Abstract
Objective
To compare practice settings and activities of pharmacists with bachelor of science (BS) in pharmacy and doctor of pharmacy (PharmD) degrees.
Methods
Data from the 2009 National Pharmacist Workforce Survey instrument were analyzed. Multivariate regression was used to examine the association of the PharmD degree with time spent in dispensing and patient care.
Results
The survey response rate by pharmacists was 52%, and 562 usable responses met our inclusion criteria. Sixty-three percent of BS and 39% of PharmD pharmacists were employed in community pharmacies, compared with 21% of BS and 38% of PharmD pharmacists employed in hospital pharmacy settings. Practicing in a community setting had the strongest influence on time spent in dispensing and time spent in patient care. Among respondents with PharmD degrees, a residency was associated with less time in dispensing and more time in patient care.
Conclusion
Time spent in dispensing and patient care were influenced more by practice setting than by educational degree and residency training.
Keywords: degrees, graduates, pharmacist, workforce
INTRODUCTION
In 1948, the American Council on Education (ACE) recommended that the professional pharmacy curriculum be a 6-year program.1 Soon after, a few colleges and schools adopted the PharmD as the first professional degree for pharmacists. In the more than 50 years that ensued, additional colleges and schools developed PharmD curricula, with many offering post-BS PharmD degrees for practicing pharmacists or new graduates seeking to advance their educational background. In June 1997, the American Council for Pharmacy Education (ACPE) officially adopted new accreditation standards, requiring the PharmD as the sole, first pharmacy degree, effective July 2000.
The path to adopting the PharmD as the first professional degree for pharmacy practice was filled with debate. Arguments were made that the change should be based on the needs and demands for clinical roles, and to enhance the profession's contributions to society. Increased prospects for career opportunities and improved professional image also were offered by proponents of the change. To the contrary, there were concerns that the new standards would create overqualified pharmacists, especially community pharmacists involved in technical dispensing functions.2,3 The debate about whether moving toward a universal degree was the right choice for pharmacy continued even after the mandate that the PharmD degree be the sole first professional degree was implemented.4 There has been a call for greater preparation, requiring residencies for pharmacists who will provide direct patient care.5
The changed first professional degree requirements have created a workforce of pharmacists who have been prepared differently for practice. Compared to curricula for BS degrees, PharmD curricula were extended by 1 year to include additional coursework in pharmacotherapy and patient care, plus expanded experiential learning with specified activities and exercises emphasizing clinical skills. Consequently, examining whether and how pharmacists differ in terms of practice setting and practice activities, such as dispensing drugs and providing drug-related patient management, is important. By examining activities of BS and PharmD degree graduates, particularly recent PharmD degree graduates, we can begin to evaluate the change to the PharmD and how different training may be translated into practice. Findings about whether and how pharmacists' practice activities have changed since transitioning to the PharmD degree also may provide some evidence about the potential implications of requiring residency training for pharmacists to provide direct patient care.
Several studies comparing practice patterns and job satisfaction of PharmD and BS degreed pharmacists were conducted before the PharmD degree requirement was adopted.6-9 Those studies showed that BS graduates were more likely to be employed in a community setting than in a hospital setting. Pharmacists' satisfaction did not differ consistently by degree, and the amount of time in clinical activities and direct patient care was relatively small and did not differ by degree. For example, in 1988, Cox and Carroll reported that pharmacists, regardless of degree, spent more than half their time in drug distribution and less than 15% of their time, on average, was devoted to direct patient care.7 Other studies have focused on individuals who completed non-traditional PharmD degrees to raise their educational credentials to the newer, higher standards. These studies suggest that completing the nontraditional PharmD degree was associated with a change in position, increased satisfaction, and involvement in more patient care and clinical activities at the pharmacists' work sites.10-13
Our literature review found no studies that compared PharmD and BS degreed pharmacists since adoption of the PharmD as the first professional degree requirement. Our first objective was to use a national sample of pharmacists to update previous studies that examined practice settings for pharmacists with different practice degrees. Further, with the emergence of more specialized practice roles for pharmacists and growing recognition that pharmacists can play a role beyond dispensing prescription drugs, examining whether and how the PharmD degree is associated with pharmacists' practice activities is important. Thus, the second objective of this study was to compare the work activities of pharmacists with PharmD and/or BS in pharmacy degrees.
METHODS
Data from the 2009 National Pharmacist Workforce Survey study were analyzed. These data were collected from a random sample of pharmacists in all states, using a mailing list from KM Lists, Inc. (Marlton, NJ) via a self-administered survey questionnaire deployed using Dillman's survey method principles with multiple follow-ups.14 A prenotification letter was mailed to 3,000 licensed pharmacists that instructed them to return the letter if they did not wish to participate or were not a licensed pharmacist. After removing from the original mailing list addresses for which the prenotification letter was returned as undeliverable, addresses of nonpharmacists, and addresses of pharmacists who indicated they were not able or unwilling to participate, survey packets were mailed to 2,667 pharmacists. The survey instrument included sections on: general employment status and work environment; work, work activities, and work parameters; and demographic and career information.
The analytic data file was restricted to responses from pharmacists who reported they were neither retired, unemployed, or not employed in a pharmacy-related career. Also, the analytical sample was restricted to respondents who had graduated from a college or school of pharmacy and were first licensed in 1984 or later, to provide a cohort of pharmacists who would have graduated from colleges or schools with curricula that included a clinical pharmacy component prior to adoption of the all PharmD degree. Preliminary analyses also revealed few PharmDs among graduates prior to 1984.
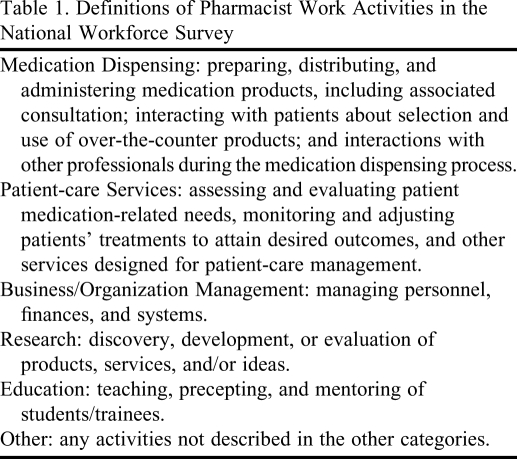
Variables included in this study were pharmacist demographics (gender, age, marital status, ethnicity), practice parameters (setting, urban/rural practice location, position), educational background (pharmacy degrees earned, whether they completed a residency or fellowship), and years of experience as a pharmacist (derived from self-reported year first licensed). As one of the work parameters, pharmacists were asked to estimate, for a typical week, the percentage of actual time spent in medication dispensing, patient-care services, business/organization management, research, education, and other activities (Table 1). Similar activity classifications have been used in previous national and state workforce survey instruments conducted by the authors and researchers studying pharmacist activities, degrees, and satisfaction, prior to the change to the PharmD first professional degree.15,16 Respondents' percentage of time estimates that did not sum to 100% (4 cases) were standardized to total 100%.
Table 1.
Definitions of Pharmacist Work Activities in the National Workforce Survey
Data were analyzed using SPSS (SPSS Inc, Chicago, IL). For the descriptive, univariate analyses comparing characteristics and time spent in professional activities, respondents were categorized into 3 groups: BS graduates, PharmD graduates, and graduates with both BS and PharmD degrees (post-BS PharmD graduates). Analysis of variance (ANOVA) and chi-square tests were conducted to examine differences across degree categories. To examine the influence of the PharmD degree on time in dispensing and patient-care activities, only data for respondents who reported practicing as a pharmacist in a community, hospital, or other patient-care practice setting were retained for analysis. Multivariate regression analyses were used to examine the influence of the PharmD degree on time in dispensing and patient-care activities controlling for setting, position, years in practice and urban/rural location. A similar multivariate regression analysis was conducted for PharmD graduates to include the influence of completing a residency on time spent in dispensing and patient-care activities. Setting, position, degree, urban/rural location, and residency were entered as dummy variables in the regression analyses.
RESULTS
The overall response rate for the 2009 National Pharmacist Workforce Survey was 52.2% (1,391 out of 2,667 survey packets sent). Applying our cohort inclusion criteria resulted in a total of 562 usable responses for analysis. Of these 562 pharmacists, 336 (59.8%) had a BS in pharmacy degree only, 167 (29.7%) had a PharmD degree only, and 59 (10.5%) had both BS and PharmD degrees. Although one of our inclusion criteria for analysis was year of first licensure in 1984 or later, the data did not include any responses from pharmacists graduating after 2006 (an artifact from the sample frame and mailing list obtained for the survey instrument).
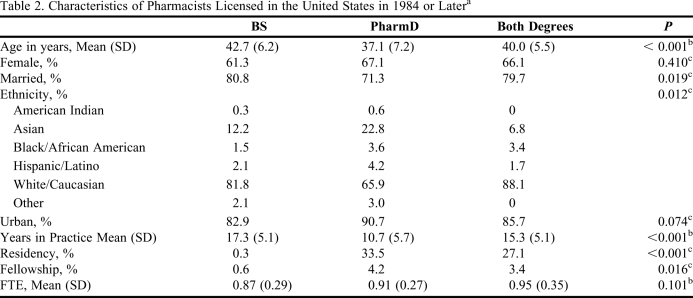
The characteristics of the respondent pharmacists are shown in Table 2. As expected, given the timing of the change to require the PharmD degree for entering practice, the average age and years of experience were lower for PharmD graduates, plus the proportion of PharmD degreed pharmacists who were married was lower than for BS degreed pharmacists. Completing a residency or fellowship was almost the exclusive domain of PharmD graduates; only 1 graduate with a BS in pharmacy reported completing a residency, and only 2 BS degreed pharmacists completed a fellowship. Ethnicity was significantly related to degree; more pharmacists with PharmD degrees were Asian or non-white, and nearly 90% of the pharmacists with both BS and PharmD degrees were white/Caucasian. There were no significant differences in contribution to the workforce in terms of full-time equivalents (FTEs) among the pharmacists with different degrees.
Table 2.
Characteristics of Pharmacists Licensed in the United States in 1984 or Latera
Abbreviations: FTE = full time equivalent; BS = bachelor of science in pharmacy; PharmD = doctor of pharmacy.
Only practicing pharmacists or pharmacists employed in a pharmacy-related field/position were included. Due to missing data, numbers of respondents ranged from 309-336 for BS in pharmacy, 159-167 for PharmD, and 56-59 for both BS and PharmD.
b via ANOVA.
c Chi-square test conducted.
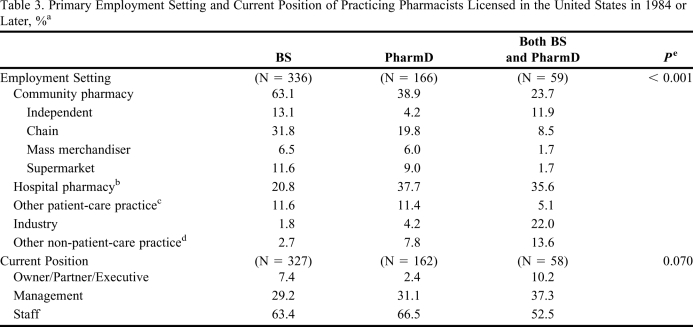
Practice setting and current positions of the respondent pharmacists are summarized in Table 3. Although approximately 80% of both BS and first professional degree PharmD pharmacists were employed in traditional community or hospital practice settings, pharmacists with a BS degree were more likely to be employed in a community pharmacy, while those with a PharmD degree were split evenly between community and hospital pharmacy settings. The proportion of pharmacists with both BS and PharmD degrees practicing in hospital pharmacies was similar to that of PharmD degreed pharmacists, but fewer post-BS PharmD graduates were employed in community pharmacies, and more worked for a pharmaceutical manufacturer or in a position where they were not providing patient care (such as pharmacy benefit administration, academic institution, or government agencies). The distribution of pharmacist respondents by position was not significantly different across the 3 degree groups; similar proportions of pharmacists with the differing degrees assumed management responsibilities.
Table 3.
Primary Employment Setting and Current Position of Practicing Pharmacists Licensed in the United States in 1984 or Later, %a
Only practicing pharmacists or pharmacists employed in a pharmacy-related field/position were included. Percentages of pharmacists with degree is shown.
b Includes both government and non-government hospitals/health systems.
c Includes clinic-based pharmacy, mail service pharmacy, nursing home/long-term care, home health/infusion, health maintenance organization (HMO) outpatient pharmacy, and nuclear pharmacy.
d Includes pharmacy benefit administration, academic institution, and government agencies.
e Chi-square test conducted for different distributions of responses across degree categories in settings and positions.
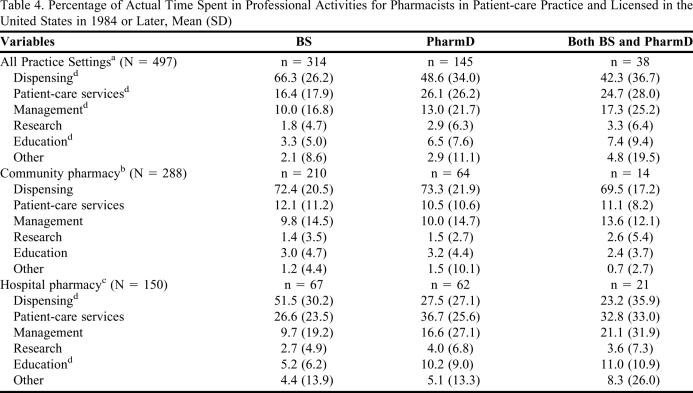
Table 4 illustrates how pharmacists practicing in patient-care settings spent their time on professional activities in a typical week. Overall, the highest proportions of pharmacists' time were spent on dispensing, regardless of degree. Across degrees, pharmacists with a BS in pharmacy reported spending a greater percentage of time on dispensing activities, and pharmacists with a PharmD degree reported spending more time on patient-care services. Pharmacists with both BS and PharmD degrees spent more time on other activities, such as management, research, and education.
Table 4.
Percentage of Actual Time Spent in Professional Activities for Pharmacists in Patient-care Practice and Licensed in the United States in 1984 or Later, Mean (SD)
Note: Total numbers varied due to missing data.
a Includes community pharmacy, hospital pharmacy, other patient-care practice (clinic-based pharmacy, mail service pharmacy, nursing home/long-term care, home health/infusion, health maintenance organization (HMO) outpatient pharmacy, and nuclear pharmacy).
b Includes independent, chain, mass merchandiser, and supermarket pharmacy.
c Includes both government and non-government hospitals/health systems.
d p < 0.05 via 1-way ANOVA
Medication Dispensing: preparing, distributing, and administering medication products, including associated consultation; interacting with patients about selection and use of over-the-counter products; and interactions with other professionals during the medication dispensing process.
Patient-care services: assessing and evaluating patient medication-related needs, monitoring and adjusting patients' treatments to attain desired outcomes, and other services designed for patient-care management.
Business/Organization Management: managing personnel, finances, and systems.
Research: discovering, developing, or evaluating products, services, and/or ideas.
Education: teaching, precepting, and mentoring students/trainees.
Other: any activities not described in the other categories.
Because there were different proportions of respondents with PharmD and BS in pharmacy degrees in community and hospital practice settings, respondents in those practice settings were analyzed separately to examine differences in time spent in activities by pharmacists with different degrees within settings. Table 4 includes a breakdown of time spent in activities by pharmacists practicing in community and hospital pharmacies with different degrees. For pharmacists practicing in community pharmacies, none of the actual time spent in specific activities differed among pharmacists with different degrees; the percentages of time in activities were similar regardless of pharmacy degree type. For hospital pharmacists, those with BS in pharmacy degrees reported nearly twice as much time in dispensing activities than pharmacists with first professional PharmD degrees. Hospital pharmacists with BS degrees also spent less time in education activities than pharmacists with PharmD degrees (both first professional PharmD and post-BS PharmD). The percentages of time in all other activities (patient care, management, research, and other) for hospital pharmacists were lower for BS in pharmacy pharmacists, but not significantly lower.
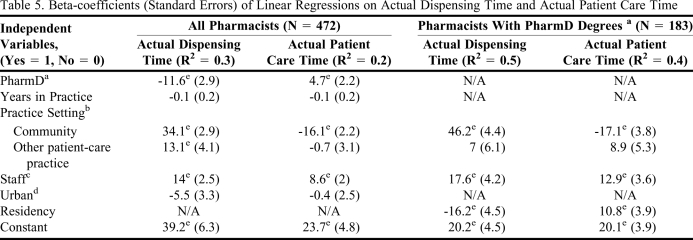
Table 5 shows the results from the regression analyses examining the association of the PharmD degree, with time in dispensing and patient-care activities controlling for setting, position, years in practice and urban/rural location. For time spent in dispensing activities, practicing in a community setting (relative to a hospital setting), and having a staff position (versus management) were associated with an increased amount of time spent; and holding a PharmD degree was associated with a decreased amount of time spent. For time spent in patient-care activities, working in a community pharmacy was associated negatively with the amount of time spent, and having a PharmD and a staff position was associated positively with the percentage of time spent. Controlling for other variables, practicing in a community setting was the most important variable positively associated with time spent in dispensing, and negatively associated with time spent in patient-care activities.
Table 5.
Beta-coefficients (Standard Errors) of Linear Regressions on Actual Dispensing Time and Actual Patient Care Time
Note: Total numbers reduced due to missing data.
a Including all pharmacists with PharmD degrees, both entry level PharmD and post-BS PharmD graduates.
b Compared with hospital setting (government and non-government hospitals/health systems). Community settings include independent, chain, mass merchandiser, and supermarket pharmacy; other settings include other patient-care practice (clinic-based pharmacy, mail service pharmacy, nursing home/long-term care, home health/infusion, health maintenance organization (HMO) outpatient pharmacy, and nuclear pharmacy).
c Compared with owner and managers.
d Compared with rural pharmacies.
e p < 0.05.
To examine the impact of completing a residency on time spent in different activities, a similar regression analysis was conducted, but only pharmacists with PharmD degrees were included, because essentially no BS in pharmacy degree pharmacists had completed a residency. In addition, years in practice and rural/urban location variables were omitted from the analysis because they were not significant in the regression including all pharmacists. For pharmacists with a PharmD degree, practicing in a community or other patient-care setting, having a staff position, and completing a residency were significant variables associated with time spent in dispensing and patient-care activities (Table 5). As with the all pharmacist regression, practicing in a community pharmacy (relative to in a hospital pharmacy) had the largest positive association with the percentage of time spent in dispensing activities, and was negatively associated with time spent in patient-care activities. Completing a residency was associated with spending less time in dispensing activities and more time in patient-care activities.
DISCUSSION
The revised accreditation standards requiring the PharmD as the first professional degree for pharmacists was a major change for pharmacy education, but few reports show whether or how the change translated into pharmacists' practice activities. Our results from a national survey revealed that pharmacists with BS in pharmacy degrees were more likely to be employed in a community pharmacy, whereas pharmacists with PharmD degrees were split more evenly between community and hospital pharmacies. This finding is consistent with results from studies during the period of debate, prior to requiring the PharmD as the first professional pharmacy degree.6-8
Several factors may have contributed to this different distribution of pharmacists into practice sites by degree, particularly a higher proportion of PharmDs in hospital settings. Hospitals have had different operational parameters that would result in a qualitatively different workforce in their environments. Pricing structures and reimbursement mechanisms have afforded or effectively included incentives for innovative service development, role expansion, and contributions by pharmacists to the overall organizational goals. Department staff sizes that typically have had more pharmacists have allowed division of labor and specialization warranting pharmacists with different backgrounds, skills, and abilities. With the range of health professionals employed and a more “closed system” environment of potential clients or customers for services, hospitals have been more successful in generating awareness, need, and appreciation for pharmacists' services within their organizations. These factors have positioned hospital pharmacies to desire and utilize the skills available from the increased clinical training provided by a PharmD education, and they have recruited successfully for more specialized staff.
Regarding the amount of time pharmacists spend in practice activities, no degree-related differences for pharmacists in community settings were found. Both BS in pharmacy and PharmD degreed pharmacists spent approximately 70% of their practice time in dispensing activities, and the remaining 30% of their time was not partitioned differently for pharmacists with different degrees. Clearly, in community pharmacy settings, dispensing-related activities remained an emphasis and priority. Comparing results for time allocation with previous research was difficult because the definition of dispensing activities was not consistent, and because researchers often did not group pharmacists by both degree and setting. Cox and Carroll did split their respondents by setting and degree, and reported a lower percentage of time in drug distribution for community pharmacists (approximately 49% for BS and 62% for PharmD degreed pharmacists), but also less time in direct patient care (5% for BS and 15% for PharmD pharmacists); however definitional differences and/or respondent interpretations likely contributed to the differences between their study and ours (their activity categories of drug distribution, direct patient care, and drug information may have had aspects of dispensing interpreted by their respondents).7
In hospital settings, pharmacists with BS in pharmacy degrees reported spending significantly more time on dispensing and less time on education activities, compared to PharmD-trained pharmacists. Although not significant, pharmacists with BS degrees also spent less time in patient-care services and management activities than pharmacists with PharmD entry-level or post-BS degrees. This confirms the notion that hospitals may have deployed PharmD degree pharmacists in different activities to take advantage of their advanced preparation and/or specialization.
The regression analyses revealed that degree, setting, and staff position were associated with the time that pharmacists spend in dispensing activities and patient-care activities. Practicing in a community pharmacy had the biggest impact on time spent in these activities, positive for dispensing and negative for patient-care services. Having a PharmD degree had the opposite effect: a positive impact on time spent in patient-care services and a negative impact on time spent in dispensing activities. The regression analysis explained less than half of the variance in time spent in dispensing or patient-care activities, suggesting that other variables also contribute to the variation in the times spent in practice activities. However, degree and setting were important variables related to time spent on practice activities.
Assuming that current market trends continue, such as the increasing age of the population and need/reliance on medications in health care, there will be a sizeable need for pharmacists practicing in community pharmacy settings. However, it is unclear how much growth will occur in the need for pharmacists to provide patient care, especially in a community setting. Although a number of factors will affect the extent to which pharmacies make patient-care services available, some roles that academics might play will help advance the profession in the community sector. First, through research and evaluations of advanced practice initiatives and interventions, researchers can help provide evidence of the value of advanced practice activities. Second, pharmacy educators should attend to the need for pharmacists' educations to provide background, skills, and competencies to develop and implement new and sustainable pharmacy services. Third, academics can help stimulate thought and creativity about innovative practice, pricing, and opportunities in their classroom, and scholarly connections with students and pharmacists.
About a third of pharmacists with PharmD degrees in our study sample pursued a residency. For PharmD-trained pharmacists, completing a residency was associated with spending less time in dispensing activities and more time in patient-care services. This suggests PharmD pharmacists who pursue advanced training with a residency are migrating to opportunities that allow them to spend more time in patient care, and/or employers are seeking these pharmacists with advanced preparation for non-dispensing patient-care activities. The dearth of pharmacists who completed residencies in community pharmacy settings could imply that there are limited needs for residency-trained pharmacists in that environment. Alternatively, needs may be present, but the development and introduction of services to meet those needs is an opportunity for pharmacists to capitalize on, and perhaps a component of, PharmD preparation that needs bolstering in our educational enterprises. If all pharmacists in direct patient care should complete a residency, there will need to be more positions and opportunities for these advance-trained pharmacists.
Some limitations of this study should be noted. First, there were differences in age, percentage married, race/ethnicity, and years in practice between the different pharmacy degree groups. Also, the percentage of PharmD respondents who had completed a residency was higher than the percentage of recent graduates pursuing residencies, which could have biased the amount of time respondents reported spending in patient care and dispensing activities.17 Due to the timing of the change in accreditation requirement, the age difference and years in practice are unavoidable. Similarly, the percentage married likely is related to the age difference between the degree groups. Although there were significant differences in the race/ethnicity of BS in pharmacy degreed respondents vs. PharmD degreed respondents, the race/ethnic distribution among PharmD respondents was similar to that which has been reported for PharmD graduates in the last 10 years.17 We are not aware of different preferences in practice settings or work activities due to race/ethnicity, and we believe that the effect of ethnicity difference on our results would be limited. Second, due to the cross-sectional nature of this study, causal relationships cannot be implied. Third, we relied on self-report of time spent in activities; how pharmacists interpreted categories of activities may have varied across pharmacists and settings. Although we achieved over a 50% response rate, caution is needed when generalizing the results. This is relevant particularly regarding recent graduates; the mailing list for our sample did not include pharmacists who graduated in 2007 or later.
CONCLUSION
In our cohort of pharmacists who graduated in 1984 or later, proportionately more pharmacists with BS in pharmacy degrees practiced in community settings and fewer in hospital settings, relative to pharmacists with PharmD degrees. Regardless of degree, pharmacists in community pharmacy practice spent most of their time in dispensing-related activities, whereas in hospital settings, pharmacists with a PharmD degree spent less time in dispensing activities and more time in patient-care activities. Controlling for other variables, practice setting most influenced time spent in dispensing activities and patient-care services, followed by whether the pharmacist had a PharmD degree. As more graduates enter practice with the PharmD as their first professional degree, determining how their advanced preparation can be translated into patient-care services beyond dispensing, particularly in community pharmacy, presents both challenges and opportunities for academicians.
ACKNOWLEDGMENTS
Support for this research came from the Pharmacy Manpower Project. Dr. Chang is supported by a fellowship from the American Foundation for Pharmaceutical Education.
REFERENCES
- 1. Findings and Recommendations of the Pharmaceutical Survey, 1948. American Council on Education: Washington, DC; 1948.
- 2.Manasse HR, Jr, Giblin PW. Commitments for the future of pharmacy: a review and opinion of the PharmD curricular debate. Drug Intell Clin Pharm. 1984;18(5):420–427. doi: 10.1177/106002808401800521. [DOI] [PubMed] [Google Scholar]
- 3.McLeod DC. All-PharmD degree alone will not significantly alter the pharmacy profession. Ann Pharmacother. 1992;26(7-8):998–1000. doi: 10.1177/106002809202600728. [DOI] [PubMed] [Google Scholar]
- 4.Ukens C. The PharmD system – a reality check. Drug Topics. 2006;150(16):28–32. [Google Scholar]
- 5.American College of Clinical Pharmacy. American College of Clinical Pharmacy's Vision of the Future: Postgraduate Pharmacy Residency Training as a Prerequisite for Direct Patient Care Practice. Pharmacotherapy. 2006;26(5):722–733. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]
- 6.Ried LD, McGhan WF. PharmD or BS: does the degree really make a difference in pharmacists' job satisfaction? Am J Pharm Educ. 1986;50(1):1–5. [PubMed] [Google Scholar]
- 7.Cox FM, Carroll NV. Comparison of practice patterns and job satisfaction of entry level PharmD and BS level graduates in hospital and community practice. Am J Pharm Educ. 1988;52(1):47–50. [PubMed] [Google Scholar]
- 8.Barnett CW, Matthews HW. Practice patterns of BS, postbaccalaureate PharmD and entry-level PharmD graduates of one school of pharmacy. Am J Pharm Educ. 1992;56(4):367–373. [Google Scholar]
- 9.Fjortoft NF, Lee MW. Comparison of activities and attitudes of baccalaureate level and entry-level doctor of pharmacy graduates of the University of Illinois at Chicago. Ann Pharmacother. 1995;29(10):977–982. doi: 10.1177/106002809502901003. [DOI] [PubMed] [Google Scholar]
- 10.Fjortoft NF, Engle JP. Effect of the nontraditional PharmD on individual practice patterns. Am J Pharm Educ. 1995;59(3):223–227. [Google Scholar]
- 11.Fjortoft NF, Weigand L, Lee M. Effect of the nontraditional PharmD degree on practice patterns based on a survey of graduates from six programs. Am J Pharm Educ. 1999;63(4):305–309. [Google Scholar]
- 12.Joyner PU, Thomason TE, Smith SR. Changes in career and practice of pharmacy after obtaining a degree through an external doctor of pharmacy program. Am J Pharm Educ. 2002;66(1):42–46. [Google Scholar]
- 13.Joyner PU, Thomason TE, Blalock SJ. Practice settings, job responsibilities, and job satisfaction of nontraditional PharmD and BS pharmacy graduates. Am J Pharm Educ. 2009;73(2) doi: 10.5688/aj730233. Article 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. New York, NY: John Wiley & Sons; 2000. [Google Scholar]
- 15.Mott DA, Doucette WR, Gaither CA, Pedersen CA, Schommer JC. Alexandria, VA: Pharmacy Manpower Project, Inc; 2000. National Pharmacist Workforce Survey: 2000. [Google Scholar]
- 16.Mott DA, Doucette WR, Gaither CA, Kreling DH, Pedersen CA, Schommer JC. Alexandria, VA: Pharmacy Manpower Project, Inc; 2005. Final Report of the National Sample Survey of the Pharmacist Workforce to Determine Contemporary Demographic and Practice Characteristics. [Google Scholar]
- 17. American Association of Colleges of Pharmacy. Graduating Pharmacy Student Survey Summary Report – 2009. http://www.aacp.org/resources/research/institutionalresearch/Documents/2009_GSS_Summary%20Report_all%20schools_83.pdf. Accessed September 22, 2010.