Diabetes mellitus (DM) is a growing health problem that has reached epidemic proportions.1 Of patients with this disease, 90% to 95% have type 2 DM.2 Extrapolated global data from the International Diabetes Federation have shown that the prevalence of type 2 DM is in excess of 285 million people worldwide and will exceed 439 million people by the year 2030.1 Factors contributing to this increase include an aging population, improved survival rates, and the increasing prevalence of overweight/obesity.3 A recent large observational cohort study showed that overweight/obesity increases the risk of coronary heart disease and cardiovascular disease in patients with type 2 DM.3 In patients with DM, the prevalence of cardiovascular disease is 2- to 4-fold higher than in those without DM, and data from the recent Framingham Heart Study indicate that patients with type 2 DM have not experienced decreases in coronary heart disease or cardiovascular risk factors in contrast to patients without DM.4
The latest data from the National Health and Nutrition Examination Survey indicate that only 57% of patients with type 2 DM achieve a target goal hemoglobin A1c level less than 7.0%, and only 12% to 13% achieve recommended target goals for hemoglobin A1c, blood pressure, and serum lipid levels.5 Thus, despite increased understanding of the pathophysiology of DM, availability of newer agents, and new treatment algorithms, we still have a long way to go in achieving optimal care for our patients.
The goal of this supplement is to provide primary care physicians (PCPs) and other health care professionals who treat patients with type 2 DM the latest information on the pathophysiology and current issues in the management of patients with type 2 DM. Topics reviewed in this supplement include the role of defects in the incretin system that contribute to the hyperglycemia of type 2 DM, the importance of cardiovascular risk factor management, and multifactorial treatment in an effort to reduce the morbidity and mortality from the disease. Finally, we evaluate the new incretin-based agents and discuss their role in the therapeutic armamentarium available to PCPs in their quest to improve the overall quality of life of patients with type 2 DM.
Dr Freeman6 reviews the physiologic and pharmacological basis for the implementation of incretin hormones in the treatment of type 2 DM. Traditionally, peripheral insulin resistance, increased hepatic gluconeogenesis, and pancreatic β-cell failure are considered core elements in the evolution of type 2 DM. However, the pathophysiology of type 2 DM is complex, and other factors, including decreased activity of glucagon-like peptide 1 (GLP-1), paradoxical glucagon secretion, and reduced amylin secretion during periods of hyperglycemia, contribute to the hyperglycemia of type 2 DM. Freeman also discusses how manipulating the incretin system with therapeutic agents can provide glycemic and other benefits to patients with type 2 DM.
Most patients with type 2 DM are overweight/obese. Although it is understood that the primary focus of treating these patients is to reduce blood glucose levels, it is important that the issue of overweight/obesity is addressed as well. To successfully manage type 2 DM in these patients, agents that promote weight loss while reducing the risk of hypoglycemia should be a priority. Drs Schwartz and Kohl7 review the data on overweight/obesity and its role as a cardiovascular risk factor, as well as the dangers of hypoglycemia and how the concern of hypoglycemia can interfere with a goal of intensive glycemic control. They also examine data on incretin-based agents and their effect on overweight/obesity, hypoglycemia, and other cardiovascular risk factors.
I review the physiology of the incretin system, how defects in the incretin system contribute to the hyperglycemia of type 2 DM, and why modulating the effects of GLP-1 receptor agonists became a target for research.8 The review also compares the differences between GLP-1 receptor agonists and dipeptidyl peptidase 4 inhibitors and their role in the management of patients with type 2 DM.
Primary care physicians treat at least 90% of the 24 million patients in the United States with DM. Dr Unger9 discusses in detail the relevance, efficacy, and safety data of incretin-based agents and their ability to favorably affect glucose control and cardiovascular risk factors present in patients with type 2 DM. He then describes the clinical perspectives for PCPs when they use these agents to treat their patients with type 2 DM and provides clinical recommendations for including these agents in their therapeutic armamentarium.
Finally, Dr Stolar10 provides a comprehensive definition of treatment success in patients with type 2 DM that includes optimization of reduction of cardiovascular risk factors associated with microvascular and macrovascular complications and slowing or stopping disease progression. He also discusses new paradigms for managing patients with type 2 DM that address concomitant risk factors and morbidities of obesity, hypertension, and dyslipidemia with equal or occasionally even greater aggressiveness than hyperglycemia.
The authors' goals in publishing this supplement are to develop a treatment strategy that can lower blood glucose levels as much as possible for as long as possible while reducing the risk of hypoglycemia and to address the numerous cardiovascular risk factors present in any given patient. In this way, we hope to reduce the morbidity and mortality of this increasingly common chronic disease.
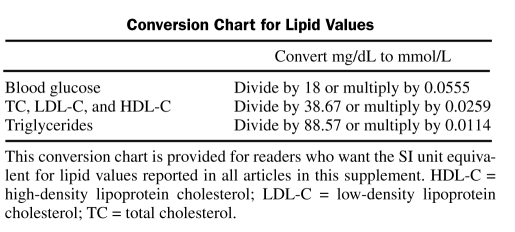
Conversion Chart for Lipid Values
Acknowledgments
The authors of this supplement thank Michael Kodack, PharmD, BlueSpark Healthcare Communications LLC, for editorial assistance.
REFERENCES
- 1. International Diabetes Federation Atlas 2009 Diabetes and impaired glucose tolerance: global burden: prevalence and projections, 2010 and 2030. International Diabetes Federation Web site. http://www.diabetesatlas.org/content/diabetes-and-impaired-glucose-tolerance Accessed September 16, 2010
- 2. National Diabetes Information Clearinghouse (NDIC) National diabetes statistics, 2007. http://diabetes.niddk.nih.gov/dm/pubs/statistics/ Last update: June 2008. Accessed September 16, 2010
- 3. Eeg-Olofsson K, Cederholm J, Nilsson PM, et al. Risk of cardiovascular disease and mortality in overweight and obese patients with type 2 diabetes: an observational study in 13,087 patients. Diabetologia. 2009;52(1):65-73 [DOI] [PubMed] [Google Scholar]
- 4. Preis SR, Pencina MJ, Hwang SJ, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120(3):212-220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cheung BM, Ong KL, Cherny SS, et al. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med. 2009;122:443-453 [DOI] [PubMed] [Google Scholar]
- 6. Freeman JS. A physiologic and pharmacological basis for implementation of incretin hormones in the treatment of type 2 diabetes mellitus. Mayo Clin Proc. 2010;85(12)(suppl):S5-S14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schwartz SS, Kohl BA. Glycemic control and weight reduction without causing hypoglycemia: the case for continued safe aggressive care of patients with type 2 diabetes mellitus and avoidance of therapeutic inertia. Mayo Clin Proc. 2010;85(12)(suppl):S15-S26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davidson JA: Incorporating incretin-based therapies into clinical practice: differences between glucagon-like peptide 1 receptor agonists and dipeptidyl peptidase 4 inhibitors. Mayo Clin Proc. 2010;85(12)(suppl):S27-S37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Unger J. Incretins: clinical perspectives, relevance, and applications for the primary care physician in the treatment of patients with type 2 diabetes. Mayo Clin Proc. 2010;85(12)(suppl):S38-S49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stolar MW. Defining and achieving treatment success in patients with type 2 diabetes mellitus. Mayo Clin Proc. 2010;85(12)(suppl):S50-S59 [DOI] [PMC free article] [PubMed] [Google Scholar]