Abstract
Objective
This report provides updated estimates on use of electronic medical records (EMRs) in US home health and hospice (HHH) agencies, describes utilization of EMR functionalities, and presents novel data on telemedicine and point of care documentation (PoCD) in this setting.
Design
Nationally representative, cross-sectional survey of US HHH agencies conducted in 2007.
Measurements
Data on agency characteristics, current use of EMR systems as well as use of telemedicine and PoCD were collected.
Results
In 2007, 43% of US HHH agencies reported use of an EMR system. Patient demographics (40%) and clinical notes (34%) were the most commonly used EMR functions among US HHH agencies. Only 20% of agencies with EMR systems had health information sharing functionality and about half of them used it. Telemedicine was used by 21% of all HHH agencies, with most (87%) of these offering home health services. Among home health agencies using telemedicine, greater than 90% used telephone monitoring and about two-thirds used non-video monitoring. Nearly 29% of HHH agencies reported using electronic PoCD systems, most often for Outcome and Assessment Information Set (OASIS) data capture (79%). Relative to for-profit HHH agencies, non-profit agencies used considerably more EMR (70% vs 28%, p<0.001) and PoCD (63% vs 9%, p<0.001).
Conclusions
Between 2000 and 2007, there was a 33% increase in use of EMR among HHH agencies in the US. In 2007, use of EMR and PoCD technologies in non-profit agencies was significantly higher than for-profit ones. Finally, HHH agencies generally tended to use available EMR functionalities, including health information sharing.
Keywords: Health information technology, electronic medical records, telemedicine, telehealth, point of care documentation, home health, hospice care, national survey, epidemiology
Introduction
Home and community-based long-term care and support services, including home health and hospice (HHH) care, are growing as cost-effective alternatives to institutionalization. Key advantages of these services include choice, added satisfaction, and improved quality of life.1 2 There is increased demand for these services as both seniors and their caregivers seek community based services to remain independent in the community and to avoid premature institutionalization. The use of health information technology (HIT), including electronic medical records (EMR), telemedicine and telehealth, as well as point of care documentation (PoCD), are increasingly viewed as essential tools for improving both the efficiency of service delivery and healthcare quality.3 The efficiencies offered by HIT are particularly evident in the home setting as they have the potential to reduce travel time, improve accuracy and timeliness of care documentation, and to facilitate preventive interventions, especially when telemedicine capabilities are used. Indeed, there is evidence to suggest that 75% of older people are willing to use telehealth and telemedicine applications that would help diagnose and/or monitor their health conditions in the home.4 Willingness to accept these technologies was based on the value older people place on receiving support in their own homes in a manner that prolongs independence.
The first nationally representative data describing use of electronic records in this service setting were collected in the 2000 National Home and Hospice Care Survey (NHHCS).5 The 2000 NHHCS asked the following questions: ‘Are the medical records of this agency computerized?’ and among those with a negative response, ‘Does this agency plan to computerize its medical records within the next year?’ Results from that survey showed that 32.3% of US HHH agencies reported use of computerized medical records (CMR) in 2000, and among non-users, 22% reported plans to adopt CMR within the next year. The survey highlighted differential CMR use across agency type and by several agency characteristics. More than 40% of mixed agencies—those providing both home health and hospice services—reported using CMR, while only 32% and 18% of agencies providing exclusively home health and hospice services, respectively, reported CMR use. Agencies with larger patient caseloads and those providing high-technology services, such as intravenous treatment, reported more CMR use. Data from the 2000 NHHCS provide a meaningful benchmark against which progress towards adoption of EMR can be evaluated in the HHH settings. However, the 2000 survey did not collect information on specific functionalities of EMR systems, electronic systems for management, education, telemedicine, or PoCD.
A recent survey6 conducted by a consulting firm provides additional insight into more recent trends in the home healthi setting. More than 58% of agencies surveyed in that report had EMR in place—a figure that is considerably higher than the 32.1% of home care agencies reporting CMR use in the 2000 NCHS report.5 The former report indicated that 69.3% of non-profit agencies that were surveyed had EMR in place—a figure that is considerably higher than the corresponding figure of 31.7% reported in the 2000 NCHS report for all sampled agencies. However, it should be noted that although the data generated by the consulting firm's report were based on a relatively large sample (n=976), both the generalizability of the sampling approach and the sampling frame are unclear. Nonetheless, 61% of agencies surveyed in that report had a point of service system in place and 17.1% reported use of telehealth or remote patient monitoring.
This report addresses important gaps in knowledge of current HIT use in the HHH settings by providing the most recent national estimates of EMR use as well as the first nationally representative data on use of several key technologies in this setting, including telemedicine and PoCD.
Methods
Study design and data collection
The 2007 NHHCS provides nationally representative data on HHH agencies, their staff, services, and patients.7 The NHHCS used a stratified two-stage probability sample design. The first stage, carried out by the Centers for Disease Control and Prevention's National Center for Health Statistics (NCHS), was the selection of HHH agencies from the sample frame of over 15 000 agencies, representing the universe of agencies providing HHH services in the United States. The sampling frame was constructed using three sources: (1) The Centers for Medicare & Medicaid Services Provider of Services file of home health agencies and hospices, (2) State licensing lists of home health agencies compiled by a private organization, and (3) The National Hospice and Palliative Care Organization file of hospices. The combined files were matched and identified duplicates were removed resulting in a sampling frame of 15 488 agencies. A sample of 1545 agencies was selected from this sampling frame. Of the 1545 agencies in the sample, 1461 (95%) met criteria for inclusion in the survey. The 84 out-of-scope agencies were ineligible for one or more of the following reasons: did not meet the definition used in the survey, had gone out of business, was a duplicate of another sampled agency, or had merged with other sampled agencies. Of in-scope agencies, 1036 agreed to participate. The NHHCS was administered in sampled HHH agencies between August 2007 and February 2008.8
Ascertainment of information technology use
Technology use in HHH agencies was collected in the Staffing Component of the 2007 NHHCS.9 10 This component involved collection of data via a self-administered questionnaire that was filled out by the agency director.
Electronic medical records
An initial question on EMR was phrased, ‘Does this agency currently have an electronic medical records system? This is a computerized version of the patient's medical information used in the management of the patient's healthcare. Exclude electronic records used only for billing purposes and required documentation such as OASIS files.’ If there was an affirmative response to this question, respondents were asked, ‘With this agency's current Electronic Medical Records system, please indicate for each component listed below, whether it is used, available but not used, or not available’ (table 1).
Table 1.
Summary of technology-related questions asked of home health and hospice care agency directors in the 2007 National Home and Hospice Care Survey
| Technology category | Notes |
| Electronic medical records (EMR) system | |
| Computerized physicians order entry (CPOE): prescriptions, labs, tests, etc | Items ascertained only from agencies that reported current use of EMR. Response options included ‘used’, ‘available/not used’ and ‘not available’ |
| Test results (chest x-rays, labs, etc) | |
| Patient demographics | |
| Electronic reminders for tests (labs, imaging, etc) | |
| Clinical decision support system (CDSS) contraindications, allergies, guidelines, etc | |
| Clinical notes | |
| Public health reporting | |
| Sharing medical records electronically with other agencies | |
| Electronic management systems | |
| Billing system | Items ascertained for all surveyed agencies. Response options included ‘no’ and ‘yes’ |
| Inventory control (ie, bar coding) | |
| Human resources management (personnel records) | |
| Staff management (eg, staffing scheduling, etc) | |
| Accounting | |
| Education systems | |
| Satellite broadcast capability (in serve, training) | Items ascertained for all surveyed agencies. Response options included ‘no’ and ‘yes’ |
| Staff internet access | |
| Patient internet access (website with patient educational materials) | |
| Telemedicine capabilities | |
| Routine telephone monitoring of patients' health, involving conversation with nurse or other healthcare provider/monitor | Items ascertained only from agencies that reported any use of telemedicine capabilities. Response options included ‘no’ and ‘yes’ |
| Email access to health professionals for patients/caregivers | |
| Video consults with healthcare professionals | |
| Routine video monitoring of patients' health involving conversation with nurse or other healthcare provider/monitor | |
| Routine non-video monitoring of patients' health without conversation (eg, regular transmission of vital signs) | |
| Other telemedicine capability | |
| Point of care documentation (PoCD) | |
| Computerized physicians order entry (prescriptions/pharmacy, labs, tests) | Items ascertained only from agencies that reported use of any system for electronic PoCD. Response options included ‘no’ and ‘yes’ |
| Test results | |
| Electronic reminders for tests | |
| Clinical Decision Support System guidelines or reference system | |
| Email communication with agency staff/other staff | |
| Scheduling appointments/visits | |
| OASIS | |
OASIS, Outcome and Assessment Information Set.
Electronic management systems
Respondents were asked, ‘For each item below, please indicate whether or not this agency uses any of the following Management Systems electronically’ (table 1).
Electronic education systems
Respondents were asked, ‘For each item below, please indicate whether or not this agency uses any of the following education systems’ (table 1).
Telemedicine
Respondents were asked, ‘Does this agency use any telemedicine capabilities? Telemedicine is the use of electronic communication and information technologies to provide or support clinical care at a distance.’ If there was an affirmative response to this question, respondents were asked, ‘For each item below, please indicate whether or not this agency uses any of the following telemedicine capabilities’ (table 1). A final question asked what percent of the agency's current patients were using telemedicine.
Electronic point of care documentation
Respondents were asked, ‘Does this agency's staff use any system for electronic point of care documentation?’ This included personal digital assistants, notebook PCs, or other portable handheld devices. If there was an affirmative response to this question, respondents were asked follow-up questions about PoCD system use by direct care and administrative staff as well as questions about specific PoCD functions (table 1).
Agency characteristics
The 2007 NHHCS contained information on ownership status (for-profit vs all others, including non-profit and government). The terms for-profit (FP) and not-for-profit (NFP) are used to describe this variable. Variables describing whether the facility was a member of a chain (yes/no), agency type (home health only; hospice only; mixed), and the current number of HHH patients were also ascertained. The median number of current patients was identified separately for home health (median 73) and hospice (median 35) agencies. Analyses focusing on patient load used a dichotomous variable representing agencies with caseloads that were at or above the median compared to those below the median.
Statistical analysis
Analyses were conducted with the PROC SURVEY procedures in SAS, which take into account the strata, cluster, and weight variables that define the complex sampling approach used in the NHHCS. In addition, the finite population correction was used per NCHS recommendations for the NHHCS staffing data file. Therefore, weighted proportions and cross-sectional associations of interest were generated in a way that renders results generalizeable to the sampling frame of all US HHH agencies in 2007. The NCHS guidelines were used to determine if estimates would be presented in this report. If the estimate is based on fewer than 30 sample cases then the value of the estimate is not reported. If the estimate is based on a sample of 30–59 cases, or on 60 or more cases and the relative SE is 30% or more, then the estimate is reported but should not be assumed reliable. This is indicated with an asterisk (*). If the estimate is based on 60 or more sample cases and the relative SE is less than 30% then the estimate is reported and is considered reliable.8
Results
Table 2 summarizes selected characteristics of US HHH agencies in 2007. Nearly 75% of HHH agencies provided only home health services, 15.3% only hospice services and about 10% provided both services. About 30% of agencies were part of a chain and nearly two-thirds were FP.
Table 2.
Selected characteristics of home health and hospice care agencies, United States, 2007
| Total | ||
| % | Weighted N |
|
| Total* | 100.0 | 14469 |
| Agency type | ||
| Home health only | 74.8 | 10816 |
| Hospice only | 15.3 | 2218 |
| Mixed | 9.9 | 1435 |
| Member of chain | ||
| Yes | 30.0 | 4343 |
| No | 70.0 | 10126 |
| Number of current patients† | ||
| Home health (median=73) | ||
| Hospice (median=35) | ||
| Ownership | ||
| For profit | 65.0 | 9406 |
| Non-profit | 35.0 | 5063 |
Data are weighted using SAS SURVEYFREQ. Some categories may not add to 100.0 due to rounding.
Estimates represent patients from both sole-service and mixed agencies.
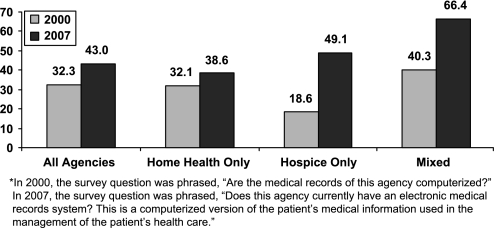
In 2007, 43% of HHH agencies reported current use of EMR. Of non-users, nearly 31% reported that they had plans to obtain an EMR system within the next year. There were marked differences in EMR use by agency type and these differences did not uniformly reflect previous patterns. Figure 1 shows EMR use overall and by agency type for both 2000 and 2007. During the 7-year period between 2000 and 2007, the approximate proportional increase in use of EMR for all agencies, home health only, hospice only, and mixed agencies were, 33.1%, 20.2%, 164%, and 64.8%, respectively.
Figure 1.
Use of electronic medical records systems* in home health and hospice care agencies, United States, 2000 and 2007.
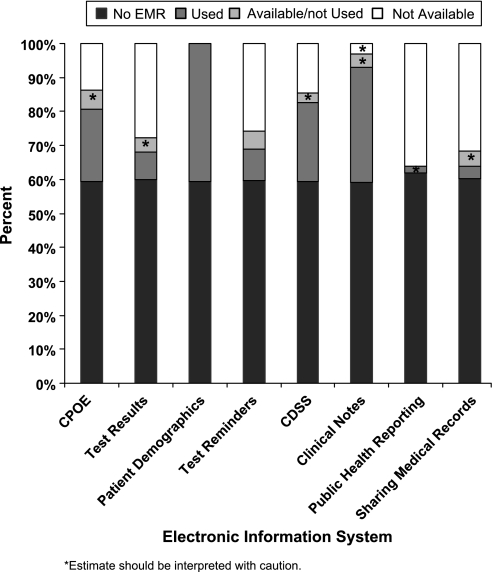
In total, 40% of all agencies reported current use of EMR for patient demographics, nearly 34% used systems for clinical notes, and 23.2% and 21.3% used systems for computerized decision support systems (CDSSs) and computerized physician order entry (CPOE), respectively (figure 2). Key functions, including test results, test reminders, public health reporting, and sharing of medical records were not available in most EMR systems that were in use at the time of the survey. It is worth noting that for some functions, EMR system capacity was available but not used.
Figure 2.
Use and functionality of electronic medical records systems in home health and hospice care agencies, United States, 2007.
Nearly all agencies with EMR systems used them for recording demographic information and about 50% used them for CPOE. Use of EMR systems for public health reporting and for sharing of medical records was sufficiently limited to preclude reporting of reliable estimates in most analyses. Nearly 95% of HHH agencies reported using an electronic billing system and 83% used electronic systems for accounting. Inventory control was managed infrequently by electronic systems (15.2%). In total, 36% of HHH agencies reported using satellite broadcast capabilities, more than 80% reported providing internet access to staff, and 26% reported having a website with patient education materials (data not shown).
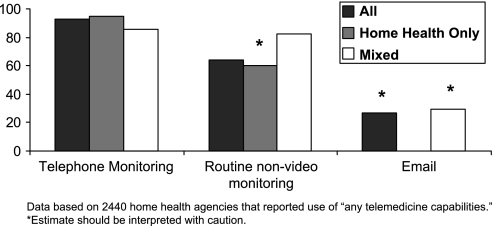
Approximately 20.6% of HHH agencies reported current use of telemedicine and, of these, the overwhelming majority (87%) provided home health services. Less than 13% of agencies providing only hospice services used telemedicine. More than 90% of agencies that provided home health services and that were using telemedicine engaged in routine telephone monitoring, about two-thirds used routine non-video monitoring, and about one-quarter provided email access to health professionals (figure 3). Many telemedicine functions were sufficiently infrequent to prevent reporting of stable estimates of their use.
Figure 3.
Current telemedicine capabilities among home health agencies using telemedicine*, United States, 2007.
Of HHH agencies reporting use of telemedicine, approximately 38% reported that less than 5% of current patients were using telemedicine, with about equal proportions (30.7%) of agencies reporting that 5–20% and ≥20% of current patients were using telemedicine (data not shown).
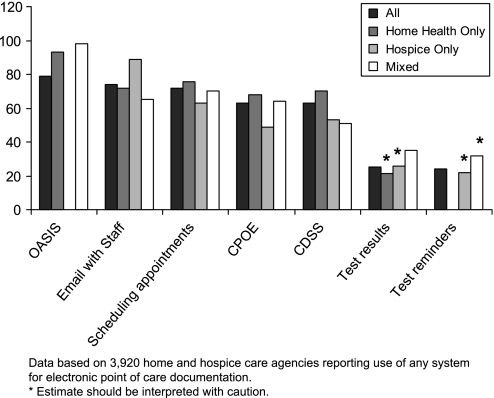
Nearly 29% of HHH agencies reported using a system for electronic PoCD. Of agencies reporting PoCD use, 66.8% and 30.4% reported that ‘some’ and ‘all’ direct care staff used these systems, respectively, and 35.1% and 49.1% of respondents reported that ‘some’ and ‘all’ of administrative staff used them, respectively. Among HHH agencies using electronic PoCD, OASIS, email communication with staff, and scheduling appointments were the most common functions for which these systems were used (figure 4). It is worth noting that among agencies using PoCD, 93.3% and 98.2% of home health only and mixed agencies, respectively, used this technology for OASIS data capture.
Figure 4.
Point of care documentation, by function and agency type, among home health and hospice agencies using these systems, United States, 2007.
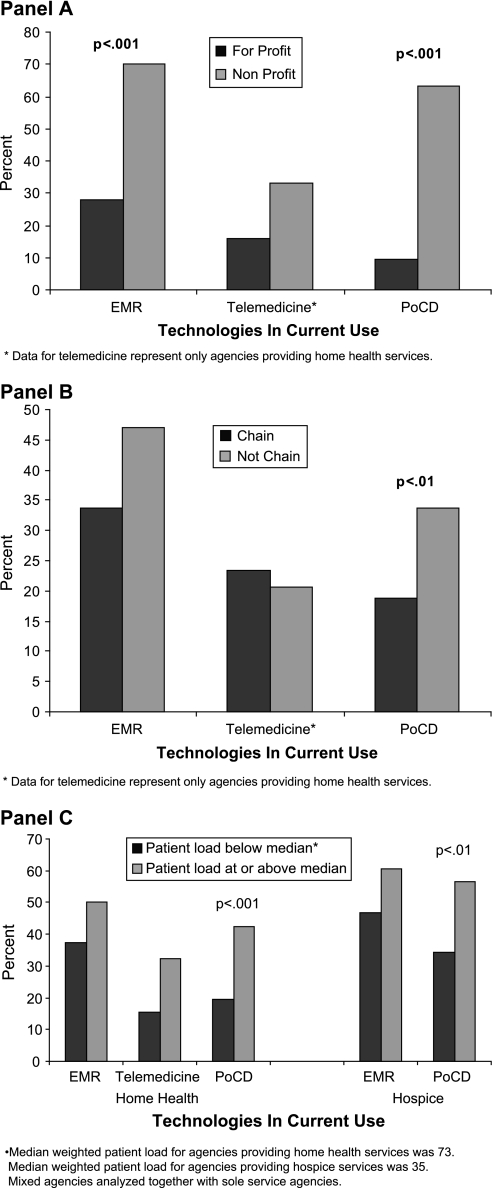
Relative to FP HHH agencies, NP agencies used more EMR (70.1% vs 27.9%, p<0.001) and PoCD (63.1% vs 9.4%, p<0.001), and compared to agencies that were part of a chain, stand-alone agencies used more PoCD (33.7% vs 18.7%, p<0.05). Finally, HHH care agencies with patient case loads at or above the median used more PoCD (figure 5, panels A–C).
Figure 5.
Relationship between selected agency characteristics and current use of technology among home health and hospice care agencies, United States, 2007.
Discussion
Significance
Over the period 2000 to 2007, adoption of EMRs by HHH providers increased from 32.3% to 43.0%; thereby, increasing the potential of these organizations to improve data capture and information sharing. The rate of adoption during this period was higher in hospice only agencies than in home health only agencies but agencies providing both services continue to have the highest overall EMR utilization rate.
This report provides the first national estimates of specific functionalities of EMR in the HHH setting. Functionality for sharing of medical information was limited among HHH agencies that had EMR systems in place—only 20% of HHH agencies with EMR reported having the functionality to share this information with other agencies. Of these, about half (10% of HHH agencies with EMR) reported using this capacity to share health information with other agencies. These data raise several important points. First, that widespread non-use of electronic health information exchange can be explained, at least in part, by the lack of this function in the EMR system that the agency uses; second, assuming that health information sharing capacity is available, about half of HHH agencies have chosen to use it. The latter point implies that at least a small proportion of HHH agencies with EMR systems that have information sharing capacity have identified other agencies or organizations with which to share this information, because health information exchange requires interoperability between the EMR systems of at least two organizations. Given the complexity of health information exchange and the lack of recognition of interoperability standards, it could be argued that 50% use on the part of agencies with records sharing capacity is a considerable achievement for the HHH sector in the current HIT environment.
While interoperability can be achieved through system integration, something that requires the collaboration of proprietary HIT system vendors, building interoperability standards into HIT systems is essential for broader use of record sharing and health information exchange. The availability and use of record sharing functionality in HHH EMR systems are expected to increase over the next few years as a result of the provisions put forth in the American Recovery and Reinvestment Act (ARRA),11 which placed increased emphasis on health information exchange among healthcare providers and set the stage to recognize national standards for interoperability of electronic health records (EHR) as well as the certification of EHR for interoperability.
Increased record sharing functionality would be significant if long-term and post-acute care settings are included in national ARRA-funded initiatives to create state-level health information exchange organizations. Moreover, increased record sharing would likely have a greater impact if HIT adoption incentives were offered to long-term and post-acute care providers—such as HHH agencies—in the future. It is for this reason that ARRA mandated that the Department of Health and Human Services conduct a study to determine if HIT adoption incentive payments should be offered to providers other than physicians and hospitals who are currently slotted for receipt of such incentives through ARRA.
Our analyses indicated a clear preference for telehealth on the part of agencies providing home health services—only 13% of agencies providing only hospice services used telehealth. This observation is somewhat intuitive given key differences in the nature of service provision in these two settings. Home health providers often work over long distances and their patients are not in a central location, as is often the case in the hospice setting. Interestingly, we observed that 26% of home health agencies using telemedicine used email to communicate with patients. This observation involves an underlying assumption related to access on the part of the patient to the internet, and willingness on the part of the agency to access and use the internet for patient care and communications purposes. It is likely that email use as a care tool will increase over time due to increased computer literacy among future cohorts of adults, and increased penetration of the internet and technology in general.
In 2007, 29% of US HHH agencies were using some kind of PoCD. Of agencies using PoCD, this technology was most often used for OASIS data capture. This was not a surprising observation given that electronic reporting of OASIS data is mandated by the Center for Medicare Medicaid Services for all Medicare certified agencies. However, among these agencies, PoCD was used almost as frequently for email communication, scheduling, and somewhat less frequently for CPOE and CDSS.
The 2000 NCHS report on HHH agencies, as well as the 2007 consulting firm report on home care agencies, both suggested that facility ownership was associated with various aspects of technology use. In the 2000 report, three ownership categories were explored: for profit, non-profit, and government. The CMR use in those categories was essentially identical: 32.2%, 31.7%, and 33.2%, respectively. Our data categorize ownership as for-profit versus non-profit and government combined; thereby introducing a notable difference in ownership categories between the 2000 and 2007 NCHS surveys. Nonetheless, during this period there was an indisputable trend in adoption of EMR. In 2007, 70.1% of non-profit/government agencies reported current EMR use—an approximate increase of 121% over the 2000 estimate—compared to 27.9% of for-profit agencies. The 70.1% figure for non-profit agencies overall is very similar to the 69.3% figure for non-profit home health agencies reported in the consulting firm survey. It should be noted that our 2007 estimate of EMR use in for-profit HHH agencies is slightly lower than the 2000 CMR estimate for the same group. However, this small reduction may be attributed to the fact that the data come from two independent, randomly selected, samples of agencies and may not represent a meaningful trend. We also showed that 63.1% of non-profit HHH agencies used some kind of PoCD documentation—an adoption rate 6.7 times that of their for-profit counterparts.
One explanation for the higher adoption of EMR in NP agencies is that these agencies might have been more recently established than their FP counterparts and, therefore, might have had the opportunity to more easily incorporate technology into their operations at the point at which the agency was established. Supplemental analyses of the 2007 NHHCS indicated that just the opposite was true: both NP home health and NP hospice agencies were considerably older than their FP counterparts (17.5 vs 7.0 years for hospice agencies and 25.4 vs 11.8 years for home health agencies): an observation that suggests increased use reflects a choice on the part of NP agencies to adopt and integrate EMR and HIT systems in their operations.
Another explanation for the higher adoption rate in NP agencies is the possibility that these agencies may provide more high-technology services than their FP counterparts. Indeed, the 2000 NCHS report indicated that agencies providing high technology services, such as respiratory, enterosomal, and intravenous treatment, were also more likely to be using CMR at that time. We replicated these analyses using the 2007 data and found a similar trend, although the difference did not meet conventional significance levels (p=0.07). Importantly, similar proportions of FP and NP agencies provided high-technology services, so provision of these services per se may not be a viable explanation for enhanced IT adoption in NP HHH agencies. However, it is possible that high-technology services represent a larger amount of the overall business of NP agencies and may, therefore, provide an incentive for these agencies to adopt EMR and PoCD systems more than FP agencies even though both ownership types provide this class of services. A final potential explanation for increased adoption of EMR in NP agencies could be the role of the Center for Aging Services Technologies (CAST) in raising awareness of and promoting adoption of these technologies in NP organizations since CAST's inception in 2003.12 The CAST operates under the auspices of the American Association of Homes and Services for the Aging (AAHSA): a NP organization of exclusively NP aging services providers. In addition to educational sessions on EMRs, telemedicine, and POCD technologies and their benefits at AAHSA's conferences, CAST activities include whitepapers,13 14 a video depicting a vision for technology-enabled home-based care for the 2005 White House Conference on Ageing,15 tools to assist providers in incorporating technology in their strategic planning,16 partnering with the American Health Information Management (AHIMA) on the first annual Long-Term Care (LTC) HIT Summit, and release of a roadmap for HIT in long-term care.17
We noted some interesting trends related to whether agencies were part of a chain. In the 2000 report, CMR use was reported among 34.2% of HHH agencies that were part of a chain and 28.7% that were not part of a chain. The corresponding figures for 2007 were 33.7% and 47.0, respectively. Thus, during the period between 2000 and 2007, use of EMR remained essentially unchanged in HHH agencies that were part of a chain, but their use increased by approximately 64% among agencies that were not part of a chain. This latter observation was partly explained by supplemental analyses that were stratified by ownership: in 2007, the vast majority (88%) of NP HHH agencies were not part of a chain compared to 60% of FP agencies. Among agencies that were not part of a chain, 70% of NP agencies were using EMR compared to only 28% of FP agencies. These data again suggest meaningful differences in EMR use by ownership status and that interpretation of EMR use according to chain membership should be understood in the context of agency ownership. Our report also showed significant differences in use of PoCD, with HHH agencies that were not part of a chain using this technology almost twice as often as their affiliated counterparts.
Study limitations
This report has several limitations that should be considered. First, the NHHCS is cross-sectional—a design feature that prevents research designed to study longitudinal associations of HIT and relevant outcomes such as client health and cost savings. However, the survey provides nationally representative data on EMR, telemedicine, and PoCD use in these agencies and permits evaluation of changes in the use of these systems and their functionalities over time in these care settings.
Further, the combination of the sample size, the use of EMR, and the lack of certain EMR functionalities among the agencies that had EMR systems made it difficult to stratify the data by agency type or ownership or obtain reliable estimates within these categories. As adoption of specific EMR functions increases in the future, analytic limitations associated with sparse cell sizes may decrease; thereby, permitting the reporting of these estimates.
Conclusion
Between 2000 and 2007, there was a 33% increase in use of EMR among HHH agencies in the United States, with the highest relative increase observed in agencies providing only hospice services. In 2007, use of EMR and PoCD technologies in non-profit HHH agencies was significantly higher than for-profit ones—a finding that was unrelated to the age of the agency or whether the agency provided high-technology services. Finally, HHH agencies who had EMR and HIT systems in place generally tended to use the available functionalities, including sharing health information with other entities. The latter functionality is expected to increase in the future as a result of ARRA and its emphasis on health information exchange and standards-based interoperability of HIT.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
The term home care was used in the report, but the authors believe the survey targeted home health rather than home care agencies.
References
- 1.National Council on Disability Consumer directed health: how well does it work? Report to the President of the United States by the National Council on Disability (NCD), 2006. http://www.ncd.gov/newsroom/publications/2004/pdf/consumerdirected.pdf (accessed 3 Oct 2009).
- 2.Doty P. Cost effectiveness of home and community-based long-term care services, 2000. http://aspe.hhs.gov/daltcp/reports/costeff.htm (accessed 3 Oct 2009).
- 3.Costs and benefits of health information technology, Southern California Evidence-Based Practice Center's Report to AHRQ, 2006. http://www.ahrq.gov/downloads/pub/evidence/pdf/hitsyscosts/hitsys.pdf (accessed 3 Oct 2009).
- 4.Barrett LL. Healthy @ Home Report. AARP Knowledge Management, 2008. http://assets.aarp.org/rgcenter/il/healthy_home.pdf (accessed 3 Oct 2009).
- 5.Pearson WS, Bercovitz AR. Use of computerized medical records in home health and hospice agencies: United States, 2000. Vital Health Stat 13 2006;13:1–14 [PubMed] [Google Scholar]
- 6.Philips National Study on the future of technology and telehealth in home care, 2008. http://dms.dartmouth.edu/nhtp/pdf/phillips_home_care.pdf (accessed May 2010).
- 7.http://www.cdc.gov/nchs/nhhcs/nhhcs_questionnaires.htm (accessed 2 Oct 2009).
- 8.http://www.cdc.gov/nchs/data/nhhcsd/NHHCS_NHHAS_web_documentation.pdf (accessed 2 Oct 2009).
- 9.http://www.cdc.gov/nchs/data/nhhcsd/Agency_NHHCS07Questionnaire.pdf (accessed 2 Oct 2009).
- 10.http://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHHCS/2007 (accessed 2 Oct 2009).
- 11.http://www.cms.hhs.gov/apps/media/press/factsheet.asp?Counter=3466 (accessed 9 Nov 2009).
- 12.http://www.aahsa.org/CAST.aspx (accessed 30 Nov 2009).
- 13.http://www.aahsa.org/section_cast.aspx?id=10454 (accessed 26 Apr 2010).
- 14.http://www.aahsa.org/section_cast.aspx?id=10456 (accessed 26 Apr 2010).
- 15.http://www.aahsa.org/article_cast.aspx?id=10153 (accessed 26 Apr 2010).
- 16.http://www.aahsa.org/section_cast.aspx?id=10453 (accessed 26 Apr 2010).
- 17.http://www.ahima.org/meetings/ltc/documents/LTC_HIT_Summit_Report_Final_122005_001.pdf (accessed 26 Apr 2010).