Introduction
The benefits of locked-plate fixation, which include improved fixation strength in osteoporotic bone1-3 and the ability to provide a more biologically friendly fixation construct4,5, have led to the rapid adoption of this technology. Biological fixation of comminuted fractures with locking plates relies on secondary fracture-healing by callus formation6,7, which is stimulated by interfragmentary motion in the millimeter range8,9. Secondary bone-healing can be enhanced by active or passive dynamization10,11. Conversely, bone-healing can be suppressed by rigid fracture fixation aimed at preventing interfragmentary motion12.
Biomechanical studies have suggested that locked-plate constructs are stiff and suppress interfragmentary motion to a level that may be insufficient to reliably promote secondary fracture-healing1,13-15. Recent clinical studies substantiate the concern that the inherently high stiffness of locked-plate constructs suppresses callus formation, contributing to a nonunion rate of up to 19% seen with periarticular locking plates16,17. Deficient healing may also contribute to late hardware failures seen with locking plates18-20 since, in the absence of osseous union, constructs remain load-bearing and eventually fail by hardware fatigue or loss of fixation.
This paper summarizes a line of research that addresses two questions of critical importance when using locked-plate constructs:
Does the high stiffness of locked-plate constructs suppress callus formation and fracture-healing?
Can a stiffness-reduced locked-plate technique, termed far cortical locking, improve fracture-healing, compared with standard locked plating, by providing flexible fixation and parallel interfragmentary motion?
First, we will present the findings of biomechanical and clinical studies of the effect of construct stiffness on interfragmentary motion and fracture-healing with locking plates. Subsequently, studies that describe the function, benefits, and clinical application of far cortical locking are summarized.
Numerical results are presented as the mean and one standard deviation. Unless otherwise noted, statistical differences were tested with use of a two-tailed, unpaired Student t test at a level of significance of α = 0.05.
Source of Funding
Financial support for this study was provided by the Zimmer Corporation and by the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH/NIAMS) Grant R21 AR053611.
The Challenge: Construct Stiffness
Are Locked-Plate Constructs Too Stiff to Reliably Promote Fracture-Healing?
The stiffness of a fixation construct is a principal determinant of fracture-site motion and thereby affects the mechanism and progression of fracture-healing9. Stiffness describes the flexibility of a fixation construct and is used to estimate interfragmentary motion in the early healing phase. Stiffness is simply calculated by dividing an applied load by the resulting displacement. However, reported stiffness values for the same implant can vary by more than one order of magnitude since they are highly influenced by the test setup, especially when stiffness is calculated from the displacement of the loading actuator. Actuator displacement represents deformation along the entire test specimen and can grossly overestimate the actual motion at the fracture site. On the basis of actuator displacement, construct stiffness of femoral locking plates has been reported to range from 63 N/mm21 to 159 N/mm22. This stiffness is comparable with that of external fixators (50 to 400 N/mm23-25), which are known to promote fracture-healing by callus formation. However, investigators who have measured the actual fracture-site motion at the far cortex (opposite the plate) have reported a more than tenfold higher stiffness (833 N/mm26 to 2100 N/mm27) for locked femoral bridge-plate constructs. Furthermore, flexion of a bridging plate causes asymmetric gap closure, whereby interfragmentary motion decreases with a decrease in the distance to the plate13. Hence, the effective motion at the near cortex (adjacent to the plate) is considerably smaller than it is at the far cortex.
To assess if locked-plate constructs are too stiff to promote secondary bone-healing by callus formation, interfragmentary motion of bridge-plate constructs was measured at the near and far cortices in a biomechanical study1.
Methods
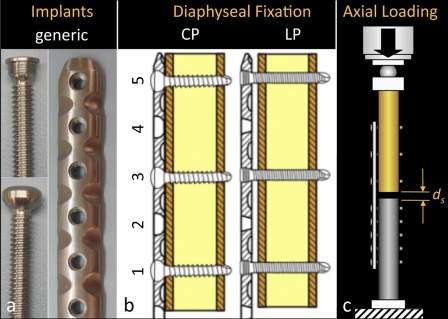
Five locked-plate constructs were applied to bridge a 10-mm-gap osteotomy site in femoral diaphysis surrogates to characterize their stiffness and the resulting interfragmentary motion. Additionally, five nonlocked conventional-plate constructs were tested for baseline comparison. All constructs consisted of a generic 4.5-mm titanium eleven-hole plate and bicortical screws (Fig. 1, a). Proximal diaphyseal fixation was achieved with three locked screws (locked-plate group) or nonlocked screws (conventional-plate group), placed in the first, third, and fifth plate-holes (Fig. 1, b). The locking plates were applied at a 1-mm elevation to simulate biological fixation with preservation of periosteal perfusion. Compressive loading was applied through a ball bearing proximally, while the distal part of the diaphysis was rigidly fixed to the base of a materials testing system (Instron 8874; Instron, Canton, Massachusetts) (Fig. 1, c)28. Construct stiffness was assessed in terms of the amount of osteotomy gap closure (ds) in response to a 400-N load representative of postoperative toe-touch weight-bearing. Gap closure was measured at the near and far cortices with use of two miniature digital calipers (KSLR4610; Blitz, Jeffersonville, Indiana) with 0.01-mm accuracy to assess the magnitude and symmetry of interfragmentary motion.
Fig. 1.
The stiffness and interfragmentary motion of locked-plate constructs was assessed. a: Generic 4.5-mm plate and screws. b: Diaphyseal fixation with a conventional plate (CP) or a locking plate (LP). c: Axial loading and assessment of resulting interfragmentary motion (ds) at the near and far cortices.
Results
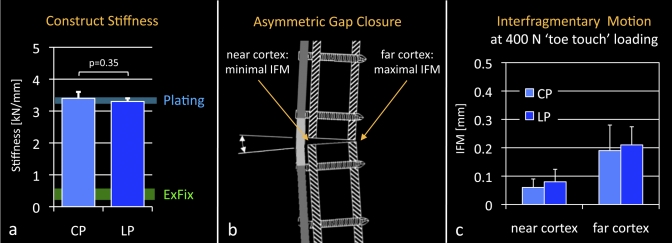
The axial stiffness of the locked-plate constructs (3.3 ± 0.1 kN/mm) was not significantly lower than that of the conventional-plate constructs (3.4 ± 0.2 kN/mm, p = 0.35) (Fig. 2, a). In both constructs, axial loading induced asymmetric gap closure as a result of plate-bending, with gap motion being attenuated toward the near cortex underlying the plate (Fig. 2, b). Gap motion in response to 400-N simulated toe-touch weight-bearing was <0.1 mm at the near cortex and remained below the motion window of 0.2 to 1 mm9,29-31 known to promote callus formation (Fig. 2, c).
Fig. 2.
a: Conventional (CP) and locked-plate (LP) constructs were comparably stiff and were approximately one order of magnitude stiffer than external fixators (ExFix)23-25. b: Axial loading caused plate bending and asymmetric gap closure, whereby interfragmentary motion (IFM) at the near cortex was minimal. c: Near-cortex motion in response to 400-N simulated toe-touch loading remained below 0.1 mm, which is considered insufficient to promote secondary bone-healing.
Conclusions
Locked-plate constructs are as stiff as nonlocked-plate constructs in compression testing, and they are one order of magnitude stiffer than external fixators are in compression. Interfragmentary motion of locked-bridge-plate constructs is asymmetric, and is minimal at the near cortex underlying the plate. Postoperative interfragmentary motion provided by locked plates may therefore be too small to promote callus formation, especially at the near cortex.
Clinical Evidence: Inconsistent Healing
Locked Plates Lead to Inconsistent and Asymmetric Callus Formation
Fractures of the distal part of the femur are commonly treated with locked-plate constructs. Initial reports of locked-plate constructs in the distal part of the femur showed high union rates with relatively few complications20,32,33. Later studies, evaluating both unicortical and bicortical diaphyseal fixation constructs, demonstrated mixed results. Some showed excellent outcomes34-36, while others demonstrated nonunion rates of 2% to 17%18,19,37,38. The authors of some of these studies reported late failures of diaphyseal fixation and implants but did not include them in the nonunion rates18-20. However, 52% of the implant failures in eight studies in which the authors reported the timing of these failures occurred more than six months after the index procedure19,20,33,34,37-40, indicating that the failure was the result of implant fatigue in the presence of an established nonunion. Proper identification of late implant failures as nonunions in studies of locked plates should further raise the concern that locked-plate constructs may be too stiff to promote reliable healing.
Given the biomechanical and clinical concerns that locked plates may be too stiff, a retrospective cohort study was conducted to investigate whether locked-plate constructs can reliably promote fracture-healing17. The authors of this study assessed the effect of stiffness on the healing rate of supracondylar femoral fractures treated with periarticular locking plates by measuring periosteal callus formation, the principal hallmark of secondary bone-healing. The effects of implant material and bridging span on fracture-healing were also analyzed, since these factors can independently influence construct stiffness.
Methods
Seventy-two adult patients with a total of seventy-five distal femoral fractures (AO 32A or 33A, B, or C) were treated with a titanium or stainless-steel locking plate between 2003 and 2008 at two institutions. Lateral and anteroposterior radiographs, along with patient charts, were reviewed at six weeks, three months, and six months postoperatively. Nonunion was defined as painful weight-bearing and the absence of progressive fracture-healing or bridging callus at the medial cortex on serial radiographs. Periosteal callus was measured on the medial, anterior, and posterior cortices with use of custom software to objectively extract callus size from radiographs without manual tracing of callus boundaries17. This software was rigorously validated and was found to measure callus area in surrogate models with an error of <5%41.
Results
There were complications following treatment in twenty-nine (39%) of the seventy-five fractures, and fourteen (19%) of the seventy-five fractures failed to heal. Comparison of the fracture-healing and fracture-nonunion groups revealed no significant differences in terms of the rates of smoking, diabetes, open or closed fractures, or infections or in the injury severity scores. Nonunions had 65% less callus than all remaining fractures (p = 0.035).
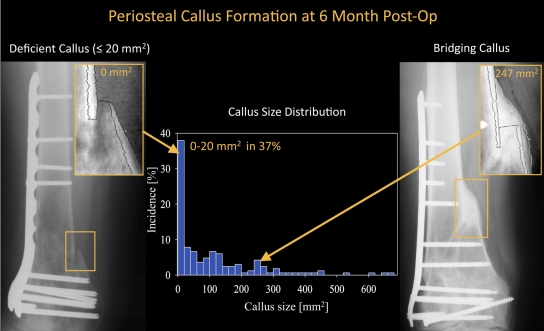
At six months, the size of the periosteal callus ranged from 0 to 670 mm2 (Fig. 3), and 37% of all fractures had little or no callus (≤20 mm2). Over all time points, the medial cortices had 64% more callus than the anterior or posterior cortices (p = 0.001); fractures treated with a titanium plate had 68% more callus than those treated with a stainless-steel plate (p < 0.001); and there was no correlation between a longer bridging span and a greater callus size (r = 0.04, p = 0.4).
Fig. 3.
Periosteal callus measurement at six months postoperatively in a study of patients yielded examples of deficient callus formation (≤20 mm2) and bridging callus (247 mm2). The callus size distribution illustrates that 37% of all fractures had formed no or very little callus (≤20 mm2) at six months.
Conclusions
This study provided clinical evidence that locked-plate constructs may be too stiff to reliably promote fracture-healing. The 19% of the femoral fractures that became nonunions exhibited less callus formation, while stable implant alignment was maintained. This suggests that callus inhibition, rather than implant failure, is the primary cause of these nonunions. Callus inhibition was readily apparent six months after surgery, as 37% of all fractures had no or very little callus. Callus formation was most inhibited closer to the plate, where the asymmetric gap closure characteristic of bridge-plate constructs causes the least interfragmentary motion.
It has been suggested that the stiffness of locked-plate constructs can be reduced by using longer bridging spans42. However, this study17 showed that longer bridging spans correlated poorly with increased callus formation. Titanium plates, which are twice as flexible as stainless-steel plates, were associated with 68% more callus formation. Nevertheless, 26% of the fracture sites stabilized with a titanium plate had deficient callus formation at six months. This finding suggests that a further reduction in plate stiffness is required to decrease the incidence of deficient callus formation leading to fracture nonunion.
Solution: Far Cortical Locking
Far Cortical Locking Reduces Construct Stiffness While Maintaining Construct Strength
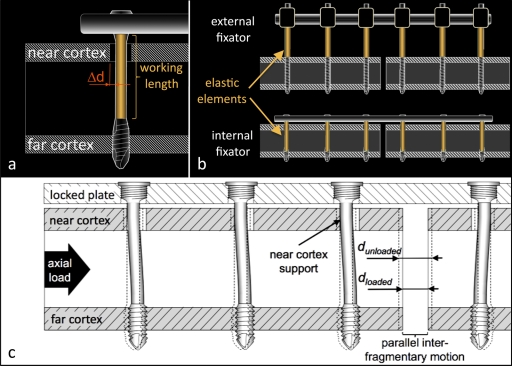
Several strategies to reduce the stiffness of locked-plate constructs have been proposed, including the use of thinner plates, increasing the plate elevation from the bone surface, using slotted holes in the near cortex, and increasing the plate span14,42-44. However, either a reduction in stiffness is gained at the cost of construct strength or stiffness remains insufficient to promote bone-healing by callus formation. Far cortical locking was introduced as an alternative strategy to reduce the stiffness of a locked-plate construct without reducing its strength13. Far-cortical-locking screws lock into the plate and the far cortex of a diaphysis and have a reduced midshaft diameter to bypass the near cortex (Fig. 4, a). Therefore, far-cortical-locking screws have an increased working length, allowing for elastic cantilever bending of the screw shaft within a controlled motion envelope (Δd) in the near cortex. Analogous to external fixators, far-cortical-locking constructs derive flexible fixation and parallel interfragmentary motion from elastic flexion of screw shafts (Fig. 4, b and c). Under elevated loading, contact of the far-cortical-locking screw shaft at the near cortex provides additional support and load-sharing with the near cortex. The ability of far-cortical-locking screws to reduce the stiffness of a locked-plate construct while retaining its strength was formally evaluated in a bench-top study of surrogates of normal and osteoporotic bone13.
Fig. 4.
Far-cortical-locking concept. a: Far-cortical-locking screws lock into the plate and the far cortex. The screws have a reduced midshaft diameter to retain a controlled motion envelope (Δd) in the near cortex, which increases the screw's working length. b: Analogous to external fixators, far-cortical-locking constructs derive a low stiffness from elastic flexion of the screw shafts. c: Flexion of far-cortical-locking screws within the near-cortex motion envelope induces parallel motion at the fracture gap.
Methods
Locked-plate constructs and far-cortical-locking constructs were tested in a diaphyseal bridge-plate configuration under axial compression, torsion, and bending. Generic 4.5-mm locking plates and screws made of titanium alloy were used in all constructs. The far cortical locking was done with locking screws that had a smooth shaft with a 3.2-mm diameter to bypass the near cortex. Plates were applied at a 1-mm elevation from the bone with three screws placed proximally in the first, third, and fifth screw holes from the fracture site and with one hole left empty over the 10-mm osteotomy gap. First, the stiffness of the locked-plate and far-cortical-locking constructs was determined in each principal loading mode in surrogates of a non-osteoporotic femoral diaphysis. Subsequently, the constructs were tested to failure in each loading mode under progressive dynamic loading to determine their strength. Finally, failure tests were repeated in a validated model of an osteoporotic femoral diaphysis45 to determine construct strength in a worst-case scenario of bridge-plate fixation in osteoporotic bone. Each loading mode and construct was tested in five specimens.
Results
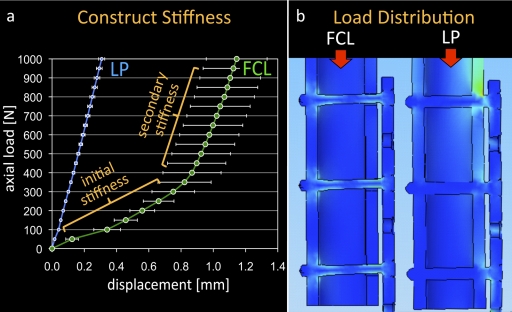
The stiffness of the far-cortical-locking constructs was 88% lower than that of the standard locked-plate constructs under axial compression up to 400 N. At elevated loading, near-cortex support of the far-cortical-locking screws provided a sixfold increase in stiffness. The resulting biphasic stiffness of the far-cortical-locking constructs (Fig. 5, a) resembled the progressive-stiffening behavior characteristic of Ilizarov external fixators. In torsion and bending, the far-cortical-locking constructs provided a 58% and 29% reduction in stiffness, respectively, compared with that of the locked-plate constructs.
Fig. 5.
a: Far-cortical-locking (FCL) constructs exhibit a biphasic stiffness profile, similar to that of Ilizarov external fixators. The primary stiffness was 88% lower than that of the standard locked-plate (LP) construct, enabling interfragmentary motion at reduced postoperative loading. At elevated loads, far-cortical-locking stiffness increases as a result of the additional support of screws at the near cortex. (Reprinted from: Bottlang M, Doornink J, Fitzpatrick DC, Madey SM. Far cortical locking can reduce stiffness of locked-plate constructs while retaining construct strength. J Bone Joint Surg Am. 2009;91:1988.) b: The elastic shaft of far-cortical-locking screws allows evenly distributed load sharing between screws and effectively prevents the stress risers seen at the end-screw of standard locked-plate constructs46.
Interfragmentary motion of the far-cortical-locking constructs in response to 200 N of loading was nearly parallel (0.51 mm and 0.59 mm at the near and far cortices, respectively). Under the same loading, locked-plate constructs yielded less motion, and motion was significantly smaller at the near cortex (0.02 mm) than at the far cortex (0.05 mm, p < 0.01).
In the non-osteoporotic diaphysis, the strength of the far-cortical-locking constructs was 7% lower in compression, 54% higher in torsion, and 21% higher in bending compared with that of the locked-plate constructs. In the osteoporotic diaphysis, the strength of the far-cortical-locking constructs was 16% lower in compression, 9% higher in torsion, and 20% higher in bending compared with that in the locked-plate constructs.
Conclusions
The results of this study demonstrate that far-cortical-locking constructs combine three key factors aimed at promoting secondary bone-healing with locking plates: stiffness reduction, parallel interfragmentary motion, and progressive stiffening. Far-cortical-locking screws reduce the initial stiffness of a locked-plate construct to that of an external fixator. Far-cortical-locking constructs deliver nearly parallel interfragmentary motion within the 0.2 to 1-mm range9,29-31, which is known to promote callus formation. Progressive stiffening of far-cortical-locking constructs provides a low initial stiffness, enabling interfragmentary motion under reduced postoperative weight-bearing, while increased secondary stiffness provides progressive stabilization at elevated loads. The far-cortical-locking constructs retained at least 84% of the axial strength of the locked-plate constructs and were up to 54% stronger in torsion and up to 21% stronger in bending than the locked-plate constructs. The considerable strength increase in torsion and bending may be attributed to evenly distributed load-sharing among all of the far-cortical-locking screws (Fig. 5, b). In contrast, the end-screw of a standard locked construct induces a stress riser, which reduces the construct strength in bending and torsion46. In summary, far-cortical-locking constructs resemble “internal fixators” that combine the benefits of fixed-angle stabilization with flexible fixation for promotion of fracture-healing by callus formation.
Benefits: Improved Healing
Far Cortical Locking Leads to Stronger and More Consistent Fracture-Healing
Determining the effects of construct stiffness on fracture-healing is of central importance to improve clinical outcomes associated with locking plates. Analyzing fracture-healing in clinical studies is complicated by the inherent variability in fracture patterns, quality of fracture reduction and fixation, associated soft-tissue injuries, and patient comorbidities. For over three decades, an ovine tibial osteotomy model has been successfully employed to investigate fracture-healing in a controlled environment47, but the model had not been used to study locking plates. In a recent study48, the ovine fracture-healing model was employed to evaluate healing of fractures stabilized with a locked-plate construct and a far-cortical-locking construct to test the hypothesis that a stiffness-reduced far-cortical-locking construct can improve fracture-healing compared with that associated with a standard locked-plate construct.
Methods
In an established ovine fracture-healing model, tibial osteotomies with a 3-mm gap were performed in twelve sheep and were randomly stabilized with a locked-plate or far-cortical-locking construct (Fig. 6, a). Each construct used the same 4.5-mm titanium locking plate, which was applied either with six locking screws (the locked-plate group) or with six far-cortical-locking screws (the far-cortical-locking group). Compared with the locked-plate constructs, the far-cortical-locking constructs had an 84% lower initial stiffness and provided parallel interfragmentary motion. Progression of fracture-healing was monitored on weekly radiographs. After the animals were killed at week 9, the implants were removed and the callus volume and density were measured with quantitative computed tomography. The mechanical strength of the healed tibiae was assessed with torsion testing to failure in a materials testing system. Finally, callus formation and bridging were analyzed on histological cross sections, harvested from the midsagittal plane of each callus specimen.
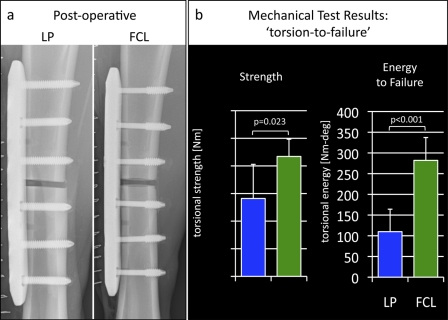
Fig. 6.
Evaluation of fracture-healing with locked-plate (LP) and far-cortical-locking (FCL) constructs in an ovine fracture-healing model. a: Postoperative radiographs depicting 3-mm-gap tibial osteotomy sites stabilized with locked-plate and far-cortical-locking constructs. b: Tibiae treated with far-cortical-locking constructs healed to be 54% stronger with torsional testing and tolerated 156% more energy to failure than tibiae treated with standard locking plates.
Results
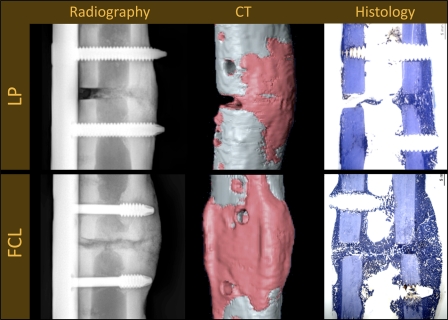
The callus seen on the weekly radiographs was significantly greater in the far-cortical-locking group than it was in the locked-plate group from weeks 4 to 9 (p = 0.004). At week 9, the far-cortical-locking group had 36% more callus (p = 0.03) and 44% more bone mineral content (p = 0.01) than did the locked-plate group. Callus formed symmetrically in the far-cortical-locking group, and there was comparable bone mineral content at the near and far cortices in that group (p = 0.91). In the locked-plate group, callus formed asymmetrically, with 49% less bone mineral content at the near cortex than at the far cortex (p = 0.003). Loading the healed tibiae to failure demonstrated that, compared with the locked-plate specimens, the far-cortical-locking specimens were 54% stronger (p = 0.023) and tolerated 156% more energy until failure (p < 0.001) (Fig. 6, b). Histological sections depicted “partial nonunions,” whereby bridging callus did not form at the near cortex, at the sites of three of the six locked-plate constructs (Fig. 7). In the far-cortical-locking group, bridging callus formed at the near and far cortices in all specimens.
Fig. 7.
Radiographic, computed tomography (CT), and histological evaluation of the tibiae after the sheep was killed at nine weeks after surgery. The locked-plate (LP) constructs suppressed callus formation at the near cortex, where gap motion is minimal, leading to partial nonunions in three of the six sheep. The far-cortical-locking (FCL) constructs induced more callus formation, symmetric callus, and reliable bridging in all six sheep.
Conclusions
This study confirms that standard locked-plate constructs can lead to inconsistent and asymmetric callus formation, whereby fracture-healing is attenuated toward the near cortex adjacent to the plate. Deficient healing is likely caused by the high stiffness and asymmetric gap closure of locked-plate constructs. This study further confirmed that far-cortical-locking constructs actively promote fracture-healing by providing flexible fixation and parallel interfragmentary motion. Compared with locked-plate constructs, far-cortical-locking constructs were associated with more callus formation as well as healing with a stronger osseous union, and they effectively prevented the partial nonunions seen with the locked-plate constructs. Therefore, it was concluded that far-cortical-locking fixation may be advisable for reduction of the stiffness of locked-plate constructs to improve fracture-healing.
Clinical Application: Periarticular Plates
Far-Cortical-Locking Fixation with Periarticular Distal Femoral Plates
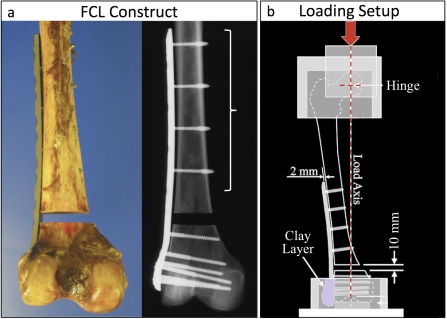
When used for periarticular distal femoral plate fixation, far-cortical-locking screws can readily be applied to the diaphyseal side of the fracture but not to metaphyseal fragments, where fixation in the far cortex cannot be obtained. Therefore, a cadaveric study was conducted to evaluate the efficacy of a hybrid far-cortical-locking construct for periarticular plate fixation whereby far-cortical-locking screws are used for diaphyseal fixation and conventional locking screws are used for metaphyseal fixation with a standard technique. We hypothesized that, compared with a standard locked plate, diaphyseal fixation of a periarticular femoral plate with far-cortical-locking screws would reduce construct stiffness and induce parallel interfragmentary motion without decreasing construct strength.
Methods
Distal femoral fractures (AO/OTA A33-3) were simulated with use of a 1-cm-gap osteotomy in twenty-two paired human femora. The dual x-ray absorptiometry (DXA) T-scores of the femora ranged from –3.4 to 2.5, enabling evaluation of the constructs in osteoporotic and strong bone. All femora were stabilized with the same periarticular locking plate (NCB; Zimmer, Warsaw, Indiana). Six 5.0-mm locking screws were used distally. For proximal fixation, one femur of each pair was stabilized with a standard locked-plate approach with four 5.0-mm locking screws (the locked-plate group); in the contralateral femur, four far-cortical-locking screws (5.0 MotionLoc; Zimmer) were used for proximal fixation (the far-cortical-locking group) (Fig. 8, a). Quasi-physiologic loading was induced along the mechanical axis intersecting the femoral head center and intercondylar notch with a materials testing system (Fig. 8, b). First, specimens were loaded stepwise to 1200 N to assess construct stiffness, which was calculated by dividing the applied load by the resulting interfragmentary motion. Subsequently, 100,000 loading cycles of 1870-N amplitude were applied to assess construct durability during simulated level walking. Finally, the specimens that survived the level-walking test were loaded to failure to assess their residual strength and failure mode. Failure was defined as osteosynthesis gap collapse of 5 mm or catastrophic fracture, whichever occurred first.
Fig. 8.
a: Periarticular far-cortical-locking (FCL) construct, whereby far-cortical-locking screws are used only in the diaphyseal segment and metaphyseal fixation is performed with a standard locked-plate technique. b: Quasi-physiologic loading of cadaveric femora along the mechanical axis to assess construct stiffness, durability, and residual strength was done with this setup.
Results
The initial stiffness of the far-cortical-locking constructs (1.2 ± 0.3 kN/mm) was 81% lower than the stiffness of the locked-plate constructs (6.1 ± 2.4 kN/mm, p < 0.001). Under elevated loading, the stiffness of the far-cortical-locking constructs increased to 3.7 ± 1.2 kN/mm as a result of the additional support of the far-cortical-locking screw shaft at the near cortex. The far-cortical-locking constructs exhibited substantially parallel interfragmentary motion, whereby loading at one times body weight (800 N) induced similar motion at the near cortex (0.57 ± 0.09 mm) and the far cortex (0.63 ± 0.11 mm, p = 0.68) (Fig. 9, a). The locked-plate constructs exhibited on average more than four times less motion (p < 0.001) in response to 800 N, and near-cortex motion (0.10 ± 0.04 mm) was 48% smaller than far-cortex motion (0.19 ± 0.09 mm, p = 0.002).
Fig. 9.
a: In response to loading at one times body weight, standard periarticular locking constructs (the locked-plate [LP] group) induced asymmetric fracture motion. Near-cortex motion remained below 0.1 mm, which is considered insufficient to promote secondary bone-healing. Under the same load, far-cortical-locking (FCL) constructs induced essentially parallel motion, sufficient to promote secondary bone-healing. b: While far-cortical-locking screws reduced construct stiffness by 81%, the far-cortical-locking constructs remained as strong as the locked-plate constructs.
The far-cortical-locking constructs were as durable as the locked-plate constructs: during dynamic loading, four locked-plate constructs and three far-cortical-locking constructs failed. Furthermore, the far-cortical-locking constructs were as strong as the locked-plate constructs: the six surviving locked-plate constructs retained a strength of 4.9 ± 1.6 kN, and the seven surviving far-cortical-locking constructs retained a strength of 5.3 ± 1.1 kN (p = 0.7) (Fig. 9, b).
Radiographs confirmed the same failure modes in the locked-plate and far-cortical-locking groups. Ten of the eleven femur pairs sustained metaphyseal fixation failure by gradual migration of distal screws. The remaining femur pair failed by diaphyseal fracture adjacent to the plate tip. None of the constructs sustained diaphyseal fixation failure, and none of the far-cortical-locking screws exhibited bending or fixation failure.
Conclusions
The results of this study confirm that a far-cortical-locking construct can be used effectively for periarticular plate fixation with the far-cortical-locking screws used only in the diaphyseal segment. When used for periarticular femoral plates, far-cortical-locking screws can reduce construct stiffness by 81% and enable parallel interfragmentary motion of sufficient magnitude to stimulate callus formation. Moreover, far-cortical-locking constructs are as strong and durable as standard-locking constructs in both normal and osteoporotic bone. Therefore, far-cortical-locking fixation may be advisable for periarticular plate fixation to stimulate fracture-healing by controlled interfragmentary motion.
Discussion
While locked-plate constructs are frequently referred to as “internal fixators,” they are much stiffer than external fixators in biomechanical testing and may not provide adequate fracture-site motion to reliably stimulate secondary bone-healing in bridge-plate constructs, especially at the near cortex, where motion is most attenuated. Clinically, attenuated fracture motion resulted in deficient callus formation and a 19% nonunion rate in a retrospective series of supracondylar femoral fractures treated with locking plates17. An ovine fracture-healing model furthermore demonstrated that locked-plate constructs cause asymmetric callus formation and suppress fracture union at the near cortex, where fracture motion is minimal. The resulting “partial nonunions” may contribute to late implant failures and may be underappreciated clinically, since the plate obscures the visibility of the near cortex on radiographs.
Far-cortical-locking screws reduce the stiffness of a locked-plate construct to that of an external fixator and provide parallel interfragmentary motion while retaining construct strength. Hence, far-cortical-locking constructs resemble a true “internal fixator” by combining fixed-angle stabilization and flexible fixation. The performance of far-cortical-locking constructs relies on a particular far-cortical-locking screw design that supports screw flexion while providing a controlled motion envelope in the near cortex to prevent flexion of screw shafts beyond their elastic limit. The ovine fracture model demonstrated that far-cortical-locking constructs outperformed locked-plate constructs by providing symmetric callus formation and reliable bridging and yielded a greater ultimate strength and a higher energy to failure. A study of cadaveric femora demonstrated that periarticular locking plates applied with far-cortical-locking screws in the diaphyseal segment effectively reduce construct stiffness and yield parallel interfragmentary motion in biomechanical testing. These periarticular far-cortical-locking constructs were as strong and durable as standard locked-plate constructs in both normal and osteoporotic bone.
In summary, this research presents further evidence that locked-plate constructs can be too stiff to promote fracture-healing by callus formation. Far-cortical-locking fixation significantly improves fracture-healing by reducing construct stiffness without sacrificing fixation strength or durability.
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases (Grant R21 AR053611) and Zimmer. In addition, one or more of the authors or a member of his or her immediate family received, in any one year, payments or other benefits in excess of $10,000 (Zimmer) and less than $10,000 (Stryker, Augen, Lilly, Biomet Trauma, and Servier) or a commitment or agreement to provide such benefits from these commercial entities.
References
- 1.Fitzpatrick DC, Doornink J, Madey SM, Bottlang M. Relative stability of conventional and locked plating fixation in a model of the osteoporotic femoral diaphysis. Clin Biomech (Bristol, Avon). 2009;24:203-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am. 2006;88 Suppl 4:189-200 [DOI] [PubMed] [Google Scholar]
- 3.Ring D, Kloen P, Kadzielski J, Helfet D, Jupiter JB. Locking compression plates for osteoporotic nonunions of the diaphyseal humerus. Clin Orthop Relat Res. 2004;425:50-4 [DOI] [PubMed] [Google Scholar]
- 4.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093-110 [DOI] [PubMed] [Google Scholar]
- 5.Tan SL, Balogh ZJ. Indications and limitations of locked plating. Injury. 2009;40:683-91 [DOI] [PubMed] [Google Scholar]
- 6.Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488-93 [DOI] [PubMed] [Google Scholar]
- 7.Perren SM. Backgrounds of the technology of internal fixators. Injury. 2003;34 Suppl 2:B1-3 [DOI] [PubMed] [Google Scholar]
- 8.Augat P, Penzkofer R, Nolte A, Maier M, Panzer S, v Oldenburg G, Pueschl K, Simon U, Bühren V. Interfragmentary movement in diaphyseal tibia fractures fixed with locked intramedullary nails. J Orthop Trauma. 2008;22:30-6 [DOI] [PubMed] [Google Scholar]
- 9.Claes LE, Heigele CA, Neidlinger-Wilke C, Kaspar D, Seidl W, Margevicius KJ, Augat P. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;355 Suppl:S132-47 [DOI] [PubMed] [Google Scholar]
- 10.Claes LE, Wilke HJ, Augat P, Rübenacker S, Margevicius KJ. Effect of dynamization on gap healing of diaphyseal fractures under external fixation. Clin Biomech (Bristol, Avon). 1995;10:227-34 [DOI] [PubMed] [Google Scholar]
- 11.Hente R, Füchtmeier B, Schlegel U, Ernstberger A, Perren SM. The influence of cyclic compression and distraction on the healing of experimental tibial fractures. J Orthop Res. 2004;22:709-15 [DOI] [PubMed] [Google Scholar]
- 12.Rahn BA, Gallinaro P, Baltensperger A, Perren SM. Primary bone healing. An experimental study in the rabbit. J Bone Joint Surg Am. 1971;53:783-6 [PubMed] [Google Scholar]
- 13.Bottlang M, Doornink J, Fitzpatrick DC, Madey SM. Far cortical locking can reduce stiffness of locked plating constructs while retaining construct strength. J Bone Joint Surg Am. 2009;91:1985-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardner MJ, Nork SE, Huber P, Krieg JC. Stiffness modulation of locking plate constructs using near cortical slotted holes: a preliminary study. J Orthop Trauma. 2009;23:281-7 [DOI] [PubMed] [Google Scholar]
- 15.Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci. 2006;11:118-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henderson CE, Bottlang M, Marsh JL, Fitzpatrick DC, Madey SM. Does locked plating of periprosthetic supracondylar femur fractures promote bone healing by callus formation? Two cases with opposite outcomes. Iowa Orthop J. 2008;28:73-6 [PMC free article] [PubMed] [Google Scholar]
- 17.Lujan TJ, Henderson CE, Madey SM, Fitzpatrick DC, Marsh JL, Bottlang M. Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma. 2010;24:156-62 [DOI] [PubMed] [Google Scholar]
- 18.Fankhauser F, Gruber G, Schippinger G, Boldin C, Hofer HP, Grechenig W, Szyszkowitz R. Minimal-invasive treatment of distal femoral fractures with the LISS (Less Invasive Stabilization System): a prospective study of 30 fractures with a follow up of 20 months. Acta Orthop Scand. 2004;75:56-60 [DOI] [PubMed] [Google Scholar]
- 19.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509-20 [DOI] [PubMed] [Google Scholar]
- 20.Schütz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, Haas N. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32 Suppl 3:SC48-54 [DOI] [PubMed] [Google Scholar]
- 21.Khalafi A, Curtiss S, Hazelwood S, Wolinsky P. The effect of plate rotation on the stiffness of femoral LISS: a mechanical study. J Orthop Trauma. 2006;20:542-6 [DOI] [PubMed] [Google Scholar]
- 22.Prayson MJ, Datta DK, Marshall MP. Mechanical comparison of endosteal substitution and lateral plate fixation in supracondylar fractures of the femur. J Orthop Trauma. 2001;15:96-100 [DOI] [PubMed] [Google Scholar]
- 23.Caja V, Kim W, Larsson S, E YC. Comparison of the mechanical performance of three types of external fixators: linear, circular and hybrid. Clin Biomech (Bristol, Avon). 1995;10:401-6 [DOI] [PubMed] [Google Scholar]
- 24.Finlay JB, Moroz TK, Rorabeck CH, Davey JR, Bourne RB. Stability of ten configurations of the Hoffmann external-fixation frame. J Bone Joint Surg Am. 1987;69:734-44 [PubMed] [Google Scholar]
- 25.Moroz TK, Finlay JB, Rorabeck CH, Bourne RB. External skeletal fixation: choosing a system based on biomechanical stability. J Orthop Trauma. 1988;2:284-96 [PubMed] [Google Scholar]
- 26.Koval KJ, Hoehl JJ, Kummer FJ, Simon JA. Distal femoral fixation: a biomechanical comparison of the standard condylar buttress plate, a locked buttress plate, and the 95-degree blade plate. J Orthop Trauma. 1997;11:521-4 [DOI] [PubMed] [Google Scholar]
- 27.Stoffel K, Lorenz KU, Kuster MS. Biomechanical considerations in plate osteosynthesis: the effect of plate-to-bone compression with and without angular screw stability. J Orthop Trauma. 2007;21:362-8 [DOI] [PubMed] [Google Scholar]
- 28.Marti A, Fankhauser C, Frenk A, Cordey J, Gasser B. Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma. 2001;15:482-7 [DOI] [PubMed] [Google Scholar]
- 29.Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br. 1985;67:650-5 [DOI] [PubMed] [Google Scholar]
- 30.Kenwright J, Richardson JB, Cunningham JL, White SH, Goodship AE, Adams MA, Magnussen PA, Newman JH. Axial movement and tibial fractures. A controlled randomised trial of treatment. J Bone Joint Surg Br. 1991;73:654-9 [DOI] [PubMed] [Google Scholar]
- 31.Kershaw CJ, Cunningham JL, Kenwright J. Tibial external fixation, weight bearing, and fracture movement. Clin Orthop Relat Res. 1993;293:28-36 [PubMed] [Google Scholar]
- 32.Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury. 2001;32 Suppl 3:SC32-47 [DOI] [PubMed] [Google Scholar]
- 33.Schandelmaier P, Partenheimer A, Koenemann B, Grün OA, Krettek C. Distal femoral fractures and LISS stabilization. Injury. 2001;32 Suppl 3:SC55-63 [DOI] [PubMed] [Google Scholar]
- 34.Raab GE, Davis CM., 3rd Early healing with locked condylar plating of periprosthetic fractures around the knee. J Arthroplasty. 2005;20:984-9 [DOI] [PubMed] [Google Scholar]
- 35.Syed AA, Agarwal M, Giannoudis PV, Matthews SJ, Smith RM. Distal femoral fractures: long-term outcome following stabilisation with the LISS. Injury. 2004;35:599-607 [DOI] [PubMed] [Google Scholar]
- 36.Weight M, Collinge C. Early results of the less invasive stabilization system for mechanically unstable fractures of the distal femur (AO/OTA types A2, A3, C2, and C3). J Orthop Trauma. 2004;18:503-8 [DOI] [PubMed] [Google Scholar]
- 37.Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20:190-6 [DOI] [PubMed] [Google Scholar]
- 38.Vallier HA, Hennessey TA, Sontich JK, Patterson BM. Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am. 2006;88:846-53 [DOI] [PubMed] [Google Scholar]
- 39.Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. J Orthop Trauma. 2004;18:565-70 [DOI] [PubMed] [Google Scholar]
- 40.Kayali C, Agus H, Turgut A. Successful results of minimally invasive surgery for comminuted supracondylar femoral fractures with LISS: comparative study of multiply injured and isolated femoral fractures. J Orthop Sci. 2007;12:458-65 [DOI] [PubMed] [Google Scholar]
- 41.Lujan TJ, Madey SM, Fitzpatrick DC, Byrd GD, Sanderson JM, Bottlang M. A computational technique to measure fracture callus in radiographs. J Biomech. 2010;43:792-5 [DOI] [PubMed] [Google Scholar]
- 42.Stoffel K, Dieter U, Stachowiak G, Gächter A, Kuster MS. Biomechanical testing of the LCP—how can stability in locked internal fixators be controlled? Injury. 2003;34 Suppl 2:B11-9 [DOI] [PubMed] [Google Scholar]
- 43.Ahmad M, Nanda R, Bajwa AS, Candal-Couto J, Green S, Hui AC. Biomechanical testing of the locking compression plate: when does the distance between bone and implant significantly reduce construct stability? Injury. 2007;38:358-64 [DOI] [PubMed] [Google Scholar]
- 44.Kowalski MJ, Schemitsch EH, Harrington RM, Chapman JR, Swiontkowski MF. A comparative biomechanical evaluation of a noncontacting plate and currently used devices for tibial fixation. J Trauma. 1996;40:5-9 [DOI] [PubMed] [Google Scholar]
- 45.Sommers MB, Fitzpatrick DC, Madey SM, Vande Zanderschulp C, Bottlang M. A surrogate long-bone model with osteoporotic material properties for biomechanical testing of fracture implants. J Biomech. 2007;40:3297-304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bottlang M, Doornink J, Byrd GD, Fitzpatrick DC, Madey SM. A nonlocking end screw can decrease fracture risk caused by locked plating in the osteoporotic diaphysis. J Bone Joint Surg Am. 2009;91:620-7 [DOI] [PubMed] [Google Scholar]
- 47.Nunamaker DM. Experimental models of fracture repair. Clin Orthop Relat Res. 1998;355 Suppl:S56-65 [DOI] [PubMed] [Google Scholar]
- 48.Bottlang M, Lesser M, Koerber J, Doornink J, von Rechenberg B, Augat P, Fitzpatrick DC, Madey SM, Marsh JL. Far cortical locking can improve healing of fractures stabilized with locking plates. J Bone Joint Surg Am. 2010;92:1652-60 [DOI] [PMC free article] [PubMed] [Google Scholar]