Abstract
Purpose
Sarcopenia plays a principal role in the pathogenesis of frailty and functional impairment that occurs with aging. There are few published accounts which examine the overall benefit of resistance exercise (RE) for lean body mass (LBM), while considering a continuum of dosage schemes and/or age ranges. Therefore the purpose of this meta-analysis was to determine the effects of RE on LBM in older men and women, while taking these factors into consideration.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations. Randomized controlled trials and randomized or non-randomized studies among adults ≥ 50 years, were included. Heterogeneity between studies was assessed using the Cochran Q and I2 statistics, and publication bias was evaluated through physical inspection of funnel plots as well as formal rank-correlation statistics. Mixed-effects meta-regression was incorporated to assess the relationship between RE dosage and changes in LBM.
Results
Data from forty-nine studies, representing a total of 1328 participants were pooled using random-effect models. Results demonstrated a positive effect for lean body mass and there was no evidence of publication bias. The Cochran Q statistic for heterogeneity was 497.8, which was significant (p < 0.01). Likewise, I2 was equal to 84%, representing rejection of the null hypothesis of homogeneity. The weighted pooled estimate of mean lean body mass change was 1.1 kg (95% CI, 0.9 kg to 1.2 kg). Meta-regression revealed that higher volume interventions were associated (β = 0.05, p < 0.01) with significantly greater increases in lean body mass, whereas older individuals experienced less increase (β = -0.03, p = 0.01).
Conclusions
RE is effective for eliciting gains in lean body mass among aging adults, particularly with higher volume programs. Findings suggest that RE participation earlier in life may provide superior effectiveness.
Keywords: Strength Training, Systematic Review, Older Adults, Hypertrophy
Introduction
The term “sarcopenia” has emerged as a designation of non-specific vulnerability to weakness, disability, comorbidity, and general diminished autonomy among older adults. Although a robust relationship exists between chronological age and virtually every associated symptom, aging per se, is merely a crude proxy for determining scarcopenic risk. Complicating the ability to sufficiently diagnose early-onset vulnerability, declines are demonstrated to manifest as a gradual, often asymptomatic process for which the chief complaints rarely correspond with a subsequent diathesis for skeletal muscle atrophy. In particular, weakness and functional deficit have been considered hallmark predictors of age-related morbidity (12) and decreased autonomy. Moreover, age-related atrophy is often paralleled with increases in intermuscular adipose tissue (IMAT) infiltration and overall fat mass (i.e. “sarcopenic obesity”) (32, 92), inflammation, metabolic syndrome, arterial stiffness, and glucose intolerance (36, 93, 94). Sarcopenia represents a complex phenotype of numerous interrelated pathologies, exposures, and behaviors, and thus failure to prevent its progression may significantly increases risk of frailty and mobility disability (11, 58), and lead to losses of independence, increased health care costs, and overall reduced quality of life (30, 59).
Although the mechanisms for muscular hypertrophy and strength are to some extent distinct, resistance exercise (RE) is considered to be the preferred approach to elicit these adaptations for healthy adults (3). At present, there is a great deal of variability in the dose-response relationship reported in the literature, and the specific efficacy of RE for muscular adaptation is inconsistent across investigations. Several studies have demonstrated similar hypertrophic-responses between untrained, young- and middle-aged individuals and gender-matched elderly subjects (57, 77, 90), whereas others suggest greater adaptation among younger cohorts (65, 105).
Notwithstanding the extensive support for RE among aging adults (i.e. “Evidence Category A.”) (26), a systematic review to scrutinize treatment effects for LBM across multiple training dosages and potential mediating variables is yet to be completed. To date, the most comprehensive reviews related to this topic have limited the analysis of LBM as a secondary outcome, and/or have synthesized data from across combined cohorts of middle-aged and older adults (60-63). In such cases in which LBM was not the primary outcome, it is likely that many suitable studies would not have met inclusion criteria. Further, most meta-analytic evidence pertaining to RE for aging is specific to functional performance, disability, and/or strength outcomes (69, 74, 84, 85, 95). Those which have synthesized data for LBM have yielded conflicting results (60-63), and thus may obscure the true efficacy of RE to elicit adaptation. Such inconsistencies may also be due to variability in the control populations and/or differences in model covariates. It is certainly conceivable that RE would serve as a valuable preventive or treatment strategy in a clinical rehabilitation setting to promote increases in LBM. However, among aging adults there are very few published accounts which examine the overall benefit of RE, while considering a continuum of dosage schemes, treatment durations, and/or age ranges. Therefore the purpose of this meta-analysis was to determine the effects of RE on LBM in older men and women, while taking these factors into consideration.
Methods
This meta-analysis was conducted in accordance with the recommendations and criteria as outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (80). The respective procedures that were incorporated during this meta-analysis including the identification, screening, eligibility, and inclusion of studies, were all agreed upon between the authors in advance.
Types of studies and participants
Any randomized, controlled trials (RCTs) or clinical trials meeting the subsequent specifications were included. Nonrandomized studies (non-RCTs) that examined intervention treatments using stratified young versus older participants, or aged men versus women, were also eligible for inclusion in the analyses. Trials were included if the mean age of participants was over 50 years. Although sarcopenia for some individuals may occur prior to the fifth decade (73), most research pertaining to the treatment of sarcopenia or age-related general weakness is limited to older cut-offs (e.g. ≥ 50 years). This a priori criterion for age was chosen to include the largest possible age continuum of “older” adults. The 2007 American College of Sports Medicine (ACSM)/American Heart Association (AHA) joint recommendations for physical activity in older adults suggests that “old age” usually applies to individuals aged ≥ 65 years, but may also be relevant to adults aged ≥ 50 years who have limitations that affect movement, fitness or physical activity (82). Therefore, similar to previous reviews (68, 69), inclusion of participants with a range in age and health complications was critical to increase external validity and generalizability of results.
Types of interventions and outcome measures
Studies with one or more cohorts participating in RE were eligible for inclusion in the analysis. RE programs ranged from in-home or senior-citizen community programs, group exercise programs, and/or individual personal training arrangements. Resistance exercise was defined as a program that included specific training for the major muscle groups of the whole body (i.e. both upper- and lower-body) (See file, SDC 1, Additional detail pertaining to the resistance exercise protocols that were considered for inclusion in the analysis).
Study inclusion was limited to three discrete measurements of LBM: (1) hydrodensitometry, (2) whole body air plethysmography, and (3) Dual energy X-ray absorptiometry (DXA). These tests were selected due to their documented validity and reliability for assessments as well as reported prevalence in the literature. Other methods of assessing LBM such as anthropometric estimates (e.g. circumference and/or skinfold measures), bioelectrical impedance analysis (BIA), or near-infrared interactance were not included in the analysis.
Search Strategy and Study Identification
Computerized searches of MEDLINE, EMBASE, PubMed, Web of Science, SPORTDiscus™, Evidence Based Medicine Reviews Multifile (EBMR) databases, and Digital Dissertations (accessed May, June, and July 2009) from their inception to July, 2009 were undertaken. Hand-searching of key exercise and sports science, geriatrics/gerontology, and medicine (i.e. general and internal) journals, reference lists and other sources (e.g. exercise physiology texts and previous meta-analyses) was also undertaken. Studies published in foreign language journals were not included. Abstracts and citations from annual scientific conferences relating to exercise science or gerontology were not examined due to the paucity of requisite data. The preliminary search yielded over 5,000 relevant abstracts and citations. Full texts of over 400 articles were obtained and examined by the primary reviewer (MP) (See file, SDC 2, Subsequent detail pertaining to the search strategy and study identification. Specific permutations of the text keyword combinations and Medical Subject Headings (MeSH) terms are provided).
Study eligibility and data extraction
Each research article was expected to contain a supervised RE intervention, and include a detailed description of the requisite information, in order for inclusion. A study (or cohort) was excluded if the intervention was specifically designed to treat a given disorder or disease, if subjects were administered anabolic hormone replacement therapy during the course of the intervention, if subjects were not previously “untrained” (i.e. if subjects had been participating in RE within 6-months prior to the study), and/or if the subjects or treatment did not meet inclusion criteria (e.g. subjects < 50 years included, resistance exercise intervention lasted less than 8 weeks, resistance exercise was unsupervised, resistance exercise was not “whole body” protocol, etc.). A specific coding tool was developed to record information pertaining to the study source, participants, experimental characteristics, and outcomes. The coding tool was derived from elements coded in previous meta-analyses of health behavior, physical activity, and exercise, as well as suggestions from both meta-analysts and resistance exercise/physical activity experts. Although all eligible studies coded for data analyses in this investigation shared a common directive, several studies examined slightly different hypotheses. As an example, Hurlbut and colleagues (54) examined whether younger and older subjects experienced differential adaptation to RE. Thus, for studies that compared outcomes between young versus older participants, only data from the older participants were coded for analysis. For each included study, the author of correspondence was contacted to obtain any missing information/data. In the event that authors could not be reached, or if the data were no longer available, the trial was not included in the meta-analyses.
Intervention operational definitions
Volume: Volume of training referred to the total number of work sets performed per session (i.e. not including warm-up sets). Since the purpose of this analysis was to examine the effectiveness of whole body RE on LBM, volume of training per whole body was considered to be an important variable. Therefore, training programs which isolated one part of the body or muscle group were not included in the analysis. There has been substantial debate concerning the appropriate operational definition of training volume within the resistance exercise literature, making this a difficult parameter to evaluate and replicate in research. A widely accepted definition for this variable is volume load (VL), which takes into account the total number of performed sets, repetitions and weight (kg) lifted (i.e. (total repetitions [no.] × external load [kg]). Although this is a readily used volume classification, published RE manuscripts do not generally include total VL as a prescription entity, and/or do not provide ample data (i.e. exact number of repetitions performed and/or exact absolute load lifted) for a meta-analyst to compute total VL for each individual training intervention. Therefore, total number of sets performed per whole body was considered to be an appropriate surrogate index of the absolute volume of physiologic stress. Frequency: Training frequency was defined as the occurrence, per unit of time (e.g. calendar week) that a full-body RE regimen was completed. In some instances, interventions which incorporated higher-volume training were partitioned to accommodate greater overall time requirements. For example, full body training, which is often prescribed two to three days per week, may be divided into two upper- and two lower-body training sessions per week (four total sessions). In this example, even though training manifested over four days, the frequency of training was still coded as 2 days (i.e. the full-body was trained twice, in a given week). Intensity: Intensity of training was defined as the percentage of one repetition maximum used for a given exercise. This operational definition for training intensity generates an objective, quantifiable unit, which is contrary to the more subjective measure of training fatigue or rating of perceived exertion.
Assessment of reviewer agreement
Inter-reviewer disagreements were resolved by consensus. The agreement rate prior to amending any such discrepancies was assessed using the kappa statistic (33), and determined to be 0.94. Two reviewers worked independently and screened titles and abstracts for eligibility. Potential references were retrieved in full text for evaluation against eligibility criteria. The kappa statistic was used to evaluate the chance adjusted inter-reviewer agreement about study eligibility (i.e. eligible or not eligible). In the case of inadequate information contained in the manuscript, the lead reviewer (MP) sought clarification from study authors.
Tests for Publication Bias and Heterogeneity
To examine for evidence of publication bias, visual inspection of Begg's funnel plots occurred (13). This process included the examination of scatterplots for LBM plotted against its standard error. As a formal check for publication bias, the tests of Begg and Mazumdar (14) and of Egger et al. (35) were implemented. The Egger's publication bias test quantifies the bias captured by the funnel plot, and more specifically, the standardized effect is regressed on precision (i.e. inverse of standard error) (18). These formal statistics are used to evaluate the same assumption as the Begg's test, and may be incorporated as a cross-check to the physical inspection of the scatter plots.
Heterogeneity between studies was assessed using the Cochran Q statistic (28). The Cochran Q uses the sum of squared deviations of the study-specific estimates derived from the pooled estimate, and weights the contribution of each study. Probability values were obtained by comparing the Q statistic with a χ2 distribution with k-1 degrees of freedom, in which k represents the number of studies included. Since heterogeneity is to a certain extent, inevitable in meta-analytic research, there is ample debate regarding the utility of assigning statistical significance to this computation. Thus we also incorporated the I2 statistic, using the following equation:
This procedure quantifies the proportion of variability in the trial results that are a function of heterogeneity, rather than chance (48, 49). With this method I2 ranges from 0% - 100% such that 0% reflects homogeneity and 100% is indicative of meaningful heterogeneity.
Standard Deviations
Treatment effects for LBM were calculated for each study following the extraction/coding of change scores and standard deviations. Specifically, the standard deviation (SD) of change was needed to calculate the effect size, and for many of the studies this value was not reported. Rather, the majority of studies obtained for this analysis included the SDs for the baseline and postintervention LBM outcomes, or in many cases the standard errors of the mean. In the event that the study reported exact P values for the change in LBM outcome, the SD of change was computed. However, for those studies which did not report exact P values the SD of change was calculated using the baseline and post-intervention SDs, as well as the within-participant bivariate correlation of LBM measures using the following equation:
For every article included, authors were contacted in an effort to retrieve SD change outcomes, the raw data for the calculation of the within-participant baseline and postintervention LBM correlations, or the specific and respective r (correlation) values. If an author could not be reached, an assumption was made that the bivariate correlation was similar across interventions. This strategy, which has been recommended by Follmann and colleagues (38) and previously used in published meta-analyses (88), allows for the computation of effect sizes for all cohorts included in a review. A within-participant correlation of r = 0.96 was used, which was derived through exact calculation from 16 of the included cohorts (44, 46, 51, 53, 56, 72, 87, 89, 96).
Effect Sizes
The analysis of pooled data was conducted with a fixed and random-effects model. While there is debate regarding the appropriate use of a fixed- or random-effects model when calculating summary estimates (47), these models generally provide similar estimates unless heterogeneity is present among the studies. In the context of analyzing resistance exercise interventions for LBM we decided that a random-effects model was a more suitable method as it decreased the risk of a type I error, and because it assumed variability among included trials. A forest plot was generated to illustrate the study-specific effect sizes along with 95% confidence intervals (CI). Combining estimates then allowed for the assessment of a pooled effect, as has been previously described (88), in which the reciprocal of the sum of two variances were accounted for including: (1) the estimated variance associated with the study, and (2) the estimated component of variance due to variation between studies. In each study, the effect size for the intervention was calculated by the difference between the means of the post-test and pre-test at the end of the intervention. The study-specific weights were derived as the inverse of the square of the respective standard errors. All statistical analyses were performed using STATA 10.0 (StataCorp LP, College Station, Texas), MINITAB 14.0 (Minitab Inc, State College, Pennsylvania), and SAS 9.2 (SAS Institute Inc., Cary, NC).
Meta-Regression and Influence Analysis
A weighted, sub-group multiple meta-regression was performed with a mixed-effects model (specified a priori), to examine the association between age, study duration, resistance training variables (i.e. training intensity, volume, frequency), type of LBM assessment, and study design (i.e. RCT versus non-RCT) with changes in LBM. For this analysis, each of the aforementioned potential predictors was entered into a model as fixed effects, and the subsequent assessment was considered to be a random effect.
To assess the influence of individual studies on the overall estimate of LBM change, we conducted an influence analysis. Using this analysis, the estimates were computed, omitting a single study in each cycle.
Results
The flow of article search and selection, from “potentially relevant” to final inclusion is depicted in Figure 1.
Figure 1.
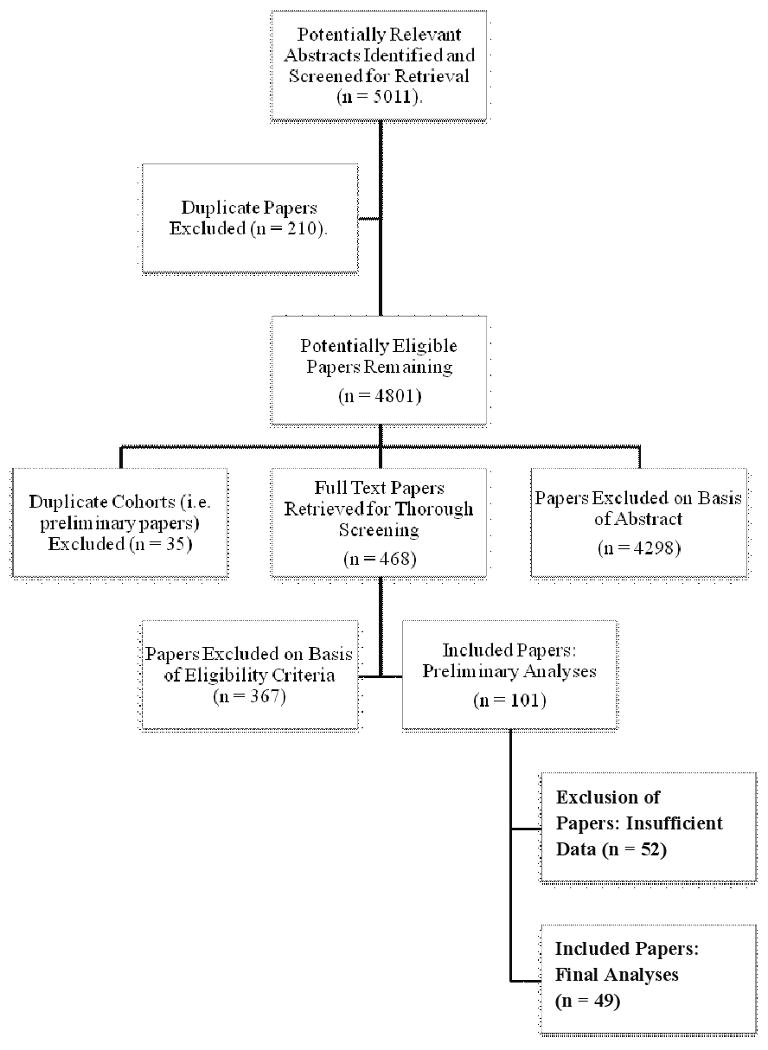
Flow of papers through the review process.
Study Characteristics
Of the 5011 references screened, 49 studies with 81 cohorts were deemed eligible according to the inclusion criteria. Of the included articles, the publication dates ranged from 1990 to 2009. Thirty-seven percent of the studies included random assignment of treatment conditions as well as control groups (RCT) (4, 5, 15, 17, 19, 20, 24, 25, 34, 37, 46, 53, 56, 72, 76, 96, 98, 100, 102). The remaining studies were classified as non-RCTs (6, 9, 10, 21-23, 27, 31, 39-41, 44, 51, 52, 54-56, 64, 70, 71, 75, 79, 81, 86, 87, 89-91, 97, 99, 107), of which six studies assessed a single cohort of older men (21, 23, 27, 64, 79, 86), four studies assessed a single cohort of older women (41, 56, 91, 99), nine studies compared the effects of training on men versus women (6, 10, 31, 39, 51, 75, 81, 97, 107), eight studies assessed the effects of combined older men and women (9, 22, 40, 44, 52, 55, 87, 89), and four studies assessed four groups, including young/middle-aged women, young/middle-aged men, older women, and older men (54, 70, 71, 90).
Subject Characteristics
Data on 1328 subjects were included in the analysis (Table 1: Supplementary Materials). The age range for subjects was between 50 and 83, with the mean age of the subjects in the majority of studies falling between 60 and 75 (mean = 65.5 ± 6.5 years). A large percentage of the assigned cohorts consisted of male and female combined groups (30 cohorts) (9, 15, 17, 19, 22, 24, 25, 34, 40, 44, 46, 52, 53, 55, 71, 72, 87, 89, 96, 101, 102), with the remaining distributed in male (23 cohorts) (4, 6, 10, 21, 23, 27, 31, 39, 51, 54, 64, 70, 75, 76, 79, 81, 86, 90, 97, 100, 107) and/or female only (28 cohorts) (4-6, 10, 20, 31, 37, 39, 41, 51, 54, 56, 70, 75, 76, 81, 90, 91, 97-99, 107) cohorts.
Treatment Characteristics
Length of training ranged from 10 to 52 weeks (mean duration = 20.5 ± 9.1 weeks), frequency from 2 to 3 times per week (mean = 2.8 ± 0.4 days/week), and intensity from 50% to 80% of 1 repetition maximum (mean = 74.6% ± 6.9 1RM). The number of sets per exercise session ranged from 7-39 (i.e. per the full-body program) (mean = 20 ± 7.3 sets), while the number of exercises performed ranged from 5-16 (mean = 8.3 ± 2.1 resistance training exercises). The within-group number of repetitions performed for each set ranged between 2 and 20 (mean = 10 repetitions), while the rest period between sets ranged from 60 to 360 seconds (mean = 110 seconds) (See Table, SDC 3: Specific detail pertaining to the important characteristics of each study included in the analysis.). Compliance, defined as the percentage of exercise sessions attended, ranged from 80 to 100% (mean = 87.2 ± 3.4%).
Publication Bias and Heterogeneity
The tests used to inspect for evidence of publication bias revealed no such bias. Examination of the Begg's funnel plots (Figure 2) demonstrated considerable symmetry, suggesting that there was no significant publication bias. Results from Begg's rank-correlation (p = 0.10) and Egger's (p = 0.26) tests further confirmed no evidence of publication bias.
Figure 2.
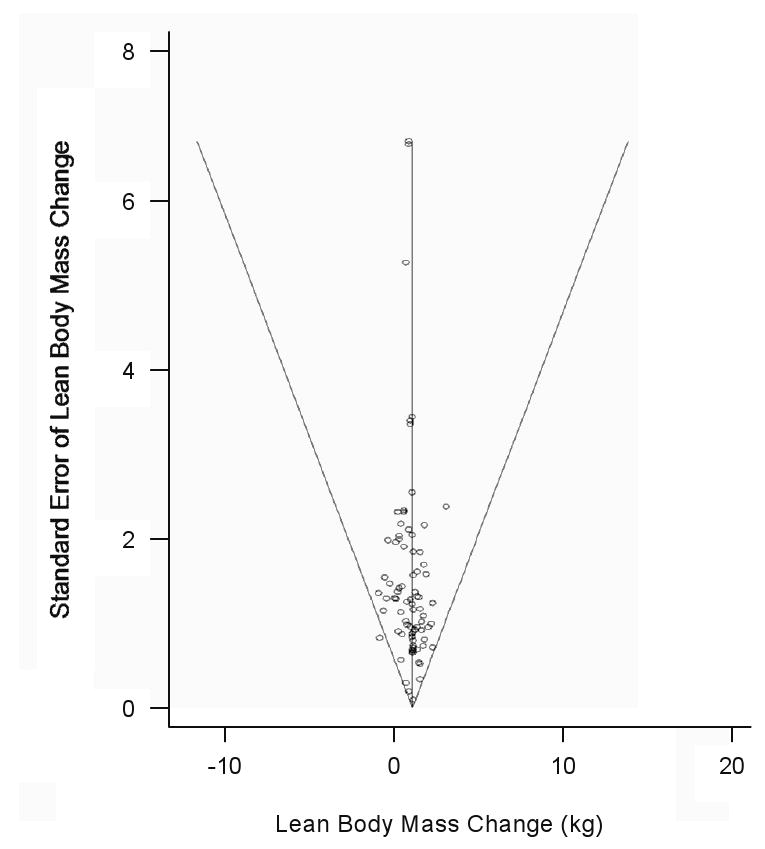
Begg's funnel plot for lean body mass, with 95% confidence limits. No evidence of publication bias was detected.
The Cochran Q statistic for heterogeneity was 497.8. Based on a chi squared (χ2) with 80 degrees of freedom, this was significant (p < 0.01). Further, I2 was 84% indicating rejection of the null hypothesis of homogeneity (49).
Intervention Effect
Many trials reported data from more than a single cohort (Table 1: SDC 3). The pooled estimate of LBM change from baseline to postintervention, combining data from 81 treatment cohorts (49 studies) was 1.1 kg (95% CI, 0.9 kg to 1.2 kg) (p < 0.001). A forest plot of the main effects for LBM as well as CIs for all 81 cohorts is provided in Figure 3. Results from the influence analysis demonstrated that removal/omission of any individual study did not alter the summary effects and 95% CIs.
Figure 3.
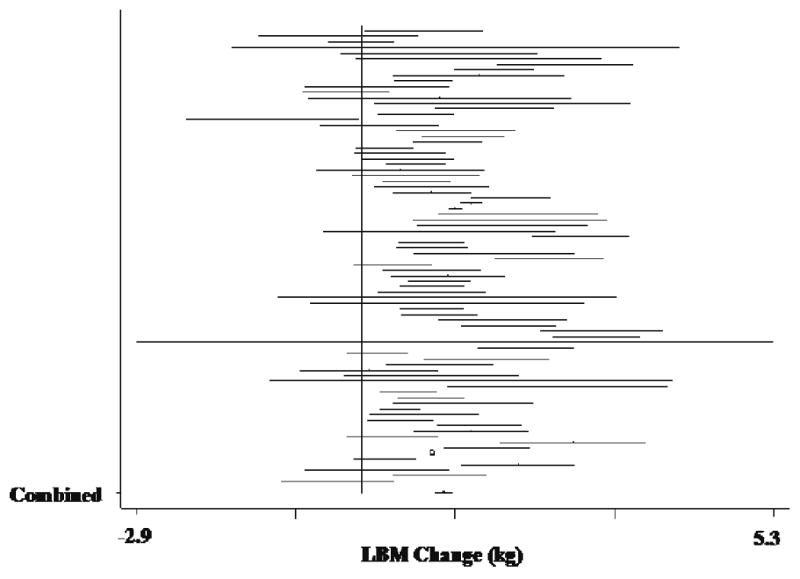
Forest plot of effect sizes and 95% confidence intervals for all 83 cohorts (50 studies) representing lean body mass, based on the fixed effects meta-analysis results.
Meta Regression
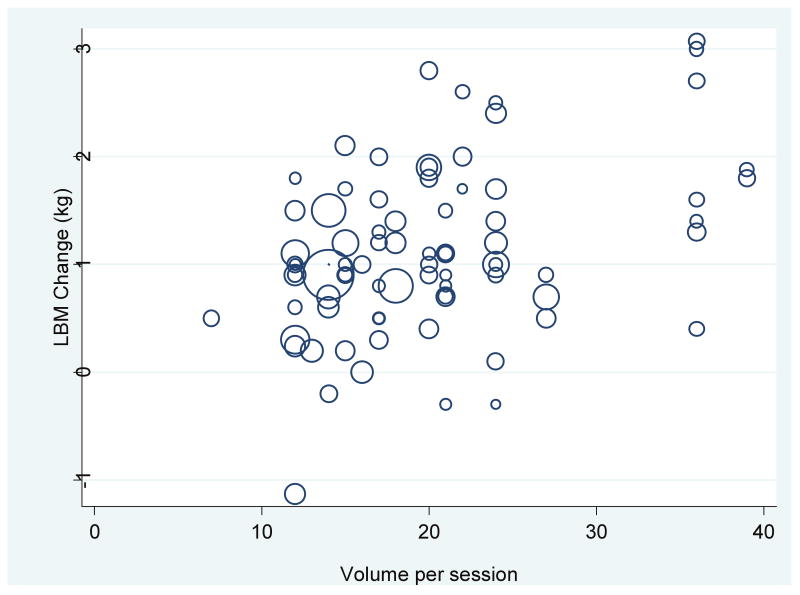
Using multiple meta-regression a strong linear association was determined between the volume of training (i.e. controlling for age, study duration, type of LBM assessment, study design, gender, training intensity, and frequency) and the magnitude of the LBM change (β = 0.05, p < 0.01), with higher volume interventions being associated with greater LBM increases (Figure 4). Further, age was associated with LBM increase (β = -0.03, p = 0.01), such that older men and women experienced less gain. Gender, intervention duration, study design, and differences in training intensity and frequency were not significantly associated with changes in LBM (p > 0.05).
Figure 4.
Lean Body Mass Change by Training Volume (sets per session), weighted by number of subjects in the study.
Discussion
Data derived from 49 studies and 81 cohorts verified a robust association between full body RE and increased LBM. Analysis revealed that after an average of 20.5-weeks of RE, aging men and women experienced a significant main effect equal to a 1.1-kilogram increase in LBM. These findings bear clinical significance, given the exaggerated rate of skeletal muscle atrophy that occurs among sedentary individuals after the age of fifty (78). As such declines appear to precipitate a heightened risk for functional disabilities, including deficits in strength, gait, mobility, and essential activities of daily living (78), preservation or increases in lean muscle mass through RE may serve as a powerful treatment/preventive strategy.
The examination in LBM is a readily attainable and usable parameter related to pathology, as well as a practical surrogate predictor of weakness and/or functional deficit. However, the net change of LBM is not a sufficient index to quantify hypertrophic/atrophic alterations of skeletal muscle, particularly over the short term. Measurement of LBM provides no specific detail regarding changes in single fiber cross-sectional area, muscle volume, satellite cell concentration/differentiation, or architectural modifications (e.g. changes in pennation angle and sarcomere length), all of which represent vital morphological characteristics associated with muscular functional capacity. For this analysis, it is plausible that such biomolecular changes would not be adequately reflected through a gross aggregate such as LBM. Case in point, numerous studies have confirmed significant hypertrophic and architectural responses among aging men and women following short bouts of RE, despite negligible or nonsignificant changes in LBM (42, 43, 45). Certainly these data, which are generally ascertained through histochemical and/or precise imaging techniques, provide superior mechanistic indices of adaptation. However, at present the collection of such data is not considered to be practical in a clinical setting. Therefore, the measurement of LBM may continue to serve as a viable proxy for diagnosis and/or observation of outcomes within longitudinal interventions or translational directives.
Results from the meta-regression identified volume of training as a significant predictor of LBM. These findings suggest that higher volumes of RE are associated with greater increases in LBM. While volume ranged from 7-39 total sets per session (for whole-body RE), the majority of included studies conformed to the original American College of Sports Medicine recommendations for resistance exercise in older adults (i.e. 8-10 exercises for 1-2 sets of full body RE) (1). Subsequent results from the meta-regression did not identify any significant relationships between program duration, intensity or frequency, and subsequent changes in LBM. It is conceivable that the overall lack of variability in training regimens across program models may have confounded these results. However, of the various RE prescription components, volume of resistance exercise has received the greatest attention with regard to effectiveness and risk-reward. In essence, if the effort-to-benefit ratio does not warrant progression in volume to accommodate increases in muscular adaptation, then the opportunity cost of performing higher dosage RE over other functional directives, e.g. balance exercise, cardiovascular/aerobic exercise, flexibility/stretching, etc. would not be justified. This is the first comprehensive, meta-analysis to confirm a significant positive association between RE volume and LBM in aging men and women. Single-set and/or fixed-volume RE programs may no longer be considered sufficient for individuals seeking progressive adaptations in LBM.
Current exercise recommendations are dissimilar for young and middle-aged healthy adults (3, 66), as compared to those for elderly populations (2, 26, 83), particularly for RE prescription. The majority of studies and subsequent recommendations for young, healthy adults have incorporated models of periodization to promote enhanced adaptation of muscle mass and fitness, whereas no such suggestions have been endorsed for the aging population. Periodization schemes call for a multidimensional approach to progressing and alternating training variables and subsequent recovery over set blocks of time, as well as systematic “non-linear” manipulation of dosages (i.e. “daily undulating periodization) to accommodate adaptations in muscular fitness (3). Based on current data, it appears that in order to facilitate progressive adaptation in LBM, it is necessary to increase the prescription dosage as individuals become more familiarized with training. In essence, merely increasing training load over time may not be sufficient beyond a certain point, as this represents an inevitable reliance on the same relative intensity. Thus, progression models for resistance training among older adults should include a systematic manipulation of volume to accommodate chronic adaptation in LBM (85).
Meta-regression also identified a negative association between age and LBM main effects. Therefore, although significant hypertrophy is possible in the “oldest old” (67), it may be expected that the benefits of early RE participation will translate to superior increases in LBM, and thus preservation of muscle function and instrumental activities of daily living, prevention of disability, and maintenance of independence. However, as a cautionary statement it should be noted that the majority of these current data were derived from healthy older adults. Indeed, more research is warranted to ascertain the influence of RE for specific disease outcomes, and across a broad spectrum of physical abilities/limitations. Previous research pertaining to efficacy of RE on hypertrophy among aging adults has demonstrated that despite a diminished pre-exercise rate (7, 103, 104, 106), significant increases in protein synthesis are indeed possible through higher volume, progressive RE (90, 108). While current data are reflective of this phenomenon, additional research is warranted to investigate the dose-response relationship between RE and adaptation-potential for fiber-specific hypertrophy, muscle quality, LBM, and changes in protein synthesis across a continuum of ages. To date, the most comprehensive review on RE for the primary outcome of “muscle pathology” (i.e. cross-sectional area, fiber area, or mass, as derived by imaging techniques) has suggested moderate- large (0.5-0.79) effect sizes for muscle hypertrophy (Type II fiber area, d = 0.71) (50).
Previous published meta-analyses which have included LBM as a secondary outcome were conducted on adults of various age ranges, and have demonstrated inconsistent findings. Specifically, effect size data vary from non-significant differences (treatment − control) in men (63) and premenopausal women (61), to significant differences of 1 to 4 kg (60, 62). For the current analysis, we included thirty-two studies that were not RCT designs, and thus, it was impossible to ascertain a treatment-control effect size calculation. Rather, we examined effect sizes from pre- to postintervention. Many meta-analyses employ only RCTs. However, there have been several recent reviews which have demonstrated no differences in effect sizes between studies with different designs (16, 29), and there is ample debate regarding the value of this quality indicator for meta-analysis study inclusion (8).
Further regarding the issue of assessing indicators of study “quality,” no acceptable scale currently exists for examining the quality of resistance exercise intervention research. According to the recently updated Cochrane Collaboration guidelines for systematic reviews, there is a general recommendation against the use of quality scales in such situations, due to an overall lack supporting evidence and validity (47). Therefore, sub-analysis for overall study quality was not carried out for the current investigation, although previous reviews have reported an overall lack of quality among the majority of resistance training literature for older adults (69). As has been suggested in these reviews, future RE research should be designed to accommodate increased internal validity, and include such features as intention to treat analysis, blinded assessors, attention control groups, and concealed randomization. The gradual acceptance of RE as a viable preventive or treatment strategy will inevitably lead to larger samples from which to recruit, and ultimately to higher quality RCTs. Therefore, it may be necessary to eventually conceptualize a specific quality rating scale for RE interventions, as such a scale would be valuable for future refinement of evidence-based RE recommendations.
As with all meta-analyses, a general limitation to the generalizability of findings is that data do not infer a causal effect. Since sarcopenia is a collection of interrelated deteriorations that occurs on a gradual basis during the aging progression, the capacity to increase LBM through participation in RE represents an effective preventive strategy to complement other behavioral interventions. However as sarcopenia is strongly related to muscular weakness, dysfunction, and disease comorbidity, certainly more translational studies are warranted to directly examine treatment options for these consequences. Nevertheless, we have also identified through meta-analyses that RE in older adults has significant value for strength outcomes (85). Collectively, these findings support the efficacy of RE as an important public health directive that may positively influence quality of life and independence for elderly individuals.
Conclusions
The results of the current meta-analysis suggest that RE elicits an approximate 1kg increase in LBM among older adults. Although modest compared to the expected adaptation with healthy young adults, this increase is in contrast to the 0.18 kg annual decline that may occur (78) through sedentary lifestyles, beyond fifty years of age. Moreover, volume of training and age of participation are important determinants of effectiveness, suggesting that higher dosages result in greater adaptive-response, and that aging individuals should consider starting a regimen of resistance exercise as early as possible, to optimize results. These findings expand upon current recommendations, which merely suggest an increase in training load, to accommodate fitness improvements.
Supplementary Material
This SDC contains continued/additional detail pertaining to the resistance exercise protocols that were considered for inclusion in the analysis.
This SDC contains continued/additional detail pertaining to the search strategy and study identification. Specific permutations of the text keyword combinations and Medical Subject Headings (MeSH) terms are provided.
This SDC table contains detail pertaining to the important characteristics of each study included in the analysis.
Acknowledgments
Dr. Mark Peterson is supported by the NIH, NICHD, NCMRR Grant #5-T32-HD007422-17. The results of the present study do not constitute endorsement by ACSM.
Footnotes
Disclosure of Funding: No financial disclosures are reported by the authors of this paper.
Conflict of Interest Statement: There are no reported conflicts of interest.
Publisher's Disclaimer: Medicine & Science in Sports & Exercise® Published ahead of Print contains articles in unedited manuscript form that have been peer reviewed and accepted for publication. This manuscript will undergo copyediting, page composition, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered that could affect the content.
References
- 1.ACSM. American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30:992–1008. [PubMed] [Google Scholar]
- 2.ACSM. American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 3.ACSM. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41:687–708. doi: 10.1249/MSS.0b013e3181915670. [DOI] [PubMed] [Google Scholar]
- 4.Ades PA, Ballor DL, Ashikaga T, Utton JL, Nair KS. Weight training improves walking endurance in healthy elderly persons. Ann Intern Med. 1996;124:568–572. doi: 10.7326/0003-4819-124-6-199603150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Ades PA, Savage PD, Brochu M, Tischler MD, Lee NM, Poehlman ET. Resistance training increases total daily energy expenditure in disabled older women with coronary heart disease. J Appl Physiol. 2005;98:1280–1285. doi: 10.1152/japplphysiol.00360.2004. [DOI] [PubMed] [Google Scholar]
- 6.Andrews RD, MacLean DA, Riechman SE. Protein intake for skeletal muscle hypertrophy with resistance training in seniors. Int J Sport Nutr Exerc Metab. 2006;16:362–372. doi: 10.1123/ijsnem.16.4.362. [DOI] [PubMed] [Google Scholar]
- 7.Balagopal P, Rooyackers OE, Adey DB, Ades PA, Nair KS. Effects of aging on in vivo synthesis of skeletal muscle myosin heavy-chain and sarcoplasmic protein in humans. Am J Physiol. 1997;273:E790–800. doi: 10.1152/ajpendo.1997.273.4.E790. [DOI] [PubMed] [Google Scholar]
- 8.Balk EM, Bonis PA, Moskowitz H, Schmid CH, Ioannidis JP, Wang C, Lau J. Correlation of quality measures with estimates of treatment effect in meta-analyses of randomized controlled trials. Jama. 2002;287:2973–2982. doi: 10.1001/jama.287.22.2973. [DOI] [PubMed] [Google Scholar]
- 9.Ballor DL, Harvey-Berino JR, Ades PA, Cryan J, Calles-Escandon J. Contrasting effects of resistance and aerobic training on body composition and metabolism after diet-induced weight loss. Metabolism. 1996;45:179–183. doi: 10.1016/s0026-0495(96)90050-5. [DOI] [PubMed] [Google Scholar]
- 10.Bamman MM, Hill VJ, Adams GR, Haddad F, Wetzstein CJ, Gower BA, Ahmed A, Hunter GR. Gender differences in resistance-training-induced myofiber hypertrophy among older adults. J Gerontol A Biol Sci Med Sci. 2003;58:108–116. doi: 10.1093/gerona/58.2.b108. [DOI] [PubMed] [Google Scholar]
- 11.Bauer JM, Sieber CC. Sarcopenia and frailty: a clinician's controversial point of view. Exp Gerontol. 2008;43:674–678. doi: 10.1016/j.exger.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev. 1999;107:123–136. doi: 10.1016/s0047-6374(98)00130-4. [DOI] [PubMed] [Google Scholar]
- 13.Begg CB, Berlin JA. Publication bias and dissemination of clinical research. J Natl Cancer Inst. 1989;81:107–115. doi: 10.1093/jnci/81.2.107. [DOI] [PubMed] [Google Scholar]
- 14.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 15.Beniamini Y, Rubenstein JJ, Faigenbaum AD, Lichtenstein AH, Crim MC. High-intensity strength training of patients enrolled in an outpatient cardiac rehabilitation program. J Cardiopulm Rehabil. 1999;19:8–17. doi: 10.1097/00008483-199901000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342:1878–1886. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 17.Binder EF, Yarasheski KE, Steger-May K, Sinacore DR, Brown M, Schechtman KB, Holloszy JO. Effects of progressive resistance training on body composition in frail older adults: results of a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:1425–1431. doi: 10.1093/gerona/60.11.1425. [DOI] [PubMed] [Google Scholar]
- 18.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to Meta-Analysis. Hoboken, NJ: Wiley; 2009. p. 421. [Google Scholar]
- 19.Borst SE, Vincent KR, Lowenthal DT, Braith RW. Effects of resistance training on insulin-like growth factor and its binding proteins in men and women aged 60 to 85. J Am Geriatr Soc. 2002;50:884–888. doi: 10.1046/j.1532-5415.2002.50215.x. [DOI] [PubMed] [Google Scholar]
- 20.Brochu M, Savage P, Lee M, Dee J, Cress ME, Poehlman ET, Tischler M, Ades PA. Effects of resistance training on physical function in older disabled women with coronary heart disease. J Appl Physiol. 2002;92:672–678. doi: 10.1152/japplphysiol.00804.2001. [DOI] [PubMed] [Google Scholar]
- 21.Campbell WW, Barton ML, Jr, Cyr-Campbell D, Davey SL, Beard JL, Parise G, Evans WJ. Effects of an omnivorous diet compared with a lactoovovegetarian diet on resistance-training-induced changes in body composition and skeletal muscle in older men. Am J Clin Nutr. 1999;70:1032–1039. doi: 10.1093/ajcn/70.6.1032. [DOI] [PubMed] [Google Scholar]
- 22.Campbell WW, Crim MC, Young VR, Joseph LJ, Evans WJ. Effects of resistance training and dietary protein intake on protein metabolism in older adults. Am J Physiol. 1995;268:E1143–1153. doi: 10.1152/ajpendo.1995.268.6.E1143. [DOI] [PubMed] [Google Scholar]
- 23.Candow DG, Chilibeck PD, Facci M, Abeysekara S, Zello GA. Protein supplementation before and after resistance training in older men. Eur J Appl Physiol. 2006;97:548–556. doi: 10.1007/s00421-006-0223-8. [DOI] [PubMed] [Google Scholar]
- 24.Cassilhas RC, Viana VA, Grassmann V, Santos RT, Santos RF, Tufik S, Mello MT. The impact of resistance exercise on the cognitive function of the elderly. Med Sci Sports Exerc. 2007;39:1401–1407. doi: 10.1249/mss.0b013e318060111f. [DOI] [PubMed] [Google Scholar]
- 25.Castaneda C, Layne JE, Munoz-Orians L, Gordon PL, Walsmith J, Foldvari M, Roubenoff R, Tucker KL, Nelson ME. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care. 2002;25:2335–2341. doi: 10.2337/diacare.25.12.2335. [DOI] [PubMed] [Google Scholar]
- 26.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, Skinner JS. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 27.Chrusch MJ, Chilibeck PD, Chad KE, Davison KS, Burke DG. Creatine supplementation combined with resistance training in older men. Med Sci Sports Exerc. 2001;33:2111–2117. doi: 10.1097/00005768-200112000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Cochran W. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. [Google Scholar]
- 29.Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342:1887–1892. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. doi: 10.1093/ageing/afq034. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Delmonico MJ, Ferrell RE, Meerasahib A, Martel GF, Roth SM, Kostek MC, Hurley BF. Blood pressure response to strength training may be influenced by angiotensinogen A-20C and angiotensin II type I receptor A1166C genotypes in older men and women. J Am Geriatr Soc. 2005;53:204–210. doi: 10.1111/j.1532-5415.2005.53104.x. [DOI] [PubMed] [Google Scholar]
- 32.Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, Boudreau R, Manini TM, Nevitt M, Newman AB, Goodpaster BH. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–1585. doi: 10.3945/ajcn.2009.28047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Donner A, Klar N. The statistical analysis of kappa statistics in multiple samples. J Clin Epidemiol. 1996;49:1053–1058. doi: 10.1016/0895-4356(96)00057-1. [DOI] [PubMed] [Google Scholar]
- 34.Dunstan DW, Daly RM, Owen N, Jolley D, De Courten M, Shaw J, Zimmet P. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care. 2002;25:1729–1736. doi: 10.2337/diacare.25.10.1729. [DOI] [PubMed] [Google Scholar]
- 35.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- 37.Figueroa A, Going SB, Milliken LA, Blew RM, Sharp S, Teixeira PJ, Lohman TG. Effects of exercise training and hormone replacement therapy on lean and fat mass in postmenopausal women. J Gerontol A Biol Sci Med Sci. 2003;58:266–270. doi: 10.1093/gerona/58.3.m266. [DOI] [PubMed] [Google Scholar]
- 38.Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45:769–773. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- 39.Galvão D, Taaffe D. Does sex affect the muscle strength and regional lean tissue mass response to resistance training in older adults? Int J Sport & Health Sci. 2006;4:36–43. [Google Scholar]
- 40.Galvão DA, Taaffe DR. Resistance exercise dosage in older adults: single- versus multiset effects on physical performance and body composition. J Am Geriatr Soc. 2005;53:2090–2097. doi: 10.1111/j.1532-5415.2005.00494.x. [DOI] [PubMed] [Google Scholar]
- 41.Goulet ED, Melancon MO, Dionne IJ, Aubertin-Leheudre M. No sustained effect of aerobic or resistance training on insulin sensitivity in nonobese, healthy older women. J Aging Phys Act. 2005;13:314–326. doi: 10.1123/japa.13.3.314. [DOI] [PubMed] [Google Scholar]
- 42.Hakkinen K, Kallinen M, Linnamo V, Pastinen UM, Newton RU, Kraemer WJ. Neuromuscular adaptations during bilateral versus unilateral strength training in middle-aged and elderly men and women. Acta Physiol Scand. 1996;158:77–88. doi: 10.1046/j.1365-201X.1996.523293000.x. [DOI] [PubMed] [Google Scholar]
- 43.Hakkinen K, Kraemer WJ, Newton RU, Alen M. Changes in electromyographic activity, muscle fibre and force production characteristics during heavy resistance/power strength training in middle-aged and older men and women. Acta Physiol Scand. 2001;171:51–62. doi: 10.1046/j.1365-201X.2001.00781.x. [DOI] [PubMed] [Google Scholar]
- 44.Hartman MJ, Fields DA, Byrne NM, Hunter GR. Resistance training improves metabolic economy during functional tasks in older adults. J Strength Cond Res. 2007;21:91–95. doi: 10.1519/00124278-200702000-00017. [DOI] [PubMed] [Google Scholar]
- 45.Haub MD, Wells AM, Tarnopolsky MA, Campbell WW. Effect of protein source on resistive-training-induced changes in body composition and muscle size in older men. Am J Clin Nutr. 2002;76:511–517. doi: 10.1093/ajcn/76.3.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008;63:83–91. doi: 10.1093/gerona/63.1.83. [DOI] [PubMed] [Google Scholar]
- 47.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009] The Cochrane Collaboration. 2009 Available from www.cochrane-handbook.org.
- 48.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 49.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huber G. The Effect of Resistance training on disablement outcomes: a meta-analysis. University of Illinois; Chicago, IL: 2005. p. 124. Dissertation. [Google Scholar]
- 51.Hunter GR, Bryan DR, Wetzstein CJ, Zuckerman PA, Bamman MM. Resistance training and intra-abdominal adipose tissue in older men and women. Med Sci Sports Exerc. 2002;34:1023–1028. doi: 10.1097/00005768-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 52.Hunter GR, Wetzstein CJ, Fields DA, Brown A, Bamman MM. Resistance training increases total energy expenditure and free-living physical activity in older adults. J Appl Physiol. 2000;89:977–984. doi: 10.1152/jappl.2000.89.3.977. [DOI] [PubMed] [Google Scholar]
- 53.Hunter GR, Wetzstein CJ, McLafferty CL, Jr, Zuckerman PA, Landers KA, Bamman MM. High-resistance versus variable-resistance training in older adults. Med Sci Sports Exerc. 2001;33:1759–1764. doi: 10.1097/00005768-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 54.Hurlbut DE, Lott ME, Ryan AS, Ferrell RE, Roth SM, Ivey FM, Martel GF, Lemmer JT, Fleg JL, Hurley BF. Does age, sex, or ACE genotype affect glucose and insulin responses to strength training? J Appl Physiol. 2002;92:643–650. doi: 10.1152/japplphysiol.00499.2001. [DOI] [PubMed] [Google Scholar]
- 55.Iglay HB, Thyfault JP, Apolzan JW, Campbell WW. Resistance training and dietary protein: effects on glucose tolerance and contents of skeletal muscle insulin signaling proteins in older persons. Am J Clin Nutr. 2007;85:1005–1013. doi: 10.1093/ajcn/85.4.1005. [DOI] [PubMed] [Google Scholar]
- 56.Igwebuike A, Irving BA, Bigelow ML, Short KR, McConnell JP, Nair KS. Lack of dehydroepiandrosterone effect on a combined endurance and resistance exercise program in postmenopausal women. J Clin Endocrinol Metab. 2008;93:534–538. doi: 10.1210/jc.2007-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ivey FM, Roth SM, Ferrell RE, Tracy BL, Lemmer JT, Hurlbut DE, Martel GF, Siegel EL, Fozard JL, Jeffrey Metter E, Fleg JL, Hurley BF. Effects of age, gender, and myostatin genotype on the hypertrophic response to heavy resistance strength training. J Gerontol A Biol Sci Med Sci. 2000;55:M641–648. doi: 10.1093/gerona/55.11.m641. [DOI] [PubMed] [Google Scholar]
- 58.Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–896. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- 59.Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52:80–85. doi: 10.1111/j.1532-5415.2004.52014.x. [DOI] [PubMed] [Google Scholar]
- 60.Kelley GA, Kelley KS. Progressive resistance exercise and resting blood pressure : A meta-analysis of randomized controlled trials. Hypertension. 2000;35:838–843. doi: 10.1161/01.hyp.35.3.838. [DOI] [PubMed] [Google Scholar]
- 61.Kelley GA, Kelley KS. Efficacy of resistance exercise on lumbar spine and femoral neck bone mineral density in premenopausal women: a meta-analysis of individual patient data. J Womens Health (Larchmt) 2004;13:293–300. doi: 10.1089/154099904323016455. [DOI] [PubMed] [Google Scholar]
- 62.Kelley GA, Kelley KS. Impact of progressive resistance training on lipids and lipoproteins in adults: a meta-analysis of randomized controlled trials. Prev Med. 2009;48:9–19. doi: 10.1016/j.ypmed.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 63.Kelley GA, Kelley KS, Tran ZV. Exercise and bone mineral density in men: a meta-analysis. J Appl Physiol. 2000;88:1730–1736. doi: 10.1152/jappl.2000.88.5.1730. [DOI] [PubMed] [Google Scholar]
- 64.Kitamura I, Takeshima N, Tokudome M, Yamanouchi K, Oshida Y, Sato Y. Effects of aerobic and resistance exercise training on insulin action in the elderly. Ger & Geront Int. 2003;3:50–55. [Google Scholar]
- 65.Kosek DJ, Kim JS, Petrella JK, Cross JM, Bamman MM. Efficacy of 3 days/wk resistance training on myofiber hypertrophy and myogenic mechanisms in young vs. older adults. J Appl Physiol. 2006;101:531–544. doi: 10.1152/japplphysiol.01474.2005. [DOI] [PubMed] [Google Scholar]
- 66.Kraemer WJ, Adams K, Cafarelli E, Dudley GA, Dooly C, Feigenbaum MS, Fleck SJ, Franklin B, Fry AC, Hoffman JR, Newton RU, Potteiger J, Stone MH, Ratamess NA, Triplett-McBride T. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34:364–380. doi: 10.1097/00005768-200202000-00027. [DOI] [PubMed] [Google Scholar]
- 67.Kryger AI, Andersen JL. Resistance training in the oldest old: consequences for muscle strength, fiber types, fiber size, and MHC isoforms. Scand J Med Sci Sports. 2007;17:422–430. doi: 10.1111/j.1600-0838.2006.00575.x. [DOI] [PubMed] [Google Scholar]
- 68.Latham N, Anderson C, Bennett D, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. 2003 doi: 10.1002/14651858.CD002759. CD002759. [DOI] [PubMed] [Google Scholar]
- 69.Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59:48–61. doi: 10.1093/gerona/59.1.m48. [DOI] [PubMed] [Google Scholar]
- 70.Lemmer JT, Ivey FM, Ryan AS, Martel GF, Hurlbut DE, Metter JE, Fozard JL, Fleg JL, Hurley BF. Effect of strength training on resting metabolic rate and physical activity: age and gender comparisons. Med Sci Sports Exerc. 2001;33:532–541. doi: 10.1097/00005768-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 71.Lemmer JT, Martel GF, Hurlbut DE, Hurley BF. Age and sex differentially affect regional changes in one repetition maximum strength. J Strength Cond Res. 2007;21:731–737. doi: 10.1519/R-20816.1. [DOI] [PubMed] [Google Scholar]
- 72.Levinger I, Goodman C, Matthews V, Hare DL, Jerums G, Garnham A, Selig S. BDNF, metabolic risk factors, and resistance training in middle-aged individuals. Med Sci Sports Exerc. 2008;40:535–541. doi: 10.1249/MSS.0b013e31815dd057. [DOI] [PubMed] [Google Scholar]
- 73.Lexell J. Ageing and human muscle: observations from Sweden. Can J Appl Physiol. 1993;18:2–18. doi: 10.1139/h93-002. [DOI] [PubMed] [Google Scholar]
- 74.Liu C, Latham N. Progressive resistance strength training for improving physical function in older adults. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lott M, Hurlbut D, Ryan A, Lemmer J, Ivey F, Zeidman J, Fleg J, Fozard J, H BF. Gender differences in glucose and insulin response to strength training in 65- to 75-year-olds. Clin Exerc Physiol. 2001;3:220–228. [Google Scholar]
- 76.Maddalozzo G. Dissertation. Oregon State University; Corvallis, OR: 1998. Effects of two resistance training protocols on insulin-like growth factors. Muscle strength and bone mass in older adults; p. 147. [Google Scholar]
- 77.Mayhew DL, Kim JS, Cross JM, Ferrando AA, Bamman MM. Translational signaling responses preceding resistance training-mediated myofiber hypertrophy in young and old humans. J Appl Physiol. 2009;107:1655–1662. doi: 10.1152/japplphysiol.91234.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Melton LJ, 3rd, Khosla S, Crowson CS, O'Connor MK, O'Fallon WM, Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000;48:625–630. [PubMed] [Google Scholar]
- 79.Miller JP, Pratley RE, Goldberg AP, Gordon P, Rubin M, Treuth MS, Ryan AS, Hurley BF. Strength training increases insulin action in healthy 50- to 65-yr-old men. J Appl Physiol. 1994;77:1122–1127. doi: 10.1152/jappl.1994.77.3.1122. [DOI] [PubMed] [Google Scholar]
- 80.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 e1000097. [PMC free article] [PubMed] [Google Scholar]
- 81.Murray-Kolb LE, Beard JL, Joseph LJ, Davey SL, Evans WJ, Campbell WW. Resistance training affects iron status in older men and women. Int J Sport Nutr Exerc Metab. 2001;11:287–298. doi: 10.1123/ijsnem.11.3.287. [DOI] [PubMed] [Google Scholar]
- 82.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 83.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 84.Orr R, Raymond J, Fiatarone Singh M. Efficacy of progressive resistance training on balance performance in older adults : a systematic review of randomized controlled trials. Sports Med. 2008;38:317–343. doi: 10.2165/00007256-200838040-00004. [DOI] [PubMed] [Google Scholar]
- 85.Peterson M, Rhea M, Sen A, Gordon P. Resistance Exercise for Muscular Strength in Older Adults: A Meta-Analysis. Ageing Res Rev. 2010;9:226–237. doi: 10.1016/j.arr.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pratley R, Nicklas B, Rubin M, Miller J, Smith A, Smith M, Hurley B, Goldberg A. Strength training increases resting metabolic rate and norepinephrine levels in healthy 50- to 65-yr-old men. J Appl Physiol. 1994;76:133–137. doi: 10.1152/jappl.1994.76.1.133. [DOI] [PubMed] [Google Scholar]
- 87.Reynolds THt, Supiano MA, Dengel DR. Regional differences in glucose clearance: effects of insulin and resistance training on arm and leg glucose clearance in older hypertensive individuals. J Appl Physiol. 2007;102:985–991. doi: 10.1152/japplphysiol.00914.2006. [DOI] [PubMed] [Google Scholar]
- 88.Richardson CR, Newton TL, Abraham JJ, Sen A, Jimbo M, Swartz AM. A meta-analysis of pedometer-based walking interventions and weight loss. Ann Fam Med. 2008;6:69–77. doi: 10.1370/afm.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Riechman SE, Andrews RD, Maclean DA, Sheather S. Statins and dietary and serum cholesterol are associated with increased lean mass following resistance training. J Gerontol A Biol Sci Med Sci. 2007;62:1164–1171. doi: 10.1093/gerona/62.10.1164. [DOI] [PubMed] [Google Scholar]
- 90.Roth SM, Ivey FM, Martel GF, Lemmer JT, Hurlbut DE, Siegel EL, Metter EJ, Fleg JL, Fozard JL, Kostek MC, Wernick DM, Hurley BF. Muscle size responses to strength training in young and older men and women. J Am Geriatr Soc. 2001;49:1428–1433. doi: 10.1046/j.1532-5415.2001.4911233.x. [DOI] [PubMed] [Google Scholar]
- 91.Ryan AS, Pratley RE, Elahi D, Goldberg AP. Resistive training increases fat-free mass and maintains RMR despite weight loss in postmenopausal women. J Appl Physiol. 1995;79:818–823. doi: 10.1152/jappl.1995.79.3.818. [DOI] [PubMed] [Google Scholar]
- 92.Schrager MA, Metter EJ, Simonsick E, Ble A, Bandinelli S, Lauretani F, Ferrucci L. Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol. 2007;102:919–925. doi: 10.1152/japplphysiol.00627.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Snijder MB, Dekker JM, Visser M, Yudkin JS, Stehouwer CD, Bouter LM, Heine RJ, Nijpels G, Seidell JC. Larger thigh and hip circumferences are associated with better glucose tolerance: the Hoorn study. Obes Res. 2003;11:104–111. doi: 10.1038/oby.2003.18. [DOI] [PubMed] [Google Scholar]
- 94.Snijder MB, Henry RM, Visser M, Dekker JM, Seidell JC, Ferreira I, Bouter LM, Yudkin JS, Westerhof N, Stehouwer CD. Regional body composition as a determinant of arterial stiffness in the elderly: The Hoorn Study. J Hypertens. 2004;22:2339–2347. doi: 10.1097/00004872-200412000-00016. [DOI] [PubMed] [Google Scholar]
- 95.Steib S, Schoene D, Pfeifer K. Dose-Response Relationship of Resistance Training in Older Adults: A Meta-Analysis. Med Sci Sports Exerc. 2010;42:902–914. doi: 10.1249/MSS.0b013e3181c34465. [DOI] [PubMed] [Google Scholar]
- 96.Stewart KJ, Bacher AC, Turner KL, Fleg JL, Hees PS, Shapiro EP, Tayback M, Ouyang P. Effect of exercise on blood pressure in older persons: a randomized controlled trial. Arch Intern Med. 2005;165:756–762. doi: 10.1001/archinte.165.7.756. [DOI] [PubMed] [Google Scholar]
- 97.Tarnopolsky M, Zimmer A, Paikin J, Safdar A, Aboud A, Pearce E, Roy B, Doherty T. Creatine monohydrate and conjugated linoleic acid improve strength and body composition following resistance exercise in older adults. PLoS One. 2007;2:e991. doi: 10.1371/journal.pone.0000991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Teixeira PJ, Going SB, Houtkooper LB, Metcalfe LL, Blew RM, Flint-Wagner HG, Cussler EC, Sardinha LB, Lohman TG. Resistance training in postmenopausal women with and without hormone therapy. Med Sci Sports Exerc. 2003;35:555–562. doi: 10.1249/01.MSS.0000058437.17262.11. [DOI] [PubMed] [Google Scholar]
- 99.Treuth MS, Hunter GR, Kekes-Szabo T, Weinsier RL, Goran MI, Berland L. Reduction in intra-abdominal adipose tissue after strength training in older women. J Appl Physiol. 1995;78:1425–1431. doi: 10.1152/jappl.1995.78.4.1425. [DOI] [PubMed] [Google Scholar]
- 100.Treuth MS, Ryan AS, Pratley RE, Rubin MA, Miller JP, Nicklas BJ, Sorkin J, Harman SM, Goldberg AP, Hurley BF. Effects of strength training on total and regional body composition in older men. J Appl Physiol. 1994;77:614–620. doi: 10.1152/jappl.1994.77.2.614. [DOI] [PubMed] [Google Scholar]
- 101.Vincent KR, Braith RW, Feldman RA, Kallas HE, Lowenthal DT. Improved cardiorespiratory endurance following 6 months of resistance exercise in elderly men and women. Arch Intern Med. 2002;162:673–678. doi: 10.1001/archinte.162.6.673. [DOI] [PubMed] [Google Scholar]
- 102.Vincent KR, Braith RW, Feldman RA, Magyari PM, Cutler RB, Persin SA, Lennon SL, Gabr AH, Lowenthal DT. Resistance exercise and physical performance in adults aged 60 to 83. J Am Geriatr Soc. 2002;50:1100–1107. doi: 10.1046/j.1532-5415.2002.50267.x. [DOI] [PubMed] [Google Scholar]
- 103.Welle S, Thornton C, Jozefowicz R, Statt M. Myofibrillar protein synthesis in young and old men. Am J Physiol. 1993;264:E693–698. doi: 10.1152/ajpendo.1993.264.5.E693. [DOI] [PubMed] [Google Scholar]
- 104.Welle S, Thornton C, Statt M, McHenry B. Postprandial myofibrillar and whole body protein synthesis in young and old human subjects. Am J Physiol. 1994;267:E599–604. doi: 10.1152/ajpendo.1994.267.4.E599. [DOI] [PubMed] [Google Scholar]
- 105.Welle S, Totterman S, Thornton C. Effect of age on muscle hypertrophy induced by resistance training. J Gerontol A Biol Sci Med Sci. 1996;51:M270–275. doi: 10.1093/gerona/51a.6.m270. [DOI] [PubMed] [Google Scholar]
- 106.Yarasheski KE. Exercise, aging, and muscle protein metabolism. J Gerontol A Biol Sci Med Sci. 2003;58:M918–922. doi: 10.1093/gerona/58.10.m918. [DOI] [PubMed] [Google Scholar]
- 107.Yarasheski KE, Pak-Loduca J, Hasten DL, Obert KA, Brown MB, Sinacore DR. Resistance exercise training increases mixed muscle protein synthesis rate in frail women and men >/=76 yr old. Am J Physiol. 1999;277:E118–125. doi: 10.1152/ajpendo.1999.277.1.E118. [DOI] [PubMed] [Google Scholar]
- 108.Yarasheski KE, Zachwieja JJ, Bier DM. Acute effects of resistance exercise on muscle protein synthesis rate in young and elderly men and women. Am J Physiol. 1993;265:E210–214. doi: 10.1152/ajpendo.1993.265.2.E210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This SDC contains continued/additional detail pertaining to the resistance exercise protocols that were considered for inclusion in the analysis.
This SDC contains continued/additional detail pertaining to the search strategy and study identification. Specific permutations of the text keyword combinations and Medical Subject Headings (MeSH) terms are provided.
This SDC table contains detail pertaining to the important characteristics of each study included in the analysis.