Abstract
Almost 25 centuries ago, Hippocrates, the father of medicine, proclaimed “Let food be thy medicine and medicine be thy food.” Exploring the association between diet and health continues today. For example, we now know that as many as 35% of all cancers can be prevented by dietary changes. Carcinogenesis is a multistep process involving the transformation, survival, proliferation, invasion, angiogenesis, and metastasis of the tumor and may take up to 30 years. The pathways associated with this process have been linked to chronic inflammation, a major mediator of tumor progression. The human body consists of about 13 trillion cells, almost all of which are turned over within 100 days, indicating that 70,000 cells undergo apoptosis every minute. Thus, apoptosis/cell death is a normal physiological process, and it is rare that a lack of apoptosis kills the patient. Almost 90% of all deaths due to cancer are linked to metastasis of the tumor. How our diet can prevent cancer is the focus of this review. Specifically, we will discuss how nutraceuticals, such as allicin, apigenin, berberine, butein, caffeic acid, capsaicin, catechin gallate, celastrol, curcumin, epigallocatechin gallate, fisetin, flavopiridol, gambogic acid, genistein, plumbagin, quercetin, resveratrol, sanguinarine, silibinin, sulforaphane, taxol, γ-tocotrienol, and zerumbone, derived from spices, legumes, fruits, nuts, and vegetables, can modulate inflammatory pathways and thus affect the survival, proliferation, invasion, angiogenesis, and metastasis of the tumor. Various cell signaling pathways that are modulated by these agents will also be discussed.
Keywords: Inflammation, NF-κB, Nutraceuticals, Therapeutics, Tumorigenesis
1 Introduction
Tumor formation in humans is a multistage process involving a series of events and generally occurs over an extended period. During this process, accumulation of genetic and epigenetic alterations leads to the progressive transformation of a normal cell into a malignant cell. Cancer cells acquire several abilities that most healthy cells do not possess: they become resistant to growth inhibition, proliferate without dependence on growth factors, replicate without limit, evade apoptosis, and invade, metastasize, and support angiogenesis [1]. Although the mechanisms by which cancer cells acquire these capabilities vary considerably among the various types of tumors, most of the physiological changes associated with these mechanisms involve alteration of signal transduction pathways. During the past quarter century, researchers’ understanding of the proteins involved in the various steps of tumor cell development has grown, providing opportunities for identifying new targets for therapeutic development (Fig. 1).
Fig. 1.
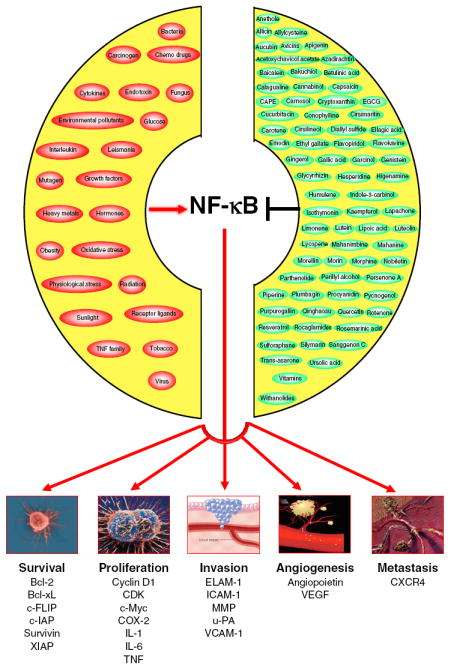
Progression of tumor cell development involves survival, proliferation, invasion, angiogenesis, and metastasis. NF-κB activation regulates tumor cell development by targeting one or more steps in the pathway. Carcinogens activate NF-κB, whereas nutraceuticals inhibit NF-κB
Despite the development of these new therapies, however, cancer remains the second-leading cause of death in the USA and accounts for nearly one in every four deaths. The American Cancer Society estimates that 569,490 Americans will die of cancer in 2010 (www.cancer.org/docroot/stt/stt_0.asp). It is now believed that 90–95% of all cancers are attributed to lifestyle, with the remaining 5–10% attributed to faulty genes [2]. In 2010, for example, about 171,000 cancer deaths will be caused by tobacco use alone. In addition, one third of all cancer deaths in America are attributed to poor nutrition, physical inactivity, overweight, and obesity [3].
Multiple epidemiological and animal studies have shown that consumption of foods rich in fruits and vegetables decreased the occurrence of cancers [4-8]. Almost 30 years ago, Professors Doll and Peto, after conducting an epidemiological study for the World Health Organization, suggested that appropriate nutrition could prevent approximately 35% of cancer deaths and that up to 90% of certain cancers could be avoided by dietary enhancement [9, 10]. A recent elegant review by Chan and Giovannucci [11] provided an overview of the epidemiological evidence supporting the roles of diet, lifestyle, and medication in reducing the risk of colorectal cancer. Similarly, a wealth of information is available, implicating dietary agents in cancers of the skin [12], prostate [13, 14], breast [15], lung [16, 17], and gastrointestinal tract [18]. These studies suggest that much of the suffering and death from cancer could be prevented by consuming a healthy diet, reducing tobacco use, performing regular physical activity, and maintaining an optimal body weight.
It is now clear that cancerous phenotypes result from the dysregulation of more than 500 genes at multiple steps in cell signaling pathways [19, 20]. This indicates that inhibition of a single gene product or cell signaling pathway is unlikely to prevent or treat cancer. However, most current anticancer therapies are based on the modulation of a single target. The ineffective, unsafe, and expensive monotargeted therapies have led to a lack of faith in these approaches. Therefore, the current paradigm for cancer treatment is either to combine several monotargeted drugs or to design drugs that modulate multiple targets. As a result, pharmaceutical companies have been increasingly interested in developing multitargeted therapies. Many plant-derived dietary agents, called nutraceuticals, have multitargeting properties. In addition, these products are less expensive, safer, and more readily available than are synthetic agents [19]. Some nutraceuticals are currently in clinical trials (www.clinicaltrials.gov), but others have already been approved for human use [21-23].
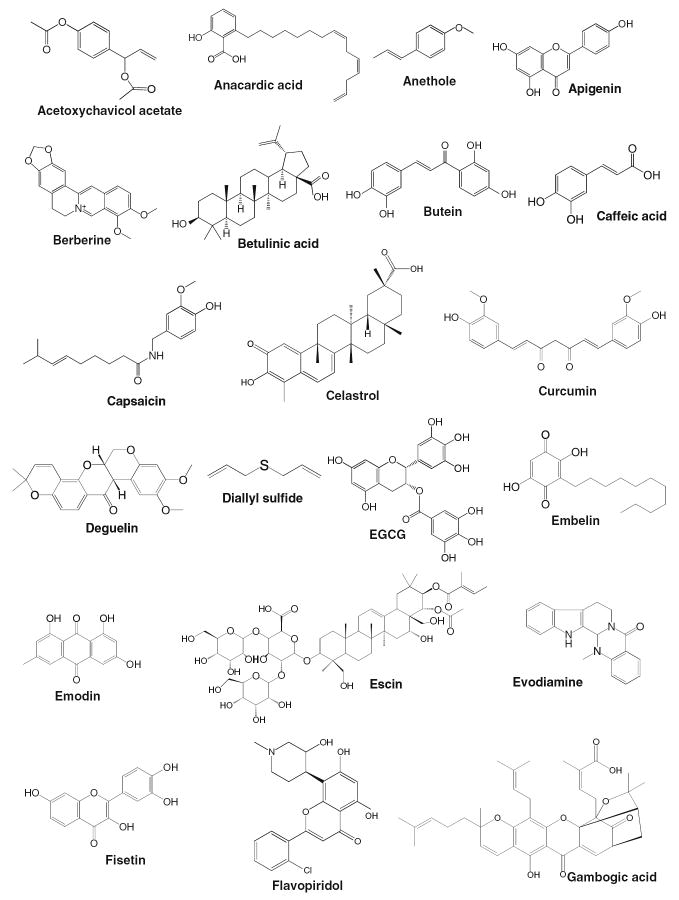
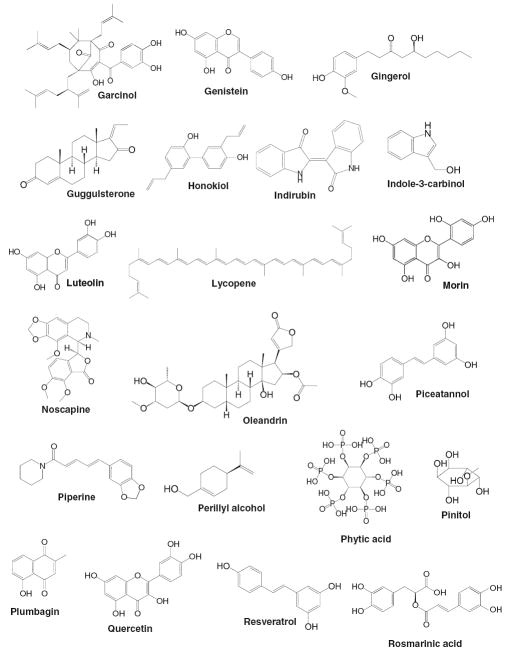
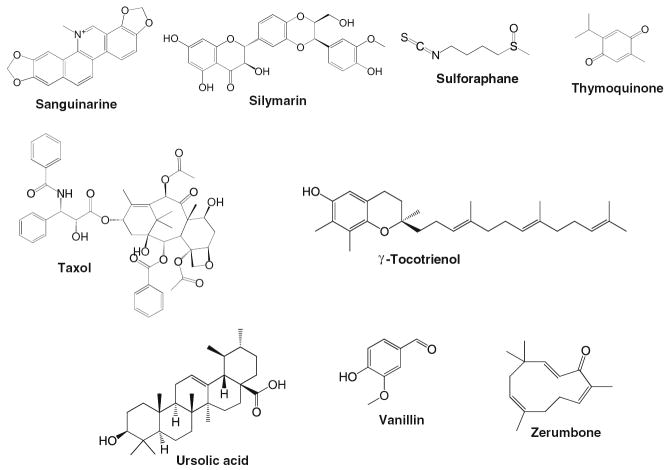
A nutraceutical (a term formed by combining the words “nutrition” and “pharmaceutical”) is simply any substance considered to be a food or part of a food that provides medical and health benefits [23, 24]. The term nutraceutical was coined by Stephen DeFelice in 1989 [23, 25]. During the past decade, a number of nutraceuticals have been identified from natural sources, some of which are shown in Fig. 2. Nutraceuticals are chemically diverse (Fig. 3) and target various steps in tumor cell development (Fig. 4; Table 1).
Fig. 2.
Common sources of nutraceuticals, which include spices, legumes, fruits, nuts, and vegetables
Fig. 3.
Chemical structure of nutraceuticals
Fig. 4.
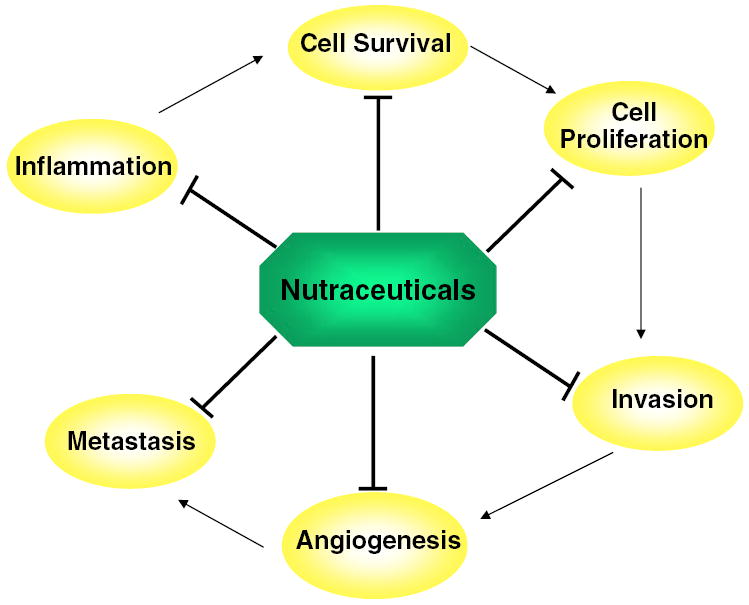
Targets of nutraceuticals during tumor progression. Nutraceuticals can target survival, proliferation, invasion, angiogenesis, and metastasis steps and can influence various steps of tumor cell development by targeting one or more molecules of inflammation
Table 1.
Sources of nutraceuticals and their molecular target linked to cancer
| Nutraceuticals (source) | Molecular target |
|---|---|
| ACA (blue ginger, Alpina galangal) | Survivin, IAP-1/-2, XIAP, Bcl-2, Bcl-xL, Bfl-1/A1, FLIP, cyclin-D1, c-Myc [95] |
| Allicin (garlic, Allium sativum) | ICAM-1, FGF2, VEGF [182] |
| Anacardic acid (cashew, Semecarpus anacardium) | Bcl-2, Bcl-xL, cFLIP, cIAP-1, survivin, cyclin-D1, COX-2 [52] |
| Apigenin (parsley, Petroselinum crispum) | ICAM-1, HIF-1, VEGF [231, 270] |
| Berberine (barberry, Berberis vulgaris) | Bcl-2, Bcl-xL, cyclin-D1, c-Myc, FAK, IKK, NF-κB, u-PA, MMP-2/-9 [59, 60, 271] |
| Butein (cashew, Semecarpus anacardium) | IAP-2, Bcl-2, Bcl-xL, cyclin-D1, c-Myc, ERK-1/-2, NF-κB [188, 189] |
| Caffeic acid (coffee, Coffea arabica) | MMP-9 [190] |
| Capsaicin (chili pepper, Capsicum) | Bcl-2, Bcl-xL, survivin, E2F, PI3K/AKT/Rac1, VEGF, p38MAPK, p125(FAK), AKT [86, 150, 191, 233] |
| Catechin gallate (red pine, Pinus resinosa) | MMP-2/-9 [194] |
| Celastrol (Chinese thunder of god vine, Tripterygium wilfordii) | Bcl-2, Bcl-xL, survivin, cyclin-B1, p21, p27, p38MAPK, FAK [79, 135, 195] |
| Curcumin (turmeric, Curcuma longa) | IAP-1, Bcl-2, survivin, PAK1, cyclin-D1, VEGF, NF-κB, AP-1 [125, 234] |
| EGCG (green tea, Camellia sinensis) | Bcl-2, Bcl-xL, Mcl-1, PI3K/AKT, Ras/ERK, JAK/STAT, NF-κB, AP-1, u-PA, VEGF, ERK-1/-2 [82, 239, 272] |
| Evodiamine (Evodia fructus, Evodia spp.) | Bcl-2, Bcl-xL, Mcl-1, cdc25c, cyclin-B1, cdc2, NF-κB, MMP-9 [96, 136] |
| Fisetin (smoke tree, Cotinus coggygria) | TAK-1, COX-2, Wnt/EGFR/NF-κB, ERK-1/-2, MMP-2, u-PA, NF-κB [144, 204, 273] |
| Flavopiridol (Dysoxylum binectariferum) | IAP-1, Bcl-2, survivin, CDKs, MMP-2/-9, c-erbB-2, HIF-1α, VEGF [61, 206, 241, 274] |
| Gambogic acid (gamboge tree, Garcinia hanburyi) | Bcl-2, p53, p21, ATR, Chk-1, VEGFR2, c-Src, FAK, AKT [63, 137, 242] |
| Garcinol (kokum, Garcinia indica) | Src, ERK, AKT, nicotinic receptor, cyclin-D3 [64, 275] |
| Genistein (soybeans, Glycine max) | Bcl-2, Bcl-xL, ATM, Chk-1/-2, cdc25, NF-κB, AP-1, u-PA, VEGF, FGF-2, NF-κB, AKT [83, 208, 245] |
| Indole-3-carbinol (broccoli, Brassica oleracea) | p53, casp-8, E-cadherin, α-, β-, and γ- catenin [65, 210] |
| Noscapine (Papaveraceae, Papaver rhoeas) | Bcl-2, COX-2 [97, 276] |
| Plumbagin (Plumbago, Plumbago europaea) | NF-κB, Bcl-2 [91] |
| Quercetin (parsley, Petroselinum crispum) | Bcl-xL, cyclin-D1, MMP-2/-9, VEGF, STAT-3 [214, 277] |
| Resveratrol (red grapes, Vitis vinifera) | Survivin, NF-κB, MMP-2/-9, VEGF, FGF, MAPK [66, 215, 251] |
| Sanguinarine (bloodroot, Sanguinaria canadensis) | Bcl-2, MMP-2/-9, VEGF, AKT [67, 69, 253] |
| Silibinin (milk thistle plant, Silybum marianum) | p53, Bax, Apaf-1, casp-3, CDK-2/-4/-6, cyclin-D1/-D3/-E, p18, p21, p27, MMP-2, u-PA, TIMP-2, NOS, COX, HIF-1α, VEGF [84, 130, 216, 254] |
| Sulforaphane (broccoli, Brassica oleracea italica) | Rb-E2F-1, MMPs [133, 219] |
| Taxol (Pacific yew, Taxus brevifolia) | VEGF [257] |
| γ-Tocotrienol (Palm, Nigella sativa) | AKT, ERK, MMP-2/-9, TIMP-1/-2, HIF-1α, VEGF, ERK-1/-2 [220, 258] |
| Ursolic acid (rosemary, Rosmarinus officinalis) | JNK, AKT, COX-2, cyclin-D1, NF-κB, MMP-9, VEGF, NO [148, 221, 259] |
| Vanillin (vanilla bean) | MMP-9, HGF, PI3K/AKT, VEGF [260] |
| Zerumbone (wild ginger, Zingiber zerumbet) | Bcl-2, cyclin-B1, cdc25c, cdc2, NF-κB, MMP-9 [81, 139, 223] |
ACA acetoxychavicol acetate, AKT AKT8 virus oncogene cellular homolog, AP-1 activator protein 1, Apaf-1 apoptotic protease activating factor 1, ATM ataxia telangiectasia mutated, ATR ataxia telangiectasia and Rad3-related protein, Bax Bcl-2-associated X protein, Bcl-2 B cell lymphoma 2, Bcl-xL B cell lymphoma extra large, casp caspase, cdc25c cell division cycle 25 homolog c (Schizosaccharomyces pombe), CDK cyclindependent kinase, Chk checkpoint kinase, c-Myc cellular v-myc myelocytomatosis viral oncogene homolog (avian), COX-2 cyclooxygenase 2, E2F elongation 2 factor, EGCG epigallocatechin gallate, EGFR epidermal growth factor receptor, ERK extracellular signal-regulated kinase, FAK focal adhesion kinase, FGF fibroblast growth factor, FLIP FLICE/caspase 8 inhibitory protein, HIF-1 hypoxia-inducible factor 1, HGF hepatocyte growth factor, IAP inhibitor of apoptosis protein, ICAM-1 intercellular adhesion molecule 1, IKK IκB kinase, JAK Janus-activated kinase, JNK c-Jun N-terminal kinase, MAPK mitogen-activated protein kinase, Mcl-1 myeloid cell leukemia 1, MMP matrix metalloproteinase, NF-κB nuclear factor kappa B, NO nitric oxide, NOS nitric oxide synthase, PAK1 p21-activated kinase 1, PI3K phosphoinositide 3 kinase, Rac1 Ras-related C3 botulinum toxin substrate 1, Ras Rat sarcoma, Rb retinoblastoma protein, u-PA urokinase-type plasminogen activator, c-Src cellular Rous sarcoma oncogene cellular homolog, STAT signal transducers and activators of transcription protein, TAK-1 TGF-β-activated kinase 1, TIMP tissue inhibitor of metalloproteinases, VEGF vascular endothelial growth factor, VEGFR2 vascular endothelial growth factor receptor 2, Wnt wint, XIAP X-chromosome-linked IAP
Because of the vast number of nutraceuticals identified to date, we cannot discuss all of them. We will therefore focus on some of the more promising nutraceuticals in this review, including allicin, apigenin, berberine, butein, caffeic acid, capsaicin, catechin gallate, celastrol, curcumin, epigallocatechin gallate (EGCG), fisetin, flavopiridol, gambogic acid, genistein, plumbagin, quercetin, resveratrol, sanguinarine, silibinin, sulforaphane, taxol, γ-tocotrienol, and zerumbone, in the context of five specific processes of tumorigenesis: survival, proliferation, invasion, angiogenesis, and metastasis. Since chronic inflammation is one of the major mediators of tumor progression and nuclear factor-κB (NF-κB) is one of the major inflammatory transcription factors involved in the regulation of various steps of tumor cell development, we will also discuss how nutraceuticals can modulate NF-κB and can thus affect survival, proliferation, invasion, angiogenesis, and metastasis of the tumor.
2 Regulation of inflammatory pathways by nutraceuticals
During the past two decades, much evidence has emerged, indicating that, at the molecular level, most chronic diseases, including cancer, are caused by a dysregulated inflammatory response [26]. One of the most important links between inflammation and cancer is proinflammatory transcription factor NF-κB. NF-κB is a ubiquitous and evolutionarily conserved transcription factor that regulates the expression of genes involved in the transformation, survival, proliferation, invasion, angiogenesis, and metastasis of tumor cells (Fig. 1).
The first clue linking NF-κB to cancer was the realization that c-rel, which is the cellular homolog of the v-rel oncogene, encodes a NF-κB subunit and that all of these proteins share the same DNA binding domain, the Rel homology domain [27]. Constitutively active NF-κB has now been identified in tissues of most cancer patients, including those with leukemia and lymphoma and cancers of the prostate, breast, oral cavity, liver, pancreas, colon, and ovary [26].
In its resting stage, NF-κB resides in the cytoplasm as a heterotrimer consisting of p50, p65, and the inhibitory subunit IκBα [28]. On activation, the IκBα protein undergoes phosphorylation, ubiquitination, and degradation. p50 and p65 are then released, are translocated to the nucleus, bind specific DNA sequences present in the promoters of various genes, and initiate their transcription. A number of proteins are involved in the NF-κB signaling pathway. Because of the relevance of the NF-κB signaling pathway in cancer, this pathway has been proven to be an attractive target for therapeutic development. More than 700 inhibitors of the NF-κB activation pathway have been reported, including antioxidants, peptides, small RNA/DNA, microbial and viral proteins, small molecules, and engineered dominant-negative or constitutively active polypeptides [29].
During the past two decades, our laboratory and other researchers’ laboratories have shown that nutraceuticals can exert anticancer activity by suppressing the NF-κB signaling pathway. Curcumin, derived from the ancient Indian medicine turmeric, is a widely studied nutraceutical. When human colonic epithelial cells were pretreated with curcumin, inhibition in tumor necrosis factor (TNF)-α-induced cyclooxygenase 2 (COX-2) gene transcription and NF-κB activation was observed [30]. Curcumin inhibited IκB degradation through downregulation of NF-κB-inducing kinase and IκB kinase (IKK). Curcumin has also been reported to suppress the TNF-α-induced nuclear translocation and DNA binding of NF-κB in a human myeloid leukemia cell line through suppression of IκBα phosphorylation and subsequent degradation [31]. Curcumin has been shown to inhibit IκBα phosphorylation in human multiple myeloma cells [32] and murine melanoma cells [33] through suppression of IKK activity, which contributed to its antiproliferative, proapoptotic, and antimetastatic activities. Recently, we showed that curcumin has the potential to sensitize human colorectal cancer to capecitabine by modulation of cyclin-D1, COX-2, matrix metalloproteinase (MMP)-9, vascular endothelial growth factor (VEGF), and CXC chemokine receptor 4 (CXCR4) expression in an orthotopic mouse model. This was accompanied by inhibition in NF-κB activation [34].
Guggulsterone, obtained from the Commiphora mukul tree, suppresses NF-κB activation through inhibition of IKK-dependent IκBα degradation [35]. Resveratrol, a phytoalexin present in grapes, was shown to induce apoptosis and suppress constitutive NF-κB in rat and human pancreatic carcinoma cell lines [36]. Mammary tumors isolated from rats treated with resveratrol displayed reduced expression of COX-2 and MMP-9, accompanied by reduced NF-κB activation [37]. Treatment of human breast cancer MCF-7 cells with resveratrol also suppressed NF-κB activation and cell proliferation [37]. Capsaicin, a major ingredient of the pepper, has shown chemopreventive and chemoprotective effects [38-42]. Topical application of capsaicin has been associated with inhibition in phorbol 12-myristate 13-acetate (PMA)-induced mouse skin tumor formation and NF-κB activation [43]. The inhibitory effect of capsaicin on NF-κB activation was attributed to blockage of IκBα degradation and NF-κB translocation into the nucleus.
Caffeic acid phenethyl ester has been shown to suppress NF-κB activation by suppressing the binding of the p50–p65 complex directly to DNA [44], whereas both sanguinarine and emodin act by blocking the degradation of IκBα. Alkaloid sanguinarine can prevent phosphorylation and degradation of IκBα in response to TNF, phorbol ester, interleukin (IL)-1, or okadaic acid stimulation [45]. Similar to sanguinarine, emodin inhibits TNF-dependent IκBα degradation [46]. Recently, emodin was shown to oxidize the redox-sensitive site on NF-κB and prevented NF-κB binding to target DNA in HeLa cells, which was associated with a reduction in tumor size [47].
EGCG, an antioxidant found in green tea, has been shown to suppress malignant transformation in a 12-O-tetradecanoylphorbol-13-acetate-stimulated mouse epidermal JB6 cell line, which is mediated by blocking NF-κB activation [48]. EGCG treatment of human epidermal keratinocytes resulted in significant inhibition of ultraviolet-B-induced activation of IKKα, phosphorylation, and subsequent degradation of IκBα and nuclear translocation of p65 [49]. More recently, EGCG was found to abrogate p300-induced p65 acetylation in vitro and in vivo, to increase the level of cytosolic IκBα, and to suppress TNF-α-induced NF-κB activation. Furthermore, EGCG treatment inhibited the acetylation of p65 and the expression of NF-κB target genes in response to diverse stimuli [50]. Another nutraceutical, gallic acid, obtained from natural products such as gallnuts, sumac, oak bark, and green tea, was recently reported to possess anti-histone acetyltransferase activity, thus showing the potential to downregulate NF-κB activation [51]. Anacardic acid, derived from traditional medicinal plants, can also inhibit NF-κB activation by inhibiting p65 acetylation [52].
Thus, nutraceuticals may block one or more steps in the NF-κB signaling pathway, such as the inhibition of IKK activity, IκBα phosphorylation, p65 nuclear translocation, p65 acetylation, and p65 DNA binding. Some nutraceuticals that have the potential to suppress NF-κB activation are shown in Fig. 1. NF-κB can be activated by various carcinogens, some of which are also shown in Fig. 1.
3 Regulation of tumor cell development by nutraceuticals
3.1 Regulation of tumor cell survival by nutraceuticals
Under normal physiological conditions, the human body maintains homeostasis by eliminating unwanted, damaged, aged, and misplaced cells. Homeostasis is carried out in a genetically programmed manner by a process referred to as apoptosis (programmed cell death) [53-55]. Cancer cells are able to evade apoptosis and grow in a rapid and uncontrolled manner. One of the most important ways by which cancer cells have gained this ability is through mutation in the p53 tumor suppressor gene. Without a functional p53 gene, cells lack the DNA-damage-sensing capability that would normally induce the apoptotic cascade. A complex set of proteins, including caspases, proapoptotic and antiapoptotic B cell lymphoma (Bcl)-2 family proteins, cytochrome c, and apoptotic protease activating factor (Apaf)-1, execute apoptosis either by an intrinsic or extrinsic pathway. The intrinsic pathway is mitochondria dependent, whereas the extrinsic pathway is triggered by death receptors (DRs).
Some antiapoptotic proteins such as Bcl-2 and B cell lymphoma extra large (Bcl-xL) [56] and survivin [57] are overexpressed in a wide variety of cancers. Therefore, selective downregulation of antiapoptotic proteins and upregulation of proapoptotic proteins and p53 in cancer cells offer promising therapeutic interventions for cancer treatment. A number of nutraceuticals have shown potential against tumor cell survival by inducing apoptosis with use of various mechanisms in multiple types of cancer cells (Table 2).
Table 2.
Effect of nutraceuticals on tumor cell survival
| Nutraceuticals | Effect |
|---|---|
| ACA | Suppressed TNF-induced NF-κB-dependent expression of survivin, IAP-1/2, XIAP, Bcl-2, Bcl-xL, Bfl-1/A1, and FLIP in nonspecific cancer cell type [95] |
| Anacardic acid | Inhibited Bcl-2, Bcl-xL, cFLIP, cIAP-1, and survivin in various cancer cells [52] |
| Anethole | Increased the survival time and reduced the weight and volume of tumor in a mice model bearing EAT [278] |
| Berberine | Reduced Bcl-2 and Bcl-xL levels and increased Bax, Bak, and casp-3 activation in A549 and H1299 human lung cancer cells [60] |
| β-Escin | Downregulated Bcl-2 and IAP-2 in leukemic and human myeloid cells through inhibition of NF-κB signaling [103] |
| Betulinic acid | Decreased the expression of survivin in LNCaP prostate cancer cells through targeted degradation of Sp proteins [75] |
| Butein | Downregulated the expression of NF-κB-regulated gene products such as IAP-2, Bcl-2, and Bcl-xL [189] |
| Capsaicin | Downregulated STAT-3-regulated expression of Bcl-2, Bcl-xL, and survivin in multiple myeloid cells [86] |
| Celastrol | Enhanced TRAIL-induced apoptosis through the downregulation of cell survival proteins and upregulation of DRs in human breast cancer cells [79] |
| Coronarin | Inhibited NF-κB-regulated expression of IAP-1, Bcl-2, and survivin [100] |
| Curcumin | Induced apoptosis in prostate cancer cells through downregulation of Bcl-2 and Bcl-XL and upregulation of p53, Bax, Bak, PUMA, Noxa, and Bim [71] |
| Deguelin | Induced apoptosis in HTLV-1-transformed T cells via inhibition of survivin and STAT-3 phosphorylation through mediation of ubiquitin/proteasome pathway [87] |
| EGCG | Inhibited survival of EFT through increased expression of Bax and decreased expression of Bcl-2, Bcl-XL, and Mcl-1 proteins and inhibition of IGFIR activity [82] |
| Embelin | Enhanced TRAIL-mediated apoptosis in malignant glioma cells by downregulation of the short isoform of FLIP [72] |
| Emodin | Inhibited IL-6-induced JAK2/STAT-3 and induced apoptosis via downregulation of Mcl-1 in myeloid cells [85] |
| Evodiamine | Reduced survival of cancer cells through downregulation of NF-κB-dependent antiapoptotic gene products [96] |
| Fisetin | Induced apoptosis in chemoresistant human pancreatic AsPC-1 cells through suppression of DR3-mediated NF-κB activation [93] |
| Flavopiridol | Induced apoptosis in human myeloid cells through activation of the bid-cytochrome–casp-9–casp-3 pathway and inhibition in AKT activation [61] |
| Gambogic acid | Induced apoptosis, upregulated p53, and downregulated Bcl-2 in MCF-7 cells [62] |
| Garcinol | Induced apoptosis through downregulation of NF-κB signaling in breast cancer cells [90] |
| Genistein | Induced apoptosis in human ovarian cancer cells by phosphorylation and activation of p53 and decrease in the ratios of Bcl-2/Bax and Bcl-xL/Bax [83] |
| Indirubin | Enhanced TNF-induced apoptosis through modulation of NF-κB signaling pathway in various cancer cells [98] |
| Indole-3-carbinol | Induced apoptosis through activation of p53 and caspase pathway in A549 cells [65] |
| Isodeoxyelephantopin | Potentiated apoptosis through suppression of NF-κB-regulated gene products in various cancer cells [99] |
| Noscapine | Sensitized leukemic cells to chemotherapeutic agents and cytokines by modulating the NF-κB signaling pathway and inducing apoptosis [97] |
| Oleandrin | Sensitized lung cancer cells to TRAIL-induced apoptosis by upregulating DR4 and DR5 [76] |
| Plumbagin | Induced apoptosis in human breast cancer cells through inactivation of NF-κB and downregulation of Bcl-2 [91] |
| Resveratrol | Downregulated survivin and induced apoptosis in human multidrug-resistant SPC-A-1/CDDP cells [66] |
| Sanguinarine | Induced apoptosis in human leukemic U937 cells via Bax upregulation, Bcl-2 downregulation, and casp-3 activation [69] |
| Silymarin | Inhibited survival of hepatic carcinoma cells by upregulating p53, Bax, Apaf-1, and casp-3 and downregulating Bcl-2 and survivin [84] |
| Sulforaphane | Inhibited growth of orthotopically implanted PC-3 tumors through upregulation of DR4, DR5, Bax, and Bak and inhibition of NF-κB, PI3K/AKT, and MEK/ERK activation pathways [94] |
| Thymoquinone | Suppressed NF-κB-dependent antiapoptotic gene products in various cancer cells [101] |
| γ-Tocotrienol | Suppressed NF-κB-dependent antiapoptotic gene products and potentiated apoptosis in various cancer cells [102] |
| Withanolides | Potentiated apoptosis in cancer cells through suppression of NF-κB activation and NF-κB-regulated antiapoptotic proteins [104] |
| Xanthohumol | Induces apoptosis in human colon cancer cells through upregulation of casp-3, casp-8, and casp-9 activation and downregulation of Bcl-2 expression [74] |
| Zerumbone | Induced apoptosis in HepG2 cells by upregulating Bax protein and downregulating Bcl-2 [81] |
ACA acetoxychavicol acetate, Apaf-1 apoptotic protease activating factor 1, Bak Bcl-2 homologous antagonist/killer, Bax Bcl-2-associated X protein, Bcl-2 B cell lymphoma 2, Bcl-xL B cell lymphoma extra large, Bim Bcl-2-interacting mediator of cell death, Bfl-1/A1 Bcl-2-related gene expressed in fetal liver protein A1, casp caspase, DR death receptor, EGCG epigallocatechin gallate, EAT Ehrlich ascites tumor, EFT Ewing family tumors, ERK extracellular signal-regulated kinase, FLIP FLICE/caspase 8 inhibitory protein, HTLV-1 human T cell leukemia virus type 1, IAP inhibitor of apoptosis protein, IGFIR insulin-like growth factor I receptor, IL-6, interleukin 6, JAK Janus-activated kinase, Mcl-1 myeloid cell leukemia 1, MEK MAPK/ERK kinase, NF-κB nuclear factor kappa B, Noxa PhoRbol-12-myristate-13-acetate-induced protein 1, PI3K phosphoinositide 3 kinase, PUMA p53 upregulated modulator of apoptosis, Sp specificity protein, STAT signal transducers and activators of transcription protein, TNF tumor necrosis factor, TRAIL TNF-related apoptosis-inducing ligand, XIAP X-chromosome-linked IAP
Some of the most common ways that nutraceuticals inhibit survival of tumor cells is by activating caspases, inducing proapoptotic proteins, and downregulating antiapoptotic proteins. Acetoxychavicol acetate, for example, a tropical ginger compound, decreased cell viability in breast-carcinoma-derived MCF-7 and MDA-MB-231 cells through a casp-3-dependent increase in apoptosis [58]. In a recent study, berberine induced apoptosis that was associated with reduction in mitochondrial membrane potential and changes in the Bcl-2-associated X protein (Bax)/Bcl-2 ratio [59]. Berberine also induced casp-3, casp-8, and casp-9 activation and the release of cytochrome c from mitochondria through generation of reactive oxygen species (ROS) [59]. Katiyar et al. [60] showed that berberine can induce apoptosis in A549 and H1299 human lung cancer cells that correlated with disruption of mitochondrial membrane potential, reduction in Bcl-2 and Bcl-xL levels, and increased Bax, Bcl-2 homologous antagonist/killer (Bak), and casp-3 activation.
Flavopiridol, a semisynthetic flavone, was shown to enhance TNF-induced apoptosis through activation of the bid-cytochrome–casp-9–casp-3 pathway in human myeloid cells. This induced apoptosis was associated with inhibited AKT8 virus oncogene cellular homolog (AKT) activation and inhibited expression of various antiapoptotic proteins such as inhibitor of apoptosis protein (IAP)-1, IAP-2, X-chromosome-linked IAP (XIAP), Bcl-2, and Bcl-xL [61]. Gu et al. [62] showed that gambogic acid can induce apoptosis in MCF-7 cancer cells through upregulation of p53 and downregulation of Bcl-2. In human malignant melanoma A375 cells, gambogic acid induced apoptosis that was associated with increased Bax expression and decreased Bcl-2 expression [63]. Garcinol was shown to induce apoptosis through inhibition of tyrosine phosphorylation of focal adhesion kinase (FAK) and downregulation of Rous sarcoma oncogene cellular homolog (Src), extra-cellular signal-regulated kinase (ERK), and AKT survival signaling in human colorectal cancer cell line HT-29 [64]. Indole-3-carbinol induced apoptosis through activation of p53 and cleavage of casp-3, casp-8, and casp-9 in lung cancer A549 cells [65].
Resveratrol induced apoptosis in human multidrug-resistant SPC-A-1/CDDP cells associated with downregulation in survivin [66]. Sanguinarine sensitized human gastric adenocarcinoma AGS cells to TNF-related apoptosis-inducing ligand (TRAIL)-induced apoptosis via downregulation of AKT and activation of casp-3 [67]. In MDA-MB-231 human breast carcinoma cells, sanguinarine induced apoptosis through mediation of ROS production, decrease in mitochondrial membrane potential, release of cytochrome c, activation of casp-3 and casp-9, and downregulation of antiapoptosis proteins XIAP and cIAP-1 [68]. Human leukemia U937 cells, when treated with sanguinarine, induced apoptosis through upregulation of Bax, induction of caspase activation, and downregulation of Bcl-2 [69]. Curcumin, the major polyphenol present in turmeric, is a potent inducer of apoptosis in cancer cells. Curcumin induces upregulation of proapoptotic proteins such as Bax, Bcl-2-interacting mediator of cell death (Bim), Bak, p53 upregulated modulator of apoptosis (Puma), and PhoRbol-12-myristate-13-acetate-induced protein 1 (Noxa) and downregulation of the antiapoptotic proteins Bcl-2 and Bcl-xL [70, 71].
Embelin was shown to enhance TRAIL-mediated apoptosis in malignant glioma cells by downregulation of the short isoform of FLICE/caspase-8 inhibitory protein [72]. Xanthohumol (XN), a chalcone, enhanced TRAIL-induced apoptosis in prostate cancer cells [73]. In human colon cancer cells, XN induced apoptosis through upregulation of casp-3, casp-8, and casp-9 activation and downregulation in Bcl-2 expression [74].
Transcription factor specificity proteins (Sp), including Sp1, Sp3, and Sp4, are known to regulate survivin and are required for survival of tumor cells. Betulinic acid, a pentacyclic triterpene, was recently shown to decrease expression of survivin and induce apoptosis in LNCaP prostate cancer cells through targeted degradation of Sp proteins [75].
Some nutraceuticals have been shown to induce apoptosis through upregulation of DRs. Oleandrin sensitized lung cancer cells to TRAIL-induced apoptosis through upregulation of DR4 and DR5 [76]. We recently showed that garcinol can sensitize human colon cancer cells to TRAIL-induced apoptosis through induction of DR4 and DR5 [77]. Capsaicin was shown to sensitize malignant glioma cells to TRAIL-mediated apoptosis via DR5 upregulation and survivin downregulation [78]. Similarly, celastrol potentiated TRAIL-induced apoptosis through downregulation of cell survival proteins and upregulation of DR4 and DR5 in human breast cancer cells [79]. Enhancement in TRAIL-induced apoptosis was recently observed in human colon cancer cells by zerumbone. This was mediated through upregulation of DR4 and DR5 and generation of ROS [80]. In another study, zerumbone triggered apoptotic events independent of functional p53 in liver cancer cells through upregulation of Bax and downregulation of Bcl-2 [81].
Insulin-like growth factor I receptor (IGFIR) has emerged as a key therapeutic target in many human malignancies, including childhood cancers such as Ewing family tumors (EFT). EGCG was found to inhibit survival of EFT through inhibition of IGFIR activity, induction of apoptosis through upregulation of Bax, and decreased expression of Bcl-2, Bcl-XL, and myeloid cell leukemia (Mcl)-1 proteins [82]. Induction of DNA damage and apoptosis in human ovarian cancer cells by genistein, a predominant isoflavone present in soybeans, was mediated through phosphorylation and activation of p53 and a decrease in the ratio of Bcl-2/Bax, Bcl-xL/Bax, and phosphorylated AKT levels [83]. Silymarin inhibited survival of hepatocellular carcinoma HepG2 cells by inducing apoptosis and facilitating cytochrome c release, upregulating proapoptotic proteins, and downregulating antiapoptotic proteins [84].
Some nutraceuticals have the potential to inhibit survival of tumor cells through mediation of the signal transducers and activators of transcription protein (STAT)-3 pathway. Muto et al. [85] showed that emodin can induce apoptosis in human myeloid cells through the elimination of Mcl-1. Emodin inhibited IL-6-induced activation of Janus-activated kinase 2 (JAK2) and phosphorylation of STAT-3; it also triggered casp-3 and casp-9 activation. Induction of apoptosis by emodin was almost abrogated in Mcl-1-overexpressing myeloma cells. These observations indicated that emodin can induce apoptosis in myeloid cells via downregulation of Mcl-1. Capsaicin has been reported to induce apoptosis in multiple myeloid cells through downregulation of STAT-3-regulated expression of Bcl-2, Bcl-xL, and survivin [86]. Adult T cell leukemia is an aggressive malignancy of peripheral T cells infected with human T cell leukemia virus type 1 (HTLV-1). Deguelin was shown to induce apoptosis in HTLV-1-transformed T cells via inhibition of survivin expression and STAT-3 phosphorylation through the ubiquitin/proteasome pathway [87]. In our laboratory, deguelin induced apoptosis in various cancer cells through the downregulation of antiapoptotic gene products [88].
Most nutraceuticals target by inhibiting NF-κB activation, thereby inhibiting NF-κB-regulated antiapoptotic proteins. Acetoxychavicol acetate inhibited cellular growth of multiple myeloma cells in vivo and in vitro through induction of apoptosis, activation of casp-8, inactivation of NF-κB, and downregulation of antiapoptotic proteins [89]. Garcinol induced apoptosis in human breast cancer MCF-7 and MDA-MB-231 cells through caspase activation and downregulation of NF-κB-regulated genes [90]. Plumbagin induced apoptosis with concomitant inactivation of Bcl-2 and the DNA binding activity of NF-κB in breast cancer cells [91]. In non-small-cell lung cancer, plumbagin induced apoptosis through mediation of c-Jun N-terminal kinase (JNK) and the casp-3 pathway [92]. In addition, Murtaza et al. [93] demonstrated that fisetin can induce apoptosis in chemoresistant human pancreatic PaC AsPC-1 cells through suppression of DR3-mediated NF-κB activation. Sulforaphane inhibited survival of orthotopically implanted PC-3 tumors through upregulation of DR4, DR5, Bax, and Bak and inhibition of NF-κB, phosphoinositide 3-kinase (PI3K)/AKT, and mitogen-activated protein kinase (MAPK)/ERK kinase (MEK) activation pathways [94].
We have identified a number of nutraceuticals from natural sources that target one or more steps in the NF-κB activation pathway to sensitize and induce apoptosis in a variety of cancer cells. The most popular among these are acetoxychavicol acetate [95], evodiamine [96], noscapine [97], indirubin [98], isodeoxyelephantopin [99], anacardic acid [52], coronarin D [100], thymoquinone [101], γ-tocotrienol [102], β-escin [103], and withanolides [104].
3.2 Regulation of tumor cell proliferation by nutraceuticals
Dysregulated proliferation is one of the major characteristics of tumorigenesis. In normal cells, proliferation is regulated by a delicate balance between growth signals and antigrowth signals. Cancer cells, however, acquire the ability to generate their own growth signals and become insensitive to antigrowth signals [1]. Their growth is controlled by cell cycle regulators at the G1/S-phase boundary, in the S phase, and during the G2/M phases of the cell cycle. A precise set of proteins called cyclins and cyclin-dependent kinases (CDKs) control the progression of cell cycle events. Whereas cyclin binding is required for CDK activity, CDK inhibitors (CKIs) such as p21 and p27 prevent CDK activity and prevent cell cycle progression. The G1-to-S-phase transition also requires cellular v-myc myelocytomatosis viral oncogene homolog (c-Myc), and inhibition of c-Myc expression leads to growth arrest [105]. Deregulated expression of c-Myc has been implicated in a number of human malignancies [106, 107]. The expression of c-Myc in turn is regulated by cdc25, a phosphatase that activates CDKs.
The well-characterized tumor suppressor p53 has been implicated in controlling the G1-to-S-phase transition and in blocking cell cycle progression at the G1 phase in response to DNA damage [108]. A number of genes controlling cell cycle progression, including the CKI p21, are transcribed in a p53-dependent manner [109, 110]. Rb is a tumor suppressor retinoblastoma protein that, like p53, functions as a negative regulator of cell growth [111]. Rb inactivation or deletion has been found in many cancers, including retinoblastomas and carcinomas of the lung, breast, bladder, and prostate. By binding to and inhibiting transcription factors such as elongation 2 factor (E2F), which are necessary for S-phase entry, Rb is believed to inhibit cell cycle progression [112]. On the other hand, phosphorylation of Rb (pRb) by CDK/cyclin complexes results in the release of active E2F species to stimulate the transcription of genes involved in DNA synthesis and S-phase progression [113-115]. COX-2, an inducible prostaglandin endoperoxide synthase 2, has been linked with tumor cell proliferation. It can be rapidly induced by growth factors, cytokines, and tumor promoters and is associated with inflammation [116-119]. Reports have demonstrated increased amounts of COX-2 in both premalignant and malignant tissues [120, 121].
Currently, a number of inhibitors based on cell cycle regulators, including nutraceuticals, are being developed as therapeutic intervention for cancer prevention. Nutraceuticals have been shown to have potential in cancer prevention for halting cell cycle progression by targeting one or more steps (Table 3) in the cell cycle. Most nutraceuticals prevent the transition of cancer cells from the G1 to S phase. Some of these nutraceuticals act through p53 and some through Rb. Acetyl-keto-beta-boswellic acid was shown to arrest colon cancer cells at the G1 phase, which was associated with decreases in cyclin-D1, cyclin-E, CDK-2, CDK-4, and pRb and an increase in p21 [122]. In Ehrlich ascites tumor cells, acetoxychavicol acetate was shown to stimulate the accumulation of tumor cells in the G1 phase of the cell cycle, which was accompanied by a decrease in pRb and an increase in Rb [123]. β-Escin, a triterpene saponin, induced cell cycle arrest at the G1/S phase by inducing p21 and reducing pRb in a p53-independent manner in HT-29 human colon cancer cells [124]. In gastric cancer cells, curcumin was shown to suppress the transition of cells from the G1 to S phase, which was accompanied by a decrease in cyclin-D1 and p21-activated kinase 1 activity [125].
Table 3.
Effect of nutraceuticals on tumor cell proliferation
| Nutraceuticals | Effect |
|---|---|
| ACA | Induced accumulation of tumor cells in the G1 phase, decreased pRb in EATC [123] |
| AKBA | Arrested colon cancer cells at the G1 phase by decreasing cyclin-D1, cyclin-E, CDK-2, CDK-4, pRb, and increasing p21 [122] |
| Anacardic acid | Downregulated NF-κB-dependent expression of cyclin-D1, COX-2, and c-Myc [52] |
| Berberine | Exhibited antiproliferative activity against human osteosarcoma cells by inducing cell cycle arrest at G1 and G2/M phase and p53-dependent upregulation of p21 [140] |
| β-Escin | Induced cell cycle arrest at the G1/S phase by inducing p21 and reducing pRb independent of p53 in HT-29 cells [124] |
| Betulinic acid | Evoked G2/M cell cycle arrest associated with a decrease in Hiwi and cyclin-B1 in human gastric adenocarcinoma cells [138] |
| Butein | Inhibited cell growth in HepG2 and Hep3B through G2/M phase arrest, phosphorylation of ATM and Chk-1/2, and reduction in cdc25c [134] |
| Capsaicin | Decreased the expression of E2F-responsive cyclin-E, thymidylate synthase, cdc25A, and cdc6 in SCLC [150] |
| Celasterol | Inhibited cell proliferation in C6 glioma cells by inducing G2/M phase arrest through upregulation of p21 and p27 and downregulation of CDK-2 [135] |
| Coronarin | Suppressed NF-κB-dependent expression of cyclin-D1, c-Myc, and COX-2 [100] |
| Curcumin | Suppressed G1/S-phase transition accompanied with a decrease in cyclin-D1 and PAK1 activity in gastric cancer cells [125] |
| Deguelin | Exhibited antiproliferative effect in breast cancer cells by arresting cells at the S phase [126] |
| Diosgenin | Inhibited proliferation through downregulation of IKK activation and expression of cyclin-D1, c-Myc, and COX-2 [145] |
| Emodin | Exhibited antiproliferative activity through p53- and p21-dependent G1-phase arrest in HepG2 cells [127] |
| Evodiamine | Arrested human thyroid ARO cancer cells at G2/M phase concomitant with a decrease in cdc2 expression [136] |
| Fisetin | Arrested LNCaP cells at G1 phase; decreased cyclin-D1, cyclin-D2, cyclin-E, CDK-2, CDK-4, and CDK-6; induced p21 and p27 [128] |
| Flavopiridol | Inhibited TNF-induced c-Myc expression through inhibition of NF-κB activation in various cancer cells [61] |
| Gambogic acid | Induced G2/M arrest in HepG2 and A549 cells through ATR/Chk-1-mediated p53/p21 activation [137] |
| Genistein | Inhibited growth of TRAMP cancer cells; repressed cyclin-B1; activated p21 through mediation of Myt-1 and Wee-1 kinases [164] |
| Gossypol | Arrested MAT-LyLu prostate cancer cells at G0/G1 phase; downregulated cyclin-D1, CDK-4, and pRb through modulation of TGF-β-1 and AKT signaling [151] |
| Guggulsterone | Suppressed proliferation of cancer cells through cell cycle arrest in S phase; downregulated cyclin-D1 and cdc2 and upregulated p21 and p27 [35] |
| Isodeoxyelephantopin | Inhibited proliferation through downregulation of NF-κB-regulated cyclin-D1, c-Myc, and COX-2 [99] |
| Morin | Suppressed NF-κB-regulated cyclin-D1 and COX-2 [146] |
| Noscapine | Inhibited proliferation of leukemic cells through suppression of NF-κB-regulated cyclin-D1 and COX-2 [97] |
| Piceatannol | Accumulated DU145 human prostate cancer cells in G1 phase; decreased expression of cyclin-A, cyclin-D1, CDK-2, and CDK-4 [129] |
| Pinitol | Suppressed NF-κB-dependent cyclin-D1 and COX-2 expression [147] |
| Quercetin | Induced cell cycle arrest at G1 phase, elevated p53, p21, and p27 in human hepatoma cell line [132] |
| Silibinin | Accumulated lung cancer cells at G1 phase; decreased activity of CDK-2 and CDK-4 [130] |
| Sulforaphane | Suppressed proliferation of EOC through G1 cell cycle arrest, reduction in pRb and free E2F-1, and upregulation in Rb [133] |
| Thymoquinone | Abrogated the progression of prostate cancer cells from G1 to S phase; upregulated p21 and p27; downregulated AR and E2F-1 [131] |
| Ursolic acid | Downregulated COX-2 and cyclin-D1 in nonspecific cell types [148] |
| Tubocapsanolide A | Induced G1 growth arrest in human lung cancer cells; inhibited binding of Rel A subunit of NF-κB to Skp2; upregulated p21 and p27 [149] |
| Zerumbone | Suppressed proliferation of leukemic NB4 cells by inducing G2/M cell cycle arrest, decreasing cyclin-B1 expression, and phosphorylating ATM/Chk-1/2 and cdc25c [139] |
ACA acetoxychavicol acetate, AKBA acetyl-11-keto-beta-boswellic acid, AKT AKT8 virus oncogene cellular homolog, AR androgen receptor, ATM ataxia telangiectasia mutated, ATR ataxia telangiectasia and Rad3-related protein, cdc25c cell division cycle 25 homolog C (S. pombe), CDK cyclin-dependent kinase, Chk checkpoint kinase, c-Myc cellular v-myc myelocytomatosis viral oncogene homolog (avian), COX-2 cyclooxygenase 2, EATC Ehrlich ascites tumor cell, E2F elongation 2 factor, EGFR epidermal growth factor receptor, ERK extracellular signal-regulated kinase, EOC epithelial ovarian cancer cells, IKK IκB kinase, JNK c-Jun N-terminal kinase, Myt-1 myelin transcription factor 1, NF-κB nuclear factor kappa B, PAK1 p21-activated kinase 1, pRb phosphorylated retinoblastoma, Rb retinoblastoma protein, SCLC small-cell lung cancer, Skp2 S-phase kinase-associated protein 2, STAT signal transducer and activator of transcription, TNF tumor necrosis factor, TGF-β transforming growth factor β, TRAMP transgenic adenocarcinoma of mouse prostate model
Deguelin exhibited an antiproliferative effect in breast cancer cells by arresting cells at the S phase [126]. Emodin showed antiproliferative activity through a p53- and p21-dependent pathway and arrested liver cancer HepG2 cells in the G1 phase [127]. Fisetin was shown to arrest prostate cancer LNCaP cells at the G1 phase, which was associated with a decrease in cyclin-D1, cyclin-D2, and cyclin-E and their activating partners CDK-2, CDK-4, and CDK-6 and with the induction of p21 and p27 [128].
The effect of piceatannol on the proliferation of DU145 human prostate cancer cells was investigated. Piceatannol caused cells to accumulate in the G1 phase and was associated with a decrease in cyclin-A, cyclin-D1, CDK-2, and CDK-4 [129]. Another nutraceutical, silibinin, caused lung cancer cells to accumulate at the G1 phase, which correlated with decreased CDK-2 and CDK-4 activities [130]. Silymarin arrested hepatocellular carcinoma HepG2 cells at the G1 phase, concomitant to a reduction in β-catenin, cyclin-D1, c-Myc, and proliferating cell nuclear antigen [84]. Thymoquinone, a component of Nigella sativa, was shown to abrogate the progression of prostate cancer cells from the G1 to S phase. These effects correlated with upregulation in p21 and p27 and downregulation in androgen receptor and E2F-1 [131]. Quercetin also induced cell cycle arrest at the G1 phase by elevating p53, p21, and p27 in a human hepatoma cell line in vitro [132]. Sulforaphane was shown to suppress proliferation of epithelial ovarian cancer cells through G1 cell cycle arrest, reduction in pRb and free E2F-1, and increase in Rb [133].
Some nutraceuticals prevent tumor cell proliferation by preventing transitions from the G2 to M phase. Butein was shown to inhibit cell growth in human hepatoma cancer cell lines—HepG2 and Hep3B—by inducing G2/M phase arrest. This inhibition in cell growth was associated with increased phosphorylation of ataxia telangiectasia mutated (ATM), checkpoint kinase (Chk)-1, and Chk-2, and reduction in cell division cycle 25 homolog c (cdc25c) levels. The inhibition in cell growth was also correlated with ROS generation and JNK activation [134]. Celasterol was shown to inhibit cell proliferation in C6 glioma cells by arresting the cells at the G2/M phase through upregulation of p21 and p27 and downregulation of CDK-2 [135]. Evodiamine exhibited antiproliferative activity by arresting human thyroid ARO cancer cells at the G2/M phase, which was associated with decreased expression of cdc2-p15 [136].
Recently, an ataxia telangiectasia and Rad3-related protein–Chk-1-mediated DNA damage response was shown to trigger p53/p21activation and G2/M arrest in HepG2 and A549 cells in response to gambogic acid treatment [137]. Betulinic acid evoked an increase in the G2/M phase population and a decrease in the S-phase population in human gastric adenocarcinoma cells. This correlated with a decrease in Hiwi and its downstream target cyclin-B1 [138]. Zerumbone was shown to suppress proliferation of leukemic NB4 cells by inducing G2/M cell cycle arrest, decreasing cyclin-B1 expression, and phosphorylating ATM/Chk-1/Chk-2 and cdc25c [139].
Berberine exhibited antiproliferative activity against human osteosarcoma cells by inducing cell cycle arrest at the G1 and G2/M phases. Whereas induction of G1 arrest was accompanied by p53-dependent upregulation of p21, G2/M arrest occurred regardless of p53 status [140]. Guggulsterone was shown to suppress the proliferation of cancer cells through inhibition of DNA synthesis and induction of cell cycle arrest in the S phase; these effects were mediated through downregulation of cyclin-D1 and cdc2 and upregulation of p21 and p27 [141].
NF-κB has been shown to bind to the promoter of genes involved in cellular proliferation. A few nutraceuticals target one or more steps in NF-κB activation to regulate tumor cell proliferation. With use of an orthotopic murine model of ovarian cancer, curcumin was shown to inhibit tumor growth that correlated with inhibition in NF-κB and a STAT-3 activation pathway [142]. In another study, curcumin exhibited antiproliferative activity in association with decreased expression of cyclin-D1 and CDK-4 in breast cancer cell lines MDA-MB-231 and BT-483 [143]. Fisetin, a naturally occurring flavonoid, was shown to downregulate COX-2 expression and to inhibit prostaglandin E2 secretion in HT29 human colon cancer cells; this correlated with decreased activity in wint signaling through downregulation of β-catenin, inhibition in epidermal growth factor receptor activity, activation of NF-κB, and subsequent decrease in cyclin-D1 expression [144].
We have identified a number of nutraceuticals with the potential to inhibit proliferation of cancer cells through inhibition of the NF-κB activation pathway and NF-κB-dependent gene products involved in proliferation such as c-Myc, COX-2, and cyclin-D1. Some of these nutraceuticals are flavopiridol [61], anacardic acid [52], coronarin D [100], diosgenin [145], isodeoxyelephantopin [99], morin [146], noscapine [97], pinitol [147], and ursolic acid [148].
S-phase kinase-associated protein 2 (Skp2), an F-box protein with an NF-κB binding site in its promoter, has been implicated in the degradation of p21 and p27. Recently, Tubocapsanolide A, a bioactive withanolide, was shown to induce G1 growth arrest in A549, H358, and H226 human lung cancer cells. The antiproliferative effects of Tubocapsanolide A were mediated through inhibition of binding of the RelA subunit of NF-κB to Skp2, inhibition of Skp2 expression, and upregulation of p21 and p27 [149].
The antiproliferative activity of capsaicin correlated with decreased expression of E2F-responsive proliferative genes such as cyclin-E, thymidylate synthase, cdc25A, and cdc6 in small-cell lung cancer [150]. Gossypol was shown to inhibit the growth of MAT-LyLu prostate cancer cells by arresting the cells at the G0/G1 phase and downregulating cyclin-D1, CDK-4, and pRb expression. These effects of gossypol were associated with modulation of transforming growth factor β-1 and AKT signaling [151].
Genistein has been shown to inhibit the growth of several cancer cells [152-157]. In breast cancer and melanoma cells, genistein induced G2/M cell cycle arrest [157, 158]. Although most studies indicated that genistein causes G2/M arrest, some showed that genistein could also arrest mouse fibroblast and melanoma cells at the G0/G1 phase of the cell cycle [159]. In addition, genistein was shown to halt cell growth by upregulating p21 in various cancer cells [160-163]. Touny and Banerjee [164] reported the involvement of upstream kinases myelin transcription factor 1 (Myt-1) and Wee-1 in the transcriptional repression of cyclin-B1 and activation of p21in prostate cancer cells. They found that genistein treatment increased Myt-1 levels and decreased Wee-1 phosphorylation, providing new insight into the possible mechanism of genistein-induced G2/M arrest.
3.3 Regulation of tumor cell invasion by nutraceuticals
Tumor cell invasion and metastasis are interrelated processes involving cell growth, cell adhesion, cell migration, and proteolytic degradation of tissue barriers such as the extracellular matrix and basement membrane. Several proteolytic enzymes, including MMPs (chiefly MMP-2 and MMP-9) [165, 166] and intercellular adhesion molecule (ICAM; chiefly ICAM-1), participate in the degradation of these barriers [167, 168]. A number of studies in lung, colon, breast, and pancreatic carcinomas have demonstrated overexpression of MMPs in malignant tissues compared with adjacent normal tissues [169-176]. Apart from MMPs, cysteine proteases [177] and serine proteases [178] such as urokinase-type plasminogen activator (u-PA) have also been involved in the invasion and metastasis of cancer cells. Since both u-PA and u-PA receptor (u-PAR) contain binding sites for NF-κB and activator protein (AP)-1 in their promoter regions [179-181], inhibition of these transcription factors will eventually result in the inhibition of u-PA–u-PAR complex and subsequent suppression of invasive behavior.
A wide variety of nutraceuticals derived from natural sources has been shown to inhibit tumor cell invasion and metastasis by targeting one or more molecules (Table 4). Allicin inhibited TNF-α-induced ICAM-1 expression in human umbilical endothelial cells (ECs) [182]. S-Allylcysteine and S-allylmercaptocysteine, obtained from garlic, suppressed the invasion ability of androgen-independent invasive prostate cancer cells [183] through restoration of E-cadherin expression. Allyl isothiocyanate (AITC) suppressed MMP-2 and MMP-9 at both protein and mRNA levels in human hepatoma SK-Hep1 cells in vitro [184]. Apigenin plays an important role in inhibiting the adhesion and motility of breast cancer cells through mediation of the HER2–HER3–PI3K–AKT pathway [185]. Apigenin inhibited metastasis of lung melanoma cells by inhibiting vascular cell adhesion molecule 1 (VCAM-1) expression in a dose-dependent manner [186].
Table 4.
Effect of nutraceuticals on tumor cell invasion
| Nutraceuticals | Effect |
|---|---|
| Allicin | Inhibited TNF-α-induced ICAM-1 expression in HUVECs [182] |
| S-Allylcysteine, | Suppressed the invasion of androgen-independent invasive PCa cells by restoration of E-cadherin expression [183] |
| AITC | Downregulated MMP-2/9 activity in human hepatoma SK-Hep1 cells [184] |
| Apigenin | Inhibited metastasis of lung melanoma cells by inhibiting VCAM-1 expression [186] |
| Berberine | Suppressed in vitro migration and invasion of human SCC-4 tongue squamous cancer cells through inhibition of FAK, IKK, NF-κB, u-PA, and MMP-2/9 [59] |
| Butein | Inhibited migration and invasion in human bladder cancer cells through the ERK-1/2 and NF-κB signaling pathways [188] |
| Caffeic acid | Inhibited MMP-9 activity in human hepatocellular carcinoma cell line [190] |
| Capsaicin | Inhibited the migration of a highly metastatic B16-F10 melanoma cells through the inhibition of the PI3K/AKT/Rac1 signaling pathway [191] |
| Carnosol | Suppressed expression and activation of MMP-9 in mouse melanoma B16-F10 cells [192] |
| β-Carotene | Inhibited the invasion of rat ascites hepatoma AH109A cells by acting as ROS quenchers [193] |
| Catechin gallate | Inhibited the invasion and migration of SK-Hep-1 human hepatocellular carcinoma cells by reducing the expression of MMP-2 and -9 [194] |
| Celastrol | Inhibited metastasis in human lung cancer 95-D and mouse melanoma B16-F10 cells through mediation of p38 MAPK and reduced phosphorylation of FAK [195] |
| Crocetin | Suppressed glycation end-product-induced ICAM-1 expression in bovine ECs [196] |
| Curcumin | Downregulated MMP-2 expression and activity and expression of integrin receptors, FAK, and MT1-MMP in Hep2 cells [198] |
| Diallyl disulfide | Inhibited MMP-2 and MMP-9 activity in HUVECs [199] |
| 3,3′-Diindolylmethane | Inhibited metastasis of breast cancer (MDA-MB-231) and ovarian cancer (BG-1) cells by lowering the level of CXCR4 and CXCL12 [200, 201] |
| EGCG | Suppressed invasion in lung carcinoma cells by preventing nuclear localization of NF-κB and downregulating MMP-9 expression [203] |
| Evodiamine | Inhibited TNF-induced invasion in human lung adenocarcinoma H1299 cells associated with inhibition in NF-κB activation and downregulation in MMP-9 expression [96] |
| Fisetin | Inhibited metastasis in human lung adenocarcinoma A549 cells through inhibition of phosphorylation of ERK-1/2 and downregulation in the expressions of MMP-2 and u-PA [204] |
| Flavopiridol | Inhibited cell invasion in MDA-MB-435 cells by inhibiting secretion of MMP-2/9 and downregulation of c-erbB-2 [206] |
| Ganoderic acid | Suppressed invasion of breast cancer cells by inhibiting AP-1 and NF-κB activity and u-PA secretion [207] |
| Genistein | Inhibited cell adhesion to vitronectin and cell migration of invasive breast cancer cells by inhibiting the transcriptional activity of AP-1 and NF-κB [208] |
| [6]-Gingerol | Suppressed expression and enzymatic activity of MMP-2/9 in human breast cancer cells [209]. |
| Indole-3-carbinol | Inhibited 17-β-estradiol-stimulated migration and invasion in MCF-7 cells associated with an increase in E-cadherin and α-, β-, and γ-catenin [210] |
| Kaempferol | Inhibited TNF-α-induced ICAM-1 expression [270] |
| Lycopene | Suppressed migration and invasion of hepatoma cell line, SK-Hep-1 by upregulating metastasis suppressor gene nm23-H1 [211] |
| Myricetin | Inhibited expression and activity of MMP-2 in colorectal cancer cells [212] |
| Piperine | Inhibited the MMP production in B16-F10 melanoma cells [213] |
| Quercetin | Decreased MMP-2 and MMP-9 expression in PC-3 cells [214] |
| Resveratrol | Inhibited HO-1-mediated NF-κB activation and MMP-9 and MMP-2 expression in A549 cells [215] |
| Sanguinarine | Inhibited invasiveness of human breast carcinoma MDA-MB-231 cells by decreasing activities of MMP-2 and MMP-9 [279] |
| Silibinin | Inhibited invasion and motility of SCC-4 tongue cancer and A459 lung cancer cells by downregulating MMP-2 and u-PA and upregulating TIMP-2 expression [216] |
| Sulforaphane | Inhibited the activation of MMPs and lung metastasis induced by melanoma cells in mice [219] |
| γ-Tocotrienol | Inhibited metastasis in gastric adenocarcinoma SGC-7901 cells that correlated with a decrease in MMP-2/9 expression and upregulation of TIMP-1 and TIMP-2 [220] |
| Ursolic acid | Downregulated MMP-9 in HT1080 human fibrosarcoma cells [280]; inhibited IL-1β or TNF-α-induced rat C6 glioma cell invasion through downregulation of NF-κB activation and MMP-9 expression [221] |
| Vanillin | Inhibited invasion and migration of cancer cells that correlated with an inhibition in MMP-9 activity [260] |
| Zerumbone | Suppressed TNF-induced tumor cell invasion associated with an inhibition in NF-κB activation and MMP-9 expression [223] |
AITC allyl isothiocyanate, AKT AKT8 virus oncogene cellular homolog, AP-1 activator protein 1, CXCL12 CXC chemokine ligand 12, CXCR4 CXC chemokine receptor 4, ECs endothelial cells, EGCG epigallocatechin-3-gallate, ERK extracellular signal-regulated kinase, FAK focal adhesion kinase, HO-1 heme oxygenase 1, HUVECs human umbilical vein endothelial cells, ICAM-1 intercellular adhesion molecule 1, IKK IκB kinase, IL-1β interleukin 1β, MAPK mitogen-activated protein kinase, MMP matrix metalloproteinase, MT1-MMP membrane-type 1 matrix metalloproteinase, NF-κB nuclear factor kappa B, PCa prostate cancer, PI3K phosphoinositide 3 kinase, ROS reactive oxygen species, TIMP-2 tissue inhibitor of metalloproteinase 2, TNF-α tumor necrosis factor α, u-PA urokinase-type plasminogen activator, VCAM-1 vascular cell adhesion molecule 1
Ezrin is highly expressed in metastatic tumors and is involved in filopodia formation as well as promotion of tumor metastasis. Berberine, an alkaloid, was recently shown to inhibit invasion and motility in nasopharyngeal carcinoma cell line 5-8F through repression of ezrin phosphorylation at Thr567 by Rho kinase and inhibition in filopodia formation [187]. Berberine has also been reported to suppress in vitro migration and invasion of human SCC-4 tongue squamous cancer cells through inhibition of FAK, IKK, NF-κB, u-PA, and MMP-2 and MMP-9 [59].
Increasing evidence has shown that epithelial–mesenchymal transition plays a critical role in tumor cell metastasis. Butein, a polyphenolic compound obtained from stem bark of cashews, was recently shown to inhibit migration and invasion through the ERK-1/ERK-2 and NF-κB signaling pathways in human bladder cancer cells. The inhibitory effect of butein was associated with the reversal of epithelial–mesenchymal transition [188]. We have shown that butein can inhibit TNF-α-induced invasion in human lung adenocarcinoma H1299 cells, which was associated with inhibition in NF-κB activation and downregulation in MMP-9 [189].
Caffeic acid had a strong inhibitory effect on MMP-9 activity in nonspecific cell types in vitro [190]. Capsaicin significantly inhibited the migration of highly metastatic B16-F10 melanoma cells through inhibition of the PI3K/AKT/rat sarcoma (Ras)-related C3 botulinum toxin substrate 1 signaling pathway [191]. Carnosol reduced MMP-9 levels in mouse melanoma cells in vitro through downregulation of NF-κB and AP-1 [192]. β-Carotene inhibited the invasion of rat ascites hepatoma AH109A cells in a dose-dependent manner by acting as ROS quenchers [193]. Catechin gallate, a phenolic compound obtained from the red pine, inhibited the invasion and migration of SK-Hep-1 human hepatocellular carcinoma cells, which strongly correlated with reduced expression of MMP-2 and MMP-9 [194]. Celastrol, a quinone methide triterpene from the medicinal plant Tripterygium wilfordii, exerted potent antimetastatic activity both in vitro and in vivo [195] through p38 MAPK, suppression of β-1 integrin ligand affinity, focal adhesion formation, reduced phosphorylation of FAK, and inhibition of cell–extracellular matrix adhesion of human lung cancer 95-D and mouse melanoma B16-F10 cells. Crocetin was shown to suppress ICAM-1 and MMPs in bovine endothelial cells [196].
Curcumin exerted a dose- and time-dependent inhibitory effect on the invasion and migration of mouse–rat hybrid retina ganglion cells (N18) in vitro [197]. This inhibited invasion was associated with downregulation of PKC, FAK, NF-κB p65, Rho A, MMP-2, and MMP-9. In Hep2 human laryngeal cancer cells, curcumin inhibited tumor cell invasion and metastasis that were associated with downregulated MMP-2 expression and reduced activity and expression of integrin receptors, FAK, and membrane-type 1 MMP [198]. Diallyl disulfide inhibited the activation of MMP-2 and MMP-9 in human umbilical vein endothelial cells (HUVECs) in vitro [199].
The chemokine receptor CXCR4, with its unique ligand CXC chemokine ligand 12 (CXCL12), is required for metastasis of breast cancer cells [200, 201]. 3, 3’-Diindolylmethane showed antimetastatic ability in MCF-7 and MDA-MB-231 breast cancer cells by lowering CXCR4 and CXCL12 levels [200, 201]. With the use of androgen-insensitive prostate cancer (DU-145) cells, Vayalil and Katiyar [202] showed that EGCG can inhibit fibroblast-conditioned medium-induced production of pro and active forms of MMP-2 and MMP-9. Nuclear localization of NF-κB, as well as MMP-9 expression and invasion, was suppressed in lung carcinoma cells treated with EGCG [203].
Takada et al. [96] recently showed that evodiamine can inhibit TNF-induced invasion in human lung adenocarcinoma H1299 cells through inhibition in NF-κB activation and downregulation in MMP-9. The antimetastatic potential of fisetin was mediated through inhibition of phosphorylation of ERK-1/ERK-2 and downregulation in expression of MMP-2 and u-PA in A549 cells [204].
c-erbB-2 is a key molecule for breast cancer metastasis, and overexpression of c-erbB-2 has been correlated with increased MMP secretion and metastatic potential in breast cancer cells [205]. Flavopiridol was found to inhibit the secretion of MMP-2 and MMP-9 in the breast cancer cells. Inhibition in MMP secretion was associated with significant downregulation of c-erbB-2 and inhibition of cell invasion [206]. Ganoderic acids isolated from Ganoderma lucidum suppressed invasive behavior of breast cancer cells by inhibiting AP-1 and NF-κB activity, resulting in inhibition of u-PA secretion [207]. Genistein inhibited cell adhesion to vitronectin and cell migration of invasive breast cancer cells by inhibiting the transcriptional activity of AP-1 and NF-κB, resulting in the suppression of u-PA secretion from cancer cells [208]. [6]-Gingerol inhibited cell adhesion, invasion, motility, and activities of MMP-2 and MMP-9 in human breast cancer cell lines in vitro [209]. Indole-3-carbinol suppressed the 17-β-estradiol-stimulated migration and invasion in estrogen-responsive MCF-7 cells. The suppressed invasion was associated with an increase in invasion suppressor molecules, E-cadherin, and α-, β-, and γ-catenin [210].
Lycopene, a dietary constituent present in tomatoes, red fruits, and vegetables, was recently shown to suppress migration and invasion of hepatoma cell line SK-Hep-1, which was associated with upregulation of a metastasis suppressor gene, nm23-H1 [211]. Myricetin inhibited MMP-2 expression and enzyme activity in colorectal carcinoma cells in vitro [212]. Piperine inhibited MMP production in melanoma cells in vitro, preventing collagen matrix invasion in a dose-dependent manner [213]. Quercetin decreased expression of MMP-2 and MMP-9 in a dose-dependent manner in PC-3 prostate cancer cells in vitro [214]. Resveratrol reduced the migratory and invasive abilities of A549 lung cancer cells and was associated with inhibition of NF-κB activation and expression of MMP-2 and MMP-9 [215]. Sanguinarine inhibited invasiveness of MDA-MB-231 human breast carcinoma cells by decreasing the activities of MMP-2 and MMP-9 [67]. Silibinin, a flavonolignan, inhibited invasion and motility of SCC-4 tongue cancer and A459 lung cancer cells by down-regulating MMP-2 and u-PA and upregulating tissue inhibitor of metalloproteinase (TIMP)-2 and PAI-1 expression [216, 217]. Recently, Lee et al. [218] reported that silibinin reduced PMA-induced invasion of MCF-7 cells through specific inhibition of AP-1-dependent MMP-9 expression. Sulforaphane inhibited the activation of MMPs, thereby inhibiting lung metastasis induced by melanoma cells in mice [219].
The invasion and metastatic capacities of SGC-7901 gastric adenocarcinoma cells and their correlation with antimetastatic mechanisms induced by γ-tocotrienol were explored. Cell attachment was decreased by the γ-tocotrienol, which was associated with decreased MMP-2 and MMP-9 expression and upregulation of TIMP-1 and TIMP-2 [220]. Ursolic acid has been reported to reduce IL-1β- or TNF-α-induced rat C6 glioma cell invasion through downregulation of NF-κB activation and MMP-9 expression [221]. Zerumbone downregulated expression of CXCR4 on HER2-overexpressing breast cancer cells in a dose- and time-dependent manner. Suppression of CXCR4 expression by zerumbone correlated with the inhibition of CXCL12-induced invasion of both breast and pancreatic cancer cells [222]. In another study, zerumbone suppressed TNF-induced NF-κB activation and NF-κB-mediated MMP-9 expression that correlated with inhibition in tumor cell invasion [223].
3.4 Regulation of tumor cell angiogenesis by nutraceuticals
Angiogenesis, the process during which new blood vessels are formed from preexisting ones, can be classified as either physiological or pathological. Physiological angiogenesis provides a driving force for organ development in ontogeny, is necessary for ovulation, and is a prerequisite for wound healing; pathological angiogenesis occurs during tumor growth at primary and metastatic sites [224]. The angiogenic cascade during tumor development consists of the release of angiogenic factors, binding of angiogenic factors to receptors on ECs, EC activation, degradation of the basement membrane by proteases, and migration and proliferation of ECs. Adhesion molecules then help to pull the sprouting blood vessels forward, and ECs are finally organized into a network of new blood vessels [225]. The signaling pathway governing tumor angiogenesis is exceedingly complex, involving various angiogenic mediators. The major signaling mediators include VEGF, platelet-derived growth factor, fibroblast growth factors (FGFs), epidermal growth factor, ephrins, angiopoietins, endothelins, integrins, cadherins, and notch [226].
Since the role of angiogenesis in tumor development was first revealed [227], a number of antiangiogenic compounds have been developed, including bevacizumab (Avastin), sunitinib (SUTENT), sorafenib (Nexavar), cediranib maleate (Recentin), and pazopanib [226]. Many nutraceuticals have shown angiogenesis-modulating properties by targeting one or more steps in the signaling pathway (Table 5).
Table 5.
Effect of nutraceuticals on tumor cell angiogenesis
| Nutraceuticals | Effect |
|---|---|
| Alliin | Inhibited FGF2 and VEGF secretion from human fibrosarcoma cells. Inhibited FGF2-induced EC tube formation and angiogenesis in a CAM model [228] |
| AITC | Exhibited potent antiangiogenic activity associated with a significant reduction in VEGF expression in a mice model bearing EAT cells [230] |
| Apigenin | Inhibited expression of HIF-1 and VEGF in cancer cells associated with a significant inhibition in tumor angiogenesis [225] |
| Caffeic acid | Suppressed STAT-3-mediated expression of HIF-1 and VEGF, inhibited vascularization and angiogenesis in mice bearing Caki-I human renal carcinoma cell line [232] |
| Capsaicin | Inhibited VEGF-induced p38 MAPK, p125 (FAK), and AKT activation, and capillary-like tube formation in human ECs [233] |
| Curcumin | Inhibited induction of VEGF synthesis in microvascular ECs through downregulation of NF-κB and AP-1 activity [234] |
| Diallyl sulfide | Reduced serum level of VEGF in B16-F10 melanoma bearing C57BL/6 mice [199] |
| EGCG | Inhibited VEGF production through inhibition of ERK-1 and ERK-2 kinases in human colon cancer cells [239] |
| Flavopiridol | Inhibited hypoxia-mediated HIF-1α expression, VEGF secretion, and tumor cell migration in human U87MG and T98G glioma cell lines [241] |
| Gambogic acid | Inhibited activation of VEGFR2, c-Src, FAK, and AKT and angiogenesis in HUVEC and human prostate cancer cells (PC3) [242] |
| Genistein | Suppressed VEGF and FGF-2 expression; inhibited tyrosine kinase and activation of NF-κB and AKT; inhibited angiogenesis in renal cell carcinoma [245] |
| [6]-Gingerol | Inhibited VEGF-induced capillary-like tube formation and sprouting in ECs in the rat aorta and new blood vessel formation in the mouse cornea [247] |
| Luteolin | Inhibited VEGF-induced survival and proliferation of HUVECs through PI3K/AKT-dependent pathways [248] |
| Perillyl alcohol | Decreased VEGF release from cancer cells and stimulated the expression of Ang2 by ECs [249] |
| Quercetin | Inhibited hypoxia-induced VEGF expression in NCI-H157 cells through suppression of STAT-3 tyrosine phosphorylation [250] |
| Resveratrol | Blocks VEGF- and FGF-receptor-mediated angiogenic responses through inhibition of MAPK phosphorylation in ECs [251] |
| Rosmarinic acid | Inhibited angiogenesis, VEGF expression, and IL-8 release in ECs [252] |
| Sanguinarine | Exhibited antiangiogenic activity through suppression of VEGF-induced proliferation and AKT activation in EC [253] |
| Silibinin | Exhibited antiangiogenic activities against human CRC HT29 xenograft growth in mice associated with downregulation of NOS, COX, HIF-1α, and VEGF expression [254] |
| Sulforaphane | Inhibited angiogenesis through activation of FOXO transcription factors and inhibition of MEK/ERK and PI3K/AKT pathways in HUVECs [256] |
| Taxol | Inhibited VEGF production in human leukemic cell lines [257]. |
| γ-Tocotrienol | Inhibited cobalt(II) chloride-induced accumulation of HIF-1α and the paracrine secretion of VEGF in human gastric adenocarcinoma SGC-7901 cell line through downregulation of ERK-1/2 pathway [258] |
| Ursolic acid | Inhibited capillary formation, reduced serum level of VEGF, NO, and proinflammatory cytokines in C57BL/6 mice bearing B16-F10 melanoma cells [259] |
| Vanillin | Suppressed HGF-induced tumor cell angiogenesis in a mouse model through inhibition of PI3K/AKT signaling and VEGF expression [260] |
AITC allyl isothiocyanate, AKT AKT8 virus oncogene cellular homolog, Ang2 angiopoietin 2, AP-1 activator protein 1, CAM chorioallantoic membrane, COX cyclooxygenase, CRC colorectal carcinoma, c-Src cellular Rous sarcoma oncogene cellular homolog, EAT Ehrlich ascites tumor, EC endothelial cell, EGCG epigallocatechin-3-gallate, ERK extracellular signal-regulated kinase, FAK focal adhesion kinase, FGF2 fibroblast growth factor 2, FOXO forkhead homeobox type O, HGF hepatocyte growth factor, HIF-1 hypoxia-inducible factor 1, HUVEC human umbilical vein endothelial cell, IL-8 interleukin 8, MAPK mitogen-activated protein kinase, MEK MAPK/ERK kinase, NF-κB nuclear factor kappa B, NO nitric oxide, NOS nitric oxide synthase, PI3K phosphoinositide 3 kinase, STAT signal transducer and activator of transcription, VEGF vascular endothelial growth factor, VEGFR2 VEGF receptor 2
Alliin showed potential to inhibit FGF-2-induced human EC tube formation and angiogenesis in a chick chorioallantoic membrane (CAM) model. Alliin also inhibited VEGF-induced angiogenesis in the CAM model [228]. In a C57BL/6 mouse model bearing B16-F10 melanoma cells, AITC inhibited NO synthesis and TNF-α production, which correlated with inhibited angiogenesis [229]. Recently, the antiangiogenic effect of AITC was investigated in Swiss albino mice into which Ehrlich ascites tumor cells were transplanted [230]. AITC significantly reduced vessel sprouting and exhibited potent antiangiogenic activity that was associated with significant reduction in VEGF expression.
Fang et al. [231] showed that apigenin can inhibit expression of hypoxia-inducible factor 1 (HIF-1) and VEGF in various types of cancer cells under normoxic and hypoxic conditions; this inhibition was associated with significant inhibition in tumor angiogenesis. In another study, caffeic acid suppressed STAT-3-mediated HIF-1 and VEGF expression, which correlated with inhibited vascularization and angiogenesis in mice bearing Caki-I human renal carcinoma cells [232].
Capsaicin has been shown to inhibit in vitro and in vivo angiogenesis. In vitro, capsaicin inhibited VEGF-induced capillary-like tube formation of primary cultured human ECs. It also inhibited VEGF-induced vessel sprouting in a rat aortic ring assay, VEGF-induced vessel formation in a mouse Matrigel plug assay, and VEGF-induced p38 MAPK, p125 (FAK), and AKT activation [233].
Curcumin was found to completely prevent induction of VEGF synthesis in microvascular ECs stimulated with glycation end products, which was mediated by downregulation of NF-κB and AP-1 activity [234]. Curcumin also inhibited angiogenesis through mediation of angiopoietins 1 and 2, HIF-1, and heme oxygenase 1 in cancer cells [235].
Diallyl sulfide reduced the serum level of VEGF in C57BL/6 mice bearing B16-F10 melanoma cells [199]. EGCG inhibited production of VEGF and IL-8 from normal human keratinocytes [236-238]. In human colon cancer cells, EGCG attenuated VEGF production through inhibition of ERK-1 and ERK-2 kinases [239]. Recently, EGCG inhibited ephrin-A1-mediated EC migration as well as tumor angiogenesis through inhibition in ERK-1/ERK-2 activation [240].
Flavopiridol decreased hypoxia-mediated HIF-1α expression, VEGF secretion, and tumor cell migration in human U87MG and T98G glioma cell lines [241]. These in vitro data were correlated with reduced vascularity of intracranial syngeneic GL261 gliomas in animals treated with flavopiridol. Gambogic acid inhibited activation of VEGF receptor 2 and of downstream kinases such as c-Src, FAK, and AKT and inhibited angiogenesis in HUVECs and human prostate cancer cells (PC3) [242]. Genistein suppressed VEGF and FGF-2 expression and inhibited tyrosine kinase phosphorylation and activation of AKT and NF-κB, resulting in inhibition of angiogenesis in renal cell carcinoma [243-246]. [6]-Gingerol, in response to VEGF, blocked capillary-like tube formation and strongly inhibited both sprouting of ECs in rat aorta and formation of new blood vessels in mouse cornea [247].
Luteolin inhibited VEGF-induced survival and proliferation of HUVECs through PI3K/AKT-dependent pathways [248]. Perillyl alcohol decreased the release of VEGF from cancer cells and stimulated expression of Ang2 by ECs, indicating that it might suppress neovascularization and induce vessel regression [249]. In another study, quercetin inhibited hypoxia-induced VEGF expression in NCI-H157 cells, which correlated with suppression in STAT-3 tyrosine phosphorylation, suggesting that inhibition of STAT-3 function may play a role in angiogenesis inhibition [250].
Resveratrol is able to suppress the growth of new blood vessels in animals. It directly inhibits capillary endothelial cell growth and blocks both VEGF- and FGF-receptor-mediated angiogenic responses through inhibition of phosphorylation of MAPK in ECs [251]. Rosmarinic acid (RA), a water-soluble polyphenolic compound, reduced the intracellular ROS level, H2O2-dependent VEGF expression, and IL-8 release of ECs. These activities were related to the antiangiogenic potential of RA [252]. Sanguinarine exhibited antiangiogenic activity by directly suppressing the proliferative effect of VEGF on ECs; this effect was mediated through downregulation of VEGF-induced AKT activation [253].
The in vivo efficacy of silibinin against human colorectal carcinoma HT29 xenograft growth in mice was investigated recently. Silibinin administration was associated with antiangiogenic activities in nude mice, resulting in downregulation of nitric oxide synthase, COX, HIF-1α, and VEGF expression [254]. In human prostate cancer cells, sulforaphane inhibited NF-κB-regulated VEGF expression in vitro [255]. In HUVECs, sulforaphane inhibited angiogenesis through activation of forkhead homeobox type O transcription factors and inhibition of MEK/ERK and PI3K/AKT pathways [256]. In human leukemic cell lines, taxol, obtained from the bark of Taxus brevifolia, showed antiangiogenic activity by inhibiting VEGF production and HIF-α expression [257]. In a human gastric adenocarcinoma SGC-7901 cell line, γ-tocotrienol inhibited cobalt(II) chloride-induced accumulation of HIF-1α and paracrine secretion of VEGF. A decrease in VEGF secretion was associated with decreased activation of ERK-1/ERK-2 [258]. The antiangiogenic activity of ursolic acid was shown recently; ursolic acid inhibited capillary formation in C57BL/6 mice bearing B16-F10 melanoma cells. Levels of serum VEGF, NO, and proinflammatory cytokines were significantly reduced in ursolic-acid-treated animals compared with those in control animals [259]. Vanillin, a food flavoring agent, suppressed hepatocyte-growth-factor-induced tumor cell angiogenesis in a mouse model that was mediated through inhibition of PI3K/AKT signaling and VEGF expression [260].
4 Summary, conclusions, and future perspective
Tumorigenesis is a multistep process regulated by multiple signaling pathways and is the target of numerous anticancer therapies. Many of the cellular pathways overlap, showing a high degree of redundancy within the system. Therefore, targeting a single molecule might ultimately have little or no effect, resulting in the need for either combination therapy or multitargeted therapy. Nutraceuticals are inexpensive, safe, and readily available and have multitargeted potential and have thus drawn considerable attention during the past decade. As this review has shown, the future of nutraceuticals as a cancer-fighting weapon seems promising. Some nutraceuticals have already progressed from the bench to the bedside either alone or in combination with existing therapy. However, greater attention is needed to clarify the following important issues.
First, several agents can inhibit as well as potentiate tumorigenesis. Numerous articles and commentaries have been published on this topic [261-266]. The fact that a given molecular component may act in opposite ways further complicates the interpretation of data. For example, although NF-κB has a negative effect on apoptosis in most situations, it may induce apoptosis under special circumstances, depending on the stimulus, cell type, and NF-κB subunit involved [261, 267, 268]. Second, although most studies have suggested that nutraceuticals kill cancer cells selectively, several studies have reported that nutraceuticals kill normal cells as well. Third, the efficacy of most nutraceuticals has been tested only in preclinical conditions, either in vitro or in vivo. Whether beneficial effects will be seen in humans is largely unknown. To date, success has been limited to a few cancers and to a few molecules. Fourth, resistance to chemoprevention is emerging, and thus a better understanding of the pathways involved in mediating tumor progression in various circumstances is necessary. Fifth, in some cases, disruption of a particular pathway can lead to pathological changes. For example, the antiangiogenic feature in resveratrol is not only limited to pathological angiogenesis but also affects physiological angiogenesis [251]. Sixth, in various cases, it is possible that the observations obtained in experimental settings were not due to the nutraceutical itself but were instead due to the intermediate formed during the process. Finally, low potency and poor bioavailability of nutraceuticals pose further challenges to scientists. Introducing synthetic analogs of nutraceuticals could be a solution for these potency and bioavailability limitations. For example, the potency of synthetic curcumin analog EF24 was shown to be approximately 10-fold greater than that of natural curcumin [269].
In light of the above facts, it is clear that we need a much better understanding of the efficacy of nutraceuticals in cancer prevention. Future studies should focus on careful and accurate characterization of nutraceuticals, better elucidation of the molecular mechanisms involved in their actions, determination of their efficacy by in vivo studies using proper animal models of cancer, and demonstration of their safety and effectiveness in clinical trials.
Acknowledgments
We thank Tamara Locke from the Department of Scientific Publications for carefully proofreading the manuscript and providing valuable comments. Dr. Aggarwal is the Ransom Horne, Jr., Professor of Cancer Research. This work was supported by a grant from the Clayton Foundation for Research (B.B.A.), a core grant from the National Institutes of Health (CA-16 672), a program project grant from National Institutes of Health (NIH CA-124787-01A2), and grant from Center for Targeted Therapy of M.D. Anderson Cancer Center.
References
- 1.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 2.Aggarwal BB, Van Kuiken ME, Iyer LH, Harikumar KB, Sung B. Molecular targets of nutraceuticals derived from dietary spices: Potential role in suppression of inflammation and tumorigenesis. Experimental Biology and Medicine (Maywood, N.J) 2009;234:825–849. doi: 10.3181/0902-MR-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270:2207–2212. [PubMed] [Google Scholar]
- 4.Reddy L, Odhav B, Bhoola KD. Natural products for cancer prevention: A global perspective. Pharmacology & Therapeutics. 2003;99:1–13. doi: 10.1016/s0163-7258(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 5.Block G, Patterson B, Subar A. Fruit, vegetables, and cancer prevention: A review of the epidemiological evidence. Nutrition and Cancer. 1992;18:1–29. doi: 10.1080/01635589209514201. [DOI] [PubMed] [Google Scholar]
- 6.Benetou V, Orfanos P, Lagiou P, Trichopoulos D, Boffetta P, Trichopoulou A. Vegetables and fruits in relation to cancer risk: Evidence from the Greek EPIC cohort study. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:387–392. doi: 10.1158/1055-9965.EPI-07-2665. [DOI] [PubMed] [Google Scholar]
- 7.Freedman ND, Park Y, Subar AF, Hollenbeck AR, Leitzmann MF, Schatzkin A, et al. Fruit and vegetable intake and head and neck cancer risk in a large United States prospective cohort study. International Journal of Cancer. 2008;122:2330–2336. doi: 10.1002/ijc.23319. [DOI] [PubMed] [Google Scholar]
- 8.Steinmetz KA, Potter JD. Vegetables, fruit, and cancer prevention: A review. Journal of the American Dietetic Association. 1996;96:1027–1039. doi: 10.1016/S0002-8223(96)00273-8. [DOI] [PubMed] [Google Scholar]
- 9.Doll R, Peto R. The causes of cancer: Quantitative estimates of avoidable risks of cancer in the United States today. Journal of the National Cancer Institute. 1981;66:1191–1308. [PubMed] [Google Scholar]
- 10.Hardy G, Hardy I, Ball PA. Nutraceuticals—A pharmaceutical viewpoint: Part II. Current Opinion in Clinical Nutrition and Metabolic Care. 2003;6:661–671. doi: 10.1097/00075197-200311000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Chan AT, Giovannucci EL. Primary prevention of colorectal cancer. Gastroenterology. 2010;138:2029.e10–2043.e10. doi: 10.1053/j.gastro.2010.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan N, Afaq F, Mukhtar H. Cancer chemoprevention through dietary antioxidants: Progress and promise. Antioxidants Redox Signaling. 2008;10:475–510. doi: 10.1089/ars.2007.1740. [DOI] [PubMed] [Google Scholar]
- 13.Syed DN, Suh Y, Afaq F, Mukhtar H. Dietary agents for chemoprevention of prostate cancer. Cancer Letters. 2008;265:167–176. doi: 10.1016/j.canlet.2008.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haseen F, Cantwell MM, O’Sullivan JM, Murray LJ. Is there a benefit from lycopene supplementation in men with prostate cancer? A systematic review. Prostate Cancer and Prostatic Diseases. 2009;12:325–332. doi: 10.1038/pcan.2009.38. [DOI] [PubMed] [Google Scholar]
- 15.Bougnoux P, Hajjaji N, Maheo K, Couet C, Chevalier S. Fatty acids and breast cancer: Sensitization to treatments and prevention of metastatic re-growth. Progress in Lipid Research. 2010;49:76–86. doi: 10.1016/j.plipres.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 16.Cranganu A, Camporeale J. Nutrition aspects of lung cancer. Nutrition in Clinical Practice. 2009;24:688–700. doi: 10.1177/0884533609352249. [DOI] [PubMed] [Google Scholar]
- 17.Goralczyk R. Beta-carotene and lung cancer in smokers: Review of hypotheses and status of research. Nutrition and Cancer. 2009;61:767–774. doi: 10.1080/01635580903285155. [DOI] [PubMed] [Google Scholar]
- 18.Bjelakovic G, Nikolova D, Simonetti RG, Gluud C. Antioxidant supplements for preventing gastrointestinal cancers. Cochrane Database of Systematic Reviews (Online) 2008:CD004183. doi: 10.1002/14651858.CD004183.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anand P, Sundaram C, Jhurani S, Kunnumakkara AB, Aggarwal BB. Curcumin and cancer: An “old-age” disease with an “age-old” solution. Cancer Letters. 2008;267:133–164. doi: 10.1016/j.canlet.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 20.Vogelstein B, Kinzler KW. Cancer genes and the pathways they control. Nature Medicine. 2004;10:789–799. doi: 10.1038/nm1087. [DOI] [PubMed] [Google Scholar]
- 21.Amin AR, Kucuk O, Khuri FR, Shin DM. Perspectives for cancer prevention with natural compounds. Journal of Clinical Oncology. 2009;27:2712–2725. doi: 10.1200/JCO.2008.20.6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez ME, Marshall JR, Giovannucci E. Diet and cancer prevention: The roles of observation and experimentation. Nature Reviews. Cancer. 2008;8:694–703. doi: 10.1038/nrc2441. [DOI] [PubMed] [Google Scholar]
- 23.Brower V. Nutraceuticals: Poised for a healthy slice of the healthcare market? Nature Biotechnology. 1998;16:728–731. doi: 10.1038/nbt0898-728. [DOI] [PubMed] [Google Scholar]
- 24.Zeisel SH. Regulation of “nutraceuticals”. Science. 1999;285:1853–1855. doi: 10.1126/science.285.5435.1853. [DOI] [PubMed] [Google Scholar]
- 25.Kalra EK. Nutraceutical–Definition and introduction. AAPS PharmSci. 2003;5:E25. doi: 10.1208/ps050325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aggarwal BB, Gehlot P. Inflammation and cancer: How friendly is the relationship for cancer patients? Current Opinion in Pharmacology. 2009;9:351–369. doi: 10.1016/j.coph.2009.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kabrun N, Enrietto PJ. The Rel family of proteins in oncogenesis and differentiation. Seminars in Cancer Biology. 1994;5:103–112. [PubMed] [Google Scholar]
- 28.Ghosh S, Karin M. Missing pieces in the NF-kappaB puzzle. Cell. 2002;109(Suppl):S81–S96. doi: 10.1016/s0092-8674(02)00703-1. [DOI] [PubMed] [Google Scholar]
- 29.Gupta SC, Sundaram C, Reuter S, Aggarwal BB. Inhibiting NF-kappaB activation by small molecules as a therapeutic strategy. Biochimica et Biophysica Acta. 2010 doi: 10.1016/j.bbagrm.2010.05.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plummer SM, Holloway KA, Manson MM, Munks RJ, Kaptein A, Farrow S, et al. Inhibition of cyclooxygenase 2 expression in colon cells by the chemopreventive agent curcumin involves inhibition of NF-kappaB activation via the NIK/IKK signalling complex. Oncogene. 1999;18:6013–6020. doi: 10.1038/sj.onc.1202980. [DOI] [PubMed] [Google Scholar]
- 31.Singh S, Aggarwal BB. Activation of transcription factor NF-kappa B is suppressed by curcumin (diferuloyl-methane) The Journal of Biological Chemistry. 1995;270:24995–25000. doi: 10.1074/jbc.270.42.24995. corrected. [DOI] [PubMed] [Google Scholar]
- 32.Bharti AC, Donato N, Singh S, Aggarwal BB. Curcumin (diferuloylmethane) down-regulates the constitutive activation of nuclear factor-kappa B and IkappaBalpha kinase in human multiple myeloma cells, leading to suppression of proliferation and induction of apoptosis. Blood. 2003;101:1053–1062. doi: 10.1182/blood-2002-05-1320. [DOI] [PubMed] [Google Scholar]
- 33.Philip S, Kundu GC. Osteopontin induces nuclear factor kappa B-mediated promatrix metalloproteinase-2 activation through I kappa B alpha/IKK signaling pathways, and curcumin (diferuloylmethane) down-regulates these pathways. The Journal of Biological Chemistry. 2003;278:14487–14497. doi: 10.1074/jbc.M207309200. [DOI] [PubMed] [Google Scholar]
- 34.Kunnumakkara AB, Diagaradjane P, Anand P, Harikumar KB, Deorukhkar A, Gelovani J, et al. Curcumin sensitizes human colorectal cancer to capecitabine by modulation of cyclin D1, COX-2, MMP-9, VEGF and CXCR4 expression in an orthotopic mouse model. International Journal of Cancer. 2009;125:2187–2197. doi: 10.1002/ijc.24593. [DOI] [PubMed] [Google Scholar]
- 35.Shishodia S, Aggarwal BB. Guggulsterone inhibits NF-kappaB and IkappaBalpha kinase activation, suppresses expression of anti-apoptotic gene products, and enhances apoptosis. The Journal of Biological Chemistry. 2004;279:47148–47158. doi: 10.1074/jbc.M408093200. [DOI] [PubMed] [Google Scholar]
- 36.Mouria M, Gukovskaya AS, Jung Y, Buechler P, Hines OJ, Reber HA, et al. Food-derived polyphenols inhibit pancreatic cancer growth through mitochondrial cytochrome C release and apoptosis. International Journal of Cancer. 2002;98:761–769. doi: 10.1002/ijc.10202. [DOI] [PubMed] [Google Scholar]
- 37.Banerjee S, Bueso-Ramos C, Aggarwal BB. Suppression of 7,12-dimethylbenz(a)anthracene-induced mammary carcinogenesis in rats by resveratrol: Role of nuclear factor-kappaB, cyclooxygenase 2, and matrix metalloprotease 9. Cancer Research. 2002;62:4945–4954. [PubMed] [Google Scholar]
- 38.Aggarwal BB, Shishodia S. Suppression of the nuclear factor-kappaB activation pathway by spice-derived phytochemicals: Reasoning for seasoning. Annals of the New York Academy of Sciences. 2004;1030:434–441. doi: 10.1196/annals.1329.054. [DOI] [PubMed] [Google Scholar]
- 39.Surh YJ, Lee SS. Capsaicin, a double-edged sword: Toxicity, metabolism, and chemopreventive potential. Life Sciences. 1995;56:1845–1855. doi: 10.1016/0024-3205(95)00159-4. [DOI] [PubMed] [Google Scholar]
- 40.Surh YJ, Lee SS. Capsaicin in hot chili pepper: Carcinogen, co-carcinogen or anticarcinogen? Food and Chemical Toxicology. 1996;34:313–316. doi: 10.1016/0278-6915(95)00108-5. [DOI] [PubMed] [Google Scholar]
- 41.Surh YJ, Lee RC, Park KK, Mayne ST, Liem A, Miller JA. Chemoprotective effects of capsaicin and diallyl sulfide against mutagenesis or tumorigenesis by vinyl carbamate and N-nitrosodimethylamine. Carcinogenesis. 1995;16:2467–2471. doi: 10.1093/carcin/16.10.2467. [DOI] [PubMed] [Google Scholar]
- 42.Surh YJ. More than spice: Capsaicin in hot chili peppers makes tumor cells commit suicide. Journal of the National Cancer Institute. 2002;94:1263–1265. doi: 10.1093/jnci/94.17.1263. [DOI] [PubMed] [Google Scholar]
- 43.Han SS, Keum YS, Seo HJ, Chun KS, Lee SS, Surh YJ. Capsaicin suppresses phorbol ester-induced activation of NF-kappaB/Rel and AP-1 transcription factors in mouse epidermis. Cancer Letters. 2001;164:119–126. doi: 10.1016/s0304-3835(01)00378-0. [DOI] [PubMed] [Google Scholar]
- 44.Natarajan K, Singh S, Burke TR, Jr, Grunberger D, Aggarwal BB. Caffeic acid phenethyl ester is a potent and specific inhibitor of activation of nuclear transcription factor NF-kappa B. Proceedings of the National Academy of Sciences of the United States of America. 1996;93:9090–9095. doi: 10.1073/pnas.93.17.9090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chaturvedi MM, Kumar A, Darnay BG, Chainy GB, Agarwal S, Aggarwal BB. Sanguinarine (pseudochelerythrine) is a potent inhibitor of NF-kappaB activation, IkappaBalpha phosphorylation, and degradation. The Journal of Biological Chemistry. 1997;272:30129–30134. doi: 10.1074/jbc.272.48.30129. [DOI] [PubMed] [Google Scholar]
- 46.Kumar A, Dhawan S, Aggarwal BB. Emodin (3-methyl-1,6,8-trihydroxyanthraquinone) inhibits TNF-induced NF-kappaB activation, IkappaB degradation, and expression of cell surface adhesion proteins in human vascular endothelial cells. Oncogene. 1998;17:913–918. doi: 10.1038/sj.onc.1201998. [DOI] [PubMed] [Google Scholar]
- 47.Jing Y, Yang J, Wang Y, Li H, Chen Y, Hu Q, et al. Alteration of subcellular redox equilibrium and the consequent oxidative modification of nuclear factor kappaB are critical for anticancer cytotoxicity by emodin, a reactive oxygen species-producing agent. Free Radical Biology & Medicine. 2006;40:2183–2197. doi: 10.1016/j.freeradbiomed.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 48.Nomura M, Ma W, Chen N, Bode AM, Dong Z. Inhibition of 12-O-tetradecanoylphorbol-13-acetate-induced NF-kappaB activation by tea polyphenols, (–)-epigallocatechin gallate and theaflavins. Carcinogenesis. 2000;21:1885–1890. doi: 10.1093/carcin/21.10.1885. [DOI] [PubMed] [Google Scholar]
- 49.Afaq F, Adhami VM, Ahmad N, Mukhtar H. Inhibition of ultraviolet B-mediated activation of nuclear factor kappaB in normal human epidermal keratinocytes by green tea constituent (–)-epigallocatechin-3-gallate. Oncogene. 2003;22:1035–1044. doi: 10.1038/sj.onc.1206206. [DOI] [PubMed] [Google Scholar]
- 50.Choi KC, Jung MG, Lee YH, Yoon JC, Kwon SH, Kang HB, et al. Epigallocatechin-3-gallate, a histone acetyltransferase inhibitor, inhibits EBV-induced B lymphocyte transformation via suppression of RelA acetylation. Cancer Research. 2009;69:583–592. doi: 10.1158/0008-5472.CAN-08-2442. [DOI] [PubMed] [Google Scholar]
- 51.Choi KC, Lee YH, Jung MG, Kwon SH, Kim MJ, Jun WJ, et al. Gallic acid suppresses lipopolysaccharide-induced nuclear factor-kappaB signaling by preventing RelA acetylation in A549 lung cancer cells. Molecular Cancer Research. 2009;7:2011–2021. doi: 10.1158/1541-7786.MCR-09-0239. [DOI] [PubMed] [Google Scholar]
- 52.Sung B, Pandey MK, Ahn KS, Yi T, Chaturvedi MM, Liu M, et al. Anacardic acid (6-nonadecyl salicylic acid), an inhibitor of histone acetyltransferase, suppresses expression of nuclear factor-kappaB-regulated gene products involved in cell survival, proliferation, invasion, and inflammation through inhibition of the inhibitory subunit of nuclear factor-kappaBalpha kinase, leading to potentiation of apoptosis. Blood. 2008;111:4880–4891. doi: 10.1182/blood-2007-10-117994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Steller H. Mechanisms and genes of cellular suicide. Science. 1995;267:1445–1449. doi: 10.1126/science.7878463. [DOI] [PubMed] [Google Scholar]
- 54.Green DR. Apoptotic pathways: Paper wraps stone blunts scissors. Cell. 2000;102:1–4. doi: 10.1016/s0092-8674(00)00003-9. [DOI] [PubMed] [Google Scholar]
- 55.Meier P, Finch A, Evan G. Apoptosis in development. Nature. 2000;407:796–801. doi: 10.1038/35037734. [DOI] [PubMed] [Google Scholar]
- 56.Wang S, Yang D, Lippman ME. Targeting Bcl-2 and Bcl-XL with nonpeptidic small-molecule antagonists. Seminars in Oncology. 2003;30:133–142. doi: 10.1053/j.seminoncol.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 57.Ambrosini G, Adida C, Altieri DC. A novel anti-apoptosis gene, survivin, expressed in cancer and lymphoma. Nature Medicine. 1997;3:917–921. doi: 10.1038/nm0897-917. [DOI] [PubMed] [Google Scholar]
- 58.Campbell CT, Prince M, Landry GM, Kha V, Kleiner HE. Pro-apoptotic effects of 1’-acetoxychavicol acetate in human breast carcinoma cells. Toxicology Letters. 2007;173:151–160. doi: 10.1016/j.toxlet.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 59.Ho YT, Lu CC, Yang JS, Chiang JH, Li TC, Ip SW, et al. Berberine induced apoptosis via promoting the expression of caspase-8, -9 and -3, apoptosis-inducing factor and endonuclease G in SCC-4 human tongue squamous carcinoma cancer cells. Anticancer Research. 2009;29:4063–4070. [PubMed] [Google Scholar]
- 60.Katiyar SK, Meeran SM, Katiyar N, Akhtar S. p53 cooperates berberine-induced growth inhibition and apoptosis of non-small cell human lung cancer cells in vitro and tumor xenograft growth in vivo. Molecular Carcinogenesis. 2009;48:24–37. doi: 10.1002/mc.20453. [DOI] [PubMed] [Google Scholar]
- 61.Takada Y, Sethi G, Sung B, Aggarwal BB. Flavopiridol suppresses tumor necrosis factor-induced activation of activator protein-1, c-Jun N-terminal kinase, p38 mitogen-activated protein kinase (MAPK), p44/p42 MAPK, and Akt, inhibits expression of antiapoptotic gene products, and enhances apoptosis through cytochrome c release and caspase activation in human myeloid cells. Molecular Pharmacology. 2008;73:1549–1557. doi: 10.1124/mol.107.041350. [DOI] [PubMed] [Google Scholar]
- 62.Gu H, Rao S, Zhao J, Wang J, Mu R, Rong J, et al. Gambogic acid reduced bcl-2 expression via p53 in human breast MCF-7 cancer cells. Journal of Cancer Research and Clinical Oncology. 2009;135:1777–1782. doi: 10.1007/s00432-009-0624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu X, Liu Y, Wang L, He J, Zhang H, Chen X, et al. Gambogic acid induces apoptosis by regulating the expression of Bax and Bcl-2 and enhancing caspase-3 activity in human malignant melanoma A375 cells. International Journal of Dermatology. 2009;48:186–192. doi: 10.1111/j.1365-4632.2009.03946.x. [DOI] [PubMed] [Google Scholar]
- 64.Liao CH, Sang S, Ho CT, Lin JK. Garcinol modulates tyrosine phosphorylation of FAK and subsequently induces apoptosis through down-regulation of Src, ERK, and Akt survival signaling in human colon cancer cells. Journal of Cellular Biochemistry. 2005;96:155–169. doi: 10.1002/jcb.20540. [DOI] [PubMed] [Google Scholar]
- 65.Choi HS, Cho MC, Lee HG, Yoon DY. Indole-3-carbinol induces apoptosis through p53 and activation of caspase-8 pathway in lung cancer A549 cells. Food and Chemical Toxicology. 2010;48:883–890. doi: 10.1016/j.fct.2009.12.028. [DOI] [PubMed] [Google Scholar]
- 66.Zhao W, Bao P, Qi H, You H. Resveratrol down-regulates survivin and induces apoptosis in human multidrug-resistant SPC-A-1/CDDP cells. Oncology Reports. 2010;23:279–286. [PubMed] [Google Scholar]
- 67.Choi WY, Jin CY, Han MH, Kim GY, Kim ND, Lee WH, et al. Sanguinarine sensitizes human gastric adenocarcinoma AGS cells to TRAIL-mediated apoptosis via down-regulation of AKT and activation of caspase-3. Anticancer Research. 2009;29:4457–4465. [PubMed] [Google Scholar]
- 68.Choi WY, Kim GY, Lee WH, Choi YH. Sanguinarine, a benzophenanthridine alkaloid, induces apoptosis in MDA-MB-231 human breast carcinoma cells through a reactive oxygen species-mediated mitochondrial pathway. Chemotherapy. 2008;54:279–287. doi: 10.1159/000149719. [DOI] [PubMed] [Google Scholar]
- 69.Han MH, Yoo YH, Choi YH. Sanguinarine-induced apoptosis in human leukemia U937 cells via Bcl-2 downregulation and caspase-3 activation. Chemotherapy. 2008;54:157–165. doi: 10.1159/000140359. [DOI] [PubMed] [Google Scholar]
- 70.Shankar S, Chen Q, Sarva K, Siddiqui I, Srivastava RK. Curcumin enhances the apoptosis-inducing potential of TRAIL in prostate cancer cells: Molecular mechanisms of apoptosis, migration and angiogenesis. Journal of Molecular Signaling. 2007;2:10. doi: 10.1186/1750-2187-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shankar S, Srivastava RK. Involvement of Bcl-2 family members, phosphatidylinositol 3’-kinase/AKT and mitochondrial p53 in curcumin (diferuloylmethane)-induced apoptosis in prostate cancer. International Journal of Oncology. 2007;30:905–918. [PubMed] [Google Scholar]
- 72.Siegelin MD, Gaiser T, Siegelin Y. The XIAP inhibitor embelin enhances TRAIL-mediated apoptosis in malignant glioma cells by down-regulation of the short isoform of FLIP. Neurochemistry International. 2009;55:423–430. doi: 10.1016/j.neuint.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 73.Szliszka E, Czuba ZP, Mazur B, Sedek L, Paradysz A, Krol W. Chalcones enhance TRAIL-induced apoptosis in prostate cancer cells. International Journal of Molecular Sciences. 2009;11:1–13. doi: 10.3390/ijms11010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pan L, Becker H, Gerhauser C. Xanthohumol induces apoptosis in cultured 40-16 human colon cancer cells by activation of the death receptor- and mitochondrial pathway. Molecular Nutrition & Food Research. 2005;49:837–843. doi: 10.1002/mnfr.200500065. [DOI] [PubMed] [Google Scholar]
- 75.Chintharlapalli S, Papineni S, Ramaiah SK, Safe S. Betulinic acid inhibits prostate cancer growth through inhibition of specificity protein transcription factors. Cancer Research. 2007;67:2816–2823. doi: 10.1158/0008-5472.CAN-06-3735. [DOI] [PubMed] [Google Scholar]
- 76.Frese S, Frese-Schaper M, Andres AC, Miescher D, Zumkehr B, Schmid RA. Cardiac glycosides initiate Apo2L/TRAIL-induced apoptosis in non-small cell lung cancer cells by up-regulation of death receptors 4 and 5. Cancer Research. 2006;66:5867–5874. doi: 10.1158/0008-5472.CAN-05-3544. [DOI] [PubMed] [Google Scholar]
- 77.Prasad S, Ravindran J, Sung B, Pandey MK, Aggarwal BB. Garcinol potentiates TRAIL-induced apoptosis through modulation of death receptors and antiapoptotic proteins. Molecular Cancer Therapeutics. 2010;9:856–868. doi: 10.1158/1535-7163.MCT-09-1113. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 78.Kim JY, Kim EH, Kim SU, Kwon TK, Choi KS. Capsaicin sensitizes malignant glioma cells to TRAIL-mediated apoptosis via DR5 upregulation and survivin downregulation. Carcinogenesis. 2010;31:367–375. doi: 10.1093/carcin/bgp298. [DOI] [PubMed] [Google Scholar]
- 79.Sung B, Park B, Yadav VR, Aggarwal BB. Celastrol, a triterpene, enhances TRAIL-induced apoptosis through the downregulation of cell survival proteins and up-regulation of death receptors. The Journal of Biological Chemistry. 2010;285:11498–11507. doi: 10.1074/jbc.M109.090209. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 80.Yodkeeree S, Sung B, Limtrakul P, Aggarwal BB. Zerumbone enhances TRAIL-induced apoptosis through the induction of death receptors in human colon cancer cells: Evidence for an essential role of reactive oxygen species. Cancer Research. 2009;69:6581–6589. doi: 10.1158/0008-5472.CAN-09-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sakinah SA, Handayani ST, Hawariah LP. Zerumbone induced apoptosis in liver cancer cells via modulation of Bax/Bcl-2 ratio. Cancer Cell International. 2007;7:4. doi: 10.1186/1475-2867-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kang HG, Jenabi JM, Liu XF, Reynolds CP, Triche TJ, Sorensen PH. Inhibition of the insulin-like growth factor I receptor by epigallocatechin gallate blocks proliferation and induces the death of Ewing tumor cells. Molecular Cancer Therapeutics. 2010;9:1396–1407. doi: 10.1158/1535-7163.MCT-09-0604. [DOI] [PubMed] [Google Scholar]
- 83.Ouyang G, Yao L, Ruan K, Song G, Mao Y, Bao S. Genistein induces G2/M cell cycle arrest and apoptosis of human ovarian cancer cells via activation of DNA damage checkpoint pathways. Cell Biology International. 2009;33:1237–1244. doi: 10.1016/j.cellbi.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 84.Ramakrishnan G, Lo Muzio L, Elinos-Baez CM, Jagan S, Augustine TA, Kamaraj S, et al. Silymarin inhibited proliferation and induced apoptosis in hepatic cancer cells. Cell Proliferation. 2009;42:229–240. doi: 10.1111/j.1365-2184.2008.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Muto A, Hori M, Sasaki Y, Saitoh A, Yasuda I, Maekawa T, et al. Emodin has a cytotoxic activity against human multiple myeloma as a Janus-activated kinase 2 inhibitor. Molecular Cancer Therapeutics. 2007;6:987–994. doi: 10.1158/1535-7163.MCT-06-0605. [DOI] [PubMed] [Google Scholar]
- 86.Bhutani M, Pathak AK, Nair AS, Kunnumakkara AB, Guha S, Sethi G, et al. Capsaicin is a novel blocker of constitutive and interleukin-6-inducible STAT3 activation. Clinical Cancer Research. 2007;13:3024–3032. doi: 10.1158/1078-0432.CCR-06-2575. [DOI] [PubMed] [Google Scholar]
- 87.Ito S, Oyake T, Murai K, Ishida Y. Deguelin suppresses cell proliferation via the inhibition of survivin expression and STAT3 phosphorylation in HTLV-1-transformed T cells. Leukemia Research. 2010;34:352–357. doi: 10.1016/j.leukres.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 88.Nair AS, Shishodia S, Ahn KS, Kunnumakkara AB, Sethi G, Aggarwal BB. Deguelin, an Akt inhibitor, suppresses IkappaBalpha kinase activation leading to suppression of NF-kappaB-regulated gene expression, potentiation of apoptosis, and inhibition of cellular invasion. Journal of Immunology. 2006;177:5612–5622. doi: 10.4049/jimmunol.177.8.5612. [DOI] [PubMed] [Google Scholar]
- 89.Ito K, Nakazato T, Murakami A, Yamato K, Miyakawa Y, Yamada T, et al. Induction of apoptosis in human myeloid leukemic cells by 1’-acetoxychavicol acetate through a mitochondrial- and Fas-mediated dual mechanism. Clinical Cancer Research. 2004;10:2120–2130. doi: 10.1158/1078-0432.ccr-1142-03. [DOI] [PubMed] [Google Scholar]
- 90.Ahmad A, Wang Z, Ali R, Maitah MY, Kong D, Banerjee S, et al. Apoptosis-inducing effect of garcinol is mediated by NF-kappaB signaling in breast cancer cells. Journal of Cellular Biochemistry. 2010;109:1134–1141. doi: 10.1002/jcb.22492. [DOI] [PubMed] [Google Scholar]
- 91.Ahmad A, Banerjee S, Wang Z, Kong D, Sarkar FH. Plumbagin-induced apoptosis of human breast cancer cells is mediated by inactivation of NF-kappaB and Bcl-2. Journal of Cellular Biochemistry. 2008;105:1461–1471. doi: 10.1002/jcb.21966. [DOI] [PubMed] [Google Scholar]
- 92.Gomathinayagam R, Sowmyalakshmi S, Mardhatillah F, Kumar R, Akbarsha MA, Damodaran C. Anticancer mechanism of plumbagin, a natural compound, on non-small cell lung cancer cells. Anticancer Research. 2008;28:785–792. [PubMed] [Google Scholar]
- 93.Murtaza I, Adhami VM, Hafeez BB, Saleem M, Mukhtar H. Fisetin, a natural flavonoid, targets chemoresistant human pancreatic cancer AsPC-1 cells through DR3-mediated inhibition of NF-kappaB. International Journal of Cancer. 2009;125:2465–2473. doi: 10.1002/ijc.24628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shankar S, Ganapathy S, Srivastava RK. Sulforaphane enhances the therapeutic potential of TRAIL in prostate cancer orthotopic model through regulation of apoptosis, metastasis, and angiogenesis. Clinical Cancer Research. 2008;14:6855–6866. doi: 10.1158/1078-0432.CCR-08-0903. [DOI] [PubMed] [Google Scholar]
- 95.Ichikawa H, Takada Y, Murakami A, Aggarwal BB. Identification of a novel blocker of I kappa B alpha kinase that enhances cellular apoptosis and inhibits cellular invasion through suppression of NF-kappa B-regulated gene products. Journal of Immunology. 2005;174:7383–7392. doi: 10.4049/jimmunol.174.11.7383. [DOI] [PubMed] [Google Scholar]
- 96.Takada Y, Kobayashi Y, Aggarwal BB. Evodiamine abolishes constitutive and inducible NF-kappaB activation by inhibiting IkappaBalpha kinase activation, thereby suppressing NF-kappaB-regulated antiapoptotic and metastatic gene expression, up-regulating apoptosis, and inhibiting invasion. The Journal of Biological Chemistry. 2005;280:17203–17212. doi: 10.1074/jbc.M500077200. [DOI] [PubMed] [Google Scholar]
- 97.Sung B, Ahn KS, Aggarwal BB. Noscapine, a benzylisoquinoline alkaloid, sensitizes leukemic cells to chemotherapeutic agents and cytokines by modulating the NF-kappaB signaling pathway. Cancer Research. 2010;70:3259–3268. doi: 10.1158/0008-5472.CAN-09-4230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sethi G, Ahn KS, Sandur SK, Lin X, Chaturvedi MM, Aggarwal BB. Indirubin enhances tumor necrosis factor-induced apoptosis through modulation of nuclear factor-kappa B signaling pathway. The Journal of Biological Chemistry. 2006;281:23425–23435. doi: 10.1074/jbc.M602627200. [DOI] [PubMed] [Google Scholar]
- 99.Ichikawa H, Nair MS, Takada Y, Sheeja DB, Kumar MA, Oommen OV, et al. Isodeoxyelephantopin, a novel sesquiterpene lactone, potentiates apoptosis, inhibits invasion, and abolishes osteoclastogenesis through suppression of nuclear factor-kappaB (nf-kappaB) activation and nf-kappaB-regulated gene expression. Clinical Cancer Research. 2006;12:5910–5918. doi: 10.1158/1078-0432.CCR-06-0916. [DOI] [PubMed] [Google Scholar]
- 100.Kunnumakkara AB, Ichikawa H, Anand P, Mohankumar CJ, Hema PS, Nair MS, et al. Coronarin D, a labdane diterpene, inhibits both constitutive and inducible nuclear factor-kappa B pathway activation, leading to potentiation of apoptosis, inhibition of invasion, and suppression of osteoclastogenesis. Molecular Cancer Therapeutics. 2008;7:3306–3317. doi: 10.1158/1535-7163.MCT-08-0432. [DOI] [PubMed] [Google Scholar]
- 101.Sethi G, Ahn KS, Aggarwal BB. Targeting nuclear factor-kappa B activation pathway by thymoquinone: role in suppression of antiapoptotic gene products and enhancement of apoptosis. Molecular Cancer Research. 2008;6:1059–1070. doi: 10.1158/1541-7786.MCR-07-2088. [DOI] [PubMed] [Google Scholar]
- 102.Ahn KS, Sethi G, Krishnan K, Aggarwal BB. Gamma-tocotrienol inhibits nuclear factor-kappaB signaling pathway through inhibition of receptor-interacting protein and TAK1 leading to suppression of antiapoptotic gene products and potentiation of apoptosis. The Journal of Biological Chemistry. 2007;282:809–820. doi: 10.1074/jbc.M610028200. [DOI] [PubMed] [Google Scholar]
- 103.Harikumar KB, Sung B, Pandey MK, Guha S, Krishnan S, Aggarwal BB. Escin, a pentacyclic triterpene, chemosensitizes human tumor cells through inhibition of nuclear factor-kappaB signaling pathway. Molecular Pharmacology. 2010;77:818–827. doi: 10.1124/mol.109.062760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ichikawa H, Takada Y, Shishodia S, Jayaprakasam B, Nair MG, Aggarwal BB. Withanolides potentiate apoptosis, inhibit invasion, and abolish osteoclastogenesis through suppression of nuclear factor-kappaB (NF-kappaB) activation and NF-kappaB-regulated gene expression. Molecular Cancer Therapeutics. 2006;5:1434–1445. doi: 10.1158/1535-7163.MCT-06-0096. [DOI] [PubMed] [Google Scholar]
- 105.Heikkila R, Schwab G, Wickstrom E, Loke SL, Pluznik DH, Watt R, et al. A c-myc antisense oligodeoxynucleotide inhibits entry into S phase but not progress from G0 to G1. Nature. 1987;328:445–449. doi: 10.1038/328445a0. [DOI] [PubMed] [Google Scholar]
- 106.Ryan KM, Birnie GD. Myc oncogenes: The enigmatic family. The Biochemical Journal. 1996;314(Pt 3):713–721. doi: 10.1042/bj3140713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Evan GI, Littlewood TD. The role of c-myc in cell growth. Current Opinion in Genetics & Development. 1993;3:44–49. doi: 10.1016/s0959-437x(05)80339-9. [DOI] [PubMed] [Google Scholar]
- 108.Kuerbitz SJ, Plunkett BS, Walsh WV, Kastan MB. Wild-type p53 is a cell cycle checkpoint determinant following irradiation. Proceedings of the National Academy of Sciences of the United States of America. 1992;89:7491–7495. doi: 10.1073/pnas.89.16.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dulic V, Kaufmann WK, Wilson SJ, Tlsty TD, Lees E, Harper JW, et al. p53-dependent inhibition of cyclin-dependent kinase activities in human fibroblasts during radiation-induced G1 arrest. Cell. 1994;76:1013–1023. doi: 10.1016/0092-8674(94)90379-4. [DOI] [PubMed] [Google Scholar]
- 110.el-Deiry WS, Tokino T, Velculescu VE, Levy DB, Parsons R, Trent JM. WAF1, a potential mediator of p53 tumor suppression. Cell. 1993;75:817–825. doi: 10.1016/0092-8674(93)90500-p. [DOI] [PubMed] [Google Scholar]
- 111.Weinberg RA. The retinoblastoma protein and cell cycle control. Cell. 1995;81:323–330. doi: 10.1016/0092-8674(95)90385-2. [DOI] [PubMed] [Google Scholar]
- 112.King KL, Cidlowski JA. Cell cycle regulation and apoptosis. Annual Review of Physiology. 1998;60:601–617. doi: 10.1146/annurev.physiol.60.1.601. [DOI] [PubMed] [Google Scholar]
- 113.Hiebert SW. Regions of the retinoblastoma gene product required for its interaction with the E2F transcription factor are necessary for E2 promoter repression and pRb-mediated growth suppression. Molecular and Cellular Biology. 1993;13:3384–3391. doi: 10.1128/mcb.13.6.3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Qian Y, Luckey C, Horton L, Esser M, Templeton DJ. Biological function of the retinoblastoma protein requires distinct domains for hyperphosphorylation and transcription factor binding. Molecular and Cellular Biology. 1992;12:5363–5372. doi: 10.1128/mcb.12.12.5363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Qin XQ, Chittenden T, Livingston DM, Kaelin WG., Jr Identification of a growth suppression domain within the retinoblastoma gene product. Genes & Development. 1992;6:953–964. doi: 10.1101/gad.6.6.953. [DOI] [PubMed] [Google Scholar]
- 116.Kujubu DA, Fletcher BS, Varnum BC, Lim RW, Herschman HR. TIS10, a phorbol ester tumor promoter-inducible mRNA from Swiss 3 T3 cells, encodes a novel prostaglandin synthase/cyclooxygenase homologue. The Journal of Biological Chemistry. 1991;266:12866–12872. [PubMed] [Google Scholar]
- 117.Maier JA, Hla T, Maciag T. Cyclooxygenase is an immediate-early gene induced by interleukin-1 in human endothelial cells. The Journal of Biological Chemistry. 1990;265:10805–10808. [PubMed] [Google Scholar]
- 118.DuBois RN, Awad J, Morrow J, Roberts LJ, 2nd, Bishop PR. Regulation of eicosanoid production and mitogenesis in rat intestinal epithelial cells by transforming growth factor-alpha and phorbol ester. Journal of Clinical Investigation. 1994;93:493–498. doi: 10.1172/JCI116998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jones DA, Carlton DP, McIntyre TM, Zimmerman GA, Prescott SM. Molecular cloning of human prostaglandin endoperoxide synthase type II and demonstration of expression in response to cytokines. The Journal of Biological Chemistry. 1993;268:9049–9054. [PubMed] [Google Scholar]
- 120.Subbaramaiah K, Dannenberg AJ. Cyclooxygenase 2: A molecular target for cancer prevention and treatment. Trends in Pharmacological Sciences. 2003;24:96–102. doi: 10.1016/S0165-6147(02)00043-3. [DOI] [PubMed] [Google Scholar]
- 121.Dannenberg AJ, Altorki NK, Boyle JO, Dang C, Howe LR, Weksler BB, et al. Cyclo-oxygenase 2: A pharmacological target for the prevention of cancer. The Lancet Oncology. 2001;2:544–551. doi: 10.1016/S1470-2045(01)00488-0. [DOI] [PubMed] [Google Scholar]
- 122.Liu JJ, Huang B, Hooi SC. Acetyl-keto-beta-boswellic acid inhibits cellular proliferation through a p21-dependent pathway in colon cancer cells. British Journal of Pharmacology. 2006;148:1099–1107. doi: 10.1038/sj.bjp.0706817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xu S, Kojima-Yuasa A, Azuma H, Huang X, Norikura T, Kennedy DO, et al. (1’S)-Acetoxychavicol acetate and its enantiomer inhibit tumor cells proliferation via different mechanisms. Chem Biol Interact. 2008;172:216–223. doi: 10.1016/j.cbi.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 124.Patlolla JM, Raju J, Swamy MV, Rao CV. Betaescin inhibits colonic aberrant crypt foci formation in rats and regulates the cell cycle growth by inducing p21(waf1/cip1) in colon cancer cells. Molecular Cancer Therapeutics. 2006;5:1459–1466. doi: 10.1158/1535-7163.MCT-05-0495. [DOI] [PubMed] [Google Scholar]
- 125.Cai XZ, Wang J, Li XD, Wang GL, Liu FN, Cheng MS, et al. Curcumin suppresses proliferation and invasion in human gastric cancer cells by downregulation of PAK1 activity and cyclin D1 expression. Cancer Biology & Therapy. 2009;8:1360–1368. doi: 10.4161/cbt.8.14.8720. [DOI] [PubMed] [Google Scholar]
- 126.Murillo G, Peng X, Torres KE, Mehta RG. Deguelin inhibits growth of breast cancer cells by modulating the expression of key members of the Wnt signaling pathway. Cancer Prevention Research (Philadelphia, PA) 2009;2:942–950. doi: 10.1158/1940-6207.CAPR-08-0232. [DOI] [PubMed] [Google Scholar]
- 127.Kuo PL, Lin TC, Lin CC. The antiproliferative activity of aloe-emodin is through p53-dependent and p21-dependent apoptotic pathway in human hepatoma cell lines. Life Sciences. 2002;71:1879–1892. doi: 10.1016/s0024-3205(02)01900-8. [DOI] [PubMed] [Google Scholar]
- 128.Khan N, Afaq F, Syed DN, Mukhtar H. Fisetin, a novel dietary flavonoid, causes apoptosis and cell cycle arrest in human prostate cancer LNCaP cells. Carcinogenesis. 2008;29:1049–1056. doi: 10.1093/carcin/bgn078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lee YM, Lim DY, Cho HJ, Seon MR, Kim JK, Lee BY, et al. Piceatannol, a natural stilbene from grapes, induces G1 cell cycle arrest in androgen-insensitive DU145 human prostate cancer cells via the inhibition of CDK activity. Cancer Letters. 2009;285:166–173. doi: 10.1016/j.canlet.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 130.Mateen S, Tyagi A, Agarwal C, Singh RP, Agarwal R. Silibinin inhibits human nonsmall cell lung cancer cell growth through cell-cycle arrest by modulating expression and function of key cell-cycle regulators. Molecular Carcinogenesis. 2010;49:247–258. doi: 10.1002/mc.20595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kaseb AO, Chinnakannu K, Chen D, Sivanandam A, Tejwani S, Menon M, et al. Androgen receptor and E2F-1 targeted thymoquinone therapy for hormone-refractory prostate cancer. Cancer Research. 2007;67:7782–7788. doi: 10.1158/0008-5472.CAN-07-1483. [DOI] [PubMed] [Google Scholar]
- 132.Hung H. Dietary quercetin inhibits proliferation of lung carcinoma cells. Forum of Nutrition. 2007;60:146–157. doi: 10.1159/000107165. [DOI] [PubMed] [Google Scholar]
- 133.Bryant CS, Kumar S, Chamala S, Shah J, Pal J, Haider M, et al. Sulforaphane induces cell cycle arrest by protecting RB-E2F-1 complex in epithelial ovarian cancer cells. Molecular Cancer. 2010;9:47. doi: 10.1186/1476-4598-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moon DO, Kim MO, Choi YH, Hyun JW, Chang WY, Kim GY. Butein induces G(2)/M phase arrest and apoptosis in human hepatoma cancer cells through ROS generation. Cancer Letters. 2010;288:204–213. doi: 10.1016/j.canlet.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 135.Ge P, Ji X, Ding Y, Wang X, Fu S, Meng F, et al. Celastrol causes apoptosis and cell cycle arrest in rat glioma cells. Neurological Research. 2010;32:94–100. doi: 10.1179/016164109X12518779082273. [DOI] [PubMed] [Google Scholar]
- 136.Chen MC, Yu CH, Wang SW, Pu HF, Kan SF, Lin LC, et al. Anti-proliferative effects of evodiamine on human thyroid cancer cell line ARO. Journal of Cellular Biochemistry. 2010;110:1495–1503. doi: 10.1002/jcb.22716. [DOI] [PubMed] [Google Scholar]
- 137.Rong JJ, Hu R, Song XM, Ha J, Lu N, Qi Q, et al. Gambogic acid triggers DNA damage signaling that induces p53/p21(Waf1/CIP1) activation through the ATR-Chk1 pathway. Cancer Letters. 2010;296:55–64. doi: 10.1016/j.canlet.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 138.Yang LJ, Chen Y, Ma Q, Fang J, He J, Cheng YQ, et al. Effect of betulinic acid on the regulation of Hiwi and cyclin B1 in human gastric adenocarcinoma AGS cells. Acta Pharmacologica Sinica. 2010;31:66–72. doi: 10.1038/aps.2009.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Xian M, Ito K, Nakazato T, Shimizu T, Chen CK, Yamato K, et al. Zerumbone, a bioactive sesquiterpene, induces G2/M cell cycle arrest and apoptosis in leukemia cells via a Fas- and mitochondria-mediated pathway. Cancer Science. 2007;98:118–126. doi: 10.1111/j.1349-7006.2006.00362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Liu Z, Liu Q, Xu B, Wu J, Guo C, Zhu F, et al. Berberine induces p53-dependent cell cycle arrest and apoptosis of human osteosarcoma cells by inflicting DNA damage. Mutation Research. 2009;662:75–83. doi: 10.1016/j.mrfmmm.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 141.Shishodia S, Sethi G, Ahn KS, Aggarwal BB. Guggulsterone inhibits tumor cell proliferation, induces S-phase arrest, and promotes apoptosis through activation of c-Jun N-terminal kinase, suppression of Akt pathway, and downregulation of antiapoptotic gene products. Biochemical Pharmacology. 2007;74:118–130. doi: 10.1016/j.bcp.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lin YG, Kunnumakkara AB, Nair A, Merritt WM, Han LY, Armaiz-Pena GN, et al. Curcumin inhibits tumor growth and angiogenesis in ovarian carcinoma by targeting the nuclear factor-kappaB pathway. Clinical Cancer Research. 2007;13:3423–3430. doi: 10.1158/1078-0432.CCR-06-3072. [DOI] [PubMed] [Google Scholar]
- 143.Liu Q, Loo WT, Sze SC, Tong Y. Curcumin inhibits cell proliferation of MDA-MB-231 and BT-483 breast cancer cells mediated by down-regulation of NFkappaB, cyclinD and MMP-1 transcription. Phytomedicine. 2009;16:916–922. doi: 10.1016/j.phymed.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 144.Suh Y, Afaq F, Johnson JJ, Mukhtar H. A plant flavonoid fisetin induces apoptosis in colon cancer cells by inhibition of COX2 and Wnt/EGFR/NF-kappaB-signaling pathways. Carcinogenesis. 2009;30:300–307. doi: 10.1093/carcin/bgn269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shishodia S, Aggarwal BB. Diosgenin inhibits osteoclastogenesis, invasion, and proliferation through the down-regulation of Akt, I kappa B kinase activation and NF-kappa B-regulated gene expression. Oncogene. 2006;25:1463–1473. doi: 10.1038/sj.onc.1209194. [DOI] [PubMed] [Google Scholar]
- 146.Manna SK, Aggarwal RS, Sethi G, Aggarwal BB, Ramesh GT. Morin (3, 5, 7, 2’, 4’-pentahydroxyflavone) abolishes nuclear factor-kappaB activation induced by various carcinogens and inflammatory stimuli, leading to suppression of nuclear factor-kappaB-regulated gene expression and up-regulation of apoptosis. Clinical Cancer Research. 2007;13:2290–2297. doi: 10.1158/1078-0432.CCR-06-2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sethi G, Ahn KS, Sung B, Aggarwal BB. Pinitol targets nuclear factor-kappaB activation pathway leading to inhibition of gene products associated with proliferation, apoptosis, invasion, and angiogenesis. Molecular Cancer Therapeutics. 2008;7:1604–1614. doi: 10.1158/1535-7163.MCT-07-2424. [DOI] [PubMed] [Google Scholar]
- 148.Shishodia S, Majumdar S, Banerjee S, Aggarwal BB. Ursolic acid inhibits nuclear factor-kappaB activation induced by carcinogenic agents through suppression of Ikappa-Balpha kinase and p65 phosphorylation: Correlation with downregulation of cyclooxygenase 2, matrix metalloproteinase 9, and cyclin D1. Cancer Research. 2003;63:4375–4383. [PubMed] [Google Scholar]
- 149.Chang HC, Chang FR, Wang YC, Pan MR, Hung WC, Wu YC. A bioactive withanolide Tubocapsanolide A inhibits proliferation of human lung cancer cells via repressing Skp2 expression. Molecular Cancer Therapeutics. 2007;6:1572–1578. doi: 10.1158/1535-7163.MCT-06-0812. [DOI] [PubMed] [Google Scholar]
- 150.Brown KC, Witte TR, Hardman WE, Luo H, Chen YC, Carpenter AB, et al. Capsaicin displays antiproliferative activity against human small cell lung cancer in cell culture and nude mice models via the E2F pathway. PloS One. 2010;5:e10243. doi: 10.1371/journal.pone.0010243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Jiang J, Ye W, Lin YC. Gossypol inhibits the growth of MAT-LyLu prostate cancer cells by modulation of TGFbeta/Akt signaling. International Journal of Molecular Medicine. 2009;24:69–75. [PubMed] [Google Scholar]
- 152.Peterson G, Barnes S. Genistein inhibits both estrogen and growth factor-stimulated proliferation of human breast cancer cells. Cell Growth & Differentiation. 1996;7:1345–1351. [PubMed] [Google Scholar]
- 153.Peterson G, Barnes S. Genistein and biochanin A inhibit the growth of human prostate cancer cells but not epidermal growth factor receptor tyrosine autophosphorylation. The Prostate. 1993;22:335–345. doi: 10.1002/pros.2990220408. [DOI] [PubMed] [Google Scholar]
- 154.Constantinou A, Kiguchi K, Huberman E. Induction of differentiation and DNA strand breakage in human HL-60 and K-562 leukemia cells by genistein. Cancer Research. 1990;50:2618–2624. [PubMed] [Google Scholar]
- 155.Buckley AR, Buckley DJ, Gout PW, Liang H, Rao YP, Blake MJ. Inhibition by genistein of prolactin-induced Nb2 lymphoma cell mitogenesis. Molecular and Cellular Endocrinology. 1993;98:17–25. doi: 10.1016/0303-7207(93)90231-8. [DOI] [PubMed] [Google Scholar]
- 156.Matsukawa Y, Marui N, Sakai T, Satomi Y, Yoshida M, Matsumoto K, et al. Genistein arrests cell cycle progression at G2-M. Cancer Research. 1993;53:1328–1331. [PubMed] [Google Scholar]
- 157.Pagliacci MC, Smacchia M, Migliorati G, Grignani F, Riccardi C, Nicoletti I. Growth-inhibitory effects of the natural phyto-oestrogen genistein in MCF-7 human breast cancer cells. European Journal of Cancer. 1994;30A:1675–1682. doi: 10.1016/0959-8049(94)00262-4. [DOI] [PubMed] [Google Scholar]
- 158.Casagrande F, Darbon JM. p21CIP1 is dispensable for the G2 arrest caused by genistein in human melanoma cells. Experimental Cell Research. 2000;258:101–108. doi: 10.1006/excr.2000.4914. [DOI] [PubMed] [Google Scholar]
- 159.Kuzumaki T, Kobayashi T, Ishikawa K. Genistein induces p21(Cip1/WAF1) expression and blocks the G1 to S phase transition in mouse fibroblast and melanoma cells. Biochemical and Biophysical Research Communications. 1998;251:291–295. doi: 10.1006/bbrc.1998.9462. [DOI] [PubMed] [Google Scholar]
- 160.Davis JN, Singh B, Bhuiyan M, Sarkar FH. Genistein-induced upregulation of p21WAF1, downregulation of cyclin B, and induction of apoptosis in prostate cancer cells. Nutrition and Cancer. 1998;32:123–131. doi: 10.1080/01635589809514730. [DOI] [PubMed] [Google Scholar]
- 161.Lian F, Bhuiyan M, Li YW, Wall N, Kraut M, Sarkar FH. Genistein-induced G2-M arrest, p21WAF1 upregulation, and apoptosis in a non-small-cell lung cancer cell line. Nutrition and Cancer. 1998;31:184–191. doi: 10.1080/01635589809514701. [DOI] [PubMed] [Google Scholar]
- 162.Li Y, Upadhyay S, Bhuiyan M, Sarkar FH. Induction of apoptosis in breast cancer cells MDA-MB-231 by genistein. Oncogene. 1999;18:3166–3172. doi: 10.1038/sj.onc.1202650. [DOI] [PubMed] [Google Scholar]
- 163.Alhasan SA, Pietrasczkiwicz H, Alonso MD, Ensley J, Sarkar FH. Genistein-induced cell cycle arrest and apoptosis in a head and neck squamous cell carcinoma cell line. Nutrition and Cancer. 1999;34:12–19. doi: 10.1207/S15327914NC340102. [DOI] [PubMed] [Google Scholar]
- 164.Touny LH, Banerjee PP. Identification of both Myt-1 and Wee-1 as necessary mediators of the p21-independent inactivation of the cdc-2/cyclin B1 complex and growth inhibition of TRAMP cancer cells by genistein. The Prostate. 2006;66:1542–1555. doi: 10.1002/pros.20495. [DOI] [PubMed] [Google Scholar]
- 165.Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annual Review of Cell and Developmental Biology. 2001;17:463–516. doi: 10.1146/annurev.cellbio.17.1.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jiang MC, Liao CF, Lee PH. Aspirin inhibits matrix metalloproteinase-2 activity, increases E-cadherin production, and inhibits in vitro invasion of tumor cells. Biochemical and Biophysical Research Communications. 2001;282:671–677. doi: 10.1006/bbrc.2001.4637. [DOI] [PubMed] [Google Scholar]
- 167.Aimes RT, Quigley JP. Matrix metalloproteinase-2 is an interstitial collagenase. Inhibitor-free enzyme catalyzes the cleavage of collagen fibrils and soluble native type I collagen generating the specific 3/4- and 1/4-length fragments. The Journal of Biological Chemistry. 1995;270:5872–5876. doi: 10.1074/jbc.270.11.5872. [DOI] [PubMed] [Google Scholar]
- 168.Kleiner DE, Jr, Stetler-Stevenson WG. Structural biochemistry and activation of matrix metalloproteases. Current Opinion in Cell Biology. 1993;5:891–897. doi: 10.1016/0955-0674(93)90040-w. [DOI] [PubMed] [Google Scholar]
- 169.Lochter A, Bissell MJ. An odyssey from breast to bone: Multi-step control of mammary metastases and osteolysis by matrix metalloproteinases. APMIS. 1999;107:128–136. doi: 10.1111/j.1699-0463.1999.tb01535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Davidson B, Goldberg I, Liokumovich P, Kopolovic J, Gotlieb WH, Lerner-Geva L, et al. Expression of metalloproteinases and their inhibitors in adenocarcinoma of the uterine cervix. International Journal of Gynecological Pathology. 1998;17:295–301. doi: 10.1097/00004347-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 171.Kugler A, Hemmerlein B, Thelen P, Kallerhoff M, Radzun HJ, Ringert RH. Expression of metalloproteinase 2 and 9 and their inhibitors in renal cell carcinoma. Journal d’Urologie. 1998;160:1914–1918. [PubMed] [Google Scholar]
- 172.Hashimoto K, Kihira Y, Matuo Y, Usui T. Expression of matrix metalloproteinase-7 and tissue inhibitor of metalloproteinase-1 in human prostate. Journal d’Urologie. 1998;160:1872–1876. [PubMed] [Google Scholar]
- 173.Sutinen M, Kainulainen T, Hurskainen T, Vesterlund E, Alexander JP, Overall CM, et al. Expression of matrix metalloproteinases (MMP-1 and -2) and their inhibitors (TIMP-1, -2 and -3) in oral lichen planus, dysplasia, squamous cell carcinoma and lymph node metastasis. British Journal of Cancer. 1998;77:2239–2245. doi: 10.1038/bjc.1998.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Gonzalez-Avila G, Iturria C, Vadillo F, Teran L, Selman M, Perez-Tamayo R. 72-kD (MMP-2) and 92-kD (MMP-9) type IV collagenase production and activity in different histologic types of lung cancer cells. Pathobiology. 1998;66:5–16. doi: 10.1159/000027989. [DOI] [PubMed] [Google Scholar]
- 175.Nawrocki B, Polette M, Marchand V, Monteau M, Gillery P, Tournier JM, et al. Expression of matrix metalloproteinases and their inhibitors in human bronchopulmonary carcinomas: Quantificative and morphological analyses. International Journal of Cancer. 1997;72:556–564. doi: 10.1002/(sici)1097-0215(19970807)72:4<556::aid-ijc2>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 176.Bramhall SR. The matrix metalloproteinases and their inhibitors in pancreatic cancer. From molecular science to a clinical application. International Journal of Pancreatology. 1997;21:1–12. doi: 10.1007/BF02785914. [DOI] [PubMed] [Google Scholar]
- 177.Chapman HA, Riese RJ, Shi GP. Emerging roles for cysteine proteases in human biology. Annual Review of Physiology. 1997;59:63–88. doi: 10.1146/annurev.physiol.59.1.63. [DOI] [PubMed] [Google Scholar]
- 178.Andreasen PA, Kjoller L, Christensen L, Duffy MJ. The urokinase-type plasminogen activator system in cancer metastasis: A review. International Journal of Cancer. 1997;72:1–22. doi: 10.1002/(sici)1097-0215(19970703)72:1<1::aid-ijc1>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 179.Nerlov C, Rorth P, Blasi F, Johnsen M. Essential AP-1 and PEA3 binding elements in the human urokinase enhancer display cell type-specific activity. Oncogene. 1991;6:1583–1592. [PubMed] [Google Scholar]
- 180.Lengyel E, Gum R, Stepp E, Juarez J, Wang H, Boyd D. Regulation of urokinase-type plasminogen activator expression by an ERK1-dependent signaling pathway in a squamous cell carcinoma cell line. Journal of Cellular Biochemistry. 1996;61:430–443. doi: 10.1002/(sici)1097-4644(19960601)61:3<430::aid-jcb10>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 181.Wang Y. The role and regulation of urokinase-type plasminogen activator receptor gene expression in cancer invasion and metastasis. Medicinal Research Reviews. 2001;21:146–170. doi: 10.1002/1098-1128(200103)21:2<146::aid-med1004>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 182.Mo SJ, Son EW, Rhee DK, Pyo S. Modulation of TNF-alpha-induced ICAM-1 expression, NO and H2O2 production by alginate, allicin and ascorbic acid in human endothelial cells. Archives of Pharmacal Research. 2003;26:244–251. doi: 10.1007/BF02976837. [DOI] [PubMed] [Google Scholar]
- 183.Chu Q, Ling MT, Feng H, Cheung HW, Tsao SW, Wang X, et al. A novel anticancer effect of garlic derivatives: Inhibition of cancer cell invasion through restoration of E-cadherin expression. Carcinogenesis. 2006;27:2180–2189. doi: 10.1093/carcin/bgl054. [DOI] [PubMed] [Google Scholar]
- 184.Hwang ES, Lee HJ. Allyl isothiocyanate and its N-acetylcysteine conjugate suppress metastasis via inhibition of invasion, migration, and matrix metalloproteinase-2/-9 activities in SK-Hep 1 human hepatoma cells. Experimental Biology and Medicine (Maywood, NJ) 2006;231:421–430. doi: 10.1177/153537020623100408. [DOI] [PubMed] [Google Scholar]
- 185.Way TD, Lin JK. Role of HER2/HER3 co-receptor in breast carcinogenesis. Future Oncology. 2005;1:841–849. doi: 10.2217/14796694.1.6.841. [DOI] [PubMed] [Google Scholar]
- 186.Piantelli M, Rossi C, Iezzi M, La Sorda R, Iacobelli S, Alberti S, et al. Flavonoids inhibit melanoma lung metastasis by impairing tumor cells endothelium interactions. Journal of Cellular Physiology. 2006;207:23–29. doi: 10.1002/jcp.20510. [DOI] [PubMed] [Google Scholar]
- 187.Tang F, Wang D, Duan C, Huang D, Wu Y, Chen Y, et al. Berberine inhibits metastasis of nasopharyngeal carcinoma 5-8F cells by targeting Rho kinase-mediated Ezrin phosphorylation at threonine 567. The Journal of Biological Chemistry. 2009;284:27456–27466. doi: 10.1074/jbc.M109.033795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zhang L, Chen W, Li X. A novel anticancer effect of butein: Inhibition of invasion through the ERK1/2 and NF-kappa B signaling pathways in bladder cancer cells. FEBS Letters. 2008;582:1821–1828. doi: 10.1016/j.febslet.2008.04.046. [DOI] [PubMed] [Google Scholar]
- 189.Pandey MK, Sandur SK, Sung B, Sethi G, Kunnumakkara AB, Aggarwal BB. Butein, a tetrahydroxychalcone, inhibits nuclear factor (NF)-kappaB and NF-kappaB-regulated gene expression through direct inhibition of Ikappa-Balpha kinase beta on cysteine 179 residue. The Journal of Biological Chemistry. 2007;282:17340–17350. doi: 10.1074/jbc.M700890200. [DOI] [PubMed] [Google Scholar]
- 190.Park WH, Kim SH, Kim CH. A new matrix metalloproteinase-9 inhibitor 3,4-dihydroxycinnamic acid (caf-feic acid) from methanol extract of Euonymus alatus: Isolation and structure determination. Toxicology. 2005;207:383–390. doi: 10.1016/j.tox.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 191.Shin DH, Kim OH, Jun HS, Kang MK. Inhibitory effect of capsaicin on B16-F10 melanoma cell migration via the phosphatidylinositol 3-kinase/Akt/Rac1 signal pathway. Experimental & Molecular Medicine. 2008;40:486–494. doi: 10.3858/emm.2008.40.5.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Huang SC, Ho CT, Lin-Shiau SY, Lin JK. Carnosol inhibits the invasion of B16/F10 mouse melanoma cells by suppressing metalloproteinase-9 through down-regulating nuclear factor-kappa B and c-Jun. Biochemical Pharmacology. 2005;69:221–232. doi: 10.1016/j.bcp.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 193.Kozuki Y, Miura Y, Yagasaki K. Inhibitory effects of carotenoids on the invasion of rat ascites hepatoma cells in culture. Cancer Letters. 2000;151:111–115. doi: 10.1016/s0304-3835(99)00418-8. [DOI] [PubMed] [Google Scholar]
- 194.Lee SJ, Lee KW, Hur HJ, Chun JY, Kim SY, Lee HJ. Phenolic phytochemicals derived from red pine (Pinus densiflora) inhibit the invasion and migration of SK-Hep-1 human hepatocellular carcinoma cells. Annals of the New York Academy of Sciences. 2007;1095:536–544. doi: 10.1196/annals.1397.058. [DOI] [PubMed] [Google Scholar]
- 195.Zhu H, Liu XW, Cai TY, Cao J, Tu CX, Lu W, et al. Celastrol acts as a potent anti-metastatic agent targeting {beta}1 integrin and inhibiting cell–ECM adhesion, partially via the p38 MAPK pathway. Journal of Pharmacology and Experimental Therapeutics. 2010;334:489–499. doi: 10.1124/jpet.110.165654. [DOI] [PubMed] [Google Scholar]
- 196.Xiang M, Qian ZY, Zhou CH, Liu J, Li WN. Crocetin inhibits leukocyte adherence to vascular endothelial cells induced by AGEs. Journal of Ethnopharmacology. 2006;107:25–31. doi: 10.1016/j.jep.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 197.Lin HJ, Su CC, Lu HF, Yang JS, Hsu SC, Ip SW, et al. Curcumin blocks migration and invasion of mouse-rat hybrid retina ganglion cells (N18) through the inhibition of MMP-2, -9, FAK, Rho A and Rock-1 gene expression. Oncology Reports. 2010;23:665–670. [PubMed] [Google Scholar]
- 198.Mitra A, Chakrabarti J, Banerji A, Chatterjee A, Das BR. Curcumin, a potential inhibitor of MMP-2 in human laryngeal squamous carcinoma cells HEp2. Journal of Environmental Pathology, Toxicology and Oncology. 2006;25:679–690. doi: 10.1615/jenvironpatholtoxicoloncol.v25.i4.70. [DOI] [PubMed] [Google Scholar]
- 199.Thejass P, Kuttan G. Antiangiogenic activity of diallyl sulfide (DAS) International Immunopharmacology. 2007;7:295–305. doi: 10.1016/j.intimp.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 200.Hsu EL, Chen N, Westbrook A, Wang F, Zhang R, Taylor RT, et al. CXCR4 and CXCL12 downregulation: A novel mechanism for the chemoprotection of 3,3′-diindolylmethane for breast and ovarian cancers. Cancer Letters. 2008;265:113–123. doi: 10.1016/j.canlet.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 201.Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 202.Vayalil PK, Katiyar SK. Treatment of epigallocatechin-3-gallate inhibits matrix metalloproteinases-2 and -9 via inhibition of activation of mitogen-activated protein kinases, c-jun and NF-kappaB in human prostate carcinoma DU-145 cells. The Prostate. 2004;59:33–42. doi: 10.1002/pros.10352. [DOI] [PubMed] [Google Scholar]
- 203.Yang J, Wei D, Liu J. Repressions of MMP-9 expression and NF-kappa B localization are involved in inhibition of lung carcinoma 95-D cell invasion by (–)epigallocatechin-3-gallate. Biomedicine & Pharmacotherapy. 2005;59:98–103. doi: 10.1016/j.biopha.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 204.Liao YC, Shih YW, Chao CH, Lee XY, Chiang TA. Involvement of the ERK signaling pathway in fisetin reduces invasion and migration in the human lung cancer cell line A549. Journal of Agricultural and Food Chemistry. 2009;57:8933–8941. doi: 10.1021/jf902630w. [DOI] [PubMed] [Google Scholar]
- 205.Tan M, Yao J, Yu D. Overexpression of the c-erbB-2 gene enhanced intrinsic metastasis potential in human breast cancer cells without increasing their transformation abilities. Cancer Research. 1997;57:1199–1205. [PubMed] [Google Scholar]
- 206.Li Y, Bhuiyan M, Alhasan S, Senderowicz AM, Sarkar FH. Induction of apoptosis and inhibition of c-erbB-2 in breast cancer cells by flavopiridol. Clinical Cancer Research. 2000;6:223–229. [PubMed] [Google Scholar]
- 207.Jiang J, Grieb B, Thyagarajan A, Sliva D. Ganoderic acids suppress growth and invasive behavior of breast cancer cells by modulating AP-1 and NF-kappaB signaling. International Journal of Molecular Medicine. 2008;21:577–584. [PubMed] [Google Scholar]
- 208.Valachovicova T, Slivova V, Bergman H, Shuherk J, Sliva D. Soy isoflavones suppress invasiveness of breast cancer cells by the inhibition of NF-kappaB/AP-1-dependent and -independent pathways. International Journal of Oncology. 2004;25:1389–1395. [PubMed] [Google Scholar]
- 209.Lee HS, Seo EY, Kang NE, Kim WK. [6]-Gingerol inhibits metastasis of MDA-MB-231 human breast cancer cells. The Journal of Nutritional Biochemistry. 2008;19:313–319. doi: 10.1016/j.jnutbio.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 210.Meng Q, Qi M, Chen DZ, Yuan R, Goldberg ID, Rosen EM, et al. Suppression of breast cancer invasion and migration by indole-3-carbinol: Associated with up-regulation of BRCA1 and E-cadherin/catenin complexes. Journal of Molecular Medicine. 2000;78:155–165. doi: 10.1007/s001090000088. [DOI] [PubMed] [Google Scholar]
- 211.Huang CS, Shih MK, Chuang CH, Hu ML. Lycopene inhibits cell migration and invasion and upregulates Nm23-H1 in a highly invasive hepatocarcinoma, SK-Hep-1 cells. The Journal of Nutrition. 2005;135:2119–2123. doi: 10.1093/jn/135.9.2119. [DOI] [PubMed] [Google Scholar]
- 212.Ko CH, Shen SC, Lee TJ, Chen YC. Myricetin inhibits matrix metalloproteinase 2 protein expression and enzyme activity in colorectal carcinoma cells. Molecular Cancer Therapeutics. 2005;4:281–290. [PubMed] [Google Scholar]
- 213.Pradeep CR, Kuttan G. Piperine is a potent inhibitor of nuclear factor-kappaB (NF-kappaB), c-Fos, CREB, ATF-2 and proinflammatory cytokine gene expression in B16F-10 melanoma cells. International Immunopharmacology. 2004;4:1795–1803. doi: 10.1016/j.intimp.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 214.Vijayababu MR, Arunkumar A, Kanagaraj P, Venkataraman P, Krishnamoorthy G, Arunakaran J. Quercetin downregulates matrix metalloproteinases 2 and 9 proteins expression in prostate cancer cells (PC-3) Molecular and Cellular Biochemistry. 2006;287:109–116. doi: 10.1007/s11010-005-9085-3. [DOI] [PubMed] [Google Scholar]
- 215.Liu PL, Tsai JR, Charles AL, Hwang JJ, Chou SH, Ping YH, et al. Resveratrol inhibits human lung adenocarcinoma cell metastasis by suppressing heme oxygenase 1-mediated nuclear factor-kappaB pathway and subsequently downregulating expression of matrix metalloproteinases. Molecular Nutrition and Food Research. 2010;54:S196–S204. doi: 10.1002/mnfr.200900550. [DOI] [PubMed] [Google Scholar]
- 216.Chen PN, Hsieh YS, Chiang CL, Chiou HL, Yang SF, Chu SC. Silibinin inhibits invasion of oral cancer cells by suppressing the MAPK pathway. Journal of Dental Research. 2006;85:220–225. doi: 10.1177/154405910608500303. [DOI] [PubMed] [Google Scholar]
- 217.Chu SC, Chiou HL, Chen PN, Yang SF, Hsieh YS. Silibinin inhibits the invasion of human lung cancer cells via decreased productions of urokinase-plasminogen activator and matrix metalloproteinase-2. Molecular Carcinogenesis. 2004;40:143–149. doi: 10.1002/mc.20018. [DOI] [PubMed] [Google Scholar]
- 218.Lee SO, Jeong YJ, Im HG, Kim CH, Chang YC, Lee IS. Silibinin suppresses PMA-induced MMP-9 expression by blocking the AP-1 activation via MAPK signaling pathways in MCF-7 human breast carcinoma cells. Biochemical and Biophysical Research Communications. 2007;354:165–171. doi: 10.1016/j.bbrc.2006.12.181. [DOI] [PubMed] [Google Scholar]
- 219.Thejass P, Kuttan G. Antimetastatic activity of sulforaphane. Life Sciences. 2006;78:3043–3050. doi: 10.1016/j.lfs.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 220.Liu HK, Wang Q, Li Y, Sun WG, Liu JR, Yang YM, et al. Inhibitory effects of gamma-tocotrienol on invasion and metastasis of human gastric adenocarcinoma SGC-7901 cells. The Journal of Nutritional Biochemistry. 2010;21:206–213. doi: 10.1016/j.jnutbio.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 221.Huang HC, Huang CY, Lin-Shiau SY, Lin JK. Ursolic acid inhibits IL-1beta or TNF-alpha-induced C6 glioma invasion through suppressing the association ZIP/p62 with PKC-zeta and downregulating the MMP-9 expression. Molecular Carcinogenesis. 2009;48:517–531. doi: 10.1002/mc.20490. [DOI] [PubMed] [Google Scholar]
- 222.Sung B, Jhurani S, Ahn KS, Mastuo Y, Yi T, Guha S, et al. Zerumbone down-regulates chemokine receptor CXCR4 expression leading to inhibition of CXCL12-induced invasion of breast and pancreatic tumor cells. Cancer Research. 2008;68:8938–8944. doi: 10.1158/0008-5472.CAN-08-2155. [DOI] [PubMed] [Google Scholar]
- 223.Takada Y, Murakami A, Aggarwal BB. Zerumbone abolishes NF-kappaB and IkappaBalpha kinase activation leading to suppression of antiapoptotic and metastatic gene expression, upregulation of apoptosis, and downregulation of invasion. Oncogene. 2005;24:6957–6969. doi: 10.1038/sj.onc.1208845. [DOI] [PubMed] [Google Scholar]
- 224.Folkman J. Angiogenesis: An organizing principle for drug discovery? Nature Reviews. Drug Discovery. 2007;6:273–286. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 225.Fan TP, Yeh JC, Leung KW, Yue PY, Wong RN. Angiogenesis: From plants to blood vessels. Trends in Pharmacological Sciences. 2006;27:297–309. doi: 10.1016/j.tips.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 226.Gordon MS, Mendelson DS, Kato G. Tumor angiogenesis and novel antiangiogenic strategies. International Journal of Cancer. 2010;126:1777–1787. doi: 10.1002/ijc.25026. [DOI] [PubMed] [Google Scholar]
- 227.Folkman J. Tumor angiogenesis: Therapeutic implications. The New England Journal of Medicine. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 228.Mousa AS, Mousa SA. Anti-angiogenesis efficacy of the garlic ingredient alliin and antioxidants: Role of nitric oxide and p53. Nutrition and Cancer. 2005;53:104–110. doi: 10.1207/s15327914nc5301_12. [DOI] [PubMed] [Google Scholar]
- 229.Thejass P, Kuttan G. Allyl isothiocyanate (AITC) and phenyl isothiocyanate (PITC) inhibit tumour-specific angiogenesis by downregulating nitric oxide (NO) and tumour necrosis factor-alpha (TNF-alpha) production. Nitric Oxide. 2007;16:247–257. doi: 10.1016/j.niox.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 230.Kumar A, D’Souza SS, Tickoo S, Salimath BP, Singh HB. Antiangiogenic and proapoptotic activities of allyl isothiocyanate inhibit ascites tumor growth in vivo. Integrative Cancer Therapies. 2009;8:75–87. doi: 10.1177/1534735408330716. [DOI] [PubMed] [Google Scholar]
- 231.Fang J, Zhou Q, Liu LZ, Xia C, Hu X, Shi X, et al. Apigenin inhibits tumor angiogenesis through decreasing HIF-1alpha and VEGF expression. Carcinogenesis. 2007;28:858–864. doi: 10.1093/carcin/bgl205. [DOI] [PubMed] [Google Scholar]
- 232.Jung JE, Kim HS, Lee CS, Park DH, Kim YN, Lee MJ, et al. Caffeic acid and its synthetic derivative CADPE suppress tumor angiogenesis by blocking STAT3-mediated VEGF expression in human renal carcinoma cells. Carcinogenesis. 2007;28:1780–1787. doi: 10.1093/carcin/bgm130. [DOI] [PubMed] [Google Scholar]
- 233.Min JK, Han KY, Kim EC, Kim YM, Lee SW, Kim OH, et al. Capsaicin inhibits in vitro and in vivo angiogenesis. Cancer Research. 2004;64:644–651. doi: 10.1158/0008-5472.can-03-3250. [DOI] [PubMed] [Google Scholar]
- 234.Okamoto T, Yamagishi S, Inagaki Y, Amano S, Koga K, Abe R, et al. Angiogenesis induced by advanced glycation end products and its prevention by cerivastatin. The FASEB Journal. 2002;16:1928–1930. doi: 10.1096/fj.02-0030fje. [DOI] [PubMed] [Google Scholar]
- 235.Conney AH. Enzyme induction and dietary chemicals as approaches to cancer chemoprevention: The Seventh DeWitt S. Goodman Lecture. Cancer research. 2003;63:7005–7031. [PubMed] [Google Scholar]
- 236.Sartippour MR, Heber D, Henning S, Elashoff D, Elashoff R, Rubio R, et al. cDNA microarray analysis of endothelial cells in response to green tea reveals a suppressive phenotype. International Journal of Oncology. 2004;25:193–202. [PubMed] [Google Scholar]
- 237.Sartippour MR, Heber D, Zhang L, Beatty P, Elashoff D, Elashoff R, et al. Inhibition of fibroblast growth factors by green tea. International Journal of Oncology. 2002;21:487–491. [PubMed] [Google Scholar]
- 238.Trompezinski S, Denis A, Schmitt D, Viac J. Comparative effects of polyphenols from green tea (EGCG) and soybean (genistein) on VEGF and IL-8 release from normal human keratinocytes stimulated with the proinflammatory cytokine TNFalpha. Archives for Dermatological Research. 2003;295:112–116. doi: 10.1007/s00403-003-0402-y. [DOI] [PubMed] [Google Scholar]
- 239.Jung YD, Kim MS, Shin BA, Chay KO, Ahn BW, Liu W, et al. EGCG, a major component of green tea, inhibits tumour growth by inhibiting VEGF induction in human colon carcinoma cells. British Journal of Cancer. 2001;84:844–850. doi: 10.1054/bjoc.2000.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Tang FY, Chiang EP, Shih CJ. Green tea catechin inhibits ephrin-A1-mediated cell migration and angiogenesis of human umbilical vein endothelial cells. The Journal of Nutritional Biochemistry. 2007;18:391–399. doi: 10.1016/j.jnutbio.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 241.Newcomb EW, Ali MA, Schnee T, Lan L, Lukyanov Y, Fowkes M, et al. Flavopiridol downregulates hypoxia-mediated hypoxia-inducible factor-1alpha expression in human glioma cells by a proteasome-independent pathway: Implications for in vivo therapy. Neuro Oncol. 2005;7:225–235. doi: 10.1215/S1152851704000997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Yi T, Yi Z, Cho SG, Luo J, Pandey MK, Aggarwal BB, et al. Gambogic acid inhibits angiogenesis and prostate tumor growth by suppressing vascular endothelial growth factor receptor 2 signaling. Cancer Research. 2008;68:1843–1850. doi: 10.1158/0008-5472.CAN-07-5944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Sasamura H, Takahashi A, Miyao N, Yanase M, Masumori N, Kitamura H, et al. Inhibitory effect on expression of angiogenic factors by antiangiogenic agents in renal cell carcinoma. British Journal of Cancer. 2002;86:768–773. doi: 10.1038/sj.bjc.6600152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Sarkar FH, Li Y. Soy isoflavones and cancer prevention. Cancer Invest. 2003;21:744–757. doi: 10.1081/cnv-120023773. [DOI] [PubMed] [Google Scholar]
- 245.Ruiz PA, Haller D. Functional diversity of flavonoids in the inhibition of the proinflammatory NF-kappaB, IRF, and Akt signaling pathways in murine intestinal epithelial cells. The Journal of Nutrition. 2006;136:664–671. doi: 10.1093/jn/136.3.664. [DOI] [PubMed] [Google Scholar]
- 246.Gille J. Antiangiogenic cancer therapies get their act together: Current developments and future prospects of growth factor- and growth factor receptor-targeted approaches. Experimental Dermatology. 2006;15:175–186. doi: 10.1111/j.1600-0625.2006.00400.x. [DOI] [PubMed] [Google Scholar]
- 247.Kim EC, Min JK, Kim TY, Lee SJ, Yang HO, Han S, et al. [6]-Gingerol, a pungent ingredient of ginger, inhibits angiogenesis in vitro and in vivo. Biochemical and Biophysical Research Communications. 2005;335:300–308. doi: 10.1016/j.bbrc.2005.07.076. [DOI] [PubMed] [Google Scholar]
- 248.Bagli E, Stefaniotou M, Morbidelli L, Ziche M, Psillas K, Murphy C, et al. Luteolin inhibits vascular endothelial growth factor-induced angiogenesis; Inhibition of endothelial cell survival and proliferation by targeting phosphatidylinositol 3′-kinase activity. Cancer Research. 2004;64:7936–7946. doi: 10.1158/0008-5472.CAN-03-3104. [DOI] [PubMed] [Google Scholar]
- 249.Loutrari H, Hatziapostolou M, Skouridou V, Papadimitriou E, Roussos C, Kolisis FN, et al. Perillyl alcohol is an angiogenesis inhibitor. The Journal of Pharmacology and Experimental Therapeutics. 2004;311:568–575. doi: 10.1124/jpet.104.070516. [DOI] [PubMed] [Google Scholar]
- 250.Anso E, Zuazo A, Irigoyen M, Urdaci MC, Rouzaut A, Martinez-Irujo JJ. Flavonoids inhibit hypoxia-induced vascular endothelial growth factor expression by a HIF-1 independent mechanism. Biochemical Pharmacology. 2010;79:1600–1609. doi: 10.1016/j.bcp.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 251.Brakenhielm E, Cao R, Cao Y. Suppression of angiogenesis, tumor growth, and wound healing by resveratrol, a natural compound in red wine and grapes. The FASEB Journal. 2001;15:1798–1800. doi: 10.1096/fj.01-0028fje. [DOI] [PubMed] [Google Scholar]
- 252.Huang SS, Zheng RL. Rosmarinic acid inhibits angiogenesis and its mechanism of action in vitro. Cancer Letters. 2006;239:271–280. doi: 10.1016/j.canlet.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 253.Basini G, Bussolati S, Santini SE, Grasselli F. Sanguinarine inhibits VEGF-induced angiogenesis in a fibrin gel matrix. BioFactors (Oxford, England) 2007;29:11–18. doi: 10.1002/biof.5520290102. [DOI] [PubMed] [Google Scholar]
- 254.Singh RP, Raina K, Sharma G, Agarwal R. Silibinin inhibits established prostate tumor growth, progression, invasion, and metastasis and suppresses tumor angiogenesis and epithelial–mesenchymal transition in transgenic adenocarcinoma of the mouse prostate model mice. Clinical Cancer Research. 2008;14:7773–7780. doi: 10.1158/1078-0432.CCR-08-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Xu C, Shen G, Chen C, Gelinas C, Kong AN. Suppression of NF-kappaB and NF-kappaB-regulated gene expression by sulforaphane and PEITC through IkappaBalpha, IKK pathway in human prostate cancer PC-3 cells. Oncogene. 2005;24:4486–4495. doi: 10.1038/sj.onc.1208656. [DOI] [PubMed] [Google Scholar]
- 256.Davis R, Singh KP, Kurzrock R, Shankar S. Sulforaphane inhibits angiogenesis through activation of FOXO transcription factors. Oncology Reports. 2009;22:1473–1478. doi: 10.3892/or_00000589. [DOI] [PubMed] [Google Scholar]
- 257.Avramis IA, Kwock R, Avramis VI. Taxotere and vincristine inhibit the secretion of the angiogenesis inducing vascular endothelial growth factor (VEGF) by wild-type and drug-resistant human leukemia T-cell lines. Anticancer Research. 2001;21:2281–2286. [PubMed] [Google Scholar]
- 258.Bi S, Liu JR, Li Y, Wang Q, Liu HK, Yan YG, et al. Gamma-tocotrienol modulates the paracrine secretion of VEGF induced by cobalt(II) chloride via ERK signaling pathway in gastric adenocarcinoma SGC-7901 cell line. Toxicology. 2010;274:27–33. doi: 10.1016/j.tox.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 259.Kanjoormana M, Kuttan G. Antiangiogenic activity of ursolic acid. Integrative Cancer Therapies. 2010;9:224–235. doi: 10.1177/1534735410367647. [DOI] [PubMed] [Google Scholar]
- 260.Lirdprapamongkol K, Kramb JP, Suthiphongchai T, Surarit R, Srisomsap C, Dannhardt G, et al. Vanillin suppresses metastatic potential of human cancer cells through PI3K inhibition and decreases angiogenesis in vivo. Journal of Agricultural and Food Chemistry. 2009;57:3055–3063. doi: 10.1021/jf803366f. [DOI] [PubMed] [Google Scholar]
- 261.Kaltschmidt B, Kaltschmidt C, Hofmann TG, Hehner SP, Droge W, Schmitz ML. The pro- or anti-apoptotic function of NF-kappaB is determined by the nature of the apoptotic stimulus. European Journal of Biochemistry. 2000;267:3828–3835. doi: 10.1046/j.1432-1327.2000.01421.x. [DOI] [PubMed] [Google Scholar]
- 262.Hsieh CY, Santell RC, Haslam SZ, Helferich WG. Estrogenic effects of genistein on the growth of estrogen receptor-positive human breast cancer (MCF-7) cells in vitro and in vivo. Cancer Research. 1998;58:3833–3838. [PubMed] [Google Scholar]
- 263.Allred CD, Ju YH, Allred KF, Chang J, Helferich WG. Dietary genistin stimulates growth of estrogen-dependent breast cancer tumors similar to that observed with genistein. Carcinogenesis. 2001;22:1667–1673. doi: 10.1093/carcin/22.10.1667. [DOI] [PubMed] [Google Scholar]
- 264.Hulka BS. Epidemiology of susceptibility to breast cancer. Progress in Clinical and Biological Research. 1996;395:159–174. [PubMed] [Google Scholar]
- 265.Messina M, McCaskill-Stevens W, Lampe JW. Addressing the soy and breast cancer relationship: Review, commentary, and workshop proceedings. Journal of the National Cancer Institute. 2006;98:1275–1284. doi: 10.1093/jnci/djj356. [DOI] [PubMed] [Google Scholar]
- 266.Kim YI. Folate and colorectal cancer: An evidence-based critical review. Molecular Nutrition & Food Research. 2007;51:267–292. doi: 10.1002/mnfr.200600191. [DOI] [PubMed] [Google Scholar]
- 267.Bernard D, Monte D, Vandenbunder B, Abbadie C. The c-Rel transcription factor can both induce and inhibit apoptosis in the same cells via the upregulation of MnSOD. Oncogene. 2002;21:4392–4402. doi: 10.1038/sj.onc.1205536. [DOI] [PubMed] [Google Scholar]
- 268.Sheehy AM, Schlissel MS. Overexpression of RelA causes G1 arrest and apoptosis in a pro-B cell line. The Journal of Biological Chemistry. 1999;274:8708–8716. doi: 10.1074/jbc.274.13.8708. [DOI] [PubMed] [Google Scholar]
- 269.Kasinski AL, Du Y, Thomas SL, Zhao J, Sun SY, Khuri FR, et al. Inhibition of IkappaB kinase-nuclear factor-kappaB signaling pathway by 3,5-bis(2-flurobenzylidene) piperidin-4-one (EF24), a novel monoketone analog of curcumin. Molecular Pharmacology. 2008;74:654–661. doi: 10.1124/mol.108.046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Chen CC, Chow MP, Huang WC, Lin YC, Chang YJ. Flavonoids inhibit tumor necrosis factor-alpha-induced up-regulation of intercellular adhesion molecule-1 (ICAM-1) in respiratory epithelial cells through activator protein-1 and nuclear factor-kappaB: Structure–activity relationships. Molecular Pharmacology. 2004;66:683–693. doi: 10.1124/mol.66.3.. [DOI] [PubMed] [Google Scholar]
- 271.Pandey MK, Sung B, Kunnumakkara AB, Sethi G, Chaturvedi MM, Aggarwal BB. Berberine modifies cysteine 179 of IkappaBalpha kinase, suppresses nuclear factor-kappaB-regulated antiapoptotic gene products, and potentiates apoptosis. Cancer Research. 2008;68:5370–5379. doi: 10.1158/0008-5472.CAN-08-0511. [DOI] [PubMed] [Google Scholar]
- 272.Slivova V, Zaloga G, DeMichele SJ, Mukerji P, Huang YS, Siddiqui R, et al. Green tea polyphenols modulate secretion of urokinase plasminogen activator (uPA) and inhibit invasive behavior of breast cancer cells. Nutrition and Cancer. 2005;52:66–73. doi: 10.1207/s15327914nc5201_9. [DOI] [PubMed] [Google Scholar]
- 273.Sung B, Pandey MK, Aggarwal BB. Fisetin, an inhibitor of cyclin-dependent kinase 6, down-regulates nuclear factor-kappaB-regulated cell proliferation, antiapoptotic and metastatic gene products through the suppression of TAK-1 and receptor-interacting protein-regulated IkappaBalpha kinase activation. Molecular Pharmacology. 2007;71:1703–1714. doi: 10.1124/mol.107.034512. [DOI] [PubMed] [Google Scholar]
- 274.Li Y, Tanaka K, Li X, Okada T, Nakamura T, Takasaki M, et al. Cyclin-dependent kinase inhibitor, flavopiridol, induces apoptosis and inhibits tumor growth in drug-resistant osteosarcoma and Ewing’s family tumor cells. International Journal of Cancer. 2007;121:1212–1218. doi: 10.1002/ijc.22820. [DOI] [PubMed] [Google Scholar]
- 275.Chen CS, Lee CH, Hsieh CD, Ho CT, Pan MH, Huang CS, et al. Nicotine-induced human breast cancer cell proliferation attenuated by garcinol through down-regulation of the nicotinic receptor and cyclin D3 proteins. Breast Cancer Research and Treatment. 2010 doi: 10.1007/s10549-010-0821-3. in press. [DOI] [PubMed] [Google Scholar]
- 276.Liu M, Luo XJ, Liao F, Lei XF, Dong WG. Noscapine induces mitochondria-mediated apoptosis in gastric cancer cells in vitro and in vivo. Cancer Chemotherapy and Pharmacology. 2010 doi: 10.1007/s00280-010-1356-3. in press. [DOI] [PubMed] [Google Scholar]
- 277.Shan BE, Wang MX, Li RQ. Quercetin inhibit human SW480 colon cancer growth in association with inhibition of cyclin D1 and survivin expression through Wnt/ beta-catenin signaling pathway. Cancer Investigation. 2009;27:604–612. doi: 10.1080/07357900802337191. [DOI] [PubMed] [Google Scholar]
- 278.al-Harbi MM, Qureshi S, Raza M, Ahmed MM, Giangreco AB, Shah AH. Influence of anethole treatment on the tumour induced by Ehrlich ascites carcinoma cells in paw of Swiss albino mice. European Journal of Cancer Prevention. 1995;4:307–318. doi: 10.1097/00008469-199508000-00006. [DOI] [PubMed] [Google Scholar]
- 279.Choi YH, Choi WY, Hong SH, Kim SO, Kim GY, Lee WH, et al. Anti-invasive activity of sanguinarine through modulation of tight junctions and matrix metalloproteinase activities in MDA-MB-231 human breast carcinoma cells. Chemico-Biological Interaction. 2009;179:185–191. doi: 10.1016/j.cbi.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 280.Cha HJ, Park MT, Chung HY, Kim ND, Sato H, Seiki M, et al. Ursolic acid-induced down-regulation of MMP-9 gene is mediated through the nuclear translocation of glucocorticoid receptor in HT1080 human fibrosarcoma cells. Oncogene. 1998;16:771–778. doi: 10.1038/sj.onc.1201587. [DOI] [PubMed] [Google Scholar]