Abstract
Objective
A longitudinal cohort of automobile manufacturing workers (n = 1214) was examined for: 1) prevalence and persistence of specific upper extremity musculoskeletal disorders (UEMSDs) such as lateral epicondylitis and de Quervain's disease, and non-specific disorders (NSDs) defined in symptomatic individuals without any specific disorder, and 2) disorder prognoses based on symptom characteristics and other factors.
Methods
Eight specific disorders were identified through case definitions based on upper extremity physical examinations and symptom surveys administered on three occasions over six years.
Results
At baseline, 41% of the cohort reported upper extremity symptoms; 18% (n = 214) of these had NSDs. In each survey, tendon-related conditions accounted for over half of the specific morbidity. Twenty-five percent had UEMSDs in multiple anatomical sites, and most with hand/wrist disorders had two or more hand/wrist UEMSDs. Persistence for all specific disorders decreased with length of follow-up. Specific UEMSDs were characterized by greater pain severity and functional impairment, and more lost work days than NSDs.
Conclusions
Upper extremity symptoms and diagnoses vary over time. NSDs may be the early stages of conditions that will eventually become more specific. NSDs and overlapping specific UEMSDs should be taken into account in UEMSD classification.
Introduction
Upper extremity musculoskeletal disorders (UEMSDs) are common among workers in a variety of manufacturing and other occupational settings. Reviews of studies examining health problems in conjunction with ergonomic stressors [Bernard 1997, National Academy of Sciences 1998, 2001] include associations with specific UEMSDs as well as with generalized symptoms such as hand pain or neck stiffness. Single epidemiologic studies of upper extremity musculoskeletal disorders (UEMSDs) in the workplace have tended to focus on either one or two specific disorders (such as rotator cuff tendonitis or carpal tunnel syndrome) or on general signs or symptoms indicative of UEMSDs without regard to diagnostic category. The literature remains sparse on the proportions and progression of specific UEMSDs that occur in particular working populations [Bovenzi 1991, Roquelaure, et al. 2002, Gerr, et al. 2002, Aublet-Cuvelier, et al. 2007]. The existence of UEMSDs that do not conform to diagnostic conventions is acknowledged [Harrington, et al. 1998, Sluiter, et al. 2000]. However, few epidemiologic studies have explicitly identified the relative frequency of such non-specific UEMSDs [Silverstein, et al. 1986, Latko, et al. 1999].
A cohort of automobile manufacturing workers has been followed over a seven-year period, with three surveys of musculoskeletal morbidity and exposures [Punnett 1998, Punnett, et al. 2004]. In each survey, symptom reports and physical examination findings were used to identify eight different sub-groups of upper extremity cases, approximating as closely as possible the findings that are typically used in the clinical setting for diagnostic purposes (specific UEMSDs). Those who had symptoms but did not conform to the criteria for these epidemiologic case definitions were regarded as having non-specific UEMSDs (NSDs).
The objective of this study was to characterize the prevalence and persistence of specific and non-specific UEMSD types in this longitudinal cohort. Additionally, symptom characteristics, lost work time, and case progression in non-specific and specific UEMSDs were compared to see if the two groups had different prognoses or if NSDs predicted progression to specific conditions. A third goal was to determine whether the probability of leaving employment was associated with either specific or non-specific disorders.
Methods
A fixed cohort of 1,214 automobile manufacturing workers (baseline demographics: 46.5 ± 8.2 years of age; 81.6% male; 21.5 ± 6.5 years company seniority) [Punnett 1998, Punnett, et al. 2004] was examined on three occasions (1992, 1993, and 1998) for signs and symptoms of UEMSDs. A physical examination assessed the presence of muscle/tendon, joint or nerve problems in four upper extremity sites: neck, shoulder/upper arm, elbow/forearm, or hand/wrist [Silverstein and Fine 1984]. An interview included questions about symptoms during the past year in each of the four sites. Those reporting symptoms were asked additional questions regarding frequency and severity of discomfort, difficulty performing activities of daily living, and medical attention sought. One-year (n = 790) and six-year (n = 519) follow-up examinations and interviews included the same data items. Recruitment at six-year follow-up was not conditional on participation at one-year follow-up; 365 subjects were seen at all three time periods. The same registered nurse performed the physical examination in all three surveys. She was blinded to subject exposure status, and had no record of previous examination results. Written informed consent was obtained at the beginning of each examination/interview.
Scores of pain severity and functional impairment for each upper extremity region were constructed from questionnaire responses. The responses to inquiries regarding current pain, pain during the past week and worst pain during the past year on visual analogue scales were summed to yield the pain severity score (range: 0-30). Functional impairment was assessed by questions derived from instruments such as the SPADI [Roach, et al. 1991] and the Brigham Carpal Tunnel questionnaire [Levine, et al. 1993] and scored as the sum of responses to ten questions specific to each body region (range: 0-50). The upper extremity site (neck, shoulder, elbow or hand/wrist) with the maximum pain severity and functional impairment score was used in each respective analysis. Those with no symptoms were assigned a score of zero for each scale.
Case definitions for specific UEMSDs were developed from criteria documents [Harrington, et al. 1998, Sluiter, et al. 2000, Piligian, et al. 2000], physician protocol [Cherniack 2001] and physician consultation [Dillon 1998]. Eight specific and not mutually exclusive syndromes were defined on the basis of physical examination findings and symptom reports: de Quervain's disease, hand/wrist/forearm (h/w/f) extensor tendonitis, h/w/f flexor tendonitis, carpal tunnel syndrome (CTS), lateral epicondylitis, medial epicondylitis, rotator cuff tendonitis and radiating neck complaints (Table I). It was not possible to detect cases of hand-arm vibration syndrome on the basis of the available signs and symptoms, and CTS was the only nerve compression disorder for which likely cases could be defined.
Table I. Upper extremity musculoskeletal disorder (UEMSD) epidemiologic case definitions **.
| Disorder | Physical examination finding(s) * | Symptoms |
|---|---|---|
| A. Carpal tunnel syndrome (CTS) | classic or probable finding on Phalen's test | classic or probable finding on Katz/Stirrat [Katz and Stirrat 1990] hand diagram |
| B. De Quervain's disease | pain on Finkelstein's test or on thumb extension | hand/wrist symptoms |
| C. Hand/wrist/forearm (h/w/f) extensor tendonitis | pain on wrist and/or finger extension | hand/wrist symptoms |
| D. H/w/f flexor tendonitis | pain on wrist and/or finger flexion | hand/wrist symptoms |
| E. Lateral epicondylitis | pain on resisted pronation with flexed wrist | elbow symptoms |
| F. Medial epicondylitis | pain on resisted pronation with clenched fist | elbow symptoms |
| G. Radiating neck complaints | pain on active or passive neck flexion, passive neck extension, or active or passive lateral rotation | neck symptoms |
| H. Rotator cuff tendonitis (neck/shoulder Disorder) | pain on shoulder abduction, resisted lateral or medial rotation, or elbow flexion | shoulder/upper arm symptoms |
Pain on a particular physical exam maneuver was defined as a rating of 3 or greater on a 0-10 scale.
Both physical examination finding and symptom criteria must be met for all case definitions.
The prevalence of each specific UEMSD was computed in each survey: baseline (T0), one-year follow-up (T1), and six-year follow-up (T2). Disorder frequencies were computed overall and by level of physical ergonomic exposure at T0, using an exposure index previously described [Punnett 1998, Punnett and van der Beek 2000]. This index summed workers' ratings of exposure to a variety of ergonomic stressors, including force, repetition and postural factors. For the present analyses, the index was dichotomized at the midpoint (0-12 vs. 13-25). Similarly, the persistence of each specific UEMSD was computed overall and by exposure status at T0. Persistence in each survey was defined as the frequency (per 100) of subjects who met the same case definitions for specific UEMSD type on the noted previous occasion.
Since there is interest in the extent of overlap among different UEMSD subgroups, for each survey, the percentage overlap per body region (elbows and hand/wrist) on a side-specific basis among prevalent cases was also computed.
Non-specific UEMSDs (NSDs) were defined as conditions in individuals with symptoms on at least 12 occasions in the past year, or lasting at least one week, that did not meet any of the specific case definitions. If a subject had a specific syndrome in any of the four upper extremity sites, s/he was classified as specific even if there were non-specific symptoms or signs in other regions. The Wilcoxon rank test was used to compare symptom characteristics between specific and non-specific UEMSDs. Comparison of percentage of subjects progressing to a 1) specific syndrome from either a NSD or a non-symptomatic state, and 2) non-symptomatic state from either a specific syndrome or a NSD, was achieved through a two-sample test of proportions. A value of p ≤ 0.05 was regarded as statistically significant.
Management information system records were reviewed to determine employment status of all cohort members at T2. Reasons for not being available for follow-up included: temporary illness/injury/disability, deceased, pensioned, moved and other permanent separation. Both temporary illness/injury/disability and permanent separation were hypothesized to be associated with musculoskeletal disorder status. The percentage of subjects unavailable at T2 due to either of these reasons was compared among specific and non-specific UEMSDs and non-cases (no physical examination findings and no symptoms) at T0. These analyses were further stratified on dichotomized exposure score at T0.
This study was approved by the Institutional Review Boards of the University of Massachusetts Lowell and Brigham & Women's Hospital. Data analysis was performed with SAS (SAS Institute Inc., Cary, NC) and Stata (Stata Corporation, College Station, TX) software for personal computer.
Results
Prevalence of specific and non-specific UEMSDs
At baseline, the overall prevalence of upper extremity symptoms (one or more sites) was 41%. Of these, 283 subjects (23% prevalence) met the screening case definition for at least one specific syndrome; 45% of these (n = 128) had two or more different syndromes, while 25% had syndromes in more than one anatomical site. The most common conditions were tendon-related, especially rotator cuff tendonitis, de Quervain's disease (tenosynovitis of the thumb extensor), and hand/wrist/forearm flexor and extensor tendonitis. Relative frequencies of these specific conditions were similar in both follow-up surveys (Table II), although the prevalences of some conditions tended to decrease over time.
Table II.
Overall prevalence [% (n)] of specific UEMSDs in each survey. Automobile manufacturing workers, Detroit, MI, USA, 1992-1998.
| UEMSD type | Baseline (T0) (n = 1198) | 1-year follow-up (T1) (n = 771) | 6-year follow-up (T2) (n = 506) |
|---|---|---|---|
| Carpal tunnel syndrome | 2.2 (27) | 3.8 (29) | 1.2 (6) |
| de Quervain's disease | 8.7 (106) | 6.9 (53) | 5.3 (27) |
| Extensor tendonitis | 7.3 (89) | 5.3 (41) | 4.4 (22) |
| Flexor tendonitis | 7.7 (94) | 6.5 (50) | 4.4 (22) |
| Lateral epicondylitis | 3.3 (40) | 3.5 (27) | 1.4 (7) |
| Medial epicondylitis | 2.2 (26) | 3.1 (24) | 3.2 (16) |
| Radiating neck complaints | 2.4 (29) | 3.9 (30) | 4.1 (21) |
| Rotator cuff tendonitis | 12.0 (145) | 11.1 (86) | 9.3 (47) |
| Non-specific disorder | 18.0 (214) | 10.4 (80) | 13.7 (69) |
Another 214 (18%) participants at T0 had only NSDs, including 49 with symptoms and examination findings and 165 with symptoms only. About one-half of the persons with NSDs had two or more upper extremity areas affected; 60% (n = 123) of them had wrist or hand findings. There were fewer relative numbers of NSDs in the follow-up surveys (see “Symptom characteristics and progression of specific and non-specific syndromes” below).
Seven-tenths of those with side-specific shoulder symptoms at T0 had findings that were consistent with rotator cuff tendonitis. This fraction increased to about 80% in each of the follow-up surveys. Among those with elbow symptoms, side-specific lateral epicondylitis and medial epicondylitis together accounted for approximately one-half of the elbow disorders at T0, one-half to two-thirds of those at T1, and 70-80 percent at T2. That is, the proportion of both side-specific shoulder and elbow NSDs decreased during the seven-year study period.
One-half of those with hand/wrist disorders on each side had specific conditions. This proportion held in each of the three survey periods. At baseline, cases were approximately evenly divided among the tendon-related disorders – h/w/f flexor tendonitis, h/w/f extensor tendonitis, and de Quervain's disease; a much smaller percentage (∼10%) met the CTS case definition at T0 and T2. At T1, the relative frequency of CTS symptoms and signs among hand/wrist disorders was somewhat higher, at around 20%. In contrast to shoulder and elbow NSDs, the percentage of hand/wrist NSDs remained a consistent one-half of all morbidity in this body region during all three surveys.
Prevalence of both specific and non-specific disorders across all three surveys was greater in those with higher self-reported baseline exposure to ergonomic stressors (Table III). Overall, there were only very small differences in ergonomic exposure scores between the workers with specific and non-specific disorders in all three survey periods.
Table III. Prevalence ratios (high exposure/low exposure*) at T0, T1 and T2.
| UEMSD type | Prevalence ratio at T0 (95% CI) | Prevalence Ratio at T1 (95% CI) | Prevalence Ratio at T2 (95% CI) |
|---|---|---|---|
| Carpal tunnel syndrome | 2.1 (0.8, 5.2) | 1.8 (0.9, 3.7) | 3.7 (0.4, 31.3) |
| De Quervain's disease | 1.3 (0.9, 2.0) | 2.0 (1.1, 3.8) | 1.8 (0.8, 4.2) |
| Extensor tendonitis | 1.5 (1.0, 2.4) | 3.0 (1.3, 6.8) | 6.6 (1.6, 28.3) |
| Flexor tendonitis | 1.7 (1.1, 2.6) | 2.5 (1.2, 5.0) | 6.6 (1.6, 28.3) |
| Lateral epicondylitis | 1.7 (0.9, 3.4) | 2.7 (1.1, 6.7) | 4.4 (0.5, 36.4) |
| Medial epicondylitis | 2.1 (0.8, 5.2) | 2.3 (0.9, 5.8) | 1.2 (0.4, 3.6) |
| Radiating neck complaints | 4.8 (1.5, 16.1) | 2.6 (1.1, 5.9) | 2.2 (0.8, 6.0) |
| Rotator cuff tendonitis | 1.4 (1.0, 2.0) | 1.7 (1.1, 2.6) | 1.8 (0.9, 3.3) |
| Non-specific disorder | 1.5 (1.2, 2.0) | 1.4 (0.9, 2.2) | 1.1 (0.7, 1.8) |
Low exposure: 0-12 exposure index score (see text for details)
High exposure: 13-25 exposure index score
95% CI: 95 percent confidence interval
Persistence of specific UEMSDs
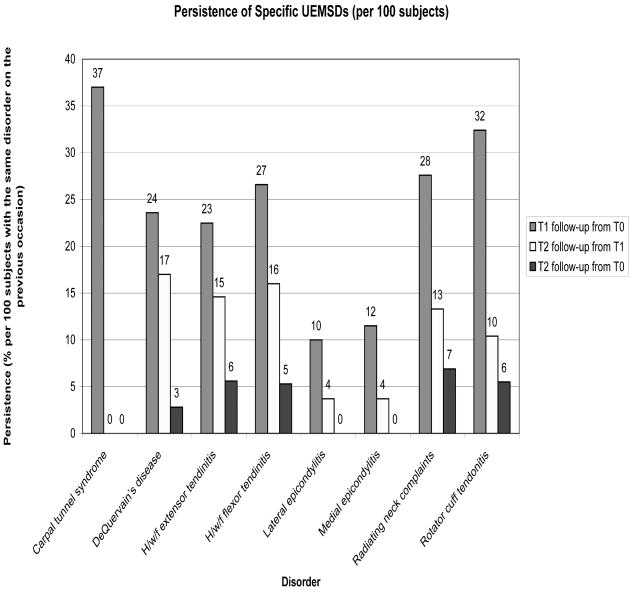
Approximately one-fourth to one-third of those with specific hand/wrist, neck or shoulder UEMSDs at baseline were still experiencing the same disorder one year later (Figure I), while persistence of elbow disorders was only ten percent. Persistence was markedly lower for all disorders from T1 to T2 and still lower from baseline to six-year follow-up.
FIGURE 1.
Persistence of specific UEMSDs (per 100 subjects) between T0, T1, and T2. Denominator¼subjects who met the same case definition for specific UEMSD type on the specified previous occasion.
In the first year of follow-up, persistence was higher for carpal tunnel syndrome and shoulder tendonitis than for the other specific disorders. However, no subjects with CTS symptoms and signs at T0 or T1 were determined to have the same at the six-year follow-up. With the possible exception of h/w/f tendonitis and neck complaints, there was little evidence that persistence of specific case types was predicted by T0 exposure level (Table IV).
Table IV. Persistence of UEMSD at follow-up, by T0 exposure status per 100 subjects with disorder in exposure category* at T0 (number of cases in parentheses).
| Follow-up survey T1 | Follow-up survey T2 | |||
|---|---|---|---|---|
| UEMSD type | Low exposure | High exposure | Low exposure | High exposure |
| Carpal tunnel syndrome | 67 (4) | 6 (1) | 0 | 0 |
| Flexor tendonitis | 8 (2) | 30 (8) | 0 | 8 (5) |
| Extensor tendonitis | 8 (2) | 27 (15) | 0 | 9 (5) |
| DeQuervain's disease | 18 (6) | 25 (16) | 3 (1) | 3 (2) |
| Lateral epicondylitis | 0 | 15 (4) | 0 | 0 |
| Medial epicondylitis | 17 (1) | 11 (2) | 0 | 0 |
| Radiating neck complaints | 0 | 38 (8) | 0 | 10 (2) |
| Rotator cuff tendonitis | 33 (14) | 36 (32) | 2 (1) | 7 (6) |
Low exposure: 0-12 exposure index score (see text for details)
High exposure: 13-25 exposure index score
Symptom characteristics and progression of specific and non-specific syndromes
In the initial survey, specific syndromes had an earlier recalled onset date than the non-specific disorders (5.7 vs. 4.5 years before baseline, p=0.004). They were characterized by more continuous pain (57% versus 41%, p=0.0004) and more days lost from work due to the condition (4.5 vs. 0.4 days, p=0.01). They were also more likely to result in seeking attention at the plant clinic (27% versus 14%, p=0.001) and in voluntary job changes (21% versus 8%, p<0.0001). The subjects with specific syndromes had more severe pain and greater functional impairment than those with NSDs, both at baseline and in the follow-up surveys (Table V).
Table V.
Severity of UEMSDs on three surveys, in subjects with one or more specific syndromes and those with non-specific disorders at baseline: Pain severity and functional impairment.
| Baseline disorder (n) | Baseline | One-year follow-up | Six-year follow-up | |||
|---|---|---|---|---|---|---|
| Paina (p<0.001)* | Functional Impairmentb (p<0.001) | Pain (p<0.001) | Functional Impairment (p<0.001) | Pain (p=0.02) | Functional Impairment (p=0.006) | |
| Specific (283) | 4.9 ± 2.3 | 21.3 ± 8.5 | 3.6 ± 2.9 | 15.2 ± 11.7 | 2.5 ± 3.1 | 9.6 ±10.1 |
| Non-specific (214) | 3.3 ± 2.4 | 15.6 ± 7.2 | 2.0 ± 2.6 | 8.1 ± 9.7 | 1.7 ± 2.9 | 5.5 ± 8.0 |
Average of 3 visual analogue scales for pain severity in specified UE region (mean±SD)
Sum of 10 items on difficulty performing activities of daily living (mean ±SD)
p-value from Wilcoxon rank test
Among subjects followed up, nearly one-fourth (n=34) of those with only NSDs at baseline had progressed to specific syndromes after one year. Among those surveyed, 19% (n=18) had done so after six years (Table VI). As compared to those who did not have symptoms at T0, those with NSDs at baseline were more likely to develop specific disorders at T1 (9% of those without symptoms vs. 24% of those with NSDs, p < 0.0001, two-sample test of proportions). Similar results held for T2 (p = 0.003, two-sample test of proportions). Conversely, the probability of reporting no symptoms at either follow-up was much lower among baseline specific syndromes than in NSD cases (two-sample test of proportions at both T1 and T2, p < 0.0001).
Table VI. UEMSD status by baseline disorder, in subjects followed 1 and 6 years from baseline survey.
| Baseline status | One-year follow-up | Six-year follow-up | ||||
|---|---|---|---|---|---|---|
| n followed | Specific syndrome(s) | No UE sx | n followed | Specific syndrome(s) | No UE sx | |
| Specific syndrome(s) | 189 | 59% | 29% | 116 | 37% | 44% |
| Non-specific UEMSDs | 140 | 24% | 54% | 93 | 19% | 62% |
| No upper extremity symptoms | 434 | 9% | 85% | 294 | 8% | 82% |
% with non-specific UEMSDs vs. % with no upper extremity symptoms at baseline progressing to specific syndrome(s) at one-year follow-up, p < 0.0001, and at six-year follow-up, p = 0.003, two sample test of proportions.
% with specific syndrome(s) vs. % with non-specific UEMSDs at baseline progressing to no upper extremity symptoms at one-year follow-up, p < 0.0001 and at six-year follow-up, p < 0.0001, two sample test of proportions.
Leave reasons at six-year follow-up
At six-year follow-up, each of the T0 specific case types had a higher percentage of workers on temporary illness/injury/disability or on “other permanent separation” than did T0 non-cases (Table VII). This was highest (27.5%) for those with radiating neck symptoms at baseline. Those with radiating neck symptoms and CTS were more likely to be absent or leave work more often than those in other specific case categories. The frequency of leaving among those with baseline non-specific disorders was within the range observed for the specific case types. Exposure status at T0 did not appear to be associated with leaving by T2, except possibly for those with radiating neck symptoms, h/w/f flexor or extensor tendonitis, and de Quervain's disease.
Table VII. Percentage lost to follow-up at T2 due to temporary illness/injury/disability or other permanent separation, by baseline UEMSD and exposure status *.
| UEMSD Type | All exposures | Low Exposure | High exposure |
|---|---|---|---|
| Carpal tunnel syndrome | 22.2 | 33.4 | 22.2 |
| De Quervain's disease | 16.2 | 9.1 | 17.4 |
| H/w/f extensor tendonitis | 17.1 | 8.0 | 19.7 |
| H/w/f flexor tendonitis | 15.1 | 8.0 | 16.7 |
| Lateral epicondylitis | 17.5 | 27.3 | 11.1 |
| Medial epicondylitis | 11.6 | 16.7 | 5.6 |
| Radiating neck complaints | 27.5 | 0.0 | 28.5 |
| Rotator cuff tendonitis | 15.9 | 16.3 | 16.7 |
| Non-specific disorder | 15.0 | 15.7 | 16.8 |
| Non-case | 9.9 | 8.2 | 11.7 |
| ALL | 11.7 |
Low exposure: 0-12 exposure index score (see text for details)
High exposure: 13-25 exposure index score
Overlap of specific UEMSDs by body region
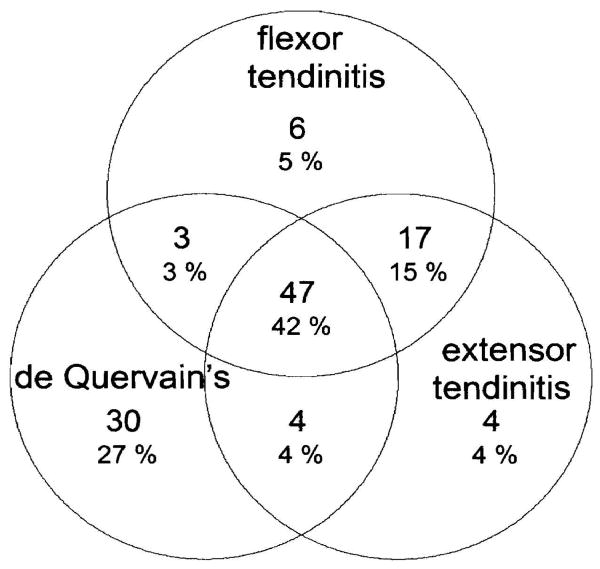
Workers with any one of the three most prevalent hand/wrist conditions (de Quervain's disease and extensor or flexor tendonitis) at baseline were very likely to have either or both of the others (Figure II). Slightly more than two-fifths met the case definitions for all three disorders, 15% had signs and symptoms of both h/w/f flexor and extensor tendonitis, and one-quarter showed indications of de Quervain's disease exclusive of the others. Results were similar on both left and right sides. These relative percentages were comparable in T1 and T2.
FIGURE 2.
Overlap of specific hand/wrist disorders at baseline (n¼111).
At baseline, almost half of subjects with specific elbow disorders had signs and symptoms simultaneously of medial and lateral epicondylitis. Slightly fewer fit the case definition of lateral epicondylitis (40%) alone. At T1, although a similar proportion met criteria for both types of epicondylitis, relatively fewer subjects had lateral epicondylitis alone (29%) and relatively more had medial epicondylitis alone (21%). By T2, most cohort members (63%) had medial epicondylitis alone, and only 21% had overlapping conditions.
Discussion
We found relatively high prevalence of both specific and non-specific upper extremity disorders in this longitudinal cohort of automobile manufacturing workers. Specific upper extremity syndromes accounted for a total UEMSD baseline prevalence of 23% in this industrial workforce; almost as many had non-specific disorders. In all three surveys of this industrial workforce, the most common specific conditions were rotator cuff tendonitis and de Quervain's disease. Between 20 and 40 percent of most specific disorders persisted over one year, but fewer than ten percent of those with each disorder at baseline had the same condition six years later. The percentage of affected cohort members with specific disorders of either shoulder or elbow, namely, rotator cuff tendonitis or epicondylitis, increased during the follow-up time periods.
Both specific and non-specific UEMSDs were more prevalent in those with higher self-reported exposures to ergonomic stressors. It did not appear that overall intensity of exposure influenced whether one differentially developed a specific or non-specific UEMSD. Neither did it determine persistence of specific UEMSDs. Further analysis would be needed to determine whether particular exposure profiles (e.g., heavy lifting, segmental vibration) were associated with specific UEMSD prevalence or persistence in this cohort.
Several other studies have examined the prevalence of specific UEMSDs in factory workers [Roquelaure, et al. 2002, Silverstein, et al. 1986, Bonde, et al. 2003, Kaergaard and Andersen 2000, Leclerc, et al. 2001, Gorsche, et al. 1999, Descatha, et al. 2003]. The prevalence ranges detailed in these studies are comparable to those found in the present paper with the exception of CTS; the present study prevalence was less than ten percent in all surveys, while other studies showed prevalences ranging from 14-22 percent. This is likely due to our more stringent definition of the disorder. Our CTS definition required both a classic or probable rating on the hand diagram [Katz and Stirrat 1990] and a positive Phalen's test (with signs similar to that of the hand diagram).
At each follow-up survey, the probability of developing a specific disorder among NSDs cases was more than twice that of non-cases. Subjects without specific syndromes had less severe disorders at T0 and were very likely to progress to more specific conditions over time. Additionally, at baseline, worse symptoms and impairment in the specific disorders coincided with their longer duration, which would be consistent with such a progression.
About one quarter of NSDs at T0 progressed toward specific MSDs at 1-year follow-up. This proportion was significantly higher than that among non-cases, in accordance with results reported by Descatha et al. [2008]. This finding indicates that those with NSDs should be considered at high risk of developing specific MSDs, possibly because they represent mild early cases of such diseases [Sluiter, et al. 2000]. These individuals should be closely monitored through hazard and medical surveillance, with exposure abatement or other job accommodation as appropriate, to prevent any morbidity progression.
Examination of reasons for loss to follow-up at T2 suggests a possible Healthy Worker Selection Effect (HWE) for several disorders, in particular radiating neck complaints and CTS. This may have deflated our estimates of follow-up prevalence and persistence of these disorders. It is possible that individuals with these syndromes were more highly symptomatic or more disabled than those with other disorders, thus providing the impetus for leaving work. However, further study would be necessary in order to confirm this hypothesis. Rates of temporary illness/injury/disability and other permanent separation in those with NSDs were comparable to those with most of the specific UEMSDs. Hence, it seems unlikely that HWE would explain away our assessment of non-specific to specific UEMSD progression.
A major strength of this study is the likely reliability (internal validity) of the physical examination, as the same examiner was employed in each survey period. The syndromes were defined through a matrix of physical examination findings and symptom reports that do not necessarily translate directly to a physician's criteria when making a diagnosis. However, these epidemiologic case definitions are the closest approximation, based on attempts to standardize UEMSD criteria for clinical diagnosis and epidemiologic case definitions [Harrington, et al. 1998, Sluiter, et al. 2000]. The syndrome classifications were not based on radiographic, laboratory or other instrumental objective findings. With the exception of CTS, for which electrodiagnostic studies were not available in this study, these syndromes do not have gold standards.
The definition of non-specific MSDs in this study is broader than non-specific diffuse forearm pain as specified by Harrington et al [1998]. It is more closely aligned to that of Sluiter et al [2000], where the existence of specific UEMSD diagnoses throughout the upper extremity are ruled out.
Approximately 10-40 percent of UEMSDs persisted for the one year following baseline, with lower rates of persistence for six years following initial case identification. Less than ten percent of each disorder persisted from baseline into the sixth year. Data on persistence of specific MSDs are scarce in the literature (in any occupational sector), although our results appear comparable with those produced by other studies for CTS and epicondylitis [Descatha, et al. 2003, Andersen, et al. 2003, Haahr and Andersen 2003]. A very wide range of estimates (31-92%) has been reported for shoulder tendonitis in industrial settings [Bonde, et al. 2003, Kaergaard and JH 2000, Silverstein, et al. 2006, Hagberg 1994].
More than one UEMSD was evident in the elbow or hand/wrist region of almost half of the cohort members with such disorders. It is possible that this reflects lack of clinical precision in our screening protocol and case definitions. On the other hand, the consensus case definitions that were used may be deficient in describing the scope of UEMSD morbidity in some individuals. Aublet-Cuvelier et al [2007] have described study subjects with UEMSDs in multiple anatomical sites. Twenty-five percent of our baseline cohort members with specific syndromes also exhibited these more broadly anatomical simultaneous UEMSDs. Some clinicians diagnose multiple simultaneous UEMSDs; seventy-one percent of Maryland workers compensation claimants reported that they had been given more than one upper extremity diagnosis [Keogh, et al. 2000].
Much work remains to be done in classifying UEMSDs. Better classification could yield a better understanding of the pathophysiology in such disorders. Our non-specific case definition does not represent a single disease entity, but rather those cases that were not readily classified on the basis of standard examination maneuvers. The combinations of signs and symptoms observed in those individuals might shed further light on this large proportion of upper extremity morbidity. Although controversial, exploratory factor analysis and cluster analysis have been used to distinguish between pathological subtypes in Alzheimer's disease [Armstrong and Wood 1994, Stopford, et al. 2007], systematic lupus erythematosus [Jacobsen, et al. 1998], complex regional pain syndrome [Harden, et al. 1999, Harden, et al. 2007], and other disorders. These methods applied to non-specific UEMSDs might shed light on clinical subtypes in this arena.
Conclusion
The progression of non-specific to specific upper extremity musculoskeletal disorders in a longitudinal cohort of automobile manufacturing workers over a six-year period was apparent, particularly in the elbow and shoulder regions. Approximately two-thirds of subjects with hand/wrist disorders met the criteria of more than one UEMSD in that anatomical region. Standardization of case definitions and examination intervals is warranted to ensure comparability of studies. This will result in improved understanding of the course of UEMSDs in the workplace.
Acknowledgments
Grant sponsor: This study was funded by the National Joint Committee (NJC) on Health and Safety of the company and the United Auto Workers (T0 and T1 surveys) and the U.S. National Institute for Occupational Safety and Health (NIOSH), grant number R01-OH003514 (T2 survey). The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. Dr. Katz was supported by NIH K24 AR 02123, NIH P60 AR47782. Data collection relied heavily on the generous assistance and cooperation of National Training Center staff, Dr. Rebecca Moreland (NJC liaison) plant managers, safety directors, UAW ergonomics trainers, and health and safety committee members. Twila Eshelman and Trudy Johnson Hall conducted the physical examinations and interviews. Preliminary findings were reported at the Fifth International Scientific Conference on Prevention of Work-related Musculoskeletal Disorders (PREMUS '04).
References
- Andersen JH, Thomsen J, Overgaard E, Lassen C, Brandt L, Vilstrup I, Kryger A, Mikkelsen S. Computer use and carpal tunnel syndrome: a 1-year follow-up study. JAMA. 2003;289:2963–2969. doi: 10.1001/jama.289.22.2963. [DOI] [PubMed] [Google Scholar]
- Armstrong R, Wood L. The identification of pathological subtypes of Alzheimer's disease using cluster analysis. Acta Neuropathology. 1994;88:60–66. doi: 10.1007/BF00294360. [DOI] [PubMed] [Google Scholar]
- Aublet-Cuvelier A, Aptel M, Weber H. The dynamic course of musculoskeletal disorders in an assembly line factory. International Archives of Occupational and Environmental Health. 2007;79:578–584. doi: 10.1007/s00420-006-0092-9. [DOI] [PubMed] [Google Scholar]
- Bernard BP. Musculoskeletal disorders and workplace factors: A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. Cincinnati, OH: National Institute of Occupational Safety and Health; 1997. [Google Scholar]
- Bonde JP, Mikkelsen S, Andersen JH, Fallentin N, Baelum J, Svendsen S, Thomsen J, Frost P, Thomsen G, Overgaard E, Kaergaard A, PRIM Health Study Group Prognosis of shoulder tendonitis in repetitive work: a follow up study in a cohort of Danish industrial and service workers. Occupational and Environmental Medicine. 2003;60:E8. doi: 10.1136/oem.60.9.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovenzi M. Occupational musculoskeletal disorders in the neck and upper limbs of forestry workers exposed to hand-arm vibration. Ergonomics. 1991;34:547–562. doi: 10.1080/00140139108967336. [DOI] [PubMed] [Google Scholar]
- Cherniack M. Physical examination protocol. Farmington, CT: 2001. [Google Scholar]
- Descatha A, Leclerc A, Chastang JF, Roquelaure Y, The Study on Repetitive Work Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. Journal of Occupational and Environmental Medicine. 2003;45:993–1001. doi: 10.1097/01.jom.0000085888.37273.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Descatha A, Roquelaure Y, Evanoff B, Chastang JF, Cyr D, Leclerc A. Do workers with self-reported symptoms have an elevated risk of developing upper extremity musculoskeletal disorders three year later? Occupational and Environmental Medicine. 2008;65:205–207. doi: 10.1136/oem.2007.033357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon C. Personal communication. Farmington, CT: 1998. Listing of principal expected isolated diagnoses. [Google Scholar]
- Gerr F, Marcus M, Ensor C, Kleinbaum D, Cohen S, Edwards A, Gentry E, Ortiz DJ, Monteilh C. Prospective study of computer users: 1. Study design and incidence of musculoskeletal symptoms and disorders. American Journal of Industrial Medicine. 2002;41:221–235. doi: 10.1002/ajim.10066. [DOI] [PubMed] [Google Scholar]
- Gorsche R, Wiley J, Renger R, Brant R, Gemer T, Sasyniuk T. Prevalence and incidence of carpal tunnel syndrome in a meat packing plant. Occupational and Environmental Medicine. 1999;56:417–422. doi: 10.1136/oem.56.6.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haahr J, Andersen J. Prognostic factors in lateral epicondylitis: a randomized trial with one-year follow-up in 266 new cases treated with minimal occupational intervention or the usual approach in general practice. Rheumatology (Oxford) 2003;42:1216–1225. doi: 10.1093/rheumatology/keg360. [DOI] [PubMed] [Google Scholar]
- Hagberg M. Neck and shoulder disorders. In: Rosenstock L, Cullen M, editors. Textbook of Occupational and Environmental Medicine. Philadelphia: W.B. Saunders; 1994. pp. 356–364. [Google Scholar]
- Harden RN, Bruehl S, Galer BS, Saltz S, Bertram M, Backonja M, Gayles R, Rudin N, Bhugra MK, Stanton-Hicks M. Complex regional pain syndrome: are the IASP diagnostic criteria valid and sufficiently comprehensive? Pain. 1999;83:211–219. doi: 10.1016/s0304-3959(99)00104-9. [DOI] [PubMed] [Google Scholar]
- Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Medicine. 2007;8:326–331. doi: 10.1111/j.1526-4637.2006.00169.x. [DOI] [PubMed] [Google Scholar]
- Harrington JM, Carter JT, Birrell L, Gompertz D. Surveillance case definitions for work-related upper limb pain syndromes. Occupational and Environmental Medicine. 1998;55:264–271. doi: 10.1136/oem.55.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen S, Petersen J, Ullman S, Junker P, Voss A, Rasmussen J, Tarp U, Poulsen L, van Overeem Hansen G, Skaarup B, Hansen T, Pødenphant J, Halberg P. A multicentre study of 513 Danish patients with systemic lupus erythematosus. I. Disease manifestations and analyses of clinical subsets. Clinical Rheumatology. 1998;17:468–477. doi: 10.1007/BF01451282. [DOI] [PubMed] [Google Scholar]
- Kaergaard A, JH A. Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: prevalence, incidence, and prognosis. Occupational and Environmental Medicine. 2000;57:528–534. doi: 10.1136/oem.57.8.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz JN, Stirrat CR. A self-administered hand diagram for the diagnosis of carpal tunnel syndrome. Journal of Hand Surgery (American) 1990;15A:360–363. doi: 10.1016/0363-5023(90)90124-a. [DOI] [PubMed] [Google Scholar]
- Keogh JP, Gucer PW, Gordon JL, Nuwayhid I. The impact of occupational injury on injured worker and family: outcomes of upper extremity cumulative trauma disorders in Maryland workers. American Journal of Industrial Medicine. 2000;38:489–506. doi: 10.1002/1097-0274(200011)38:5<498::aid-ajim2>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Latko WA, Armstrong TJ, Franzblau A, Ulin SS, Werner RA, Albers JW. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. American Journal of Industrial Medicine. 1999;36:248–259. doi: 10.1002/(sici)1097-0274(199908)36:2<248::aid-ajim4>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Leclerc A, Landre M, Chastang J, Niedhammer I, Roquelaure Y, The Study Group on Repetitive Work Upper-limb disorders in repetitive work. Scandinavian Journal of Work Environment Health. 2001;27:268–278. doi: 10.5271/sjweh.614. [DOI] [PubMed] [Google Scholar]
- Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. The Journal of Bone and Joint Surgery. 1993;75-A:1585–1592. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- National Academy of Sciences. Steering Committee for the Workshop on Work-Related Musculoskeletal Injuries: The Research Base Committee on Human Factors, National Research Council . Work-Related Musculoskeletal Disorders: A Review of the Evidence. Washington, D.C.: National Academy Press; 1998. [Google Scholar]
- National Academy of Sciences. Panel on Musculoskeletal Disorders and the Workplace Commission on Behavioral and Social Sciences and Education, National Research Council . Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. Washington, D.C.: National Academy Press; 2001. [Google Scholar]
- Piligian G, Herbert R, Hearns M, Dropkin J, Landsbergis P, Cherniack M. Evaluation and management of chronic work-related musculoskeletal disorders of the distal upper extremity. American Journal of Industrial Medicine. 2000;37:75–93. doi: 10.1002/(sici)1097-0274(200001)37:1<75::aid-ajim7>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Punnett L. Ergonomic stressors and upper extremity disorders in vehicle manufacturing: cross sectional exposure-response trends. Occupational and Environmental Medicine. 1998;55:414–420. doi: 10.1136/oem.55.6.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L, van der Beek AJ. A comparison of approaches to modeling the relationship between ergonomic exposures and upper extremity disorders. American Journal of Industrial Medicine. 2000;37:645–655. doi: 10.1002/(sici)1097-0274(200006)37:6<645::aid-ajim9>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Punnett L, Gold JE, Katz JN, Gore R. Ergonomic stressors and upper extremity disorders in automotive manufacturing: a one-year follow-up study. Occupational and Environmental Medicine. 2004;61:668–674. doi: 10.1136/oem.2003.008979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roach K, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care and Research. 1991;4:143–149. [PubMed] [Google Scholar]
- Roquelaure Y, Mariel J, Fanello S, Boissière JC, Chiron H, Dano C, Bureau D, Penneau-Fontbonne D. Active epidemiological surveillance of musculoskeletal disorders in a shoe factory. Occupational and Environmental Medicine. 2002;59:452–458. doi: 10.1136/oem.59.7.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein BA, Fine LJ. Evaluation of upper extremity and low back cumulative trauma disorders: a screening manual. Ann Arbor, MI: University of Michigan, School of Public Health, Center for Ergonomics; 1984. [Google Scholar]
- Silverstein BA, Fine LJ, Armstrong TJ. Hand wrist cumulative trauma disorders in industry. British Journal of Industrial Medicine. 1986;43:779–784. doi: 10.1136/oem.43.11.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein BA, Viikari-Juntura E, Fan ZJ, Bonauto D, Bao S, Smith C. Natural course of nontraumatic rotator cuff tendinitis and shoulder symptoms in a working population. Scandinavian Journal of Work Environment Health. 2006;32:99–108. doi: 10.5271/sjweh.985. [DOI] [PubMed] [Google Scholar]
- Sluiter JK, Rest KM, Frings-Dresen MH. Criteria Document for Evaluation of the Work-Relatedness of Upper Extremity Musculoskeletal Disorders. Coronel Institute for Occupational and Environmental Health, University of Amsterdam; The Netherlands: 2000. [Google Scholar]
- Stopford C, Snowden J, Thompson J, Neary D. Distinct memory profiles in Alzheimer's disease. Cortex. 2007;43:846–857. doi: 10.1016/s0010-9452(08)70684-1. [DOI] [PubMed] [Google Scholar]