Abstract
The role of the psychiatric pharmacist in the care of the mentally ill has continually evolved since the late 1960s and early 1970s. Pharmacists in the field of psychiatric pharmacy work to improve the health, safety, and welfare of those impacted by one or more psychiatric conditions. Specialty residency training programs are accredited to establish minimum training standards and a board-certification process ensures that individuals provide a high level of quality of care. It is the position of the College of Psychiatric and Neurologic Pharmacists (CPNP) that Psychiatric Pharmacy residency programs obtain American Society of Health-System Pharmacy (ASHP) accreditation and help the profession move forward as a recognized specialty.
Keywords: psychiatric pharmacy, residency, postgraduate education, American Society of Health-System Pharmacists (ASHP)
INTRODUCTION
Approximately 58 million Americans are affected by a psychiatric disorder, making mental illness a leading cause of disability and associated healthcare costs in the United States.1 Approximately 36 prescriptions for psychotropic medications are written per 100 outpatient office visits within the general US population. While annual retail drug costs for mental health medications in the United States exceed $20 billion, the total economic burden of mental illness, including direct and indirect costs, is approximately $317 billion annually.2,3 The need for specialized clinical pharmacists in areas such as psychiatry has been recognized by pharmacy practice and professional education organizations. Despite slow gains in acceptance by the public, government, and insurance entities, the clinical pharmacist is recognized as having an increasing role as a primary healthcare provider.
Individual pharmacy practitioners who provide care to those with mental health disorders are identified by different designations and descriptors including mental health pharmacist, psychiatric pharmacist, and psychopharmacologist. Psychiatric pharmacy is a recognized specialty with clinicians practicing in a multitude of diverse settings. However, the psychiatric pharmacy profession is relatively young and has undergone many changes in the last 40 years. The purpose of this paper is to express the College of Psychiatric and Neurologic Pharmacists (CPNP) support for the American Society of Health-System Pharmacists (ASHP) accreditation process of second postgraduate year (PGY2) psychiatric pharmacy residency programs.
HISTORY OF PSYCHIATRIC PHARMACY AND RESIDENCY PROGRAMS
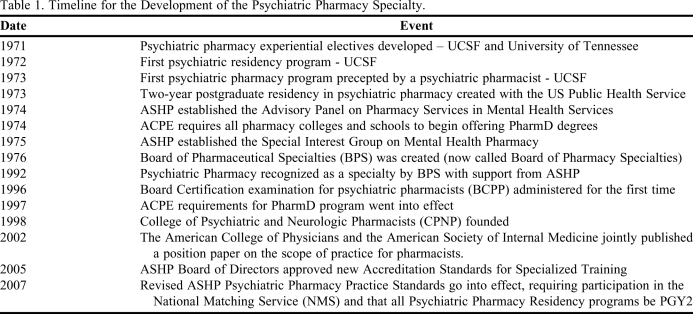
The roots of psychiatric clinical pharmacy date back to the 1960s and early 1970s (Table 1). In 1971, the US Public Health Service assigned a pharmacist to a psychiatric unit in Alaska, which was later the setting for the first published case describing the activities of a psychiatric pharmacist.4 The psychiatric pharmacist worked with psychiatrists to complete medication histories, educate the treatment team, assist in the selection of optimal medications, and monitor/manage the bothersome side effects of psychotropics commonly used at the time, such as chlorpromazine and lithium. Clinical pharmacists were working not only in psychiatric inpatient and outpatient settings, but also in methadone and disulfiram clinics and mental retardation centers.4,5 During this time, business models describing these practice paradigms were developed. The University of Tennessee created contracts to provide pharmacy dispensing and clinical services for several local psychiatric facilities.5 This treatment paradigm mirrored some of the collaborative drug therapy management and medication therapy management (MTM) systems commonly employed today. Those referred to pharmacists were mental health patients who had previously been diagnosed and stabilized by psychiatrists. They pharmacists provided medication management, including the completion of prescriptions, which were pre-signed by psychiatrists.
Table 1.
Timeline for the Development of the Psychiatric Pharmacy Specialty.
With the new role came the need for additional education. The US Public Health Service created a 2-year psychiatric pharmacy training program in 1973.4 This early training experience was designed to provide a year of didactic training with a college of pharmacy and a year of practice in a psychiatric environment. The first year of the program concentrated on pharmacological literature, research, and didactic coursework in psychiatric pharmacy, as well as training in administering injectable medications and obtaining blood work for laboratory testing. The second year was spent at a psychiatric hospital and included more in-depth study of psychiatric illness and treatment options. The trainee was taught to work with the patients and treatment teams as part of a multidisciplinary approach to health care. The program was set up to mirror the training that first-year psychiatry residents received and led to the addition of one of the first pharmacists to a school of medicine teaching faculty.
The need for additional coursework in the curricula of US schools and colleges of pharmacy became apparent as more pharmacists began working in mental health settings. In the late 1960s, some pharmacy schools began sponsoring continuing education programs in mental health topics.5 However, most colleges and schools of pharmacy did not include psychiatry in their curricula. In 1971, psychiatric clerkship experiences began to be developed and implemented into their respective pharmacy school curriculums as electives. One of the earliest described clerkship experiences was at the University of California San Francisco (UCSF) School of Pharmacy where students were offered a 12-week clerkship that included both didactic training and several weeks of clinical experience.6 The training directly led to students accepting mental health positions in clinical or academic settings and to the development of psychiatric pharmacy residency programs, the first being at UCSF in 1972. The first psychiatric pharmacy residency precepted by a psychiatric pharmacist also occurred at UCSF in 1973.7 On July 1, 1974, the American Council on Pharmaceutical Education (ACPE) dictated that all pharmacy schools would offer a clinical pharmacy curriculum. By the 1980s, a handful of colleges and schools of pharmacy and affiliated psychiatric pharmacy residency programs were regularly training residents (eg, University of Texas, University of Tennessee, University of Southern California, University of Missouri-Kansas City, University of Nebraska) and pharmacy students about the management of psychiatric disorders.
The pharmacy profession continued to evolve, with the American Pharmaceutical Association's (currently known as the American Pharmacists Association) creation of the Board of Pharmacy Specialties (BPS) in 1976.8 In 1983 a certificate program in psychiatric pharmacy practice was described, further helping to identify this specialty area of practice.9 Psychiatric pharmacy was recognized by BPS as a specialty in 1992.10 Four years later, several psychiatric pharmacists formed a group that would later become the CPNP. CPNP then negotiated with the Board of Pharmacy Specialties (BPS) and ASHP for recognition and an approved certification procedure. The first board certification examination for psychiatric pharmacists was administered in 1996. In order to earn board certification, the examinees were required to have graduated from an ACPE-accredited pharmacy school, have an active pharmacy license, complete a specialty residency and/or equivalent work experience, and achieve a passing test score. Of the first 191 examinees, 159 practitioners became board certified upon initial testing.10
By the late 1990s, many pharmacy colleges and schools were phasing out the bachelor of science in pharmacy program. ACPE required that colleges and schools develop a doctor of pharmacy (PharmD) program by 1997 to meet the growing clinical demands of the profession. Subsequently, the number of psychiatric pharmacy residency programs also continued to grow. The standard process was for these residency programs to be accredited and recognized as 1-year programs in psychiatric pharmacy practice, which could be started directly after completing the Pharm.D. degree. While most programs were residencies seeking ASHP accreditation, there were a number of 1- and 2-year unaccredited programs that allowed training of practicing psychiatric pharmacists to complete a fellowship or master's degree.
Throughout the evolution of the board-certification process, psychiatric pharmacists became more organized as a specialty and met on a regular basis at national meetings such the New Clinical Drug Evaluation Update (NCDEU) and through specialty-practice group meetings at ASHP annual midyear meetings. On March 24, 1998, CPNP was established as a professional society and held their first annual meeting in Orlando, Florida, that same year. CPNP worked to develop educational programming, improve patient care, foster research, and support board certification for psychiatric pharmacists. At their annual meetings, the organization offered high-level programming in psychiatric pharmacy and neurology and encouraged networking and the formation of strong professional relationships.
Also by the late 1990s, the contributions that psychiatric pharmacists were making to patient care began to be more recognized.11-13 Psychiatric pharmacists were being employed in federal (veteran's hospitals and department of defense hospitals) and state mental health care facilities, as well as in research, the pharmaceutical industry, managed care, ambulatory care, and hospitals. In 2002, the American College of Physicians and the American Society of Internal Medicine jointly published a position on the scope of practice for pharmacists.8 The paper supported an expanded role, including pharmacist-physician collaborative agreements. In a memorandum written by Deputy Under Secretary of Health William F. Feeley, the Veterans Health Administration (VHA) recommended that clinical pharmacists be included on care teams in mental health services.14
With the changes in practice and pharmacy education, along with a growing number of board-certified psychiatric practitioners, pharmacy residency training programs also began to transform and subsequently moved to a 2-year medical model of residency training. In 2002, fearing that proposed “changes are quite likely to decrease the number of practice environments offering psychiatric experiences, and to decrease flexibility in program design,” CPNP opposed a proposal by ASHP to adopt language “requiring that applicants to specialized residencies must have completed an ASHP accredited pharmacy practice residency or have an equivalent level of 3 years of prior experience in pharmacy practice.” CPNP also opposed the ASHP proposal requiring that all residency applicants participate in the matching program.
CHANGES IN ACCREDITATION STANDARDS
In 2005, the ASHP Board of Directors approved new Accreditation Standards for Specialized Training, which went into effect on January 1, 2007.15 The major change in the new standards, which impacted Psychiatric Pharmacy and other PGY2 programs, was found under Principle 1.1, indicating “the applicant must have completed an accredited PGY1 pharmacy residency program.” In addition, psychiatric pharmacy residencies were required to participate in the National Match System (NMS) and become recognized as second-year postgraduate (PGY-2) programs.
In 2009, there were 548 board-certified psychiatric pharmacists, 30 residency programs, and 955 members of CPNP practicing with varied responsibilities and in a wide range of practice settings.16,17 In 2010, the number of candidates seeking postdoctoral training increased for both PGY1 residencies (16% increase) and PGY2 specialty residencies (25% increase) over 2009 numbers.18 Additionally, there was a 9% increase in the number of PGY1 candidates matching and a 24% increase in the number of PGY2 candidates matching.18 The number of psychiatric specialty training programs as of June 2010 was 29, with 20 of those being ASHP accredited with 22 possible accredited PGY2 positions due to some programs having multiple positions.18 Of the 22 accredited positions, 5 were filled early and 16 were included in the ASHP resident matching program through which 13 were filled in the initial matching process.18
The role of psychiatric pharmacists continues to expand in clinical practice, administration, research, and the pharmaceutical industry/business. Training and certification also will continue to evolve. In 2013, all candidates for BCPP will be required to have completed an accredited specialty residency in psychiatric pharmacy and have 1 year of work experience with at least 50% of time spent in psychiatric pharmacy activities.19 For those who do not meet this requirement, 4 or more years of relevant work experience will be expected.
Psychiatric pharmacy and therapeutics has not been a major focus in pharmacy education in US colleges and schools of pharmacy. In 2007, Cates et al noted that, while 75% of pharmacy colleges/schools employed a psychiatric pharmacist, less than 50% of pharmacy faculty members teaching didactic courses in psychiatry were psychiatric pharmacy specialists, and only 9.5% of coursework was devoted to pyschiatric topics.20
In discussing the need for change in the standard pharmacy curriculum, the American Association of Colleges of Pharmacy (AACP) stated that specialization will become the norm. Additionally, they emphasized that pharmacy educators should offer a curriculum that prepares student pharmacists to provide patient-centered, interprofessional care that incorporates self-directed learning skills.21 A further recommendation of the 2002 AACP Task Force on the Role of Colleges and Schools in Residency Training is that full-time pharmacy practice faculty members have a PharmD degree plus a minimum of 1 year of graduate pharmacy training (PGY1/PGY2 residencies) or equivalent experience.22
The American College of Clinical Pharmacy (ACCP) goes a step beyond the AACP in recommending that completion of a PGY1 residency should be a minimum requirement for academic appointment as an adjunct clinical faculty member or preceptor and “residency training will become mandatory before one can enter clinical practice.”23 ACCP also has noted that professional organizations both within pharmacy and in other health care professions recognize that the first professional pharmacy degree from an ACPE-accredited school of pharmacy and licensure as a pharmacist are not sufficient to prepare the clinical pharmacist for advanced pharmacy practice.24 The Board of Pharmacy Specialties requires that clinical pharmacists who sit for board certification examinations have graduated from an ACPE-accredited pharmacy program, hold a current US pharmacy license, and have completed either (1) 4 years of pharmacy practice with at least 50% of time spent in psychiatric pharmacy activities or (2) a PGY2 residency program in psychiatric pharmacy and have an additional year of practice where at least 50% time is spent in psychiatric pharmacy activities. In order for the pharmacy profession to advance its ability to positively impact both patient outcomes and economic burden, it must embrace both the need for accredited PGY1 and PGY2 residency training programs and board certification in pharmacotherapy and/or a specialty pharmacy area.
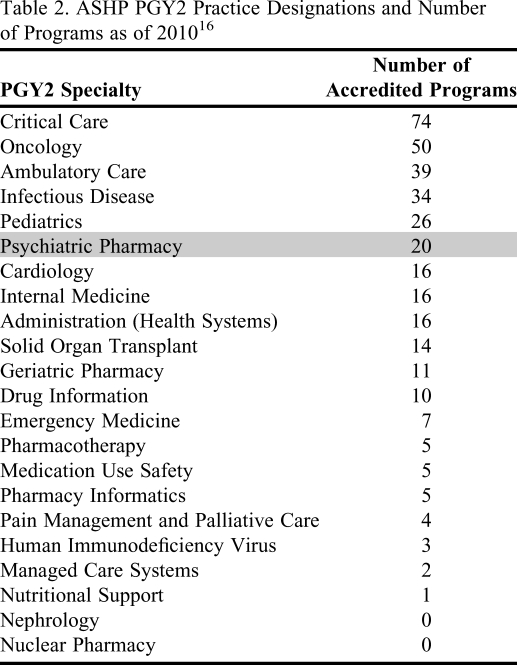
Under ASHP-based residency standards, 22 specialty program designations exist with ASHP PGY2 specialty practice classification, including psychiatric pharmacy. Within the accredited pharmacy residencies in psychiatry, there are 20 programs that currently hold ASHP residency accreditation status (Table 2), placing psychiatric pharmacy high on the list of accredited specialty PGY2 programs.
Table 2.
ASHP PGY2 Practice Designations and Number of Programs as of 201016
Before 2007, more psychiatric pharmacy residency programs were successful in filling their open specialty positions. Since implementation of the new standards and requirement of PGY1 residency, there was a reduction in the number of applicants for PGY2 residencies in psychiatry pharmacy. Approximately 25%-30% of the available accredited PGY2 psychiatric pharmacy positions were being filled with qualified candidates through the matching process, leaving many programs without residents. These unfilled positions raised concern that some programs might lose their funding for failure to fill the position or even lose accreditation for failure to fill their position in 3 consecutive recruitment cycles. While there are efforts by CPNP and other organizations (eg, Veterans Affairs medical centers) to attract more mid-career level pharmacists into psychiatric pharmacy, failure to have residents enrolled in specialty training will put the specialty at risk for survival. The 2010 residency recruitment cycle showed a positive reversal in the declining number of psychiatric pharmacy residents, with a dramatic shift in the percentage of accredited psychiatric pharmacy programs matching and filling their open positions (18 of 22 positions or 81.8% filling through the match process).18
Many in psychiatric pharmacy practice had identified the change in the ASHP Accreditation standards as the cause in the significant reduction in the number of eligible residency candidates. Some residency programs have made the decision to not pursue ASHP accreditation and to function independently from the accreditation standards, possibly resulting in inconsistency in the training of residents going into psychiatric pharmacy. The standards that have been developed as part of the ASHP Accreditation process may never be fully agreed upon by all residency programs; however, they establish minimum criteria that programs should strive to achieve. The standards themselves do not guarantee a program will be successful, but if a program is held accountable to these minimum standards, there is a greater likelihood that the resident will have experiences that will better prepare them to advance the practice of psychiatric pharmacy. Accreditation offers a system of checks and balances to ensure that programs have a clear set of goals and objectives that are consistent across the specialty and ensure the growth of the specialty practice of psychiatric pharmacy.
Regardless of the impact of the ASHP accreditation process on the numbers of slots and applicants in residency programs, it is the position of the College of Psychiatric and Neurologic Pharmacists that psychiatric pharmacy residency programs work to obtain ASHP accreditation and to help the profession move forward as a true “specialty.”
CPNP POSITION ON RESIDENCY TRAINING AND ACCREDITATION
Action Steps
(1) Encourage the development of additional PGY1 training programs to increase the opportunities available to pharmacy graduates, which will in turn serve to increase the applicant pool for PGY2 specialty training programs.
- (2)Enhance the recognition of psychiatric pharmacy as a true specialty within pharmacy practice.
- (a) Establish the value of board certification in psychiatric pharmacy (BCPP).
- (i) Encourage organizations to incentivize board certification
- (b) Promote BCPP recertification through the implementation of rigorous recertification activities.
- (c) Promote the establishment of a central psychiatric pharmacy resource or information- sharing mechanism that promotes the role of psychiatric pharmacists (ie, journal to promote practice and research).
- (d) Promote the profession to help fulfill the projected pharmacist shortfall by 2020 for the provision of primary, secondary, and tertiary care services. Failure to increase the role of pharmacists in this manner will result in a surplus of pharmacists to fulfill the dispensing function, given that there are currently 120 schools and colleges with ACPE accreditation status and many schools have increased their enrollments to help meet the projected shortage and to also generate revenue. These graduates should be educated to meet the projected demand for patient care services providing service to the patient and sustaining the value of the profession.
- (e) Encourage BCPP-certified pharmacists to take on increasingly active roles within their practice sites and to promote the image of being a psychiatric pharmacy specialist. Board certification of pharmacists is one means to legitimize value. However, board-certified psychiatric pharmacists need to take advantage of the recognition this designation provides and pursue leadership positions and increased activities to promote acceptance from other direct patient care providers.
- (3) Promote early integration of psychiatric pharmacy into US colleges and schools of pharmacy to increase student awareness of psychiatric pharmacy as a specialty and to generate interest.
- (a) Establish a marketing campaign that includes a recruitment video that can be shared on various technology outlets and promoted at colleges and schools of pharmacy and hospitals to students and midcareer professionals. Earlier integration of psychiatry pharmacy into the minds of students will enhance their knowledge of the specialty at a time when they are considering career paths of interest.
- (4) Increase the recognition of the value-added benefits of a psychiatric clinical pharmacy specialist to patient-centered care outcomes, focusing not on direct cost-savings to institutions, but rather on improved psychiatric and physical health outcomes of the patient.
- (a) There are reports of economic benefits of psychiatric pharmacy specialists; however, the cost savings needs to go beyond typical measures, such as changing from a brand name to generic or the utilization of cheaper medication alternatives. While this is important in the overall costs to the healthcare system, psychiatric pharmacy specialists should promote comprehensive improvements in health-related outcomes and patient safety.
(5) Encourage all PGY2 psychiatric pharmacy residency programs to become accredited by the ASHP Commission on Credentialing.
ACKNOWLEDGMENT
The authors acknowledge the following for their contributions to the development of this paper: Sheila Botts, PharmD, BCPP, FCCP; Charles F. Caley, PharmD, BCPP; Julie A. Dopheide, PharmD, BCPP; Larry Ereshefsky, PharmD, BCPP, FCCP; Matthew A. Fuller, PharmD, BCPP, BCPS, FASHP; Cherry W. Jackson, PharmD, BCPP, FASHP; Roger W. Sommi, PharmD, BCPP, FCCP; Glen L. Stimmel, PharmD, BCPP; Stanley S. Weber, PharmD, BCPP, FASHP.
REFERENCES
- 1. U.S. Census Bureau Population Estimates by Demographic Characteristics. Table 2: Annual Estimates of the Population by Selected Age Groups and Sex for the United States: April 1, 2000 to July 1, 2004 (NC-EST2004–02) Source: Population Division, U.S. Census Bureau Release Date: June 9, 2005. http://www.census.gov/popest/national/asrh/ Accessed October 15, 2010.
- 2. Health, United States, 2008. Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/hus/mentalhealth.htm Accessed November 15, 2009.
- 3.Hogan MR. Assessing the economic costs of serious mental illness. Am J Psych. 2008;165(6):663–665. doi: 10.1176/appi.ajp.2008.08030366. [DOI] [PubMed] [Google Scholar]
- 4.Chadwick GI. Psychiatric pharmacy residency and services. Military Med. 1976;141(8):537–539. [PubMed] [Google Scholar]
- 5.Coleman JH, Evans RL, Rosenbluth SA. Extended clinical roles for the pharmacist in psychiatric care. Am J Hosp Pharm. 1973;30(12):1143–1146. [PubMed] [Google Scholar]
- 6.Stimmel GL, Katcher BS, Levin RH. The emerging role and training program of clinical pharmacy in psychiatry. Am J Pharm Educ. 1974;38:179–185. [Google Scholar]
- 7.Stimmel GL. Clinical pharmacy practice in a community mental health center. J Am Pharm Assoc. 1975;15:400–418. doi: 10.1016/s0003-0465(15)32088-7. [DOI] [PubMed] [Google Scholar]
- 8.Keely JL. Pharmacist scope of practice. Ann Intern Med. 2002;136(1):79–85. doi: 10.7326/0003-4819-136-1-200201010-00014. [DOI] [PubMed] [Google Scholar]
- 9.Wells BG, Rawls WN, Ryan MR, Rosenbluth SA. A certificate continuing education program in psychiatric pharmacy practice. Am J Pharm Educ. 1983;47(3):244–249. [Google Scholar]
- 10.Crismon ML, Fankhauser MP, Hinkle GH, et al. Psychiatric pharmacy practice specialty certification process. Am J Health-Syst Pharm. 1998;55(15):1594–1598. doi: 10.1093/ajhp/55.15.1594. [DOI] [PubMed] [Google Scholar]
- 11.Finley PR, Crismon ML, Rush AJ. Evaluating the impact of pharmacists in mental health: a systematic review. Pharmacotherapy. 2003;23(12):1634–1644. doi: 10.1592/phco.23.15.1634.31952. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins MH, Bond CA. The impact of clinical pharmacists on psychiatric patients. Pharmacotherapy. 1996;16(4):708–714. [PubMed] [Google Scholar]
- 13.Cohen LJ. The role of neuropsychiatric pharmacists. J Clin Psychiatr. 1999;60(19):54–57. [PubMed] [Google Scholar]
- 14. Feeley WH. VHA Mental Health Clinical Pharmacists [memorandum]. Veterans Health Administration, United States Department of Veterans Affairs, Washington, DC. November 14, 2008.
- 15. American Association of Health-System Pharmacists. Required Educational Outcomes, Goals, and Objectives for Postgraduate Year Two (PGYS) Pharmacy Residencies in Psychiatry. http://www.ashp.org/s_ashp/docs/files/accreditation/RTP_ObjPsychiatric032608.doc Accessed October 15, 2010.
- 16. Board of Pharmaceutical Specialties. Online 2008 annual report. http://www.bpsweb.org/pdfs/2008_Annual_Report.pdf Accessed October 15, 2010.
- 17. College of Psychiatric and Neurologic Pharmacists. Online residency directory. http://cpnp.org/career/residencies Accessed October 15, 2010.
- 18. National Matching Service. Online summary of programs and positions offered and filled by program type. Available from http://www.natmatch.com/ashprmp/index.htm Accessed October 15, 2010.
- 19. Board of Pharmaceutical Specialties. Online psychiatric pharmacy eligibility requirements. http://www.bpsweb.org/specialties/psychiatric.cfm Accessed August 16, 2010.
- 20.Cates ME, Monk-Tutor MR, Drummond SO. Mental health and psychiatric pharmacy instruction in US colleges and schools of pharmacy. Am J Pharm Educ. 2007;71(1) doi: 10.5688/aj710104. Article 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. American Association of Colleges of Pharmacy. Addressing competencies for the future in the professional curriculum. Available at: http://www.aacp.org/meetingsandevents/othermeetings/curricularchangesummit/Documents/Addressing%20Competencies%20for%20the%20Future%20in%20the%20Professional%20Curriculum.pdf Accessed October 15, 2010.
- 22. American Association of Colleges of Pharmacy Task Force on the Roles of Colleges and Schools in Residency Training. http://www.aacp.org/governance/councildeans/Documents/FinalTaskForceReportResidencies.pdf Accessed October 15, 2010.
- 23.Murphy JE, Nappi JM, Bosso JA, Saseen JJ, et al. ACCP Position Statement. American College of Clinical Pharmacy's vision of the future: postgraduate residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;36(5):722–733. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]
- 24.Blair MM, Freitag RT, Keller DL, Kiser TH, et al. ACCP White Paper: proposed revision to the existing specialty and specialist certification framework for pharmacy practitioners. Pharmacotherapy. 2009;29(4):3e–13e. doi: 10.1592/phco.29.4.489. [DOI] [PubMed] [Google Scholar]