Compared with our parents or grandparents, we are spending increasing amounts of time in environments that not only limit physical activity but require prolonged sitting—at work, at home, and in our cars and communities.1 Work sites, schools, homes, and public spaces have been (and continue to be) re-engineered in ways that minimize human movement and muscular activity. These changes have a dual effect on human behavior: people move less and sit more. From an evolutionary perspective, humans were designed to move—to locomote and engage in all manner of manual labor throughout the day. This was essential to our survival as a species. The recent shift from a physically demanding life to one with few physical challenges has been sudden, occurring during a tiny fraction of human existence.
Societal indicators of reductions in human energy expenditure and increases in sedentary behavior during the past several decades are particularly striking. In 1970, 2 in 10 working Americans were in jobs requiring only light activity (predominantly sitting at a desk), whereas 3 in 10 were in jobs requiring high-energy output (eg, construction, manufacturing, farming).2 By 2000, more than 4 in 10 adults were in light-activity jobs, whereas 2 in 10 were in high-activity jobs.2 Moreover, during the past 20 years, total screen time (ie, using computers, watching television, playing video games) has increased dramatically. In 2003, nearly 6 in 10 working adults used a computer on the job and more than 9 in 10 children used computers in school (kindergarten through grade 12).3 Between 1989 and 2009, the number of households with a computer and Internet access increased from 15% to 69%.3 Other significant contributors to daily sitting time—watching television and driving personal vehicles—are at all-time highs, with estimates of nearly 4 hours and 1 hour, respectively.4,5
Scientists studying the ill effects of this decrease in physical activity have revealed a complex, multifaceted relationship among physical work, energy expenditure, and health.6,7 Clinical and basic research has focused on the benefits of incorporating regular bouts of exercise into modern life to adjust to some extent for the loss of the physically active life led by our ancestors.6 Current public health recommendations propose engaging in at least 150 minutes per week of moderate-to-vigorous activity to help prevent and manage multiple chronic conditions, notably cardiovascular disease, type 2 diabetes, obesity, and some cancers.7 The evidence base that supports this exercise recommendation is substantial. (Here, we use the terms exercise and moderate-to-vigorous activity interchangeably, recognizing that, by some definitions, exercise refers specifically to intentional activity carried out for health/fitness purposes.7)
Those who do not exercise have by convention been termed sedentary. However, this is no longer an adequate perspective. Recent epidemiologic evidence suggests that the metabolic and long-term health consequences of habitual sedentary behavior (too much sitting) are distinct from those associated with a lack of moderate-to-vigorous activity (too little exercise).8,9 This shift in perspective is being clarified through innovations in technology used to characterize movement patterns in populations.
New Technology Characterizes Sedentary and Physically Active Time in Populations
Nonexercise behaviors can be differentiated into 2 categories: sedentary behavior, which may be defined as sitting, lying down, and expending very little energy (approximately 1.0-1.5 metabolic equivalents [METs]), and light-intensity activity, such as standing, self-care activities, and slow walking, which require low energy expenditure (approximately 1.6-2.9 METs).10 Advances in microelectronic technologies, specifically the accelerometer, have enabled the time spent in sedentary, light-intensity, and exercise behaviors to be objectively derived. This has greatly improved the methodology for measuring activity patterns among free-living humans, which previously relied mainly on self-report of behavior.11
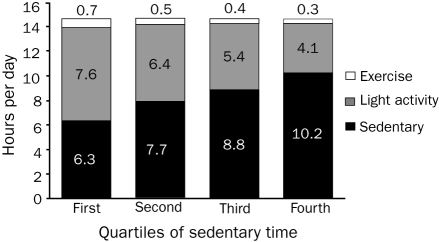
Examining 7 days of accelerometer data from a nationally representative sample of 1714 white adults aged 20 to 59 years from the US National Health and Nutrition Examination Survey,12 it is striking that the vast majority of daily nonsleeping time was spent in either sedentary behavior (58%) or light-intensity activity (39%), and only 3% in exercise time. Figure 1 shows the differences in time spent in light activity and exercise across quartiles of sedentary time. Most of the variance in sedentary time is due to the change in the proportion of time spent in light-intensity activity. For example, sedentary time increases from 6.3 hours in quartile 1 to 10.2 hours in quartile 4, a 62% increase with nearly all of the sedentary time coming out of the block of light activity.
FIGURE 1.
Quartiles of sedentary time. Based on 1 week of accelerometer data in 1712 adults, these stacked column graphs show the allocation of waking hours spent sedentary, in light activity, and in exercise, from the lower to the upper quartile of overall sedentary time.
Data from the National Health and Nutrition Examination Survey.12
Sedentary time and light activity time were also highly negatively correlated (r = −0.96) in a sample of Australian adults.13 Although the precise magnitude of changes cannot be determined, the shift from time spent in light activities to time being sedentary undoubtedly has increased substantially in recent decades. This shift has likely contributed to the increasing rates of obesity and type 2 diabetes.
New Insights Into Sedentary Behavior and Cardiometabolic Risk
Recent studies have documented deleterious associations of adults' reported television viewing time and overall sedentary time with central adiposity (larger waist circumference) and with fasting triglyceride levels and markers of insulin resistance (ie, fasting insulin level, 2-hour glucose) that are independent of both central adiposity and exercise time.13-17 With prolonged periods of sitting, fewer skeletal muscle contractions may result in reduced lipoprotein lipase activity and clearance of triglycerides, reduced clearance of an oral glucose load, and less glucose-stimulated insulin secretion.18-20 Moreover, time in sedentary behaviors is associated with increased cardiovascular and all-cause mortality; this has now been shown for television viewing time,8 overall daily sitting time,4 and time spent sitting in cars.21
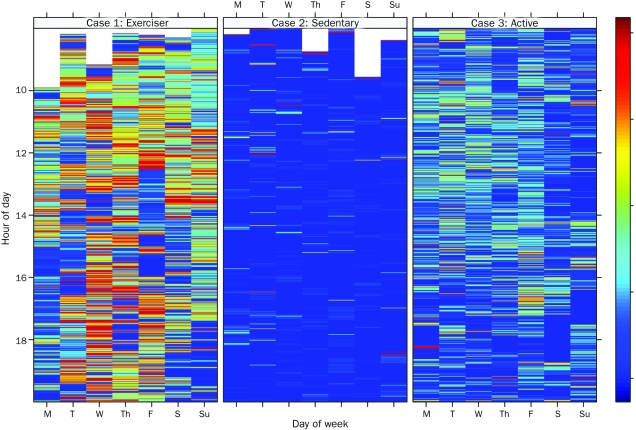
Another intriguing finding is that breaks in sedentary time have beneficial associations with waist circumference, body mass index, triglyceride levels, and 2-hour glucose levels that are independent of total sedentary time and exercise time.22 In Figure 2, the variability in sedentary behavior and associated breaks for 3 persons across 1 week is illustrated using cluster heat maps.23 Case 1 reflects a healthy daily pattern that includes time spent in exercise and intermittent periods of light activity that break up periods of sedentary behavior, whereas case 2 illustrates a preponderance of sitting with the balance in light activity (and no exercise). The “exerciser” profile meets the accepted public health standard for sufficient exercise but is the exception and not the rule, whereas the “sedentary” profile is prevalent in the US population. In case 3, a variation of case 2, many bouts of light activity have replaced sedentary time throughout the day. This increased frequency of light activities may be by necessity (for example, being a mechanic, a physician with multiple examination rooms, or a mother with young children) or by choice. This “active” profile is not uncommon, but its potential salutary effect has been overlooked.
FIGURE 2.
Daily activity patterns. Three different activity patterns are illustrated using cluster heat maps derived from accelerometer data (counts/min): the “exerciser” profile, the “sedentary” profile, and the “active” profile.
Data from the National Health and Nutrition Examination Survey.12
These 3 cases show the limited perspective provided when a person is identified as being physically active or not solely on the basis of the 3% or so of time spent in moderate or vigorous activity. Conventionally quoted population averages obscure the wide distribution of individual differences in allocation of time spent in behaviors that require very low, light, and moderate or high energy expenditure; they also fail to portray the frequency of beneficial breaks in very low energy output (sedentary) behaviors. Recent findings indicate that helping people shift from the “sedentary” profile toward the “active” profile would reap important health benefits.22,24
On the basis of our analysis, 1 in 4 white US adults spend about 70% of their waking hours sitting, 30% in light activities, and little or no time in exercise. Feasible steps to break up prolonged sitting with short bouts of light activity include walking down the hall to speak with coworkers instead of emailing, extending walking distance during trips to the break room or bathroom, and standing or pacing when on the phone. Prolonged sitting is easy to recognize and occurs in many settings, and interventions targeting it involve small changes that may be readily accepted. Every minute of sedentary behavior replaced with light activity would expend 1 additional kilocalorie (calculated assuming 1.5 vs 2.3 METs for a person weighing 72 kg). Greater energy expenditure is a simple benefit to cite. Yet, as the findings already summarized suggest, weight control is one of several important potential benefits of spending less time sitting.19
Conclusion
In recent decades, affluent populations have become increasingly sedentary, with many adults spending 70% or more of their waking hours sitting. Parallel with this change, evidence has emerged identifying habitual sedentary behavior (prolonged sitting) as a novel risk factor for cardiometabolic disease and all-cause mortality, independent of time spent in exercise. As this evidence is primarily observational in nature, further experimental research investigating potential mechanisms and dose-response relationships is necessary. For example, a daily quantity of neuromuscular stimulation (some combination of duration and frequency) that occurs during standing and light activities may be necessary to sustain components of musculoskeletal and metabolic health.
These new insights into the health risks of sedentary behavior broaden the accepted perspective on physical activity and health by identifying the need to reduce prolonged sitting and increase light-intensity activities (eg, standing and incidental walking), in addition to engaging in regular moderate-to-vigorous activity. The importance of exercise counseling in the primary care setting is well established.25 Excellent resources providing practical advice for incorporating behavioral counseling in medical settings are available.26,27
In light of recent findings, it has become clear that most patients face 2 obstacles: too little exercise and too much sitting. The American Academy of Pediatrics counsels parents to limit children's screen time—television, DVDs, and video games—to no more than 2 hours per day.28 Parents still tell their children to get off the sofa and go out and play. Recent evidence is compelling that adults too need similar advice from their physicians. Patients need to get out of their chairs more frequently, both at work and at home. Advising patients to reduce prolonged sitting can be readily combined with current recommendations on exercise and weight management.
REFERENCES
- 1.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299(5608):853-855 [DOI] [PubMed] [Google Scholar]
- 2.Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421-443 [DOI] [PubMed] [Google Scholar]
- 3.US Census Bureau Internet Use in the United States: October 2009. US Census Bureau Web site. http://www.census.gov/population/www/socdemo/computer/2009.html Accessed August 24, 2010
- 4.Nielsen Company Three Screen Report. 1st Quarter 2010. What consumers watch: technology enhances the video experience HDTV, timeshifting, broadband and smartphones contribute to higher levels of video viewing-http://en-us.nielsen.com/content/dam/nielsen/en_us/documents/pdf/Three%20Screen%20Reports/Nielsen_Three%20Screen%20Report_Q12010.PDF Accessed August 24, 2010
- 5.US Department of Transportation Summary of travel trends: National Household Travel Survey (NHTS). NHTS Web site. ReleasedDecember2004. http://nhts.ornl.gov/2001/pub/STT.pdf Accessed August 24, 2010
- 6.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081-1093 [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services 2008 physical activity guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008-2009. http://www.health.gov/paguidelines/ Accessed August 24, 2010 [Google Scholar]
- 8.Dunstan DW, Barr ELM, Healy GN, et al. Television viewing time and mortality: the AusDiab study. Circulation. 2010;121(3):384-391 [DOI] [PubMed] [Google Scholar]
- 9.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998-1005 [DOI] [PubMed] [Google Scholar]
- 10.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(suppl 9):S498-S504 [DOI] [PubMed] [Google Scholar]
- 11.Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. In press [DOI] [PMC free article] [PubMed]
- 12.Centers for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey Data 2003-2004, 2005-2006. Atlanta, GA: Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS); 2009-2010. http://www.cdc.gov/nchs/nhanes.htm Accessed August 24, 2010 [Google Scholar]
- 13.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369-371 [DOI] [PubMed] [Google Scholar]
- 14.Dunstan DW, Salmon J, Healy GN, et al. Association of television viewing with fasting and 2-h postchallenge plasma glucose levels in adults without diagnosed diabetes. Diabetes Care. 2007;30(3):516-522 [DOI] [PubMed] [Google Scholar]
- 15.Ford ES, Li C, Zhao G, Pearson WS, Tsai J, Churilla JR. Sedentary behavior, physical activity, and concentrations of insulin among US adults. Metabolism. 2010;59(9):1268-1275 [DOI] [PubMed] [Google Scholar]
- 16.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384-1389 [DOI] [PubMed] [Google Scholar]
- 17.Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardio-metabolic risk biomarkers: AusDiab 2004-2005. Diabetes Care. 2010;33(2):327-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamburg NM, McMackin CJ, Huang AL, et al. Physical inactivity rapidly induces insulin resistance and microvascular dysfunction in healthy volunteers. Arterioscler Thromb Vasc Biol. 2007;27(12):2650-2656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton MT, Hamilton DG, Zderic TW. The role of low energy expenditure and sitting on obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655-2667 [DOI] [PubMed] [Google Scholar]
- 20.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551(2):673-682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blair SN. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42(5):879-885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661-666 [DOI] [PubMed] [Google Scholar]
- 23.Wilkinson L, Friendly M. The history of the cluster heat map. Am Stat. 2009;63(2):179-184 [Google Scholar]
- 24.Levine JA. Nonexercise activity thermogenesis: liberating the life-force. J Intern Med. 2007;262(3):273-287 [DOI] [PubMed] [Google Scholar]
- 25.Chakravarthy MV, Joyner MJ, Booth FW. An obligation for primary care physicians to prescribe physical activity to sedentary patients to reduce the risk of chronic health conditions. Mayo Clin Proc. 2002;77(2):165-173 [DOI] [PubMed] [Google Scholar]
- 26.Exercise is Medicine Web site. http://exerciseismedicine.org/physicians.htm Accessed August 24, 2010
- 27.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406-441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics Children, adolescents, and television. Pediatrics. 2001;107:423-426 [DOI] [PubMed] [Google Scholar]