Abstract
Objective
To identify factors associated with perceptions of care coordination in a diverse sample of breast cancer patients.
Methods
Breast cancer patients reported to the metropolitan SEER registries of Detroit or Los Angeles from 6/05 to 2/07 were surveyed after diagnosis (N=2268, RR= 72.4%). Outcomes were two dichotomous measures reflecting patient appraisal of care coordination during their treatment experience. Primary independent variables were race/ethnicity (white, African American, Latina-high acculturated, Latina-low acculturated) and health literacy (low, moderate, high). Logistic regression was used to evaluate factors associated with both measures of care coordination.
Results
2,148 subjects were included in the analytic dataset. 16.4% of women perceived low care coordination and 12.5% reported low satisfaction. Race/ethnicity was not significantly associated with care coordination. Women with low subjective health literacy were 3–4 times as likely as those with high health literacy to perceive low care coordination and low satisfaction with care coordination (OR=3.88; 95% CI: 2.78–5.41; OR=3.19 95% CI:2.25–4.52, respectively).
Conclusions
Many breast cancer patients positively appraised their care coordination, but patients with low health literacy perceived low care coordination.
Practice Implications
Providers should be aware of health literacy deficits that may contribute to their patients’ attitudes towards their breast cancer care coordination.
Keywords: coordination of care, health literacy, breast cancer
1. Introduction
Breast cancer care has become increasingly complex in the United States. Patients are often faced with numerous treatment decisions, including surgery, radiation therapy, and chemotherapy, all of which usually involve consultation with different specialists. Optimal cancer care usually requires several physicians to work together in a coordinated fashion to communicate effectively to patients and deliver the best treatments [1–4]. Good care coordination also necessitates that patients have an accurate understanding about treatment and care management options [3,5–6]. Ensuring access to and use of coordinated breast cancer services has been identified as an important element of quality care [3–4; 6–7].
Several specific aspects of cancer care delivery may contribute to coordinated care, including: surgeon access to clinical information at the time of treatment consult, availability of multidisciplinary teams of providers, and comprehension of their treatment and management plan [1–4; 8–9]. Yet in one study surgeons in community based practices reported low utilization of or access to these elements [9]. Despite the focus on trying to improve care coordination, there is virtually no research evaluating how breast cancer patients themselves perceive the extent of care coordination they received during their treatment experience. In fact, because so few objective measures of this construct exist, the Agency for Healthcare Research and Quality (AHRQ) Report on Care Coordination has noted that patient perceptions may reflect the best measure of care coordination [10].
Moreover, specific patient populations, such as ethnic minorities and those of low educational attainment and/or literacy may be at risk for receiving poor care coordination due to difficulty in navigating the healthcare system and comprehending complex information [11–13]. While one study suggests that literacy may contribute to perceptions of low care coordination in colorectal cancer [14], there are no studies to date specifically evaluating this association. Although vulnerable patients, including ethnic minorities and those with low health literacy, may be those most likely to benefit from coordinated care, they have been largely omitted from research describing care coordination in the treatment of breast cancer.
To address these gaps in the literature, we sought to evaluate perceptions of care coordination in a large and diverse sample of breast cancer patients. Our study had two objectives: 1) to describe perceptions of care coordination among racially/ethnically diverse breast cancer patients, including perceived extent of care coordination and satisfaction with that coordination; and 2) to evaluate factors associated with breast cancer patients’ perceptions of their care coordination, focusing on race/ethnicity and health literacy. We hypothesized that factors previously associated with patterns of breast cancer treatment, including patient demographic and clinical factors [15–19], might also be associated with patient appraisal of their care coordination.
2. Methods
2.1. Study populations
We identified a population-based sample of women in the metropolitan areas of Los Angeles and Detroit aged 21–79 years diagnosed from June 2005 through February 2007 with primary ductal carcinoma in-situ (DCIS) or invasive breast cancer. Participants were recruited from the Surveillance, Epidemiology and End Results (SEER) program registries for the metropolitan areas of Detroit, Michigan and Los Angeles, California. Patients were excluded if they had Stage 4 breast cancer, had died prior to the survey, or could not complete a questionnaire in English or Spanish. African American and Latina patients were over-sampled by surveying all women whose race/ethnicity was African American according to the SEER data. Because Hispanic/Latina ethnicity is not always accurately collected by treating hospitals, we selected all women in Los Angeles who were designated as Hispanic in SEER and whose surname had a high probability of being Latina based on a list generated from the 1980 US Census [20]. We then selected an approximate 11% random sample of the remaining (non-Spanish surname) patients meeting eligibility criteria in Los Angeles and a random sample of approximately 67% of the remaining non-African American patients in Detroit. Asian women were not included since they were being enrolled in other studies. We identified all attending surgeons from patient report and pathology records.
2.2. Data collection and management
We notified the physician on record of our intent to contact his or her patient and allowed them the option to exclude any patient(s). Barring physician objection, eligible patients were mailed an introductory letter, a survey and return envelope, an informed consent form outlining the risks and benefits of participation, and a $10 gift. The Dillman method was then implemented to encourage survey completion which included follow up postcard reminders and a telephone reminder from a bilingual SEER staff member [21]. If needed, participants were mailed second copies of the survey materials and a telephone survey option was offered.
All Los Angeles patients who had a Spanish surname were mailed materials in both English and Spanish. The survey instrument was translated from English into Spanish by a native Spanish speaker and back-translated into English by another native Spanish speaker. Details regarding the identification of Latinas included in this study have been previously published [22]. Patient survey information merged with SEER clinical data and with a surgeon identifier. The study protocol, including all contact with human subjects, followed established SEER procedure and was approved by the Institutional Review Boards of the University of Michigan, the University of Southern California and Wayne State University.
2.3. Study sample and response rate
3252 patients were identified and potentially eligible. A total of 119 were excluded because the physician refused contact (n=20), the patient did not speak English or Spanish (n=17), the patient was too ill or not competent (n=59), or the patient did not acknowledge having breast cancer (n=23). Of the remaining 3133, 2268 responded (72.4% response rate). Of these, 96.5% completed the survey by mail and 3.5% by phone. Spanish speaking Latinas more often utilized the telephone option compared to other non Spanish speakers (6% vs. 2%). Half the surveys (50%) sent to those with Spanish surnames were returned or completed in Spanish [18]. Response rates were 73.5% for Latinas, 66.4% for African Americans, and 74.2% for whites (P<0.001). Compared with respondents, non-respondents were likely to have later stage disease (stage II or III vs. stage 0 or I, P<0.05) and were less likely to have received lumpectomy than mastectomy (P<0.02).
We identified attending surgeons for 98.9% of the patient sample (n=419 surgeons). Of the 2,268 patients in the final sample, complete data linked to surgeon identifiers was available for an analytic sample of 2,148 patients.
2.4. Measures
2.4.1. Primary outcome measures: breast cancer care coordination
We evaluated two self-reported measures of breast cancer care coordination: perceptions of care coordination and satisfaction with care coordination. The first consisted of a 5-tems scale designed to evaluate patient perceptions of the degree to which their breast cancer care was coordinated, while the second was a 1-item question designed to assess patients’ overall satisfaction with their care coordination. These items were developed based on the AHRQ report which provides suggested constructs care coordination [10]. The items were also informed by the cancer quality of care literature, which outlines key elements of multidisciplinary care [1–4, 23]. The 5 items included in the perceived care coordination scale were each rated on a 5-point Likert scale (1 = ‘never’; 5 = ‘always’): 1) How often did your surgeon(s) or their staff help you with referrals to other physicians for treatments such as radiation or chemotherapy? 2) How often did you know who to ask when you had questions about breast cancer or your treatment? 3) How often were you given confusing or contradictory information about breast cancer or your treatment? (item was reverse coded); 4) How often did you know what the next step in your treatment would be?; and 5) How often did your physicians have the medical information they needed to make decisions about your breast cancer treatment? The Cronbach’s coefficient was α = 0.67, which is considered acceptable [24].
For purposes of analyses, this variable was further categorized into two groups using a 75% cut point: low (never/rarely/sometimes = 1) perceived care coordination vs. high (often/always = 0). The one question used to assess overall satisfaction with care coordination was: Overall, how satisfied were you with how your physicians worked together (1 = ‘not at all’; 5 = ‘extremely’)? For analysis, we recoded satisfaction with care coordination into two groups using a 75% cut point, reflecting low satisfaction (not at all/a little/somewhat = 1) vs. higher satisfaction (very/extremely = 0).
2.4.2. Independent variables: patient characteristics
The primary independent variable for this analysis was self-reported patient race/ethnicity which was categorized into white, African American, and Latina. Latina participants were further categorized by level of acculturation using the Short Acculturation for Hispanics Scale (SASH) [25]. The SASH includes 5 questions that are largely based on the respondents’ language preference when reading, thinking or talking.). The SASH has been widely used to measure acculturation in Hispanic populations [26–27]. We used the recommended cut point to categorize Latina women into low vs. highly acculturated [25]. Prior work by our team provides extensive detail on the assessment of this measure and its validation against other constructs in our survey [22].
Other patient demographics obtained from the survey included age at diagnosis (continuous), educational attainment (high school degree or less vs. some college or more), income (annual household income of $50,000 or less, > $50,000, and a missing category), and insurance (Medicare/state coverage, employer/self-purchased/spouse, other, or none). Clinical factors included patient comorbidities obtained from the survey (0, 1 or 2+ chronic conditions), whether or not the patient reported having a clinical contraindication to breast conservation surgery (e.g., prior use of radiation, yes/no), and tumor stage obtained from the SEER data. These variables were chosen because of their association with patterns of treatment for breast cancer [15–19] and our hypothesis that they may also be associational with patient appraisal of care coordination.
2.4.3 Independent variable: health literacy
This measure was included based on research suggesting that health literacy is an important potential factor in receipt of coordinated services, regardless of race/ethnicity [11–14; 28]. Our health literacy measure was sell-reported and based on work by Chew and colleagues [28] who developed a 3-item measure of subjective health literacy by validating the self-reported items against existing measures such as the REALM. These 3 questions reflected how often patients had: (1) trouble understanding written information about breast cancer; (2) someone help them read written information; and (3) trouble filling out medical forms alone. Each question had a 5-point Likert response scale from 1 (always) to 5 (never). The individual items were averaged to yield an overall score (range = 1–5, Cronbach’s coefficient α = 0.63 [24]), with higher scores indicating higher levels of health literacy. This score was then categorized to create a 3-level measure of health literacy: low, moderate, and high, consistent with our prior work in this area [29].
2.5. Statistical analyses
We first described the characteristics of the patient sample. We next generated frequencies of all the independent variables, patient perceptions of care coordination and their satisfaction with care coordination. We evaluated associations between the two measures of coordination of care and patient characteristics using chi-square tests for categorical variables and t-tests for continuous variables. Sampling weights were applied to account for differential selection by race/ethnicity and non response.
Because of our a priori hypothesis that all independent variables might be associated with patient perceptions of and/or satisfaction with care coordination, all were included in the regression analysis regardless of bivariate results. We conducted logistic regression in a forward stepwise approach to evaluate factors associated with each measure of care coordination. Race/ethnicity was forced into each model. Model 1 for each outcome included all other demographics and clinical factors, and Model 2 additionally included our 3-level measure of health literacy. Wald chi-square statistics were used to assess associations between groups of variables (race/ethnicity and health literacy) and the outcomes. A two-sided p-value of <0.05 was considered statistically significant. Each model adjusted the standard errors for clustering of patients within surgeons [22]. In addition to logistic regression, we ran both models using Ordinary Least Squares regression using the ordinal outcome measure (perceived care coordination scale, range 5–25; satisfaction with care coordination question, range 1–5). These results were highly consistent with those from the logistic regression and thus the manuscript presents results from the logistic regression analysis. All analyses were conducted with STATA for Windows (Version 10.0, StataCorp, College Station, Texas).
3. Results
A minority of patients perceived having low care coordination (16.9%) or reported low satisfaction with care coordination (12.5%). There was a correlation coefficient of 0.47 between the two outcome variables. While 48.2% of those perceiving low coordination also reported low satisfaction, 51.8% of those perceiving low coordination did not report low satisfaction with these services. Table 1 provides the univariate statistics for both measures of care coordination, including the means and standard deviations for the individual items used in the perceived care coordination scale.
Table 1.
Description of outcome measures (N=2,148)
| Outcome measures | Sample N | Weighted % | Mean (SD), range |
|---|---|---|---|
| Perceived Care Coordination | 2,148 | 21.1 (XX), 5–25 | |
| Low | 363 | 16.9 | |
| High | 1,785 | 83.1 | |
| Perceived Care Coordination items | |||
| 1) How often did your surgeon(s) or their staff help you with referrals to other physicians for treatments such as radiation or chemotherapy? | 4.3 (1.3), 1–5 | ||
| 2) How often did you know who to ask when you had questions about breast cancer or your treatment? | 4.4 (0.9), 1–5 | ||
| 3) How often were you given confusing or contradictory information about breast cancer or your treatment? (item was reverse coded) | 1.7 (1.0), 1–5 | ||
| 4) How often did you know what the next step in your treatment would be? | 4.5 (0.8), 1–5 | ||
| 5) How often did your physicians have the medical information they needed to make decisions about your breast cancer treatment? | 4.7 (0.7), 1–5 | ||
| Satisfaction with Care Coordination: | 2,148 | 4.2 (0.9), 1–5 | |
| Overall, how satisfied were you with how your physicians worked together? | |||
| Low | 278 | 12.5 | |
| High | 1,870 | 87.5 | |
3.1. Patient characteristics
Using sampling weights, the sample was 67.4% white, 14.8% African American, 7.9% Latina-highly acculturated and 8.8% Latina-less acculturated (1.1% were of other race/ethnicity). Just over 15% of respondents had low health literacy, 28.6% had moderate levels of health literacy and most (55.5%) had high health literacy.
Most patients had relatively high levels of educational attainment with two-thirds (65%) having some college or a college degree. The mean age was 57 (SD 11.3). About half the patients (50.6%) reported an annual family income of over $50,000, and most had some type of insurance. Respondents were diagnosed with varying stages of cancer, but most had invasive (Stage I–III) breast cancer (76.6%). While 44.1% of women reported none of the chronic conditions presented, 28.4% reported having one and 27.4% reported two or more.
The bivariate analyses revealed that minority patients more often reported perceiving poor care coordination than their white counterparts (22.1% of less acculturated Latinas, 20.2% of highly acculturated Latinas, 17.2% of African Americans and 14.4% of white patients, P=0.17)), but there were no significant differences in the reports of satisfaction with care coordination by race/ethnicity. Patients with low subjective health literacy more often reported low perceived care coordination and low satisfaction with care coordination (Figure 1).
Figure 1.
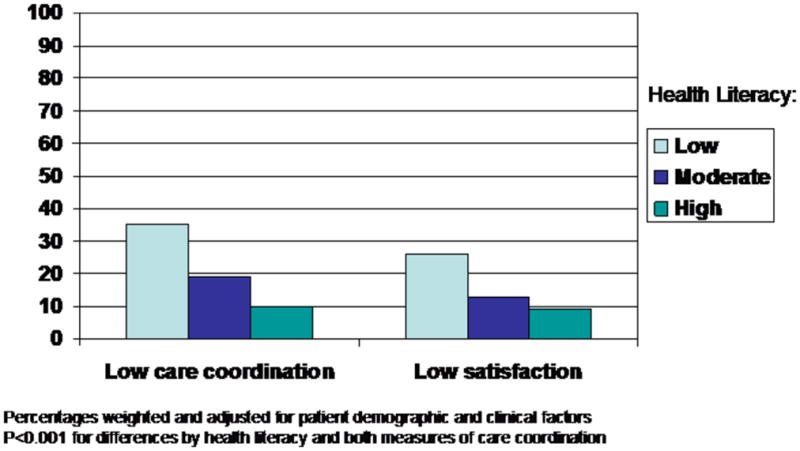
Care coordination perceptions by level of health literacy
Bivariate analyses also found some demographic factors (lower educational attainment, lower income and having no insurance) were significantly (P<0.05) associated with perceptions of low care coordination, while lower income and more comorbid conditions were associated (P<0.05) with low satisfaction with care coordination. Tumor stage was not associated with either measure of care coordination in the bivariate analysis. (results not shown).
3.2. Factors associated with patients’ perception of care coordination
Table 3 shows the logistic regression results for factors associated with low perceived care coordination. The table displays the results for all independent variables included in the model. All other factors included in the model that were not significantly associated with perceived care coordination are indicated in the footnote to the table.
Table 3.
Logistic regression: Factors associated with perceptions of low care coordination among racially/ethnically diverse breast cancer patients (N=2,148)
| Model 1 Adjusted OR (95% CI) | Model 2 Adjusted OR (95% CI) | |
|---|---|---|
| Age | 0.98 (0.97–0.99) | 0.98 (0.97–0.99) |
| Race/ethnicity | ||
| White | Referent | Referent |
| AA | 1.06 (0.77–1.46) | 1.06 (0.76–1.48) |
| Latina-low | 1.19 (0.78–1.83) | 0.86 (0.54–1.34) |
| Latina-high | 1.36 (0.94–1.98) | 1.38 (0.94–2.00) |
| other | 1.27 (0.60–2.68) | 1.23 (0.57–2.67) |
| Wald Test | Chi-sq=4.46, p=0.348 | Chi-sq=4.51; p=0.342 |
| Educational attainment | ||
| Some college or more | Referent | |
| High school or less | 0.64 (0.48–0.85) | 0.74 (0.55–0.98) |
| Annual family income | ||
| ≤ $50,000 | Referent | Referent |
| > $50,000 | 1.03 (0.66–1.59) | 0.99 (0.63–1.57) |
| Missing | 0.73 (0.46–1.14) | 0.77 (0.48–1.22) |
| Insurance | ||
| Medicare/state coverage | Referent | Referent |
| Employer/self/spouse coverage | 1.07 (0.60–1.91) | 1.14 (0.64–2.01) |
| Other | 1.04 (0.58–1.84) | 1.04 (0.62–1.09) |
| No coverage | 0.93 (0.46–1.87) | 0.98 (0.48–1.99) |
| Tumor behavior | ||
| Invasive | Referent | Referent |
| DCIS | 0.86 (0.66–1.13) | 0.82 (0.62–1.08) |
| Comorbid conditions | ||
| None | Referent | Referent |
| One | 0.97 (0.72–1.29) | 0.94 (0.91–1.74) |
| Two or more | 1.31 (0.95–1.77) | 1.26 (0.91–1.73) |
| Health literacy | ||
| High | Referent | |
| Moderate | 1.91 (1.44–2.55) | |
| Low | 3.88 (2.78–5.41) | |
| Wald Test | Chi-sq=65.26; p<0.001 | |
Standard errors are adjusted for clustering of patients within surgeons.
As seen in Model 1, race/ethnicity was not significantly associated with perception of low care coordination. Age was inversely associated with perceptions of low care coordination; older women were less likely to perceive low care coordination than younger women (OR: 0.98; 95% CI: 0.97–0.99). Educational attainment was also inversely associated with perceptions of care coordination; women with higher levels of education were less likely to perceive low care coordination than those with lower educational attainment (OR=0.64; 05% CI: 0.48–0.85). No other patient factors were associated with perceptions of care coordination.
Model 2 shows that the addition of health literacy to the model did not substantially change the results of Model 1. The association between education and perception of low care coordination was slightly attenuated by the inclusion of subjective health literacy, but remained statistically significant at p<0.05. Health literacy was independently and significantly associated with perception of low care coordination. Patients with moderate or low health literacy were significantly more likely to report low care coordination than those with high health literacy. In particular, those with low health literacy were almost 4 times as likely as those with high health literacy to report low care coordination (OR=3.88; 95% CI: 2.78–5.41).
3.3. Factors associated with patients’ satisfaction with coordination of care
Table 4 shows the same logistic regression models for low satisfaction with care coordination, with inclusion of all independent variables. Model 1 indicates that, as with perceptions of low care coordination, race/ethnicity was not significantly associated with low satisfaction with care coordination. Age was similarly inversely associated with satisfaction with care coordination; older women less often reported low satisfaction than younger women (OR=0.98; 95% CI: 0.97–0.99). In this model, having two or more comoribid conditions, compared to no comorbid conditions, was associated with low satisfaction with care coordination (OR=1.46; 95% CI: 1.02–2.11).
Table 4.
Logistic regression: Factors associated with low satisfaction with care coordination among racially/ethnically diverse breast cancer patients (N=2,148)
| Model 1 Adjusted OR (95% CI) | Model 2 Adjusted OR (95% CI) | |
|---|---|---|
| Age | 0.98 (0.97–0.99) | 0.98 (0.97–0.99) |
| Race/ethnicity | ||
| White | Referent | Referent |
| AA | 0.93 (0.66–1.31) | 0.94 (0.65–1.33) |
| Latina-low | 1.35 (0.85–2.13) | 1.02 (0.64–1.61) |
| Latina-high | 1.31 (0.87–1.96) | 1.35 (0.90–2.03) |
| other | 0.99 (0.42–2.33) | 1.00 (0.42–2.36) |
| Wald Test | Chi-sq=5.11; p=0.277 | Chi-sq=3.43; p=0.658 |
| Educational attainment | ||
| Some college or more | Referent | Referent |
| High school or less | 1.01 (0.75–1.36) | 1.20 (0.88–1.64) |
| Annual family income | ||
| ≤ $50,000 | Referent | Referent |
| > $50,000 | 1.32 (0.80–2.18) | 1.34 (0.79–2.27) |
| Missing | 0.89 (0.52–1.53) | 0.97 (0.55–1.69) |
| Insurance | ||
| Medicare/state coverage | Referent | Referent |
| Employer/self/spouse coverage | 1.12 (0.58–2.17) | 1.18 (0.61–2.29) |
| Other | 0.99 (0.53–1.89) | 1.00 (0.53–1.89) |
| No coverage | 0.79 (0.35–1.75) | 0.85 (0.39–1.88) |
| Tumor behavior | ||
| Invasive | Referent | Referent |
| DCIS | 1.36 (0.97–1.89) | 1.27 (0.91–1.77) |
| Number of comorbidities | ||
| None | Referent | Referent |
| One | 1.18 (0.84–1.65) | 1.18 (0.84–1.66) |
| Two or more | 1.47 (1.02–2.12) | 1.49 (1.03–2.15) |
| Health Literacy | ||
| High | Referent | |
| Moderate | 1.67 (1.22–2.26) | |
| Low | 3.19 (2.25–4.52) | |
| Wald Test | Chi-sq=42.95; p<0.001 | |
Standard errors are adjusted for clustering of patients within surgeons.
Model 2 shows that adding health literacy did not appreciably affect the associations observed in Model 1. As observed in the perceived low care coordination models (Table 2), patients with moderate or low subjective health literacy were significantly more likely than those with high health literacy to report low satisfaction with their care coordination. Again, those with low health literacy were substantially more likely than those with high health literacy to report low satisfaction (OR=3.19; 95% CI: 2.25–4.52)
Table 2.
Description of the patient sample (N=2,148)
| Demographics | ||
|---|---|---|
| Age | 2,148 | 57 (11.3) |
| Race/ethnicity | ||
| Latina-less acculturated | 285 | 8.8 |
| Latina-highly acculturated | 262 | 7.9 |
| African American | 581 | 14.8 |
| White | 974 | 67.4 |
| Other | 46 | 1.1 |
| Health literacy | ||
| Low | 342 | 15.9 |
| Moderate | 962 | 28.7 |
| High | 1,186 | 55.5 |
| Education | ||
| High school degree or less | 865 | 35.0 |
| Some college or more | 1,285 | 65.0 |
| Annual Family Income | ||
| ≤ $50,000 | 964 | 39.1 |
| > $50,000 | 1,006 | 50.6 |
| Missing | 178 | 10.3 |
| Insurance | ||
| None | 129 | 4.2 |
| Medicare/State coverage | 1,198 | 58.8 |
| Employer/Private/Spouse coverage | 636 | 27.9 |
| Other coverage | 158 | 9.1 |
| Clinical | ||
| Tumor Stage | ||
| Stage 0 (DCIS) | 419 | 19.1 |
| Stage I | 778 | 36.2 |
| Stage II | 655 | 30.3 |
| Stage III | 238 | 10.1 |
| Other/unknown | 58 | 2.7 |
| Cormorbid conditions | ||
| None | 931 | 44.1 |
| 1 | 585 | 28.4 |
| 2 or more | 632 | 27.4 |
4. Discussion
4.1. Discussion
There is a dearth of literature describing perceptions of care coordination in population-based samples of cancer patients with sufficient representation by race/ethnic minority groups. Prior research documenting low rates of care coordination has largely focused on other disease conditions [31–32], relied on small, qualitative studies [7,23], or has reported the impact of interventions on receipt of coordinated services [32–33]. The AHRQ has identified patient-reported perceptions as an important method for understanding more about how patients’ themselves appraise their treatment experiences.
To contribute to the literature, we evaluated correlates of patient perceptions of the degree of breast cancer care coordination they received, as well as their satisfaction with this coordination in a population-based sample of racially/ethnically and socioeconomically diverse breast cancer patients. We found that, overall, breast cancer patients positively appraised their care coordination, with relatively small proportions of patients perceiving low levels of care coordination or reporting low satisfaction with their care coordination. While this may seem like “good news” at a time when the management of breast cancer is becoming increasingly complex [6–7], we did find that some particularly vulnerable subgroups in our population did not perceive such a positive experience with the coordination of their care.
Perhaps the most concerning finding from this study was patients in our sample with low levels of subjective health literacy were between 3 and 4 times as likely as those with higher levels to report low coordination or low satisfaction. Those with moderate subjective health literacy also more often reported low coordination and low satisfaction. Little research has been done to evaluate care coordination in populations with varying levels of health literacy and/or educational attainment with which to compare our results. Our findings seem consistent, however, with the study by Ayanian and colleagues who found that non English-speaking white patients, assumed to have lower literacy, reported greater difficulty with the coordination of their care than other white patients [14]. They are also in line with prior work by our team showing those with low health literacy were most likely to report being dissatisfied with the information they received about breast cancer treatment, as well as with their treatment decision making process [29–30]. Together these results suggest that, even in settings where coordinated services may be available, there are populations that may be less able to take advantage of them.
We also found that younger women perceived lower levels of care coordination and satisfaction than older women. Women with lower educational attainment perceived low care coordination more often than their more highly educated counterparts, and women with two or more comorbid conditions had low satisfaction relative to those with none. Our finding that those with more comorbid conditions reported lower satisfaction with care coordination suggests that it may difficult to achieve high levels of care coordination for patients with additional complexities to the management of their treatment. This result is consistent with work by Gagliardi and colleagues [34] who found that from the surgeon perspective, patients with comorbid conditions presented significant care coordination challenges.
Addressing deficits in health literacy levels of patients has been identified as important for improving the quality of care for patients with a variety of conditions [13]. Low health literacy, as well as low educational attainment, limits the patients’ ability to comprehend treatment and care management information [11–13; 35], and can impede their ability to navigate the healthcare system [13; 34–36]. Low health literacy can also influence patient-provider communication, since patients may be less able to contribute to or understand treatment discussions [11,36]. Our results suggest that providers need to be more aware of potential health literacy deficits in their patients which could serve as a barrier to patients’ ability to capitalize on available services and/or navigate their care, particularly for a disease such as breast cancer for which there are a growing number of treatment management options. These results are consistent with the recommendations of others that simple and directed interventions, such as plain language materials should be used with low literacy patients [34–38]. Our findings would support the use of such materials, outlining the various steps in breast cancer treatment and management, as a possible method for improving perceptions of care coordination in these patients.
Our results must be considered in the context of some key limitations. The cross sectional design prevents us from inferring causality between variables and only allows us to evaluate associations between independent variables and our measures of care coordination. Although the importance of evaluating patient perceptions about care coordination has been highlighted nationally [10], both our outcome measures were self reported and may be subject to response bias. Our study may have also been subject to response bias because of the time delay between completion of our items and receipt of treatment (mean of 9 months). While we developed our measures based on recommendations about elements that should be part of coordinated care [9–10,23], we may have overlooked important aspects of care coordination by not including them in our measures. We were not able to validate these measures against objective assessments of care coordination and strongly feel additional research to conduct such validation is needed.
Although our analyses did account for the effects of individual surgeons, we could not fully account for additional practice or health system factors that could affect perceptions of coordination. Lastly, the locations of our study sample limit our ability to generalize these results to other geographic areas.
4.2. Conclusion
In general, patients with breast cancer appear to have positive attitudes towards the care coordination they received during their treatment experience. However, some patients, especially those with lower subjective health literacy, were less likely to perceive positive care coordination experiences. As well, those with lower education, more comorbid conditions and younger women, may more often perceived that their care was poorly coordinated than their counterparts. Efforts to understand more about how patient factors, such as low health literacy, impact patient perceptions of their treatment experiences are warranted.
4.3. Practice implications
Taken together, our results suggest that perceptions of poor care coordination may be highest among the more vulnerable patients groups, such as those with lower subjective health literacy. Providers should be aware that while many breast cancer patients report positive care coordination experiences, some groups, such as those with lower education, and those with more complicated management resulting from comorbidities may be at risk for perceiving lower levels of coordination.
Targeted research is needed to identify the specific barriers to coordination of care and the most successful intervention approaches for patients with low health literacy. Our results indicate that surgeons should be aware of deficits in health literacy and language that may put certain patients at high risk for perceiving poor care coordination, even in settings where coordinated services are available. Improving patients’ ability to navigate and comprehend their treatment and management plan may eventually translate into better outcomes for patients with breast cancer.
Acknowledgments
The collection of Los Angeles County cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the NCI’s Surveillance, Epidemiology and End Results (SEER) Program under contract N01-PC-35139 awarded to the University of Southern California, contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The collection of metropolitan Detroit cancer incidence data was supported by the NCI SEER Program contract N01-PC-35145. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the NCI, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
We acknowledge the out-standing work of our project staff: Barbara Salem, MS, MSW, Paul Abrahamse, MS, and Ashley Gay, BA (University of Michigan); Ain Boone, BA, Cathey Boyer, MSA, and Deborah Wilson, BA (Wayne State University); and Alma Acosta, Mary Lo, MS, Norma Caldera, Marlene Caldera, and Maria Isabel Gaeta, (University of Southern California), as well as the editorial assistance of Shan-san Wu, BA (Memorial Sloan-Kettering Cancer Center). All of these individuals received compensation for their assistance. We acknowledge Sarika Das, M.D., who contributed to initial outlines of the paper. We also acknowledge the breast cancer patients who responded to our survey. We thank the American College of Surgeons Commission on Cancer (David Winchester, MD, and Connie Bura) for their support of this research.
Footnotes
Conflict of Interest
The authors report no conflict of interest.
Authorship: All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hulvat MC, Hansen HM, Jeruss JS. Multidisciplinary care for patients with breast cancer. Surg Clin North Am. 2009;89:133–76. doi: 10.1016/j.suc.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Shuster TD, Girshovich L, Whitney TM, Hughes KS. Multidisciplinary care for patients with breast cancer. Surg Clin North Am. 2000;80:505–33. doi: 10.1016/s0039-6109(05)70199-7. [DOI] [PubMed] [Google Scholar]
- 3.Pruthi S, Boughey JC, Brandt KR, Degnim AC, Gy GK, Gotees MP, Perez EA, Reynolds CA, Schomberg PJ, Ingle JN. A multidisciplinary approach to the management of breast cancer, part 1: prevention and diagnosis. Mayo Clin Proc. 2007;82:999–1012. doi: 10.4065/82.8.999. [DOI] [PubMed] [Google Scholar]
- 4.Pruthi S, Boughey JC, Brandt KR, Degnim AC, Gy GK, Gotees MP, Perez EA, Reynolds CA, Schomberg PJ, Ingle JN. A multidisciplinary approach to the management of breast cancer, part 2: therapeutic considerations. Mayo Clin Proc. 2007;82:1131–40. doi: 10.4065/82.9.1131. [DOI] [PubMed] [Google Scholar]
- 5.O’Leary KA, Eastabrooks CA, Olson K, Cumming C. Information acquisition for women facing surgical treatment for breast cancer: influencing factors and selected outcomes. Patient Educ Couns. 2007;69:5–19. doi: 10.1016/j.pec.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Wolf SH, Chan ECY, Harris R, Sheridan SL, Braddock CH, Kaplan RM, Krist A, O’Connor AM, Tunis S. Promoting informed choice: transforming health care to dispense knowledge for decision making. Ann Int Med. 2005;143:293–300. doi: 10.7326/0003-4819-143-4-200508160-00010. [DOI] [PubMed] [Google Scholar]
- 7.Bickell NA, Young GJ. Coordination of care for early stage breast cancer patients. J Gen Intern Med. 2001;16:737–42. doi: 10.1111/j.1525-1497.2001.10130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh J, Young JM, Harrison JD, Butow PN, Solomon MN, Masya L, White K. What is important in cancer care coordination? A qualitative investigation. Eu J Cancer Care. 2010 doi: 10.1111/j.1365-2354.2010.01187.x. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Katz SJ, Hawley ST, Griggs JJ, Morrow M, Jagsi R, Friese C, Hamilton A, Graff J, Hofer T. Coordinating Cancer Care: Patient and Practice Management Processes Among Surgeons Who Treat Breast Cancer. Medical Care. 2010;48:45–51. doi: 10.1097/MLR.0b013e3181bd49ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonald KM, Dundaram V, Bravata DM, Lewis R, Lin N, Kraft S, et al., editors. Technical Review 9 (prepared by the Stanford University UCSF Evidence Based Practice Center under contract 290-02-0017) AHRQ publication no 04(07)-0051-7. Rockville, MD: Agency for Healthcare Research and Quality; Jun, 2007. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. [Google Scholar]
- 11.Amalraj S, Starkweather C, Nguyen C, Naeim A. Health literacy, communication and treatment decision making in older cancer patients. Oncology. 2009;23:369–75. [PubMed] [Google Scholar]
- 12.Oates DJ, Silliman RA. Health literacy: improving patient understanding. Oncology. 2009;23:376–9. [PubMed] [Google Scholar]
- 13.Nielsen-Bohlman Lynn, Panzer Allison M, Kindig David A., editors. Health Literacy: A Prescription to End Confusion. National Academies Press; Washington, DC: 2004. Committee on Health Literacy. [PubMed] [Google Scholar]
- 14.Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost KJ, Creech CM, Cress RD, O’Connor LC, West DW, Wright ME. Patients perceptions of quality of care for colorectal cancer by race, ethnicity and language. J Clin Oncol. 2005;23:6576–86. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 15.Lee MC, Rogers K, Griffith K, Diehl KA, Breslin TM, Cimmino VA, et al. Determinants of breast conservation rates: reasons for mastectomy at a comprehensive cancer center. Breast J. 2009;15:34–40. doi: 10.1111/j.1524-4741.2008.00668.x. [DOI] [PubMed] [Google Scholar]
- 16.Katz SJ, Lantz PM, Fagerlin A, Schwartz K, Liu L, Deapen D, et al. Patterns and correlates of local therapy for women with ductal carcinoma in situ. J Clin Oncol. 2005;23:3001–7. doi: 10.1200/JCO.2005.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith GL, Xu Y, Shih YC, Giordano SH, Smith BD, Hunt KK, et al. Breast conserving surgery in older patients with invasive breast cancer: current patterns of treatment across the United States. J Am Coll Surg. 2009;209:425–33. doi: 10.1016/j.jamcollsurg.2009.06.363. [DOI] [PubMed] [Google Scholar]
- 18.Jagsi R, Abrahamse P, Morrow M, Hawley ST, Griggs JJ, Graff JJ, et al. Patterns and correlates of adjuvant radiotherapy receipt after lumpectomy and after mastectomy for breast cancer. J Clin Oncol. 2010;28:2396–403. doi: 10.1200/JCO.2009.26.8433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States. J Clin Oncol. 2010 doi: 10.1200/JCO.2009.27.6774. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Katz SJ, Lantz PM, Zemenchuk J. Correlates of surgical treatment type for women with noninvasive and invasive breast cancer. J Women’s Health & Gender-based Medicine. 2001;10:659–70. doi: 10.1089/15246090152563533. [DOI] [PubMed] [Google Scholar]
- 21.Word D, Perkins JR. Technical Working Paper No. 13. U.S. Census Bureau; 1996. Building a Spanish surname list for the 1990’s—a new approach to an old problem. [Google Scholar]
- 22.Dillman DA. Mail and Telephone Surveys. New York: John Wiley and Sons, Inc; 1978. [Google Scholar]
- 23.Hamilton A, Hofer T, Hawley ST. Latinas and breast cancer outcomes: population based sampling, ethnic identity and acculturation assessment. Cancer Epidemiol Biomarkers Prev. 2009;18:2022–29. doi: 10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walsh JM, Harrison JD, Young JM, Butow PN, Solomon MJ, Masya L. What are the barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res. 2010;20:132. doi: 10.1186/1472-6963-10-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nunnally Jum C. Psychometric Theory. 1. New York: McGraw-Hill; 1967. [Google Scholar]
- 26.Marin G, Sabogal F, VanOss Marin B, Otero-Sabogal F, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 27.Mainous AG, Dias VA, Geesy ME. Acculturation and healthy lifestyle among Latinos with diabetes. Ann Fam Med. 2008;6:131–7. doi: 10.1370/afm.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larson KL, McQuiston C. Walking out of one culture into another: health concerns of early adolescent Latinos. J Sch Nurs. 2008;24:88–94. doi: 10.1177/10598405080240020701. [DOI] [PubMed] [Google Scholar]
- 29.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hawley ST, Janz NK, Hamilton A, Griggs JJ, Alderman A, Mujahid M, Katz SJ. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Educ Couns. 2008;73:363–70. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janz NK, Mujahid M, Hawley ST, Griggs JJ, Hamilton A, Katz SJ. Racial/ethnic disparities in the adequacy of information and support for women with breast cancer. Cancer. 2008;113:1058–67. doi: 10.1002/cncr.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary Care Physicians’ Links to Other Physicians Through Medicare Patients: The Scope of Care Coordination. Ann Int Med. 2009;150:236–42. doi: 10.7326/0003-4819-150-4-200902170-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chumbler NR, Vogel WB, Garel M, Haijing Q, Kobb R, Ryan P, Peikes D, Chen A, Schore J, Brown R. Health Services Utilization of a Care Coordination/Home-Telehealth Program for Veterans With Diabetes: A Matched-cohort. Effects of Care Coordination on Hospitalization, Quality of Care, and Health Care Expenditures Among Medicare Beneficiaries: results from 15 Randomized Trials. JAMA. 2009;301:603–618. [Google Scholar]
- 34.Gagliardi AR, Wright FC, Davis D, McLeod RS, Urbach DR. Challenges in multidisciplinary cancer care among general surgeons in Canada. BMC Med Dec Making. 2008;8:59–64. doi: 10.1186/1472-6947-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Apter AJ, Paasche-Orlow MK, Remillard JT, Bennett IM, Ben-Joseph EP, Batista RM, Hyde J, Rudd RE. Numeracy and communication with patients: they are counting on us. J Gen Intern Med. 2008;23:2117–24. doi: 10.1007/s11606-008-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safeer RS, Keenen J. Health literacy: the gap between physicians and patients. Am Fam Physician. 2005;72:463–8. [PubMed] [Google Scholar]
- 37.Agency for Healthcare Research and Quality. Navigating the health care system. [accessed on 10/31/09];What is your health literacy score? Advice from Carolyn M. Clancy, M.D. available online at: http://www.ahrq.gov/consumer/cc/cc052008.htm.
- 38.Protheroe J, Nutbeam D, Rowlands G. Health literacy: a necessary for increasing participation in health care. Br J Gen Pract. 2009;59:721–3. doi: 10.3399/bjgp09X472584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Osborne H. Health Literacy from A to Z: Practical Ways to Communicate your Health Message. Jones and Bartlett Publishers; Sudbury, MA: 2005. [Google Scholar]


