Abstract
The SWISSspine registry is the first mandatory registry of its kind in the history of Swiss orthopaedics and it follows the principle of “coverage with evidence development”. Its goal is the generation of evidence for a decision by the Swiss federal office of health about reimbursement of the concerned technologies and treatments by the basic health insurance of Switzerland. Recently, developed and clinically implemented, the Dynardi total disc arthroplasty (TDA) accounted for 10% of the implanted lumbar TDAs in the registry. We compared the outcomes of patients treated with Dynardi to those of the recipients of the other TDAs in the registry. Between March 2005 and October 2009, 483 patients with single-level TDA were documented in the registry. The 52 patients with a single Dynardi lumbar disc prosthesis implanted by two surgeons (CE and OS) were compared to the 431 patients who received one of the other prostheses. Data were collected in a prospective, observational multicenter mode. Surgery, implant, 3-month, 1-year, and 2-year follow-up forms as well as comorbidity, NASS and EQ-5D questionnaires were collected. For statistical analyses, the Wilcoxon signed-rank test and chi-square test were used. Multivariate regression analyses were also performed. Significant and clinically relevant reduction of low back pain and leg pain as well as improvement in quality of life was seen in both groups (P < 0.001 postop vs. preop). There were no inter-group differences regarding postoperative pain levels, intraoperative and follow-up complications or revision procedures with a new hospitalization. However, significantly more Dynardi patients achieved a minimum clinically relevant low back pain alleviation of 18 VAS points and a quality of life improvement of 0.25 EQ-5D points. The patients with Dynardi prosthesis showed a similar outcome to patients receiving the other TDAs in terms of postoperative low back and leg pain, complications, and revision procedures. A higher likelihood for achieving a minimum clinically relevant improvement of low back pain and quality of life in Dynardi patients was observed. This difference might be due to the large number of surgeons using other TDAs compared to only two surgeons using the Dynardi TDA, with corresponding variations in patient selection, patient-physician interaction and other factors, which cannot be assessed in a registry study.
Keywords: Dynardi, Total disc arthroplasty, Health technology assessment, Registry, Outcome
Introduction
The SWISSspine registry on cervical and lumbar disc prostheses has recently been introduced [1, 2]. Total disc arthroplasty (TDA) is an alternative concept for the treatment of degenerative disc disease (DDD). However, in an environment of increasingly scarce healthcare funds, costly innovations are more thoroughly scrutinized regarding their comparative effectiveness. As a governmentally mandated national registry, SWISSspine assesses aspects of safety and efficacy of TDA to complement conventional sources of evidence in the literature. Based on the acquired national and international results, the Swiss Federal Office of Public Health (SFOPH) will ultimately decide whether the Swiss basic health insurance should reimburse this technology.
At present, five different suppliers sell five types of lumbar TDAs in Switzerland. Since all devices are documented in the same standardized way SWISSspine offers the possibility of benchmarking, i.e. comparing outcomes of specific implants with pooled outcomes of the other implants.
Dynardi® (Zimmer GmbH, Winterthur, Switzerland) is a relatively recent intervertebral disc prosthesis developed in Switzerland, the clinical results of which have not yet been published. The current article presents the outcomes of all single-level Dynardi TDAs compared with all other prostheses in the SWISSspine data pool.
Materials and methods
SWISSspine, a governmentally mandated registry for lumbar TDA was initiated in March 2005 and is ongoing today. The structure and setup of the registry have been described elsewhere [1, 3]. Currently, 46 surgeons from 32 hospitals have been contributing an average of 9–10 cases per surgeon to the registry. A unique maneuver by Swiss medical profession policy makers was the formation of an expert group in the Swiss Spinal Society to decide on the certification of spine surgeons for this procedure. All Swiss spine surgeons who intend to perform TDAs must submit a formal application to this group with proof of qualification and adequate infrastructure. With this application, the surgeons must sign a written agreement to document all their interventions.
Documentation content and follow-up schedules
At the time of surgery, the surgeon completes primary intervention and implant forms. The patient gives an informed written consent for participation in the registry along with a completed set of EQ-5D, NASS and comorbidity questionnaires. During follow-ups scheduled at 3 months, 1 year, and annually thereafter, the surgeon completes follow-up questionnaires, and patients complete EQ-5D and NASS questionnaires as before surgery.
Dynardi specifications
The Dynardi prosthesis (Dynardi® Dynamic Artificial Disc System) was developed by Zimmer GmbH in Switzerland, and has been available on the Swiss market since April 2006. As of October 2009, the Dynardi prostheses constituted approximately 10% of the cases in the registry database.
The implant consists of two metal plates and a polyethylene insert (Fig. 1). The cranial and caudal plates, which are of the same size, are made of Protasul® 20 (cobalt-chromium-molybdenum with a porous titanium coating). They have a convex form and two anchor pins to ensure solid primary fixation (Fig. 1). A unique tunnel in each plate increases the contact surface with the bone, and a central pin in the plate prevents luxation of the insert. The insert is made of Sulene® PE.
Fig. 1.

The image shows the Dynardi implant (© 2009 Zimmer GmbH, Winterthur, Switzerland) consisting of two metal plates and a polyethylene insert
Statistical analysis
The Wilcoxon rank-sum test was used for comparison between the Dynardi sample and the Data pool. For comparisons between baseline and follow-up examinations of continuous variables such as pain VAS within the samples Wilcoxon signed-rank test was used. When comparing proportions, the χ2 test was used. Confidence intervals for group differences were computed. In the Wilcoxon test, the Hodges–Lehmann estimator was used; in the χ2 test, risk for the proportion difference was calculated.
Multiple logistic regression models were built in order to identify possible covariates with a significant influence on the three outcomes, which were minimum clinically relevant improvements (MCRI) of 18 points in low back and leg pain and of 0.25 points on EQ-5D score [1, 4]. Device used, gender, age at operation, preoperative pain levels, preoperative EQ-5D score, surgical volume of center of intervention, and pharmacologically treated depression were included as covariates in the initial models.
To achieve statistically stable modeling, the continuous variables age, preoperative pain levels and preoperative EQ-5D score were each categorized into three groups of equivalent size. The age groups were: (1) between 19 and 38.1, (2) between 38.2 and 45.6, and (3) between 45.7 and 65 years. Three groups were created according to preoperative low back pain levels: (1) <70 VAS points, (2) ≥70 to <80 points, and (3) ≥80 points. Three groups were created according to preoperative leg pain levels: (1) <50 VAS points, (2) ≥50 to <75 points, and (3) ≥75 points. Finally, the three groups according to preoperative EQ-5D score were: (1) <0.088 points, (2) ≥0.088 to <0.62 points, and (3) ≥0.62 points.
Using backward elimination of covariates with α = 0.05, a list of significant variables was received. This level of significance was used for all analyses. All statistical analyses were conducted using SAS 9.1 (SAS Institute Inc, Cary, NC, USA).
Sample characteristics
The maximum follow-up time for both patient samples was limited to 2.5 years to achieve homogenous follow-up distributions. The Dynardi prosthesis was introduced to the market 1 year after the registry was launched.
Dynardi sample
In October 2009, 56 months after registry launch, there were 52 patients with a single-level lumbar Dynardi TDA: 37 women (71%) and 15 men (29%). The mean age at the time of surgery for both sexes was 41.5 years (SD 8.7 years; age range for women was 24.6–55.9 years, for men 26.2–58.1 years). Four of these patients (7.7%) had depression and regularly took medication for it (Fig. 2). Each of the two surgeons (working in two different hospitals) implanted 26 single-level Dynardi devices.
Fig. 2.
Comorbidities in both patient samples
Overall, 105 Dynardi lumbar TDA follow-up records from 43 to 769 days postoperative were completed by the surgeons and stored in the database. The mean follow-up time was 1 year. There were 164 EQ-5D forms (52 preoperative, 112 follow-up) and 159 NASS forms (52 preop, 108 follow-up) available for evaluation of general and disease-specific quality of life. Using follow-up data no later than 2.5 years after surgery, 50 records could be used for the regression analysis. In addition, 52 comorbidity questionnaires were assessed. The 3-month, 1-year, and 2-year follow-up rates were 92, 67 and 37%, respectively.
Data pool: benchmark
There were 431 patients with single-level lumbar TDAs other than Dynardi in the data pool. These included 250 women (58%) and 181 men (42%). The mean age at the time of surgery was 42.0 years overall (SD 9.2 years), 41.2 years for the women (SD 9.4 years; range 18.5–64.7 years) and 43.1 years for the men (SD 8.8 years; range 19.6–64.7 years). Approximately 10.4% of these patients suffered from depression and regularly took medication for it (Fig. 2). The preoperative depression rate of the Dynardi patients was not significantly different from that of the pool of patients with the other TDAs (7.7 vs. 10.4%, P = 0.58, 95% CI for the difference −5 to 10%).
Overall, 1,083 follow-up records of the pooled lumbar TDAs were completed by surgeons from 32 to 901 days postoperatively. The mean follow-up time was 1.1 years. Also 1,580 (427 preoperative, 1,153 follow-up) EQ-5D forms and 1,487 (415 preop, 1,072 follow-up) NASS forms for evaluation of general and disease-specific quality of life were available for evaluation. For the regression analysis, the last available follow-up up to 2.5 years after surgery was used resulting in inclusion of 403 records. In the pooled group, 414 comorbidity questionnaires were assessed. The 3-month, 1-year, and 2-year follow-up rates were 81, 58 and 35%, respectively.
Results
Pain relief
Pain was measured with two separate low back and leg pain VAS on the NASS questionnaires.
Low back pain
The mean preoperative low back pain in the Dynardi sample was 69 points (SD 15.6). At the 3-month follow-up it was reduced to a mean of 24.4 points (SD 18.5), to 22.6 points at 1 year postoperatively (SD 24.3), and to 23.3 points at 2 years postoperatively (SD 23.2) (preop vs. postop: P < 0.001 for all follow-up intervals).
The mean preoperative low back pain in the data pool was 70.4 points (SD 21.2). At the 3-month follow-up it was reduced to a mean of 32 points (SD 26.2), and then slightly decreased to 31.1 points at 1 year postoperatively (SD 28), and decreased to 28 points at the 2-year follow-up (SD 25.6) (preop vs. postop: P < 0.001 for all follow-up intervals) (Fig. 3).
Fig. 3.
Low back pain in the Dynardi sample and in the data pool
The comparison of postoperative low back pain between Dynardi and the data pool showed no significant differences at the 3-month (P = 0.29, 95% CI 0–10 VAS points), 1-year (P = 0.085, 95% CI 0–10 VAS points) and 2-year follow-up (P = 0.51, 95% CI −10 to 20 VAS points). Also the comparison of low back pain relief in the second postoperative year between Dynardi (46.5 points) and the data pool (37.5 points) showed no significant difference (P = 0.074, 95% CI 0–20 VAS points).
Leg pain
The mean preoperative leg pain in the Dynardi sample was 55 points (SD 26.6). A reduction to 15.9 points after 3 months (SD 19.7), to 16.2 points at 1 year (SD 23.6), and 22 points at 2-year follow-up (SD 24.3) (preop vs. postop: P < 0.001 for all follow-up intervals) was observed (Fig. 4).
Fig. 4.
Leg pain in the Dynardi sample and in the data pool
The mean preoperative leg pain in the data pool was 54.5 points (SD 28.1). A reduction to 24.6 points after 3 months (SD 26.8), to 22.4 points at 1 year (SD 25.6) and 19.9 points at 2-year follow-up (SD 24.5) (preop vs. postop: P < 0.001 for all follow-up intervals) was documented (Fig. 4).
The comparison of postoperative leg pain between the Dynardi sample and the data pool showed no significant differences at the 3-month (P = 0.16, 95% CI 0–10 VAS points), 1-year (P = 0.26, 95% CI 0–10 VAS points) and 2-year follow-up (P = 0.62, 95% CI −10 to 10 VAS points). In addition, the comparison of leg pain relief between Dynardi and the data pool at the last available follow-up (36.3 and 31.3 points, respectively) showed no significant difference (P = 0.27, 95% CI 0–20 VAS points).
Quality of life (QoL) improvement
Values of the EQ-5D range from 1 (best possible QoL) to −0.6 (QoL worse than death).
Dynardi
On preoperative examination, the mean EQ-5D score was 0.37 points (SD 0.31). It improved to 0.82 points at the three-month (SD 0.15), to 0.89 points at the 1-year (SD 0.13) and to 0.85 at the 2-year follow-up (SD 0.16) (preop vs. postop: P < 0.001 for all follow-up intervals). Thirteen percent of patients indicated a preoperative QoL below zero and postoperatively all patients indicated a QoL above zero.
Data pool
On preoperative examination, the mean EQ-5D score was 0.32 points (SD 0.34). It improved to 0.71 points at 3-month (SD 0.29), to 0.72 points at 1-year (SD 0.3) and further to 0.77 at 2 years postoperatively (SD 0.25) (preop vs. postop: P < 0.001 for all follow-up intervals). Twenty-nine percent of patients indicated a preoperative QoL below zero and postoperatively 5.5% of patients indicated a QoL below zero.
The comparison of EQ-5D scores between the samples preoperatively and at 3-month, 1-year and 2-year follow-ups revealed significant differences for the first two follow-ups (P = 0.29 preop, P = 0.011 3-month follow-up, P < 0.001 1-year follow-up and P = 0.26 at 2-year follow-up) (Fig. 5). The comparison of EQ-5D score improvement from preoperative to 2 years after surgery between Dynardi (0.48 points) and the data pool (0.45 points) showed no significant difference (P = 0.14).
Fig. 5.
Difference in postoperative QoL in the Dynardi and pool patients
Factors influencing pain relief and QoL improvement
Low back pain
Among the covariates analyzed, preoperative low back pain (P < 0.001) had an influence on the achievement of MCRI for low back pain, i.e. at least 18 points. This finding was consistent with previous analyses of the SWISSspine registry [1]. Furthermore, the patient sample (Dynardi vs. pool; P = 0.004) had an influence on the MCRI in low back pain.
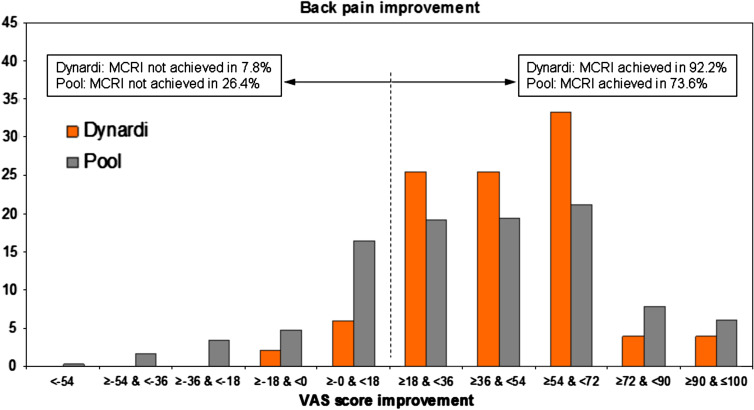
The likelihood for the achievement of MCRI in low back pain was 2.7 times higher (95% CI, 1.3–6.0) in the Dynardi sample compared with the pool (Fig. 6).
Fig. 6.
Percentage of patients with low back pain improvement/worsening until their last follow-up within 2.5 years by sample
Leg pain
Preoperative leg pain (P < 0.001) had an influence on postoperative leg pain relief. The likelihood for the achievement of a MCRI (18 points) was 6.9 times higher (95% CI, 4.2–11.6) if the preoperative leg pain VAS score was between 50 and 75 points and 16.6 times higher (95% CI, 8.7–31.6) if the preoperative score was higher than 75 points in comparison with the patients whose score was lower than 50 points.
Quality of life (EQ-5D)
The preoperative EQ-5D score (P < 0.001) and the patient sample (Dynardi vs. pool, P = 0.007) had a significant influence on the achievement of the MCRI in quality of life. The likelihood of a MCRI in QoL was 2.6 times higher (95% CI, 1.3–5.1) in the Dynardi sample compared to the pooled group.
Pain thresholds and MCRI in low back/leg pain and QoL
According to the previously reported results, the preoperative pain “threshold-value” for clinically relevant low back pain alleviation is 43.8 points [1]. There were 11.5% of patients in the Dynardi sample and 11.1% of patients in the data pool below this threshold preoperatively. Among the patients who had a Dynardi, 92.2% achieved MCRI in low back pain up to the last follow-up within 2.5 years as opposed to 73.6% of the patients in the data pool (Fig. 6). This difference was statistically significant (P = 0.004).
In the Dynardi sample 66.7% and in the data pool 65.7% of patients achieved MCRI for leg pain (P = 0.89) (Fig. 7).
Fig. 7.
Percentage of patients with leg pain improvement/worsening until their last follow-up within 2.5 years by sample
In the Dynardi sample 74.5% and in the data pool 58.0% of the patients achieved MCRI in QoL (Fig. 8). This difference was statistically significant (P = 0.024).
Fig. 8.
Percentage of patients with QoL improvement/worsening until their last follow-up within 2.5 years by sample
Complications and revisions
Three (5.8%) of the patients with a Dynardi had an intraoperative complication compared to 3.9% in the data pool (Table 1) (Dynardi vs. data pool P = 0.21). There were no re-interventions in the Dynardi sample, but 2.1% of cases in the data pool had a re-intervention. The follow-up complication rate was 11.5% in the patients with Dynardi versus 21.2% in the pool but this difference failed to reach significance (P = 0.081). The follow-up complications in the SWISSspine lumbar cohort were recently reported [1].
Table 1.
The table shows complications and revisions in both samples (patient based rates)
| Dynardi | Data pool | |
|---|---|---|
| Intraoperative complications (%) | 5.8 | 3.9 |
| Blood vessel injury | 3 | 13 |
| Sintering of implant | 0 | 1 |
| Urethra injury | 0 | 1 |
| Vertebral body injury | 0 | 1 |
| Dura lesion | 0 | 1 |
| Revision during hospitalization (%) | 0 | 2.1 |
| Follow-up complications (%) | 11.5 | 21.2 |
| Revision with a 2nd hospitalization (%) | 3.8 | 3.7 |
| Dorsal spondylodesis | 1 | 4 |
| Ventral spondylodesis | 0 | 4 |
| Diam stabilization | 0 | 2 |
| Implant removal | 0 | 2 |
| Lumbar pain | 0 | 2 |
| Decompression | 1 | 1 |
| Abscess revision | 0 | 1 |
| Implant failure | 0 | 1 |
| Wound revision | 0 | 1 |
| Not specified | 0 | 1 |
Revisions with a second hospitalisation were similar in the two samples (Dynardi vs. data pool P = 0.97) (Table 1).
Discussion
The SWISSspine registry was instituted 4.5 years ago. Recently, 1-year follow-up data from this registry showed that lumbar TDA significantly reduced low back and leg pain [1]. This pain alleviation was accompanied by a substantial improvement in quality of life. The authors of that report concluded that TDA demonstrated good short-term efficacy and safety [1].
Given the rapidly increasing interest in TDA and the incertitude regarding advantages and disadvantages of the different prosthetic designs, benchmarking of these devices has an undeniable appeal. The governmentally mandated SWISSspine registry with its uniform documentation for all implanted prostheses makes such an endeavor possible. Previously, comparisons of different disc implants were possible only by comparing different publications [5–9]. The study designs of these investigations, however, are frequently quite different, resulting in difficult and inaccurate comparisons. To the best of our knowledge, this is the first literature report that involves benchmarking of a spinal prosthesis against a group of others within one and the same scientific investigational project.
One of the main limitations of such a registry is the fact that the accuracy of the data depends on the sincerity of each surgeon. The certification of Swiss surgeons by the expert group of the Swiss Spinal Society as well as their commitment to accurately document their cases is currently the only existing indirect data quality control. Further data quality control measures such as audits of surgeons by the Spine Society, insurance companies or government authorities are under consideration. A further limitation of our registry results are the relatively low 2-year follow-up rates. Since some patients have simply not reached the according follow-up time yet, or because the questionnaires often arrive with delay (as they are stored in the treating institutions and are later sent in batches) the presented rates are dynamic and further increasing with time. In addition, we consider the article by Mannion et al. [10] an important argument in demonstrating that outcomes of most spinal procedures are quasi-final after about 3 months postoperatively. Hence, the 3-month and 1-year follow-up data should be sufficient in estimating the clinical outcomes after lumbar TDA, given that the prosthesis maintains a proper function. Furthermore, the 1- and 2-year follow-up rates of SWEspine, the Swedish spinal registry, are about 55–65% (personal communication) and SWISSspine is well within that range with its 1-year follow-ups.
There is a constantly growing demand by regulatory agencies and health care payers for evidence-based justification of medical procedures and devices. Randomized controlled trials, which provide level I evidence, are often unfeasible due to ethical aspects, organizational complexity or cost issues. Consequently, the utilization of the simpler and less expensive register studies is on the rise.
Among the five TDA types currently used in the SWISSspine registry, the Dynardi prosthesis was selected for a comparison with the data pool because this new implant was recently developed in Switzerland and its results have not yet been published. Furthermore, the implant accounts for about 10% of cases in the registry and was therefore suitable for rigorous statistical analysis. Regarding demographic characteristics and preoperative clinical status, the 52 patients with the Dynardi TDA were similar to the patients in the data pool. Both samples had the same mean age at operation of 42 years, but there were 13% less women in the data pool. The rate of patients with pharmacologically treated depression in both samples was comparable. There was only 1 month difference in average follow-up time.
There was no significant difference between the Dynardi group and the patient pool in terms of postoperative low back and leg pain alleviation. However, the Dynardi patients had a higher likelihood for the achievement of MCRI in low back pain and QoL than did the other patients.
Postoperative low back pain and QoL were lower, respectively, better, in the Dynardi sample, and this relation remained stable until the second postoperative year. The values for QoL at the 3-month and 1-year follow-ups were even significantly better in the Dynardi sample. Postoperative leg pain in Dynardi patients was better at the early stages but slightly worsened (6 points from 3-month to 2-year follow-up) and reached values similar to other patients with a 2-year follow-up.
The Dynardi sample did not have significantly different rates of intraoperative and follow-up complications or revisions with a new hospitalisation than the pooled group. However, there were no re-interventions within the same hospital stay in the Dynardi sample. Thus, the Dynardi prosthesis seems to be at least as safe as other prostheses in the registry.
The higher likelihood for Dynardi patients in achieving MCRI in low back pain and QoL are findings with no obvious technical explanation. They are probably not related to the prosthesis itself. The higher rate of female patients is a possible factor but the regression analysis had not found patient sex as a covariate with significant influence on QoL or low back pain improvement. Another possible factor may be the higher percentage of patients with a pharmacologically treated depression in the data pool, a factor that was previously reported to have an influence on QoL [1]. However, that difference was not significant. In the first evaluation, pharmacologically treated depression was a significant covariate; however, a slight tendency of convergence of postoperative EQ score curves for depressive and non-depressive patients was observed [1].
The preoperative medication analysis (not reported) showed that surgeons in the pooled group operated on patients with a two times higher percentage of morphine intake as the Dynardi patients, though the preoperative pain levels were very similar. This may represent patients with more chronic pain in the pool or with a higher pain perception, which also remains after surgery. The duration of symptoms was unfortunately not recorded as part of the registry protocols. The physician skills and the patient–physician interaction with the resulting compliance, social and work circumstances, education, large number of surgeons using other TDAs compared to only two using the Dynardi TDA are further possible factors which could have influenced the outcomes and which we could not assess in the dataset. The satisfaction not only with pain relief but also with the treating physician and even the hospital service may be responsible for the better short term QoL in the Dynardi sample.
Regarding the higher likelihood of Dynardi patients for achieving the MCRI in low back pain, we assume that predominantly patient selection was responsible. It is the general consensus that patient selection is the primary key in achieving a favorable outcome [11, 12]. The proportion of patients with a low back pain MCRI in the Dynardi group compared with that in the pool and in the previous analysis [1] impressively demonstrates the potential of TDA if the indication is well made.
Published total complication rates range between 3 and 50% and those in SWISSspine (between 4 and 21%) are relatively low [13]. A possible explanation is the framework of SWISSspine where only surgeons with a proven expertise in spinal surgery received certification for the intervention. In addition, there may have been benefits from advancements in instrumentation and surgical approach as well as surgical techniques that the first movers of the technology did not have.
As opposed to cervical disc prostheses, mid- and long-term outcomes of the lumbar implants have been under observation for many more years. Nevertheless, long-term outcomes are still rarely reported [9]. The few available investigations are rather critical in their conclusions as opposed to the reported more promising mid- and short-term results [13]. Further investigations are undoubtedly needed. The current analysis cannot yet shed light onto long-term results of lumbar TDA but SWISSspine registry results are constantly updated and monitored and a special 5-year follow-up study is under preparation. Until then short-term outcomes of yet another new implant, the Dynardi lumbar TDA, can be considered equivalent to the other models on the market.
Acknowledgments
We are indebted to Prof. M. Aebi and all staff members of the Institute for Evaluative Research in Orthopaedic Surgery involved in the SWISSspine project. Without his belief in the absolute necessity of outcome documentation, the vision of an academic data clearing house with proprietary data collection system and the endurance of turning this vision into reality in the past 8 years, the SWISSspine registry would not have become a successful postmarket surveillance project within such a short time frame. We thank Daniel Dietrich, PhD, for statistical consulting in all analyses presented in the current article. We are thankful to SGS and the SWISSspine registry group who made this research possible by populating the database with their valuable and much appreciated entries. Aebi M, Baerlocher C, Baur M, Berlemann U, Binggeli R, Boos N, Boscherini D, Cathrein P, Favre J, Forster T, Grob D, Hasdemir M, Hausmann O, Heini P, Heilbronner R, Huber J, Jeanneret B, Kast E, Kleinstueck F, Kroeber M, Lattig F, Lutz T, Maestretti G, Marchesi D, Markwalder T, Martinez R, Min K, Morard M, Moulin P, Otten P, Payer M, Porchet F, Ramadan A, Renella R, Richter H, Schaeren S, Schizas C, Seidel U, Selz T, Sgier F, Stoll T, Tessitore E, Van Dommelen K, Vernet O, Wernli F.
Footnotes
On behalf of the SWISSspine Registry Group.
References
- 1.Schluessmann E, Diel P, Aghayev E, Zweig T, Moulin P, Roder C. SWISSspine: a nationwide registry for health technology assessment of lumbar disc prostheses. Eur Spine J. 2009;18:851–861. doi: 10.1007/s00586-009-0934-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schluessmann E, Aghayev E, Staub L, Moulin P, Zweig T, Roder C (2010) SWISSspine: the case of a governmentally required HTA-registry for total disc arthroplasty. Results of cervical disc prostheses. Spine (in press) [DOI] [PubMed]
- 3.Diel P, Reuss W, Aghayev E, Moulin P, Roder C (2009) SWISSspine-a nationwide health technology assessment registry for balloon kyphoplasty: methodology and first results. Spine J. doi:10.1016/j.spinee.2009.08.452 [DOI] [PubMed]
- 4.Hagg O, Fritzell P, Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 5.Bertagnoli R, Yue JJ, Shah RV, Nanieva R, Pfeiffer F, Fenk-Mayer A, Kershaw T, Husted DS. The treatment of disabling single-level lumbar discogenic low back pain with total disc arthroplasty utilizing the Prodisc prosthesis: a prospective study with 2-year minimum follow-up. Spine. 2005;30:2230–2236. doi: 10.1097/01.brs.0000182217.87660.40. [DOI] [PubMed] [Google Scholar]
- 6.Lafuente J, Casey AT, Petzold A, Brew S. The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment of cervical spondylosis: 46 consecutive cases. J Bone Joint Surg Br. 2005;87:508–512. doi: 10.1302/0301-620X.87B4.15436. [DOI] [PubMed] [Google Scholar]
- 7.Nabhan A, Ahlhelm F, Pitzen T, Steudel WI, Jung J, Shariat K, Steimer O, Bachelier F, Pape D. Disc replacement using Pro-Disc C versus fusion: a prospective randomised and controlled radiographic and clinical study. Eur Spine J. 2007;16:423–430. doi: 10.1007/s00586-006-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI, Pape D. The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine. 2007;32:1935–1941. doi: 10.1097/BRS.0b013e31813162d8. [DOI] [PubMed] [Google Scholar]
- 9.Putzier M, Funk JF, Schneider SV, Gross C, Tohtz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F. Charite total disc replacement—clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15:183–195. doi: 10.1007/s00586-005-1022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D. The quality of spine surgery from the patient’s perspective. Part 1: the core outcome measures index in clinical practice. Eur Spine J. 2009;18(Suppl 3):367–373. doi: 10.1007/s00586-009-0942-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guyer RD, Siddiqui S, Zigler JE, Ohnmeiss DD, Blumenthal SL, Sachs BL, Hochschuler SH, Rashbaum RF. Lumbar spinal arthroplasty: analysis of one center’s twenty best and twenty worst clinical outcomes. Spine (Phila Pa 1976) 2008;33:2566–2569. doi: 10.1097/BRS.0b013e318185941a. [DOI] [PubMed] [Google Scholar]
- 12.Patel AA, Brodke DS, Pimenta L, Bono CM, Hilibrand AS, Harrop JS, Riew KD, Youssef JA, Vaccaro AR. Revision strategies in lumbar total disc arthroplasty. Spine (Phila Pa 1976) 2008;33:1276–1283. doi: 10.1097/BRS.0b013e3181714a1d. [DOI] [PubMed] [Google Scholar]
- 13.de Kleuver M, Oner FC, Jacobs WC. Total disc replacement for chronic low back pain: background and a systematic review of the literature. Eur Spine J. 2003;12:108–116. doi: 10.1007/s00586-002-0500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]