Abstract
Objective
To analyze the effects that hands-free communication device (HCD) systems have on healthcare organizations from multiple user perspectives.
Design
This exploratory qualitative study recruited 26 subjects from multiple departments in two research sites located in Portland, Oregon: an academic medical center and a community hospital. Interview and observation data were gathered January through March, 2007.
Measurements
Data were analyzed using a grounded theory approach. Because this study was exploratory, data were coded and patterns identified until overall themes ‘emerged’.
Results
Five themes arose: (1) Communication access—the perception that HCD systems provide fast and efficient communication that supports workflow; (2) Control—social and technical considerations associated with use of an HCD system; (3) Training—processes that should be used to improve use of the HCD system; (4) Organizational change—changes to organizational design and behavior caused by HCD system implementation; and (5) Environment and infrastructure—HCD system use within the context of physical workspaces.
Conclusion
HCD systems improve communication access but users experience challenges integrating the system into workflow. Effective HCD use depends on how well organizations train users, adapt to changes brought about by HCD systems, and integrate HCD systems into physical surroundings.
This paper describes a qualitative investigation into the impact that hands-free communication device (HCD) systems had on two healthcare organizations from the viewpoints of key stakeholder constituencies: staff nurses, nurse managers, and information technology staff.
Clinical environments are dynamic and ‘event driven’ workspaces in which clinicians must effectively communicate to make accurate healthcare-critical decisions.1 Research has shown that clinicians exhibit a high degree of mobility.2 In addition, clinicians consistently prefer synchronous, real-time, communication channels, such as telephone conversations, over asynchronous, delayed communication channels such as email.3 This preference unfortunately results in an interruptive workplace that can lead to “diversion of attention, forgetfulness, and errors”.1
The availability of traditional information and communication technologies (ICTs) as well as the introduction and integration of newer ICTs add to the challenges presented by dynamic and interruptive workplaces. The introduction of new ICTs adds yet another layer in what Coiera and Alvarez describe as a “multilayered approach to communication” in hospitals4 and increases opportunity for medical errors (table 1).5
Table 1.
Advantages and disadvantages of common clinical communication technologies
| Device | Advantages | Disadvantages |
| Pager15 16 17 |
|
|
| Cell phone6 18 |
|
|
| Telephone19 |
|
|
| Overhead page20 |
|
|
| Planning board1 21 |
|
|
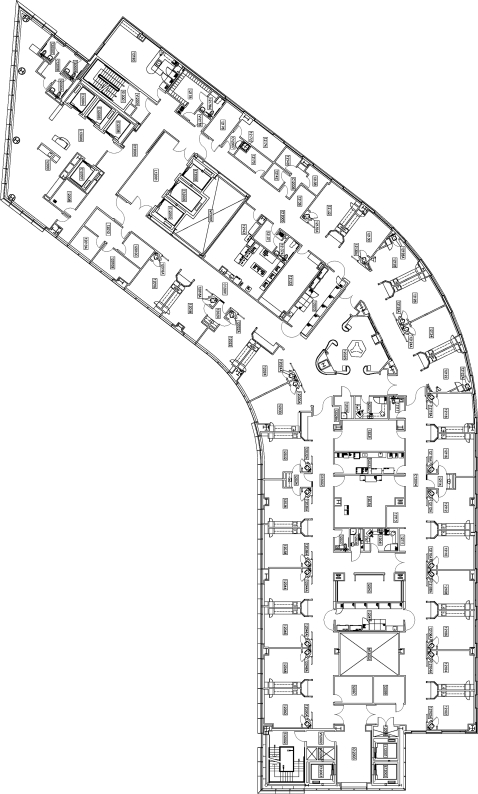
The HCD systems are relatively new ICTs that are being introduced into clinical environments. HCD systems have three primary attributes: (1) HCD systems provide wireless verbal communication among healthcare staff by using Voice-over Internet Protocol over a Wireless Local Area Network; (2) Users communicate through lightweight devices that are meant to be worn around the neck or clipped to a lapel thereby allowing the user to freely use his or her hands while communicating, and (3) HCD systems enable users to make outgoing calls, pick up incoming calls, or dictate other call-handling instructions by using specific verbal commands. For example, the verbal command, “Call Jane Smith,” would instruct a sender's HCD to make a call to Jane Smith's HCD. Jane Smith's HCD would then notify her of an incoming call to which she would verbally say “yes” to answering the call or “no” so that the call may route to her voicemail. The HCD systems are currently manufactured by only one company, Vocera Communications, Inc., and therefore users often reference the brand name when discussing HCD systems (figure 1).
Figure 1.
Researcher wearing a hands-free communication device.
The utility of HCD systems, particularly for healthcare settings,3 6 7 8 is that they support both real-time verbal communications as well as asynchronous voice communications, enable conversation-based information exchange, and allow staff to contact one another by speaking a person's name, nickname, or organizational role. Users can attribute nicknames to other users in order to account for name variations, to provide alternate names for those whose names are difficult to pronounce, or to provide users with the means to personalize friends and colleagues at work. The HCD system can automatically transfer urgent calls among clinicians until a clinician responds; this ensures that an urgent message is ultimately received. The organization or individual users may determine when and how calling options are configured. Few studies have been published about the impact of HCD systems. St Jacques et al9 used a time study and survey to compare an HCD system to a pager system within an anesthesia unit. Over 4 months subjects wore both pagers and HCDs. Researchers sent subjects no more than two pages or HCD calls each day and subject response times were recorded. Those with HCD technology had response rates almost four times faster than those with pagers (HCD system: 30 s average, n=43 vs pager system: 118 s average, n=30). Surveys were used to collect ‘system performance’ and ‘user preference data’ for the HCD system and the pager system. Users preferred the HCD system (71%) over the pager system. However, 97% of respondents rated pagers as the more reliable of the two technologies. Reliability issues stemmed from concern that HCDs could broadcast private patient data into public spaces and that environmental noise accidentally activated the HCD. The authors surmised that additional training could adequately address clinicians’ concerns with the HCD system.
Breslin et al10 compared nurse communications in one unit that used overhead pages, phones, and pager systems to a similar unit that used the same communication technologies plus an HCD system. Through a process of shadowing nurses and reviewing call logs, researchers found that responses to HCD calls were significantly faster than responses to other technologies. Furthermore, overhead paging was reduced by 94% on the unit that possessed an HCD system. In a follow-up survey, nurses in the test unit ranked the HCD system as their most preferred means for communication; whereas nurses in the control unit reported overhead pages as the most preferred. The authors concluded that HCDs improved workflow, saved time, and reduced environmental noise.
Kurozovich et al11 conducted a mixed-method study of nurses in intensive care units (ICUs). The researchers found that HCD systems integrated with nurse call systems significantly reduced the average nurse response time to patient calls by 51% after controlling for unit differences and types of requests (127 s–62 s, p<0.001). In addition, the researchers observed that nurses changed the way they organized meetings after the HCD system was installed. The authors concluded that HCD systems quantitatively and qualitatively reduced ‘load’ on the study's subjects.
These studies provide valuable insights into how HCD systems impact clinical communication, particularly how HCD systems reduce the duration between user calls and responses. However, we wanted to gain a deeper understanding of the impact this new ICT had on clinical communication in particular, and organizational communication in general. We believe that a qualitative grounded theory approach is most appropriate for gaining a deeper understanding of a technology's impact on users and organizations. In addition, a grounded approach has not been used before for HCD system evaluation, so it can further validate previous findings, reveal new findings, or both.
We therefore set out to understand how the introduction and use of HCD systems affected communication in healthcare organizations. The research questions were: (1) how did HCD systems affect nurse, nurse manager, and IT staff communication? (2) How did HCD systems affect communication in healthcare organizations? (3) What were any unintended consequences associated with the implementation and use of HCD systems?
Methods
We selected grounded theory qualitative methods for this study because they can be especially useful for exploring social, technical, and organizational changes.12 HCD system implementations can vary across study sites by unit size, staff size, floor plans, and the types of units; and qualitative methods can account for variability in implementations, subjects, and use across these sites. Furthermore, the iterative nature of grounded theory qualitative methodology can provide opportunities for further investigation into issues that require follow-up and deeper understanding.
The grounded theory method has been used extensively in biomedical informatics to discover technology's impact in such areas as care provider order entry,13 14 wireless pagers,15 16 and clinical decision support.22 23 24 These studies have given valuable insight into users’ perceptions of how a particular technology fits into workflow and meets organizational objectives. Results of these studies have explained why some informatics applications and systems are more readily accepted within each of their particular settings.
Grounded theory is a qualitative approach in which the researcher iteratively reviews interview and observation data, applies labels or ‘codes’ to data that are considered important, and blends codes until overall themes ‘emerge’ from that data.25 The method is well suited to handle ‘maximum variability’ within a sample group, aiming to understand the range of perspectives and experiences relating to a topic of inquiry. Interviews and observations occurred from January through March 2007.
Site selection and recruitment
Two hospital organizations were purposively selected for this study. The hospitals differed in that one was an academic medical center and the other was a community hospital. This provided an opportunity to compare themes associated with HCD systems across hospital types.
Linstone's26 model of multiple perspectives guided this study's purposive subject sampling. Linstone argues that the evaluation of a technology should take into account users from multiple perspectives: personal, organizational, and technical. After consulting the literature and clinical informatics experts, we selected three target groups to represent each of the different perspectives: (1) staff nurses represented the personal perspective because they are the primary users of HCDs, (2) nurse managers were selected because they are responsible for insuring the devices are used according to organizational values and goals, and (3) IT staff were included because they are responsible for the technical function of the HCD systems.
Subjects were recruited at each study site by using a ‘snowball’ methodology. This method relied upon executive sponsors, organizational liaisons, and the subjects themselves to identify potential subject participants. With their guidance the first author approached potential new subjects via email or in person to ask about their willingness to participate. Table 2 outlines the roles and unit types of the 26 total subjects we recruited from the two hospitals.
Table 2.
Roles of IT staff and units of nurse managers and staff nurses
| IT staff roles | Nurse manager units | Staff nurse units |
| Network engineer | OR | Clinical neurosciences |
| CIO | Clinical neurosciences | Cardiac telemetry |
| Senior manager of infrastructure engineering | Cardiac/medical ICU (interim manager) | Cardiac telemetry |
| Telecom systems engineer | Cardiac/vascular ICU | OR |
| Telecom systems engineer | Sterile processing | OR |
| Computer technician | Neurosurgery and ENT | Bedside/charge in cardiac/medical ICU |
| Director of technology | Cardio-thoracic and vascular surgery | Orthopedics and neurology |
| CMIO | Orthopedics and neurology | Orthopedics and neurology |
| Senior project leader | Orthopedic coordinator for surgery |
CIO, Chief Information Officer; CMIO, Chief Medical Information Officer; ENT, ear nose and throat; ICU, intensive care unit; OR, operating room.
Interviews and observations
In the winter of 2007, the first author gathered data using audio recorded, semi-structured interviews (box 1). Twenty-three interviews were conducted face-to-face, and due to scheduling constraints, three were conducted over the telephone. The first author also conducted participant observations of clinicians wearing HCDs in clinical settings. Observations varied between 1 and 2 hours at a time, for a total of 9 hours. Field notes during observations were taken with pen and paper. To ensure greater trustworthiness, summary results were sent to each study participant who was then given the opportunity to provide feedback and suggest revisions. All comments that were received validated the results. The study was approved by institutional review boards at both study sites.
Box 1. Interview guide.
-
History
How long have you been using Vocera?
Why do you think Vocera was something the organization wanted to implement?
-
Problem Gap
What was communication like before Vocera?
-
Vocera's impact
What effect has Vocera had upon communication among staff?
What effects has Vocera had upon communication in the organization?
-
Unintended consequences
What about Vocera has surprised you?
Data analysis
Audio recorded interviews and observational field notes were transcribed and imported into NVivo 7.0, a qualitative data management tool. The first author coded interviews and field notes and a second researcher reviewed the coding to test the validity of the coding scheme. Codes were then organized into larger groupings of themes and subthemes using an iterative card sorting technique.27 The card sorting technique resulted in five overarching themes.
Results
Analysis of the interview transcripts and observational field notes led to five themes pertaining to the effects of HCD systems:
Communication access—subjects felt the HCD system provided fast and efficient communication that supported workflow;
Control—subjects described social barriers associated with HCD technology as well as technical difficulties associated with the HCD system itself;
Training—subjects expressed issues related to training that helped, or could help, them overcome challenges to control;
Organizational change—subjects described how HCDs impacted patient care and organizational strategies;
Environment and infrastructure—subjects described challenges of using HCD technology within the context of their [facilities'] physical layouts and workspaces.
We only summarize data for the themes communication access and control, as a detailed analysis has been published elsewhere.28 Results for the remaining three themes: training, organizational change, and environment and infrastructure have not before been published and we therefore cover them in greater detail for this article. Each theme and subtheme is described using the following conventions: theme names are in italics; quotes have been selected because they are representative; square brackets are placed around words added by the authors for clarity; and ellipses are used to indicate deleted words.
Theme 1: Communication access
The term communication access describes how users perceived the HCD systems provided fast and efficient communication that supported workflow. An IT subject described the lack of communication access as, “[the] whole nightmare of trying to call… [and]… then you can't find the other person”. A nurse manager described lack of communication access on workflow as “a lot of hurry up and wait”. Communication access includes eight subthemes: (1) Finding a phone, (2) Immediacy, (3) Brevity, (4) Directness, (5) Streamlining, (6) Locating or finding, (7) Obtaining help, and (8) Dependence.
Subjects explained that the immediacy and directness of HCD system communications provided greater communication access to and among staff than when subjects solely relied on telephone systems. Subjects perceived that an increase in communication access allowed them to locate or find one another more quickly and that telephone calls did not interrupt workflow as often as before the HCD system implementations. As a result, users explained that they had become dependent on HCD communications in performing their work.
Theme 2: Control
‘Control’ is the ability to manage the social and technical properties of HCD communications in order to achieve safe and efficient work. A nurse manager explained, “it does take a little while to realize that you need to control [the HCD]…don't let it control you”. By ‘social control’ we refer to individual users being able to manage the social aspects of the technology which are: (1) frequent interruptions from others, (2) prioritizing conflicting communications, (3) relying upon a common etiquette, and (4) adhering to patient confidentiality requirements. ‘Technical control’ includes the ability to use: (1) the speech recognition features, and (2) ease of use.
Regarding social control, subjects described that although they perceived fewer telephone interruptions they instead had to manage interruptive HCD calls and prioritize their HCD communications. In addition, subjects described challenges to developing agreed upon communication protocols and ‘etiquette’ such as best practices for communicating confidential patient information. Subjects found HCDs generally easy to use but also described challenges to HCD technical functions such as name and command recognition. In sum, the HCD systems challenged the subjects’ abilities to control their communications with one another.
Theme 3: Training
We define training as processes of teaching, advocating, and encouraging user learning to help gain HCD acceptance. Training was noted by many subjects as critically important for effectively integrating the HCD systems into workflow.
One nurse manager found there had been a learning curve for users. “[There's a] huge learning curve [and] a lot of…getting used to the system”. That learning curve extended to IT staff as well. An IT staff member stated, “I think we're still in a learning curve…and we're still in a training curve…I think [the HCD system is] already sparking a lot of conversation”.
Another IT staff member considered HCD training the most important factor for effective communication with the system: “Training. I think that's the biggest thing”. IT subjects often reported the need for user training and many reported that users’ perceptions of the HCD systems changed after training: “[Users] don't want to come to training…[but] after they see the functionality…[a] light bulb goes off…[it's] really neat to see that so quickly”.
Subjects had varying accounts of what was learned and not learned at training. A nurse manager remembered learning “pretty basic” directions for using call functions. A staff nurse thought training should teach people to begin HCD calls with introductory questions to prevent any patient information from being mistakenly revealed, “clarify that the other person can talk to you before you say anything”. A staff nurse felt training could have included more hands on experience. “…instead of just hearing about it they could actually have people calling each other using the [HCD system]”.
Hands-on use of HCDs was reported as an important factor for effective training. Employees at one hospital were given training 3 weeks before the HCD system went live. Those subjects commonly stated the 3-week gap between training and usage was unhelpful and that they desired retraining. “…you should go back and…retrain because there are so many things that [were] missed, because the technology was so new”. A nurse manager noted the effect of the gap between training and use results in staff not using the full functionality of HCDs. “I'm trying to get into my staff's head when they call a physician they can call the physician directly…we need to go back for retraining”. An IT staffer concurred, “[W]hat we've learned is, is you really have to go back and refresh that training”.
Some nurse managers reported having to continually advocate using the HCD system to staff after implementation. A nurse manager explained, “…it's just constant reinforcement…that [nurses] have to use the tool…that's part of [their] job”. Another nurse manager added, “You also kind of feel a little bit like a sales rep…you're trying to sell it and that's been…weird”. An IT worker said she had underestimated the difficulty of gaining HCD acceptance among users: “The level of commitment…at the end user level was a little bit more than I anticipated”. In counterpoint, a staff nurse described difficulty keeping up with HCD updates: “I'm not going to spend my lunch hour reading five different updates…I just delete [the emails]”.
Theme 4: Organizational change
Organizational change describes how the HCD systems affected communication among teams and between departments across the organizations. Concepts related to this theme are: (1) understanding other departments’ work, (2) having to resolve organizational issues of authority and responsibility, and (3) achieving goals of the organization.
IT staff subjects related how working on HCD system implementations enabled them to better understand the nature of clinical work. One IT staff member explained, “[I]t's made me more sympathetic to what [nurses] go through”. Another IT staff member's experiences highlighted the differences in clinical and IT work, “it's expected of us to check email constantly…it's interesting to see other areas where patient care is their number one focus and that [email is] not a priority. A third IT person commented, “you…really see how the nurses interact and how more day-to-day workflow goes…it's sort of an eye opener”.
Nurse managers reported increased communications with IT staff. A nurse manager explained, “I think they [IT] learned from us about workflow and about how we communicate…I learned more about…databases and how to build them and what can interface with what and all those types of things”.
One nurse manager described how the HCD system provided greater access to other departments, “[the HCD system] has allowed me to have quicker communication with other departments”. As did another nurse manager, “[I]f [my coworker]…is over at [another facility] I can [call] her…So that's really nice”.
An IT member described how the “congruence of voice and data” through HCD systems represented a particular challenge for assigning departmental responsibility and authority. He explained, “[The challenge] sort of ‘snuck up’ on us…to whom do [users] call? Is [the HCD] a phone and they call our communications department? Or is [the HCD] an IP device and they call the network group?”.
Some subjects believed that the HCD system would significantly change clinical staffing. An IT subject asked, “…if you're going paperless to an electronic health record and you have the easy [HCD-based] communication…do you need [unit secretaries]?”. A nurse manager foresaw reductions in clinical staff after the HCD system directly connects patients to nurses, “…[unit secretaries are] not going to be in one centralized station and eventually we may not need them”.
Theme 5: Environment and infrastructure
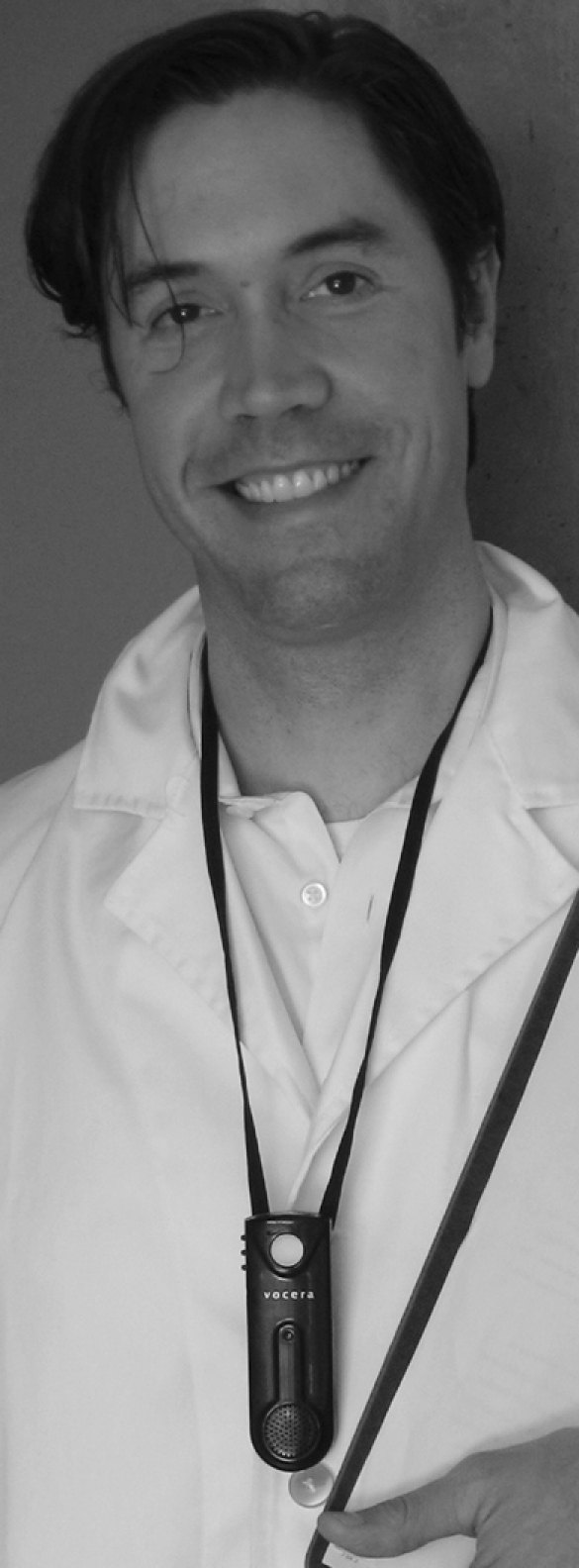
Environment and infrastructure describes issues related to how the building designs and wireless architectures affected HCD-based communications. A considerable factor for users in one hospital was that the floor plan was designed in such a way that staff nurses on one end of a unit could not see nurses at another end of the unit, and there were decentralized nurse's stations (figure 2).
Figure 2.
A hands-free communication device system was cited as a tool that connected nurses whose sight lines were blocked by the hospital unit's curved floor plan.
A nurse manager commented on the impact of the building design on communication, “…[staff are] spread out…they tend to communicate differently”. An IT staff member added, “the units are huge…and so it takes so much time to find someone…[The HCD system] was their way to reduce all that waste of time and improve productivity”. One nurse manager stated, “…I think the staff realized right away that [the HCD system] would help them because…we were much further apart from each other”.
An IT staff member noted that the building was designed to help support wireless communications, “Had there been more walls, more concrete, more interference it would have plagued a wireless infrastructure”.
Considerations of space were of a concern at the second hospital site as well. One staff nurse recalled a situation, “…[nurses] take some patients [to the showers] and try to use [the HCDs]…they'd get that [wireless signal] reflection and it didn't work well”.
Discussion
The themes demonstrate how the HCD systems impact clinical and organizational communication for subjects. We address each of the themes in turn and subsequently use those themes to answer our research questions. We end our discussion with comments about our research design, possibilities for future research, and study limitations.
Communication access
Subjects from both organizations greatly appreciated the degree of communication access that HCD systems afforded and perceived that the HCD systems reduced the duration time between calls and responses. The perceptions of reduced call and response times qualitatively support Breslin et al and St Jacques et al quantitative results.9 10
Greater communication access meant subjects could more readily reach one another for help. Users provided examples when the sound of a person's voice over an HCD conveyed the level of priority that should be attributed to a specific communication. This had an advantage over pager systems because pagers have limited ability to convey urgency thereby resulting in ‘missing context’.15 For HCD users, increased context was beneficial for a number of communication tasks such as obtaining answers to patient-related questions, querying staff members about their current location in the workplace, or even contacting people outside the unit such as vendors.
The HCD system enabled subjects to reach each other by using personal names, nicknames, or roles. Coiera et al have detailed the critical need for ICTs in clinical settings to support mobility and accessibility by name as well as by role.1 7 HCD systems appear to provide that support. In addition, the HCD systems enabled subjects to conduct real-time, short communications that supported clinical workflow and coordination among staff. Communications of these types are similar to Reddy et al's description of ‘organizational questions’ which accounted for a notable proportion of information needs in an emergency department and a surgical ICU.29 30 These aspects of clinician communication and information seeking had been largely unknown to this study's IT staff subjects prior to installation of the HCD systems.
Control
Although subjects from both organizations expressed appreciation for the greater degree of communication access they tempered those feelings with the need to control their availability and accessibility through the HCD system. Subjects found the HCD systems changed the ways in which they communicated and interacted with each other. Most crucially, staff nurses and nurse managers perceived the HCD system did not stop interruptions during the course of clinical work. Rather, the HCD system provided a new channel through which interruptions could occur. Users described having to adapt the new source of interruptions into their workflow. In earlier work we described how subjects tried to ‘balance’ increased communication access with social and technical control.28
Training
The challenges associated with HCD use highlighted needs for additional training as well as new considerations for training. First, clinical subjects desired and IT subjects recognized the need for training and retraining. IT subjects noted that training was critical not only for efficient HCD use but also for increased likelihood of HCD acceptance. Subjects recommended having HCD system training sessions as close to go-live as possible as well as retraining to reinforce effective use and utilization of new HCD system features. Nurse managers appeared to be a constituency who advocated the use of the HCD system. In fact, one subject described feeling like an HCD “company representative”. Any organization that invests in an HCD system may want to consider how nurse managers can be supported as they advocate HCD system use to staff nurses. Finally, HCD system training should account for social aspects of the technology which would include proper and improper use of HCD systems, limiting interruptions, and patient privacy protocols.
Organizational change
The installation of HCD systems brought about changes in departmental relationships that required the organizations to institute new policies and procedures. First, many IT subjects explained greater understanding and appreciation of the challenges to clinical work. With their appreciation they described being more patient and understanding when nurses reported problems with the HCD system or other IT systems. Second, the HCD system implementation caused one organization to revisit IT roles and responsibilities. The HCD system architecture is a voice communication technology that uses wireless networks; as such, the organization realized after implementation that they had to decide whether to treat the HCD system as either a telecom or a computer network entity. That organization ultimately decided that the HCD system should be treated as a computer network.
Environment and infrastructure
The clinical environment and infrastructure showed itself to have an important relationship to the HCD systems. In the case of one organization's hospital, the HCD system supported clinical teams who were distributed across a large physical space. The system provided a degree of connectedness despite nurses having fewer person-to-person interactions at a centralized nursing station. Additionally, that same hospital was designed with open floor spaces and materials that would facilitate wireless signals across clinical spaces. Subjects described having to be cognizant of the physical space around them in case the settings would cut them off from communications with the rest of the group. Showers, for example, were noted as one physical environment where the HCD system would not work and therefore nurses had to be aware of other means for communication in emergencies when they were helping patients to bathe.
This study is unique in its use of a grounded theory approach to understand the effects that HCDs had on communication within organizations, especially among IT staff, nurse managers, and staff nurses. Observations and interviews demonstrated subjects’ acceptance of using HCDs to supplement existing clinical voice communication technologies. For some, HCDs were the preferred communication tool while conducting clinical work.
Research questions
HCD systems changed communication among staff nurses, nurse managers, and IT staff by providing a greater degree of communication access. Greater communication access through the HCD system enabled subjects to feel they could obtain help more readily, locate one another more quickly, and streamline work. This perception was shared by not only staff nurses, and nurse managers, but also IT staff as well. However, greater access to one another through the HCD system also brought about control challenges that impacted group cohesion and clinical practice. Staff nurses, in particular, described how the lack of HCD etiquette hindered their ability to integrate the technology into their work. In addition, staff nurses described instances when HCD calls were interruptive and may have interfered with nurse-patient relationships. Effective and efficient HCD system communication requires users to develop a balance between communication access and control.
Observations and interviews highlighted how much patient care relies on the efficiency and effectiveness of organizational communication among staff nurses, nurse managers, and IT staff.
Organizational communication practices as they relate to training must address the nature of clinical work. Staff nurses and nurse managers are highly mobile workers who heavily rely on personal interactions. Therefore, HCD system training and communications should be conducted in person as much as possible, such as through nurse staff meetings, as opposed to online training and email updates. Furthermore, clinical communication relies heavily on team-based interactions. Organizational training should provide guidance as to how groups communicate through HCD systems. HCD systems brought about organizational change by changing how IT staff and clinicians talked to one another. IT staff altered their perceptions of nurses and clinical work through collaborations and conversations pertaining to the HCD system. Conversely, nurses were made more aware of IT issues pertaining to networks, servers, and databases. Staff nurses, nurse managers, and IT staff described having more of an understanding of one another's roles.
We believe that an unintended consequence revealed by this study was the impact the environment and infrastructure had on the two HCD systems. In one hospital the HCD system was an important tool to connect nurses and nurse managers who were unable to see one another across a large ICU floor. Staff nurses and nurse managers appreciated having greater communication access in such an environment. Staff nurses and nurse managers explained having to be aware of their physical whereabouts on clinic floors in case they were out of HCD range. The HCD systems seemed to cause subjects to be more aware of their physical surroundings and the impact on their workflow.
This study greatly benefited from the inclusion of multiple perspectives. First, having perspectives from people in three different roles lends more rigor and credibility to our study than if we had perspectives from subjects from only one role. Second, multiple perspectives helped us see how perceptions of technology can be differ by organizational role. We believe that the more an organization is able to address challenges identified by people in different roles the better the organization can integrate the technology into work flow and work life.
Future research should explore barriers and facilitators associated with the use of HCD systems. First, one area to study is the rate and impact of interruptions on clinicians, and in addition, the rate and impact of voice recognition failures on clinicians. Interruptions and voice recognition failures were commonly noted as frustrations associated with the HCD system. Second, it would be valuable to gather satisfaction measures from patients whose nurses send and receive HCD calls while in patient rooms. In this study, staff nurses perceived patients as being dissatisfied when HCD calls were made or received in patient rooms. The perception became a barrier to use among staff nurses even though there were no data to describe patient preferences. Third, it would be of interest to understand how best to design a user interface that relies on verbal commands and prompts. Fourth, we believe it would be valuable to use HCD system logs to track clinical communication patterns and their relationships to information sharing, flow, and bottlenecks. Finally, it would be valuable to test our themes of HCD system-based communication using different healthcare professionals in different settings.
There are limitations to this study. First, all the grounded theory coding of transcripts was carried out by one researcher which limited triangulation. Second, observation of training practices occurred at only one of the two research sites. Third, observations were limited to sessions between 1 and 2 hours in length. Finally, the results of this and any qualitative study are not generalizable. Rather, the results are ‘transferrable’31 meaning that before applying any of these findings to other sites readers should consider if the study context is similar to that of their workplace.
Conclusion
HCD systems improve communication access, defined as: the degree to which subjects initiate and receive communications, the flexibility in ability to contact other users, and the perceived reduction in call and response times. Users easily grasped the concept of HCD systems and quickly grew accustomed to using the technology in their work. Acceptance of the technology occurred despite the challenges to social control that subjects described: interruptions, unresolved etiquette, privacy concerns, and conflicting communication channels. HCD system acceptance also occurred despite challenges to technical control: speech recognition inconsistency and the lack of helpful command prompts. Organizations can address some of these challenges by training and retraining users to the appropriateness of certain HCD communications, patient privacy, and group-based instruction in addition to individual-based instruction. The HCD system manufacturer can also address certain limitations that pertain to speech recognition limitations as well as the lack of user command prompts. Organizations should be aware that HCD systems may bring about changes to IT and clinical departmental relationships and challenges to HCD support roles and responsibilities. An important consideration is the manner in which the HCD system fits within the physical surroundings of clinical areas because nurses may require communications in places IT might least expect. HCD systems have the potential to become a fruitful realm for research within the field of biomedical informatics.
Footnotes
Funding: The authors would like to acknowledge funding support from the National Library of Medicine Training Grant 2-T15-LM007088.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Coiera E, Tombs V. Communication behaviours in a hospital setting: an observational study. BMJ 1998;316:673–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Welton JM, Decker M, Adam J, et al. How far do nurses walk? Medsurg Nurs 2006;15:213–16 [PubMed] [Google Scholar]
- 3.Coiera E, Jayasuriya RA, Hardy J, et al. Communication loads on clinical staff in the emergency department. Med J Aust 2002;177:333–5 [DOI] [PubMed] [Google Scholar]
- 4.Alvarez G, Coiera E. Interdisciplinary communication: an uncharted source of medical error? J Crit Care 2006;21:236–42; discussion 242. [DOI] [PubMed] [Google Scholar]
- 5.Alvarez G, Coiera E. Interruptive communication patterns in the intensive care unit ward round. Int J Med Inform 2005;74:791–6 [DOI] [PubMed] [Google Scholar]
- 6.Taylor D, Coakley A, Reardon G, et al. An analysis of inpatient nursing communications needs. Medinfo 2004;11(Part 2):1393–7 [PubMed] [Google Scholar]
- 7.Coiera E. When conversation is better than computation. J Am Med Inform Assoc 2000;7:277–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coiera E. Clinical communication: a new informatics paradigm. Proc AMIA Annu Fall Symp 1996:17–21 [PMC free article] [PubMed] [Google Scholar]
- 9.Jacques PS, France DJ, Pilla M, et al. Evaluation of a hands-free wireless communication device in the perioperative environment. Telemed J E Health 2006;12:42–9 [DOI] [PubMed] [Google Scholar]
- 10.Breslin S, Greskovich W, Turisco F. Wireless technology improves nursing workflow and communications. Comput Inform Nurs 2004;22:275–81 [DOI] [PubMed] [Google Scholar]
- 11.Kuruzovich J, Angst CM, Faraj S, et al. Wireless communication role in patient response time: a study of vocera integration with a nurse call system. Comput Inform Nurs 2008;26:159–66 [DOI] [PubMed] [Google Scholar]
- 12.Friedman CP, Wyatt J. Evaluation methods in medical informatics. New York: Springer, 2006 [Google Scholar]
- 13.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc 2004;11:104–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ash J, Gorman P, Lavelle M, et al. Multiple perspectives on physician order entry. Proc AMIA Symp 2000:27–31 [PMC free article] [PubMed] [Google Scholar]
- 15.Reddy MC, Pratt W, McDonald DW, et al. Challenges to physicians’ use of a wireless alert pager. AMIA Annu Symp Proc 2003:544–8 [PMC free article] [PubMed] [Google Scholar]
- 16.Reddy MC, McDonald DW, Pratt W, et al. Technology, work, and information flows: lessons from the implementation of a wireless alert pager system. J Biomed Inform 2005;38:229–38 [DOI] [PubMed] [Google Scholar]
- 17.Mates J, Branstetter BF, Morgan MB, et al. ‘Wet Reads’ in the age of PACS: technical and workflow considerations for a preliminary report system. J Digit Imaging 2007;20:296–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sneiderman CA, Ackerman MJ. Cellular radio telecommunication for health care: benefits and risks. J Am Med Inform Assoc 2004;11:479–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fowkes W, Christenson D, McKay D. Analysis of the use of the telephone in the management of patients in skilled nursing facilities. J Am Geriatr Soc 1997;45:67–70 [DOI] [PubMed] [Google Scholar]
- 20.Olson LL. Commentary on introducing a two-way wireless communication system. [original article by Minnick A et al appears in Nurs Manage 1994;25(7):42–7]. AONE's Leadership Prospectives 1995;3:17. [PubMed] [Google Scholar]
- 21.Bardram JE. I love the system—I just don't use it! Proceedings of the international ACM SIGGROUP conference on Supporting group work: the integration challenge. Phoenix, Arizona, USA: ACM Press, 1997 [Google Scholar]
- 22.Kaplan B. Evaluating informatics applications—some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inform 2001;64:39–56 [DOI] [PubMed] [Google Scholar]
- 23.Kaufman D, Roberts WD, Merrill J, et al. Applying an evaluation framework for health information system design, development, and implementation. Nurs Res 2006;55(Suppl 2):S37–42 [DOI] [PubMed] [Google Scholar]
- 24.Ash J, Sittig DF, Campbell EM, et al. Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc 2007. October 11:26–30 [PMC free article] [PubMed] [Google Scholar]
- 25.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. New York: Aldine De Gruyter, 1967 [Google Scholar]
- 26.Linstone HA. Decision making for technology executives: using multiple perspectives to improve performance. Boston, MA: Artech House, 1999 [Google Scholar]
- 27.Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park, CA: SAGE Publications, Inc., 1984 [Google Scholar]
- 28.Richardson JE, Ash J. The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc 2008:621–5 [PMC free article] [PubMed] [Google Scholar]
- 29.Reddy M, Spence PR. Finding answers: information needs of a multidisciplinary patient care team in an emergency department. AMIA Annu Symp Proc 2006:649–53 [PMC free article] [PubMed] [Google Scholar]
- 30.Reddy MC, Pratt W, Dourish P, et al. Asking questions: information needs in a surgical intensive care unit. Proc AMIA Symp 2002:647–51 [PMC free article] [PubMed] [Google Scholar]
- 31.Patton MQ. Qualitative research and evaluation methods. 3rd edn Thosand Oaks, CA: Sage Publications, 2001 [Google Scholar]