Abstract
Objective
To study how social interactions influence physician adoption of an electronic health records (EHR) system.
Design
A social network survey was used to delineate the structure of social interactions among 40 residents and 15 attending physicians in an ambulatory primary care practice. Social network analysis was then applied to relate the interaction structures to individual physicians' utilization rates of an EHR system.
Measurements
The social network survey assessed three distinct types of interaction structures: professional network based on consultation on patient care-related matters; friendship network based on personal intimacy; and perceived influence network based on a person's perception of how other people have affected her intention to adopt the EHR system. EHR utilization rates were measured as the proportion of patient visits in which sentinel use events consisting of patient data documentation or retrieval activities were recorded. The usage data were collected over a time period of 14 months from computer-recorded audit trail logs.
Results
Neither the professional nor the perceived influence network is correlated with EHR usage. The structure of the friendship network significantly influenced individual physicians' adoption of the EHR system. Residents who occupied similar social positions in the friendship network shared similar EHR utilization rates (p<0.05). In other words, residents who had personal friends in common tended to develop comparable levels of EHR adoption. This effect is particularly prominent when the mutual personal friends of these ‘socially similar’ residents were attending physicians (p<0.001).
Conclusions
Social influence affecting physician adoption of EHR seems to be predominantly conveyed through interactions with personal friends rather than interactions in professional settings.
Social influence pervades our lives. Watching a movie recommended by friends, reading a news article referred by colleagues, dressing up for a formal social event (assuming everybody else will do the same), and so on, are all examples of how other people's opinions or behavior affect our everyday choices. Social influence theories therefore postulate that people are neither born with beliefs or behavior nor are beliefs or behavior developed in isolation. Their formation and evolution occur primarily through social interactions as people compare their own beliefs or behavior with those of others, in particular, similar others.1
Social influence plays the same role in the process of innovation diffusion. This is especially true when an innovation is complex entailing unknown costs or unknown consequences. For example, it has been shown that physicians who are ‘socially proximate’ in a social environment often use one another as information sources or behavior referents to manage the uncertainty of adopting new antibiotic drugs.2 Does social influence exert a similar effect on physician adoption of complex technological innovations such as electronic health records (EHR)?
Answering this question is very important in a healthcare policy climate in which strong emphasis has been placed on increased and improved use of health information technology, and EHR in particular. Furthermore, EHR is much more complex than other types of medical innovations. The adoption of EHR not only requires significant financial investments and learning effort, but also introduces radical change to every single aspect of clinical work. Understanding the social mechanisms underlying physician adoption of EHR is therefore critical to identifying effective strategies to accelerate EHR diffusion and to promote its meaningful use. Unfortunately, such an understanding has been largely missing,3 4 resulting in failed implementations5 and suboptimal or even adverse outcomes.6 7 Given this context, we designed and conducted a study to examine physician adoption of EHR through the lens of social influence.
Social influence, often crystallized as opinion exchange and behavior ‘imitating’, is conveyed in physicians' interpersonal social interactions. Social network analysis (SNA), which views the structure of social interactions as networks composed of nodes (physicians) interconnected by edges (social relations), is an ideal approach for delineating interaction patterns to study how social influence is transmitted among physicians and how it affects their contingent behavior such as EHR adoption. In particular, we designed and conducted a SNA study to assess the social structures among physicians in an ambulatory primary care practice and then relate these structures to individual physicians' utilization rates of an EHR system.
Background
In this section, we briefly discuss two theoretical frameworks that have informed this study. The first framework, intention models originating in social psychology, studies how various factors influence people's decision to conduct (or not to conduct) a certain behavior such as adoption of technological innovations. While this family of models incorporates a theoretical construct known as ‘subjective norm’ for assessing a person's perceived behavioral influence received from others, they do not provide a structure-based means to explicate how this effect is transmitted through different types of social interaction mechanisms. This motivated us to investigate the second theoretical framework, the social contagion literature and the SNA approach that we discuss in the second part of this section. At the end of this section, we present a review of prior SNA studies conducted in medicine and health sciences-related domains, several gaps in the literature that we identified, and our research hypotheses accordingly formulated to address some of these gaps.
Technology acceptance theories
People's decision to accept or reject a technological innovation is driven by multiple factors. Some factors are intrinsic, such as personal characteristics and cognitive styles8; some are extrinsic, such as those relating to the idiosyncrasies of a technology system (eg, ergonomics and speed) or the adequacy of end-user training and support. Other germane factors such as gender,9 age,10 cultural backgrounds,11 professional autonomy,12 and level of user participation in innovation design and implementation,13 are also found to play important roles. These factors and their interplay with social influence received from others may collectively determine a person's attitude toward an innovation, their intention to adopt it, and the eventual decision to accept it in her day-to-day work routines.14 15
The technology acceptance model (TAM) is the prevalent method for studying technology acceptance,16 which is derived from the well-established social psychology theories of reasoned action (TRA) and planned behavior (TPB).17 18 TRA, TPB, and TAM are intention models postulating that a person's behavior (such as innovation adoption) can be predicted by her intention to conduct the behavior, which is in turn a function of her attitude toward the behavior, subjective norm, and other facilitating factors. The unified theory of the acceptance and use of technology, the latest extension of TAM, further theorizes these behavioral antecedents as consisting of four principal constructs: performance expectancy (perceived usefulness), effort expectancy (perceived ease of use), social influence, and facilitating conditions; in addition to four moderating variables: gender, age, experience, and voluntariness of use.19
The subjective norm construct incorporated in these models is meant to capture the effect of social influence that a person receives from others. This construct assesses (1) a person's normative belief that people who are important to her think she should or should not conduct a behavior; and (2) the person's willingness to conform to other people's expectations.17 18 As the effect of social influence is difficult to measure directly,16 the operationalization of this construct usually relies on Likert-scaled survey questions; for example, ‘People who influence my behavior think that I should [adopt the innovation]’ and ‘People who are important to me think that I should [adopt the innovation]’, 19 (p 460). These perceptual measures, however, provide limited insights as to how social influence is transmitted via interpersonal interactions, how it affects people's actual behavior, and how we may harness its power—through manipulating the social structures conveying its effect—to develop social or organizational interventions to facilitate technology adoption and acceptance. Therefore, we resort to the social contagion theory and the SNA approach that provide a means for directly measuring and studying different types of social influence mechanisms.
Social contagion theory
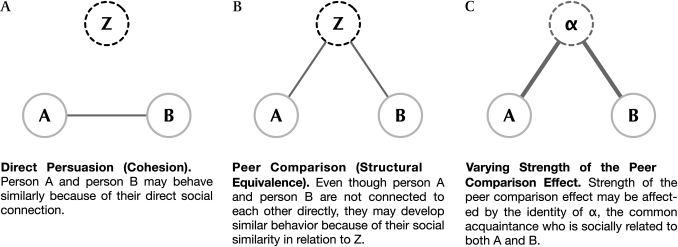
Social contagion theory postulates that as social agents, people's beliefs or behavior is subject to the beliefs or behavior of others who are important to them.20 Social influence resulting in behavioral change, or social contagion, occurs when a person (‘ego’) adapts her beliefs or behavior to those of others (‘alter’). According to social contagion theory, the effect of social contagion travels through interpersonal social structures in two basic forms: direct persuasion and peer comparison. Direct persuasion is transmitted during direct communications between egos and alters leading toward the same or similar behavior (the process of cohesion);21 whereas in peer comparison, a person uses other people who occupy similar social positions as a reference to form her own beliefs or behavior, an effect resulting from structural equivalence.22 Furthermore, the strength of the peer comparison effect may vary based on how the ‘socially equivalent’ individuals are related to each other in a given social structure. For example, two students may develop similar behavior because of a common acquaintance they have. The actual strength of this effect, however, may be different depending on the identity of the common acquaintance (eg, another student, a teacher, or a role model). Burt23 (1987) provides more examples of the peer comparison effect: ‘two siblings close in age and trying to get good grades in the same subjects who are encouraged by their parents, two graduate students publishing the same kind of work and trained by the same professors, or two physicians trying to keep up with the rush of medical development in order to live up to their image of a good physician and maintain their position in the social structure of medical advice and discussion’ (p 1291).
We illustrate these different social contagion mechanisms linking persons A, B, and C, using three diagrams shown in figure 1. In figure 1A, person A and person B may behave similarly because of their direct social connection (direct persuasion or cohesion). In figure 1B, A and B may develop resembling behavior because they are socially similar in relation to Z, even though A and B are not connected to each other directly (peer comparison or structural equivalence). In figure 1C, the strength of the social comparison effect may vary according to the identity of α, the common acquaintance who is socially related to both A and B.
Figure 1.
Illustration of common social contagion mechanisms.
In this paper, we report an empirical study conducted to examine how social influence affecting physicians' EHR adoption behavior is transmitted via these two basic forms of social contagion mechanisms, referred to as ‘cohesion networks’ and ‘structure equivalence derivatives’, respectively.
Applications of SNA in health care
Social network analysis is a widely used approach in modern sociology, anthropology, social psychology, and organization studies for examining human relations and interpersonal interaction patterns. In healthcare, the pioneer work of Anderson and Jay24 (1985) applied SNA to assess physician adoption of early-generation information technologies. By clustering 24 physician participants into four subgroups based on their social relationships, the study found that different ‘physician cliques’ demonstrated distinct behavior in adopting of a mainstream hospital information system. In another study, Rice and Aydin25 (1991) surveyed 104 healthcare workers at a large urban hospital. They found that ‘social cues’ received from others significantly influenced the subjects' attitude toward an integrated hospital information system, ‘over and above other traditional sources’ (p 238). In recent years, numerous studies have applied SNA or SNA-like approaches to examine information sharing among patients and the resulting behavior contagion phenomena26–28 and professional advice exchange among medical professionals.29–32 However, to our knowledge, no recent studies have used the SNA approach to explore the impact of the social contagion effect on physician adoption of modern, complex technological innovations such as EHR. This research was designed to address this gap.
Research hypotheses
Two dimensions of social structures, professional and personal (friendship), have been found to be primary channels through which values affecting people's beliefs or behavior are transmitted.33 Accordingly, we measured and studied these two social structures in this study. In the medical context, the professional social network is formed based on professional consultation on patient care-related matters; the friendship social network originates in personal intimacy.25 Informed by the social psychology intention models discussed earlier,16–19 we also assessed a third social structure in this study, the perceived influence network, soliciting a person's perception of how other people have affected her intention to adopt an innovation. Based on this three-dimensional social structure scheme, we formulated our study hypotheses as follows:
Hypothesis 1a–b: Cohesion over professional network (1a) and friendship network (1b) is positively correlated with cohesion over perceived influence network.
Hypothesis 1c: Cohesion over professional network is positively correlated with cohesion over friendship network.
Hypothesis 2a–b: Structural equivalence of professional network (2a) and friendship network (2b) is positively correlated with structural equivalence of perceived influence network.
Hypothesis 2c: Structural equivalence of professional network is positively correlated with structural equivalence of friendship network.
The hypotheses above test the correlation between the three cohesion networks and between their structural equivalence derivatives. To relate these social structures to physician adoption of EHR, we further test the following hypotheses:
Hypothesis 3a–c: Level of EHR adoption will be predicted by cohesion over professional network (3a), friendship network (3b), and perceived influence network (3c).
Hypothesis 4a–c: Level of EHR adoption will be predicted by structural equivalence of professional network (4a), friendship network (4b), and perceived influence network (4c).
The results obtained from testing each of these study hypotheses, collectively, may help shed light on how these different social structures are related to each other, how social influence is transmitted through them, and which structures may convey influential social contagion effects resulting in actual behavioral change (physician adoption of EHR). In the remaining sections of this paper, we label the professional network Pro, the friendship network Fri, and the perceived influence network PcI. Their structural equivalence derivatives are labelled ProSE, FriSE, and PcISE, respectively.
Methods
Empirical study setting
The study reported in this paper was part of a larger project to evaluate the adoption and impact of an EHR system in the ambulatory care environment. The empirical setting was an outpatient primary care practice at the Western Pennsylvania Hospital, a 512-bed, tertiary care medical facility serving Pittsburgh and the surrounding areas. This practice administers the hospital's internal medicine residency training program in which residents treat patients under the supervision of attending physicians. Residents are assigned to work with the same attending physician for at least 1 year but they may interact with other attending physicians regularly due to vacations and assignment conflicts.
A homegrown EHR system was deployed in the study clinic and was available for use by all physicians.34 35 The resident physicians used the system to document and retrieve patient care data. The attending physicians used the system to review and approve the residents' work. Because the attending physicians' interactions with the system were not directly related to patient care, their usage was not included in the EHR usage analysis. Among the residents, use of the system during all patient visits was highly recommended; however, it was not mandatory. Therefore, we can reasonably assume that the EHR utilization rates reported in this paper reflect the residents' true, self-motivated intention to use the system in their day-to-day clinical activities.
Study participants
The empirical study involved all 55 physicians affiliated with the study clinic at the time this research was conducted, including 15 attending physicians; 12 second-year and 15 third-year residents; and 13 physicians who completed the residency training program in the spring of 2006 (referred to as ‘PGY4 graduates’ in this paper).
Of the 12 second-year and 15 third-year residents, 24 actively practiced in the clinic throughout the 14-month EHR usage data collection time period. They were recruited in the study as ‘active participants’ and were invited to complete the social network survey in which they reported their social interactions with their fellow residents and their attending physicians. The attending physicians and the PGY4 graduates were included in the study as ‘social actors’ but not as ‘active participants’. This is because the attending physicians did not use the system's EHR functionality and the PGY4 residents had already graduated when the social network survey was administrated.
The hospital's Institutional Review Board reviewed and approved the research protocol of this study. All identifying information was removed from the data collected; in addition, the participating residents were assured that their survey responses and their EHR utilization rates would only be seen by the clinic management in an aggregated format and therefore could not be used in any evaluative ways. This study did not collect any patient information.
Electronic health records usage
Usage of an EHR system can be defined in multiple ways; for example, certain meaningful use measures may only take into account EHR usage that contributes directly to the improvement of patient outcomes or efficiency gains. In this study, we used a surrogate measure, utilization of the EHR system signified by ‘sentinel use events’ (consisting of patient data documentation or retrieval activities), that must occur before any meaningful use of EHR can be achieved. Such usage is a prerequisite to more sophisticated use of the value-augmenting EHR functionalities such as chronic disease management templates or e-prescribing modules. A resident's EHR utilization rate was thus calculated as the number of patient encounters assigned to the resident in which patient data documentation or retrieval activities were recorded within 24 h of a patient visit, divided by the total number of patient visits assigned to the resident and checked in by clerical staff (to remove no-show or cancelled appointments). The EHR usage data included in the analysis were collected from the system's audit trail logs recorded between June 28, 2005, the system's ‘go-live’ date, and August 18, 2006, when a social network survey was administered.
Survey instruments
Social network survey
The social network survey was jointly developed by the researchers and two attending physicians from the study clinic. The survey instrument went through several rounds of pilot testing and revisions. The final instrument used three questions to assess, respectively, the structure of the professional, friendship, and perceived influence networks in the study clinic: (1) ‘Which colleagues do you go to as a source of information on patient care-related matters’; (2) ‘Which colleagues do you consider to be your personal friends’; and (3) ‘Which colleagues have generally influenced your intention to use [name of the EHR system]’. Each question was provided with a roster of the respondent's physician colleagues in the study clinic and a checkbox next to each person's name.
Survey of personal characteristics
Informed by TAM and other intention models, we also administered a survey to assess several personal characteristics known to influence people's technology adoption and acceptance behavior. These include: (1) gender; (2) work experience, measured as the residents' postgraduate year (PGY); (3) computer literacy composed of computer experience, computer knowledge, and computer optimism; and (4) perceived usefulness and perceived ease of use of the EHR system. Facilitating conditions, age, and voluntariness of use were not assessed in this study because there was little or no variation in these variables in our study sample (average age of the resident physicians: 28.6±1.7).
Computer literacy was assessed using Cork's instrument measuring physicians' use of, knowledge about, and attitudes toward computers.36 The TAM constructs were assessed using its original validated survey instrument,16 with slight rewording to suit the context of this study.
Social network analysis methods
We used two SNA measures to assess the overall structure of the three social networks delineated: (1) density, defined as the number of social relations identified divided by the total number of relations that could possibly be present37; and (2) Freeman's degree centrality, which measures the degree to which a social network is organized around its well-connected central nodes.38 These measures reflect how well the physicians in the study practice were connected to each other and whether there might be a few key individuals who possess pivotal positions in the practice's social space.
Structural equivalence of a cohesion network was derived using the correlation method, which captures the similarity between the interaction patterns of pairs of actors in a given social network.39 To test network correlations (hypotheses 1a through 2c), we used the quadratic assignment procedure (QAP). QAP is a permutation-based, non-parametric method for testing the correlation, that is, the structural similarity, between different social network structures. The computational details of QAP can be found in Krackhardt40 (1988).
We used the network effects model (NEM) to assess the influence of the three social structures on the residents' EHR usage (hypotheses 3a through 4c). NEM is a network autocorrelation model that evaluates the impact of social network structures on the measurements of a response variable, in this context, the physicians' utilization rates of the EHR system. NEM takes the form of:
where the dependent variable, y, is a vector of individual residents' utilization rates of the EHR system; ρ is the network autoregressive coefficient; W is a matrix of row-normalized network weights that models the structure of a social network or its structural equivalence derivative;42 and X is a covariate matrix incorporating all other local effects (eg, gender and work experience). The mathematical underpinning of NEM can be found in Doreian41 (1980) and Leenders42 (2002).
In the autocorrelation regression, we represented gender as a binomial variable (0: female) and PGY as an interval ordinal variable (starting with 0, which represents the second-year residents). Other local effect measures such as computer literacy scores were normalized to a 0–1 continuous scale.
We used UCINET to perform dyadic matrix manipulations and the QAP permutation (Analytic Technologies, Lexington, Kentucky, USA). To estimate the model parameters of NEM, we used the routines for social network analysis (sna package) in R, a programming language and software environment for statistical computing and graphics (http://www.r-project.org/). Network topologies (figure 2) were drawn using GUESS, an open-source graph exploration system (http://graphexploration.cond.org).
Figure 2.
Sociograms of the three social networks delineated. Circles, resident physicians; Squares, attending physicians; Blue (darker) shades, areas enclosed by the active participants of the study (the second- and third-year residents); Green (lighter) shades, areas enclosed by the attending physicians. The size of a node is proportional to its eigenvector centrality. Better connected nodes are larger.
Results
Electronic health records usage
During the 14-month EHR usage data collection period, the study clinic scheduled a total of 9938 outpatient appointments, 4795 of which were checked in and 1922 had EHR usage recorded. The ratio of no-show or cancellation was 52%. The overall EHR utilization rate was 40% (SD ±18.3%).
The total number of appointments assigned to the ‘active participants’ in the study (the second and third-year residents) was 3836, of which 1796 were checked in. EHR usage was documented in 776 of these checked-in patient visits. The average no-show or cancellation ratio among the second and third-year residents was 53%. Their overall EHR utilization rate was 43% (SD ±19.6%). There is no evidence that the distribution of workload among these residents was skewed such that it might have an impact on an individual's EHR utilization rate. The average number of monthly appointments assigned to these residents was 10.1 and the SD was ±3.4.
Survey responses
The social network survey was distributed between August 14–18, 2006. Out of the 24 eligible ‘active participants’ who were invited to participate, 20 responded and 18 responses were valid. One returned questionnaire was removed from the analysis because the respondent checked every colleague's name to all three questions; the other was excluded because only one question was answered. The 18 active participants who returned valid survey responses included nine second-year (five women and four men) and nine third-year (three women and six men) residents.
The survey assessing the physicians' personal characteristics was conducted in the summer of 2005 at the end of each individual EHR training session. All participants returned valid responses. Some attributes such as gender and PGY were retrieved from the hospital's human resources database. Note that this survey was administered before the EHR usage data collection. This is an intended design so that the personal characteristics assessed at baseline can be analyzed as predictors of individual physicians' EHR adoption level.
Social network analysis
Descriptive results
Through the social network survey, the 18 active participants reported a total of 614 social relationships with their physician colleagues in the study clinic, including 162 professional relationships, 417 friendship relationships, and 35 perceived influence relationships (33 professional, 181 friendship, and seven perceived influence relationships were among the 18 residents). The density of the three cohesion networks is 0.055, 0.14, and 0.012, respectively. The Freeman's degree centrality measure is 27.53%, 75.19%, and 11.08%, respectively. Compared with the professional and the perceived influence network, the friendship network is more densely populated; in addition, it has more well-connected central nodes.
It should be noted that not all social relations studied in this research were necessarily reciprocal, that is, the relationships claimed by the 18 ‘active participants’ with other ‘social actors’ were not reciprocally confirmed. This does not affect the validity of the research findings of this study. While the non-reciprocal ties only reflect a person's self-evaluation of how she is related to other actors in a given social environment, social influence could be effectively transmitted through non-reciprocal relationships. For example, people may elect to consider a person with an extraordinarily pleasant personality as a friend, while this ‘friend’ may not necessarily confirm the friendship relations with everybody else. This non-reciprocal friendship, however, may still convey significant social cognation effects.
Sociograms
Figure 2 shows the sociograms depicting each of the three social networks delineated. Circles represent the residents and squares represent the attending physicians. The size of a node is proportional to its eigenvector centrality measure,43 indicating the ‘popularity’ of a person measured as the extent to which the person is connected with other actors in a social network. In figure 2A–C, the network nodes are spatially distributed so that those with more connections are placed closer to each other and relatively in the center of the graphs. For a more effective visual inspection, we used blue color (darker) to designate the zones enclosed by the nodes representing the second and third-year residents, and green color (lighter) to designate the zones connecting the attending physician nodes. The nodes outside the colored convexes thus represent the PGY4 graduates.
Note that those isolated nodes were not plotted in the sociograms in figure 2. As a result, the professional network left out two third-year residents who were not related to anybody else in the clinic's social system when this study was conducted. In the more sparsely populated perceived influence network, 30 people were left out (who were not reported to have either given or received direct influence on the adoption of the EHR system). All physicians in the study clinic were involved in the friendship network with varying degrees of participation.
Network correlations
Network correlation scores obtained by performing the QAP permutation are shown in table 1. The three cohesion networks are significantly correlated with one another (Pro-Frn: p<0.001; Pro-PcI: p<0.05; Frn-PcI: p<0.05). Hypotheses 1a through 1c are therefore all accepted even though the correlation between the perceived influence network (PcI) and the other two networks is much weaker compared with the correlation between the professional and the friendship networks (Pro-Frn). Furthermore, the QAP results confirm hypothesis 2c (ProSE-FrnSE, p<0.05) while rejecting hypotheses 2a (ProSE-PcISE) and 2b (FrnSE-PcISE). Nonetheless, all QAP correlation scores are small suggesting that no considerable similarities exist between the three cohesion networks and between their structural equivalence derivatives.
Table 1.
Network correlation test results
| Pro | Frn | PcI | ProSE | FrnSE | PcISE | ||
| Pro | – | – | – | ProSE | – | – | – |
| Frn | 0.27*** | – | – | FrnSE | 0.28* | – | – |
| PcI | 0.15* | 0.13* | – | PcISE | 0.001 | 0.061 | – |
p<0.05
p<0.001.
Network effects model regression results
Network effects model regression results are reported in table 2 (upper portion: cohesion networks; lower portion: structural equivalence derivatives). Hypothesis 4b is supported by the NEM results (ρ=2.02, p<0.05), suggesting that the structural equivalence of the friendship network predicts the level of EHR adoption of individual physicians. Neither the autoregressive coefficients of the three cohesion networks nor those of the structural equivalence derivatives of the professional and the perceived influence network are statistically significant. Therefore, we reject hypotheses 3a–c, testing whether the three cohesion social structures are associated with individual physicians' EHR utilization rates; and hypotheses 4a and 4c, testing whether the structural equivalence derivatives based on the professional and the perceived influence network have an influence on physicians' adoption of EHR.
Table 2.
Results of the network autocorrelation regression
| Variable | Pro | Frn | Z | PcI | Z | |
| Coefficient | Z | Coefficient | Coefficient | |||
| ρ | 0.25 | 0.60 | −0.36 | −0.45 | 0.038 | 0.13 |
| Gender | −0.0093 | −0.12 | −0.018 | −0.23 | −0.011 | −0.14 |
| PGY | 0.04 | 0.53 | 0.059 | 0.78 | 0.057 | 0.69 |
| CE | −0.11 | −0.19 | −0.22 | −0.39 | −0.25 | −0.45 |
| CK | −0.84 | −3.11** | −0.73 | −2.45* | −0.77 | −2.53* |
| CO | 0.75 | 1.37 | 0.95 | 2.12* | 0.91 | 1.78 |
| PU | −0.19 | −0.44 | −0.34 | −0.88 | −0.31 | −0.82 |
| PEoU | 0.46 | 1.36 | 0.61 | 2.15* | 0.58 | 2.09* |
| Variable | ProSE | Z | FrnSE | Z | PcISE | Z |
| Coefficient | Coefficient | Coefficient | ||||
| ρ | 0.2 | 1.52 | 0.22 | 2.02* | 0.12 | 1.13 |
| Gender | 0.0071 | 0.095 | 0.041 | 0.55 | −0.0025 | −0.033 |
| PGY | 0.059 | 0.84 | 0.022 | 0.32 | 0.026 | 0.34 |
| CE | −0.57 | −1.03 | −0.16 | −0.33 | −0.24 | −0.44 |
| CK | −0.85 | −3.39*** | −0.73 | −3.04** | −0.74 | −2.85** |
| CO | 1.06 | 2.47** | 0.72 | 1.71 | 0.86 | 1.96* |
| PU | −0.11 | −0.29 | −0.5 | −1.4 | −0.33 | −0.91 |
| PEoU | 0.33 | 1.07 | 0.55 | 2.18* | 0.48 | 1.69 |
p<0.05
p<0.01
p<0.001.
CE, computer experience; CK, computer knowledge; CO, computer optimism; PGY, postgraduate year; PEoU, perceived ease of use; PU, perceived usefulness.
Among the seven local effect covariates, computer knowledge is negatively associated with EHR usage; and computer optimism and perceived ease of use generally have a positive effect over usage. Gender, PGY, computer experience, and perceived usefulness do not seem to exert a significant influence. The results of these local effects are consistent with the findings of an earlier study evaluating the pilot implementation of the EHR system in the same clinic.34
As the study sample included both residents and attending physicians, we further conducted a drill-down analysis by partitioning each of the social structures into two parts: (1) the segments among all residents (labeled as Pro_Res, ProSE_Res, and so forth); and (2) the segments with only the resident-attending relationships retained (Pro_Att, ProSE_Att, and so forth). This drill-down analysis was intended to detect whether the social interactions among the residents may have a different impact on EHR adoption as compared with the interactions between the residents and their attending physicians. The findings are reported in table 3 (non-significant results are not shown). Similar to the findings based on the entire study sample, the structural equivalence derivatives of the friendship network (FriSE_Res, and FriSE_Att) are the only social structures that found to have a significant influence over EHR usage. As table 3 shows, the effect of the social influence transmitted between the residents and their attending physicians is notably more significant (p<0.001) than the social influence transmitted among the residents (p<0.05).
Table 3.
Results of the drill-down analysis
| Variable | FrnSE_Res | Z | FrnSE_Att | Z |
| Coefficient | Coefficient | |||
| ρ | 0.15 |
|
0.15 |
|
| Gender | −0.046 | −0.57 | 0.027 | 0.42 |
| PGY | 0.059 | 0.81 | −0.0072 | −0.11 |
| CE | 0.14 | 0.26 | −0.12 | −0.25 |
| CK | −0.47 | −1.65 | −0.69 | −3** |
| CO | 0.51 | 1.12 | 0.56 | 1.37 |
| PU | −0.52 | −1.47 | −0.3 | −0.92 |
| PEoU | 0.43 | 1.66 | 0.59 | 2.49* |
p<0.05
p<0.01.
CE, computer experience; CK, computer knowledge; CO, computer optimism; PGY, postgraduate year; PEoU, perceived ease of use; PU, perceived usefulness.
Discussion
Insights from the sociograms
Besides the well-connected attending physicians, several residents also served as information hubs in the professional network (figure 2A) providing consultation on patient care-related matters to other residents. This suggests that in the study clinic a considerable proportion of professional advice was conveyed through likely ‘curbside’ communications among the resident peers. In the friendship network, not surprisingly, the residents were more likely to be considered as personal friends by their fellow residents. However, each of the attending physicians also received at least one friendship relation; and a few appeared to be popular personal friends among the residents.
The perceived influence network has sparser connections and far fewer nodes. This suggests that the social interactions conveying direct behavioral influence over the adoption of the EHR system rarely took place in the study clinic. It is also possible that such influence could not be consciously recalled by the survey respondents and therefore was not fully reported in response to the question ‘Which colleagues have generally influenced your intention to use [name of the EHR system]?’ This question, inherited from the unified theory of the acceptance and use of technology, requires the survey respondents to: (1) retrospectively retrieve relevant social interaction events (eg, a curbside conversation) that may occur sporadically over a long period of time; and (2) make a deterministic judgment of the significance of the events worth reporting.44 45 This measurement issue could preclude an accurate and comprehensive assessment of the ‘perceived influence’ construct, which may also explain partly why none of the PGY4 graduates appeared in the perceived influence network. The self-reported subjective norm measure commonly used in the intention model-based studies thus may not adequately capture the effect of social influence.
Mechanisms of social influence
None of the cohesion networks were found to have a significant impact on individual residents' utilization rates of the EHR system. This suggests that the residents who had direct communications with each other did not seem to develop comparable levels of EHR usage. One explanation may be, as shown in the literature, that while cohesion could alter beliefs, altered beliefs do not necessarily result in actual behavior change.46 However, we are unable to make a conclusive assertion within the scope of this study that behavior-altering social influence does not transmit through physicians' cohesion networks.
On the other hand, the structural equivalence derivative of the friendship network is strongly correlated with EHR usage, suggesting that the residents who occupied similar social positions in the friendship network—those who had personal friends in common—tended to develop similar levels of EHR adoption. This finding is consistent with what has been reported in the literature.
First, personal intimacy is more likely to be associated with trust and thus stronger power of persuasion; whereas interactions in professional settings, particularly in the residency training environment where the empirical study was conducted, are by and large formed around ad hoc situational proximities (eg, supervising relationships). Such interactions do not always convey the traits of shared values and interests, reciprocal liking, mutual positive affect, and emotional commitment.47 These traits are, on the other hand, the defining characteristics of friendship relations.33 Furthermore, compared with professional relationships, friendship usually takes a longer time to establish and is more stable once established, allowing the influence to accumulate and result in actual belief or behavior alterations.48
Second, previous research has shown that compared with direct persuasion, peer comparison is a more influential social force deriving people's beliefs or behavior.23 49 When evaluating a decision situation and the associated behavioral consequences, people often use ‘structurally equivalent’ peers as a frame of reference even though these structurally equivalent individuals do not communicate with each other directly. As Burt23 (1987) argued, peer comparison is triggered when people compare themselves with socially similar others: they watch over their shoulders to learn what others do and adapt their behavior accordingly to meet the expectation of mutual acquaintances, live up to their image of being an outstanding professional, and maintain their positions in a given social environment. This effect, in essence, reflects a person's evaluation in a situated social context: ‘what would another person do if he were in my shoes?’42 (p 27).
The peer comparison effect becomes more prominent within the friendship network segment between the residents and their attending physicians. The residents who were socially similar in this manner—those who had the same attending physicians as personal friends—were more likely to develop comparable EHR adoption behavior. The leadership member exchange theory provides a rationale for this finding, which views cross-hierarchical friendship developed in the workspace is a special kind of interpersonal relation that transcends the boundary of traditional friendship notions to allow lower-rank actors (the residents) to establish intimate relationships with higher-status actors (the attending physicians).47 Due to the asymmetry of power, which often leads to greater physical and social distancing, such supervisor–subordinate friendship is more difficult to establish.50 However, once established, it also exerts a stronger behavioral influence because of the performance appraisal and career promotion mechanisms built into it.51
These three social influence mechanisms can be better explained using the illustrations presented earlier in figure 1. Figure 1A displays a scenario in which residents A and B hold direct social relationships. We hypothesized that A and B would therefore demonstrate similar EHR adoption behavior because of the cohesion effect. This hypothesis was not supported by the empirical data. Figure 1B shows that residents A and B, who are structurally equivalent in relation to Z, may develop similar behavior because of the peer comparison effect. This hypothesis was confirmed. In figure 1C, the peer comparison effect is further intensified by a mutually acquainted attending physician, α, who has a cross-hierarchical friendship relation with both resident A and resident B.
Implications for alternative strategies to facilitate diffusion of innovation
Leveraging on opinion leaders' personal influence to promote information dissemination or behavior change has been shown to be an effective approach; for example in the areas of improving physician's coherence to clinical guidelines52 and patients' compliance to recommended behavior.53 Similarly, researchers have argued that the recognition and nurturing of opinion leaders (‘special people’ or ‘super users’) should be among the highest priorities of those implementing complex technological systems in healthcare settings.54 55 Nonetheless, what makes an opinion leader credible and influential has been poorly understood.56 In this study, we show that identifying opinion leaders who also profess ‘personal intimacy’ with many other actors in a medical practice's social space could yield more rewarding results in promoting and accelerating innovation diffusion.
Implications for studying innovation adoption among healthcare professionals
A growing number of studies have applied TAM, TRA, TPB, or their model variants to examine the technology adoption and acceptance behavior of healthcare professionals.57–63 These studies, however, have shown conflicting results. Some reported that subjective norm is a significant behavioral determinant of clinicians' innovation adoption,62 63 whereas others found that social influence only has a negligible impact. For example, Chau and Hu60 (2001) argued that ‘physicians, in general, may rely highly on their own assessments in making technology acceptance decisions’ because of professional autonomy and their specialized training encouraging independent thinking (p 175).60 This argument, however, contradicts a large body of social science research illustrating that physicians commonly use their peers as a crucial source of information, advice, and behavior referent.2 23 64 65 Furthermore, it has been well documented that socially constructed knowledge disseminated by word of mouth is a key instrument translating scientific findings of medical research into clinical practice.64 66 Therefore, we argue that the negligible impact of social influence on clinicians' innovation adoption, as reported in many intention model based studies, is loosely grounded. An extended discussion on this topic has been reported elsewhere.67
It should be noted that several intention model studies introduced new constructs to accommodate the effect of social influence, including ‘perceived usefulness towards professional status’,58 ‘image’,59 and ‘physician self-identity’.62 These constructs were assessed using survey questions such as ‘I use the system because of the proportion of coworkers who use it’ and ‘Having the system is a status symbol in my organization’. These psychosocial constructs are essentially measuring the peer comparison effect although not stated in an explicit manner.
Study limitations
The empirical study reported in this paper should be interpreted in the context of its limitations. First, the sample size was relatively small. It is unfortunate that the PGY4 graduates could not be included in the study as ‘active participants’ due in part to administrative delays. Second, the social network survey was only able to capture a one-time snapshot of the social structures in the study clinic. It could not reveal the evolving dynamics in the development of the physicians' social relationships during the entire EHR adoption process. Third, the empirical study was conducted in a residency training environment; internal medicine residents were the primary users of the EHR system. The research findings therefore may not be generalizable to other types of clinicians or other types of medical facilities. Finally, in this study, EHR usage was measured as whether sentinel use events consisting of patient data documentation and retrieval activities were recorded. This measure does not fully assess whether the system had been used meaningfully to contribute to broader quality and efficiency improvement goals.
Conclusions
This research aims to improve our understanding of physician EHR adoption through the lens of social influence. We applied SNA to study the structure of social interactions that may affect individual physicians' EHR adoption behavior. Through the empirical application, we demonstrate that the SNA approach, which allows for a structure-based exploration of the pattern of social interactions, can yield more objective and more accurate assessments of the social contagion effect compared with using perception-based measures. We therefore encourage other researchers also to consider this approach when studying the effect of social influence on clinician adoption of EHR, or other types of health information technologies more generally.
In the empirical study reported in this paper, conducted in an ambulatory primary care practice at an urban teaching hospital, we found that the friendship social network based on personal intimacy reveals more robust and more influential interpersonal ties particularly among those ‘structurally equivalent’ individuals. Within the scope of this study, we could not make a conclusive assertion that friendship is the only interaction channel by which behavior-altering social influence is transmitted. However, the empirical data do indicate that personal trust, or power of persuasion, is more likely to develop through friendship relations, particularly through cross-hierarchical friendship between residents and attending physicians. This finding suggests that using opinion leaders as physician champions to promote innovation adoption may not yield optimal results if the opinion leaders possess little ‘capital’ in the friendship social space of a given clinical environment. Identifying those ‘popular’ physicians who are mutual personal friends of many other people could be a more effective alternative strategy.
Footnotes
Competing interests: None.
Ethics approval: The Institutional Review Board at the Western Pennsylvania Hospital reviewed and approved the research protocol of this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Erickson BH. The relational basis of attitudes. In: Wellman B, Berkowitz SD, eds. Social structures: a network approach. New York: Cambridge University Press, 1988:99–121 [Google Scholar]
- 2.Coleman J, Katz E, Menzel H. Medical innovation: a diffusion study. 2nd edn New York, NY: Bobbs-Merrill, 1966 [Google Scholar]
- 3.Kaplan B. Evaluating informatics applications—some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inf 2001;64:39–56 [DOI] [PubMed] [Google Scholar]
- 4.Delpierre C, Cuzin L, Fillaux J, et al. A systematic review of computer-based patient record systems and quality of care: more randomized clinical trials or a broader approach? Int J Qual Health Care 2004;16:407–16 [DOI] [PubMed] [Google Scholar]
- 5.Goddard BL. Termination of a contract to implement an enterprise electronic medical record system. J Am Med Inform Assoc 2000;7:564–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kazley AS, Ozcan YA. Do hospitals with electronic medical records (EMRs) provide higher quality care? An examination of three clinical conditions. Med Care Res Rev 2008;65:496–513 [DOI] [PubMed] [Google Scholar]
- 7.Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005;116:1506–12 [DOI] [PubMed] [Google Scholar]
- 8.Agarwal R, Prasad J. The role of innovation characteristics and perceived voluntariness in the acceptance of information technologies. Decision Sci 1997;28:557–82 [Google Scholar]
- 9.Venkatesh V, Morris MG. Why don't men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS Quart 2000;24:115–39 [Google Scholar]
- 10.Morris MG, Venkatesh V. Age differences in technology adoption decisions: implications for a changing work force. Pers Psychol 2000;53:375–403 [Google Scholar]
- 11.Straub D, Keil M, Brenner W. Testing the technology acceptance model across cultures: a three country study. Inf Manage 1997;33:1–11 [Google Scholar]
- 12.Edwards N, Kornacki MJ, Silversin J. Unhappy doctors: what are the causes and what can be done? BMJ 2002;324:835–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barki H, Hartwick J. Measuring user participation, use involvement, and user attitude. MIS Quart 1994;18:59–82 [Google Scholar]
- 14.Mead GH. Mind, self and society. Chicago, IL: The University of Chicago Press, 1934 [Google Scholar]
- 15.Blumer H. Symbolic interactionism, perspective and method. Berkeley, CA: University of California Press, 1969 [Google Scholar]
- 16.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quart 1989;13:319–40 [Google Scholar]
- 17.Fishbein M, Ajzen I. Beliefs, attitude, intention and behavior: an introduction to theory and research. Reading, MA: Addison-Wesley, 1975 [Google Scholar]
- 18.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, eds. Springer series in social psychology. Berlin: Springer, 1985:11–39 [Google Scholar]
- 19.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: toward a unified view. MIS Quart 2003;27:425–78 [Google Scholar]
- 20.Merton RK, Rossi AS. Contributions to the theory of reference group behavior. In: Merton RK, ed. Social theory and social structure. New York: Free Press, 1950:279–334 [Google Scholar]
- 21.Homans GC. The human group. New York: Harcourt Brace, 1950 [Google Scholar]
- 22.Burt RS. Cohesion versus structural equivalence as a basis for network subgroups. Sociol Methods Res 1978;7:189–212 [Google Scholar]
- 23.Burt RS. Social contagion and innovation: cohesion versus structural equivalence. Am J Sociol 1987;92:1287–35 [Google Scholar]
- 24.Anderson JG, Jay SJ. Computers and clinical judgment: the role of physician networks. Soc Sci Med 1985;20:969–79 [DOI] [PubMed] [Google Scholar]
- 25.Rice RE, Aydin C. Attitudes toward new organizational technology: network proximity as a mechanism for social information processing. Adm Sci Q 1991;36:219–44 [Google Scholar]
- 26.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370–9 [DOI] [PubMed] [Google Scholar]
- 27.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med 2008;358:2249–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ 2008;337:a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott J, Tallia A, Crosson JC, et al. Social network analysis as an analytic tool for interaction patterns in primary care practices. Ann Fam Med 2005;3:443–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keating NL, Ayanian JZ, Cleary PD, et al. Factors affecting influential discussions among physicians: a social network analysis of a primary care practice. J Gen Intern Med 2007;22:794–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Westbrook JI, Braithwaite J, Georgiou A, et al. Multimethod evaluation of information and communication technologies in health in the context of wicked problems and sociotechnical theory. J Am Med Inform Assoc 2007;14:746–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Merrill J, Hripcsak G. Using social network analysis within a department of biomedical informatics to induce a discussion of academic communities of practice. J Am Med Inform Assoc 2008;15:780–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gibbons DE. Friendship and advice networks in the context of changing professional values. Adm Sci Q 2004;49:238–62 [Google Scholar]
- 34.Zheng K, Padman R, Johnson MP, et al. An adoption study of a clinical reminder system in ambulatory care using a developmental trajectory approach. Stud Health Technol Inform 2004;107:1115–19 [PubMed] [Google Scholar]
- 35.Zheng K, Padman R, Johnson MP, et al. An interface-driven analysis of user interactions with an electronic health records system. J Am Med Inform Assoc 2009;16:228–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cork RD, Detmer WM, Friedman CP. Development and initial validation of an instrument to measure physicians' use of, knowledge about, and attitudes toward computers. J Am Med Inform Assoc 1998;5:164–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wasserman S, Faust K. Social network analysis: methods and applications. New York: Cambridge University Press, 1994 [Google Scholar]
- 38.Freeman LC. A set of measures of centrality based on betweenness. Sociometry 1977;40:35–41 [Google Scholar]
- 39.Breiger R, Boorman S, Arabie P. An algorithm for clustering relational data with applications to social network analysis and comparison with multidimensional scaling. J Math Psychol 1975;12:328–83 [Google Scholar]
- 40.Krackhardt D. Predicting with networks: noparametric multiple regression analysis of dyadic data. Soc Networks 1988;10:359–81 [Google Scholar]
- 41.Doreian P. Linear models with spatially distributed data. Sociol Methods Res 1980;9:29–60 [Google Scholar]
- 42.Leenders RTAJ. Modeling social influence through network autocorrelation: constructing the weight matrix. Soc Networks 2002;24:21–47 [Google Scholar]
- 43.Bonacich P. Factoring and weighting approaches to clique identification. J Math Sociol 1972;2:113–20 [Google Scholar]
- 44.Robinson MD, Clore GL. Belief and feeling: evidence for an accessibility model of emotional self-report. Psychol Bull 2002;128:934–60 [DOI] [PubMed] [Google Scholar]
- 45.Bradburn NM, Rips LJ, Shevell SK. Answering autobiographical questions: the impact of memory and inference on surveys. Science 1987;236:157–61 [DOI] [PubMed] [Google Scholar]
- 46.Merton RK. The unanticipated consequences of purposive action. Am Sociol Rev 1936;1:894–904 [Google Scholar]
- 47.Berman EM, West JP, Richter MN. Workplace relations: friendship patterns and consequences (according to managers). Public Admin Rev 2002;62:217–30 [Google Scholar]
- 48.Shah PP. Network destruction: the structural implications of downsizing. Acad Manage J 2000;43:101–12 [Google Scholar]
- 49.Burkhardt ME. Social interaction effects following a technological change: a longitudinal investigation. Acad Manage J 1994;37:868–96 [Google Scholar]
- 50.Bass BM. Bass and Stodgill's handbook of leadership. 3rd edn New York: Free Press, 1990 [Google Scholar]
- 51.Boyd NG, Taylor RR. A developmental approach to the examination of friendship in leader-follower relationships. Leadership Quart 1998;9:1–25 [Google Scholar]
- 52.Gifford DR, Holloway RG, Frankel MR, et al. Improving adherence to dementia guidelines through education and opinion leaders. a randomized, controlled trial. Ann Intern Med 1999;131:237–46 [DOI] [PubMed] [Google Scholar]
- 53.Valente TW. Opinion leader interventions in social networks. BMJ 2006;333:1082–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ash JS, Stavri PZ, Dykstra R, et al. Implementing computerized physician order entry: the importance of special people. Int J Med Inf 2003;69:235–50 [DOI] [PubMed] [Google Scholar]
- 55.Halbesleben JR, Wakefield DS, Ward MM, et al. The relationship between super users' attitudes and employee experiences with clinical information systems. Med Care Res Rev 2009;66:82–96 [DOI] [PubMed] [Google Scholar]
- 56.Locock L, Dopson S, Chambers D, et al. Understanding the role of opinion leaders in improving clinical effectiveness. Soc Sci Med 2001;53:745–57 [DOI] [PubMed] [Google Scholar]
- 57.Gaither CA, Bagozzi RP, Ascione FJ, et al. A reasoned action approach to physicians' utilization of drug information sources. Pharm Res 1996;13:1291–8 [DOI] [PubMed] [Google Scholar]
- 58.Succi MJ, Walter ZD. Theory of user acceptance of information technologies: An examination of health care professionals. In: Proceedings of the 32nd Annual Hawaii International Conference, 1999. Washington DC, USA: IEEE Computer Society, 1999 [Google Scholar]
- 59.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Mgmt Sci 2000;46:186–204 [Google Scholar]
- 60.Chau PYK, Hu PJH. Information technology acceptance by individual professionals: a model comparison approach. Decision Sci 2001;32:699–719 [Google Scholar]
- 61.Chismar WG, Wiley-Patton S. Test of the technology acceptance model for the internet in pediatrics. Proc AMIA Symp 2002;155–9 [PMC free article] [PubMed] [Google Scholar]
- 62.Gagnon MP, Godin G, Gagné C, et al. An adaptation of the theory of interpersonal behaviour to the study of telemedicine adoption by physicians. Int J Med Inf 2003;71:103–15 [DOI] [PubMed] [Google Scholar]
- 63.Wu JH, Shen WS, Lin LM, et al. Testing the technology acceptance model for evaluating healthcare professionals' intention to use an adverse event reporting system. Int J Qual Health Care 2008;20:123–9 [DOI] [PubMed] [Google Scholar]
- 64.Kuo D, Gifford DR, Stein MD. Curbside consultation practices and attitudes among primary care physicians and medical subspecialists. JAMA 1998;280:905–9 [DOI] [PubMed] [Google Scholar]
- 65.Beatty PC, Beatty SF. Anaesthetists'intentions to violate safety guidelines. Anaesthesia 2004;59:528–40 [DOI] [PubMed] [Google Scholar]
- 66.Ferlie E, Fitzgerald L, Wood M. Getting evidence into clinical practice: an organisational behaviour perspective. J Health Serv Res Policy 2000;5:96–102 [DOI] [PubMed] [Google Scholar]
- 67.Zheng K, Padman R, Johnson MP, et al. Evaluation of healthcare IT applications: the user acceptance perspective. In: Vaidya S, Jain LC, Yoshida H, eds. Advanced computational intelligence paradigms in healthcare. Heidelberg, Germany: Springer-Verlag, 2007;2:49–78 [Google Scholar]