounced the older the individuals were. Since these results were achieved in a small sample of individuals and involved short lasting effects, additional testing of the effects of multiple tDCS sessions applied in synchrony with specific motor training protocols is warranted to evaluate facilitatory effects over longer time scales.
Acknowledgments
This research was supported by the intramural program of the NINDS and from a grant from the Alexander von Humboldt Foundation (Feodor-Lynen) to F.H.
Footnotes
Interest Declaration: The authors have no competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allum JH, Carpenter MG, Honegger F, Adkin AL, Bloem BR. Age-dependent variations in the directional sensitivity of balance corrections and compensatory arm movements in man. J Physiol. 2002;542:643–663. doi: 10.1113/jphysiol.2001.015644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirjani N, Ashworth NL, Gordon T, Edwards DC, Chan KM. Normative values and the effects of age, gender, and handedness on the Moberg Pick-Up Test. Muscle Nerve. 2007;35:788–792. doi: 10.1002/mus.20750. [DOI] [PubMed] [Google Scholar]
- Anstey KJ, Wood J, Lord S, Walker JG. Cognitive, sensory and physical factors enabling driving safety in older adults. Clin Psychol Rev. 2005;25:45–65. doi: 10.1016/j.cpr.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Bennett KM, Castiello U. Reach to grasp: changes with age. J Gerontol. 1994;49:P1–7. doi: 10.1093/geronj/49.1.p1. [DOI] [PubMed] [Google Scholar]
- Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, Akos R, Conzelmann M, Dick W, Theiler R. Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32:315–320. doi: 10.1093/ageing/32.3.315. [DOI] [PubMed] [Google Scholar]
- Brown P, Ridding MC, Werhahn KJ, Rothwell JC, Marsden CD. Abnormalities of the balance between inhibition and excitation in the motor cortex of patients with cortical myoclonus. Brain. 1996;119:309–317. doi: 10.1093/brain/119.1.309. [DOI] [PubMed] [Google Scholar]
- Burke SN, Barnes CA. Neural plasticity in the ageing brain. Nat Rev Neurosci. 2006;7:30–40. doi: 10.1038/nrn1809. [DOI] [PubMed] [Google Scholar]
- Butefisch CM, Khurana V, Kopylev L, Cohen LG. Enhancing encoding of a motor memory in the primary motor cortex by cortical stimulation. J Neurophysiol. 2004;91:2110–2116. doi: 10.1152/jn.01038.2003. [DOI] [PubMed] [Google Scholar]
- Carey JR, Fregni F, Pascual-Leone A. rTMS combined with motor learning training in healthy subjects. Restor Neurol Neurosci. 2006;24:191–199. [PubMed] [Google Scholar]
- Celnik P, Stefan K, Hummel F, Duque J, Classen J, Cohen LG. Encoding a motor memory in the older adult by action observation. Neuroimage. 2006;29:677–684. doi: 10.1016/j.neuroimage.2005.07.039. [DOI] [PubMed] [Google Scholar]
- Chapman PF. Cognitive aging: recapturing the excitation of youth? Curr Biol. 2005;15:R31–33. doi: 10.1016/j.cub.2004.12.018. [DOI] [PubMed] [Google Scholar]
- Chouinard PA, Leonard G, Paus T. Changes in effective connectivity of the primary motor cortex in stroke patients after rehabilitative therapy. Exp Neurol. 2006;201:375–387. doi: 10.1016/j.expneurol.2006.04.037. [DOI] [PubMed] [Google Scholar]
- Cole JD, Katifi HA. Evoked potentials in a man with a complete large myelinated fibre sensory neuropathy below the neck. Electroencephalogr Clin Neurophysiol. 1991;80:103–107. doi: 10.1016/0168-5597(91)90147-p. [DOI] [PubMed] [Google Scholar]
- Cole KJ, Rotella DL. Old age affects fingertip forces when restraining an unpredictably loaded object. Exp Brain Res. 2001;136:535–542. doi: 10.1007/s002210000613. [DOI] [PubMed] [Google Scholar]
- Cole KJ, Rotella DL, Harper JG. Mechanisms for age-related changes of fingertip forces during precision gripping and lifting in adults. J Neurosci. 1999;19:3238–3247. doi: 10.1523/JNEUROSCI.19-08-03238.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Disterhoft JF, Oh MM. Alterations in intrinsic neuronal excitability during normal aging. Aging Cell. 2007;6:327–336. doi: 10.1111/j.1474-9726.2007.00297.x. [DOI] [PubMed] [Google Scholar]
- Enoka RM, Christou EA, Hunter SK, Kornatz KW, Semmler JG, Taylor AM, Tracy BL. Mechanisms that contribute to differences in motor performance between young and old adults. J Electromyogr Kinesiol. 2003;13:1–12. doi: 10.1016/s1050-6411(02)00084-6. [DOI] [PubMed] [Google Scholar]
- Erim Z, Beg MF, Burke DT, de Luca CJ. Effects of aging on motor-unit control properties. J Neurophysiol. 1999;82:2081–2091. doi: 10.1152/jn.1999.82.5.2081. [DOI] [PubMed] [Google Scholar]
- Fecteau S, Pascual-Leone A, Theoret H. Paradoxical facilitation of attention in healthy humans. Behav Neurol. 2006;17:159–162. doi: 10.1155/2006/632141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floel A, Breitenstein C, Hummel F, Celnik P, Gingert C, Sawaki L, Knecht S, Cohen LG. Dopaminergic influences on formation of a motor memory. Ann Neurol. 2005;58:121–130. doi: 10.1002/ana.20536. [DOI] [PubMed] [Google Scholar]
- Floel A, Cohen LG. Contribution of noninvasive cortical stimulation to the study of memory functions. Brain Res Rev. 2007;53:250–259. doi: 10.1016/j.brainresrev.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Francis KL, Spirduso WW. Age differences in the expression of manual asymmetry. Exp Aging Res. 2000;26:169–180. doi: 10.1080/036107300243632. [DOI] [PubMed] [Google Scholar]
- Fregni F, Boggio PS, Lima MC, Ferreira MJ, Wagner T, Rigonatti SP, Castro AW, Souza DR, Riberto M, Freedman SD, Nitsche MA, Pascual-Leone A. A sham-controlled, phase II trial of transcranial direct current stimulation for the treatment of central pain in traumatic spinal cord injury. Pain. 2006;122:197–209. doi: 10.1016/j.pain.2006.02.023. [DOI] [PubMed] [Google Scholar]
- Fregni F, Boggio PS, Mansur CG, Wagner T, Ferreira MJ, Lima MC, Rigonatti SP, Marcolin MA, Freedman SD, Nitsche MA, Pascual-Leone A. Transcranial direct current stimulation of the unaffected hemisphere in stroke patients. Neuroreport. 2005;16:1551–1555. doi: 10.1097/01.wnr.0000177010.44602.5e. [DOI] [PubMed] [Google Scholar]
- Gandiga PC, Hummel FC, Cohen LG. Transcranial DC stimulation (tDCS): A tool for double-blind sham-controlled clinical studies in brain stimulation. Clin Neurophysiol. 2006;117:845–850. doi: 10.1016/j.clinph.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Giampaoli S, Ferrucci L, Cecchi F, Lo Noce C, Poce A, Dima F, Santaquilani A, Vescio MF, Menotti A. Hand-grip strength predicts incident disability in non-disabled older men. Age Ageing. 1999;28:283–288. doi: 10.1093/ageing/28.3.283. [DOI] [PubMed] [Google Scholar]
- Hackel ME, Wolfe GA, Bang SM, Canfield JS. Changes in hand function in the aging adult as determined by the Jebsen Test of Hand Function. Phys Ther. 1992;72:373–377. doi: 10.1093/ptj/72.5.373. [DOI] [PubMed] [Google Scholar]
- Heuninckx S, Wenderoth N, Swinnen SP. Systems neuroplasticity in the aging brain: recruiting additional neural resources for successful motor performance in elderly persons. J Neurosci. 2008;28:91–99. doi: 10.1523/JNEUROSCI.3300-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzer R, Friedman R, Lipton RB, Katz M, Xue X, Verghese J. The relationship between specific cognitive functions and falls in aging. Neuropsychology. 2007;21:540–548. doi: 10.1037/0894-4105.21.5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard DV, Howard JH, Jr, Japikse K, DiYanni C, Thompson A, Somberg R. Implicit sequence learning: effects of level of structure, adult age, and extended practice. Psychol Aging. 2004;19:79–92. doi: 10.1037/0882-7974.19.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel F, Celnik P, Floel A, Duque J, Gandiga P, Gerloff C, Cohen LG. Effects of noninvasive cortical stimulation (tDCS) of the intact hemisphere in patients with chronic stroke on (II) interhemispheric inhibition. Neuroimage. 2005;26:S34. [Google Scholar]
- Hummel F, Celnik P, Giraux P, Floel A, Wu WH, Gerloff C, Cohen LG. Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke. Brain. 2005;128:490–499. doi: 10.1093/brain/awh369. [DOI] [PubMed] [Google Scholar]
- Hummel F, Voller B, Celnik P, Floel A, Giraux P, Gerloff C, Cohen LG. Effects of brain polarization on reaction times and pinch force in chronic stroke. BMC Neurosci. 2006;7 doi: 10.1186/1471-2202-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel FC, Cohen LG. Drivers of brain plasticity. Curr Opin Neurol. 2005;18:667–674. doi: 10.1097/01.wco.0000189876.37475.42. [DOI] [PubMed] [Google Scholar]
- Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319. [PubMed] [Google Scholar]
- Jeffery DT, Norton JA, Roy FD, Gorassini MA. Effects of transcranial direct current stimulation on the excitability of the leg motor cortex. Exp Brain Res. 2007;182:281–287. doi: 10.1007/s00221-007-1093-y. [DOI] [PubMed] [Google Scholar]
- Kannus P, Parkkari J, Niemi S, Palvanen M. Fall-induced deaths among elderly people. Am J Public Health. 2005;95:422–424. doi: 10.2105/AJPH.2004.047779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketcham CJ, Seidler RD, Van Gemmert AW, Stelmach GE. Age-related kinematic differences as influenced by task difficulty, target size, and movement amplitude. J Gerontol B Psychol Sci Soc Sci. 2002;57:P54–64. doi: 10.1093/geronb/57.1.p54. [DOI] [PubMed] [Google Scholar]
- Kobayashi M, Hutchinson S, Theoret H, Schlaug G, Pascual-Leone A. Repetitive TMS of the motor cortex improves ipsilateral sequential simple finger movements. Neurology. 2004;62:91–98. doi: 10.1212/wnl.62.1.91. [DOI] [PubMed] [Google Scholar]
- Kwon YH, Ko MH, Ahn SH, Kim YH, Song JC, Lee CH, Chang MC, Jang SH. Primary motor cortex activation by transcranial direct current stimulation in the human brain. Neurosci Lett. 2008;435:56–59. doi: 10.1016/j.neulet.2008.02.012. [DOI] [PubMed] [Google Scholar]
- Lang N, Nitsche MA, Paulus W, Rothwell JC, Lemon RN. Effects of transcranial direct current stimulation over the human motor cortex on corticospinal and transcallosal excitability. Exp Brain Res. 2004;156:439–443. doi: 10.1007/s00221-003-1800-2. [DOI] [PubMed] [Google Scholar]
- Lang N, Siebner HR, Ward NS, Lee L, Nitsche MA, Paulus W, Rothwell JC, Lemon RN, Frackowiak RS. How does transcranial DC stimulation of the primary motor cortex alter regional neuronal activity in the human brain? Eur J Neurosci. 2005;22:495–504. doi: 10.1111/j.1460-9568.2005.04233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age Ageing. 2006;35 2:ii12–ii18. doi: 10.1093/ageing/afl078. [DOI] [PubMed] [Google Scholar]
- Nitsche MA, Cohen LG, Wassermann E, Priori A, Lang N, Antal A, Paulus W, Hummel F, Boggio PS, Fregni F, Pascual-Leone A. Transcranial direct current stimulation: state of the art 2008. Brain Stimulation. doi: 10.1016/j.brs.2008.06.004. in press. [DOI] [PubMed] [Google Scholar]
- Nitsche MA, Doemkes S, Karakose T, Antal A, Liebetanz D, Lang N, Tergau F, Paulus W. Shaping the effects of transcranial direct current stimulation of the human motor cortex. J Neurophysiol. 2007;97:3109–3117. doi: 10.1152/jn.01312.2006. [DOI] [PubMed] [Google Scholar]
- Nitsche MA, Liebetanz D, Lang N, Antal A, Tergau F, Paulus W. Safety criteria for transcranial direct current stimulation (tDCS) in humans. Clin Neurophysiol. 2003;114:2220–2222. doi: 10.1016/s1388-2457(03)00235-9. author reply 2222-2223. [DOI] [PubMed] [Google Scholar]
- Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(pt 3):633–639. doi: 10.1111/j.1469-7793.2000.t01-1-00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitsche MA, Schauenburg A, Lang N, Liebetanz D, Exner C, Paulus W, Tergau F. Facilitation of Implicit Motor Learning by Weak Transcranial Direct Current Stimulation of the Primary Motor Cortex in the Human. J Cogn Neurosci. 2003;15:619–626. doi: 10.1162/089892903321662994. [DOI] [PubMed] [Google Scholar]
- Nitsche MA, Seeber A, Frommann K, Klein CC, Rochford C, Nitsche MS, Fricke K, Liebetanz D, Lang N, Antal A, Paulus W, Tergau F. Modulating parameters of excitability during and after transcranial direct current stimulation of the human motor cortex. J Physiol. 2005 doi: 10.1113/jphysiol.2005.092429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt JG, Lea ES, Van Houten L, Schuff RA, Sexton GJ. Determinants of tapping speed in normal control subjects and subjects with Parkinson's disease: differing effects of brief and continued practice. Mov Disord. 2000;15:843–849. doi: 10.1002/1531-8257(200009)15:5<843::aid-mds1013>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Olafsdottir H, Zhang W, Zatsiorsky VM, Latash ML. Age-related changes in multifinger synergies in accurate moment of force production tasks. J Appl Physiol. 2007;102:1490–1501. doi: 10.1152/japplphysiol.00966.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Oliviero A, Profice P, Tonali PA, Pilato F, Saturno E, Dileone M, Ranieri F, Di Lazzaro V. Effects of aging on motor cortex excitability. Neurosci Res. 2006;55:74–77. doi: 10.1016/j.neures.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Power HA, Norton JA, Porter CL, Doyle Z, Hui I, Chan KM. Transcranial direct current stimulation of the primary motor cortex affects cortical drive to human musculature as assessed by intermuscular coherence. J Physiol. 2006;577:795–803. doi: 10.1113/jphysiol.2006.116939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt J, Chasteen AL, Abrams RA. Rapid aimed limb movements: age differences and practice effects in component submovements. Psychol Aging. 1994;9:325–334. doi: 10.1037//0882-7974.9.2.325. [DOI] [PubMed] [Google Scholar]
- Reis J, Celnik P, Swayne O, Krakauer JW, Cohen LG. Lasting motor learning induced by transcranial direct current stimulation of the primary motor cortex in combination with physical training. Annals of Neurology. 2008;60:644. [Google Scholar]
- Ruiz PJ, Bernardos VS, Bartolome M, Torres AG. Capit timed tests quantify age-related motor decline in normal subjects. J Neurol Sci. 2007;260:283–285. doi: 10.1016/j.jns.2007.04.034. [DOI] [PubMed] [Google Scholar]
- Sarlegna FR. Impairment of online control of reaching movements with aging: a double-step study. Neurosci Lett. 2006;403:309–314. doi: 10.1016/j.neulet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Sawaki L, Yaseen Z, Kopylev L, Cohen LG. Age-dependent changes in the ability to encode a novel elementary motor memory. Ann Neurol. 2003;53:521–524. doi: 10.1002/ana.10529. [DOI] [PubMed] [Google Scholar]
- Scuteri A, Palmieri L, Lo Noce C, Giampaoli S. Age-related changes in cognitive domains. A population-based study. Aging Clin Exp Res. 2005;17:367–373. doi: 10.1007/BF03324624. [DOI] [PubMed] [Google Scholar]
- Shea CH, Park JH, Braden HW. Age-related effects in sequential motor learning. Phys Ther. 2006;86:478–488. [PubMed] [Google Scholar]
- Stern EB. Stability of the Jebsen-Taylor Hand Function Test across three test sessions. Am J Occup Ther. 1992;46:647–649. doi: 10.5014/ajot.46.7.647. [DOI] [PubMed] [Google Scholar]
- Talelli P, Ewas A, Waddingham W, Rothwell JC, Ward NS. Neural correlates of age-related changes in cortical neurophysiology. Neuroimage. 2008;40:1772–1781. doi: 10.1016/j.neuroimage.2008.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talelli P, Waddingham W, Ewas A, Rothwell JC, Ward NS. The effect of age on task-related modulation of interhemispheric balance. Exp Brain Res. 2008;186:59–66. doi: 10.1007/s00221-007-1205-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale N, Stelmach GE, Breunig A. Postural sway characteristics of the elderly under normal and altered visual and support surface conditions. J Gerontol. 1991;46:B238–244. doi: 10.1093/geronj/46.6.b238. [DOI] [PubMed] [Google Scholar]
- Vines BW, Nair DG, Schlaug G. Contralateral and ipsilateral motor effects after transcranial direct current stimulation. Neuroreport. 2006;17:671–674. doi: 10.1097/00001756-200604240-00023. [DOI] [PubMed] [Google Scholar]
- Voelcker-Rehage C, Alberts JL. Age-related changes in grasping force modulation. Exp Brain Res. 2005;166:61–70. doi: 10.1007/s00221-005-2342-6. [DOI] [PubMed] [Google Scholar]
- Voss M, Bays PM, Rothwell JC, Wolpert DM. An improvement in perception of self-generated tactile stimuli following theta-burst stimulation of primary motor cortex. Neuropsychologia. 2007;45:2712–2717. doi: 10.1016/j.neuropsychologia.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner T, Valero-Cabre A, Pascual-Leone A. Noninvasive human brain stimulation. Annu Rev Biomed Eng. 2007;9:527–565. doi: 10.1146/annurev.bioeng.9.061206.133100. [DOI] [PubMed] [Google Scholar]
- Ward NS, Swayne OB, Newton JM. Age-dependent changes in the neural correlates of force modulation: An fMRI study. Neurobiol Aging. 2008;29:1434–1446. doi: 10.1016/j.neurobiolaging.2007.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T, Hallett M. The influence of normal human ageing on automatic movements. J Physiol. 2005;562:605–615. doi: 10.1113/jphysiol.2004.076042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yordanova J, Kolev V, Hohnsbein J, Falkenstein M. Sensorimotor slowing with ageing is mediated by a functional dysregulation of motor-generation processes: evidence from high-resolution event-related potentials. Brain. 2004;127:351–362. doi: 10.1093/brain/awh042. [DOI] [PubMed] [Google Scholar]
- Yousry TA, Schmid UD, Alkadhi H, Schmidt D, Peraud A, Buettner A, Winkler P. Localization of the motor hand area to a knob on the precentral gyrus. A new landmark. Brain. 1997;120(Pt 1):141–157. doi: 10.1093/brain/120.1.141. [DOI] [PubMed] [Google Scholar]


