Abstract
Background
During the final stages of differentiation of mammalian erythroid cells, the chromatin is condensed and enucleated. We previously reported that Rac GTPases and their downstream target, mammalian homolog of Drosophila diaphanous 2 (mDia2), are required for enucleation of in vitro cultured mouse fetal liver erythroblasts. However, it is not clear how chromatin condensation is achieved and whether it is required for enucleation.
Design and Methods
Mouse fetal liver erythroblasts were purified from embryonic day 14.5 pregnant mice and cultured in erythropoietin-containing medium. Enucleation was determined by flow-cytometry based analysis after treatment with histone deacetylase inhibitors or infection with lentiviral short harirpin RNA.
Results
We showed that histone deacetylases play critical roles in chromatin condensation and enucleation in cultured mouse fetal liver erythroblasts. Enzymatic inhibition of histone deacetylases by trichostatin A or valproic acid prior to the start of enucleation blocked chromatin condensation, contractile actin ring formation and enucleation. We further demonstrated that histone deacetylases 1, 2, 3 and 5 are highly expressed in mouse fetal erythroblasts. Short hairpin RNA down-regulation of histone deacetylase 2, but not of the other histone deacetylases, phenotypically mimicked the effect of trichostatin A or valproic acid treatment, causing significant inhibition of chromatin condensation and enucleation. Importantly, knock-down of histone deacetylase 2 did not affect erythroblast proliferation, differentiation, or apoptosis.
Conclusions
These results identify histone deacetylase 2 as an important regulator, mediating chromatin condensation and enucleation in the final stages of mammalian erythropoiesis.
Keywords: histone deacetylase 2, HDAC2, chromatic condensation, enucleation, mammalian erythropoiesis
Introduction
Mammalian erythropoiesis from the colony-forming unit - erythroid (CFU-E) progenitor cell involves sequential erythropoietin-dependent and -independent stages.1 In the early stages erythropoietin prevents CFU-E cell apoptosis; it supports rapid cell divisions and induction of hundreds of genes encoding erythrocyte-important proteins. The latter stages are erythropoietin-independent and involve chromatin condensation, cell cycle arrest, and enucleation. Whereas in all vertebrates the erythrocyte nucleus becomes highly condensed, enucleation is unique to mammalian erythrocytes. The extruded nucleus is surrounded by a plasma membrane that shows a distinct surface protein expression profile with low levels of glycophorin A and transferrin receptor compared to the incipient reticulocyte; little cytoplasm remains in the extruded nucleus.2 The membrane enveloping the nucleus also contains high levels of phosphatidylserine, which serves as a signal for engulfment by macrophages.3 Although our understanding of mammalian erythroid cell enucleation has increased since morphological studies decades ago,4,5 most of the molecular mechanisms remain unknown. Recent studies suggest that non-apoptotic activities of caspases6,7 and of the tumor suppressor protein Rb8,9 play important roles in erythroid enucleation. In addition, several studies suggest that enucleation requires that the erythroid cells interact with extracellular matrix proteins,10 macrophages,11,12 or sinusoidal endothelium.13 These observations, however, are limited and there is little evidence demonstrating that any single regulatory pathway plays a primary role in the enucleation process.
Using an in vitro cultured mouse fetal liver erythroblast system,14 we previously demonstrated that deregulation of Rac GTPases during the late stages of erythropoiesis completely blocked enucleation of cultured mouse fetal erythroblasts without affecting normal proliferation or differentiation. A contractile actin ring normally forms on the plasma membrane of late-stage erythroblasts at the boundary between the cytoplasm and nucleus of enucleating cells; formation of this cytoskeletal structure was disrupted when Rac GTPase was inhibited in late stages of erythropoiesis. Rac GTPase activity is mediated by the downstream target protein, mammalian homolog of Drosophila diaphanous 2 (mDia2), a formin required for nucleation of unbranched actin filaments.2 These results revealed important roles for the Rac GTPase and mDia2 in enucleation of mammalian erythroblasts.15
Chromatin condensation during the late stages of erythropoiesis involves many histone modifications such as deacetylation, presumably catalyzed by histone deacetylases (HDAC). There are 18 known HDAC. HDAC1, 2, 3 and 8 belong to class I; these HDAC are homologous to the yeast RPD3 protein and reside in the nucleus. HDAC4, 5, 7 and 9 belong to class IIa and they shuttle between the nucleus and the cytoplasm. HDAC6 and HDAC10 are class IIb HDAC that contain two catalytic HD domains. All of these HDAC contain a zinc catalytic domain that is inhibited by trichostatin A.16 HDAC play essential roles in chromatin remodeling, epigenetic regulation, and gene expression, processes that are critical for normal cell differentiation and proliferation.17–19 HDAC also play important roles in determining the fate of hematopoietic cells. In red cells, HDAC negatively regulate the interleukin-3-mediated growth of early erythroid precursors by suppressing their responsiveness to interleukin-3, and play an important role in erythropoietin-mediated differentiation and survival of erythroid precursors.20
HDAC also play critical roles in terminal erythropoiesis. Popova et al. recently demonstrated that the activities of HDAC are required for chromatin condensation in Friend-virus infected murine spleen erythroblasts (FVA cells).21 In this study, HDAC5 expression was shown to be increased during terminal erythropoiesis. However, a role for HDAC5 in mammalian erythroblast chromatin condensation and enucleation needs to be re-examined as no loss of function studies have been done. The use of FVA cells also raises concerns, as retrovirus infection often introduces genetic and epigenetic modifications.
Here we used an in vitro mouse fetal erythroblast culture system to investigate the role of HDAC in chromatin condensation and subsequent enucleation of primary mouse erythroblasts.
Design and Methods
Materials
Mouse monoclonal antibodies against HDAC1, HDAC2, HDAC3 and H4K16ac were purchased from Abcam. The poly-clonal antibody against HDAC5 was purchased from Cell Signaling Technology. The monoclonal antibody against mDia2 was purchased from Santa Cruz Biotechnology. All antibodies for flow cytometric analysis were purchased from BD Biosciences. Alexa Fluor 488 phalloidin for contractile actin ring staining was purchased from Invitrogen Molecular Probes.
Purification and culture of fetal liver cells
Purification and in vitro culture of mouse fetal liver erythroblast precursors (CFU-E; TER119-negative cells) were modified based on the procedures previously described.14 In brief, fetal liver cells were isolated from E13.5 C57BL/6 embryos and mechanically dissociated by pipetting in phosphate-buffered saline containing 10% fetal bovine serum (GIBCO). Single-cell suspensions were prepared by passing the dissociated cells through 70 μm and 25 μm cell strainers. Total fetal liver cells were labeled with biotin-conjugated anti-TER119 antibody (1:100) (BD Pharmingen), and TER119-negative cells were purified through a StemSep column according to the manufacturer’s instructions (Stem Cell Technologies). Purified cells were seeded in fibronectin-coated wells (BD Pharmingen) at a cell density of 1×105/mL. The purified cells were cultured in Iscove’s modified Dulbecco’s medium containing 15% fetal bovine serum (StemCell Technologies), 1% detoxified bovine serum albumin, 200 μg/mL holo-transferrin (Sigma), 10 μg/mL recombinant human insulin (Sigma), 2 mM L-glutamine, 10−4 M β-mercaptoethanol, and 2 U/mL erythropoietin (Amgen).
Generation of lentivirus and infection of fetal liver erythroblasts
The hairpin-pLKO.1 bacterial glycerol stocks were purchased from the Broad Institute (Cambridge, MA, USA). A mixture of five lentiviral vectors encoding different short hairpin RNA (shRNA) sequences was employed for each HDAC. The sequences of the shRNA are given in the Online Supplementary Design and Methods. Lentivirus production from 293T cells was performed as instructed (http://www.broadinstitute.org/genome_bio/trc/publicProtocols.html). For infection of the purified TER119-negative fetal liver cells, 1×105 cells were resuspended in 1 mL thawed viral supernatant containing 10 μg/mL polybrene (Sigma) and centrifuged at 2000 rpm for 1 h at 37°C. The cells were then changed to differentiation medium as above for 2 days.
Flow cytometric analysis
Flow cytometric analysis of the differentiation status of cultured mouse fetal erythroblasts was described previously.2 Briefly, fetal liver cells were immunostained with phycoerythrin-conjugated anti-TER119 (1:200) (BD Pharmingen) and fluorescein isothio-cyanate-conjugated anti-CD71 (1:200) (BD Pharmingen) antibodies, for 15 min at room temperature. Propidium iodide was added to exclude dead cells from analysis. For enucleation analyses, cells were stained with 10 μg/mL Hoechst 33342, in addition to other fluorophore-conjugated antibodies, for 15 min at room temperature.
Confocal microscopy and estimation of nuclear volume
Images of erythroblast nuclei were collected at vertical intervals of 0.75 μm using a LSM 510 Meta confocal microscope system (100M, NA 1.4 Plan-Apochromat lens). Stacks of images were then processed using the isosurface module of Imaris 6.4 (Bitplane, Scientific Solutions) to obtain the estimated nuclear volume. We defined the mean estimated nuclear volume of control cells as 100%. Statistical analysis was performed with Graph Pad Prism software, using the unpaired t-test with a confidence interval of 95%.
Cell cycle analysis
Cultured mouse fetal erythroid cells (2×106) were harvested and resuspended in 200 μL phosphate-buffered saline containing 2% fetal bovine serum (GIBCO). To permeablize the cells, we added 5 mL 95% ethanol drop-wise while vortexing the cells at low speed. The cells were stored at 4°C for 1 h or overnight. The cells were then washed once with phosphate-buffered saline (2% fetal bovine serum) and resuspended in 1 mL propidium iodide staining solution that contains 50 μg/mL propidium iodide, 10 mM Tris pH 7.5, 5 mM MgCl2, and 10 μg/mL RNase. After incubation for 30 min at 37°C, the cells were subjected to flow cytometry for cell cycle profile analysis.
Contractile actin ring staining
Contractile actin ring staining was performed as described previously.2 Essentially, cultured mouse fetal erythroid cells were harvested and resuspended in phosphate-buffered saline containing 10 mM glucose and 1 mg/mL bovine serum albumin (resuspension buffer). Cells were pelleted at 900g for 5 min and then fixed in 100 mL 0.5% acrolein phosphate-buffered saline for 5 min in solution. Resuspension buffer was then added to adjust cells to approximately 5×106 cells/mL. Cells (100 μL) were applied to poly-l-lysine-coated slides (Electron Microscopic Science) and allowed to sit for 40 min at room temperature. The slides were rinsed three times in phosphate-buffered saline containing 0.1 M glycine (rinsing buffer) to remove unbound cells. Cells were permeabilized in rinsing buffer containing 0.05% Triton X-100 for 15 s, followed by three washes in the same buffer without detergent. Cells were then incubated in rinsing buffer for an additional 30 min followed by incubation in blocking buffer (phosphate-buffered saline containing 0.5 mM glycine, 0.2% fish skin gelatin and 0.05% sodium azide) for 1 h. These cells were then incubated with 1 U/mL Alexa Fluor 488–phalloidin in blocking buffer for 1 h. Cells were then washed three times in blocking buffer followed by 4′, 6-diamidino-2-phenylindole (DAPI) staining for 5 min. Images were taken with a Nikon inverted TE300 epi-fluorescence microscope.
Hemoglobin quantification
Mouse fetal liver TER119-negative cells were purified, infected and cultured for 2 days as described above. Hemoglobin was quantified by lysing 1×106 cells in 200 mL Drabkin’s reagent according to the manufacturer’s instructions (Sigma Aldrich). Spectrophotometric reading was then performed at 540 nm.
Statistical analysis
Statistical analysis was performed using GraphPad Prism software. Student’s t-test was used to determine the significance of differences between results from experimental groups compared to those from control ones.
Results
Inhibition of the activities of histone deacetylases at the late stages of mouse fetal erythropoiesis blocks enucleation but not normal differentiation or proliferation
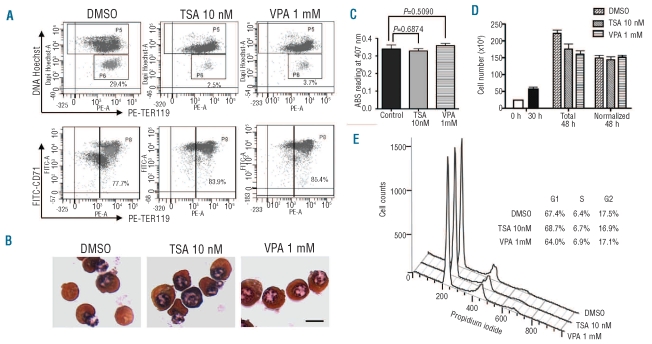
Our previous study demonstrated that the nuclei of cultured mouse fetal erythroblasts undergo gradual condensation before enucleation.2 In the light of the significant roles of HDAC in chromatin remodeling, we tested whether pharmacological inhibition of these enzymes blocked enucleation of primary mouse erythroblasts. To this end, we purified TER119- (an antigen associated with erythroid cell-surface glycophorin A22) negative erythroid progenitor cells from E13.5 mouse fetal livers and cultured them for 2 days in fibronectin-coated plates with erythropoietin; these erythroblasts mimic erythroid cell development in vivo in that they undergo four to five terminal cell divisions, up-regulate hemoglobins and erythroid cell-specific membrane proteins, and undergo chromatin condensation followed by enucleation.14 On day 2, roughly 30% of cells had enucleated.2 We treated the cells with tricostatin A (TSA), a pan-HDAC inhibitor, or valproic acid (VPA), a class I-specific HDAC inhibitor,23,24 at 30 h of culture, roughly the starting time of enucleation.2 Figure 1A shows that treatment of erythroblasts with 10 nM TSA or 1 mM VPA dramatically blocked enucleation at 48 h; the percentage of TER119highHoechstlow cells (incipient reticulocytes) was dramatically decreased compared to the percentage of incipient reticulocytes among dimethylsulfoxide-treated control cells. Importantly, TSA or VPA treatment did not block normal differentiation of erythroblasts since the cells exhibited full induction of TER119 by 48 h in culture (Figure 1A lower panels). The percentage of the TER119-positive population appeared to be increased in TSA- or VPA-treated cells, but this is due to the fact that Ter119 staining of the extruded nuclei in the control cell population (CD71medTER119low cells)2 (Online Supplementary Figure S1) was decreased. In addition, benzidine-Giemsa staining of the same cells from Figure 1A showed that TSA- or VPA-treated cells contained similar hemoglobin levels (orange benzidine-positive cells) as control cells, which demonstrates again that TSA or VPA treatment does not block normal mouse fetal liver erythroid differentiation (Figure 1B). These results were further confirmed by the studies illustrated in Figure 1C, showing that the concentration of the hemoglobin levels in TSA- or VPA-treated cells was the same as in control cells.
Figure 1.
Histone deacetylases are required for enucleation, but not terminal differentiation or proliferation, of cultured mouse fetal liver erythroblasts. (A) Purified TER119-negative E13.5 mouse fetal liver erythroid progenitor cells were cultured in vitro in fibronectin-coated plates in medium containing serum and erythropoietin (Epo). Tricostatin A 10 nM or valproic acid (VPA) 1 mM was added after 30 h in culture and cells were harvested after 48 h. The enucleation and differentiation status of cultured cells after TSA or VPA treatment were analyzed by flow cytometric analysis using staining with Hoechst 33342 and TER119–PE, and FITC–CD71 and TER119–PE, respectively. The percentages of enucleated incipient reticulocytes (top panels) and TER119-positive cells (bottom panels) are illustrated. (B) The same cells as in A were stained with benzidine-Giemsa. The scale bar represents 7 μm. (C) Hemoglobin concentrations of indicated cells analyzed at 48 h in culture. (D) The same cells as in A were counted at 0, 30 and 48 h in culture and the total number is shown. The total number of cells at 48 h was normalized, calculated as the number of nucleated erythroblasts plus one half of the total numbers of reticulocytes and nuclei. (E) Cell cycle analysis of the indicated cells at 40 h in culture. The percentages of the cells at G1, S, and G2 phases are shown.
There was also no difference in apoptosis between treated and control cells (data not shown). We further tested whether treatment of the cultured mouse fetal liver erythroblasts with TSA or VPA blocked cell proliferation. Indeed, the total number of cells at 48 h decreased when the cells were treated with TSA or VPA at 30 h in culture (Figure 1D). But since enucleation forms one nucleus and one reticulocyte, as we described before, we took this factor into account2 and found that there was no significant decrease in cell number when cells were treated with TSA or VPA at 30 h of culture (Figure 1D).
We also performed cell cycle analysis on these cells. To this end, cell cycle profiles at different time points during the in vitro culture of TER119-negative erythroblasts were first obtained. Online Supplementary Figure S2 shows that a significant number of the cultured TER119-negative cells were in S phase during the first 30 h in culture. The cells quickly became arrested at G1 phase after 30 h. We compared the cell cycle profile of TSA- or VPA-treated cells with that of the control ones at 40 h in culture and found no detectable difference (Figure 1E). Taken together, these results demonstrate that the activities of HDAC are required for enucleation, but not for terminal differentiation or proliferation of primary mouse fetal erythroblasts.
Histone deacetylases regulate chromatin condensation and contractile actin ring formation during the late stages of mouse fetal erythropoiesis
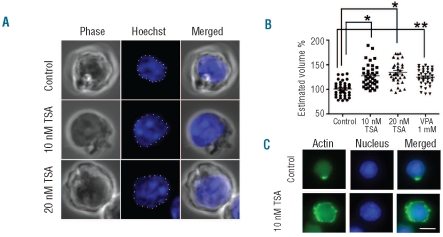
To test directly whether inhibition of the activities of HDAC block chromatin condensation in terminal erythropoiesis, we treated the cultured fetal liver erythroblasts with 10 nM or 20 nM of TSA at 30 h in culture. We fixed the cells at 42 h and stained them with Hoechst to detect nuclei. Figure 2A demonstrates that TSA-treated erythroid cells exhibited significantly enlarged nuclei compared to control cells. VPA treatment had similar effects (data not shown). The size of the nucleus was quantified using Z-stacks, and Figure 2B shows that the estimated nuclear volume of TSA or VPA-treated cells was significantly larger than that of control cells.
Figure 2.
Histone deacetylases are required for chromatin condensation of cultured mouse fetal liver erythroblasts. (A) Confocal microscopy analysis of TSA-treated mouse fetal liver erythroblasts. TER119-negative mouse fetal liver erythroblasts were cultured as in Figure 1. After 30 h, the indicated amount of TSA was added. Cells were harvested after 42 h and analyzed by confocal microscopy. Z-projections of DNA (blue) are shown. The scale bar represents 5 μm (B) Quantification of the estimated nuclear volume of the cells shown in A and VPA-treated cells. *P<0.001, **P<0.0001. (C) The same cells as in A treated with 10 nM of TSA after 30 h in culture were harvested after 48 h and stained with Alexa Fluor 488–phalloidin. The scale bar represents 8 μm.
We also analyzed the formation of the contractile actin ring during the enucleation process2 in the presence and absence of TSA or VPA. Figure 2C shows that TSA-treated erythroblasts exhibited irregular actin distribution compared to the normal bright green dots characteristic of the contractile actin ring. VPA-treated cells showed similar changes (data not shown). These results confirm our hypothesis that chromatin condensation, regulated by HDAC, is required for enucleation. The blockage of contractile actin ring formation also suggests that this activity of the HDAC may occur before activation of the RacGTPase-mDia2 pathway and formation of the contractile actin ring.2
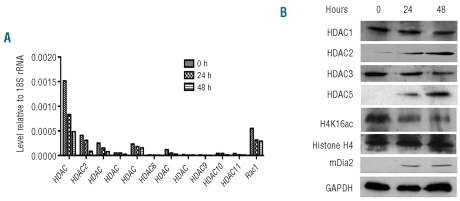
Histone deacetylases 1, 2, 3 and 5 are highly expressed in mouse fetal erythroblasts
To determine the expression levels of different HDAC during erythropoiesis, we performed real-time polymerase chain reaction analyses of cultured fetal liver erythroblasts harvested at 0, 24, and 48 h in culture. Figure 3A shows that the mRNA expression levels of HDAC1, HDAC2, HDAC3, and HDAC5 are higher than those of other HDAC in erythroid cells. Rac1 was used as a positive control as we have demonstrated that it is highly expressed in erythroid cells.2 It is notable that the mRNA expression level of each HDAC is decreased during terminal proliferation and differentiation of mouse fetal erythroblasts. Consistent with their gradually decreased mRNA levels during erythropoiesis, the protein levels of HDAC1 and HDAC3 also decreased during the 48 h culture (Figure 3B). In contrast, the protein levels of HDAC2 and HDAC5 increased and reached a maximal level at 48 h in culture. We also found that acetylation of histone H4-K16 (H4K16ac), which controls the global chromatin structure and protein interactions,25 is gradually decreased during erythropoiesis (Figure 3B).
Figure 3.
HDAC 1, 2, 3 and 5 are highly expressed in cultured mouse fetal liver erythroblasts. (A) The mRNA expression levels of different HDAC during in vitro culture of TER119-negative mouse fetal erythroblasts, as quantified by quantitative real-time polymerase chain reaction analysis. The relative level compared to 18S rRNA was calculated using the ΔΔCt method. (B) Protein expression levels of HDAC 1, 2, 3 and 5, as well as histone H4 and acetylated H4K16 during in vitro culture of TER119-negative mouse fetal erythroblasts analyzed by western blot. The mDia2 and GAPDH protein levels are shown as positive and internal loading controls, respectively.
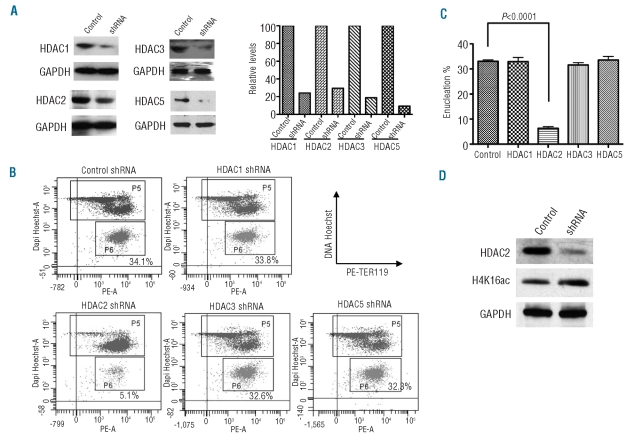
Histone deacetylase 2, but not histone deacetylase 1, 3, or 5, is required for chromatin condensation, contractile actin ring formation and enucleation
To directly test whether any HDAC is required for erythroid cell chromatin condensation and enucleation, we infected isolated TER119-negative mouse fetal erythroid progenitor cells before culture with lentiviruses encoding shRNA targeting mRNA encoding HDAC1, 2, 3 or 5. Cells were harvested at 48 h of culture for western blot analysis to detect the knockdown level of each individual HDAC, and flow cytometry analysis was performed to detect enucleation. A maximum decrease of the corresponding mRNA levels was achieved after approximately 30 h in culture2 and levels of each mRNA were decreased by more than 80%. Figure 4A illustrates the decreased protein expression levels of HDAC1, 2, 3 and 5 with lentiviral shRNA infection. Significantly, analysis at 48 h in culture showed that only down-regulation of HDAC2 dramatically inhibited erythroblast enucleation, whereas HDAC1, HDAC3 or HDAC5 down-regulation had no effects (Figure 4B and 4C). As we expected, the level of acetylated H4K16 was increased when HDAC2 was down-regulated (Figure 4D).
Figure 4.
Depletion of HDAC2 inhibits enucleation and chromatin condensation (A) Depletion of HDAC 1, 2, 3 and 5 in primary erythroid cells by shRNA. TER119-negative mouse fetal erythroblasts were infected with lentiviral vectors encoding shRNA specific for HDAC 1, 2, 3 or 5 and cultured for 48 h. Lysates were subjected to western blotting for individual proteins as indicated. Controls show GAPDH levels. The gels were scanned and quantified. Controls were set as 100. (B) Flow cytometric analysis of cells infected with lentirviruses encoding HDAC 1, 2, 3 or 5 shRNA and cultured for 2 days, as in Figure 1. Cells were stained with TER119–PE and Hoechst 33342 and analyzed by FACS. The percentages of incipient reticulocytes are indicated. (C) Quantification of incipient reticulocytes in cells infected with indicated lentiviruses. (D) Western blot analysis of acetylated H4K16 when HDAC2 was down-regulated by shRNA.
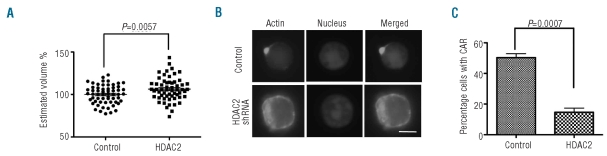
Similar to TSA or VPA treatment, knockdown of HDAC2 also significantly blocked nuclear condensation (Figure 5A). Alexa Fluor 488-phalloidin staining of the HDAC2 shRNA-infected cells after 48 h in culture demonstrated defects in contractile actin ring formation compared to that of the control shRNA-infected cells (Figure 5B and 5C). Cells in which HDAC5 was knocked down showed no defects in these processes (data not shown).
Figure 5.
Depletion of HDAC2 blocks chromatin condensation and contractive actin ring (CAR) formation of cultured mouse fetal liver erythroblasts. (A) Quantification of the estimated nuclear volume of 2-day cultured mouse fetal liver erythroblasts infected with lentiviruses expressing HDAC2 shRNA. (B) Alexa Fluor 488–phalloidin staining the same cells as in A. The scale bar represents 5 μm. (C). Quantification from B of cells containing a CAR. Three independent experiments were performed with roughly 200 cells counted in randomly picked areas.
Knockdown of histone deacetylase 2 at the late stages of mouse fetal erythropoiesis does not affect normal differentiation or proliferation
We next performed flow cytometric analysis of the levels of cell surface expression of glycophorin A (TER119) and the transferrin receptor (CD71). Figure 6A demonstrates that by this criterion down-regulation of HDAC1, HDAC2, HDAC3 or HDAC5 did not affect normal erythroid differentiation. It is notable that the percentage of the TER119-positive cells in the HDAC2 knockdown model was higher than in the others (Figure 6A and 6B). As with TSA- and VPA-treated cells (Figure 1A), this is due to the fact that the population of the extruded nuclei,2 which is CD71medTER119low, was decreased after HDAC2 knockdown. Again, as for TSA and VPA treatment, knockdown of HDAC2 did not affect the degree of benzidine staining compared with that of cells treated with control shRNA (Figure 6C). As further confirmation that down-regulation of HDAC2 only affects chromatin condensation and enucleation, Figure 6D shows that there was no detectable difference in the concentration of adult hemoglobin levels between HDAC2 shRNA-infected cells and control shRNA-infected cells. Also similar to TSA and VPA treated cells, down-regulation of HDAC2 had no significant effect on cell proliferation (Figure 6E). In addition, and as we expected, HDAC2 knockdown did not affect cell cycle profiles compared to control shRNA-infected cells (data not shown).
Figure 6.
Depletion of HDAC2 does not block terminal differentiation and proliferation of cultured mouse fetal liver erythroblasts. (A) Flow cytometric analysis of cells infected with lentivirus encoding HDAC1, HDAC2, HDAC3 or HDAC5 shRNA and cultured for 2 days, as in Figure 4B. Cells were stained with TER119–PE and FITC-CD71 and analyzed by FACS. The percentages of TER119-positive cells are quantified. (B) Quantification of TER119-positive cells from A. (C) Benzidine-Giemsa staining of cells 48 h after infection with lentivirus encoding control or HDAC2 shRNA. The scale bar represents 8 μm. (D) Hemoglobin concentration of cells 48 h after infection with lentivirus encoding control or HDAC2 shRNA. (C) The same cells as in A were counted after 48 h in culture. The total number and the normalized number, as in Figure 1D, are shown.
Discussion
In this study we demonstrated that HDAC2, but not other HDAC, is required for terminal erythroblast chromatin condensation and subsequent enucleation. We hypothesize that significant chromatin condensation must precede enucleation and may well signal activation of this complex cellular process.
We showed that treatment of mouse fetal liver erythroblasts with HDAC inhibitors late in terminal erythropoiesis inhibits chromatin condensation and completely blocks enucleation, but does not affect cell proliferation or erythroid differentiation. A similar result was obtained by knocking down HDAC2 in early erythroblasts. It is widely known that acetylation of lysine residues on histone tails, which reduces the net protein positive charge, allows localized chromatin expansion and facilitates gene expression. On the other hand, deacetylation of histone tails by HDAC induces chromatin condensation and repression of gene expression. Since terminal erythropoiesis involves large-scale transcriptional repression, histone modifications, and chromatin condensation, a role for HDAC in chromatin and nuclear condensation is not surprising.
We do not know how HDAC-induced chromatin condensation promotes enucleation. Hypothetically, HDAC may directly activate the Rac GTPases-mDia2 pathway to induce enucleation. Alternatively, condensed nuclei may activate the Rac GTPases-mDia2 pathway through unknown factors. For instance, prior to enucleation the membrane of the condensed nucleus becomes closely apposed to a segment of the plasma membrane, effectively squeezing out the cytosol from this segment. How this happens is not known but it could require nuclear condensation below a specific value. Indeed, our data show that inhibition of HDAC activities or knockdown of HDAC2 blocks contractile actin ring formation, a prerequisite for enucleation.
We emphasize that proteins that are required for terminal erythropoiesis may also play important roles in the early stages of erythropoiesis. For example, we previously demonstrated that Rac GTPases regulate mouse fetal erythroblast enucleation through mDia2.2 But Rac GTPases have recently been shown to be necessary also for early stages of erythropoiesis in bone marrow.26 Like Rac GTPases, HDAC may also play a role in the early stages of erythropoiesis. Indeed, Fujieda et al. demonstrated that treatment of human erythroid cells with an HDAC inhibitor blocks their differentiation.27 Our unpublished results also indicate that TSA treatment of mouse fetal erythroblasts at early time points in culture does block normal differentiation, but we have not attempted to elucidate the possible roles of any HDAC at early stages of erythropoiesis.
Our study identified HDAC2 as the critical regulator in mediating chromatin condensation and enucleation during terminal mouse fetal liver erythropoiesis. Physiologically, HDAC2 also plays important roles in cardiovascular and neuronal systems. HDAC2 null mice have reduced body size and cardiovascular defects.28 Tissue-specific knock-out of HDAC2 in neurons increases synapse number and memory facilitation.29 There were no hematopoietic phenotypes reported in these mice, possibly due to compensatory effects of other HDAC or the microenvironment surrounding the erythroblast. In this respect, our in vitro mouse fetal liver erythroblast culture system made it possible to study cell autonomous functions of individual HDAC during erythropoiesis. In addition, this system also allowed us to dissect the enucleation process properly from earlier stages of erythropoiesis.
Popova et al. recently demonstrated that enzymatic activities of HDAC are required for chromatin condensation in Friend-virus infected murine spleen erythroblasts (FVA cells).21 In this study, HDAC5 expression was shown to be increased during FVA cell terminal erythroid differentiation, but no loss-of-function studies were done. We showed here that the level of HDAC5 protein increased during the 2-day in vitro culture of mouse fetal erythroblasts, consistent with findings in FVA cells. However, shRNA knockdown of HDAC5 to over 90% at late stages of erythropoiesis had no effect on either chromatin condensation or enucleation, and we can, therefore, eliminate HDAC5 as a critical regulator of these processes.
The fact that VPA also blocks enucleation further confirms the critical role of HDAC2 in the late stages of erythropoiesis. VPA specifically blocks the activities of the class I HDAC, including HDAC 1, 2, and 3. Given the fact that we were able to achieve only partial (~80%) knockdown of HDAC 1 and 3, we cannot rule out possible functions for these HDAC in chromatin condensation and enucleation. It is interesting that VPA not only blocks the enzymatic function of HDAC2, but also selectively induces the degradation of HDAC2 through the ubiquitin-proteasome pathway.30 However, the protein level of HDAC2 was not decreased after treatment with VPA at 30 h in our culture system (data not shown). It is possible that the half-life of HDAC2 in erythroblasts is long and that the treatment of VPA at 30 h in culture did not provide sufficient time to down-regulate HDAC2. This explanation is consistent with the fact that at 48 h in culture, although the mRNA level of HDAC2 decreased, the HDAC2 protein level had increased considerably (Figure 3). All of these results establish the critical role of HDAC2 in mammalian terminal erythropoiesis. Future studies, with a focus on how HDAC2 mediates chromatin condensation and provides signals to promote enucleation, will help us to understand the detailed mechanisms of mammalian terminal erythropoiesis.
HDAC inhibitors are increasingly being developed as anti-tumor compounds in clinical trials.31,32 These compounds, including hydroxamic acids, butyrate, and cyclic tetrapeptides, induce cancer cell apoptosis, cell cycle arrest, and terminal differentiation.33 In addition, HDAC inhibitors are also being used in patients with thalassemia to improve erythropoiesis and hemoglobin production.34 Although so far no systematic clinical study has shown that patients treated with HDAC inhibitors develop anemia, attention should be paid to situations such as targeted bone marrow drug delivery, or the administration of HDAC isotype-specific inhibitors.
Acknowledgments
the authors would like to thank Francisco Sánchez-Rivera for helpful comments and discussion; Glenn Paradis and Patti Wisniewski for help with flow cytometry, and Ferenc Reinhardt and Tony Chavarria for assistance with animal experiments.
Footnotes
Funding: this study was supported by NIH grant P01 HL 32262 and a research grant from Amgen, Inc. to HFL, and by intramural funds from the Temasek Life Sciences Laboratory to MM-H. PJ is a recipient of a Leukemia and Lymphoma Society fellowship and a National Institutes of Health (NIH) Pathway to Independence Award (K99/R00).
The online version of this article has a Supplementary Appendix.
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Richmond TD, Chohan M, Barber DL. Turning cells red: signal transduction mediated by erythropoietin. Trends Cell Biol. 2005;15(3):146–55. doi: 10.1016/j.tcb.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Ji P, Jayapal SR, Lodish HF. Enucleation of cultured mouse fetal erythroblasts requires Rac GTPases and mDia2. Nat Cell Biol. 2008;10(3):314–21. doi: 10.1038/ncb1693. [DOI] [PubMed] [Google Scholar]
- 3.Yoshida H, Kawane K, Koike M, Mori Y, Uchiyama Y, Nagata S. Phosphatidylserine-dependent engulfment by macrophages of nuclei from erythroid precursor cells. Nature. 2005;437(7059):754–8. doi: 10.1038/nature03964. [DOI] [PubMed] [Google Scholar]
- 4.Koury ST, Koury MJ, Bondurant MC. Cytoskeletal distribution and function during the maturation and enucleation of mammalian erythroblasts. J Cell Biol. 1989;109(6 Pt 1):3005–13. doi: 10.1083/jcb.109.6.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chasis JA, Prenant M, Leung A, Mohandas N. Membrane assembly and remodeling during reticulocyte maturation. Blood. 1989;74(3):1112–20. [PubMed] [Google Scholar]
- 6.Carlile GW, Smith DH, Wiedmann M. Caspase-3 has a nonapoptotic function in erythroid maturation. Blood. 2004;103(11):4310–6. doi: 10.1182/blood-2003-09-3362. [DOI] [PubMed] [Google Scholar]
- 7.Zermati Y, Garrido C, Amsellem S, Fishelson S, Bouscary D, Valensi F, et al. Caspase activation is required for terminal erythroid differentiation. J Exp Med. 2001;193(2):247–54. doi: 10.1084/jem.193.2.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iavarone A, King ER, Dai XM, Leone G, Stanley ER, Lasorella A. Retinoblastoma promotes definitive erythropoiesis by repressing Id2 in fetal liver macrophages. Nature. 2004;432(7020):1040–5. doi: 10.1038/nature03068. [DOI] [PubMed] [Google Scholar]
- 9.Clark AJ, Doyle KM, Humbert PO. Cell-intrinsic requirement for pRb in erythropoiesis. Blood. 2004;104(5):1324–6. doi: 10.1182/blood-2004-02-0618. [DOI] [PubMed] [Google Scholar]
- 10.Patel VP, Lodish HF. A fibronectin matrix is required for differentiation of murine erythroleukemia cells into reticulocytes. J Cell Biol. 1987;105(6 Pt 2):3105–18. doi: 10.1083/jcb.105.6.3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanspal M, Smockova Y, Uong Q. Molecular identification and functional characterization of a novel protein that mediates the attachment of erythroblasts to macrophages. Blood. 1998;92(8):2940–50. [PubMed] [Google Scholar]
- 12.Kawane K, Fukuyama H, Kondoh G, Takeda J, Ohsawa Y, Uchiyama Y, et al. Requirement of DNase II for definitive erythropoiesis in the mouse fetal liver. Science. 2001;292(5521):1546–9. doi: 10.1126/science.292.5521.1546. [DOI] [PubMed] [Google Scholar]
- 13.Tavassoli M. Red cell delivery and the function of the marrow-blood barrier: a review. Exp Hematol. 1978;6(3):257–69. [PubMed] [Google Scholar]
- 14.Zhang J, Socolovsky M, Gross AW, Lodish HF. Role of Ras signaling in erythroid differentiation of mouse fetal liver cells: functional analysis by a flow cytometry-based novel culture system. Blood. 2003;102(12):3938–46. doi: 10.1182/blood-2003-05-1479. [DOI] [PubMed] [Google Scholar]
- 15.Ji P, Lodish HF. Rac GTPases play multiple roles in erythropoiesis. Haematologica. 2010;95(1):2–4. doi: 10.3324/haematol.2009.015511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Ruijter AJ, van Gennip AH, Caron HN, Kemp S, van Kuilenburg AB. Histone deacetylases (HDACs): characterization of the classical HDAC family. Biochem J. 2003;370(Pt 3):737–49. doi: 10.1042/BJ20021321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu P, Martin E, Mengwasser J, Schlag P, Janssen KP, Gottlicher M. Induction of HDAC2 expression upon loss of APC in colorectal tumorigenesis. Cancer Cell. 2004;5(5):455–63. doi: 10.1016/s1535-6108(04)00114-x. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Yamashita H, Toyama T, Sugiura H, Ando Y, Mita K, et al. Quantitation of HDAC1 mRNA expression in invasive carcinoma of the breast. Breast Cancer Res Treat. 2005;94(1):11–6. doi: 10.1007/s10549-005-6001-1. [DOI] [PubMed] [Google Scholar]
- 19.Halkidou K, Gaughan L, Cook S, Leung HY, Neal DE, Robson CN. Upregulation and nuclear recruitment of HDAC1 in hormone refractory prostate cancer. Prostate. 2004;59(2):177–89. doi: 10.1002/pros.20022. [DOI] [PubMed] [Google Scholar]
- 20.Yamamura K, Ohishi K, Katayama N, Yu Z, Kato K, Masuya M, et al. Pleiotropic role of histone deacetylases in the regulation of human adult erythropoiesis. Br J Haematol. 2006;135(2):242–53. doi: 10.1111/j.1365-2141.2006.06275.x. [DOI] [PubMed] [Google Scholar]
- 21.Popova EY, Krauss SW, Short SA, Lee G, Villalobos J, Etzell J, et al. Chromatin condensation in terminally differentiating mouse erythroblasts does not involve special architectural proteins but depends on histone deacetylation. Chromosome Res. 2009;17(1):47–64. doi: 10.1007/s10577-008-9005-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kina T, Ikuta K, Takayama E, Wada K, Majumdar AS, Weissman IL, et al. The monoclonal antibody TER-119 recognizes a molecule associated with glycophorin A and specifically marks the late stages of murine erythroid lineage. Br J Haematol. 2000;109 (2):280–7. doi: 10.1046/j.1365-2141.2000.02037.x. [DOI] [PubMed] [Google Scholar]
- 23.Khan N, Jeffers M, Kumar S, Hackett C, Boldog F, Khramtsov N, et al. Determination of the class and isoform selectivity of small-molecule histone deacetylase inhibitors. Biochem J. 2008;409(2):581–9. doi: 10.1042/BJ20070779. [DOI] [PubMed] [Google Scholar]
- 24.Gottlicher M, Minucci S, Zhu P, Kramer OH, Schimpf A, Giavara S, et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 2001;20(24):6969–78. doi: 10.1093/emboj/20.24.6969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shogren-Knaak M, Ishii H, Sun JM, Pazin MJ, Davie JR, Peterson CL. Histone H4-K16 acetylation controls chromatin structure and protein interactions. Science. 2006;311(5762):844–7. doi: 10.1126/science.1124000. [DOI] [PubMed] [Google Scholar]
- 26.Kalfa TA, Pushkaran S, Zhang X, Johnson JF, Pan D, Daria D, et al. Rac1 and Rac2 GTPases are necessary for early erythropoietic expansion in the bone marrow but not in the spleen. Haematologica. 2010;95(1):27–35. doi: 10.3324/haematol.2009.006239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fujieda A, Katayama N, Ohishi K, Yamamura K, Shibasaki T, Sugimoto Y, et al. A putative role for histone deacetylase in the differentiation of human erythroid cells. Int J Oncol. 2005;27(3):743–8. [PubMed] [Google Scholar]
- 28.Trivedi CM, Luo Y, Yin Z, Zhang M, Zhu W, Wang T, et al. Hdac2 regulates the cardiac hypertrophic response by modulating Gsk3 beta activity. Nat Med. 2007;13(3):324–31. doi: 10.1038/nm1552. [DOI] [PubMed] [Google Scholar]
- 29.Guan JS, Haggarty SJ, Giacometti E, Dannenberg JH, Joseph N, Gao J, et al. HDAC2 negatively regulates memory formation and synaptic plasticity. Nature. 2009;459(7243):55–60. doi: 10.1038/nature07925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kramer OH, Zhu P, Ostendorff HP, Golebiewski M, Tiefenbach J, Peters MA, et al. The histone deacetylase inhibitor valproic acid selectively induces proteasomal degradation of HDAC2. EMBO J. 2003;22 (13):3411–20. doi: 10.1093/emboj/cdg315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bolden JE, Peart MJ, Johnstone RW. Anticancer activities of histone deacetylase inhibitors. Nat Rev Drug Discov. 2006;5(9):769–84. doi: 10.1038/nrd2133. [DOI] [PubMed] [Google Scholar]
- 32.Stimson L, Wood V, Khan O, Fotheringham S, La Thangue NB. HDAC inhibitor-based therapies and haematological malignancy. Ann Oncol. 2009;20(8):1293–302. doi: 10.1093/annonc/mdn792. [DOI] [PubMed] [Google Scholar]
- 33.Thiagalingam S, Cheng KH, Lee HJ, Mineva N, Thiagalingam A, Ponte JF. Histone deacetylases: unique players in shaping the epigenetic histone code. Ann NY Acad Sci. 2003;983:84–100. doi: 10.1111/j.1749-6632.2003.tb05964.x. [DOI] [PubMed] [Google Scholar]
- 34.Rodgers GP, Saunthararajah Y. Advances in experimental treatment of beta-thalassaemia. Expert Opin Investig Drugs. 2001;10(5):925–34. doi: 10.1517/13543784.10.5.925. [DOI] [PubMed] [Google Scholar]