Abstract
Lysophosphatidic acid (LPA) is the umbrella term for lipid signaling molecules that share structural homology and activate the family of LPA receptors. Farnesyl Pyrophosphate (FPP) is commonly known as an intermediate in the synthesis of steroid hormones; however, its function as a signaling lipid is beginning to be explored. FPP was recently shown to an activator of the G-protein coupled receptor 92 (also known as LPA5) of the calcium channel TRPV3. The LPA receptors (including GPR92) are associated with the signal transduction of noxious stimuli, however, very little is known about the distribution of their signaling ligands (LPAs and FPP) in the brain. Here, using HPLC/MS/MS, we developed extraction and analytical methods for measuring levels of FPP and 4 species of LPA (palmitoyl, stearoyl, oleoyl and arachidonoyl-sn-glycerol-3 phosphate) in rodent brain. Relative distributions of each of the five compounds was significantly different across the brain suggesting divergent functionality for each as signaling molecules based on where and how much of each is being produced. Brainstem, midbrain, and thalamus contained the highest levels measured for each compound, though none in the same ratios while relatively small amounts were produced in cortex and cerebellum. These data provide a framework for investigations into functional relationships of these lipid ligands in specific brain areas, many of which are associated with the perception of pain.
Keywords: LPA, FPP, GPR92, TRPV3, LC/MS/MS, pain
1. Introduction
Lysophosphatidic acid (LPA) is not a single molecule, but a collection of signaling molecules that share structural homology and activate the family of LPA receptors. LPAs are structurally composed of a fatty acid linked to sn-glycerol-3 phosphate (e.g., arachidonoyl-sn-glycerol-3 phosphate). They induce their effects through binding to members of the superfamily of G protein-coupled receptors (GPCRs) including LPA1 (also named VZG-1, MREC1.3 or EDG-2) [1,2], LPA2 (or EDG-4) [3], LPA3 (or EDG-7) [4,5], LPA4 (formerly GPR23) [6] and more recently discovered LPA5 (formerly GPR92) [7]. These receptors couple to at least three different types of G proteins, notably Gq/11, Gi/o and G12/13 [8]. LPA receptors coupled to Gi proteins drive the activation of the PI3K-Akt pathway [9], whereas, LPA receptors bound to G12/13 activate the small GTPase RhoA [10]. LPA ligands have been known to influence a wide range of cellular functions including cell proliferation, apoptosis, and migration [9,11,12]. Overwhelming evidence points to the function of LPA in pain because LPA (1) stimulates cyclooxygenase-2 expression (COX-2) [13], which contributes to inflammatory pain; (2) increases reactive oxygen species (ROS) release [14], which is involved in the development and maintenance of neuropathic pain [15]; (3) induces nociception-producing activity and substance P release on sensory neurons [16]; and (4) is involved in the initiation of neuropathic pain [3,17,18]
Farnesyl pyrophosphate (FPP) is a key intermediate in the biosynthesis of steroids including cholesterol as well as the donor of the farnesyl group for isoprenylation of many proteins, including the βγ subunit of some G proteins and GTPases, Ras and Rho [19]. FPP is synthesized from farnesol via two successive phosphorylation reactions mediated by farnesol kinase and farnesyl phosphate kinase, transitioning first through farnesyl monophosphate (FMP) then to FPP [20].
The actions of a class of cholesterol-lowering drugs called Statins (e.g., Atorvastatin, Lipitor) suggest the impact of FPP on pain. These drugs inhibit HMG-CoA reductase (3-hydroxsyl-3- methylglutaryl coenzyme A reductase), the first committed enzyme of the cholesterol synthesis pathway [21]. Recent data indicate that Statins are also anti-inflammatory and anti-nociceptive compounds [22]. This report also showed that Atorvastatin lowers hyperalgesia produced by bradykinin and cytokines as well as being associated with a drop in inflammatory mediators such as TNF-α and IL-1β. Because FPP is a key intermediate for cholesterol synthesis, a reduced level of such intermediates may contribute to reduced hyperalgesia.
Recent data indicated that FPP acts as a ligand of GPR92/LPA5 [23], suggesting an underlying mechanism for FPP in relation to pain. Activation of GPR92/LPA5 by FPP increases IP production, cAMP levels, and Ca2+ levels in a concentration-dependent manner. Oh and colleagues further demonstrated that FPP and LPA are able to activate Gq/11 and Gs-mediate signaling pathways. Evidence for a role in pain comes from the fact that GPCR92/LPA5 is highly expressed in and largely co-localized with TRPV1 in mouse and human dorsal root ganglion [23], suggesting that this receptor may contribute to the processing of noxious sensory stimuli. However, FPP may not interact with GPR92 in a typical receptor-ligand manner. A report by Yin and colleagues [24] states that FPP was not effective in recruiting beta arrestin in a GPR92 expression system. A more recent report shows that FPP is also a potent activator of TPRV3, which adds yet another dimension on how FPP may play a role in the processing of noxious stimuli [25]. It will be important to investigate any potential interactions of GPR92/LPA5 with TRPV3 to further elucidate this complex signaling system.
In order to begin investigations of FPP and LPA’s functional relevance as signaling molecules in the central nervous system, we developed HPLC/MS/MS extraction protocols for each compound from brain tissue and examined the relative distribution of FPP and four different endogenous LPAs; oleoyl-LPA (O-LPA), arachidonyl-LPA (A-LPA), palmitoyl-LPA (P-LPA) and stearoyl-LPA (S-LPA) were measured here in 9 distinct regions of the brain. Our findings show there is not a uniform distribution throughout the brain of any of the 5 compounds measured lending support to the hypothesis that they are working as signaling molecules and not simply as structural lipids. While the relative distributions are not the same, the highest concentrations of each are found primarily in brainstem and midbrain providing a focus for future research.
2. Results and Discussion
2.1. Distribution of FPP in Rat Brain
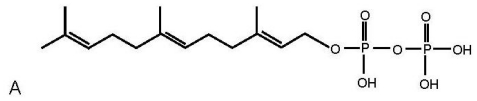
Co-eluting peaks for synthesized FPP and a brain constituent that matched the HPLC/MS/MS fingerprint of FPP were observed in each area of the brain examined (representative brain region shown in Figure 1). The average rate of recoveries across brain areas was 59%. FPP was not distributed equally throughout the brain (Figure 1). The highest production of FPP was measured in the brainstem (89.55E-12 ± 17.10E-12 moles/gram tissue), followed by the midbrain (56.95E-12 ± 19.89E-12) and thalamus (64.95E-12 ± 15.20E-12), moderate levels were measured in the hypothalamus (39.91E-12 ± 6.8E-12), cerebellum (33.62E-12 ± 8.94E-12), hippocampus (37.31E-12 ± 4.98E-12) and striatum (45.19E-12 ± 12.51E-12), and the lowest levels were measured in the pituitary (11.81E-12 ± 4.81E-12) and cortex (23.09E-12 ± 6.78E-12).
Figure 1.
(A) structure of FPP (B) co-eluting peaks for synthesized FPP (standard FPP) and a representative brain constituent (Endogenous FPP) (C) distribution of FPP in selective brain areas. Abbreviations: PIT, pituitary; CTX, cortex; CER, cerebellum; HIPP, hippocampus; HYP, hypothalamus; STR, striatum; MB, midbrain; THAL, thalamus; BS, brain stem.
2.2. Distribution of Four LPA Species in Rat Brain
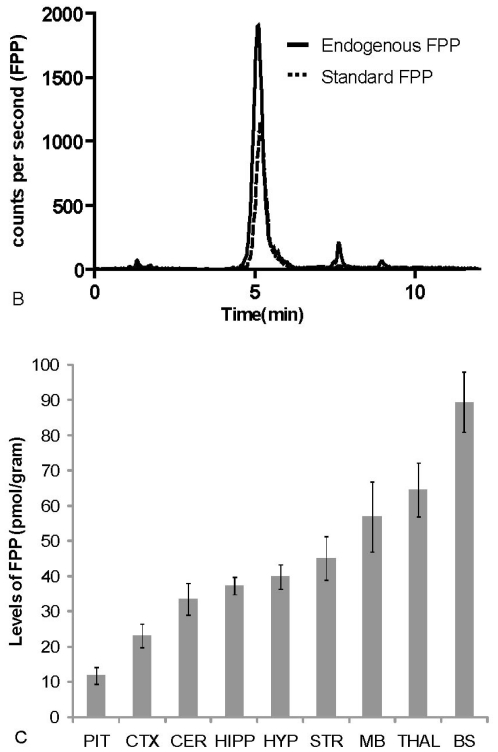
Co-eluting peaks for all four synthesized LPA molecules and a corresponding brain constituent were observed in each area of the brain examined. Figure 2 demonstrates the chromatograms of the LPAs HPLC/MS/MS methods in which each LPA species is measured from the complex brain lipid extract. Using the C18 reversed-phased analytical column the arachidonoyl species elutes first, followed by the palmitoyl, oleoyl and finally stearoyl species.
Figure 2.
Structure of four LPA species and corresponding HPLC/MS/MS chromatographs for each of these species from brain extracts. Colors for each chromatographic peak correspond to the color bar next to the name of the LPA. Using the C18 reversed phase analytical column the least saturated LPA (arachidonoyl-sn-glycerol-3 phosphate) elutes first and the longest and completely saturated LPA (stearoyl-sn-glycerol-3 phosphate) elutes last.
Like FPP, the highest amounts of LPAs were measured in the brainstem, midbrain, and thalamus, though not equally distributed (Table 1). Relative abundance of each LPA species was not consistent in any brain areas tested (Table 1). A-LPA shows the most divergence from the other three LPA species in that it is least abundant in cortex and the levels in the hypothalamus are equivalent to those in the brainstem. Averaged recoveries were equivalent across compounds: A-LPA (90 ± 6%), O-LPA (70 ± 17%), P-LPA (70 ± 23%), and S-LPA (65 ± 8%).
Table 1.
Levels of 4 LPA species in 8 areas of the rat brain determined by HPLC/MS/MS. Amounts are listed in acceding order by brain area.
| P-LPA in nmols/gr | A-LPA in pmols/gr | ||
|---|---|---|---|
| Hypothalamus | 4.22 ± 0.81 | Cortex | 220 ± 30.2 |
| Hippocampus | 6.16 ± 0.37 | Cerebellum | 285 ± 25.1 |
| Cortex | 6.96 ± 1.19 | Striatum | 299 ± 23.2 |
| Striatum | 7.88 ± 1.11 | Hippocampus | 316 ± 15.3 |
| Cerebellum | 13.4 ± 1.58 | Hypothalamus | 339 ± 67.6 |
| Thalamus | 19.6 ± 0.58 | Brain Stem | 364 ± 16.3 |
| Brain Stem | 25 ± 3.17 | Thalamus | 478 ± 29.6 |
| Midbrain | 28.6 ± 2.26 | Midbrain | 536 ± 41.8 |
|
S-LPA in nmols/gr |
O-LPA in nmols/gr |
||
| Hypothalamus | 4.34 ± 1.64 | Hypothalamus | 7.58 ± 1.83 |
| Hippocampus | 6.30 ± 0.62 | Hippocampus | 9.76 ± 1.22 |
| Striatum | 7.68 ± 0.46 | Striatum | 11.4 ± 1.01 |
| Cortex | 10.7 ± 0.55 | Cortex | 17.5 ± 3.27 |
| Cerebellum | 11.2 ± 0.51 | Thalamus | 37.8 ± 4.05 |
| Brain Stem | 13 ± 0.56 | Cerebellum | 28.1 ± 5.34 |
| Midbrain | 14 ± 1.99 | Midbrain | 63.6 ± 7.48 |
| Thalamus | 15.7 ± 2.24 | Brain Stem | 69.5 ± 4.30 |
2.3. Discussion
This study provides a framework to examine FPP and LPA production that will direct future studies on functional relevance of each as signaling molecules. This is particularly important in that these data show that the relative distributions are significantly different and, therefore, their contributions as substrates and signaling molecules is dependent on the population and phenotype of cells within a region. That there is not an equal distribution throughout the brain also provides evidence to suggest that the use of plasma levels of these lipids is an inadequate method for measuring central nervous system activity. While these lipids are detectable in plasma, it is important to recognize the distinction between those derived likely from circulating immune cells and those that are made on demand within a specific region of the CNS.
The highest levels of FPP, A-LPA, O-LPA and P-LPA were detected in the brain stem and midbrain in our study. Interestingly, these areas overlap with the descending modulatory system for pain. Rostral ventromedial medullar (RVM) in the brainstem was established as an integral relay in the descending modulation of pain [26,27]. Additionally, the periaqueductal gray (PAG) has extensive involvement in the descending inhibition of pain and is a rich area of study for both opioid [26] and cannabinoid analgesia [28,29].
Electrical stimulation in the lateral and medial midbrain PAG and intraplantar formalin injection caused significant increases in the production of the endogenous cannabinoid anandamide in the PAG [29]. Acute stress was also shown to suppress pain by increasing the production of the endocannabinoids 2-AG and anandamide in the PAG region, which are known to be associated with stress-induced analgesia [28]. In the same study there was a relationship with the elevation of endocannabinoid levels in the PAG after injection of inhibitors of endocannabinoid degradation enzymes and an increase in tolerance to noxious stimuli. Here we show that FPP and LPA are significantly more abundant in the midbrain and brainstem. Their abundance here may be an indication that they are involved in the descending regulatory pathways for pain including the PAG and the RVM, providing yet another aspect of the fine-tuning of the PAG and RVM systems.
By examining the relative levels of these lipids in distinct brain regions we also demonstrate that they are not merely structural components of the cell membrane. If they were simply produced in this capacity their levels should be more consistent throughout the brain. Even with the growing interest in LPAs and FPP as signaling molecules over the last decade, few studies have examined levels of these lipids in the CNS. One study measured the level of FPP using LC/MS/MS in human frontal cortex tissue [30] from post-mortem brains in five elderly patients and found it to be in the range of 4.5 ng/mg. Here, we show that levels of FPP in rat cortex are ~7 ng/mg, so these levels are in an equivalent range.
A current therapy aimed at the reduction of lipogensis related to high blood pressure and heart disease is the use of Statins. These are already known to reduce hypernociception likely mediated by changes in the levels of bradykinin and cytokines, IL-1β, and PGE2 [22]. However, the antinociceptive effect of Statins also appears to be tightly related to reducing the production of FPP in that exogenous malvonate, the precursor of FPP, reversed the antinociception by Statins in the same study. Also, inhibition of isoprenoid production by Statins has been shown to increase NOS expression which prevents hypernociceptive activity [31]. Although Statins do not cross the blood brain barrier [32], the peripheral action of statins may reduce central sensitization by decreasing peripheral nociceptive input to the central nervous system [33]. Along with HMG CoA reductase, bisphosphonate is also known to decrease FPP levels primarily by inhibiting farnesyl diphosphate synthase (FPPS) [34]. Interestingly, bisphosphanate also has antinociceptive effects [35] in that chronic treatment with bisphosphanate attenuated hyperalgesia associated with chronic peripheral neuropathy and inflammation.
The roles of LPAs in pain are also currently under intense study and have been recently reviewed by many authors [36,37]. LPA causes reactive oxygen species (ROS) release [38], which is involved in signaling of noxious stimuli and the perception of pain [39,40]. LPA-induced activation of phosphatidylinositol–3 kinase (PI3K) has been suggested to play an essential role in the induction of pain hypersensitivity [41]. PI3K is involved in capsaicin-induced heat hyperalgesia, perhaps through TRPV1 sensitization in that capsaicin-induced TRPV1 current enhancement was blocked by PI3K inhibition. LPA was also shown to cause sensory neuron sensitization through Gi/0 activation and substance P (SP) release [42]. Substance P directly activates IL-8 release from macrophages leading to hyperalgesia through sympathetic neurons stimulation [43,44]. Moreover, Inoue M. et al. showed that intrathecal injection of LPA into wild-type animals elicited mechanical allodynia and thermal hyperalgesia effects similar to those induced by peripheral nerve injury [18]. These effects of LPAs on peripheral sensory processing underscore their potency and the need to understand LPA functions in the CNS.
3. Experimental Section
3.1. Sample Preparation
Hypothalamus, pituitary, thalamus, brainstem, cerebellum, hippocampus, striatum, cortex and midbrain were dissected from 10 female Sprague-Dawley rats and immediately frozen at −80 °C until used for extractions. For FPP extractions, tissue was homogenized on ice in an ethanol/butanol/70 mM (1:1.25:1.25. v/v/v) ammonium hydroxide solution using a polytron homogenizer. The homogenate was centrifuged at 20,000 g, 25 °C for 5 min. The supernatant was loaded on polymeric solid phase extraction columns (Strata-X SPE, Phenomena), washed with 40% HPLC methanol and eluted with 100% HPLC methanol/1% triethyl amine. For LPA extractions, tissue was homogenized in 100% HPLC-grade methanol, homogenate was centrifuged at 20,000 g, 25 °C for 20 min, the supernatant then diluted with HPLC-grade water to make a 30% organic solution which was then loaded on pre-conditioned Empore C8 SPE columns (Varian, Palo Alto, CA), columns were washed with HPLC-grade water, 40% HPLC-grade methanol, and eluted with 100% HPLC-grade methanol.
3.2. HPLC/MS/MS
Levels of each compound were analyzed by multiple reactions monitoring (MRM) mode on a triple quadrupole mass spectrometer API 3000, with electrospray ionization. Samples were loaded using Shimadzu SCL10Avp autosampler. The flow rate was 200 uL/min achieved by a system comprised of a Shimadzu controller and two Shimadzu LC10ADvp pumps.
3.2.1. FPP Analysis
The chromatographic analysis was performed on a C18 reversed phase column (Phenomenex Gemini C18 column, 50 × 2.0 mm, 3 μM) guarded by SecurityGuard Cartridge System (Phenomenex). Mobile phase A, 1.0% triethyl amine (TEA), and mobile phase B, 90% isopropanol with 1.0% TEA, were used for gradient elution. Mobile phase B was held constant at 2% for 2 min (mobile phase A at 98%) after sample injection, then a linear gradient increased B to 100% between 2 and 12 min, which was maintained for 2 min and brought back to 2% at 14.50 prior to 2 minutes of column equilibration. Columns were maintained at 40 °C. Recoveries were determined by spiking supernatant from paired brain areas and analyzing the% recovery of the spiked samples. FPP levels were determined using MRM in negative ion mode where the parent mass (MH-) was 381.0 m/z and the two product ions measured where 79.0 and 158.8 m/z.
3.2.2. LPA Analysis
The chromatographic analysis was performed on a 210 mm Zorbax Eclipse XDB-C18 reversed phase HPLC (3.5 um internal diameter) column maintained at 40 °C. Mobile phase A: 80/20 H2O/MeOH with 10mM ammonium acetate and 1% acetic acid and mobile phase B: 100% Methanol with 10mM ammonium acetate and 1% acetic acid were used for gradient loading and elution. LPA parent and fragment masses monitored via MRM are as follows: P-LPA parent mass 409.48 fragment mass 153.10; O-LPA parent mass 435.57 fragment mass 153.10; S-LPA parent mass 437.27 fragment mass 153.10; and A-LPA parent mass 457.30 fragment mass 153.10. Due to a lack of deuterium-labeled standards to use as internal standards to calculate percent recoveries, they were determined by using the alternate half of the brain dissections from those used for extractions of unknown amounts and spiking brain areas with μM quantities of each LPA subtype to estimate overall recoveries.
4. Conclusions
In this study, levels of FPP and four species of LPA were shown to be differentially produced throughout the rodent brain. These data provide a framework for investigations into the functional relationships of these lipid ligands in these specific brain areas, many of which are associated with pain.
Acknowledgements
We thank Bo Tan for technical assistance. SL and SR were supported through Metacyte grants. HBB and JMW were supported by DA018224
References
- 1.An S, Dickens MA, Bleu T, Hallmark OG, Goetzl EJ. Molecular cloning of the human edg2 protein and its identification as a functional cellular receptor for lysophosphatidic acid. Biochem. Biophys. Res. Commun. 1997;231:619–622. doi: 10.1006/bbrc.1997.6150. [DOI] [PubMed] [Google Scholar]
- 2.Hecht JH, Weiner JA, Post SR, Chun J. Ventricular zone gene-1 (vzg-1) encodes a lysophosphatidic acid receptor expressed in neurogenic regions of the developing cerebral cortex. J. Cell Biol. 1996;135:1071–1083. doi: 10.1083/jcb.135.4.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An S, Goetzl EJ, Lee H. Signaling mechanisms and molecular characteristics of G protein-coupled receptors for lysophosphatidic acid and sphingosine 1-phosphate. J. Cell Biochem. Suppl. 1998;30–31:147–157. [PubMed] [Google Scholar]
- 4.Bandoh K, Aoki J, Hosono H, Kobayashi S, Kobayashi T, Murakami-Murofushi K, Tsujimoto M, Arai H, Inoue K. Molecular cloning and characterization of a novel human G-protein-coupled receptor, EDG7, for lysophosphatidic acid. J. Biol. Chem. 1999;274:27776–27785. doi: 10.1074/jbc.274.39.27776. [DOI] [PubMed] [Google Scholar]
- 5.Im D-S, Heise CE, Harding MA, George SR, O'Dowd BF, Theodorescu D, Lynch KR. Molecular cloning and characterization of a lysophosphatidic acid receptor, Edg-7, expressed in prostate. Mol. Pharm. 2000;57:753–759. [PubMed] [Google Scholar]
- 6.Lee C-W, Rivera R, Dubin AE, Chun J. LPA4/GPR23 is a lysophosphatidic acid (LPA) receptor utilizing Gs-, Gq/Gi-mediated calcium signaling and G12/13-mediated rho activation. J. Biol. Chem. 2007;282:4310–4317. doi: 10.1074/jbc.M610826200. [DOI] [PubMed] [Google Scholar]
- 7.Lee C-W, Rivera R, Gardell S, Dubin AE, Chun J. GPR92 as a New G12/13- and Gq-coupled Lysophosphatidic Acid Receptor That Increases cAMP, LPA5. J. Biol. Chem. 2006;281:23589–23597. doi: 10.1074/jbc.M603670200. [DOI] [PubMed] [Google Scholar]
- 8.Moolenaar WH. Bioactive lysophospholipids and their G protein-coupled receptors. Exp. Cell Res. 1999;253:230–238. doi: 10.1006/excr.1999.4702. [DOI] [PubMed] [Google Scholar]
- 9.Zhang H, Wang D, Sun H, Hall RA, Yun CC. MAGI-3 regulates LPA-induced activation of Erk and RhoA. Cell. Sign. 2007;19:261–268. doi: 10.1016/j.cellsig.2006.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Q, Liu M, Kozasa T, Rothstein JD, Sternweis PC, Neubig RR. Thrombin and lysophosphatidic acid receptors utilize distinct rhoGEFs in prostate cancer cells. J. Biol. Chem. 2004;279:28831–28834. doi: 10.1074/jbc.C400105200. [DOI] [PubMed] [Google Scholar]
- 11.Tigyi G, Parrill AL. Molecular mechanisms of lysophosphatidic acid action. Prog. Lipid Res. 2003;42:498–526. doi: 10.1016/s0163-7827(03)00035-3. [DOI] [PubMed] [Google Scholar]
- 12.Kranenburg O, Moolenaar WH. Ras-MAP kinase signaling by lysophosphatidic acid and other G protein-coupled receptor agonists. Oncogene. 2001;20:1540–1546. doi: 10.1038/sj.onc.1204187. [DOI] [PubMed] [Google Scholar]
- 13.Oyesanya R, Lee Z, Wu J, Chen J, Song Y, Mukherjee A, Dent P, Kordula T, Zhou H, Fang X. Transcriptional and post-transcriptional mechanisms for lysophosphatidic acid-induced cyclooxygenase-2 expression in ovarian cancer cells. FASEB J. 2008;22:2639–2651. doi: 10.1096/fj.07-101428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Q, Olashaw N, Wu J. Participation of reactive oxygen species in the lysophosphatidic acid-stimulated mitogen-activated protein kinase kinase activation pathway. J. Biol. Chem. 1995;270:28499. doi: 10.1074/jbc.270.48.28499. [DOI] [PubMed] [Google Scholar]
- 15.Kim H, Park S, Zhou J, Taglialatela G, Chung K, Coggeshall R, Chung J. Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain. 2004;111:116–124. doi: 10.1016/j.pain.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Renbäck K, Inoue M, Ueda H. Lysophosphatidic acid-induced, pertussis toxin-sensitive nociception through a substance P release from peripheral nerve endings in mice. Neurosci. Lett. 1999;270:59–61. doi: 10.1016/s0304-3940(99)00464-4. [DOI] [PubMed] [Google Scholar]
- 17.Pietruck FBS, Virchow S, Brockmeyer N, Siffert W. Signalling properties of lysophosphatidic acid in primary human skin fibroblasts: Role of pertussis toxin-sensitive GTP-binding proteins. Naunyn. Schmiedebergs. Arch. Pharmacol. 1997;355:1–7. doi: 10.1007/pl00004906. [DOI] [PubMed] [Google Scholar]
- 18.Inoue M, Rashid M, Fujita R, Contos J, Chun J, Ueda H. Initiation of neuropathic pain requires lysophosphatidic acid receptor signaling. Nat. Med. 2004;10:712–718. doi: 10.1038/nm1060. [DOI] [PubMed] [Google Scholar]
- 19.Liliom K, Baksa A, Tsukahara T, Tsukahara R, Zelman-Femiak M, Swiezewska E, Tigyi G. Farnesyl phosphates are endogenous ligands for lysophosphatidic acid receptors. Febs. J. 2006;273:98–98. doi: 10.1016/j.bbalip.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Westfall D, Aboushadi N, Shackelford JE, Krisans SK. Metabolism of farnesol: Phosphorylation of farnesol by rat liver microsomal and peroxisomal fractions. Biochem. Biophys. Res. Commun. 1997;230:562–568. doi: 10.1006/bbrc.1996.6014. [DOI] [PubMed] [Google Scholar]
- 21.Liao J. Isoprenoids as mediators of the biological effects of statins. Am. Soc. Clin. Investig. 2002;110:285–288. doi: 10.1172/JCI16421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santodomingo-Garzon T, Cunha TM, Verri WA, Jr, Valerio DA, Parada CA, Poole S, Ferreira SH, Cunha FQ. Atorvastatin inhibits inflammatory hypernociception. Br. J. Pharmacol. 2006;149:14–22. doi: 10.1038/sj.bjp.0706836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oh da Y, Yoon JM, Moon MJ, Hwang JI, Choe H, Lee JY, Kim JI, Kim S, Rhim H, O'Dell DK, Walker JM, Na HS, Lee MG, Kwon HB, Kim K, Seong JY. Identification of farnesyl pyrophosphate and N-arachidonylglycine as endogenous ligands for GPR92. J. Biol. Chem. 2008;283:21054–21064. doi: 10.1074/jbc.M708908200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yin H, Chu A, Li W, Wang B, Shelton F, Otero F, Nguyen DG, Caldwell JS, Chen YA. Lipid G protein-coupled receptor ligand identification using beta-arrestin PathHunter assay. J. Biol. Chem. 2009;284:12328–12338. doi: 10.1074/jbc.M806516200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bang S, Yoo S, Yang TJ, Cho H, Hwang SW. Farnesyl pyrophosphate is a novel pain-producing molecule via specific activation of TRPV3. J. Biol. Chem. 2010;285:19362–19371. doi: 10.1074/jbc.M109.087742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fields H. Pain modulation: Expectation, opioid analgesia and virtual pain. Prog. Brain Res. 2000;122:245. doi: 10.1016/s0079-6123(08)62143-3. [DOI] [PubMed] [Google Scholar]
- 27.Walker J, Huang S. Endocannabinoids in pain modulation. Prostaglandins Leukot. Essent. Fatty Acids. 2002;66:235–242. doi: 10.1054/plef.2001.0361. [DOI] [PubMed] [Google Scholar]
- 28.Hohmann AG, Suplita RL, Bolton NM, Neely MH, Fegley D, Mangieri R, Krey JF, Walker JM, Holmes PV, Crystal JD, Duranti A, Tontini A, Mor M, Tarzia G, Piomelli D. An endocannabinoid mechanism for stress-induced analgesia. Nature. 2005;435:1108–1112. doi: 10.1038/nature03658. [DOI] [PubMed] [Google Scholar]
- 29.Walker JM, Hohmann AG, Martin WJ, Strangman NM, Huang SM, Tsou K. The neurobiology of cannabinoid analgesia. Life Sci. 1999;65:665–673. doi: 10.1016/s0024-3205(99)00289-1. [DOI] [PubMed] [Google Scholar]
- 30.Hooff G, Volmer D, Wood W, Müller W, Eckert G. Isoprenoid quantitation in human brain tissue: A validated HPLC–fluorescence detection method for endogenous farnesyl-(FPP) and geranylgeranylpyrophosphate (GGPP) Anal. Bioanal. Chem. 2008;392:673–680. doi: 10.1007/s00216-008-2306-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laufs U. Beyond lipid-lowering: Effects of statins on endothelial nitric oxide. Eur. J. Clin. Pharmacol. 2003;58:719–731. doi: 10.1007/s00228-002-0556-0. [DOI] [PubMed] [Google Scholar]
- 32.Sparks DL, Connor DJ, Browne PJ, Lopez JE, Sabbagh MN. HMG-CoA reductase inhibitors (statins) in the treatment of Alzheimer's disease and why it would be ill-advise to use one that crosses the blood-brain barrier. J. Nutr. Health Aging. 2002;6:324–331. [PubMed] [Google Scholar]
- 33.Millan MJ. The induction of pain: An integrative review. Prog. Neurobiol. 1999;57:1–164. doi: 10.1016/s0301-0082(98)00048-3. [DOI] [PubMed] [Google Scholar]
- 34.Guo RT, Cao R, Liang PH, Ko TP, Chang TH, Hudock MP, Jeng WY, Chen CK, Zhang Y, Song Y, Kuo CJ, Yin F, Oldfield E, Wang AH. Bisphosphonates target multiple sites in both cis- and trans-prenyltransferases. Proc. Natl. Acad. Sci. USA. 2007;104:10022–10027. doi: 10.1073/pnas.0702254104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walker K, Medhurst SJ, Kidd BL, Glatt M, Bowes M, Patel S, McNair K, Kesingland A, Green J, Chan O, Fox AJ, Urban LA. Disease modifying and anti-nociceptive effects of the bisphosphonate, zoledronic acid in a model of bone cancer pain. Pain. 2002;100:219–229. doi: 10.1016/S0304-3959(02)00040-4. [DOI] [PubMed] [Google Scholar]
- 36.Ueda H. Molecular mechanisms of neuropathic pain-phenotypic switch and initiation mechanisms. Pharmacol. Ther. 2006;109:57–77. doi: 10.1016/j.pharmthera.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Choi JW, Herr DR, Noguchi K, Yung YC, Lee C-W, Mutoh T, Lin M-E, Teo ST, Park KE, Mosley AN, Chun J. LPA Receptors: Subtypes and biological actions. Annu. Rev. Pharmacol. Toxicol. 2010;50:157–186. doi: 10.1146/annurev.pharmtox.010909.105753. [DOI] [PubMed] [Google Scholar]
- 38.Chen Q, Olashaw N, Wu J. Participation of reactive oxygen species in the lysophosphatidic acid-stimulated mitogen-activated protein kinase kinase activation pathway. J. Biol. Chem. 1995;270:28499–28502. doi: 10.1074/jbc.270.48.28499. [DOI] [PubMed] [Google Scholar]
- 39.Zeinab K, Tao L, Robert DH. Free radicals contribute to the reduction in peripheral vascular responses and the maintenance of thermal hyperalgesia in rats with chronic constriction injury. Pain. 1999;79:31–37. doi: 10.1016/S0304-3959(98)00143-2. [DOI] [PubMed] [Google Scholar]
- 40.Salter M, Strijbos PJLM, Neale S, Duffy C, Follenfant RL, Garthwaite J. The nitric oxide-cyclic GMP pathway is required for nociceptive signalling at specific loci within the somatosensory pathway. Neuroscience. 1996;73:649–655. doi: 10.1016/0306-4522(96)00060-7. [DOI] [PubMed] [Google Scholar]
- 41.Sun R, Yan J, Willis WD. Activation of protein kinase B/Akt in the periphery contributes to pain behavior induced by capsaicin in rats. Neuroscience. 2007;144:286–294. doi: 10.1016/j.neuroscience.2006.08.084. [DOI] [PubMed] [Google Scholar]
- 42.Renbäck K, Inoue M, Ueda H. Lysophosphatidic acid-induced, pertussis toxin-sensitive nociception through a substance P release from peripheral nerve endings in mice. Neuroscience Letters. 1999;270:59–61. doi: 10.1016/s0304-3940(99)00464-4. [DOI] [PubMed] [Google Scholar]
- 43.Lotz M, Vaughan J, Carson D. Effect of neuropeptides on production of inflammatory cytokines by human monocytes. Science. 1988;241:1218–1221. doi: 10.1126/science.2457950. [DOI] [PubMed] [Google Scholar]
- 44.Taub DD, Oppenheim JJ. Chemokines, inflammation and the immune system. Ther. Immunol. 1994;1:229–246. [PubMed] [Google Scholar]