TLR-mediated induction of cholesterol 25-hydoxylase transcription in dendritic cells and macrophages is dependent on IFN-α/IFN-β and signaling through INF-αR and STAT1.
Keywords: innate immunity, lung, STAT1, TLR, LPS, poly I:C
Abstract
The oxysterol-producing enzyme CH25H plays an important role in regulating lipid metabolism, gene expression, and immune activation. In vitro experiments using a panel of TLR agonists to activate BMDCs and macrophages demonstrated that Ch25h expression is induced rapidly, selectively, and robustly by the TLR ligands poly I:C and LPS. The mechanism of TLR3- and TLR4-induced transcription levels of Ch25h relies on the TRIF-mediated production of type I IFNs and requires signaling through the IFNαR and JAK/STAT1 pathway. Treatment of BMDCs and macrophages with IFN-α or IFN-β induces Ch25h in a STAT1-dependent manner. IFN-γ also up-regulated Ch25h expression by signaling through STAT1, suggesting that multiple pathways regulate the production of this enzyme. In addition, we demonstrated that regulation of Ch25h expression in vivo in lung-derived DCs and macrophages is dependent on signaling through the IFNαR and STAT1. The results suggest that the rapid induction of Ch25h and subsequent oxysterol synthesis may represent a component of the regulatory network that modulates the magnitude of innate immune reactions and possibly the nature and intensity of subsequent adaptive responses.
Introduction
Cholesterol, which makes up the vast majority of all sterols in mammals, plays a number of key roles in maintaining homeostasis. In addition to being a major component of cell membranes required to maintain appropriate fluidity and permeability, cholesterol is a precursor of a number of important signaling molecules. Oxysterols, the short-lived, oxygenated derivatives of cholesterol, have evolved to serve physiological roles in the trafficking of cholesterol within and between tissues [1], the activation of nuclear hormone receptors [2, 3] and steroid hormone synthesis [4], and the regulation of genes that participate in cholesterol biosynthesis [5].
The oxysterols 24HC, 25HC, and 27HC are the main products of the membrane-associated enzymes CH24H, CH25H, and CH27H, respectively [1]. In several tissues, cholesterol is converted into the more-readily, soluble oxysterol form and transported to the liver, where the oxysterols are converted into the bile acids that are critical for normal vitamin and lipid metabolism [6, 7]. In addition to their contributions to basic metabolic processes, oxysterols are involved in signaling pathways that regulate inflammation through their influence on the activation status and function of macrophages [8–10], mast cells [11], T cells [12, 13], and B cells [14]. Oxysterols are also implicated to play a role in the pathogenesis of chronic diseases such as Alzheimer's disease [15] and atherosclerosis [16].
Human and mouse CH25H is a 31.6-kDa ER-associated glycoprotein encoded by an intronless gene [17]. Unlike CH24H and CH27H, which are cytochrome P450 family proteins, CH25H is a member of a small family of molecules that uses diiron cofactors to catalyze the hydroxylation of hydrophobic substrates. Although expression levels at steady-state are low-to-undetectable in most tissues [17], Ch25h is induced rapidly in the heart, brain, muscle, kidney, lung, and most notably, liver upon in vivo exposure to a TLR4 agonist [14]. Studies have also demonstrated that macrophages are potentially a rich source of inducible CH25H in these tissues and that transcription is selectively induced by TLR3 and TLR4 agonists [14, 18].
The observations that TLR ligands rapidly induce significantly elevated Ch25h expression levels in multiple tissues suggest that Ch25h and 25HC are important components of the innate immune response pathogens. Indeed, recent reports from our lab [19, 20] and from others [21–23] have shown that Ch25h is up-regulated rapidly and significantly in the lungs of mice in response to a pathogen or to a nonpathogen challenge. Although it is clear that Ch25h expression is induced under a variety of conditions, the cellular sources and molecular mechanisms that control this expression are yet to be defined.
In the work presented here, we demonstrate for the first time that DCs as well as macrophages are a significant source of CH25H and that the induction of Ch25h innate expression in DCs and macrophages is largely restricted to signaling through TLR3 and TLR4. In addition, we establish that TLR-mediated expression of Ch25h is dependent on TRIF, production of type I IFN, and signaling through the IFNR/JAK/STAT1 pathway. The results identify Ch25h as an IFN-responsive gene in DCs and macrophages during innate immune responses. The early expression of Ch25h implies a role for oxysterols in regulating innate immunity.
MATERIALS AND METHODS
Mice
BALB/cJ, C57BL/6, myd88−/−, trif−/−, and stat6−/− were purchased from The Jackson Laboratory (Bar Harbor, ME, USA). ifnar−/− mice on a BALB/cJ background [24, 25] were obtained with permission from Michael Aguet (Swiss Institute for Experimental Cancer Research, Lausanne, Switzerland). Stat1−/− mice on a 129S6/SvEvTac background and the WT 129S6/SvEvTac controls were purchased from Taconic (Rockville, MD, USA). Male mice at 6–8 weeks of age were used for the experiments. All animal procedures described in this study were performed under the approval of the Johns Hopkins Animal Care and Use Committee (Baltimore, MD, USA) in accord with the guidelines set by the National Research Council's Guide for Care and Use of Laboratory Animals.
Isolation of lung macrophages
Lungs were harvested and processed for the isolation of CD11c+ lung macrophages as outlined previously [20]. Briefly, finely chopped lungs were suspended in RPMI (Invitrogen, Carlsbad, CA, USA) and digested for 30 min with 1 mg/ml Collagenase II (Gibco, Carlsbad, CA, USA) and 30 μg/ml DNase I (Roche, Indianapolis, IN, USA). After passing through a sterile strainer (352360, BD Falcon, Franklin Lakes, NJ, USA), RBCs were removed, and CD11c+ cells were isolated by the IMag™ cell separation system protocol (BD PharMingen, San Diego, CA, USA). The purity of the cells was checked by flow cytometry (FACSCalibur, BD Biosciences, San Jose, CA, USA) and was typically >90% CD11c+ cells.
Preparation of BMDCs and BMMs
Marrow cells were collected from long bones using a syringe fitted with a 25-G needle, filtered through strainers (BD Falcon), and treated with ACK Lysing Buffer (Quality Biologicals, Gaithersburg, MD, USA) to remove RBCs. For BMDCs, cells were cultured with IMDM (Invitrogen) and supplemented with 10% FBS, 1× antibiotic-antimycotic (Invitrogen), 55 μM 2-ME (Sigma-Aldrich, St. Louis, MO, USA), and 20 ng/ml GM-CSF (Invitrogen). Half of the culture medium was changed at Days 3, 5, and 7. On Day 8 or 9 of culture, CD11c+ cells were isolated by the IMag™ cell separation system protocol (BD PharMingen) using the manufacturer's protocol. For BMM differentiation, cells were cultured in supplemented IMDM containing 30% L929 cell culture supernatant. Half of the medium was changed at Days 3 and 5 of culture. At Day 6, floating cells were removed, and the culture medium was changed to IMDM, supplemented 10% FBS without L929 culture supernatant. On Day 7, fully differentiated macrophage cultures were used for stimulation.
Stimulation of cells with TLR ligands and IFNs
In vitro stimulations of the BMDC, BMM, and CD11c+ lung macrophages were carried out with 1 × 106 cells/well in a 24-well plate (BD Falcon). The cells were exposed to a panel of TLR agonists (Invivogen) that included 1 μg/ml Pam3CSK4 (TLR1/2 agonist), 1 × 108/ml HKLM (TLR2 agonist), 25 μg/ml poly I:C (TLR3 agonist), 1 μg/ml of ultra-pure LPS (TLR4 agonist) from Escherichia coli K12, 1 μg/ml flagellin from Salmonella typhimurium (TLR5 agonist), 1 μg/ml FSL-1 (TLR6/2 agonist), 1 μg/ml ssRNA40 (TLR7 agonist), and 2.5 μM CpG ODN1826 (TLR9 agonist). Cells were also stimulated with IFN-α (1000 units/ml; 12105-1, PBL InterferonSource, Piscataway, NJ, USA), IFN-β (1000 units/ml; I9032, Sigma-Aldrich), or IFN-γ (1 μg/ml; I4777, Sigma-Aldrich) for 6 h. Cells were harvested for RNA isolation as described below.
Real-time RT-PCR
Lung tissues were homogenized in Trizol (Invitrogen), and RNA cleanup was performed using RNeasy mini columns from Qiagen (Valencia, CA, USA) with on-column DNase I treatment. Total RNA was isolated from 106 cultured cells using the RNeasy mini kit (Qiagen) with on-column DNase I treatment. Total RNA (1.0 μg) was reverse-transcribed with SuperScript II (Invitrogen) using random hexamers following the manufacturer's protocols. The following primer-probe sets were obtained as Taqman® gene expression assays-on-demand (Applied Biosystems, Foster City, CA, USA): Ch25h (Mm00515483_s1), ifnβ (Mm004395496_s1), Taqman® rRNA control reagent. A standard curve was constructed from the expression levels in serial dilutions of pooled cDNAs from known positive samples. The data obtained using the ABI 7500 were normalized to the expression of the gene encoding the 18S rRNA.
JAK inhibition
BMDCs and BMMs were exposed to 0.2, 1.0, or 5.0 μM InSolution™ JAK inhibitor 1 (Calbiochem, San Diego, CA, USA) for 1 h prior to stimulation with 25 μg/ml poly I:C, 1 μg/ml LPS, or 1000 units/ml IFN-β. After 6 h, the cells were harvested for RNA isolation. The inhibition of STAT1-phosphorylation by JAK inhibitor 1 was confirmed using immunostained Western blots of cell extracts harvested after 3 h of stimulation using anti-STAT1 (BD PharMingen), antiphospho-STAT1 (Cell Signaling Technologies, Danvers, MA, USA), and anti-actin (Abcam, Cambridge, MA, USA).
Statistical analysis
The Student's t test and ANOVA were used to calculate statistical significance using Prism 4 (GraphPad Software, La Jolla, CA, USA).
RESULTS
TLR ligands induce Ch25h in BMMs and BMDCs
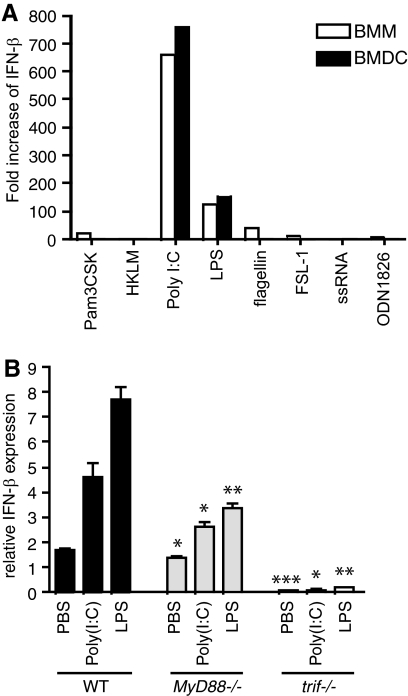
Recent studies have reported that TLR4 and TLR3 agonists selectively induce Ch25h expression in macrophages [14, 18]. To determine if DCs also express Ch25h in response to TLR ligands, transcription levels of Ch25h were measured in BMDCs stimulated with a panel of eight TLR ligands for 1, 3, 6, or 24 h. As reported for macrophages, the ligands for TLR3 (poly I:C) and TLR4 (LPS) robustly increased Ch25h expression in BMDC (Fig. 1A). By comparison, the other six TLR agonists induced small but detectable levels of Ch25h transcription. Under these in vitro conditions, the highest poly I:C- and LPS-induced transcription levels of Ch25h by BMDCs were measured at 6 h (Fig. 1A). The same TLR ligands were tested for their ability to induce Ch25h in BMMs after 6 h of stimulation. As observed for BMDCs, ligands for TLR3 and TLR4 induced robust Ch25h expression in BMMs, and the ligands for other TLRs had only a modest effect (Fig. 1B).
Figure 1. TLR-mediated induction of Ch25h expression.
(A) BMDCs derived from a single BALB/c mouse were stimulated with a panel of TLR ligands for 1, 3, 6, or 24 h and then harvested for real-time RT-PCR analysis of Ch25h expression. The data are from a single experiment that is representative of three biological replicates. (B) BMDCs and BMMs derived from a single BALB/c mouse were stimulated with a panel of TLR ligands for 6 h and then harvested for real-time RT-PCR analysis of Ch25h expression. The data are from a single experiment that is representative of three biological replicates. (C) BMDCs from WT C57BL/6, myd88−/−, and trif−/− mice were cultured and stimulated with PBS, poly I:C, LPS, or IFN-β for 6 h and then harvested for real-time RT-PCR analysis of Ch25h expression, which was normalized to 18S rRNA levels and expressed as relative units or as fold-change over PBS controls. Statistical significance for each treatment between WT and gene-deficient strains was assessed by Student's t test. *P < 0.05; **P < 0.005.
Signal transduction events initiated by TLRs rely on two adaptor molecules: MyD88 and TRIF. TLR3 signals solely through a TRIF-dependent pathway, and TLR4 uses the MyD88 and TRIF pathways [26]. To test the role of these adaptor proteins in TLR-mediated expression of Ch25h, BMDCs were generated from myd88−/− and trif−/− animals. In the absence of MyD88, poly I:C-induced expression of Ch25h in BMDCs was not different from WT controls (Fig. 1C). LPS treatment of myd88−/− BMDCs resulted in a modest but statistically significant reduction, indicating that MyD88 has a role to play in the regulation of this enzyme. In contrast, there was little to no TLR3- or TLR4-mediated Ch25h transcription in trif−/− BMDCs, suggesting that TLR-mediated expression of this enzyme functions primarily through a TRIF-dependent mechanism. The importance of TRIF in the mechanism of Ch25h expression is underscored by the near-total absence of transcription levels in the TRIF-deficient BMDCs even under control conditions (Fig. 1C).
Ch25h expression is controlled primarily by type I IFN signaling
TRIF-dependent signaling culminates in the activation of NF-κB and IRF3, subsequently leading to the induction of IFN-β [26]. Indeed, the same BMDCs and BMMs that demonstrated a significant up-regulation of Ch25h expression after poly I:C or LPS treatment also exhibited an induction in ifnβ transcription (Fig. 2A). Under the conditions used here, none of the other six TLR ligands induced significant levels of ifnβ expression. Using BMDCs from WT, myd88−/−, and trif−/− animals, it was demonstrated that TRIF signaling had a dominant effect on the transcription levels of type I IFN in poly I:C- and LPS-treated cells (Fig. 2B) and that the levels of ifnβ expression paralleled that of Ch25h for each treatment (Fig. 1C).
Figure 2. TLR-mediated ifnβ expression.
(A) ifnβ expression in BMDCs and BMMs stimulated with a panel of TLR ligands for 6 h. Transcription was measured by real-time RT-PCR, the results were normalized to 18S rRNA expression, and ifnβ transcription was expressed as a fold-change over PBS controls. The data are from a single experiment that is representative of biological replicates. (B) BMDCs from WT C57BL/6, myd88−/−, and trif−/− mice were cultured and stimulated with PBS, poly I:C, LPS, or IFN-β for 6 h. Transcription of ifnβ was measured by real-time RT-PCR, normalized to 18S rRNA levels, and expressed in relative units. Statistical significance for each treatment between WT and gene-deficient strains was assessed by Student's t test. *P < 0.05; **P < 0.005; ***P < 0.0005.
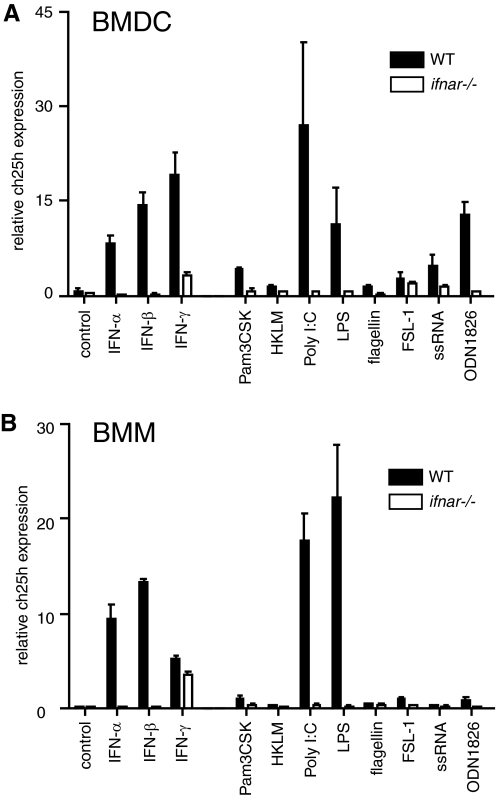
These results suggested that induction of Ch25h by poly I:C/TLR3 and LPS/TLR4 is indirectly controlled through IFNβR–IFNαR interactions. To determine the role of type I IFN signaling in the regulation of Ch25h expression, BMMs and BMDCs from type 1 ifnar−/− and WT mice were stimulated with IFN-α or IFN-β. After 6 h, the cells were harvested, and the transcription level of Ch25h was measured by real-time RT-PCR. IFN-α and IFN-β treatment resulted in a significant induction of Ch25h transcription in the BMMs and BMDCs from WT mice but not in cells from ifnar−/− mice (Fig. 3). IFN-α and IFN-β appeared to be equally potent in inducing Ch25h expression in BMDCs and BMMs.
Figure 3. Type1 IFN-mediated Ch25h expression is IFNR-dependent.
BMDCs (A) and BMMs (B) from WT BALB/cJ and ifnar−/− mice were stimulated with IFN-α, IFN-β, IFN-γ, or a panel of TLR ligands for 6 h, and the transcription of Ch25h was measured by real-time RT-PCR. Ch25h transcription was expressed in relative units normalized to 18S rRNA. Each bar represents the mean (sd) of the measurements from three biological replicates. The differences in Ch25h expression between WT- and ifnar−/−-derived BMDCs for poly I:C, LPS, ODN1826, IFN-α, IFN-β, and IFN-γ treatments were statistically significant at P < 0.05 (two-way ANOVA). The differences in Ch25h expression between WT- and ifnar−/−-derived BMMs for poly I:C, LPS, IFN-α, and IFN-β treatments were statistically significant at P < 0.0001 (two-way ANOVA).
BMDCs and BMMs from ifnar−/− mice were also stimulated with the panel of TLR agonists. In the absence of the IFNαR, neither the BMDC nor the BMM responded to TLR activation with Ch25h expression (Fig. 3). These results support the hypothesis that TLR-mediated induction of Ch25h expression is controlled indirectly through type I IFN signaling.
As a control experiment, the type II IFN, IFN-γ, was included. Interestingly, IFN-γ also induced significant levels of Ch25h transcription in BMDCs and BMMs from WT animals that were modulated but not fully suppressed in the cells from ifnar−/− animals (Fig. 3). Thus, it appears that IFN-γ-mediated signaling also has a role in the regulation of Ch25h expression.
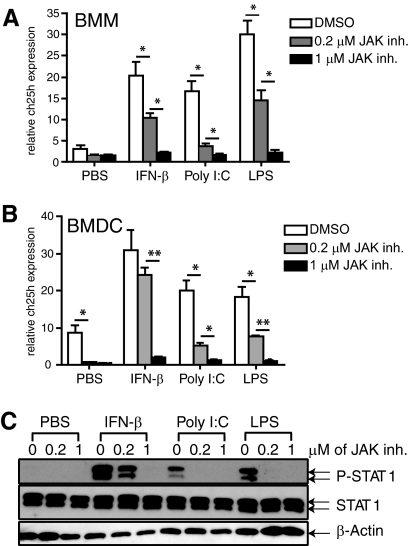
Induction of Ch25h is JAK- and STAT1-dependent
The IFNαR-dependent nature of Ch25h expression is also supported by the results of experiments in which the activity of JAKs was blocked. Using a JAK inhibitor, the levels of Ch25h transcription induced by IFN-β, poly I:C, or LPS were reduced in a dose-dependent manner in BMMs and BMDCs from WT mice (Fig. 4A and B). To verify the action of the JAK inhibitor, immunostained Western blots of BMDC extracts were used to demonstrate that the activation via phosphorylation of STAT1, a key transcription factor in the IFN-β (and IFN-γ) signaling pathway, was blocked (Fig. 4C).
Figure 4. Induction of Ch25h in BMMs and BMDCs is JAK-dependent.
BMMs (A) and BMDCs (B) were treated with 0, 0.2, or 1.0 μM JAK inhibitor 1 (inh.) for 1 h and then stimulated with 25 μg/ml poly I:C, 1 μg/ml LPS, or 1000 units/ml IFN-β for 6 h. Transcription of Ch25h was measured by real-time RT-PCR, and the data were normalized to 18S rRNA levels and expressed in relative expression units. Bars represent the mean (sd) response from three mice/group. *P < 0.05; **P < 0.005, by Student's t test. (C) BMDCs treated with 0, 0.2, or 1.0 μM JAK inhibitor 1 for 1 h and then incubated for 3 h with PBS, 1000 units/ml IFN-β, 25 μg/ml poly (I:C), or 1 μg/ml LPS. Cells were harvested and processed for Western blotting and immunostaining for the presence of phospho-STAT1 (P-STAT1), STAT1, or β-actin.
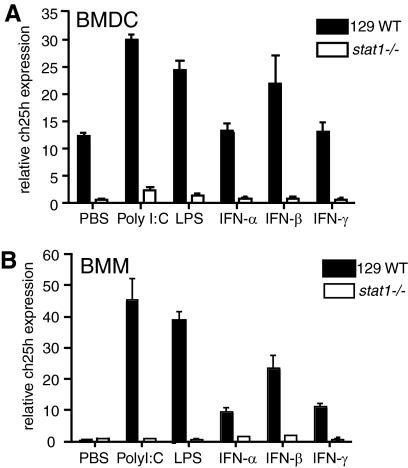
To determine further if the induction of Ch25h transcription was STAT1-dependent, BMMs and BMDCs were generated from stat1−/− and WT animals and stimulated with TLR ligands, IFN-α, IFN-β, or IFN-γ for 6 h. Induction of Ch25h was abolished effectively in BMDCs and BMMs from stat1−/− in all of the treatment groups (Fig. 5). Thus, in BMMs and BMDCs, Ch25h expression is regulated directly by the actions of type I or type II IFNs that signal in a JAK- and STAT1-dependent manner.
Figure 5. TLR- and IFN-induced Ch25h expression is STAT1-dependent.
BMDCs (A) and BMMs (B) cultured from 129 WT and stat1−/− mice were stimulated with poly I:C, LPS, IFN-α, IFN-β, or IFN-γ for 6 h, and then, Ch25h transcription was measured by real-time RT-PCR. Bars represent the mean (sd) of the response from three mice/strain for each treatment after normalization to 18S rRNA levels. The differences in expression of Ch25h between 129 WT and stat1−/− for BMMs and BMDCs for each treatment were statistically significant at P < 0.0001 (two-way ANOVA).
Regulation of Ch25h in vivo
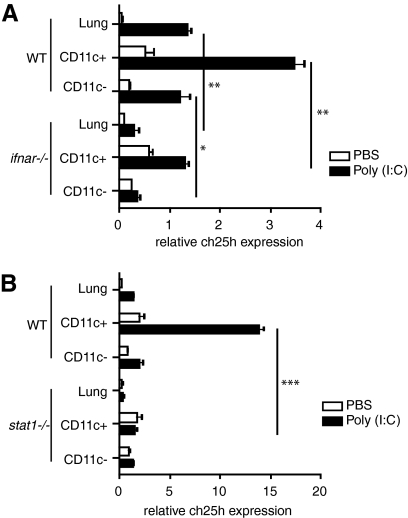
To determine if TLR-mediated induction of Ch25h was also dependent on signaling though IFNRα and STAT1 in vivo, we administered poly I:C intratracheally to ifnar−/−, stat1−/−, and strain-matched control mice and processed the lungs to determine Ch25h levels in the RNA isolated from whole lung tissue and from an enriched population of CD11c+ DCs and macrophages (lung macrophages and DCs express elevated levels of CD11c [27]). In WT animals, administration of poly I:C resulted in a significant up-regulation of Ch25h in the whole lung with a majority of the response derived from the CD11c+ cell population (Fig. 6A and B). The Ch25h levels were diminished significantly in the whole lungs and CD11c+ cells isolated from ifnar−/− (Fig. 6A) and stat1−/− (Fig. 6B) mice. The results indicate that similar to the responses observed in vitro, TLR-mediated induction of Ch25h in DCs and macrophages in vivo is type I IFN- and STAT1-dependent.
Figure 6. Ch25h expression in mouse lung is stat1-dependent.
Naïve Balb/cJ WT and ifnar−/− (A) and 129 WT and stat1−/− (B) were challenged intratracheally with 90 μg poly I:C. Whole lungs as well as the CD11c+ and CD11c– cells were isolated at 24 h post-exposure and processed for real-time PCR analysis of Ch25h transcription. Each bar represents the mean (sd) of the results from three animals normalized to 18S rRNA levels and presented as relative expression units. *P < 0.05; **P < 0.005; ***P < 0.0005, by Student's t test.
DISCUSSION
The significance of the Ch25h up-regulation in DCs and macrophages during innate immune responses presumably lies in the production of 25HC, an oxysterol that has the capacity to regulate lipid metabolism, gene expression, and immune activation. Of the three naturally occurring oxysterols, 25HC, 24HC, and 27HC, 25HC has proven to be the most potent regulator of gene expression [2, 28, 29]. Oxysterols bind to and activate the nuclear LXR, which in turn, regulates the expression of other lipid-metabolizing genes that promote the conversion of cholesterol in the liver into bile acids [2, 30]. Oxysterols are also powerful down-regulators of gene activation. They block cleavage of sterol regulatory element-binding proteins-1 and -2, which prevents these transcription factors from entering the nucleus and activating a suite of genes encoding molecules that regulate cholesterol supply and synthesis [5]. Oxysterols also down-regulate 3-hydroxy-3-methylglutaryl-CoA reductase production [1], a key regulatory enzyme in the cholesterol and isoprenoid biosynthesis pathways [31].
By virtue of their effects on gene expression and lipid metabolism, oxysterols influence immune responses. Oxysterols have been shown to bind and modulate the action of LXR [30, 32, 33], which in turn, exerts immunomodulatory effects on immune cells. Activation of LXR in vivo reduced inflammation in a contact dermatitis model [34], inhibited inflammatory gene expression in the aortas of atherosclerotic mice [35], and reduced inflammation in the lung [12, 36, 37]. In macrophages, oxysterol-mediated activation of LXR leads to the suppression of TLR-mediated innate immune responses as measured by a reduced production of cytokines (IL-6, IL-1β), chemokines (MCP-1, MCP-3), and effector molecules (iNOS, COX-2, MMP-9) [38, 39], while promoting macrophage survival [9]. In DCs, stimulation of LXR during innate activation decreases CD86 and IL-12 production, enhances secretion of IL-10, and blocks the ability to activate T cells [40]. The connection between LXR and TLR signaling in macrophages is underscored by the report that TLR3- and TLR4-mediated, IRF3-dependent activation of macrophages blocks induction of LXR target genes and inhibits cholesterol efflux [8]. In contrast, our data and recently published observations [14, 18] demonstrate that TLR3 and TLR4 agonists induce CH25H and presumably, oxysterol synthesis, which would predict that immune modulation would be accompanied by LXR target gene induction and enhanced cholesterol efflux. It is possible that in addition to oxysterol synthesis, TLR activation induces the production of oxysterol-metabolizing enzymes such as SULT2B1 [12] and CYP7B1 [41], which would lead to a net suppression of the LXR pathway. It is clear that additional work is necessary to define the role of LXR signaling in macrophage function.
Oxysterols also have an impact on lymphocyte proliferation and activation. It has been demonstrated that 25HC produced by macrophages inhibits lymphocyte growth [42]. Proliferation of B and T cells is inhibited by oxysterols in a dose-dependent manner through their ability to activate LXR in lymphocytes and alter the intracellular sterol metabolism [12]. Furthermore, 25HC treatment of naïve B cells suppresses IL-2-mediated proliferation and reduces the expression of activation-induced cytidine deaminase, which blocks class-switching to IgA [14].
Although type I IFNs are shown to be key regulators of innate expression, the control of Ch25h expression is clearly more complex. Pam3CSK, ODN1826, and ssRNA, TLR ligands that resulted in no significant increase in ifnβ (Fig. 2A), induced detectable levels of Ch25h expression, especially in BMDCs (Figs. 1A and 3A). IFN-γ also induces expression of the enzyme in BMDCs through a mechanism that appears to be STAT1-dependent. Indeed, consensus IFN-γ activation-site elements and IFN-stimulated response elements are located upstream of the Ch25h ORF in the mouse genome (data not shown). Thus, in addition to a possible role in modulating innate responses, IFN-γ-induced, CH25H-mediated production of 25HC by DCs, macrophages, or other cell types may be important in regulating certain aspects of adaptive immune responses.
Recent reports have demonstrated that Ch25h transcription and CH25H protein are induced through TLR3- and TLR4-mediated stimulation of peritoneal macrophages and BMMs [14, 18]. Here, we extend these observations in BMDCs and to lung-derived DCs and macrophages and establish that TLR-mediated induction of this enzyme is through a mechanism that is dependent on signaling through the IFN-α/IFN-β receptor and STAT1. The results suggest that the rapid induction of Ch25h and subsequent oxysterol synthesis may represent a component of the regulatory network that modulates the magnitude of innate immune reactions and possibly the nature and intensity of subsequent adaptive responses.
ACKNOWLEDGMENTS
This work was supported by grants from NIH National Heart, Lung, and Blood Institute (U01 HL66623), NIH training grant T32AI007417, and Johns Hopkins University Malaria Research Institute. K.P. derived support from the Katherine E. Welsh and the Otis and Calista Causey Fellowships. We thank F. Housseau, Fidel Zavala, and Delisa Fairweather for providing mice; and Matt Craig for discussion and critique.
Footnotes
- 24/25/27HC
- 24/25/27-hydroxycholestrol
- BMDC
- bone marrow-derived DC
- BMM
- bone marrow-derived macrophage
- CH24/25/27H
- cholesterol 24/25/27-hydoxylase
- FSL-1
- synthetic lipoprotein Pam2CGDPKHPKSF
- HKLM
- heat-killed Listeria monocytogenes
- ifnar−/−
- IFNαR-deficient mice
- IRF
- IFN regulatory factor
- LXR
- liver X receptor
- NIH
- National Institutes of Health
- ODN1826
- oligodeoxynucleotide 1826
- Pam3CSK4
- palmitoyl-3-cysteine-serine-lysine-4
- poly I:C
- polyinosinic:polycytidylic acid
- TRIF
- Toll/IL-1R domain-containing adaptor-inducing IFN-β
AUTHORSHIP
K.P. designed and carried out the experiments and composed the manuscript. A.L.S. designed the experiments and wrote the manuscript.
REFERENCES
- 1.Russell D. W. (2000) Oxysterol biosynthetic enzymes. Biochim. Biophys. Acta 1529, 126–135 [DOI] [PubMed] [Google Scholar]
- 2.Lehmann J. M., Kliewer S. A., Moore L. B., Smith-Oliver T. A., Oliver B. B., Su J. L., Sundseth S. S., Winegar D. A., Blanchard D. E., Spencer T. A., Willson T. M. (1997) Activation of the nuclear receptor LXR by oxysterols defines a new hormone response pathway. J. Biol. Chem. 272, 3137–3140 [DOI] [PubMed] [Google Scholar]
- 3.Wang Y., Kumar N., Crumbley C., Griffin P. R., Burris T. P. (2010) A second class of nuclear receptors for oxysterols: regulation of RORα and RORγ activity by 24S-hydroxycholesterol (cerebrosterol). Biochim. Biophys. Acta 1801, 917–923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nes W. D., Lukyanenko Y. O., Jia Z. H., Quideau S., Howald W. N., Pratum T. K., West R. R., Hutson J. C. (2000) Identification of the lipophilic factor produced by macrophages that stimulates steroidogenesis. Endocrinology 141, 953–958 [DOI] [PubMed] [Google Scholar]
- 5.Brown M. S., Goldstein J. L. (1997) The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell 89, 331–340 [DOI] [PubMed] [Google Scholar]
- 6.Ishibashi S., Schwarz M., Frykman P. K., Herz J., Russell D. W. (1996) Disruption of cholesterol 7α-hydroxylase gene in mice. I. Postnatal lethality reversed by bile acid and vitamin supplementation. J. Biol. Chem. 271, 18017–18023 [DOI] [PubMed] [Google Scholar]
- 7.Schwarz M., Lund E. G., Russell D. W. (1998) Two 7 α-hydroxylase enzymes in bile acid biosynthesis. Curr. Opin. Lipidol. 9, 113–118 [DOI] [PubMed] [Google Scholar]
- 8.Castrillo A., Joseph S. B., Vaidya S. A., Haberland M., Fogelman A. M., Cheng G., Tontonoz P. (2003) Crosstalk between LXR and Toll-like receptor signaling mediates bacterial and viral antagonism of cholesterol metabolism. Mol. Cell 12, 805–816 [DOI] [PubMed] [Google Scholar]
- 9.Joseph S. B., Bradley M. N., Castrillo A., Bruhn K. W., Mak P. A., Pei L., Hogenesch J., O′Connell R. M., Cheng G., Saez E., Miller J. F., Tontonoz P. (2004) LXR-dependent gene expression is important for macrophage survival and the innate immune response. Cell 119, 299–309 [DOI] [PubMed] [Google Scholar]
- 10.Torocsik D., Szanto A., Nagy L. (2009) Oxysterol signaling links cholesterol metabolism and inflammation via the liver X receptor in macrophages. Mol. Aspects Med. 30, 134–152 [DOI] [PubMed] [Google Scholar]
- 11.Nunomura S., Endo K., Makishima M., Ra C. (2010) Oxysterol represses high-affinity IgE receptor-stimulated mast cell activation in liver X receptor-dependent and -independent manners. FEBS Lett. 584, 1143–1148 [DOI] [PubMed] [Google Scholar]
- 12.Bensinger S. J., Bradley M. N., Joseph S. B., Zelcer N., Janssen E. M., Hausner M. A., Shih R., Parks J. S., Edwards P. A., Jamieson B. D., Tontonoz P. (2008) LXR signaling couples sterol metabolism to proliferation in the acquired immune response. Cell 134, 97–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cuthbert J. A., Lipsky P. E. (1981) Sterol metabolism and lymphocyte responsiveness: inhibition of endogenous sterol synthesis prevents mitogen-induced human T cell proliferation. J. Immunol. 126, 2093–2099 [PubMed] [Google Scholar]
- 14.Bauman D. R., Bitmansour A. D., McDonald J. G., Thompson B. M., Liang G., Russell D. W. (2009) 25-Hydroxycholesterol secreted by macrophages in response to Toll-like receptor activation suppresses immunoglobulin A production. Proc. Natl. Acad. Sci. USA 106, 16764–16769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shibata N., Kawarai T., Lee J. H., Lee H. S., Shibata E., Sato C., Liang Y., Duara R., Mayeux R. P., St George-Hyslop P. H., Rogaeva E. (2006) Association studies of cholesterol metabolism genes (CH25H, ABCA1 and CH24H) in Alzheimer′s disease. Neurosci. Lett. 391, 142–146 [DOI] [PubMed] [Google Scholar]
- 16.Carter C. J. (2007) Convergence of genes implicated in Alzheimer′s disease on the cerebral cholesterol shuttle: APP, cholesterol, lipoproteins, and atherosclerosis. Neurochem. Int. 50, 12–38 [DOI] [PubMed] [Google Scholar]
- 17.Lund E. G., Kerr T. A., Sakai J., Li W. P., Russell D. W. (1998) cDNA cloning of mouse and human cholesterol 25-hydroxylases, polytopic membrane proteins that synthesize a potent oxysterol regulator of lipid metabolism. J. Biol. Chem. 273, 34316–34327 [DOI] [PubMed] [Google Scholar]
- 18.Diczfalusy U., Olofsson K.E., Carlsson A.M., Gong M., Golenbock D.T., Rooyackers O., Flaring U., Bjorkbacka H. (2009) Marked up-regulation of cholesterol 25-hydroxylase expression by lipopolysaccharide. J. Lipid Res. 50, 2258–2264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reece J. J., Siracusa M. C., Scott A. L. (2006) Innate immune responses to lung-stage helminth infection induce alternatively activated alveolar macrophages. Infect. Immun. 74, 4970–4981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siracusa M. C., Reece J. J., Urban J. F., Jr., Scott A. L. (2008) Dynamics of lung macrophage activation in response to helminth infection. J. Leukoc. Biol. 84, 1422–1433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haston C. K., Tomko T. G., Godin N., Kerckhoff L., Hallett M. T. (2005) Murine candidate bleomycin induced pulmonary fibrosis susceptibility genes identified by gene expression and sequence analysis of linkage regions. J. Med. Genet. 42, 464–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewis C. C., Aronow B., Hutton J., Santeliz J., Dienger K., Herman N., Finkelman F. D., Wills-Karp M. (2009) Unique and overlapping gene expression patterns driven by IL-4 and IL-13 in the mouse lung. J. Allergy Clin. Immunol. 123, 795–804e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sciuto A. M., Phillips C. S., Orzolek L. D., Hege A. I., Moran T. S., Dillman J. F., III (2005) Genomic analysis of murine pulmonary tissue following carbonyl chloride inhalation. Chem. Res. Toxicol. 18, 1654–1660 [DOI] [PubMed] [Google Scholar]
- 24.Auerbuch V., Brockstedt D. G., Meyer-Morse N., O′Riordan M., Portnoy D. A. (2004) Mice lacking the type I interferon receptor are resistant to Listeria monocytogenes. J. Exp. Med. 200, 527–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muller U., Steinhoff U., Reis L. F., Hemmi S., Pavlovic J., Zinkernagel R. M., Aguet M. (1994) Functional role of type I and type II interferons in antiviral defense. Science 264, 1918–1921 [DOI] [PubMed] [Google Scholar]
- 26.Yamamoto M., Takeda K., Akira S. (2004) TIR domain-containing adaptors define the specificity of TLR signaling. Mol. Immunol. 40, 861–868 [DOI] [PubMed] [Google Scholar]
- 27.Van Rijt L. S., Jung S., Kleinjan A., Vos N., Willart M., Duez C., Hoogsteden H. C., Lambrecht B. N. (2005) In vivo depletion of lung CD11c+ dendritic cells during allergen challenge abrogates the characteristic features of asthma. J. Exp. Med. 201, 981–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown M. S., Goldstein J. L. (1974) Suppression of 3-hydroxy-3-methylglutaryl coenzyme A reductase activity and inhibition of growth of human fibroblasts by 7-ketocholesterol. J. Biol. Chem. 249, 7306–7314 [PubMed] [Google Scholar]
- 29.Peet D. J., Turley S. D., Ma W., Janowski B. A., Lobaccaro J. M., Hammer R. E., Mangelsdorf D. J. (1998) Cholesterol and bile acid metabolism are impaired in mice lacking the nuclear oxysterol receptor LXR α. Cell 93, 693–704 [DOI] [PubMed] [Google Scholar]
- 30.Chen W., Chen G., Head D. L., Mangelsdorf D. J., Russell D. W. (2007) Enzymatic reduction of oxysterols impairs LXR signaling in cultured cells and the livers of mice. Cell Metab. 5, 73–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards P. A., Ericsson J. (1999) Sterols and isoprenoids: signaling molecules derived from the cholesterol biosynthetic pathway. Annu. Rev. Biochem. 68, 157–185 [DOI] [PubMed] [Google Scholar]
- 32.Bjorkhem I. (2009) Are side-chain oxidized oxysterols regulators also in vivo? J. Lipid Res. 50 (Suppl.), S213–S218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janowski B. A., Willy P. J., Devi T. R., Falck J. R., Mangelsdorf D. J. (1996) An oxysterol signaling pathway mediated by the nuclear receptor LXR α. Nature 383, 728–731 [DOI] [PubMed] [Google Scholar]
- 34.Fowler A. J., Sheu M. Y., Schmuth M., Kao J., Fluhr J. W., Rhein L., Collins J. L., Willson T. M., Mangelsdorf D. J., Elias P. M., Feingold K. R. (2003) Liver X receptor activators display anti-inflammatory activity in irritant and allergic contact dermatitis models: liver-X-receptor-specific inhibition of inflammation and primary cytokine production. J. Invest. Dermatol. 120, 246–255 [DOI] [PubMed] [Google Scholar]
- 35.Joseph S. B., McKilligin E., Pei L., Watson M. A., Collins A. R., Laffitte B. A., Chen M., Noh G., Goodman J., Hagger G. N., Tran J., Tippin T. K., Wang X., Lusis A. J., Hsueh W. A., Law R. E., Collins J. L., Willson T. M., Tontonoz P. (2002) Synthetic LXR ligand inhibits the development of atherosclerosis in mice. Proc. Natl. Acad. Sci. USA 99, 7604–7609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smoak K., Madenspacher J., Jeyaseelan S., Williams B., Dixon D., Poch K. R., Nick J. A., Worthen G. S., Fessler M. B. (2008) Effects of liver X receptor agonist treatment on pulmonary inflammation and host defense. J. Immunol. 180, 3305–3312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Birrell M. A., Catley M. C., Hardaker E., Wong S., Willson T. M., McCluskie K., Leonard T., Farrow S. N., Collins J. L., Haj-Yahia S., Belvisi M. G. (2007) Novel role for the liver X nuclear receptor in the suppression of lung inflammatory responses. J. Biol. Chem. 282, 31882–31890 [DOI] [PubMed] [Google Scholar]
- 38.Castrillo A., Joseph S. B., Marathe C., Mangelsdorf D. J., Tontonoz P. (2003) Liver X receptor-dependent repression of matrix metalloproteinase-9 expression in macrophages. J. Biol. Chem. 278, 10443–10449 [DOI] [PubMed] [Google Scholar]
- 39.Joseph S. B., Castrillo A., Laffitte B. A., Mangelsdorf D. J., Tontonoz P. (2003) Reciprocal regulation of inflammation and lipid metabolism by liver X receptors. Nat. Med. 9, 213–219 [DOI] [PubMed] [Google Scholar]
- 40.Geyeregger R., Zeyda M., Bauer W., Kriehuber E., Saemann M. D., Zlabinger G. J., Maurer D., Stulnig T. M. (2007) Liver X receptors regulate dendritic cell phenotype and function through blocked induction of the actin-bundling protein fascin. Blood 109, 4288–4295 [DOI] [PubMed] [Google Scholar]
- 41.Wada T., Kang H. S., Angers M., Gong H., Bhatia S., Khadem S., Ren S., Ellis E., Strom S. C., Jetten A. M., Xie W. (2008) Identification of oxysterol 7α-hydroxylase (Cyp7b1) as a novel retinoid-related orphan receptor α (RORα) (NR1F1) target gene and a functional cross-talk between RORα and liver X receptor (NR1H3). Mol. Pharmacol. 73, 891–899 [DOI] [PubMed] [Google Scholar]
- 42.Kato H., Horino A., Taneichi M., Fukuchi N., Eto Y., Ushijima H., Komuro K., Uchida T. (1998) Macrophage inhibition of lymphocyte and tumor cell growth is mediated by 25-hydroxycholesterol in the cell membrane. Int. Arch. Allergy Immunol. 117, 78–84 [DOI] [PubMed] [Google Scholar]