Introduction
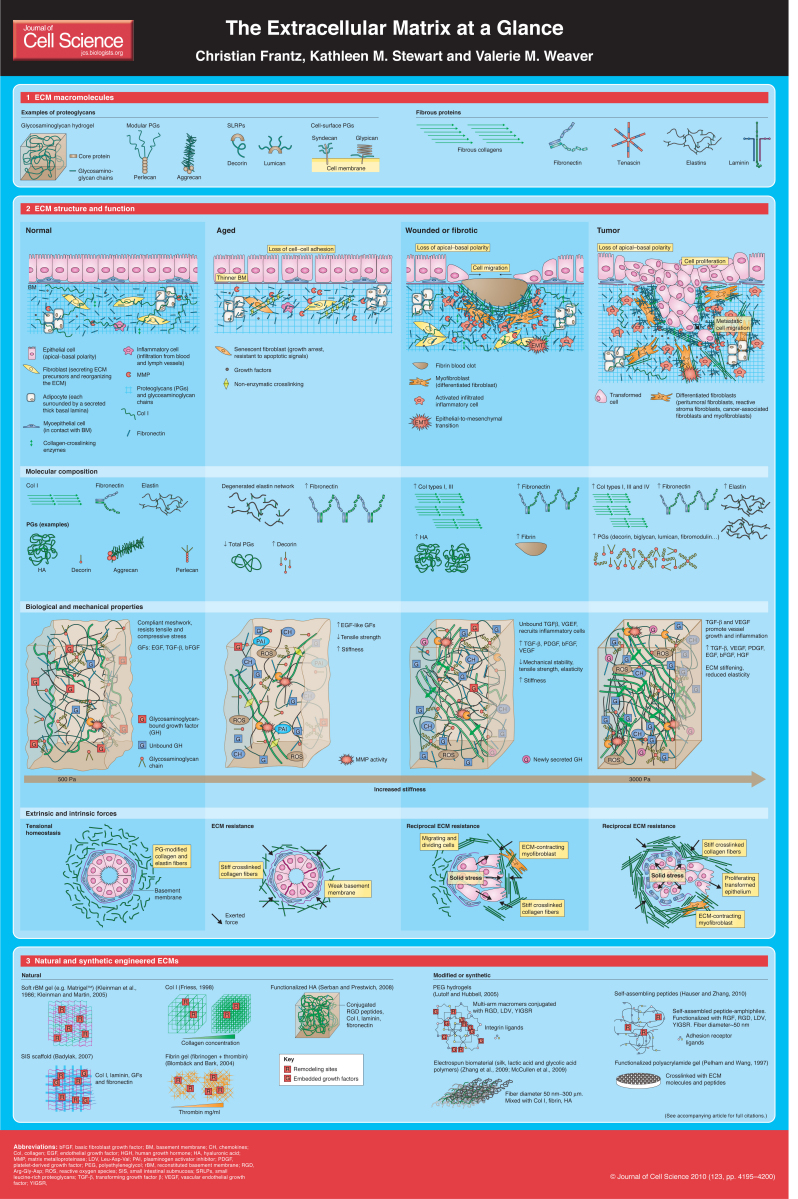
The extracellular matrix (ECM) is the non-cellular component present within all tissues and organs, and provides not only essential physical scaffolding for the cellular constituents but also initiates crucial biochemical and biomechanical cues that are required for tissue morphogenesis, differentiation and homeostasis. The importance of the ECM is vividly illustrated by the wide range of syndromes, which can be anything from minor to severe, that arise from genetic abnormalities in ECM proteins (Jarvelainen et al., 2009). Although, fundamentally, the ECM is composed of water, proteins and polysaccharides, each tissue has an ECM with a unique composition and topology that is generated during tissue development through a dynamic and reciprocal, biochemical and biophysical dialogue between the various cellular components (e.g. epithelial, fibroblast, adipocyte, endothelial elements) and the evolving cellular and protein microenvironment. Indeed, the physical, topological, and biochemical composition of the ECM is not only tissue-specific, but is also markedly heterogeneous. Cell adhesion to the ECM is mediated by ECM receptors, such as integrins, discoidin domain receptors and syndecans (Harburger and Calderwood, 2009; Humphries et al., 2006; Leitinger and Hohenester, 2007; Xian et al., 2010). Adhesion mediates cytoskeletal coupling to the ECM and is involved in cell migration through the ECM (Schmidt and Friedl, 2010). Moreover, the ECM is a highly dynamic structure that is constantly being remodeled, either enzymatically or non-enzymatically, and its molecular components are subjected to a myriad of post-translational modifications. Through these physical and biochemical characteristics the ECM generates the biochemical and mechanical properties of each organ, such as its tensile and compressive strength and elasticity, and also mediates protection by a buffering action that maintains extracellular homeostasis and water retention. In addition, the ECM directs essential morphological organization and physiological function by binding growth factors (GFs) and interacting with cell-surface receptors to elicit signal transduction and regulate gene transcription. The biochemical and biomechanical, protective and organizational properties of the ECM in a given tissue can vary tremendously from one tissue to another (e.g. lungs versus skin versus bone) and even within one tissue (e.g. renal cortex versus renal medulla), as well as from one physiological state to another (normal versus cancerous). In this Cell Science at a Glance article, we briefly describe the main molecular components of the ECM and then compare and contrast the ECM within a normal simple epithelial tissue with that found within a pathologically modified tissue, as exemplified in aged tissue, wounded or fibrotic tissue and tumors. We particularly focus on the composition and architecture of the ECM and interactions with its cellular constituents, and describe in detail common post-translational modifications that evoke defined topological and viscoelasticity changes in the tissue. We thereafter discuss the functional consequences of ECM remodeling on cellular behaviors including altered GF sensitivity elicited by changes in ECM tension. Owing to space limitations and because the basement membrane (BM) is a unique ECM that has been reviewed in detail elsewhere (LeBleu et al., 2007), we focus here on the interstitial stroma of simple glandular epithelial tissues. We complete our review with a brief discussion of the application of natural and synthetic ECMs that can be used to either recapitulate the interstitial ECM in culture to study tissue behaviors or to deconstruct and analyze how specific ECM parameters (stiffness, fiber orientation, ligand presentation, dimensionality) provoke specific cellular behaviors.
Bits and pieces – molecular composition of the ECM
The ECM is composed of two main classes of macromolecules: proteoglycans (PGs) and fibrous proteins (see Boxes 1 and 2) (Jarvelainen et al., 2009; Schaefer and Schaefer, 2010). The main fibrous ECM proteins are collagens, elastins, fibronectins and laminins (see panel 1 of the poster) (Alberts et al., 2007). PGs fill the majority of the extracellular interstitial space within the tissue in the form of a hydrated gel (Box 1) (for details, see Jarvelainen et al., 2009). PGs have a wide variety of functions that reflect their unique buffering, hydration, binding and force-resistance properties. For example, in the kidney glomerular BM, perlecan has a role in glomerular filtration (Harvey and Miner, 2008; Morita et al., 2005). By constrast, in ductal epithelial tissues, decorin, biglycan and lumican associate with collagen fibers to generate a molecular structure within the ECM that is essential for mechanical buffering and hydration and that, by binding GFs, provides an easy, enzymatically accessible repository for these factors (Iozzo and Murdoch, 1996).
Box 1. Structure and function of proteoglycans
Proteoglycans (PGs) are composed of glycosaminoglycan (GAG) chains covalently linked to a specific protein core (with the exception of hyaluronic acid) (Iozzo and Murdoch, 1996; Schaefer and Schaefer, 2010). PGs have been classified according to their core proteins, localization and GAG composition. The three main families are: small leucine-rich proteoglycans (SLRPs), modular proteoglycans and cell-surface proteoglycans (Schaefer and Schaefer, 2010). The GAG chains on the protein core are unbranched polysaccharide chains composed of repeating disaccharide units [sulfated N-aceltylglucosamine or N-acetylgalactosamine, D-glucuronic or L-iduronic acid and galactose (−4 N-acetylglucosamine-β1,3-galactose-β1)] that can be divided further into sulfated (chondroitin sulfate, heparan sulfate and keratan sulfate) and non-sulfated (hyaluronic acid) GAGs (Schaefer and Schaefer, 2010). These molecules are extremely hydrophilic and, accordingly, adopt highly extended conformations that are essential for hydrogel formation and that enable matrices that are formed by these molecules to withstand high compressive forces. Many genetic diseases have been linked to mutations in PG genes (Jarvelainen et al., 2009; Schaefer and Iozzo, 2008). SLRPs have been involved in multiple signaling pathways including binding to and activation of epidermal growth factor receptor (EGFR), insulin-like growth factor 1 receptor (IGFIR) and low-density lipoprotein-receptor-related protein 1 (LRP1), regulation of inflammatory response reaction, binding to and activation of TGFβ (Goldoni and Iozzo, 2008; Schaefer and Iozzo, 2008; Schaefer and Schaefer, 2010). Modular PGs can modulate cell adhesion, migration and proliferation (Schaefer and Schaefer, 2010). Basement membrane modular PGs (perlecan, agrin and collagen type XVIII) have a dual function as pro- and anti-angiogenic factors (Iozzo et al., 2009). Cell-surface PGs (syndecans and glypicans) can act as co-receptor facilitating ligand encounters with signaling receptors (Schaefer and Schaefer, 2010).
Box 2. Collagen and fibronectin synthesis
To date, 28 types of collagen have been identified in vertebrates (Gordon and Hahn, 2010). The majority of collagen molecules form a triple-stranded helix that subsequently can assemble into supramolecular complexes, such as fibrils and networks, depending on the type of collagen. Fibrous collagens form the backbone of the collagen fibril bundles within the interstitial tissue stroma, whereas network collagens are incorporated into the basal membrane (BM). Synthesis of collagen type I involves a number of enzymatic post-translational modifications (Gordon and Hahn, 2010; Myllyharju and Kivirikko, 2004), mainly the hydroxylation of proline and lysine residues, glycosylation of lysine and the cleavage of N- and C-terminal propeptides. Following their cleavage, collagen fibrils are strengthened by the covalent crosslinking between lysine residues of the constituent collagen molecules by lysyl oxidases (LOX) (Myllyharju and Kivirikko, 2004; Robins, 2007).
FN is secreted as a dimer joined by two C-terminal disulfide bonds and has several binding sites to other FN dimers, to collagen, to heparin and also to cell-surface integrin receptors (Pankov and Yamada, 2002). Cell-surface binding of the soluble FN dimer is essential for its assembly into longer fibrils. Moreover, cell contraction through the actomyosin cytoskeleton and the resulting integrin clustering promotes FN–fibril assembly by exposing cryptic binding sites, thus allowing them to bind one another (Leiss et al., 2008; Mao and Schwarzbauer, 2005; Vakonakis and Campbell, 2007).
Collagen is the most abundant fibrous protein within the interstitial ECM and constitutes up to 30% of the total protein mass of a multicellular animal. Collagens, which constitute the main structural element of the ECM, provide tensile strength, regulate cell adhesion, support chemotaxis and migration, and direct tissue development (Rozario and DeSimone, 2010). The bulk of interstitial collagen is transcribed and secreted by fibroblasts that either reside in the stroma or are recruited to it from neighboring tissues (De Wever et al., 2008). By exerting tension on the matrix, fibroblasts are able to organize collagen fibrils into sheets and cables and, thus, can dramatically influence the alignment of collagen fibers. Although within a given tissue, collagen fibers are generally a heterogeneous mix of different types, one type of collagen usually predominates.
Collagen associates with elastin, another major ECM fiber. Elastin fibers provide recoil to tissues that undergo repeated stretch. Importantly, elastin stretch is crucially limited by tight association with collagen fibrils (Wise and Weiss, 2009). Secreted tropoelastin (the precursor of elastin) molecules assemble into fibers and become highly crosslinked to one another via their lysine residues by members of the lysyl oxidase (LOX) enzyme family, which include LOX and LOXL (Lucero and Kagan, 2006). Elastin fibers are covered by glycoprotein microfibrils, mainly fibrillins, which are also essential for the integrity of the elastin fiber (Wise and Weiss, 2009).
A third fibrous protein, fibronectin (FN) is intimately involved in directing the organization of the interstitial ECM and, additionally, has a crucial role in mediating cell attachment and function. FN can be stretched several times over its resting length by cellular traction forces (Smith et al., 2007). Such force-dependent unfolding of FN exposes cryptic integrin-binding sites within the molecule that result in pleiotrophic changes in cellular behavior and implicate FN as an extracellular mechano-regulator (Smith et al., 2007). Indeed, ‘tensed’ FN modulates the catch bond ‘force-activation’ and adhesion assembly of α5β1-integrin through exposure of its synergy site (Friedland et al., 2009). FN is also important for cell migration during development and has been implicated in cardiovascular disease and tumor metastasis (Rozario and DeSimone, 2010; Tsang et al., 2010). Like FN, other ECM proteins such as tenascin exert pleiotrophic effects on cellular behavior, including the promotion of fibroblast migration during wound healing (Trebaul et al., 2007; Tucker and Chiquet-Ehrismann, 2009). Indeed, levels of tenascins C and W are elevated in the stroma of some transformed tissues where they can inhibit the interaction between syndecan4 and FN to promote tumor growth and metastasis (Tucker and Chiquet-Ehrismann, 2009).
The definition of normal – the ECM and tissue homeostasis
Normal glandular epithelial tissues are composed of a simple layer of epithelial cells that adopt apical–basal polarity, where the basal side contacts the BM and the apical side is opposite the fluid-filled lumen. In some glandular epithelium there is a basal or myoepithelial cell layer that separates the luminal epithelium from the interstitial ECM (Barsky and Karlin, 2005). Epithelial tissue homeostasis depends on the maintenance of tissue organization and a dynamic dialogue with a surrounding stroma composed primarily of non-activated fibroblasts and adipocytes, and a steady-state population of transiting, non-stimulated leukocytes (Ronnov-Jessen et al., 1996). Thus, non-activated tissue fibroblasts secrete and organize type I and III collagens, elastin, fibronectin, tenascin and a repertoire of PGs (hyaluronic acid and decorin), which all maintain the structural and functional integrity of the interstitial ECM. Most glandular epithelial tissues including breast, saliva gland, lung, and prostate are in a state of tensional homeostasis so that their normal state is highly mechanically compliant (Paszek and Weaver, 2004). The ECM in a compliant tissue is composed of a relaxed meshwork of type I and III collagens and elastin that, together with FN, form a relaxed network of fibers that are surrounded by and embedded in a hydrogel of glycosaminoglycan-chain-containing PGs (Bosman and Stamenkovic, 2003). Consequently, the relaxed network of collagen and elastin fibers allow the healthy ECM to resist a wide range of tensile stresses. A functionally competent normal tissue can also easily resist compressive stresses because of the binding of the hydrated glycosaminoglycan (GAG) network to the fibrous ECM molecules (Scott, 2003). Thus, the tissue ECM is a highly dynamic entity that continuously undergoes regulated remodeling, whose precise orchestration is crucial to the maintenance of normal function (Egeblad et al., 2010; Kass et al., 2007). Tissue homeostasis is mediated by the coordinated secretion of fibroblast metalloproteinases (MMPs) (Mott and Werb, 2004); this is counterbalanced by tissue inhibitors of metalloproteinases (TIMPs) (Cruz-Munoz and Khokha, 2008) and the controlled activity of other enzymes, such as LOX, and also transglutaminases that crosslink and, consequently, stiffen the ECM (Lucero and Kagan, 2006). A plethora of GFs that are bound to the ECM direct these processes (Friedl, 2010; Hynes, 2009; Macri et al., 2007; Murakami et al., 2008; Oehrl and Panayotou, 2008). These ECM-bound GFs differentially modulate cell growth and migration and, when released, comprise part of a tightly controlled feedback circuit that is essential for normal tissue homeostasis (Hynes, 2009).
Stiffening up – the ECM and tissue aging
As a tissue ages the levels of junctional proteins such as cadherin, catenin or occludin decrease and this loss can compromise junctional integrity as revealed by the appearance of gaps between the epithelial cells (Akintola et al., 2008; Bolognia, 1995). Old tissue is also characterized by a thinning of the BM, probably because of elevated MMP-mediated degradation and reduced BM protein synthesis (Callaghan and Wilhelm, 2008). Moreover, the resident fibroblasts in aged tissues are growth-arrested and resistant to apoptotic cues, which is indicative of senescence (Campisi and d'Adda di Fagagna, 2007). Indeed, senescent fibroblasts typically express elevated levels of FN, MMPs, GFs, interleukins and cytokines, as well as high levels of the plasminogen activator inhibitor (PAI) (Coppe et al., 2010) and mitochondrial-related reactive oxygen species (ROS) (Untergasser et al., 2005) and, as a result, are frequently in a state of chronic inflammation. Indeed, the combination of chronic inflammation and elevated MMPs, PAI and ROS destroy the integrity of the elastin network and modify the collagen fiber network, whereas reduced levels of tissue-associated GAGs compromise the integrity of the BM (Callaghan and Wilhelm, 2008; Calleja-Agius et al., 2007; Nomura, 2006). Nevertheless, and somewhat paradoxically, in an aging tissue, collagen fibers are frequently – inappropriately – crosslinked through glycation, by byproducts of lipid oxidation and through exposure to UV light (Robins, 2007). The combination of elevated and inappropriate collagen crosslinking contributes to tissue stiffening so that an aged tissue is mechanically weaker and less elastic but also more rigid than a young tissue (Calleja-Agius et al., 2007; Robins, 2007). This aberrant mechanical state can severely compromise ECM organization, and modify epithelial organization and function, potentially promoting age-related diseases such as cancer (Coppe et al., 2010; Freund et al., 2010; Sprenger et al., 2008).
Tensional homeostasis and fibrosis
Acute injury activates the fibrogenic machinery and induces wound healing. One of the first events that characterize a wound response is vascular damage and the formation of a fibrin clot, which stimulates monocyte infiltration to the damaged ECM. Upon binding to ECM-degradation products and cytokines, monocytes rapidly differentiate into macrophages (Clark, 2001). These activated macrophages, in turn, secrete and release multiple GFs, MMPs and cytokines that promote angiogenesis and stimulate fibroblast migration and proliferation (Schultz and Wysocki, 2009). Thereafter, recruited fibroblasts begin to synthesize and deposit large quantities of ECM proteins, including collagen type I and III, FN and hyaluronic acid. The elevated mechanical stress associated with this profound ECM deposition can induce the transdifferentiation of fibroblasts and other tissue-resident cells – i.e. epithelial-to-mesenchymal transition (EMT) of epithelial cells – or of circulating bone marrow-derived mesenchymal stem cells into myofibroblasts (Schultz and Wysocki, 2009; Velnar et al., 2009). Myofibroblasts, which have a high capacity to synthesize ECM components and are highly contractile, can promote the formation of large, rigid collagen bundles that, if crosslinked by LOX enzymes, mechanically strengthen and stiffen the tissue (Szauter et al., 2005). This wounded ‘stiffened’ microenvironment disrupts the BM that surrounds the epithelium and compromises tissue integrity with loss of apical–basal polarity and destabilized cell–cell adhesions. The remodeled ECM also promotes the directional migration of cells within the tissue towards the wound site (Schafer and Werner, 2008). In some instances, the release of transforming growth factor β (TGF-β) by tension and MMPs induces EMT of the resident epithelium (Schultz and Wysocki, 2009; Wipff et al., 2007; Xu et al., 2009). In a healthy tissue, once the wound has been repopulated, strict feedback mechanisms are initiated that ensure restoration of tissue homeostasis and resolution of fibrosis (Schultz and Wysocki, 2009; Velnar et al., 2009). Under extreme conditions, such as repeated injury or when normal feedback mechanisms are compromised, continuous ECM synthesis, deposition and remodeling ensue and myofibroblasts remain, in which TIMP production prevails over MMP synthesis. These aberrant conditions promote chronic vascular remodeling and enhanced ECM crosslinking that eventually leads to aberrant fibrosis and an inability of the tissue to heal properly. This aberrant wound healing scenario is characterized by the altered mechanical stability and reduced elasticity that is typical of scarred tissue (Kisseleva and Brenner, 2008). In extreme cases, a chronic wound can also promote a tumor phenotype (De Wever et al., 2008).
Tumors – a tough situation
Cancer is the loss of tissue organization and aberrant behavior of the cellular components. Cell transformation results from genetic mutations and epigenetic alterations. Yet, tumors have also been likened to wounds that fail to heal (Schafer and Werner, 2008). Thus, the tumor stroma exhibits some of the characteristics found in an unresolved wound (Bissell and Radisky, 2001). For example, tumors are characteristically stiffer than the surrounding normal tissue. The stiffening of tumors is induced by ECM deposition and remodeling by resident fibroblasts, and by increased contractility of the transformed epithelium (Butcher et al., 2009; Levental et al., 2009). Moreover, chemokines and GFs (De Wever et al., 2008) induce inflammation and modify the repertoire of infiltrating T lymphocytes (Tan and Coussens, 2007). Tissue inflammation potentiates stromal fibroblast activation and induces their transdifferentiation into myofibroblasts, thus exacerbating and promoting tissue desmoplasia (De Wever et al., 2008; Desmouliere et al., 2004). Myofibroblasts deposit copious quantities of ECM proteins, secrete GFs and exert strong contraction forces on the ECM (De Wever et al., 2008; Desmouliere et al., 2004). As a consequence, newly deposited and remodeled collagen and elastin fibers are reoriented and, thereafter, crosslinked by LOX and transglutaminase, thus generating larger, more-rigid fibrils that further stiffen the tissue ECM (Butcher et al., 2009; Erler and Weaver, 2009; Levental et al., 2009; Lucero and Kagan, 2006; Payne et al., 2007; Rodriguez et al., 2008). MMPs, which are secreted and activated by tumor cells and by myofibroblasts (De Wever et al., 2008; Kessenbrock et al., 2010), also remodel the BM surrounding the tumor and release and activate ECM-embedded GFs (Bosman and Stamenkovic, 2003; Kessenbrock et al., 2010). The release of GFs, including vascular endothelial growth factor (VEGF), enhances vascular permeability and promotes new vessel growth, which generates interstitial tissue pressure. Thus, an amplifying circuitry between tumor-associated ECM stiffening, an ensuing reciprocal ECM resistance that is induced by resident tumor cells, and myoepithelial and cell-generated contractility act as a vicious, positive-feedback loop to potentiate tumor growth and survival. This induces angiogenesis and invasion and, eventually, fosters metastasis (Butcher et al., 2009; Erler and Weaver, 2009; Paszek and Weaver, 2004; Paszek et al., 2005).
Where do we go from here? Challenges encountered with natural and synthetic ECMs
Considering the importance of the ECM to so many fundamental cellular processes, a myriad of tissue-culture models have been developed to study the interplay between its biochemical and biophysical properties, and to understand the molecular origins of cellular behaviors regulated by ECM ligation. With respect to assessing the fundamental nature of cell adhesion and its effects on cell behavior, the majority of cancer researchers have relied on coating tissue culture dishes (whether plastic or glass) with purified preparations or mixtures of ECM proteins in order to obtain 2D monolayers (Kuschel et al., 2006). To address the issue of ECM rigidity, functionalized polyacrylamide (PA) gels crosslinked with reconstituted basement membrane (rBM) – generated from Engelbreth-Holm-Swarm mouse carcinoma (commercially available as Matrigel™), collagen type I, FN or ECM peptides – has become the standard approach (Johnson et al., 2007; Pelham and Wang, 1997). Yet, none of these strategies faithfully recapitulates the behavior of cells within tissues, which demand not only a 3D format, but an ECM that can be readily remodeled. To address the aspect of 3D and ECM remodeling, researchers have used natural ECM and reconstituted ECM gels to recapitulate specific aspects of tissue-specific differentiation and architecture (see poster, panel 3). For instance, the rBM, which mimics some of the biochemical and biophysical properties of endogenous epithelial basement membranes, has been used frequently in 3D organotypic culture assays, for xenograft manipulations or tissue engineering, and to study tissue-specific morphogenesis (e.g. branching, acini formation) and differentiation (Kleinman and Martin, 2005; Kleinman et al., 1986). Unfortunately, BM preparations such as Matrigel™, although useful for studying normal epithelial or endothelial behavior and to distinguish between the ‘normal’ and ‘malignant’ behavior of some tissues, has a complex and rudimentarily defined composition, and fails to reconstruct the physical state of the native interstitial ECM. Fibrin has also been used as natural biodegradable scaffold with reasonable success in vascular tissue engineering, but lacks the mechanical strength and durability of native interstitial ECM (Blomback and Bark, 2004; Shaikh et al., 2008). By contrast, type I collagen is reasonably useful and can be combined with rBM, purified laminin or FN to reconstitute some of the biological aspects of normal and diseased interstitial ECM (Friess, 1998; Gudjonsson et al., 2002). Moreover, collagen type I readily assembles into a mechanically tense network of fibrils that can be oriented, functionally modified, and enzymatically or chemically crosslinked and stiffened. Thus collagen I gels are useful substrates to assess the role of collagen and FN stiffness, and organization on the pathogenesis of tumor progression and invasion (Levental et al., 2009; Provenzano et al., 2009). Nevertheless, collagen gels are quite heterogeneous, and modifying their architecture changes their organization, pore size and ligand concentration, thereby complicating the interpretation of data generated from experiments conducted by using this natural scaffold (Johnson et al., 2007). To overcome this issue, tissue engineers and biomaterial specialists have generated denuded ECM scaffold from various tissues (Macchiarini et al., 2008). These scaffolds, combined with colonies of seeded stem cells, can reconstitute normal tissues with reasonable fidelity (Lutolf et al., 2009). ECMs have also been isolated and extracted from various tissues, such as small intestine, skin (from cadavers), pancreas and breast (Rosso et al., 2005), and these ECMs have been used to engineer skin grafts (Badylak, 2007), enhance wound healing and to study tumor progression. One such example is given by porcine-derived small intestinal submucosa (SIS), which has proven clinical success for treating patients with hernias (Franklin et al., 2002) (reviewed in Badylak, 2007). Although these purified ECMs certainly have useful applications, their use is limited in scope owing to the need for well-defined microenvironments in tissue regeneration and stem cell transplantation in which animal byproducts and contaminants are limited. Moreover, to understand the molecular and biophysical mechanisms by which the ECM elicits diverse effects on cellular differentiation and morphogenesis it is crucial to use chemically and physically defined, modular ECMs that can be reliably reproduced. In this respect, synthetic matrices have been developed that feature defined and tunable compositions, organization, mechanics and ECM remodeling capabilities. Indeed, in response to this need there has been literally an explosion of publications describing the generation and application of synthetic ECMs for tissue regeneration, and the reader is referred to some excellent reviews on these topics (Ayres et al., 2009; Dutta and Dutta, 2009; Lutolf and Hubbell, 2005; McCullen et al., 2009; Rosso et al., 2005; Zisch et al., 2003). One example is given by polyethylene glycol (PEG) hydrogels – frequently used biologically compatible synthetic matrices that support cell adhesion, viability and growth (Lutolf and Hubbell, 2005). Although these matrices can be covalently modified with ECM ligands and collagenase-degradable peptides and GFs (Ehrbar et al., 2007; Zisch et al., 2003), they do not mimic the organizational features of native collagen gels and all too often their pore sizes strongly impede cell migration. By contrast, peptide-based hydrogels, such as peptideamphiphiles, assemble into secondary structures that recapitulate the collagen triple helix, and readily support stem cell growth and viability, and direct multicellular morphogenesis (Hauser and Zhang, 2010; Sieminski et al., 2008; Smith and Ma, 2004; Ulijn and Smith, 2008). These peptides-amphiphiles are amenable to modification by covalent binding of native proteins and MMP-degradable ECM peptides. Alternatively, poly(lactic-co-glycolic acid) (PLGA), a copolymer of glycolic acid and lactic acid (McCullen et al., 2009) that is inherently biodegradable as it is hydrolyzed into lactic acid and glycolic acid, has been developed and can be readily conjugated to various ECM ligands and peptides, or coated with collagen or chitosan to support cell adhesion, viability and growth. Indeed, one of the most exciting recent advances in the field has been the development of modular biocompatible ECMs, which contain ligand-binding cassettes and have tunable stiffness features that permit a precise patterning of cell adhesion in 2D and 3D formats (Serban and Prestwich, 2008). The realization that ECM organization is a crucial aspect of cellular behavior has led to the development of new methodologies and generated ECMs whose fiber size, orientation, stiffness, ligand-binding function and remodeling potential can be strictly controlled and monitored – including electrospun silk, and lactic-acid polymer (PLLA) and PLGA scaffolds (Zhang et al., 2009). Anisotropically nanofabricated substrates formed from scalable biocompatible PEG (Kim et al., 2010; Smith et al., 2009) are exciting new developments in the biomaterials field, whose only major impediment to their biological application appears to be a lack of functional assessment in physiological culture assays and animal models. Although only time can tell whether this new generation of biomaterials will indeed prove useful, it is an appealing time to be an ECM biologist and our next challenge will be to embrace this smorgasbord of enticing new tools – which hopefully will at last allow us to decipher the language of the matrix.
Acknowledgments
This work was supported by the NIH grants U54CA143836 and CA138818-01A1 and the DOD grant W81XWH-05-1-0330 to V.M.W. Deposited in PMC for release after 12 months.
References
- Akintola A. D., Crislip Z. L., Catania J. M., Chen G., Zimmer W. E., Burghardt R. C., Parrish A. R. (2008). Promoter methylation is associated with the age-dependent loss of N-cadherin in the rat kidney. Am. J. Physiol. Renal Physiol. 294, F170-F176 [DOI] [PubMed] [Google Scholar]
- Alberts B., Johnson A., Lewis J., Raff M., Roberts K., Walter P. (2007). Molecular Biology of the Cell. London: Garland Science; [Google Scholar]
- Ayres C. E., Jha B. S., Sell S. A., Bowlin G. L., Simpson D. G. (2009). Nanotechnology in the design of soft tissue scaffolds: innovations in structure and function. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2, 20-34 [DOI] [PubMed] [Google Scholar]
- Badylak S. F. (2007). The extracellular matrix as a biologic scaffold material. Biomaterials 28, 3587-3593 [DOI] [PubMed] [Google Scholar]
- Barsky S. H., Karlin N. J. (2005). Myoepithelial cells: autocrine and paracrine suppressors of breast cancer progression. J. Mammary Gland Biol. Neoplasia 10, 249-260 [DOI] [PubMed] [Google Scholar]
- Bissell M. J., Radisky D. (2001). Putting tumours in context. Nat. Rev. Cancer 1, 46-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blombäck B., Bark N. (2004). Fibrinopeptides and fibrin gel structure. Biophys. Chem. 112, 147-151 [DOI] [PubMed] [Google Scholar]
- Bolognia J. L. (1995). Aging skin. Am. J. Med. 98, 99S-103S [DOI] [PubMed] [Google Scholar]
- Bosman F. T., Stamenkovic I. (2003). Functional structure and composition of the extracellular matrix. J. Pathol. 200, 423-428 [DOI] [PubMed] [Google Scholar]
- Butcher D. T., Alliston T., Weaver V. M. (2009). A tense situation: forcing tumour progression. Nat. Rev. Cancer 9, 108-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan T. M., Wilhelm K. P. (2008). A review of ageing and an examination of clinical methods in the assessment of ageing skin. Part 2, Clinical perspectives and clinical methods in the evaluation of ageing skin. Int. J. Cosmet. Sci. 30, 323-332 [DOI] [PubMed] [Google Scholar]
- Calleja-Agius J., Muscat-Baron Y., Brincat M. P. (2007). Skin ageing. Menopause Int. 13, 60-64 [DOI] [PubMed] [Google Scholar]
- Campisi J., d'Adda di Fagagna F. (2007). Cellular senescence: when bad things happen to good cells. Nat. Rev. Mol. Cell Biol. 8, 729-740 [DOI] [PubMed] [Google Scholar]
- Clark R. A. (2001). Fibrin and wound healing. Ann. NY Acad. Sci. 936, 355-367 [DOI] [PubMed] [Google Scholar]
- Coppe J. P., Desprez P. Y., Krtolica A., Campisi J. (2010). The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu. Rev. Pathol. 5, 99-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Munoz W., Khokha R. (2008). The role of tissue inhibitors of metalloproteinases in tumorigenesis and metastasis. Crit. Rev. Clin. Lab. Sci. 45, 291-338 [DOI] [PubMed] [Google Scholar]
- De Wever O., Demetter P., Mareel M., Bracke M. (2008). Stromal myofibroblasts are drivers of invasive cancer growth. Int. J. Cancer 123, 2229-2238 [DOI] [PubMed] [Google Scholar]
- Desmouliere A., Guyot C., Gabbiani G. (2004). The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. Int. J. Dev. Biol. 48, 509-517 [DOI] [PubMed] [Google Scholar]
- Dutta R. C., Dutta A. K. (2009). Cell-interactive 3D-scaffold; advances and applications. Biotechnol. Adv. 27, 334-339 [DOI] [PubMed] [Google Scholar]
- Egeblad M., Rasch M. G., Weaver V. M. (2010). Dynamic interplay between the collagen scaffold and tumor evolution. Curr. Opin. Cell Biol. 22, 697-706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrbar M., Rizzi S. C., Schoenmakers R. G., Miguel B. S., Hubbell J. A., Weber F. E., Lutolf M. P. (2007). Biomolecular hydrogels formed and degraded via site-specific enzymatic reactions. Biomacromolecules 8, 3000-3007 [DOI] [PubMed] [Google Scholar]
- Erler J. T., Weaver V. M. (2009). Three-dimensional context regulation of metastasis. Clin. Exp. Metastasis 26, 35-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin M. E., Jr, Gonzalez J. J., Jr, Michaelson R. P., Glass J. L., Chock D. A. (2002). Preliminary experience with new bioactive prosthetic material for repair of hernias in infected fields. Hernia 6, 171-174 [DOI] [PubMed] [Google Scholar]
- Freund A., Orjalo A. V., Desprez P. Y., Campisi J. (2010). Inflammatory networks during cellular senescence: causes and consequences. Trends Mol. Med. 16, 238-246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedl A. (2010). Proteoglycans: master modulators of paracrine fibroblast-carcinoma cell interactions. Semin. Cell Dev. Biol. 21, 66-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedland J. C., Lee M. H., Boettiger D. (2009). Mechanically activated integrin switch controls alpha5beta1 function. Science 323, 642-644 [DOI] [PubMed] [Google Scholar]
- Friess W. (1998). Collagen-biomaterial for drug delivery. Eur. J. Pharm. Biopharm. 45, 113-136 [DOI] [PubMed] [Google Scholar]
- Goldoni S., Iozzo R. V. (2008). Tumor microenvironment: modulation by decorin and related molecules harboring leucine-rich tandem motifs. Int. J. Cancer 123, 2473-2479 [DOI] [PubMed] [Google Scholar]
- Gordon M. K., Hahn R. A. (2010). Collagens. Cell Tissue Res. 339, 247-257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudjonsson T., Ronnov-Jessen L., Villadsen R., Rank F., Bissell M. J., Petersen O. W. (2002). Normal and tumor-derived myoepithelial cells differ in their ability to interact with luminal breast epithelial cells for polarity and basement membrane deposition. J. Cell Sci. 115, 39-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harburger D. S., Calderwood D. A. (2009). Integrin signalling at a glance. J. Cell Sci. 122, 159-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey S. J., Miner J. H. (2008). Revisiting the glomerular charge barrier in the molecular era. Curr. Opin. Nephrol. Hypertens. 17, 393-398 [DOI] [PubMed] [Google Scholar]
- Hauser C. A., Zhang S. (2010). Designer self-assembling peptide nanofiber biological materials. Chem. Soc. Rev. 39, 2780-2790 [DOI] [PubMed] [Google Scholar]
- Humphries J. D., Byron A., Humphries M. J. (2006). Integrin ligands at a glance. J. Cell Sci. 119, 3901-3903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynes R. O. (2009). The extracellular matrix: not just pretty fibrils. Science 326, 1216-1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iozzo R. V., Murdoch A. D. (1996). Proteoglycans of the extracellular environment: clues from the gene and protein side offer novel perspectives in molecular diversity and function. FASEB J. 10, 598-614 [PubMed] [Google Scholar]
- Iozzo R. V., Zoeller J. J., Nystrom A. (2009). Basement membrane proteoglycans: modulators Par Excellence of cancer growth and angiogenesis. Mol. Cells 27, 503-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvelainen H., Sainio A., Koulu M., Wight T. N., Penttinen R. (2009). Extracellular matrix molecules: potential targets in pharmacotherapy. Pharmacol. Rev. 61, 198-223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K. R., Leight J. L., Weaver V. M. (2007). Demystifying the effects of a three-dimensional microenvironment in tissue morphogenesis. Methods Cell Biol. 83, 547-583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kass L., Erler J. T., Dembo M., Weaver V. M. (2007). Mammary epithelial cell: influence of extracellular matrix composition and organization during development and tumorigenesis. Int. J. Biochem. Cell Biol. 39, 1987-1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessenbrock K., Plaks V., Werb Z. (2010). Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141, 52-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. H., Lipke E. A., Kim P., Cheong R., Thompson S., Delannoy M., Suh K. Y., Tung L., Levchenko A. (2010). Nanoscale cues regulate the structure and function of macroscopic cardiac tissue constructs. Proc. Natl. Acad. Sci. USA 107, 565-570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisseleva T., Brenner D. A. (2008). Mechanisms of fibrogenesis. Exp. Biol. Med. (Maywood) 233, 109-122 [DOI] [PubMed] [Google Scholar]
- Kleinman H. K., Martin G. R. (2005). Matrigel: basement membrane matrix with biological activity. Semin. Cancer Biol. 15, 378-386 [DOI] [PubMed] [Google Scholar]
- Kleinman H. K., McGarvey M. L., Hassell J. R., Star V. L., Cannon F. B., Laurie G. W., Martin G. R. (1986). Basement membrane complexes with biological activity. Biochemistry 25, 312-318 [DOI] [PubMed] [Google Scholar]
- Kuschel C., Steuer H., Maurer A. N., Kanzok B., Stoop R., Angres B. (2006). Cell adhesion profiling using extracellular matrix protein microarrays. Biotechniques 40, 523-531 [DOI] [PubMed] [Google Scholar]
- LeBleu V. S., Macdonald B., Kalluri R. (2007). Structure and function of basement membranes. Exp. Biol. Med. (Maywood) 232, 1121-1129 [DOI] [PubMed] [Google Scholar]
- Leiss M., Beckmann K., Giros A., Costell M., Fassler R. (2008). The role of integrin binding sites in fibronectin matrix assembly in vivo. Curr. Opin. Cell Biol. 20, 502-507 [DOI] [PubMed] [Google Scholar]
- Leitinger B., Hohenester E. (2007). Mammalian collagen receptors. Matrix Biol. 26, 146-155 [DOI] [PubMed] [Google Scholar]
- Levental K. R., Yu H., Kass L., Lakins J. N., Egeblad M., Erler J. T., Fong S. F., Csiszar K., Giaccia A., Weninger W., et al. (2009). Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 139, 891-906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero H. A., Kagan H. M. (2006). Lysyl oxidase: an oxidative enzyme and effector of cell function. Cell. Mol. Life Sci. 63, 2304-2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutolf M. P., Hubbell J. A. (2005). Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat. Biotechnol. 23, 47-55 [DOI] [PubMed] [Google Scholar]
- Lutolf M. P., Gilbert P. M., Blau H. M. (2009). Designing materials to direct stem-cell fate. Nature 462, 433-441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macchiarini P., Jungebluth P., Go T., Asnaghi M. A., Rees L. E., Cogan T. A., Dodson A., Martorell J., Bellini S., Parnigotto P. P., et al. (2008). Clinical transplantation of a tissue-engineered airway. Lancet 372, 2023-2030 [DOI] [PubMed] [Google Scholar]
- Macri L., Silverstein D., Clark R. A. (2007). Growth factor binding to the pericellular matrix and its importance in tissue engineering. Adv. Drug Deliv. Rev. 59, 1366-1381 [DOI] [PubMed] [Google Scholar]
- Mao Y., Schwarzbauer J. E. (2005). Fibronectin fibrillogenesis, a cell-mediated matrix assembly process. Matrix Biol. 24, 389-399 [DOI] [PubMed] [Google Scholar]
- McCullen S. D., Ramaswamy S., Clarke L. I., Gorga R. E. (2009). Nanofibrous composites for tissue engineering applications. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 1, 369-390 [DOI] [PubMed] [Google Scholar]
- Morita H., Yoshimura A., Inui K., Ideura T., Watanabe H., Wang L., Soininen R., Tryggvason K. (2005). Heparan sulfate of perlecan is involved in glomerular filtration. J. Am. Soc. Nephrol. 16, 1703-1710 [DOI] [PubMed] [Google Scholar]
- Mott J. D., Werb Z. (2004). Regulation of matrix biology by matrix metalloproteinases. Curr. Opin. Cell Biol. 16, 558-564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami M., Elfenbein A., Simons M. (2008). Non-canonical fibroblast growth factor signalling in angiogenesis. Cardiovasc. Res. 78, 223-231 [DOI] [PubMed] [Google Scholar]
- Myllyharju J., Kivirikko K. I. (2004). Collagens, modifying enzymes and their mutations in humans, flies and worms. Trends Genet. 20, 33-43 [DOI] [PubMed] [Google Scholar]
- Nomura Y. (2006). Structural change in decorin with skin aging. Connect. Tissue Res. 47, 249-255 [DOI] [PubMed] [Google Scholar]
- Oehrl W., Panayotou G. (2008). Modulation of growth factor action by the extracellular matrix. Connect. Tissue Res. 49, 145-148 [DOI] [PubMed] [Google Scholar]
- Pankov R., Yamada K. M. (2002). Fibronectin at a glance. J. Cell Sci. 115, 3861-3863 [DOI] [PubMed] [Google Scholar]
- Paszek M. J., Weaver V. M. (2004). The tension mounts: mechanics meets morphogenesis and malignancy. J. Mammary Gland Biol. Neoplasia 9, 325-342 [DOI] [PubMed] [Google Scholar]
- Paszek M. J., Zahir N., Johnson K. R., Lakins J. N., Rozenberg G. I., Gefen A., Reinhart-King C. A., Margulies S. S., Dembo M., Boettiger D., et al. (2005). Tensional homeostasis and the malignant phenotype. Cancer Cell 8, 241-254 [DOI] [PubMed] [Google Scholar]
- Payne S. L., Hendrix M. J., Kirschmann D. A. (2007). Paradoxical roles for lysyl oxidases in cancer-a prospect. J. Cell Biochem. 101, 1338-1354 [DOI] [PubMed] [Google Scholar]
- Pelham R. J., Jr, Wang Y. (1997). Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc. Natl. Acad. Sci. USA 94, 13661-13665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provenzano P. P., Eliceiri K. W., Keely P. J. (2009). Shining new light on 3D cell motility and the metastatic process. Trends Cell. Biol. 19, 638-648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins S. P. (2007). Biochemistry and functional significance of collagen cross-linking. Biochem. Soc. Trans. 35, 849-852 [DOI] [PubMed] [Google Scholar]
- Rodriguez C., Rodriguez-Sinovas A., Martinez-Gonzalez J. (2008). Lysyl oxidase as a potential therapeutic target. Drug News Perspect. 21, 218-224 [DOI] [PubMed] [Google Scholar]
- Ronnov-Jessen L., Petersen O. W., Bissell M. J. (1996). Cellular changes involved in conversion of normal to malignant breast: importance of the stromal reaction. Physiol. Rev. 76, 69-125 [DOI] [PubMed] [Google Scholar]
- Rosso F., Marino G., Giordano A., Barbarisi M., Parmeggiani D., Barbarisi A. (2005). Smart materials as scaffolds for tissue engineering. J. Cell Physiol. 203, 465-470 [DOI] [PubMed] [Google Scholar]
- Rozario T., DeSimone D. W. (2010). The extracellular matrix in development and morphogenesis: a dynamic view. Dev. Biol. 341, 126-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer L., Iozzo R. V. (2008). Biological functions of the small leucine-rich proteoglycans: from genetics to signal transduction. J. Biol. Chem. 283, 21305-21309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer L., Schaefer R. M. (2010). Proteoglycans: from structural compounds to signaling molecules. Cell Tissue Res. 339, 237-246 [DOI] [PubMed] [Google Scholar]
- Schafer M., Werner S. (2008). Cancer as an overhealing wound: an old hypothesis revisited. Nat. Rev. Mol. Cell Biol. 9, 628-638 [DOI] [PubMed] [Google Scholar]
- Schmidt S., Friedl P. (2010). Interstitial cell migration: integrin-dependent and alternative adhesion mechanisms. Cell Tissue Res. 339, 83-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz G. S., Wysocki A. (2009). Interactions between extracellular matrix and growth factors in wound healing. Wound Repair Regen. 17, 153-162 [DOI] [PubMed] [Google Scholar]
- Scott J. E. (2003). Elasticity in extracellular matrix ‘shape modules’ of tendon, cartilage, etc. A sliding proteoglycan-filament model. J. Physiol. 553, 335-343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serban M. A., Prestwich G. D. (2008). Modular extracellular matrices: solutions for the puzzle. Methods 45, 93-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaikh F. M., Callanan A., Kavanagh E. G., Burke P. E., Grace P. A., McGloughlin T. M. (2008). Fibrin: a natural biodegradable scaffold in vascular tissue engineering. Cells Tissues Organs 188, 333-346 [DOI] [PubMed] [Google Scholar]
- Sieminski A. L., Semino C. E., Gong H., Kamm R. D. (2008). Primary sequence of ionic self-assembling peptide gels affects endothelial cell adhesion and capillary morphogenesis. J. Biomed. Mater. Res. A 87, 494-504 [DOI] [PubMed] [Google Scholar]
- Smith I. O., Liu X. H., Smith L. A., Ma P. X. (2009). Nanostructured polymer scaffolds for tissue engineering and regenerative medicine. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 1, 226-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L. A., Ma P. X. (2004). Nano-fibrous scaffolds for tissue engineering. Colloids Surf. B Biointerfaces 39, 125-131 [DOI] [PubMed] [Google Scholar]
- Smith M. L., Gourdon D., Little W. C., Kubow K. E., Eguiluz R. A., Luna-Morris S., Vogel V. (2007). Force-induced unfolding of fibronectin in the extracellular matrix of living cells. PLoS Biol. 5, e268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprenger C. C., Plymate S. R., Reed M. J. (2008). Extracellular influences on tumour angiogenesis in the aged host. Br. J. Cancer 98, 250-255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szauter K. M., Cao T., Boyd C. D., Csiszar K. (2005). Lysyl oxidase in development, aging and pathologies of the skin. Pathol. Biol. 53, 448-456 [DOI] [PubMed] [Google Scholar]
- Tan T. T., Coussens L. M. (2007). Humoral immunity, inflammation and cancer. Curr. Opin. Immunol. 19, 209-216 [DOI] [PubMed] [Google Scholar]
- Trebaul A., Chan E. K., Midwood K. S. (2007). Regulation of fibroblast migration by tenascin-C. Biochem. Soc. Trans. 35, 695-697 [DOI] [PubMed] [Google Scholar]
- Tsang K. Y., Cheung M. C., Chan D., Cheah K. S. (2010). The developmental roles of the extracellular matrix: beyond structure to regulation. Cell Tissue Res. 339, 93-110 [DOI] [PubMed] [Google Scholar]
- Tucker R. P., Chiquet-Ehrismann R. (2009). The regulation of tenascin expression by tissue microenvironments. Biochim. Biophys. Acta 1793, 888-892 [DOI] [PubMed] [Google Scholar]
- Ulijn R. V., Smith A. M. (2008). Designing peptide based nanomaterials. Chem. Soc. Rev. 37, 664-675 [DOI] [PubMed] [Google Scholar]
- Untergasser G., Madersbacher S., Berger P. (2005). Benign prostatic hyperplasia: age-related tissue-remodeling. Exp. Gerontol. 40, 121-128 [DOI] [PubMed] [Google Scholar]
- Vakonakis I., Campbell I. D. (2007). Extracellular matrix: from atomic resolution to ultrastructure. Curr. Opin. Cell Biol. 19, 578-583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velnar T., Bailey T., Smrkolj V. (2009). The wound healing process: an overview of the cellular and molecular mechanisms. J. Int. Med. Res. 37, 1528-1542 [DOI] [PubMed] [Google Scholar]
- Wipff P. J., Rifkin D. B., Meister J. J., Hinz B. (2007). Myofibroblast contraction activates latent TGF-beta1 from the extracellular matrix. J. Cell Biol. 179, 1311-1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise S. G., Weiss A. S. (2009). Tropoelastin. Int. J. Biochem. Cell Biol. 41, 494-497 [DOI] [PubMed] [Google Scholar]
- Xian X., Gopal S., Couchman J. R. (2010). Syndecans as receptors and organizers of the extracellular matrix. Cell Tissue Res. 339, 31-46 [DOI] [PubMed] [Google Scholar]
- Xu J., Lamouille S., Derynck R. (2009). TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 19, 156-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Reagan M. R., Kaplan D. L. (2009). Electrospun silk biomaterial scaffolds for regenerative medicine. Adv. Drug Deliv. Rev. 61, 988-1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisch A. H., Lutolf M. P., Hubbell J. A. (2003). Biopolymeric delivery matrices for angiogenic growth factors. Cardiovasc. Pathol. 12, 295-310 [DOI] [PubMed] [Google Scholar]