Abstract
Objective
To determine if vitamin and mineral supplement use among children and adolescents in the United States is associated with nutrition, food security, physical activity, and health care access.
Design
Secondary analysis of nationally representative data from the 1999–2004 National Health and Nutrition Examination Survey.
Setting
Questionnaires, household interviews, and medical examinations.
Participants
Children and adolescents 2 to 17 years of age (N = 10 828).
Main Exposure
Vitamin and mineral supplement use in the past month.
Main Outcome Measures
Demographics, nutrition, food security, physical activity, and health care access.
Results
Approximately 34% (SE 1.2) used vitamin and mineral supplements in the past month, with underweight subjects reporting greater intake. Younger age, non-Hispanic white race/ethnicity, being born in the United States, higher milk intake, lower total fat and cholesterol intake, higher dietary fiber intake, higher income, greater food security, lower media/computer use, greater physical activity, lower body mass index, health insurance coverage, better health care access, and better self-reported health were associated with greater use of vitamin and mineral supplements. Such supplements contributed significantly to total daily dietary intakes of vitamins and minerals.
Conclusions
A large number of US children and adolescents use vitamin and mineral supplements, which for most may not be medically indicated. Such supplements contribute significantly to total dietary intakes of vitamins and minerals, and studies of nutrition should include their assessment. Since vitamin and mineral supplement users report greater health care access, health care providers may be in a position to provide screening and counseling regarding dietary adequacy and indications for supplement use.
Supplemental vitamin and mineral (VM) use is common in the United States.1–3 The reasons for VM supplementation appear to be multifactorial and such supplements are largely deemed unnecessary if one has a varied diet.4–6 Still, almost $2 billion is spent annually on VM supplements, and they are the third most common category of medications used in the United States.7 Multivitamin preparations for older children and adolescents are not regulated by the Food and Drug Administration and may result in adverse effects ranging from nausea, vomiting, and abdominal pain to increased cerebrospinal pressure, liver abnormalities, and neuropathy.8 The American Academy of Pediatrics does not recommend supplemental vitamin use for healthy children older than 1 year who consume a varied diet. Supplemental vitamins are only recommended for certain groups of children, eg, those with chronic diseases, eating disorders, malabsorption, and liver disease and obese children in weight loss programs.8
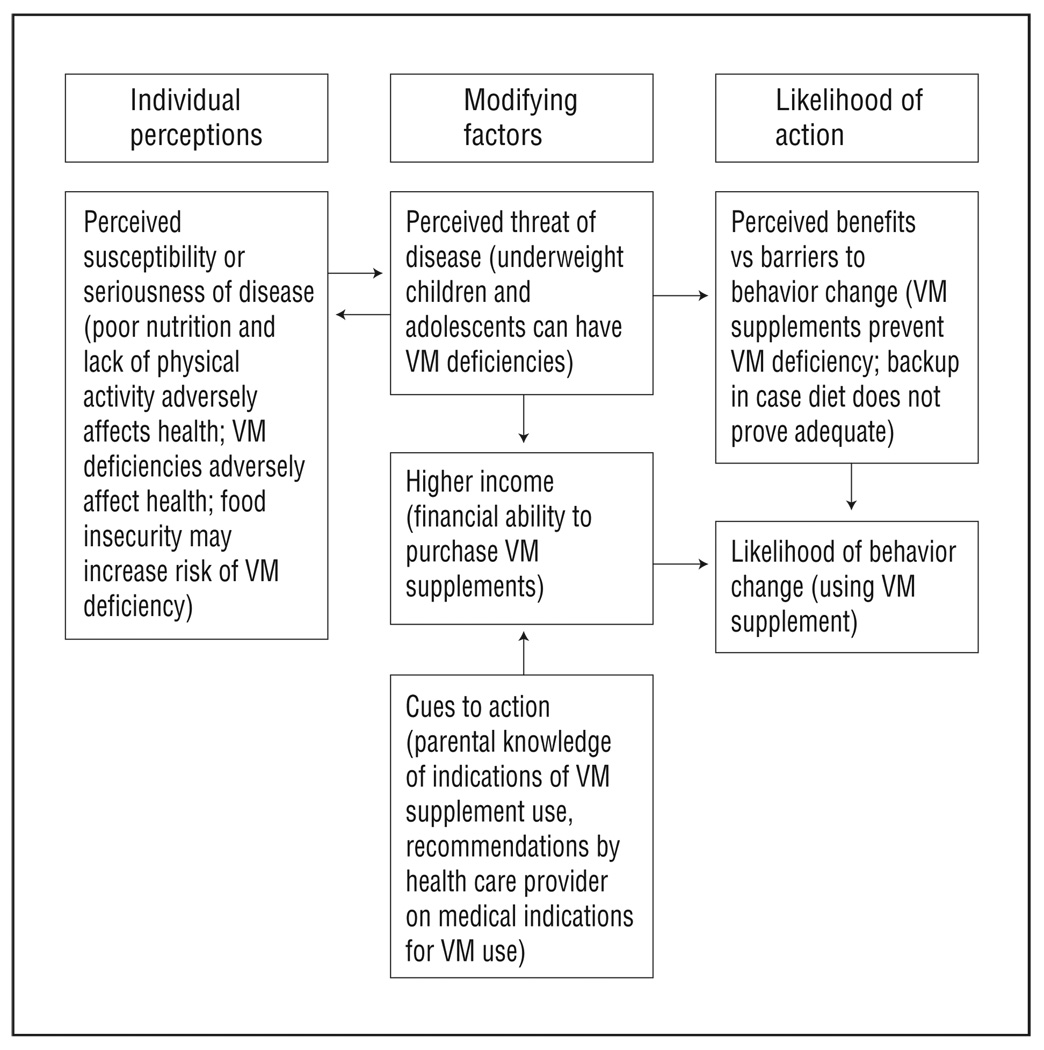
Research focusing on the association of VM use with nutrition practices and physical activity has been conducted mainly in adolescents and adults.1,4,5,9–11 Studies using a theoretical framework that examine the relationship of VM use with food security and health care access are limited. The Health Belief Model (HBM) is a theoretical framework used to explain and predict health behaviors by focusing on attitudes and beliefs. Constructs of the HBM have successfully been applied to explain and improve preventive health behaviors and health care use behaviors in adults, such as folate consumption for the prevention of neural tube defects and calcium supplementation for the prevention of osteoporosis.12–15 According to this model, an individual will take a health-related action if he or she feels and expects that it will help avoid a negative condition. 16 Constructs of the HBM include perceived susceptibility, perceived severity, perceived benefits, and perceived barriers to performing the action. The HBM may explain why some individuals may choose to use VM supplements (perceptions that one’s diet is inadequate, VM deficiency affects health, or using VM supplements will benefit health or stimulate appetite; individual financial ability to afford VM supplements; and health care provider guidance with respect to the need for VM supplementation).
Based on theoretical constructs of the HBM, we posited that VMs might be used to ameliorate the adverse effects of less healthy nutrition, lower food security, and lower levels of physical activity or as insurance against barriers to full health care access. Using data from the 1999–2004 National Health and Nutrition Examination Survey (NHANES), we tested the following hypotheses: (1) VM use is higher in children and adolescents with unhealthy nutrition habits compared with those with healthy nutrition habits, (2) VM use is higher in children and adolescents who experience lower food security compared with those who experience greater food security, (3) VM use is higher in children and adolescents with lower levels of physical activity compared with those with higher levels of physical activity, (4) VM use is higher in children and adolescents who have lower health care access compared with those who have higher health care access, and (5) VM use is higher in underweight children and adolescents compared with those who are not underweight.
METHODS
We analyzed the NHANES 1999–2004, which contains nationally representative data on comprehensive dietary supplement use in the United States. Sampling weights were used to produce population estimates, and subgroups oversampled included those with low incomes as well as African American individuals, Mexican American individuals, and adolescents.17 The survey entailed administration of a questionnaire, a household interview, and a medical examination. Signed consent was provided by parents of all children, and adolescents additionally signed an information form.
Our study sample included 10 828 children, aged 2 to 17 years, who had parent- or guardian-reported response to the VM supplement intake question and measured height and weight. Aggregate response rates for the NHANES 1999–2004 interview component were approximately 82% and completion rates for the medical examination component were 77%.17
VM SUPPLEMENT DATA COLLECTION
Intake of VM in the NHANES database was measured by determining whether the child had used any VM supplements in the 30 days prior to the interview, as well as the frequency and duration of supplement use. Parents were shown a card with examples of multiple types of VM supplements. Interviewers additionally recorded names of supplements from container labels. If a container was unavailable, the interviewer asked for the exact name of the product. If the exact name was unknown, general category of VM supplement was assessed. Trained NHANES nutritionists subsequently matched and categorized supplement databases on standardized classification rules.17
SOCIODEMOGRAPHIC AND FOOD SECURITY DATA COLLECTION
Demographic characteristics of subjects included age, sex, race/ethnicity, country of birth, poverty status, and food security. We stratified the age variable into the following 3 categories: 2 to 4 years (preschool age), 5 to 11 years (school age), and 12 to 17 years (adolescents). We categorized poverty status into the following 3 categories: living below the poverty level (<1 poverty income ratio), near poor (1 to <2 poverty income ratio), and nonpoor (≥2 poverty income ratio). Food security data were classified within the NHANES as food secure, marginally food secure, food insecure without hunger, and food insecure with hunger. Additional information on food security in the NHANES relates to receipt of food assistance in the form of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) benefits, food stamps, and reduced-price or free school meals.
HEALTH STATUS AND HEALTH CARE ACCESS DATA COLLECTION
Medical and health care access factors included current health status, long-term health problems, health insurance coverage, access to a routine place for health care, place used most often for health care, number of times health care was received over the past year, and length of time since last health care visit. We used measured height and weight to calculate age- and sex-specific body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared). We then classified BMI as underweight (<fifth BMI percentile), healthy weight (fifth to <85th BMI percentile), overweight (≥85th to <95th BMI percentile), and obese (≥95th BMI percentile).18,19
NUTRITION AND PHYSICAL ACTIVITY DATA COLLECTION
Nutrition behavior was assessed during the NHANES interview by the number of times per week restaurant food was eaten, number of times per month dark-green vegetables were eaten, and frequency of milk consumption in the past 30 days. The frequency of milk consumption was reported as never, rarely (less than once a week), sometimes (once a week or more but less than once a day), or often (once a day or more). Nutrient intake was determined from foods and beverages reported in the 24-hour dietary recall. Intake of micronutrients commonly present in multivitamin and mineral supplements was additionally considered. The intake of each nutrient variable was categorized into terciles prior to analysis.
Physical activity was assessed during the NHANES interview by determining the frequency and duration of walking or bicycling over the past month for those 12 years and older. The level of self-reported physical activity in the past month was classified in the NHANES database as vigorous (causing heavy sweating or a large increase in breathing or heart rate for at least 10 minutes) or moderate activity (causing light sweating or a slight to moderate increase in breathing or heart rate for at least 10 minutes). Subjects were also asked to compare their level of physical activity with others of the same age. Sedentary activity was assessed by asking about the number of hours per day of television/video viewing and computer use.
STATISTICAL ANALYSIS
Data were analyzed using SAS for Windows (SAS Institute, Inc, Cary, North Carolina) and SUDAAN (Research Triangle Institute, Research Triangle Park, North Carolina), a statistical package that accounts for the complex survey design of the NHANES. All analyses were weighted and adjusted for nonresponse to be representative of the US population. χ2 Tests were used to compare the prevalence of VM use by sociodemographic, health status, health care access, nutrition, and physical activity characteristics. Multivariable logistic regression was used to examine associations of VM use with age, sex, race/ethnicity, country of birth, and poverty. In addition, independent associations with nutritional factors, food security, physical activity, and health care access were assessed controlling for race and poverty interactions.
RESULTS
In the previous 30 days, 34.2% (SE 1.2) of 2- to 17-year-old children and adolescents in our sample had taken a VM supplement (Table 1). Almost half of children and adolescents took VM supplements daily.
Table 1.
Prevalence of VM Supplement Use Among 10 828 Children and Adolescents by Sociodemographic Characteristics, National Health and Nutrition Examination Survey, United States, 1999–2004
| Characteristic | VM Users, % (SE) | P Value |
|---|---|---|
| Overall | 34.2 (1.2) | |
| Age, y | ||
| 2–4 | 43.1 (2.0) | <.001a |
| 5–11 | 37.4 (1.7) | |
| 12–17 | 26.6 (0.9) | |
| Sex | ||
| M | 33.0 (1.3) | .11 |
| F | 35.4 (1.5) | |
| Race/ethnicity | ||
| Mexican American | 23.8 (1.4) | <.001a |
| Other Hispanic | 29.9 (3.2) | |
| Non-Hispanic white | 41.5 (1.6) | |
| Non-Hispanic African American | 18.1 (1.0) | |
| Other race (including multiracial) | 26.7 (3.1) | |
| Country of birth | ||
| United States | 35.1 (1.2) | <.001a |
| Mexico | 13.2 (1.8) | |
| Elsewhere | 23.1 (3.5) | |
| Poverty status | ||
| Below poverty level (<1 poverty income ratio) | 22.3 (1.3) | <.001a |
| Near poor (1 to <2 poverty income ratio) | 26.7 (2.2) | |
| Nonpoor (>2 poverty income ratio) | 43.1 (1.5) | |
| Household food security category | ||
| Fully food secure | 37.6 (1.3) | <.001a |
| Marginally food secure | 23.9 (2.6) | |
| Food insecure without hunger | 21.6 (2.3) | |
| Food insecure with hunger | 25.9 (3.7) | |
| Adult food security category | ||
| Fully food secure | 37.5 (1.3) | <.001a |
| Marginally food secure | 23.7 (2.3) | |
| Food insecure without hunger | 21.1 (2.3) | |
| Food insecure with hunger | 25.1 (3.4) | |
| Child food security category | ||
| Food quality and quantity unaffected | 36.1 (1.2) | <.001a |
| Marginally food secure | 26.2 (3.4) | |
| Reduced food quality or quantity | 23.9 (2.1) | |
| Food insecure with hunger | 15.0 (6.6) | |
| Authorized for food stamps in past year | ||
| Respondent authorized for food stamps | 18.0 (2.4) | <.001a |
| Other household member authorized for food stamps | 19.3 (3.6) | |
| No one in household authorized for food stamps | 38 (1.4) | |
| No. of months authorized for food stamps in past year | ||
| None | 36.3 (1.3) | <.001a |
| 1–11 | 25.1 (5.7) | |
| 12 | 13.3 (2.9) | |
| No. of people in household authorized for food stamps | ||
| None | 38.0 (1.4) | <.001a |
| 1 Person | 20.5 (3.8) | |
| ≥2 People | 16.9 (2.3) | |
| Participated in WIC program | ||
| Yes | 24.2 (2.3) | <.001a |
| No | 36.9 (1.4) | |
| School breakfast price (≥4 y) | ||
| Free | 18.4 (2.0) | .03a |
| Reduced price | 17.8 (4.4) | |
| Full price | 36.7 (5.3) | |
| School lunch price (≥4 y) | ||
| Free | 17.4 (1.1) | <.001a |
| Reduced price | 29.2 (3.3) | |
| Full price | 40.2 (2.0) |
Abbreviations: VM, vitamin and mineral; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Statistically significant.
BIVARIATE ANALYSES
Sociodemographic Characteristics and Food Security
Prevalence of VM use was significantly higher in younger age groups, with the prevalence in 2- to 4-year-olds, 5- to 11-year-olds, and 12- to 17-year-olds being 43.1%, 37.4%, and 26.6%, respectively (P < .001). There was no significant difference in VM use by sex. Non-Hispanic white individuals were statistically significantly more likely to be users of VM supplements and non-Hispanic African American individuals were least likely to be VM users. Children and adolescents born in the United States and those living in households with higher incomes were more likely to use VM supplements. Users of VM supplements were more likely to live in households that were fully food secure or experienced food insecurity with hunger than in households that were marginally food secure or food insecure without hunger. Additionally, users of VM supplements were more likely to live with adults who were fully food secure or experienced food insecurity with hunger than with adults who were marginally food secure or experienced food insecurity without hunger. Analysis of child and adolescent food security demonstrated a statistically significant relationship with VM use; the prevalence of VM supplement use was highest among those whose food quality and quantity remained unaffected (36.1%) and declined if children or adolescents were marginally food secure (26.2%), experienced reduced food quality or quantity (23.9%), and experienced food insecurity with hunger (15%). Users of VM supplements were significantly less likely to receive food assistance in the form of WIC benefits, food stamps, and reduced-price or free school meals (Table 1).
Health Status and Health Care Access
Use of VM supplements was significantly higher in children and adolescents whose health status was reported as excellent (37.1%) or very good (34.7%) compared with those whose health status was reported as good (26.7%) or fair/poor (28.3%). There was no association of VM supplement use with self-reported long-term health impairment. Use of VM supplements showed a statistically significant relationship with BMI category; the prevalence of VM use was highest among those who were underweight (41.6%) and declined in those who were a healthy body weight (36.0%), overweight (30.5%), or obese (28.6%). Those with health insurance coverage were more likely to use VM supplements compared with those without health insurance. Children and adolescents who reported having a routine place to go for health care were significantly more likely to use VM supplements than those without a routine place to go for health care. Use of VM supplements was more prevalent in children and adolescents whose usual source of health care was a physician’s office or freestanding health maintenance organization (38.5%), compared with those whose usual source of care was a community health center (24.6%) or an emergency department (18.0%). Analysis of the number of times health care was received over the past year demonstrated a statistically significant relationship with VM use; the prevalence of VM supplement use was highest among those who received health care 4 or more times in the last year (39.1%) and was lowest if no health care was obtained in the last year (25.3%). Children and adolescents who reported receiving health care services more frequently over the past year (≥4 times per year) also reported more VM use. Those who reported their last health care visit to have occurred in the past year were significantly more likely to use VM supplements than those who had health care visits 2 or more years ago (Table 2).
Table 2.
Prevalence of VM Supplement Use Among 10 828 Children and Adolescents by Health Status and Health Care Access, National Health and Nutrition Examination Survey, United States, 1999–2004
| Characteristic | VM Users, % (SE) | P Value |
|---|---|---|
| General health condition | ||
| Excellent | 37.1 (1.5) | <.001a |
| Very good | 34.7 (1.5) | |
| Good | 26.7 (1.4) | |
| Fair/poor | 28.3 (3.4) | |
| Long-term impairment/health problem | ||
| Yes (n=302) | 34.0 (4.4) | .74 |
| Impaired but not long-term (n=69) | 44.2 (12.0) | |
| No impairment (n=10 438) | 34.2 (1.2) | |
| BMI percentile for age and sex | ||
| Underweight (<5th BMI percentile) | 41.6 (4.2) | .001a |
| Healthy weight (5th to <85th BMI percentile) |
36.0 (1.4) | |
| Overweight (≥85th to <95th BMI percentile) |
30.5 (1.7) | |
| Obese (≥95th BMI percentile) | 28.6 (1.9) | |
| Covered by health insurance (private or public) |
||
| Yes | 35.2 (1.2) | <.001a |
| No | 26.4 (2.2) | |
| Routine place to go for health care | ||
| Yes | 34.8 (1.2) | .003a |
| No | 24.9 (2.9) | |
| Type of place most often go for health care | ||
| Clinic/health center | 24.6 (1.7) | <.001a |
| Physician’s office/health maintenance organization |
38.5 (1.5) | |
| ED/OPD/other | 18.0 (3.9) | |
| No usual place | 24.9 (2.9) | |
| No. of times received health care over past year |
||
| None | 25.3 (2.9) | <.001a |
| 1 | 31.4 (1.8) | |
| 2–3 | 35.6 (1.2) | |
| ≥4 | 39.1 (1.7) | |
| How long since last health care visit, y | ||
| In the past year | 35.4 (1.2) | .001a |
| 2–3 | 25.7 (2.7) | |
| >3/Never | 23.7 (6.4) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ED, emergency department; OPD, outpatient department; VM, vitamin and mineral;
Statistically significant.
Nutrition and Physical Activity
Use of VM supplements was lowest in children and adolescents who never ate restaurant food or ate it less than weekly (29.3%), compared with those who ate restaurant food 1 or more times a week (35.9%). There was no relationship of VM supplement use with frequency of dark-green vegetable consumption. Use of VM supplements was significantly associated with frequency of milk consumption in the past 30 days. When dietary intakes of specific nutrients were assessed, those with higher dietary fiber intake, lower-tercile total fat, and lower- and middle tercile cholesterol intake reported higher VM use. There was no difference in VM use with respect to dietary intake of energy, protein, carbohydrates, total sugars, and total saturated fat. Those with higher intakes of micronutrients commonly present in VM supplements, namely vitamin A, thiamine, riboflavin, niacin, vitamin B6, folic acid, vitamin B12, vitamin C, calcium, iron, and zinc, all had greater reported VM use.
Subjects 12 years and older who participated in vigorous physical activity in the past month and who reported that they were more physically active compared with others of the same age were significantly more likely to use VM supplements. In addition, adolescents who participated in moderate physical activity in the past month and those more likely to have played or exercised hard showed a trend toward more VM use, although the association was not statistically significant. Adolescents who used VM supplements were statistically significantly more likely to report that they were more physically active compared with others of the same age. Use of VM supplements was significantly associated with lower (≤2 hours per day) of television/ video viewing or computer use (Table 3).
Table 3.
Prevalence of VM Supplement Use Among 10 828 Children and Adolescents by Physical Activity and Nutrition Characteristics, National Health and Nutrition Examination Survey, United States, 1999–2004
| Characteristic | VM Users, % (SE) | P Value |
|---|---|---|
| Walked or bicycled over past 30 d (age ≥12 y) | ||
| Yes | 25.8 (1.4) | .38 |
| No | 27.6 (1.3) | |
| Vigorous activity over past 30 d (age ≥12 y) | ||
| Yes | 29.0 (1.0) | .001a |
| No | 20.5 (2.1) | |
| Moderate activity over past 30 d (age ≥12 y) | ||
| Yes | 28.0 (1.2) | .10 |
| No | 24.4 (1.6) | |
| No. of times/wk play or exercise hard (age 2–11 y) |
||
| <7 | 38.5 (1.8) | .66 |
| ≥7 | 39.4 (2.0) | |
| Compare activity with others the same age (age ≥12 y) |
||
| More active | 30.6 (1.6) | .02a |
| Less active | 26.4 (2.5) | |
| About the same | 24.8 (1.1) | |
| No. of hours/d of television, video, or computer use |
||
| ≤2 | 38.2 (1.6) | <.001a |
| >2 | 30.2 (1.2) | |
| No. of times/wk eat restaurant food | ||
| Never/less than weekly | 29.3 (2.0) | .001a |
| ≥1 | 35.9 (1.2) | |
| No. of times/mo eat dark-green vegetables (2001–2002 only) |
||
| Never/less than monthly | 37.6 (2.6) | .10 |
| 1–4 | 38.2 (3.1) | |
| 5–8 | 35.1 (4.3) | |
| 9–13 | 32.1 (2.9) | |
| 14–29 | 40.4 (4.1) | |
| ≥30 | 39.4 (3.1) | |
| Past 30-d milk product consumption | ||
| Never/rarely | 26.3 (2.7) | .006a |
| Sometimes | 29.9 (1.9) | |
| Often | 35.5 (1.3) | |
| Energy intake | ||
| Lower tercile | 34.8 (1.6) | .32 |
| Middle tercile | 34.8 (1.5) | |
| Upper tercile | 32.8 (1.2) | |
| Protein intake | ||
| Lower tercile | 33.2 (1.7) | .16 |
| Middle tercile | 36.0 (1.5) | |
| Upper tercile | 33.2 (1.2) | |
| Carbohydrate intake | ||
| Lower tercile | 32.7 (1.8) | .45 |
| Middle tercile | 34.7 (1.5) | |
| Upper tercile | 35.0 (1.5) | |
| Total sugar intake (2001–2004 only) | ||
| Lower tercile | 34.5 (2.0) | .72 |
| Middle tercile | 35.7 (2.1) | |
| Upper tercile | 36.0 (1.6) | |
| Dietary fiber intake | ||
| Lower tercile | 31.5 (1.5) | .04a |
| Middle tercile | 34.6 (1.8) | |
| Upper tercile | 36.4 (1.5) | |
| Total fat intake | ||
| Lower tercile | 36.4 (1.6) | .04a |
| Middle tercile | 34.0 (1.7) | |
| Upper tercile | 32.1 (1.3) | |
| Total saturated fat intake | ||
| Lower tercile | 34.7 (1.7) | .46 |
| Middle tercile | 34.9 (1.4) | |
| Upper tercile | 32.8 (1.6) | |
| Cholesterol intake | ||
| Lower tercile | 35.3 (1.8) | .03a |
| Middle tercile | 35.4 (1.5) | |
| Upper tercile | 31.7 (1.2) | |
| Vitamin A intake (RAE) (2001–2004 only) | ||
| Lower tercile | 28.3 (1.9) | <.001a |
| Middle tercile | 37.3 (2.2) | |
| Upper tercile | 40.6 (2.0) | |
| Thiamine intake | ||
| Lower tercile | 32.0 (1.6) | .02a |
| Middle tercile | 36.3 (1.6) | |
| Upper tercile | 34.1 (1.4) | |
| Riboflavin intake | ||
| Lower tercile | 28.6 (1.5) | <.001a |
| Middle tercile | 36.2 (1.7) | |
| Upper tercile | 37.7 (1.4) | |
| Niacin intake | ||
| Lower tercile | 32.6 (1.7) | .18 |
| Middle tercile | 35.6 (1.4) | |
| Upper tercile | 34.3 (1.4) | |
| Vitamin B6 intake | ||
| Lower tercile | 32.1 (1.7) | .10 |
| Middle tercile | 35.8 (1.4) | |
| Upper tercile | 34.5 (1.3) | |
| Folic acid intake (2001–2004 only) | ||
| Lower tercile | 33.9 (2.2) | .34 |
| Middle tercile | 35.6 (2.1) | |
| Upper tercile | 36.8 (1.9) | |
| Vitamin B12 intake | ||
| Lower tercile | 31.5 (1.3) | .008a |
| Middle tercile | 34.1 (1.9) | |
| Upper tercile | 36.9 (1.4) | |
| Vitamin C intake | ||
| Lower tercile | 31.0 (1.7) | .02a |
| Middle tercile | 35.9 (1.3) | |
| Upper tercile | 35.6 (1.6) | |
| Calcium intake | ||
| Lower tercile | 28.5 (1.6) | <.001a |
| Middle tercile | 36.4 (1.5) | |
| Upper tercile | 37.5 (1.6) | |
| Iron intake | ||
| Lower tercile | 32.1 (1.6) | .06 |
| Middle tercile | 36.1 (1.6) | |
| Upper tercile | 34.2 (1.3) | |
| Zinc intake | ||
| Lower tercile | 32.4 (1.6) | .07 |
| Middle tercile | 36.1 (1.4) | |
| Upper tercile | 33.9 (1.4) |
Abbreviations: RAE, retinol activity equivalents; VM, vitamin and mineral.
Statistically significant.
MULTIVARIATE ANALYSES
Table 4 presents a multivariate model analysis of adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for the following sociodemographic characteristics: age, sex, race/ethnicity, country of birth, and poverty status. Significant positive associations for the use of VM supplements were noted for younger (2–4 years, OR, 2.5 and 5–11 years, OR, 1.8) and nonpoor (OR, 2.2) children and adolescents. Mexican American (OR, 0.6) and African American (OR, 0.4) children were less likely to use VM supplements than white children. Mexican-born children (OR, 0.6) were less likely to use VM supplements than US-born children.
Table 4.
Demographic Characteristics Independently Associated With Vitamin and Mineral Supplement Use, National Health and Nutrition Examination Survey, United States, 1999–2004
| Characteristic | Odds Ratio (95% Confidence Interval) | P Value |
|---|---|---|
| Age, y | ||
| 2–4 | 2.5 (2.0–3.0) | <.001 |
| 5–11 | 1.8 (1.5–2.1) | <.001 |
| 12–17 | 1 [Reference] | |
| Sex | ||
| M | 0.9 (0.8–1.03) | .13 |
| F | 1 [Reference] | |
| Race/ethnicity | ||
| Mexican American | 0.6 (0.5–0.7) | <.001 |
| Other Hispanic | 0.8 (0.6–1.1) | .10 |
| Non-Hispanic white | 1 [Reference] | |
| Non-Hispanic African American | 0.4 (0.3–0.5) | <.001 |
| Other race/multiracial | 0.6 (0.4–0.8) | .005 |
| Country of birth | ||
| United States | 1 [Reference] | |
| Mexico | 0.6 (0.4–0.9) | .01 |
| Elsewhere | 0.7 (0.5–1.2) | .17 |
| Poverty status | ||
| Below poverty level (<1 poverty income ratio) |
1 [Reference] | |
| Near poor (1 to <2 poverty income ratio) |
1.1 (0.9–1.4) | .34 |
| Nonpoor (>2 poverty income ratio) | 2.2 (1.9–2.6) | <.001 |
When controlling for race × poverty interactions, the following characteristics were associated with increased odds of VM use: having 2 or more visits to a health care provider in the past year (OR, 1.4), greater activity levels compared with others in the same age group (OR, 1.3), and 2 hours or less of television/video/computer use per day (OR, 1.3). The following were associated with lower use of VM: good health status compared with excellent health (OR, 0.81; 95% CI, 0.67–0.98) and obtaining health care at a community health center (OR, 0.76; 95% CI, 0.61–0.94) or emergency department (OR, 0.57; 95% CI, 0.32–0.99) compared with a physician’s office. Adult or child food security, having a routine place to go for health care, frequency of eating restaurant food, milk product intake, and vigorous activity in those 12 years and older were not associated with VM use when accounting for the interaction of race and poverty.
Frequency of health care visits, diet and physical activity patterns, and sedentary behaviors may potentially vary by age group. Therefore, we constructed 5 separate regression models to adjust for the effect of age of the child on each of the following variables: number of health care visits in the past year, how long ago the last health care visit occurred, frequency of eating restaurant food, frequency of milk consumption in the past 30 days, and hours per day of television/video viewing or computer use. The only variable that became nonsignificant when controlling for age of the child was milk consumption (P = .23). All others variables remained significant at P < .01.
COMMENT
More than one-third of the 10 828 children and adolescents 2 to 17 years of age in the 1999–2004 NHANES took VM supplements in the preceding month. Our results supported our hypothesis that underweight children would have the highest use of VM supplements. However, in contrast to what we expected to find, children and adolescents with healthier nutrition, more active lifestyles, greater food security, and greater health care access were more likely to use VM supplements.
Published literature supports the high prevalence of VM use. More than half of all 3-year-olds in the 1991 Longitudinal Follow-up to the 1988 National Maternal and Infant Health Survey used a VM supplement.9 Consistent with our study’s findings, children who received supplementation tended to have eating problems or poor appetites. Mothers who gave their children supplements were more likely to be non-Hispanic white, married, and older and have higher education and greater household income than mothers who did not give their children supplements.9 Data from the 1981 Child Health Supplement to the National Health Interview Survey (NHIS) demonstrate that approximately 50% of children from birth to 6 years of age received a VM supplement.10 In a study using 1986 NHIS data, 43% of children aged 2 to 6 years received VM supplements in the previous 2 weeks.1 Results from the Fourth Child and Adolescent Trial for Cardiovascular Health study demonstrated that one in four 12th graders used VM supplements.4,11 Consistent with our findings, other studies have demonstrated that adolescents who use VM supplements tend to have more healthful diets, lower television viewing, greater levels of physical activity, greater participation in team and organized sports, and less obesity than those who do not.4,5
More recently, Picciano et al20 examined dietary supplement use among infants, children, and adolescents in the United States using the 1999–2002 NHANES data set. Dietary supplement use was associated with higher family income, not participating in the WIC program, a smoke-free environment, less screen-viewing time (television, video games, and computer use), and lower BMI. The association of dietary supplement (specifically VM) use with nutrition, food security, physical activity, and health care access was not examined.20 Therefore, analyses of other national data sets show demographic and lifestyle characteristic associations similar to those in our study, with higher VM use among non-Hispanic white individuals and those with higher socioeconomic status, healthier diets, and level of physical activity as well as those with less obesity.
Dixon et al21 analyzed the Third NHANES to determine if dietary intakes and serum nutrient levels differed between adults from food-insufficient and food-sufficient families. After adjusting for family income, adults from food-insufficient families had lower intakes of milk products, fruits and vegetables, energy, calcium, vitamin E, vitamin B6, iron, and zinc. Our study did not find any association between adult or child food security and VM use after controlling for poverty.
Strengths of our study are that the NHANES yields a nationally representative sample and provides respondent sampling weights to account for nonresponse and selection bias. The in-person interview and rigorous methods of classifying VM supplements enable high-quality data collection. We acknowledge the following limitations of this study: (1) We did not include other dietary supplement use in our analyses; the rationale for focusing on VM supplements was that published data demonstrate that VMs are the most commonly used dietary supplements both in children and adults.2 (2) Analysis of individual components of VM preparations was beyond the scope of this study. (3) The NHANES data use a short referent time frame of the past 30 days to assess VM supplement use. Although this time frame is used to increase accuracy of self-report and for comparability with other NHANES data, it may not provide a complete picture of VM use. For example, the short time frame may not capture episodic use of VM supplements, such as supplemental vitamin C use during viral upper respiratory tract infections, if the most recent infection was prior to the 30-day period. (4) Since NHANES data are cross-sectional, analyses of VM supplement use with the lifestyle and health conditions measured in NHANES cannot presume causality, but only an association. In spite of these limitations, we believe that the results of our study offer guidance to health care providers on the extent of data gathering and counseling needed regarding diet, physical activity, and VM supplement use during clinical encounters.
Our study indicates that children and adolescents who may face the greatest risks for VM deficiencies, such as those with less healthy nutrition and activity patterns, greater obesity, lower income, lower food security, poorer health, and lower health care access, use VM supplements the least. There exist multiple competing demands for limited financial resources in families facing financial disparities, and purchasing VM supplements to mitigate the ill effects of a suboptimal diet might not take precedence for such families. Thus, although individuals’ perceptions within the framework of the HBM may play a role in their intentions to use VM supplements, modifying factors, such as financial ability to purchase VM supplements, as depicted in the Figure, may supersede such intentions. We also note that sociodemographic factors influencing VM supplement use are similar to those affecting health behaviors related to maintaining a nutritious diet, greater physical activity, and healthy body weight.
Figure 1.
The Health Belief Model as a framework to explain vitamin and mineral (VM) supplement use.
Some children and adolescents who are underweight may potentially benefit from VM supplementation, but for other groups of VM users, medical benefits are less clear. Since VM supplements significantly contribute to total nutrient intakes in children and adolescents, history of their use and reasons for using them should be specifically elicited. Because of greater health care access of VM supplement users, health care providers are well positioned to screen patients regarding nutritional quality of their diet and VM supplement use. Health care providers can then counsel parents that the American Academy of Pediatrics does not recommend use of VM supplements in children and adolescents with varied and healthy diets. It is important to counsel parents of underweight children that use of VM supplements is not a substitute for a physiologically appropriate diet. Our study also suggests that since VM supplements contribute significantly to total dietary intakes of vitamins and minerals, epidemiologic and clinical studies of nutrition should include assessment of VM supplement use. Further qualitative research is needed to explore the relative importance of factors that influence parental decision to use VM supplements for their children, especially in those groups of children who face the highest risks of VM deficiencies.
Acknowledgments
Funding/Support: This publication was made possible by grant S-CMNSU04 from the University of California Davis Medical Center Children’s Miracle Network and grant UL1 RR024146 from the National Center for Research Resources, a component of the National Institutes of Health.
Footnotes
Author Contributions: Study concept and design: Shaikh and Byrd. Acquisition of data: Shaikh, Byrd, and Auinger. Analysis and interpretation of data: Shaikh, Byrd, and Auinger. Drafting of the manuscript: Shaikh. Critical revision of the manuscript for important intellectual content: Byrd and Auinger. Statistical analysis: Shaikh, Byrd, and Auinger. Obtained funding: Shaikh. Study supervision: Byrd.
Financial Disclosure: None reported.
REFERENCES
- 1.Moss AJ, Levy AS, Kim I, Park YK. Use of Vitamin and Mineral Supplements in the United States: Current Users, Types of Products, and Nutrients. Hyattsville, MD: National Center for Health Statistics; 1989. Advance Data From Vital and Health Statistics No. 174. [Google Scholar]
- 2.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160(4):339–349. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 3.Ervin RB, Wright JD, Reed-Gillette D. Prevalence of leading types of dietary supplements used in the Third National Health and Nutrition Examination Survey, 1988–1994. Adv Data. 2004;349(349):1–7. [PubMed] [Google Scholar]
- 4.Dwyer JT, Garceau A, Evans M, et al. Do adolescent vitamin-mineral supplement users have better nutrient intakes than nonusers? Observations from the CATCH tracking study. J Am Diet Assoc. 2001;101(11):1340–1346. doi: 10.1016/s0002-8223(01)00321-2. [DOI] [PubMed] [Google Scholar]
- 5.Stang J, Story M, Harnack L, Neumark-Sztainer D. Relationships between vitamin and mineral supplement use, dietary intake, and dietary adequacy among adolescents. J Am Diet Assoc. 2000;100(8):905–910. doi: 10.1016/S0002-8223(00)00262-5. [DOI] [PubMed] [Google Scholar]
- 6.Lyle BJ, Mares-Perlman JA, Klein BE, Klein R, Greger JL. Supplement users differ from nonusers in demographic, lifestyle, dietary, and health characteristics. J Nutr. 1998;128(12):2355–2362. doi: 10.1093/jn/128.12.2355. [DOI] [PubMed] [Google Scholar]
- 7.Council for Responsible Nutrition. 1988 Overview of the Nutritional Supplement Market. Washington, DC: Council for Responsible Nutrition; 1989. [Google Scholar]
- 8.Kleinman RE. Pediatric Nutrition Handbook. 5th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2004. [Google Scholar]
- 9.Yu SM, Kogan MD, Gergen P. Vitamin-mineral supplement use among preschool children in the United States. [Accessed February 3, 2006];Pediatrics. 1997 100(5):E4. doi: 10.1542/peds.100.5.e4. http://pediatrics.aappublications.org/cgi/content/full/100/5/e4. [DOI] [PubMed] [Google Scholar]
- 10.Kovar MG. Use of medication and vitamin-mineral supplements by children and youths. Public Health Rep. 1985;100(5):470–473. [PMC free article] [PubMed] [Google Scholar]
- 11.Reaves L, Steffen LM, Dwyer JT, et al. Vitamin supplement intake is related to dietary intake and physical activity: the Child and Adolescent Trial for Cardiovascular Health (CATCH) J Am Diet Assoc. 2006;106(12):2018–2023. doi: 10.1016/j.jada.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 12.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 13.Shillitoe RW, Christie MJ. Determinants of self-care: the health belief model. J Interprof Care. 1989;4(1):3–17. [Google Scholar]
- 14.Kloeblen AS, Batish SS. Understanding the intention to permanently follow a high folate diet among a sample of low-income pregnant women according to the Health Belief Model. Health Educ Res. 1999;14(3):327–338. doi: 10.1093/her/14.3.327. [DOI] [PubMed] [Google Scholar]
- 15.Tussing L, Chapman-Novakofski K. Osteoporosis prevention education: behavior theories and calcium intake. J Am Diet Assoc. 2005;105(1):92–97. doi: 10.1016/j.jada.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 16.Glanz K, Lewis FM, Rimer BK. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed. Indianapolis, IN: Jossey-Bass Inc; 2002. [Google Scholar]
- 17.Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed September 12, 2007];National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/about/major/nhanes/nhanes_cps_totals.htm. Updated August 28, 2007.
- 18.Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed June 30, 2007];National Health and Nutrition Examination Survey Z-score Data Files. http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/zscore/zscore.htm.
- 19.Barlow SE. Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 20.Picciano MF, Dwyer JT, Radimer KL, et al. Dietary supplement use among infants, children, and adolescents in the United States, 1999–2002. Arch Pediatr Adolesc Med. 2007;161(10):978–985. doi: 10.1001/archpedi.161.10.978. [DOI] [PubMed] [Google Scholar]
- 21.Dixon LB, Winkleby MA, Kathy L, Radimer KL. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988–1994. J Nutr. 2001;131(4):1232–1246. doi: 10.1093/jn/131.4.1232. [DOI] [PubMed] [Google Scholar]