Abstract
We retrospectively studied the cases with tuberculous spondylitis of thoracolumbar region with two or more levels of involvement that underwent posterior instrumentation and fusion and anterior fusion with titanium mesh following anterior decompression using simultaneous successive posterior–anterior–posterior surgery. Among all patients with tuberculous spondylitis accompanied by medium or severe kyphosis, 20 patients who underwent simultaneous successive decompression, fusion and instrumentation with posterior–anterior–posterior surgery between 1999 and 2004 were included in the study. Patients were evaluated for fusion formation and neurological and functional status. Kyphosis angles were measured at early and long-term follow-up. Antituberculosis chemotherapy was initiated in all patients and continued for 9 months; initially as quadruple therapy for 3 months, and then as triple therapy. Average follow-up period was 52.7 months (range 37–94). Solid fusion was achieved in all patients. All patients returned to their previous occupation; 75% (15 subjects) with mild pain or no pain and 15% (3 subjects) with major limitations. There were 11 patients with neurological deficit, 9 of these achieved complete neurological recoveries. Regarding kyphosis angle, an average 35.1° correction (84.8%) was obtained in postoperative period (p < 0.001) and there was no significant correction loss during the follow-up period (p < 0.05). There were no grafts or instrumentation-related stabilization problems. In subjects with tuberculous spondylitis with involvements at two or more levels accompanied by medium and severe kyphosis, decompression, fusion and instrumentation by simultaneous successive posterior–anterior–posterior surgery is an effective and safe management method for effective kyphosis correction with high fusion rates.
Keywords: Tuberculous spondylitis, Surgical treatment, Simultaneous successive posterior–anterior–posterior surgery, Kyphosis
Introduction
The incidence of tuberculosis varies with economic development conditions of the countries. The frequency of the disease is closely related to the patient’s social, economical and education status [13]. Today, the frequency of tuberculosis infection increased particularly due to immune deficiency caused by HIV virus and drug-resistant tuberculosis strains have emerged [11, 19, 23].
Paraplegia and kyphotic deformity development are two major disease-related problems. The aims of treatment are to eradicate the disease and also to prevent the development of paraplegia and kyphotic deformity and if exists, to manage the pathological picture [9, 11, 20, 23]. Active disease can be eradicated by efficient chemotherapy [20, 21, 30, 32]. However, chemotherapy alone or long periods of bed rest or external supports combined with chemotherapy may not be effective in the prevention of paraplegia and kyphosis [20, 22, 26]. The British Medical Research Council recommended that spinal tuberculosis is best treated by specialist surgeons and by chemotherapy and radical anterior intervention under appropriate conditions [20, 30]. The kyphotic correction and cord decompression achieved by radical anterior intervention as described by Hodgson and Stock may be under risk with the collapses, breaks or insufficiency problems that may result resorption in the grafts used [12, 22, 26, 29]. The reinforcement of correction performed in kyphotic deformity with posterior or anterior instrumentation prevents the collapse or breakdown of the graft, decreases pseudoarthrosis rate, and allows early ambulation and rehabilitation [1, 2, 6, 9, 12, 15, 16, 22, 25, 26, 29, 31, 33].
In this study, we retrospectively evaluated the results of anterior decompression–fusion using titanium mesh cage combined with posterior instrumentation and fusion by simultaneous successive posterior–anterior–posterior approach in tuberculous spondylitis with two or more levels of involvement accompanied by medium and severe kyphosis requiring surgical treatment.
Materials and methods
Between 1999 and 2006, 26 patients underwent surgical decompression, correction and 360° fusion via simultaneous posterior–anterior–posterior technique. Twenty of these patients were included in the study, and six were excluded because they were not reached by telephone to be called for final evaluation. Twelve subjects were male and eight were female. The mean age was 41.35 (range 12–69). Eleven (55%) subjects had neurological deficits (Table 1). Frankel Scoring System was used to assess the neurological status [7]. Two subjects (10%) were treated for active pulmonary tuberculosis. All subjects were screened by direct radiography, CT and MRI for involvement due to vertebral infection. Eight patients had involvement of two vertebral body levels, nine had three levels of involvement, and three had four levels of involvement. Kyphotic deformity was present in all subjects and the average kyphosis angle was 41.35° (range 25–70) (Table 1).
Table 1.
Patient data
| Gender | Age | Neurological gradea | No. of affected segments | Preop. kyphosis angle | Postop. neurological gradea | Postop kyphosis angle | Fusion time (months) | Follow-up period (months) | Kyphosis angle following Follow-up period | Functional outcomea | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 32 | E | T12–L2 | 72 | E | 20 | 6 | 55 | 22 | E |
| 2 | F | 63 | D | L1–L3 | 38 | E | −5 | 5 | 38 | −5 | E |
| 3 | M | 50 | C | T11–T12 | 31 | D | 5 | 9 | 57 | 5 | G |
| 4 | M | 22 | D | T10–T12 | 55 | E | 18 | 7 | 45 | 20 | E |
| 5 | M | 12 | E | L2–L3 | 25 | E | −10 | 4 | 70 | −8 | E |
| 6 | F | 18 | E | L1–L2 | 25 | E | −5 | 13 | 46 | −4 | E |
| 7 | F | 45 | E | T10–T12 | 38 | E | 10 | 8 | 42 | 10 | E |
| 8 | M | 64 | B | T11–L2 | 40 | B | 5 | 6 | 37 | 5 | F |
| 9 | F | 28 | E | T9–T11 | 35 | E | 15 | 5 | 39 | 15 | E |
| 10 | M | 56 | C | L1–L2 | 20 | E | −8 | 10 | 64 | −7 | E |
| 11 | M | 67 | D | T11–T12 | 45 | E | 10 | 8 | 41 | 10 | E |
| 12 | M | 34 | E | T10–L1 | 36 | E | 14 | 6 | 40 | 15 | E |
| 13 | M | 42 | D | T11–L1 | 57 | E | 15 | 5 | 39 | 16 | E |
| 14 | F | 69 | B | L1–L2 | 25 | E | −10 | 9 | 38 | −8 | E |
| 15 | M | 40 | D | T10–L2 | 62 | E | 15 | 6 | 67 | 15 | E |
| 16 | M | 29 | E | T11–L1 | 42 | E | 12 | 8 | 80 | 12 | E |
| 17 | F | 35 | E | T12–L1 | 37 | E | 10 | 7 | 65 | 11 | E |
| 18 | F | 28 | D | T11–L2 | 44 | E | 5 | 8 | 47 | 5 | E |
| 19 | M | 42 | E | T10–L1 | 52 | E | 14 | 9 | 50 | 15 | E |
| 20 | F | 51 | D | T12–L1 | 28 | E | −5 | 6 | 94 | −3 | E |
aNeurological grade evaluated according to Frankel et al. [7]
Surgery was indicated in cases of waist and back pain that did not resolve with conservative therapy methods, neurological deficits, progressive kyphosis and instability. All patients underwent simultaneous successive posterior–anterior–posterior surgery. Microbiological examination of tissue and abscess samples obtained during operation had growth of M. tuberculosis bacilli in 12 subjects. Diagnosis of tuberculous spondylitis was verified by histopathological evaluation in all subjects. Subjects received antituberculosis chemotherapy for 9 months (3 months of INH–rifampicin–pyrazinamide–streptomycin therapy, followed by 6-month INH–rifampicin–pyrazinamide therapy).
In the last visit, patients were evaluated for pain and functional status using the scale recommended by Denis et al. (Table 2) [3]. Kyphosis angles were measured in the preoperative, postoperative and follow-up periods and were examined statistically. Kyphosis angles were calculated by measuring the angle between longitudinal lines passing through the endplates of the lower and upper vertebrae. Statistical analysis was performed using “paired t” test according to two-way p values (Tables 3, 4). Fusion development was assessed with plain radiographs; we did not use CT reconstructions routinely. The fusion development can be assessed by observing the regression or progression of the clinical findings. Neurological condition was observed at follow-up visits.
Table 2.
Scale used for assessment of pain and function
| Assessment of pain | Grade | Assessment of function |
|---|---|---|
| No pain | 0 | Returning to previous occupation |
| Intermittent pain not requiring analgesics | 1 | Returning to previous occupation or daily activities with mild limitations |
| Frequent mild pain occasionally requiring non-narcotic analgesics | 2 | Returning to previous occupation or daily activities with major limitations |
| Infrequent moderate pain requiring analgesics | 3 | Not completely returning to previous occupation and daily activities and needing energy saving life style |
| Intense pain occasionally requiring narcotic analgesics | 4 | Significant loss of function, limitations even in routine daily activities |
| Very intense pain requiring regular narcotic analgesic intake | 5 | Complete loss of function |
Table 3.
Statistical analysis of preoperative and postoperative measurements of kyphosis angle
| Preop. kyphosis angle | Postop. kyphosis angle | |
|---|---|---|
| Mean | 40.35 | 6.25 |
| SD | 13.701 | 9.915 |
| SEM | 3.064 | 2.217 |
| p | <0.001 | |
Table 4.
Statistical analysis of postoperative and post follow-up measurements of kyphosis angle
| Postoperative kyphosis angle | Post follow-up kyphosis angle | |
|---|---|---|
| Mean | 6.25 | 7.05 |
| SD | 9.915 | 9.768 |
| SEM | 2.217 | 2.184 |
| p | 0.7985 | |
Surgical technique
Patients were positioned in prone position which allows posterior exposure. Bilateral pedicle screws were inserted at two or three upper and two or three lower segments from the lesion level (Medtronic, Stryker, Evrevmed, Tasarımmed). Rods were placed without correcting the existing kyphosis for temporary fixation. Subcutis and skin were closed and patient was placed in lateral position. Abscess was drained through anterior exposure on the right side of patients who would undergo thoracotomy and through anterior exposure on the left side in patients who would undergo surgery via thoracoabdominal approach. Sequestered bone fragments of affected vertebrae were removed through corpectomy. Decompression was carried out until dura mater was visible through anterior approach, so all affected vertebrae were extracted. Then, posterior incision was opened again and the rods were removed. To correct the kyphotic deformity, a titanium mesh cage (medtronic-pyramesh) filled with spongious chips allograft was placed in anterior corpectomy site. Giving an appropriate contour, rods were placed via posterior approach and the system was locked. Posterior fusion was complemented with allograft chips and the operation was completed (Figs. 1, 2, 3, 4).
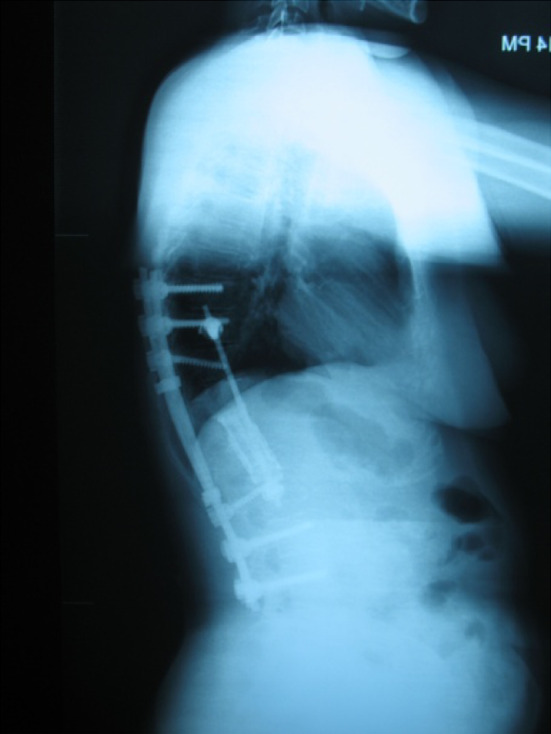
Fig. 1.
Preoperative AP radiograph of 32-year-old female patient
Fig. 2.
Preoperative lateral radiograph of 32-year-old female patient
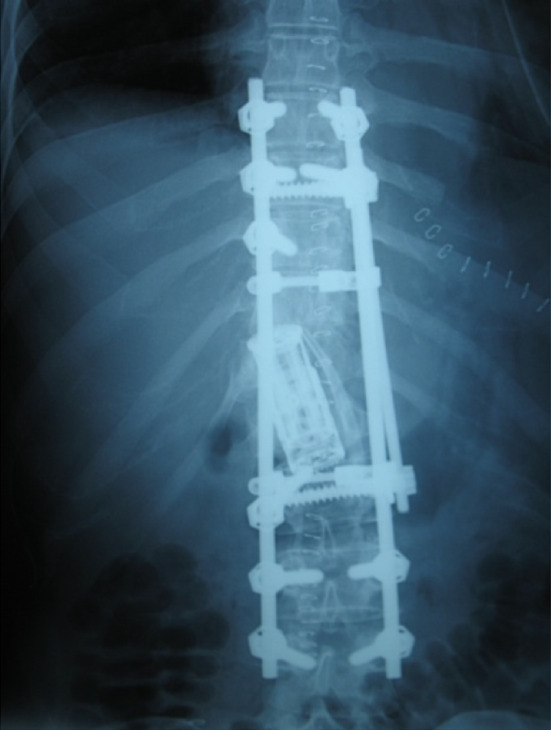
Fig. 3.

+94-month follow-up AP radiograph of the same patient
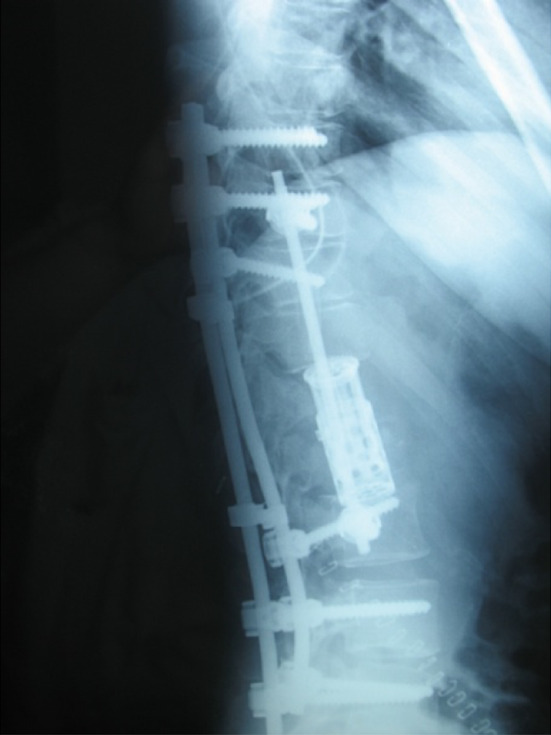
Fig. 4.
+94-month follow-up lateral radiograph of the same patient
Results
Average hospitalization period prior to operation was 15.2 days (range 3–26) and 7.3 days (range 5–18) after the operation. After the operation, all patients were observed in the intensive care unit for an average of 2.12 (range 1–4) days. Mean blood loss was found to be 340 (range 250–460) cc. After weeks 3 and 6, the patients were called for examination and radiological investigation in weeks 3, 6 and 12 in the first year, and subsequently once in 12 months. Average follow-up period was 52.7 months (range 37–94).
Among all operated patients, 75% returned to their previous occupation (15 subjects) with mild pain or no pain, 15% (3 subjects) with major limitations. Ten percent (2 subjects) of the patients whose neurological deficits showed no improvement could not return to their previous occupation because of functional insufficiency. Among 17 patients who were completely able to return to their previous occupations, 10 had sedentary and 7 had tough working conditions. Patients who partially returned to their previous occupations were a wall painter, a bus driver and ship worker. Follow-up radiographies proved that solid fusion was achieved in all subjects. Average fusion period was 7.25 months (range 5–13). None of the patients had radiologic findings of failure in posterior fusion (screw loosening, screw or rod breakage, cage subsidence, etc.) and none reported any clinical complaints regarding failure of posterior fusion or instrumentation. Therefore, further studies for radiologic evaluation of anterior fusion were not carried out. In our opinion, regression of the clinical findings like pain and disability shows that the fusion was developed. In 11 subjects with neurological deficit, 9 showed complete neurological recovery. One subject with an initial Frankel C classification recovered to Frankel D but one patient with Frankel B showed no recovery (Table 1).
Kyphosis angle showed a correction of average 35.1° (84.8%) in the postoperative period (p < 0.001) and there was no significant correction loss at the end of follow-up period (p > 0.05) (Tables 3, 4).
No stabilization problems associated with grafting or instrumentation were encountered. In the postoperative period, superficial wound infection in one patient was treated with debridement and antibiotic therapy. No patients showed recurrence of tuberculosis infection.
Discussion
The aims of spinal tuberculosis treatment are to eradicate the disease, to prevent the development of paraplegia and kyphotic deformity, to manage the existing deformity and neurological deficit, to allow early ambulation and to return the patient back to daily life [9, 11, 13, 19, 20, 23].
Methods for the treatment of tuberculosis of vertebra are still controversial. Chemotherapy is a very effective way of controlling and treating the disease and is an indispensable treatment strategy [9, 20, 30]. Conservative treatment includes medical therapy as well as external supports such as bed rest and/or full body plaster immobilization or body braces. Conservative management is indicated for mild to moderate form of the disease if there is no marked abscess formation, spinal deformity and collapse or neural and vertebral instability [20, 21, 30]. Conservative treatment has been shown to be successful in various reports, despite the evidence of progressive kyphosis, neurological deficit and union delay [32]. Working on treatment strategies since 1963, The British Medical Research Council Tuberculosis Units (MRC) have been studying spondylitis patients treated with immobilization and chemotherapy or with chemotherapy alone or with anterior surgery. They concluded that best results are achieved in the group treated with anterior resection, debridement and fusion using autogenous bone grafts (Hong Kong procedure) [20, 30]. Anterior debridement and arthrodesis allow reaching the focal point of the disease directly, effective debridement of the focal point, rapid bony union with the grafts and prevent progressive collapse and kyphosis [12, 20, 21, 30, 32]. However, it has been reported that such successful outcomes are not observed regarding progressive collapse and kyphosis, particularly in the case of two or more levels of involvement, risks of graft insufficiency and increased kyphotic deformity [1, 3, 9, 11, 15, 23, 25]. Moon et al. stated that interbody fusion performed with classical anterior radical surgery per se in ineffective in the correction of kyphosis. Moon [22] suggests that in addition to its failure in some cases to correct the existing kyphosis, anterior arthrodesis does not prevent the increase in kyphosis angle. Rajasekaran et al. [26] also reported a progression in kyphosis particularly in anterior arthrodesis at two or more levels and recommended additional stabilization methods.
The reported drawbacks of anterior radical surgery suggest that anterior arthrodesis combined with anterior or posterior instrumentation may be useful to maintain the correction achieved [1, 6, 8, 14–17, 25, 26, 29, 31]. Studies have shown that implants can be safely used in tuberculosis infections. In their study on stainless steel, Oga et al. [24] reported that M. tuberculosis has low adhesion capability and forms only a few microcolonies surrounded by a biofilm. Benli et al., Yılmaz et al. and Jin et al. [1, 14, 33] showed that anterior implant can be safely used in tuberculous spondylitis. Liljenqvist et al. and Hee et al. [10, 18] reported the titanium mesh cage to be safe in vertebral osteomyelitis. Studies showed that anterior arm can be efficiently reconstructed, existing kyphotic deformities can be safely corrected and complications due to grafts alone can be avoided in subjects in whom thoracolumbar corpectomy using titanium mesh cage was performed [4, 5, 27]. There is inadequate literature regarding the safety of titanium cage in tuberculosis infections. The demonstration of the lack of any negative effect of titanium cage in the treatment of infection, and also the demonstration of its efficacy in anterior support with respect to mechanical stability are significant findings of our study.
In the literature, there are many studies showing that in addition to anterior debridement and arthrodesis, anterior or posterior stabilization is an effective method for correcting the existing kyphosis and maintaining the correction achieved [1, 6, 8, 14–17, 25, 26, 29, 31]. It is clear that posterior instrumentation is more effective in kyphosis correction and prevention of late-term progression especially in kyphosis with two or more levels of involvement or in moderate or severe kyphosis [12, 15, 17, 26, 29]. In a study, Wen-Jer et al. [31] has obtained 56% kyphosis correction with two-stage anterior–posterior surgery and reported 3° of correction loss during the follow-up period. Moon et al. [22] suggested that posterior surgery was useful for early control of the disease, early fusion and prevention of kyphosis progression. Safran et al. [28] showed that anterior decompression and posterior stabilization at the same day was an effective and safe method of controlling the disease and stabilization of the affected segments. Klockner et al. [16] suggested that posterior instrumentation should be combined with anterior debridement and fusion in deformities affecting many levels and/or in excessive kyphotic deformities. Laheri et al. [17] achieved 62.5% correction performing costotransversectomy and decompression, anterior interbody fusion and posterior instrumentation at the same stage in patients with kyphosis due to tuberculosis with dorsolumbar involvement and reported an average of 3.2° correction loss in kyphosis angle following 5.8 years of follow-up period.
In our study, kyphosis correction in the early postoperative period was 84.8% and there was no significant loss during follow-up period (Table 3). This value is above the rates reported in literature.
In conclusion, we suggest that 360° spinal fusion method using posterior–anterior–posterior titanium mesh cage and posterior instrumentation in tuberculosis spondylitis affecting two or more levels accompanied by moderate or severe kyphosis that requires surgery, achieves kyphosis correction comparable to normal anatomic degrees, allows efficient stabilization and early mobilization, and is effective in maintenance of the correction achieved.
References
- 1.Benli IT, Acaroglu E, Akalin S, Kis M, Duman E, Un A. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12:224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res. 2002;398:50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Armstrong GWD, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit a comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984;189:125–141. [PubMed] [Google Scholar]
- 4.Dvorak MF, Kwon BK, Fisher CG, Eiserloh HL, 3rd, Boyd M, Wing PC. Effectiveness of titanium mesh cylindrical cages in anterior column reconstruction after thoracic and lumbar vertebral body resection. Spine. 2003;28:902–908. doi: 10.1097/00007632-200305010-00012. [DOI] [PubMed] [Google Scholar]
- 5.Eck KR, Bridwell KH, Ungacta FF, Lapp MA, Lenke LG, Riew KD. Analysis of titanium mesh cages in adults with minimum two-year follow-up. Spine. 2000;25:2407–2415. doi: 10.1097/00007632-200009150-00023. [DOI] [PubMed] [Google Scholar]
- 6.Faraj AA. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Jt Surg (Am) 2001;83:463–464. doi: 10.2106/00004623-200103000-00027. [DOI] [PubMed] [Google Scholar]
- 7.Frankel HL, Hancock DO, Hyskop G. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 8.Fukuta S, Miyamoto K, Masuda T, Hosoe H, Kodama H, Nishimoto H, Sakaeda H, Shimizu K. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine. 2003;28:302–308. doi: 10.1097/00007632-200308010-00025. [DOI] [PubMed] [Google Scholar]
- 9.Hamzaoğlu A (1999) Granulomatous infection of the spine. In: Floman Y (ed) State of the art reviews, spinal infections. Hanley and Belfus, Philadelphia, pp 45–78
- 10.Hee HT, Majd ME, Holt RT, Pienkowski D. Better treatment of vertebral osteomyelitis using posterior stabilization and titanium mesh cages. J Spinal Disord Tech. 2002;15:149–156. doi: 10.1097/00024720-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Hilibrand AS, Quartararo LG, Moulton MRJ (2003) Spinal infections. In: Koval KJ (ed) Orthopaedic knowledge uptake 7. American Academy of Orthopaedic Surgeons, pp 661–672
- 12.Hodgson AR, Stock FE. Anterior spinal fusion: preliminary communication on radical treatment of Pott’s disease and Pott’s paraplegia. Clin Orthop Relat Res. 1994;300:16–23. [PubMed] [Google Scholar]
- 13.Janssens JP, de Haller R. Spinal tuberculosis in a developed country. A review of 26 cases with special emphasis on abscesses and neurologic complications. Clin Orthop Relat Res. 1990;257:67–75. [PubMed] [Google Scholar]
- 14.Jin D, Qu D, Chen J, Zhang H. One-stage anterior interbody autografting and instrumentation in primary surgical management of thoracolumbar spinal tuberculosis. Eur Spine J. 2004;13:114–121. doi: 10.1007/s00586-003-0661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim DJ, Yun YH, Moon SH, Riew KD. Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine. 2004;29:275–279. doi: 10.1097/01.BRS.0000129027.68574.06. [DOI] [PubMed] [Google Scholar]
- 16.Klockner C, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine. 2003;15:1036–1042. doi: 10.1097/00007632-200305150-00016. [DOI] [PubMed] [Google Scholar]
- 17.Laheri VJ, Badhe NP, Dewnany GT. Single stage decompression, anterior interbody fusion and posterior instrumentation for tuberculous kyphosis of the dorso-lumbar spine. Spinal Cord. 2001;39:429–436. doi: 10.1038/sj.sc.3101185. [DOI] [PubMed] [Google Scholar]
- 18.Liljenqvist U, Lerner T, Bullmann V, Hackenberg L, Halm H, Winkelmann W. Titanium cages in the surgical treatment of severe vertebral osteomyelitis. Eur Spine J. 2003;12:606–612. doi: 10.1007/s00586-003-0614-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luk KD. Tuberculosis of the spine in the new millennium. Eur Spine J. 1999;8:338–345. doi: 10.1007/s005860050185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medical Research Council Working Party On Tuberculosis of the Spine A 10-year assessments of controlled trials comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong-Kong. J Bone Jt Surg (Br) 1982;64:393–398. doi: 10.1302/0301-620X.64B4.7047536. [DOI] [PubMed] [Google Scholar]
- 21.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Moon MS, Woo YK, Lee KS, et al. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spine. Spine. 1995;20:1910–1916. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Moon MS. Spine update. Tuberculosis of the spine: controversies and new challenge. Spine. 1997;22:1791–1797. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 24.Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine. 1993;18:1890–1894. doi: 10.1097/00007632-199310000-00028. [DOI] [PubMed] [Google Scholar]
- 25.Ozdemir M, Us K, Ogun T. The role of anterior spinal instrumentation and allograft fibula for treatment of Pott disease. Spine. 2003;28:474–479. doi: 10.1097/00007632-200303010-00012. [DOI] [PubMed] [Google Scholar]
- 26.Rajasekaran S, Soundarapandian S. Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Jt Surg (Am) 1989;71:1314–1323. [PubMed] [Google Scholar]
- 27.Robertson PA, Rawlinson HJ, Hadlow AT. Radiologic stability of titanium mesh cages for anterior spinal reconstruction following thoracolumbar corpectomy. J Spinal Disord Tech. 2004;17:44–52. doi: 10.1097/00024720-200402000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Safran O, Rand N, Kaplan L, Sagiv S, Floman Y. Sequential or simultaneous, same-day anterior decompression and posterior stabilization in the management of vertebral osteomyelitis of the lumbar spine. Spine. 1998;23:1885–1890. doi: 10.1097/00007632-199809010-00018. [DOI] [PubMed] [Google Scholar]
- 29.Sundararaj GD, Behera S, Ravi V, Venkatesh K, Cherian VM, Lee V. Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Jt Surg (Br) 2003;85:100–106. doi: 10.1302/0301-620X.85B1.13300. [DOI] [PubMed] [Google Scholar]
- 30.Thirteenth Report Of The Medical Research Council Working Party On Tuberculosis Of The Spine A 15-year assessment of controlled trials of the management of tuberculosis of the spine in Korea and Hong Kong. J Bone Jt Surg (Br) 1998;80:456–462. doi: 10.1302/0301-620X.80B3.8544. [DOI] [PubMed] [Google Scholar]
- 31.Wen-Jer C, Chi-Chuan W, Chi-Hsiung J. Combined anterior and posterior surgeries in the treatment of tuberculous spondylitis. Clin Orthop Relat Res. 2002;398:50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Wimmer C, Ogon M, Sterzinger W, Landauer F, Stockl B. Conservative treatment of tuberculous spondylitis: a long-term follow-up study. J Spinal Disord. 1997;10:417–419. doi: 10.1097/00002517-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Yilmaz C, Selek HY, Gurkan I, Erdemli B, Korkusuz Z. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Jt Surg (Am) 1999;81:1261–1267. doi: 10.2106/00004623-199909000-00007. [DOI] [PubMed] [Google Scholar]


