Abstract
Clinical studies reported frequent failure with anterior instrumented multilevel cervical corpectomies. Hence, posterior augmentation was recommended but necessitates a second approach. Thus, an author group evaluated the feasibility, pull-out characteristics, and accuracy of anterior transpedicular screw (ATPS) fixation. Although first success with clinical application of ATPS has already been reported, no data exist on biomechanical characteristics of an ATPS-plate system enabling transpedicular end-level fixation in advanced instabilities. Therefore, we evaluated biomechanical qualities of an ATPS prototype C4–C7 for reduction of range of motion (ROM) and primary stability in a non-destructive setup among five constructs: anterior plate, posterior all-lateral mass screw construct, posterior construct with lateral mass screws C5 + C6 and end-level fixation using pedicle screws unilaterally or bilaterally, and a 360° construct. 12 human spines C3–T1 were divided into two groups. Four constructs were tested in group 1 and three in group 2; the ATPS prototypes were tested in both groups. Specimens were subjected to flexibility test in a spine motion tester at intact state and after 2-level corpectomy C5–C6 with subsequent reconstruction using a distractable cage and one of the osteosynthesis mentioned above. ROM in flexion–extension, axial rotation, and lateral bending was reported as normalized values. All instrumentations but the anterior plate showed significant reduction of ROM for all directions compared to the intact state. The 360° construct outperformed all others in terms of reducing ROM. While there were no significant differences between the 360° and posterior constructs in flexion–extension and lateral bending, the 360° constructs were significantly more stable in axial rotation. Concerning primary stability of ATPS prototypes, there were no significant differences compared to posterior-only constructs in flexion–extension and axial rotation. The 360° construct showed significant differences to the ATPS prototypes in flexion–extension, while no significant differences existed in axial rotation. But in lateral bending, the ATPS prototype and the anterior plate performed significantly worse than the posterior constructs. ATPS was shown to confer increased primary stability compared to the anterior plate in flexion–extension and axial rotation with the latter yielding significance. We showed that primary stability after 2-level corpectomy reconstruction using ATPS prototypes compared favorably to posterior systems and superior to anterior plates. From the biomechanical point, the 360° instrumentation was shown the most efficient for reconstruction of 2-level corpectomies. Further studies will elucidate whether fatigue testing will enhance the benefit of transpedicular anchorage with posterior constructs and ATPS.
Keywords: Cervical spine, Biomechanical study, Corpectomy, Pedicle screw, Reconstruction
Introduction
Anterior surgical strategies are increasingly recognized as advantageous for multilevel cervical decompression of the anteriorly compromised spinal cord, providing the ability for anterior release, durable reconstruction of physiologic alignment and instrumented fusion through a less traumatic approach compared to the posterior neck dissection [3, 6, 20, 37, 38, 40, 45−47, 55]. With anterior procedures, decompression of the neurologic structures can be accomplished by means of segmental discectomy or partial corpectomy. With the number of decompressed levels, particularly corpectomies performed, the intrinsic stability of the spine drops, which is a challenge to current anterior instrumentations [10]. Likewise, two reviews of literature identified a high rate of complications in reconstructive multilevel (>2 levels) cervical spine surgery, particularly if decompression required multiple corpectomies and a posterior supplemental instrumentation was not performed [3, 31]. Accordingly, for a successful outcome with ≥2-level corpectomies, a combined anterior and posterior approach was found a sound rationale [32] but necessitating a second posterior approach with significant morbidity. Hence, an anterior cervical instrumentation that increases primary construct stability by providing increased screw–bone anchorage, while avoiding the need for posterior augmentation, would be a valuable adjunct for spine surgeons facing the biomechanical challenges of advanced cervical instabilities.
In virtue of the described clinical challenges, a group of authors initiated research on increasing anterior construct rigidity by use of anterior transpedicular screw–plate anchorage [5, 30, 63]. In 2008, the anatomical feasibility of ATPS insertion was demonstrated, and implications for a rigid screw–plate system were defined [53]. Later on [29], pull-out strength characteristics of ATPS were shown 2.5-fold that of vertebral body screws (VBS), and results of insertion accuracy with a manual technique were promising [29]. In 2009, accuracy of ATPS placement could be increased to zero for critical breaches using an electronic conductivity device. Coincidently, two clinical series reported on the successful application of ATPS for anterior cervical spine reconstructions: one transfixing fibular grafts to cervical vertebrae [6] and one using a non-constrained single-hole plate for segmental instrumentation [63]. Yet, a constrained screw–plate system that enables the placement of ATPS besides that of VBS while providing common modern features of rigid screw–plate systems does not exist. Likewise, although transpedicular screw fixation was shown to confer highest fixation characteristics [26, 27, 29, 34], there are no data on the biomechanical characteristic of an ATPS plate to resist the loads that challenge multilevel constructs.
Therefore, the purposes of the current study were (1) to analyze primary construct stability of different instrumentations currently in use for the reconstruction of a 2-level corpectomy, (2) to test an ATPS plate prototype system and its performance compared to common anterior and posterior instrumentations, and (3) to assess the general impact of end-level unilateral transpedicular screw anchorage within anterior, posterior, and combined instrumentations compared to bilateral-pedicle screw anchorage at the end-levels. We performed a biomechanical comparative study of different instrumentations for the reconstruction of a 2-level corpectomy model with special interest on ATPS as a new anchorage principle for the reconstruction of advanced cervical spine instabilities.
Materials and methods
Laboratory study assessing primary construct stability among six osteosynthesis used a 2-level cervical corpectomy model for reconstruction. We acquired 12 fresh-frozen cervical spines C0–T1 from six female and six male donors. Spine were processed at C2–C3 leaving C3–T1 for testing. Mean age of the specimens was 71.5 ± 1.2 years (range 70–74 years). The specimens were subjected to multislice computerized tomography scanning (Somatom Volume Zoom, Siemens, Erlangen, Germany), and none of the spines revealed evidence of neither infectious, neoplastic or traumatic disease, nor congenital cervical spine deformation. Quantitative computer tomography of the cervical spines was performed, and the mean BMD was 211.2 ± 41.3 mg Ca-HA/ml (range 172–320 mg Ca-HA/ml). Afterwards, cadavers were stored at −20°C in triple-sealed bags until preparation.
On the day of testing, the specimens were thawed, and soft-tissues excluding the lateral parts of the longus colli and longus capiti were removed while the osteoligamentous structures were preserved. To prevent desiccation during preparation, specimens were kept moist with saline solution. Handling specimens in the described manner does not affect their biomechanical properties [42, 59].
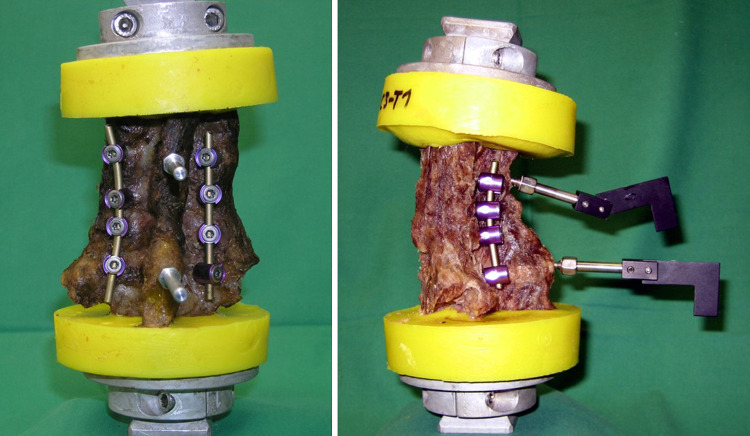
The specimens were mounted in a previously described spine tester (Fig. 1) [58]. For fixation in the spine tester, short wood-screws were partially inserted in the cranial and caudal end-vertebrae, C3 and T1, and embedded in polymethylmetacrylate (PMMA, Technovit 3040, Heraeus Kulzer GmbH, Wehrheim, Germany). The segmental motion between C4 and C7 was measured by a high-resolution optical motion analysis system (Vicon-Motion System LTD, Oxford, UK). Customized screws carrying triaxial markers were placed in the spinous processes of C4 and C7 to track motion. Motion was measured as a change in terms of three rotation angles (Ry for flexion–extension; Rz for axial Rotation; Rx for lateral bending) from the cephalad and caudad markers.
Fig. 1.
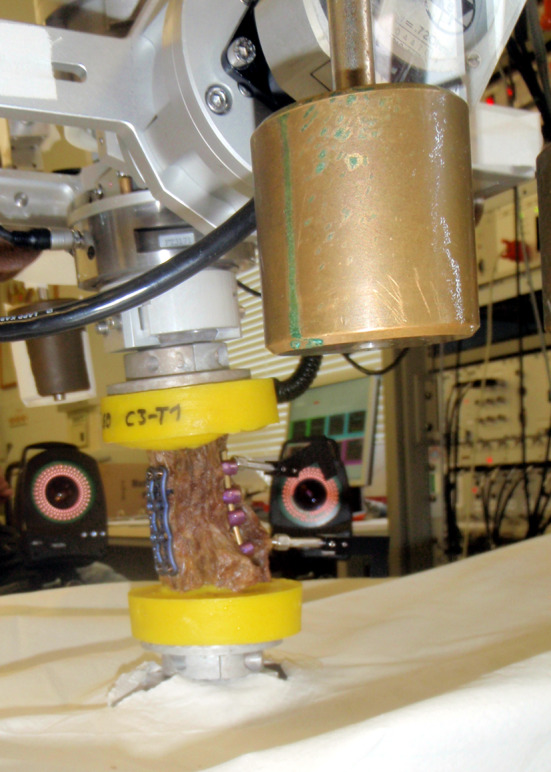
Laboratory test setup. Specimen after 2-level corpectomy and instrumentation using the 360° construct is tested in flexion–extension. Motion is tracked with posteriorly placed reflective devices in the spinous processes
The spines were non-destructively tested and loads applied as pure moments in alternating sequences for right/left lateral bending (±Mx), flexion/extension (±My) and right/left axial rotation (±Mz) with 2.5 Nm in all directions. To precondition the specimens and minimize viscoelastic effects, each sequence was tested with three cycles. The total range of motion (ROM) and neutral zone (NZ) were determined for each direction. The ROM was the displacement at maximum loads, and the neutral zone (NZ) was the displacement at zero loads, with both measured during the third cycle. The last cycle was used for statistical evaluation. Motion data were assessed as degrees and further processed as normalized values after standardization to the intact ROM state which was set at 100%. Normalization was performed to mitigate the effects of variability in stiffness naturally expected in human cadaveric specimens. The testing procedure was conducted according to the recommendations for the standardization of in vitro stability testing of spinal implants [60].
With 12 specimens available we yielded for comparative tests of six techniques. Hence, specimens were randomly divided into two groups in order to decrease bone stock degradation through serial testing of different techniques within one specimen. After measurement in the intact state, corpectomies of C5 and C6 were created using ordinary clinical instruments (e.g., rongeur, chisel, high-speed drill), including resection of the posterior longitudinal ligament (PLL). The dissection was proceeded laterally to release the uncovertebral joints according to the clinical procedure where an anterior release is frequently indicated to reconstruct a physiologic cervical lordosis that serves for indirect decompression by posterior shift of the spinal cord. The corpectomy defect was reconstructed using a distractable anterior cervical cage system (Synthes, Oberdorf, Switzerland).
Following tests were applied in alternating order:
- Group 1: testing at intact state
- anterior plate (Vectra),
- CPS unilat (LMS fixation at C4–C7 right and CPS fixation at C4 + C7 left with LMS fixation at C5–C6 left),
- CPS bilat (LMS fixation at C5–C6 bilateral and CPS fixation at C4 + C7 bilateral),
- ATPS-1 (customized ATPS-plate prototype).
- Group 2: testing at intact state
- All LMS (LMS fixation at C4–C7 bilaterally),
- 360° construct (anterior plate and LMS fixation at C4–C7 bilaterally),
- ATPS-2 (customized ATPS-plate prototype, same as in Group 1).
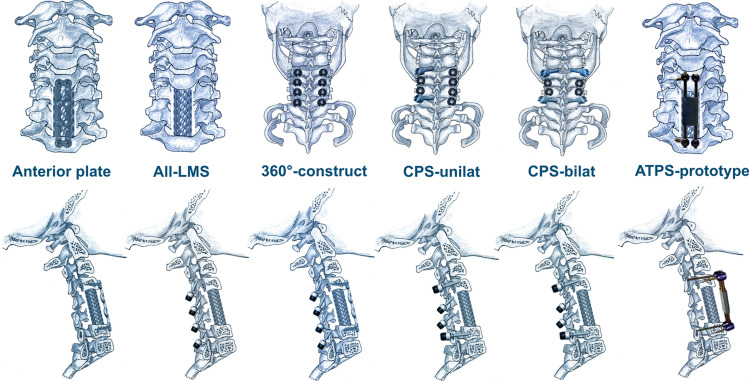
Schematics of the osteosynthesis with a cage for corpectomy reconstruction are shown in Fig. 2. All instrumentations were from Synthes (Oberdorf, Germany). They included an anterior semi-constrained screw–plate system (Vectra™) with 14 mm VBS placed unicortically. The plate offers benefits from plate to bone friction by lag screw compression as well as dynamic graft loading during the clinical course. The plate is used for trauma, corpectomy, and tumor instabilities. For posterior instrumentations, we used a constrained posterior screw and rod system (Synapse™) using 14 mm unicortical LMS and 28 mm unicortical CPS, both 3.5 mm in diameter. Instrumentation was performed by two of the authors experienced in posterior LMS and CPS placement. For ATPS-plate testing, two prototypes were available: one primary solution and one as back-up. Both entailed placing a 3.5-mm pedicle screw into the right pedicles of the end-vertebra C4 and C7 while VBS with 14 mm length were placed unicortically on the left side.
Fig. 2.
Schematics of the osteosynthesis constructs applied after corpectomy of C5 and C6 and reconstruction using the distractable cervical cage (here, a mesh cage). Top anterior and posterior views of constructs tested. Bottom lateral views of constructs tested
The in vitro model and the test protocol were carefully designed. To restrict the number of human specimens and to enable comparison between standard techniques for 2-level corpectomy reconstruction as well as a new osteosynthesis type (ATPS), each specimen was subjected to four and three instrumented tests, respectively, in a manner that the preceding test did not compromise bony anchors for the subsequent test. Accordingly, osteosynthesis were applied in an alternating fashion with exception of the CPS-bilat in group 1. To minimize damage to the specimens during testing, CPS-bilat was tested at the end because of overlapping screw trajectories of LMS and CPS with the latter weakening the bone mass for LMS if placed first.
Statistical analysis
For comparison of the standardized ROM values, median as well as 25 and 75% quartiles were computed. For paired samples, Wilcoxon’s matched pairs test was used, and for unpaired samples, the median test was used. For the comparison of age and BMD, Students t test was used. A p value less than 5% was considered statistically significant. All computations and illustrations were done with Statistica 6.1 (StatSoft, Tulsa, OK, USA).
Results
Analysis of BMD and age between groups 1 and 2 showed that both were similar. Mean age was 71.5 years in both groups (p = 0.99), and BMD was 223.15 mg Ca-HA/ml in group 1 and 186.7 mg Ca-HA/ml in group 2 (p = 0.07). Thus, groups were deemed comparable.
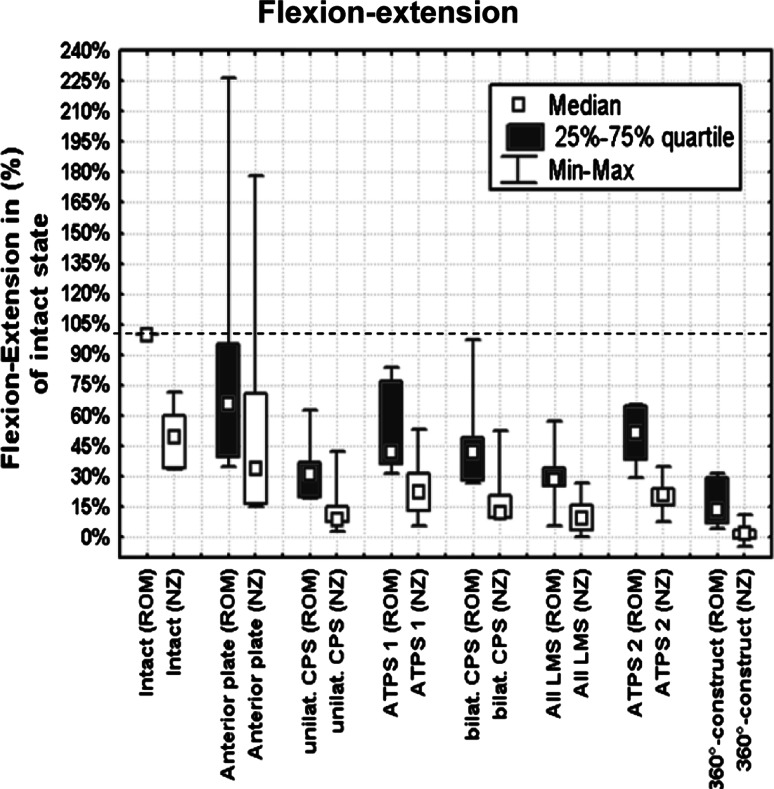
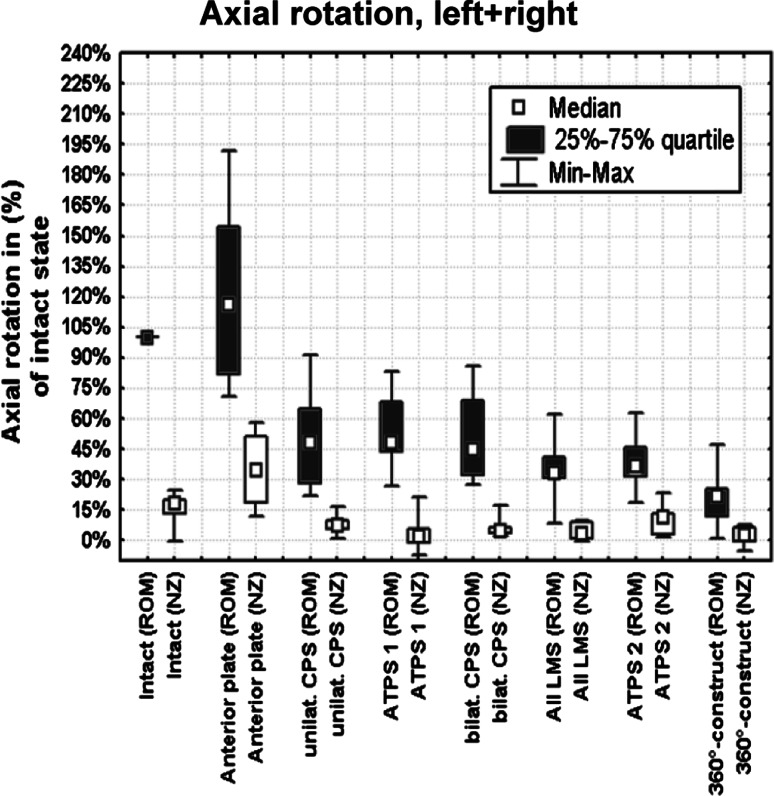
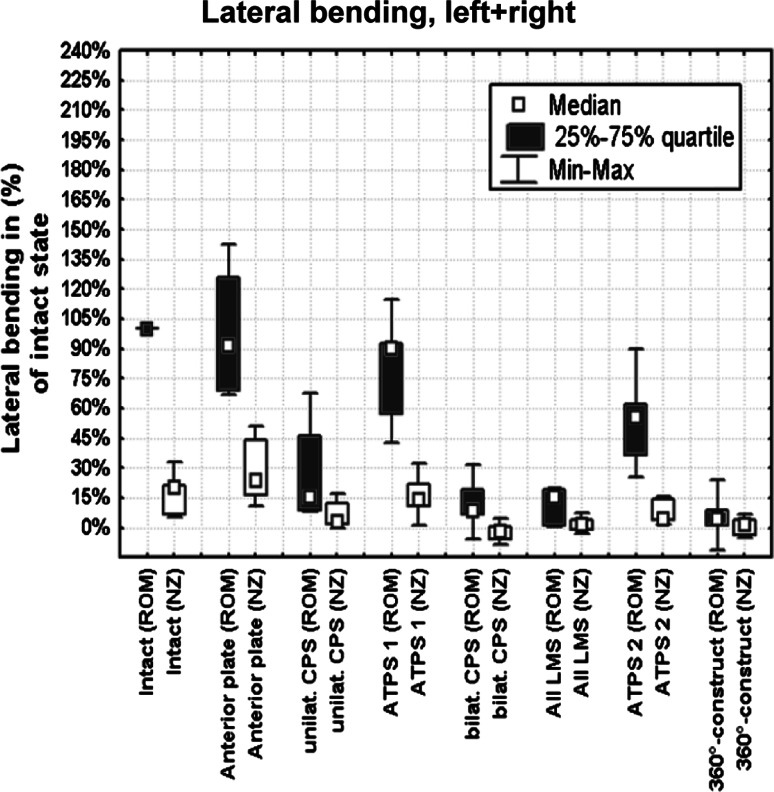
All instrumentations showed a significant reduction of ROM for all directions compared to the intact state (Figs. 3, 4, 5) except for the anterior plate. The anterior plate failed to reduce ROM below the intact state once in flexion–extension, four times in axial rotation, and three times in lateral bending.
Fig. 3.
Results of flexion–extension testing
Fig. 4.
Results of axial rotation testing, left + right
Fig. 5.
Results of lateral bending testing, left + right
The main results concerning normalized ROM values in all loading directions among the six constructs are summarized in Table 1a–c and illustrated in Figs. 3, 4, and 5. Results of statistical analysis regarding differences between the instrumentations are listed in Table 2a–c. Results concerning stabilization at the neutral zone (NZ) are illustrated in Figs. 3, 4, and 5 and followed the trends of the ROM data.
Table 1.
Restriction of total ROM with the six constructs tested
| Percentage of intact | Median | 25% quartile | 75% quartile |
|---|---|---|---|
| (a) Flexion–extension | |||
| 360° | 13.4 | 7.3 | 29.6 |
| All-LMS | 28.2 | 25.4 | 34.2 |
| CPS-unilat | 31.4 | 19.9 | 36.9 |
| ATPS-1 | 41.7 | 36.3 | 76.9 |
| CPS-bilat | 42.2 | 28.1 | 49 |
| ATPS-2 | 51.6 | 38.2 | 64.8 |
| Anterior plate | 65.6 | 39.8 | 95.4 |
| (b) Axial rotation, left + right | |||
| 360° | 21.8 | 11.5 | 25.1 |
| All-LMS | 33.4 | 30.7 | 40.9 |
| ATPS-2 | 36.6 | 31.3 | 45.9 |
| ATPS-1 | 41.7 | 36.3 | 76.9 |
| CPS-bilat | 44.9 | 32.4 | 68.8 |
| CPS-unilat | 47.8 | 28.3 | 64.5 |
| Anterior plate | 116 | 82 | 154.7 |
| (c) Lateral bending, left + right | |||
| 360° | 4.2 | 1.2 | 8.9 |
| CPS-bilat | 8.5 | 6.4 | 18.8 |
| All-LMS | 15 | 1.2 | 18.9 |
| CPS-unilat | 15.3 | 8.5 | 46.1 |
| ATPS-2 | 55.7 | 26.1 | 62.1 |
| ATPS-1 | 89.8 | 56.9 | 92.6 |
| Anterior plate | 91.4 | 68.9 | 126 |
Normalized values in % compared to intact state
Order of constructs sorted according to median values
Table 2.
Analysis of differences of ROM among the six cervical stabilization constructs (p values)
| 360° | All LMS | CPS bilat | CPS unilat | Anterior plate | ATPS-1 | ATPS-2 | |
|---|---|---|---|---|---|---|---|
| (a) Flexion–extension | |||||||
| 360° | |||||||
| All-LMS | NS | ||||||
| CPS-bilat | 0.03 | NS | |||||
| CPS-unilat | NS | NS | 0.03 | ||||
| Anterior plate | <0.001 | 0.02 | 0.03 | 0.03 | |||
| ATPS-1 | <0.001 | 0.02 | NS | NS | NS | ||
| ATPS-2 | 0.003 | NS | NS | NS | NS | NS | |
| (b) Axial rotation, left + right | |||||||
| 360° | |||||||
| All-LMS | 0.03 | ||||||
| CPS-bilat | 0.02 | NS | |||||
| CPS-unilat | 0.02 | NS | NS | ||||
| Anterior plate | <0.001 | <0.001 | 0.03 | 0.03 | |||
| ATPS-1 | 0.02 | NS | NS | NS | 0.04 | ||
| ATPS-2 | NS | NS | NS | NS | 0.01 | NS | |
| (c) Lateral bending, left + right | |||||||
| 360° | |||||||
| All-LMS | NS | ||||||
| CPS-bilat | NS | NS | |||||
| CPS-unilat | NS | NS | NS | ||||
| Anterior plate | <0.001 | <0.001 | 0.03 | 0.03 | |||
| ATPS-1 | 0.005 | <0.001 | 0.04 | 0.04 | NS | ||
| ATPS-2 | 0.04 | 0.04 | 0.01 | NS | NS | NS | |
Flexion–extension
In flexion/extension (Tables 1a, 2a; Fig. 3), the highest single normalized ROM value was found for the anterior plate with 226% of the intact state and the lowest for the 360° construct with 4.6%. Specimens tested in flexion–extension showed a wide range of ROM, e.g., 27–97.1% for the CPS-bilat.
Statistical comparison between constructs revealed no significant difference concerning primary stability in flexion–extension loading between the 360° construct, all-LMS, and CPS-unilat. Notably, there was a significant difference between the CPS-unilat and CPS-bilat in flexion–extension testing with the latter being slightly outperformed by the former. These findings will be discussed in detail later.
Although there was a significant difference between the 360° and the CPS-bilat as well as between the 360° and the ATPS-1/ATPS-2, the ATPS constructs were not significantly different from the CPS bilat, CPS unilat, and all-LMS (true for ATPS-2 with direct intragroup comparison). Although there were large differences concerning means and medians between CPS-unilat, CPS-bilat, ATPS, all-LMS, and the anterior plate, analysis of statistical differences yielded significance for all but the ATPS constructs.
Axial rotation
In axial rotation (Tables 1b, 2b; Fig. 4), the highest single normalized ROM value was found for the anterior plate with 192% of the intact state and the lowest with 1% for the 360° construct. Specimens tested in axial rotation showed a wide range of ROM values, e.g., 21.8–91.0% for the CPS-unilat.
Statistical comparison between constructs revealed significant differences concerning primary stability in axial rotation between the 360° construct and all other constructs except for the ATPS-2 that performed similar to the 360° construct. In addition, there were no significant differences between the ATPS constructs, the all-LMS, CPS-unilat, and CPS-bilat. CPS-bilat and CPS-unilat were not significantly different concerning restriction of axial rotation. The anterior plate was significantly outperformed by all other constructs.
Lateral bending
In lateral bending (Tables 1c, 2c; Fig. 5), the highest single normalized ROM value was found for the anterior plate with 142% of the intact state and the lowest with 0% for the 360° construct. Again, specimens tested in lateral bending showed a wide range of ROM values, e.g., 25.3–66.6% for the ATPS.
Concerning primary stability in lateral bending, there were no significant differences between the 360° construct, all-LMS, CPS-bilat, and CPS-unilat, whereas the anterior plate was outperformed by all these constructs. In lateral bending, the ATPS constructs were shown superior to the anterior plate but inferior, in particular if compared to the 360° and the all-LMS (ATPS-1: p = 0.005 and p < 0.001; ATPS-2: p = 0.04 and p = 0.04, respectively) and if compared to the CPS-bilat and CPS-unilat (ATPS-1: p = 0.04 and p = 0.04; ATPS-2: p = 0.01 and p = ns, respectively). Notably, there were no significant differences between the unilateral transpedicular anchorage systems, namely the CPS-unilat and the ATPS-2.
Anterior transpedicular screw
All specimens instrumented with ATPS underwent sequential testing without early construct failure or significant loosening of implants excluding two premature ATPS prototypes tested at the beginning. At the first test of both groups 1 and 2, the first ATPS plate prototype failed at its screw–plate junction during the loading cycles. Being aware of potentials for failure with the first time having the ATPS concept on a test bed, we planned ATPS-prototype testing in each specimen to have a total of 12 test options available. Thus, in the ten remaining specimens the back-up solution was used (see Fig. 2), and no implant-related failure occurred. The two failed ATPS plate tests at the beginning (instrumented once at first position and once at last position in order of testing) were excluded from statistical analysis.
Analysis of ROM showed that there were no significant differences for all loading directions between the ATPS constructs tested in groups 1 and 2 while statistical analysis between the ATPS and the 360° constructs showed intergroup differences for ATPS-1 and ATPS-2 (Table 2a). Analysis of primary stability data showed that the ATPS construct was able to reduce ROM below intact state for all modes of testing in all specimens, except once in lateral bending. In addition, the ATPS construct achieved comparable results to its posterior counterparts in several modalities. In flexion–extension, there were no significant differences between ATPS-1/ATPS-2 and the posterior pedicle screw-based constructs. Moreover, there were no significant differences between the ATPS-2 and the all-LMS of group 2 (direct intragroup comparison). In axial rotation, there were also no significant differences compared to the posterior constructs, while there were only significant differences between the 360° construct and the ATPS-1 but not for the ATPS-2 (direct intragroup comparison: 360° vs. ATPS-2, p = 0.46; Table 2b). In lateral bending, differences in reduction of ROM between the posterior systems and the ATPS construct just yielded statistical difference. Although there were differences regarding means and median (Table 1c) comparing the anterior plate and the ATPS, the differences did not yield significance.
Concerning the ability to reduce ROM compared to the intact state, the ATPS constructs showed significant differences compared to the anterior plate in axial rotation testing. Even though there were considerable differences concerning means and medians between the anterior plate and the ATPS-1/ATPS-2 also in flexion–extension and lateral bending, analysis of differences did not yield significance. As with the posterior instrumentations, the ATPS plate was outperformed by the 360° construct in all modes with one exception; in axial rotation, there were no differences between the ATPS-2 and the 360° construct (direct intragroup comparison).
Discussion
Multilevel cervical constructs generate a large lever-arm at their end-level anchors that can cause construct failure before fusion matures [31, 41]. Several reviews of literature documented the challenge with anterior multilevel fusions [3, 10, 31, 32]. Reports of failure with anterior-only instrumentation of 2- and even 1-level corpectomies continue. A recent article focusing on 42 patients with a median of 2-level corpectomies reported hardware failure in 17% and significant problems that urged the authors to go posteriorly in subsequent cases [35]. Sembrano [53] reported a revision rate of 36% with anterior-only instrumented fusions for 3–5-level decompressions and in another article in 2009, analyzing 39 patients subjected to anterior-only instrumented 2-level corpectomies, the loosening rate was 18%, 10% requiring revision [57]. On the contrary, Aryan [6] did not observe any failure in 53 patients subjected to multiple corpectomies using a 360° construct. As concerns clinical failures, previous biomechanical studies already served evidence for explanations. Singh [54] performed anterior-only instrumentation C3–C6 using a constrained plate for the stabilization of (1) segmental discectomies, (2) hybrid reconstruction (corpectomy C4, discectomy C5–C6), and (3) 2-level corpectomy. The segmental and hybrid reconstructions were significantly more rigid in most loading modes than the latter. Similarly, Porter [43] showed that hybrid constructs yielded higher primary stability than anterior-only instrumented 3-level corpectomies using non-constrained plates. Segmental anterior fixation using a constrained plate was also shown comparable to CPS stabilization in a 2-level injury model [8]. Hence, authors recommended segmental fixation which is in line with clinical rationales [8, 31]. But in selected cases corpectomies at multiple levels are indicated, and in our 2-level corpectomy model the 360° construct outperformed all others, the least concerning its median ROM values (Figs. 3, 4, 5). Our biomechanical findings go in concert with previous studies showing benefits by circumferential stabilization compared to anterior- or posterior-only stabilization [4, 8, 17, 33, 50] and echo the clinical trend that multilevel anterior decompressions, particularly ≥2-level corpectomies, shall receive a 360° stabilization. In addition, we performed the first study comparing various osteosynthesis for a 2-level corpectomy stabilization (a 3-level fusion), resembling the threshold between a ‘short’ and ‘long’ cervical fusion, and analyzed the differences in primary construct stability including a new technique, ATPS, as well as selective end-level unilateral and bilateral posterior CPS fixation. The selective usage of CPS based on safety concerns previously elaborated in the journal [32, 56]. We observed that, except for the anterior-only plating, a 2-level corpectomy model stabilized with an anterior distractable cage and modern posterior instrumentations or an ATPS construct performed well restricting ROM significantly compared to that of intact specimens. Our findings are further enlightened when put into perspective of literature: Dmitriev [16] reported the results of anterior, posterior, and combined stabilization using constrained implants for 2- and 3-level decompressions. As in the current study, the anterior plate was outperformed by the 360° construct while there were only small differences between the posterior and the 360° construct. Particularly in lateral bending, the posterior constructs afforded more stability than the anterior, like in our study. With our 2-level corpectomy model, the 360° construct reduced ROM better than the posterior constructs, especially in axial rotation (Figs. 3, 4, 5); in flexion–extension, a significant difference was observed only for comparison with the CPS-bilat. The posterior-only and the 360° construct outperformed the anterior-only in multilevel constructs in several studies including the current which is consistent with expectations based on the design of the constructs [8, 17, 50, 51]: The configuration of LMS and CPS allows increased leverage for posterior constructs, particularly against flexion–extension, compared to the anterior plates with the osseus anchor being far more off the segmental instantaneous center of rotation (ICR) [7]. The position of the anterior plate is close to the ICR and provides a short lever arm, which is not as effective at stabilizing multilevel constructs.
With anterior cervical decompression, plating is a surgical standard, and non-instrumented 2-level corpectomies followed by a posterior instrumentation are rare. But in cases that preclude anterior plating because of existing serious dysphagia, recalcitrant infections and concerns regarding implants, cost issues, or if a posterior release and corrective maneuver are scheduled after anterior release and grafting was done; our study showed that with posterior-only stabilization there will be no meaningful difference concerning primary stability whether a segmental all-LMS, end-level bilateral, or unilateral CPS fixation is used. Nevertheless, most 2-level corpectomies are likely to undergo anterior plating during the same anesthesia. So, for the most common scenario our study showed that with an anteriorly plated 2-level corpectomy, an all-LMS augmentation will be sufficient in terms of primary stability. Accordingly, reconstructions of most cervical disorders do not require CPS. But, of the current techniques, transpedicular anchorage provides highest stability [2, 3, 22, 31, 38, 44, 62], and in selected patients with advanced instability, CPS fixation is a sound treatment [12, 21, 28, 62] with high accuracy rates in the hands of trained surgeons, particularly at C2 and C7 [1, 9, 25, 29, 62]. Our study offers new biomechanical data for the selective usage of CPS. We evaluated the rigidity of unilateral versus bilateral CPS end-level fixation in a 3-level instrumentation C4–C7, and statistical analysis revealed no inferior results in terms of primary stability for the unilateral pedicle anchorage. Our observations are of particular interest concerning risk–benefit calculations regarding vertebral artery injury during bilateral CPS insertion [32], in cases where bilateral CPS placement cannot be performed due to anatomical restraints or due to complications.
The results of our study must be carefully compared to other biomechanical studies and transferred to the clinical setting. We constructed a 2-level corpectomy model with removal of the PLL, others did not [16, 34, 49], while the PLL is a known main segmental stabilizer [15]. Ianuzi [23] analyzed the stability afforded by an anterior constrained plate, posterior-constrained LMS, and 360° construct for a 1-level corpectomy model. The latter was superior to anterior or posterior stabilizations, but the anterior and posterior constructs were shown equal. That data are in sharp contrast to the current results, however, we reported the results of reconstructions of a 2-level corpectomy model and results in 1- or 3-level constructs might differ.
We used modern anterior and posterior implants. In literature, differences exist within similar 1-level corpectomy models whether constrained or non-constrained instrumentations were used [17, 23], and Schmidt [50] showed that using constrained screw-rod systems significantly impacts primarily stability. Therefore, comparisons of our results concerning stability afforded by the rigid posterior implants are difficult to transfer to results of non-rigid constructs. In addition, we analyzed stability afforded with segmental posterior instrumentations using LMS, CPS, and combinations thereof. Hence, screws at each level were implanted posteriorly which confers different mechanics as supposed with end-level fixation only. One of the authors [51] already reported that if end-level posterior constrained fixation is applied to stabilize anterior grafted 3-level corpectomies, there are considerable differences concerning primary stability whether LMS or CPS were used. Such observations are in line with that of Cheng [13] and Ames [4]. Cheng performed biomechanical testing of posterior fixation at C0–T1 and found no significant differences in flexion–extension ROM between segmental fixation at each level and selective/skipped fixation at C0, C4, and T1. But, in lateral bending and axial rotation, overall motion increased significantly with the selective/skipped fixation. Similar to the current study, Cheng provided some level of comfort if LMS or CPS cannot be placed at every level in long posterior stabilizations or if a CPS cannot be placed bilaterally. Ames constructed a 3-column injury model C6–T1, and compared constrained posterior to anterior and combined stabilizations. Change of number of posterior fixation points had a significant stabilizing effect on adjacent levels within the construct. Summarizing, it has to be stressed that results of our model are representative for posterior constructs in which screws can be placed at each segment C4–C7.
The current biomechanical study assessed primary construct stability in terms of reduction of ROM. Notably, failure of an anterior plate or LMS construct is primarily caused by increased motion between the vertebral body and the screws [41]. Hence, fatigue analyses are indicated that might show distinct differences among the constructs tested here [19, 41]. Kothe [34] performed segmental stabilization of 3-level circumferentially destabilized spines with segmental fixation C3–C6 using all-LMS or all-CPS constructs. Significant differences in primary stability existed only for lateral bending. But, after cyclic loading, the decrease in stability was less with CPS fixation and ROM was significantly more reduced with CPS compared to the LMS construct. For the LMS, but not for the CPS construct, BMD was also shown to influence stability after cyclic loading with degradation and loosening observed at the end-level anchors. Isomi [24] tested stability patterns of an anterior construct using constrained plates for 1- and 3-level corpectomy models. After instrumentation, they noted an 80% decrease of ROM for both models. After fatigue, loading ROM increased significantly in the 3-level corpectomy group, but not in the 1-level group. Their study showed that 1- and 3-level systems afforded similar primary stability, but the capability of the 3-level system was significantly reduced with fatigue loading. We assessed primary stability, and no account was taken for the forces and fatigue noted during repetitive cyclic loading experienced clinically. Repetitive cyclic loading challenges constructs with short screw end-level fixation in merely cancellous bone (anterior plate, all-LMS) far more than those with the transpedicular cortical screw anchorage (CPS-bilat, CPS unilat and ATPS) [33, 34]. The mechanical superior characteristics of transpedicular anchorage compared to screws in the lateral mass or vertebral body [26, 27] might have significant impact on construct survival. Therefore, because failure mechanisms and fatigue properties of our instrumentations were not studied, further research is needed to obtain a complete understanding of the constructs studied.
In the current study, the order of construct testing was alternated to eliminate bias by intratesting degeneration. Although it would have been desirable to test all constructs in a random order to account for any changes, this was not possible. We tested the CPS-bilat last in each specimen of group 1 because LMS placement after CPS was deemed inappropriate regarding degraded bone for the LMS placement. On the contrary, axial pull-out tests of CPS placed for revision of LMS showed no significant difference in pull-out strength compared to primary CPS placed in virgin bone [22]. Nevertheless, some degradation of the lateral mass and even pedicle core was recognized during testing that placed the CPS-bilat group into slight disadvantage compared to the others and in particular to the CPS-unilat. The right-sided CPS within the CPS-bilat was tested last in Group 1. Hence, degradation of the cancellous bone rather than the cortical pedicle by the preceding tests of the ATPS-1 might have reduced osseus anchorage of the right-sided CPS. In addition, rod bending can impact ROM testing [36]. For the CPS-bilat, the rods had to be bent in the coronal plane on both sides to accommodate locking to the CPS at C4 and C7 and to the LMS at C5 and C6 (Fig. 6). Thus, load resistance of the 3.5 mm rods was reduced in sagittal plane in comparison to the CPS-unilat and the all-LMS. With the all-LMS there was no rod contortion at all. This can explain that we found statistically significant differences between the CPS-bilat and CPS-unilat in flexion–extension in favor for the latter.
Fig. 6.
Example of a potted specimen after testing with CPS-unilat. CPS left-sided at the end-levels C4 and C7 necessitating bending of the 3.5 mm rod in the coronal plane to accommodate connection with the LMS at C5 and C6. Right side instrumented sequentially from C4 to C7 using LMS. Note straight rod on the right side
Report of ATPS-plate prototype testing
Multilevel construct failures and the ignition of failure process most often occur early during the postoperative course depending on the immediate stability conferred by the construct [24, 31, 49]. With ATPS, enhanced anchorage by transpedicular fixation was suggested [30]. Thus, we sought to evaluate multidirectional stabilizing capabilities of common anterior, posterior, and combined instrumentations compared to an ATPS-plate prototype. The first two prototypes failed at their screw–plate connection which was related to prototyping issues and particulary due to the large angle formed by the ATPS trajectory and the anterior vertebral body cortex that has to be accomplished by any ATPS plate [30]. Our back-up solution incorporated the concept of ATPS placement at one single level among placement of a VBS (Fig. 2). Even though the plate-like system enabled us to test the concept of ATPS [30], it did not resemble the constrained properties of anterior plates in use including a rectangular solid design that is not susceptible to bending in flexion–extension and that can be pressed flush to the anterior vertebral body cortex, thus affording plate–bone friction and compression by screw fixation. However, even with the current design, we showed that ROM was reduced below the intact state in all modes of testing for all specimens. In addition, a biomechanically more rigid construct could be constructed in comparison to the standard anterior plate for all modes of testing in all specimens although statistical significance was limited to the axial rotation testing. Notably, the ATPS plate was comparable to its posterior counterparts in several modalities. In flexion–extension, the ability to reduce ROM was distributed among the posterior instrumentations (see Table 1a) while significant differences existed only compared to the all-LMS construct of group 2 compared to the ATPS-1 of group 1 and compared to the 360° construct. One would assume that flexion–extension forces are the most important forces instrumentations that have to resist during the postoperative bracing period. Actually, patients immobilized in a cervical collar after multilevel surgery are likely to experience the least restriction axial rotation in the collar [48, 52]. Thus, it is to be noted that with axial rotation the ATPS plate performed best without significant differences to the posterior counterparts and even not different between the ATPS-2 and the 360° construct. With ATPS fixation and anterior plate connection, a larger lever arm is constructed in regard to the ICR in axial plane when compared to the posterior constructs. In contrast, in lateral bending, there was a marked difference between the ATPS and posterior systems. Both ATPS and VBS had to be placed close to each other within the ATPS prototype, and thus, close to the ICR of lateral bending in the coronal plane affording a lever-arm similar to that of the anterior plate but smaller compared to the posterior systems (Table 1c).
Limitations
The current laboratory study was comparable to previous ones concerning number and distribution of specimens, alternation of instrumentations, and the setup [4, 8, 13−17, 23, 24, 43, 50, 54]. However, there are limitations in this study. We studied isolated cadaveric specimens with the muscular tissue removed. Therefore, the study did not include forces representing muscular interactions that might have altered the load-deformation characteristics. Muscular contractions and compressive preloading stabilize the cervical spine. Thus, when our findings are applied to the clinical scenario, the clinical stability is likely to be better than documented.
Biomechanical testing was performed at C4–C7 not including the increased forces faced at the occipito-cervical [61] or cervico-thoracic junction [39]. Hence, the benefit by transpedicular anchorage as used in the current study might be enhanced if these transition zones are incorporated in multilevel constructs.
The anterior plate was outperformed by the other constructs in most tests. We used a semi-rigid plate although constrained ones are thought to provide better fixation. But we assessed primary construct stability, and studies showed that rigid and semi-rigid plates perform similarly concerning primary construct stability [11, 18]. Moreover, the current screw–plate construct provided excellent compression of the plate to the vertebrae. We do not expect a meaningful change of results with the use of different plates.
When an anterior corpectomy defect is successfully reconstructed using a distractable cage, an all-LMS construct serves comparable results to the CPS-unilat, CPS-bilat, and the 360° construct. Most biomechanical studies analyze the performance of posterior constructs after an anterior corpectomy reconstruction [50] or with the anterior column left intact, as in a study of Dahdaleh [14] who noted no significant difference between an LMS construct and a 360° construct (C3–C7). But it is to be noted that Dahdaleh’s and our model do not offer information for the clinical setting where posterior instruments have to shield loads from the anterior weakened column as in posterior multilevel stabilizations for palliative tumor care or in fracture treatment [4, 39]. In such cases, the usage of CPS compared to LMS as well as bilateral compared to unilateral CPS might be of advantage [34].
Conclusions
There are reasons for inventing a technique for anterior-only fixation offering increased primary stability, such as ATPS, in selected pathologies with high instability [29, 30, 32]. With the current study, we offer first biomechanical characteristics of the ATPS concept incorporated in a prototype and offer valuable information regarding selective usage of posterior and anterior transpedicular anchorage within instrumentations intended to stabilize a 2-level corpectomy.
As regards our three main research questions: (1) our results add data to a biomechanical rationale opting for circumferential stabilization after 2-level corpectomies; (2) the first ATPS prototype tested offered encouraging results with primary stability comparing well to its clinically accepted posterior counterparts; and (3) unilateral end-level pedicle screw fixation for stabilization of 2-level corpectomy constructs was shown sufficient avoiding the potential risks with bilateral pedicle screw placements.
In conclusion, fatigue load testing of an advanced ATPS prototype with a modern state-of-the-art-constrained screw–plate interface will have to show its biomechanical characteristics under cyclic loading and failure load characteristics.
Acknowledgments
The authors thank Synthes for financial support to perform the biomechanical study and for implants provided. With the ATPS concept, there is no patent closed or pending that might hinder further engineering on the issue.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00586-011-1792-8
References
- 1.Abddullah KG, Steinmetz MP, Mroz TE. Morphometric and volumetric analysis of the lateral masses of the lower cervical spine. Spine. 2009;34:1476–1479. doi: 10.1097/BRS.0b013e3181a8f649. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Shono Y, Taneichi H, Itoh M, Kaneda K. Correction of cervical kyphosis using pedicle screw fixation systems. Spine. 1999;24:2456–2462. doi: 10.1097/00007632-199912010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Acosta LF, Aryan HE, Chou D, Ames CP. Long-term biomechanical stability and clinical improvement after extended multilevel corpectomy and circumferential reconstruction of the cervical spine using titanium mesh cages. J Spinal Disord Tech. 2008;21:165–174. doi: 10.1097/BSD.0b013e3180654205. [DOI] [PubMed] [Google Scholar]
- 4.Ames PC, Bozkus MH, Chamberlain RH, Acosta FL, Papadopoulos SM, Sonntag VKH, Crawford NR. Biomechanics of stabilization after cervicothoracic compression-flexion injury. Spine. 2005;30:1505–1512. doi: 10.1097/01.brs.0000167824.19875.e9. [DOI] [PubMed] [Google Scholar]
- 5.Aramomi M, Masaki Y, Koshizuka, Kadota R, Okawa A, Koda M, Yamazaki M. Anterior pedicle screw fixation for multilevel cervical corpectomy and spinal fusion. Acta Neurochir. 2008;150:575–582. doi: 10.1007/s00701-008-1574-1. [DOI] [PubMed] [Google Scholar]
- 6.Aryan HE, Sanchez-Mejia RO, Ben-Haim S, Ames CP. Successful treatment of cervical myelopathy with minimal morbidity by circumferential decompression and fusion. Eur Spine J. 2007;16:1401–1409. doi: 10.1007/s00586-006-0291-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech. 2000;15:633–648. doi: 10.1016/S0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 8.Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VKH, Papadopoulos SM, Crawford NR. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine. 2005;30:915–922. doi: 10.1097/01.brs.0000158949.37281.d7. [DOI] [PubMed] [Google Scholar]
- 9.Bransford RJ, Russo A, Freeborn M, Nuyen Q, Lee MJ, Chapman J, Bellabarba C (2009) Posterior C2 instrumentation: accuracy and risks associated with four techniques. In: 16th international meeting on advanced spine technologies, Vienna [DOI] [PubMed]
- 10.Brazenor GA. Comparison of multisegment anterior cervical fixation using bone graft versus a titanium rod and buttress prosthesis. Spine. 2007;32:63–71. doi: 10.1097/01.brs.0000250304.24001.24. [DOI] [PubMed] [Google Scholar]
- 11.Brodke DS, Klimo P, bachus KN, Braun JT, Dailey AT. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg. 2006;88-A:1566–1573. doi: 10.2106/JBJS.E.00305. [DOI] [PubMed] [Google Scholar]
- 12.Cha SH, Kim C, Choi BK, Kim HJ, Baek SY. C-arm assessment of cervical pedicle screw-coaxial fluoroscopy and oblique view. Eur Spine J. 2007;32:1721–1727. doi: 10.1097/BRS.0b013e3180b9f29b. [DOI] [PubMed] [Google Scholar]
- 13.Cheng BC, Hafez MA, Cunningham B, Hassan S, Welch WC. Biomechanical evaluation of occipitocervicothoracic fusion: impact of partial or sequential fixation. Spine J. 2008;8:821–826. doi: 10.1016/j.spinee.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 14.Dahdaleh NS, Nakamura S, Torner JC, Lim TH, Hitchon PW. Biomechanical rigidity of cadaveric cervical spine with posterior versus combined posterior and anterior instrumentation. J Neurosurg Spine. 2009;10:133–138. doi: 10.3171/2008.11.SPI08416. [DOI] [PubMed] [Google Scholar]
- 15.Dailey A, Fassett D, Finn M, Bacchus K, Brodke D (2008) Do dynamic cervical plates provide adequate stability in flexion distraction injuries? In: Annual meeting of the CSRS, Austin, TX
- 16.Dmitriev AE, Kuklo TR, Jr Lehman RA, Rosner MK. Stabilizing potential of anterior, posterior, and circumferential fixation for multilevel cervical arthrodesis. Spine. 2007;32:E188–E196. doi: 10.1097/01.brs.0000257577.70576.07. [DOI] [PubMed] [Google Scholar]
- 17.Do Koh Y, Lim TH, Won You J, Eck J, An HS. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine. 2001;26:15–21. doi: 10.1097/00007632-200101010-00005. [DOI] [PubMed] [Google Scholar]
- 18.Dvorak MF, Pitzen T, Zhu Q, Gordon JD, Fisher CG, Oxland TR. Anterior cervical plate fixation: a biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine. 2005;30:294–301. doi: 10.1097/01.brs.0000152154.57171.92. [DOI] [PubMed] [Google Scholar]
- 19.Hart R, Gillard J, Prem S, Shea M, Kitchel S. Comparison of stiffness and failure load of two cervical spine fixation techniques in an in vitro human model. J Spinal Disord Tech. 2005;18:S115–S118. doi: 10.1097/01.bsd.0000132288.65702.6e. [DOI] [PubMed] [Google Scholar]
- 20.Hart RA, Tatsumi RL, Hiratzka JR, Yoo JU. Perioperative complications of combined anterior and posterior cervical decompression and fusion crossing the cervico-thoracic junction. Spine. 2008;33:2887–2891. doi: 10.1097/BRS.0b013e318190affe. [DOI] [PubMed] [Google Scholar]
- 21.Hasegawa K, Hirano T, Shimoda H, Homma T, Morita O. Indications for cervical pedicle screw instrumentation in nontraumatic lesions. Spine. 2008;33:2284–2289. doi: 10.1097/BRS.0b013e31818043ce. [DOI] [PubMed] [Google Scholar]
- 22.Hostin RA, Wu C, Perra JH, Polly DW, Akesen B, Wroblewski M. A biomechanical evaluation of three revision screw strategies for failed lateral mass fixation. Spine. 2008;33:2415–2421. doi: 10.1097/BRS.0b013e31818916e3. [DOI] [PubMed] [Google Scholar]
- 23.Ianuzzi A, Zambrano I, Tataria J, Ameerally A, Agulnick M, Little Goodwin JSL, Stephen M, Khalsa PS. Biomechanical evaluation of surgical constructs for stabilization of cervical teardrop fractures. Spine J. 2006;6:514–523. doi: 10.1016/j.spinee.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Isomi T, Panjabi MM, Wang JL, Vaccaro AR, Garfin SR, Patel T. Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine. 1999;24:2219–2223. doi: 10.1097/00007632-199911010-00008. [DOI] [PubMed] [Google Scholar]
- 25.Ito Y, Sugimoto Y, Tomioka M, Hasegawa Y, Nakago K, Yagata Y. Clinical accuracy of 3D fluoroscopy-assisted cervical pedicle screw insertion. J Neurosurg Spine. 2008;9:450–453. doi: 10.3171/SPI.2008.9.11.450. [DOI] [PubMed] [Google Scholar]
- 26.Johnston LT, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–672. doi: 10.1016/j.spinee.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 28.Kast E, Mohr K, Richter HP, Börm W. Complications of transpedicular screw fixation in the cervical spine. Eur Spine J. 2006;15:327–334. doi: 10.1007/s00586-004-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koller H, Acosta F, Tauber M, Fox M, Martin H, Forstner R, Augat P, Penzkofer R, Pirich C, Kässmann H, Resch H, Hitzl W. Cervical anterior transpedicular screw fixation (ATPS)—Part II. Accuracy of manual insertion and pull-out strength of ATPS. Eur Spine J. 2008;17:539–555. doi: 10.1007/s00586-007-0573-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koller H, Hempfing A, Acosta F, Fox M, Scheiter A, Tauber M, Holz U, Resch H, Hitzl W. Cervical anterior transpedicular screw fixation. Part I: Study on morphological feasibility, indications, and technical prerequisites. Eur Spine J. 2008;17:523–538. doi: 10.1007/s00586-007-0572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koller H, Hempfing A, Ferraris L, Meier O, Metz-Stavenhagen P. 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J. 2006;16:2055–2071. doi: 10.1007/s00586-007-0398-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koller H, Hitzl W, Acosta F, Tauber M, Zenner J, Resch H, Yukawa Y, Meier O, Schmidt R, Mayer M (2009) In vitro study of accuracy of cervical pedicle screw insertion using an electronic conductivity device (ATPS part III). Eur Spine J 18(9):1300–1313 [DOI] [PMC free article] [PubMed]
- 33.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 34.Kothe R, Rüter W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29:1869–1875. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 35.Kristof RA, Kiefer T, Thudium M, Ringel F, Stoffel M, Kovacs A, Mueller C-A (2009) Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J 18(12):1951–1956 [DOI] [PMC free article] [PubMed]
- 36.Lindsey C, Deviren V, Xu Z, Yeh RF, Puttlitz CM. The effects of rod countering on spinal construct fatigue strength. Spine. 2009;31:1680–1687. doi: 10.1097/01.brs.0000224177.97846.00. [DOI] [PubMed] [Google Scholar]
- 37.Lu J, Wu X, Li Yonggang, Kong X. Surgical results of anterior corpectomy in the aged patients with cervical myelopathy. Eur Spine J. 2007;17:129–135. doi: 10.1007/s00586-007-0518-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mummaneni PV, Dhall SS, Rodts GE, Haid RW. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515–521. doi: 10.3171/SPI.2008.10.08226. [DOI] [PubMed] [Google Scholar]
- 39.O’Brien JR, Dmitriev AE, Yu W, Gelb D, Ludwig S. Posterior-only stabilization of 2-column and 3-column injuries at the cervicothoracic junction. J Spinal Disord. 2009;22:340–346. doi: 10.1097/BSD.0b013e31816f68d9. [DOI] [PubMed] [Google Scholar]
- 40.O’Shaughnessy BA, Liu JC, Hsieh PC, Koski TR, Ganju A, Ondra SL. Surgical treatment of fixed cervical kyphosis with myelopathy. Spine. 2008;33:771–778. doi: 10.1097/BRS.0b013e3181695082. [DOI] [PubMed] [Google Scholar]
- 41.Panjabi MM, Isomi T, Wang JL. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs. Spine. 1999;24:2383–2388. doi: 10.1097/00007632-199911150-00016. [DOI] [PubMed] [Google Scholar]
- 42.Panjabi MM, Krag M, Summers D, videmann T. Biomechanical time-tolerance of fresh cadaveric human spine specimens. J Orthop Res. 1985;3:292–300. doi: 10.1002/jor.1100030305. [DOI] [PubMed] [Google Scholar]
- 43.Porter RW, Crawford NR, Chamberlain RH, Park SC, Detwiler PW, Apostolides PJ, Sonntag VKH. Biomechanical analysis of multilevel cervical corpectomy and plate constructs. J Neurosurg. 2003;99:98–103. doi: 10.3171/spi.2003.99.1.0098. [DOI] [PubMed] [Google Scholar]
- 44.Rath SA, Moszko S, Schäffner PM, Cantone G, Braun V, Richter HP, Antoniadis G. Accuracy of pedicle screw insertion in the cervical spine for internal fixation using frameless stereotactic guidance. J Neurosurg Spine. 2008;8:237–245. doi: 10.3171/SPI/2008/8/3/237. [DOI] [PubMed] [Google Scholar]
- 45.Ratliff J, Cooper PR. Cervical laminoplasty: a critical review. J Neurosurg. 2003;98:230–238. doi: 10.3171/spi.2003.98.3.0230. [DOI] [PubMed] [Google Scholar]
- 46.Sakamoto T, Neo M, Nakamura T. Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine. 2004;22:2510–2514. doi: 10.1097/01.brs.0000144404.68486.85. [DOI] [PubMed] [Google Scholar]
- 47.Sakaura H, Hosono N, Mukai Y, Ishii T, Iwasaki M, Yoshikawa H. Long-term outcome of laminoplasty for cervical myelopathy due to disc herniation: a comparative study of laminoplasty and anterior spinal fusion. Spine. 2005;30:756–759. doi: 10.1097/01.brs.0000157415.79713.7e. [DOI] [PubMed] [Google Scholar]
- 48.Sandler AJ, Dvorak J, Humke T, Grob D, Daniels W. The effectiveness of various cervical orthoses. Spine. 1996;21:1624–1629. doi: 10.1097/00007632-199607150-00002. [DOI] [PubMed] [Google Scholar]
- 49.Schlenk RP, Stewart T, Benzel EC (2003) The biomechanics of iatrogenic spinal destabilization and implant failure. Neurosurg Focus 15(3):E2 [DOI] [PubMed]
- 50.Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M. Effect of constrained posterior screw and rod systems for primary stability: biomechanical in vitro comparison of various instrumentations in a single-level corpectomy model. Eur Spine J. 2005;14:372–380. doi: 10.1007/s00586-004-0763-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M. Pedicle screws enhance primary stability in multilevel cervical corpectomies: biomechanical in vitro comparison of different implants including constrained and nonconstrained posterior instruments. Spine. 2003;16:1821–1828. doi: 10.1097/01.BRS.0000083287.23521.48. [DOI] [PubMed] [Google Scholar]
- 52.Schneider AM, Hipp JA, Nguyen L, Reitman CA. Reduction in head and intervertebral motion provided by 7 contemporary cervical orthoses in 45 individuals. Spine. 2007;32:E-1–E-6. doi: 10.1097/01.brs.0000251019.24917.44. [DOI] [PubMed] [Google Scholar]
- 53.Sembrano JN, Mehbod AA, Garvey TA, Denis F, Perra JH, Schwender JD, Transfeldt EE, Winter RB, Wroblewski M. A concomitant posterior approach improves fusion rates but not overall reoperation rates in multilevel cervical fusion for spondylosis. J Spinal Disord Tech. 2009;22:162–169. doi: 10.1097/BSD.0b013e318175d821. [DOI] [PubMed] [Google Scholar]
- 54.Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2003) Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine 28:2352–2357, 2358 [DOI] [PubMed]
- 55.Steinmetz MP, Stewart TJ, Kager CD, Benzel EC, Vaccaro AR. Cervical deformity correction. Neurosurg. 2007;60(Suppl):S90–S97. doi: 10.1227/01.NEU.0000249237.43354.D9. [DOI] [PubMed] [Google Scholar]
- 56.Suda K, Kajino T, Moridaira H, Limoto S, Taneichi H. How to avoid fatal vascular complications caused by pedicle screws—surgical strategy for safe screw placement. Geneva: Spineweek; 2008. [Google Scholar]
- 57.Wei-bing X, Wun-Jer S, Lv Gang, Yue Z, Ming-xi J, Lian-shun J. Reconstructive techniques study after anterior decompression of multilevel cervical spondylotic myelopathy. J Spinal Disord Tech. 2009;22:511–515. doi: 10.1097/BSD.0b013e3181a6a1fa. [DOI] [PubMed] [Google Scholar]
- 58.Wilke HJ, Claes L, Schmitt H, Wolf S. A universal spine tester for in vitro experiments with muscle force simulation. Eur Spine J. 1994;3:91–97. doi: 10.1007/BF02221446. [DOI] [PubMed] [Google Scholar]
- 59.Wilke HJ, Jungkunz B, Wenger K, Claes LE. Spinal segment range of motion as a function of in vitro test conditions: effects of exposure period, accumulated cycles, angular-deformation rate, and moisture condition. Anat Rec. 1998;251:15–19. doi: 10.1002/(SICI)1097-0185(199805)251:1<15::AID-AR4>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 60.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7:148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wolfa CE. Anatomical, biomechanical, and practical considerations in posterior occipitocervical instrumentation. Spine J. 2006;6:225S–232S. doi: 10.1016/j.spinee.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 62.Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H, Machino M. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2008;18:1293–1299. doi: 10.1007/s00586-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yukawa Y, Kato F, Ito K, Nakashima H, Machino M. Anterior cervical pedicle screw and plate fixation using fluoroscope-assisted pedicle axis view imaging: a preliminary report of a new cervical reconstruction technique. Eur Spine J. 2009;18:911–916. doi: 10.1007/s00586-009-0949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]