Abstract
The prognosis for hilar cholangiocarcinoma is limited by tumor spread along the biliary tree leading to refractory obstructive cholestasis, cholangitis, and liver failure. Palliation with biliary endoprostheses results in median survival times of 4-6 months for advanced bile duct cancer. Photodynamic therapy (PDT) is a local photochemical tumor treatment consisting of a photosensitizing agent combined with laser irradiation of a distinct wavelength. Tumor ablation with PDT combined with biliary stenting reduces cholestasis and significantly improves median survival time. However, the treatment is not widely available, and the photosensitizers used for PDT cause prolonged photosensitivity. Optimum control of tumor spread along the bile ducts and control of cholestasis and cholangitis will prolong survival in one to two thirds of patients, and renders them suitable for other antitumor therapies.
Keywords: Cholangiocarcinoma, Bile duct neoplasms, Photodynamic therapy, Photosensitizing agents
INTRODUCTION
Photodynamic therapy (PDT) is based on the relatively specific accumulation of photosensitizers, such as porphyrins, in dysplastic or malignant cells. After intravenous, oral, or topical applications, the photosensitizer drug predominantly concentrates in tumor tissue and remains inactive until exposed to a specific wavelength of light. When light is delivered to the target cancer site, the photodynamic reaction induces photochemical destruction of tumor tissue mediated by singlet molecular oxygen and other reactive species generated by the reaction of the activated photosensitizer and mucosal oxygen. Damage to tissue occurs by several pathways including cell necrosis, apoptosis, and ischemia with vascular shutdown. The importance of inflammatory and immune responses has been recognized [1]. Modern PDT varies in the type of photosensitizer, the wavelength and intensity of light used to activate the drug, and the type of light distribution system used to apply the light [2]. Following health agency approvals throughout the world for various cancers and other diseases, PDT is gradually being accepted as a standard modality to be added to the medical practioner's armamentarium [3].
Cholangiocarcinoma (CC) is the primary cancer of bile ducts. Complete resection with negative margins is the only treatment with a potential for cure, and 5-year survival rates are 20 to 40% [4,5]. However, patients usually present at an advanced stage, with more than 50% of cases being unresectable at the time of diagnosis. Recently, two randomized controlled trials have shown a significant survival benefit in patients with unresectable CC treated with PDT [6,7]. One of these studies also showed a significant improvement in quality of life after PDT and stenting [7].
Rationale for PDT as a local tumor ablation in hilar CC
CC is characterized by a slow growth rate and a low propensity for metastasis. However, because of late symptoms, a close proximity to important vascular structures in the hilum of the liver, and a tendency to grow into perineural tissue, CCs are seldom curative at the time of diagnosis [8].
Even with an aggressive surgical approach, only 33% to 50% of CCs are resectable, and negative histological margins are obtained in only 28% [9]. A significant survival advantage occurs for patients with negative margins. The median survival time in a recent study by Burke et al. [9] was 40 months overall in all resected patients, 22 months in those with positive margins, and greater than 60 months in those with negative margins.
Usually the only therapeutic strategy for nonresectable CCs is to improve cholestasis by endoscopic or percutaneous drainage or biliary bypass. Although these procedures do not influence tumor growth, and it is unclear if they increase survival, they significantly improve mental outlook and ameliorate symptoms such as fatigue, diarrhea, anorexia, pruritus, jaundice, and poor sleep patterns [10]. However, these procedures carry some risk for procedure-related morbidity and mortality. Early morbidity and 30-day mortality are significantly higher following surgical procedures, whereas long-term complications occur more frequently with endoscopic therapy [11]. Interventional techniques are preferred, because long-term complications are of minor importance, with reported poor median survival times of 147 and 182 days, respectively [11].
Cholestasis can be relieved quickly in the majority of patients with tumor stenoses in the distal and middle part of the bile duct. Palliative intervention is limited in proximal bile duct cancers. Independent of the type of stricture, technically successful endoprosthesis placement is possible in 84 to 96% of these patients [12,13]. However, successful drainage (bilirubin decrease > 30% to 50%) is only achieved in 69% to 91% of Bismuth type I and II stenoses and in 15% to 73% of Bismuth type III and IV tumors, which is reflected in the survival time of these patients: 149 to 160 days for Bismuth type I, 84 to 131 days for Bismuth type II, and 62 to 70 days for Bismuth type III strictures [12,14].
Although inserting a metal stent improves occlusion rates and reduces the number of therapeutic interventions, median survival time is not ameliorated [15]. Attempts to affect tumor growth have been made with radiotherapy or chemotherapy. Until now, however, no randomized prospective studies concerning the effect of these already long-used additional therapies are yet available. The only retrospective comparative palliative radiation therapy study showed no improvement in median survival time (300 vs. 210 days) between endoscopic biliary stenting alone and additional external-beam radiotherapy and internal 192Ir brachytherapy [16]. A survival advantage in the radiotherapy group was observed in the first 9 months. The median hospital stay was 50 days with radiotherapy versus only 7 days with endoprosthesis alone.
Developing a treatment modality for local ablation of the primary tumor could improve the outcome of curative as well as palliative therapies. An 192Ir dose of 35 Gy in a 1-cm distance did not prolong median survival time (4.3 to 5 months) [17], but when combined with external beam radiotherapy (30 Gy), palliative brachytherapy resulted in median survival times of 10 to 10.5 months [15]. Another modality for local tumor ablation of CC is PDT.
Biological mechanism of PDT
PDT is a two-step procedure. A photosensitizing drug known to preferentially accumulate in tumor cells is administered, and the tumor is exposed to nonthermal laser light of the appropriate photoactivating wavelength after a time interval required for the drug to accumulate in tumor tissue. A variety of candidate photosensitizing agents are available for use in PDT, which are based upon modifications of porphyrin, chlorine, and chlorophyll. Phorphyrin-based photosensitizers, such as hematoporphyrin derivatives and its partly purified commercial preparation, porfimer sodium (Photofrin II, Axcan, Montreal, QC, Canada), are the most commonly used sensitizers. Photofrin accumulates in CC cells with a tumor to a normal tissue fluorescence ratio of 2:1, 24 and 48 hours after administration [18]. Photofrin preferentially accumulates in CC cells, reaching peak values during the first 2 days. This leads to a photochemical reaction, particularly a type II reaction, and generates cytotoxic singlet oxygen or other oxygen-derived free radicals [19]. These toxic products interact with a number of cellular components such as microsomes, mitochondria, nuclei, and cell membranes. The initial trigger is not yet known. The selective sensitivity of the tumor microvasculature to PDT also seems to play an important role [20].
The only relevant side-effect of PDT is phototoxicity. For the most often used hematoporphyrin derivative, phototoxicity lasts for 4 to 6 weeks after drug administration [21].
Technical aspects of PDT for cholangiocarcinoma
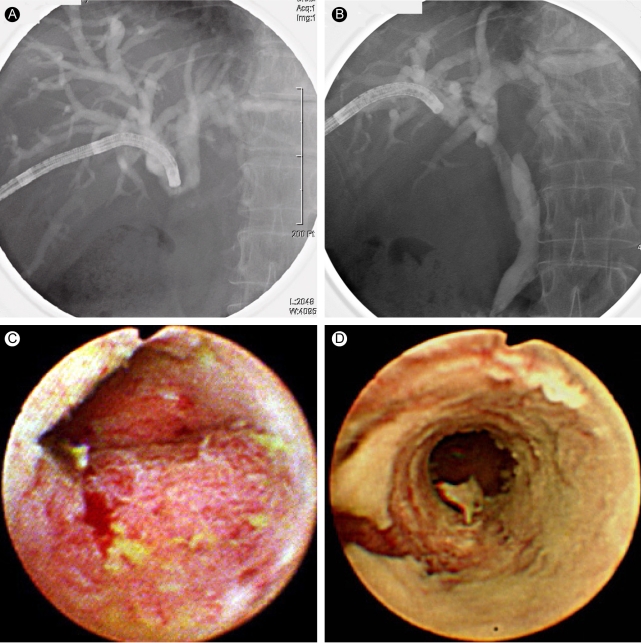
A translucent endoscopic retrograde cholangiography cannula (triple lumen for guidewire, diffuser, and contrast injection) is inserted into the tumor stenosis through which a 400-µm thin quartz fiber with a cylindrical light diffuser and radiopaque markers at the tip (Optiguide DCYL 200 series, QLT Phototherapeutics Inc., Vancouver, Canada) is placed under fluoroscopic guidance across the tumor stenosis. An alternative technique uses a preloaded catheter [22]. After positioning a 0.035-inch guidewire proximal to the biliary stricture, the preloaded catheter is advanced over the guidewire using the monorail technique and positioned into the stricture. The guidewire is then withdrawn, and the diffuser tip with its radiopaque markers is positioned across the stricture. However, the peroral transpapillary approach has some limitations with regard to appropriate application and patient follow-up. Although flexible tip diffusing fibers are usually employed, they may be rendered ineffective as a result of partial or complete fracture of the laser diffuser tip caused by bending during cannulation via the peroral route. In comparison, percutaneous cholangioscopy-guided PDT can provide an effective, homogeneous irradiation of the targeted lesion with direct visual control (Fig. 1). This procedure is easily performed and can be monitored repeatedly without periodic peroral endoscopy, having similar merits to the brief application and relatively less pain associated with the routine exchange of stents in percutaneous transhepatic biliary drainage treatment [23]. The PDT site is usually temporarily obstructed due to swelling and coagulation necrotic changes within 1 week after PDT; therefore, it is necessary to insert an exchangeable plastic endoprostheses or external drainage tube.
Figure 1.
Percutaneous cholangiographic and choledochoscopic images of an advanced bile duct adenocarcinoma before and 4 months after the first photodynamic therapy (PDT) session. (A) Percutaneous cholangioscopy shows complete luminal obstruction of the common hepatic duct as seen on percutaneous cholangioscopy. (B) Complete recannalization of the common hepatic duct is seen on percutaneous cholangioscopy 4 months after PDT. (C) Complete luminal obstruction is seen at the bifurcation on cholangioscopy before PDT. (D) A recannalized bile duct can be seen on cholangioscopy 4 months after PDT.
Photodynamic effect on cholangiocarcinoma
Wong et al. [24] showed up to a 60% reduction in tumor volume after PDT with hematoporphyrin and chlorine in nude mice inoculated with a human CC cell line. The first hint of an in vivo beneficial effect for PDT came from a single case report of McCaughan et al. [25]. CC cell lines show favorable cellular uptake kinetics for sodium porfimer and excellent phototoxic cell damage in response to PDT in vitro and in vivo in a human CC xenograft model in nude mice [26]. The PDT effect was evaluated after inoculating Buffalo female rats with rat hepatoma cells. The mean complete necrosis size for a single PDT session was 10.2 mm3 [27]. Neoadjuvant PDT for CC revealed that the tumoricidal depth of PDT using porfimer is limited to 4- to 4.5-mm of tissue penetration [28], which cannot eradicate a primary tumor when invasion extends to a depth of 7 to 9 mm. Newer photosensitizers lead to deeper tumor necrosis and a shorter photosensitivity period. Meso-tetrahydroxyphenyl chlorine has absorption in the near-infrared spectrum (652 nm) and has the above characteristics.
PDT outcomes for advanced hilar cholangiocarcinoma
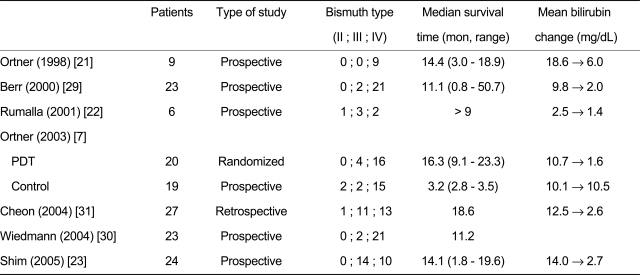
In numerous uncontrolled studies, the combination of PDT and biliary drainage has shown promising results in patients with unresectable hilar CC (Table 1).
Table 1.
Outcomes of photodynamic therapy for hilar bile duct cancer
In a pilot study, Ortner et al. [21] performed PDT in patients with nonresectable CC Bismuth types III and IV who, having failed endoprostheses placement, had the poorest prognosis. Intraluminal photoactivation was performed cholangioscopically 2 days after the intravenous application of a hematoporphyrin derivative (Photofrin II). Red light at 630 nm was emitted by an argon-dye laser, and laser fibers with a core diameter of 400 mm with flexible cylindrical diffuser tips of 2.5 and four lengths were used. The light flux was 310 and 190 mW/cm2 with an 800 mW output, and the resulting dose was 180 J/cm2 by changing the irradiation time. Serum bilirubin levels declined from 318 ± 72 µmol/L 103 ± 35 mmol/L (p = 0.0039) with no significant increase during the two monthly follow-ups. Quality of life indices improved dramatically (Karnofsky index 32.3 ± 8.13% to 68.9 ± 6.1%, p = 0.0078; World Health Organization index 3.2 ± 0.36 to 1.7 ± 0.4, p = 0.016; performance rating scale 13.6 ± 1.6 to 5 ± 0.93, p = 0.0078) and remained stable during follow-up. Thirty-day mortality was 0%, 1-year survival was 77.7%, and median survival time was 439 days. A recent prospective, open-label, randomized, multicenter study with a group sequential design compared PDT plus stenting (group A) with stenting alone (group B) in patients with nonresectable CC [7]. PDT resulted in survival prolongation (group A: n = 20; median, 493 days; group B: n = 19; median, 98 days; p < 0.0001). PDT also improved biliary drainage and quality of life. The authors concluded that PDT, given in addition to best supportive care, improves survival in patients with nonresectable CC. The study was terminated prematurely, because PDT was so superior to simple stenting that further randomization was deemed unethical. Similar results were obtained by another study [31]. Twenty patients were treated with endoscopic biliary drainage alone (group A), and 27 patients were treated with PDT under percutaneous cholangioscopy with additional percutaneous biliary drainage (group B) and were analyzed retrospectively. The mean bilirubin level declined effectively in both groups after treatment. One-year survival was 28% in group A and 52% in group B (p < 0.05). Median survival time was 288 days in group A and 558 days in group B (p = 0.0143).
PDT for recurrent tumors after resection or as a neoadjuvant treatment
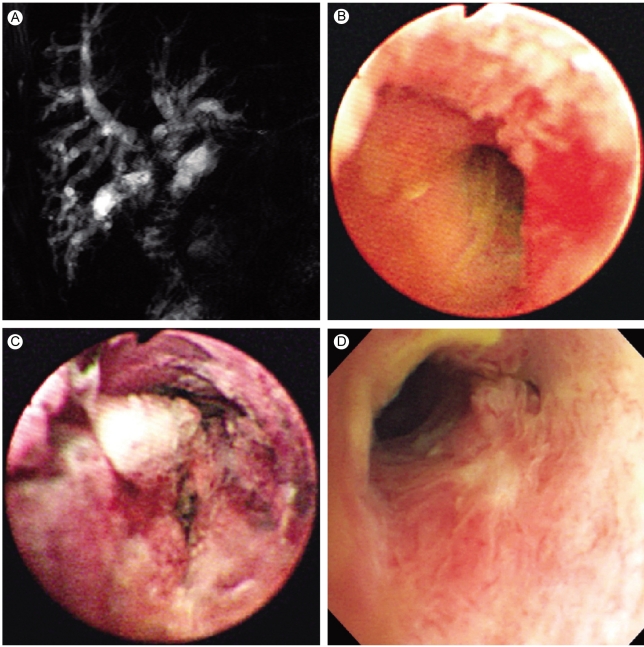
We experienced a case in which the survival time was remarkably extended after applying PDT to a postoperative recurrent tumor (Fig. 2). A small (n = 8) uncontrolled study showed marked destruction of recurrent tumors, and 75% of patients were disease free after 2 years [32].
Figure 2.
Photodynamic therapy (PDT) for a postoperative recurrent tumor. A 76-year-old man was referred to our hospital with jaundice. He had undergone Whipple's operation due to a hilar cholangiocarcinoma 1 year ago. (A) Magnetic resonance imaging shows a contrast enhanced hilar mass with an obstructing anastomosis site. (B) A choledochoscopy shows mucosal nodularity and neovascularization at the anastomosis site. Biopsy specimens revealed adenocarcinoma. (C) Two days after PDT, a choledochoscopy shows circumferential coagulation necrosis at the PDT-treated lesion. (D) A recannalized anastomotic site and small papillary changes with no abnormal vessels can be seen on cholangioscopy 1 year after PDT. Choledochoscopic biopsy specimens revealed chronic nonspecific inflammation.
Neoadjuvant PDT was evaluated in seven patients with advanced Bismuth type III and IV carcinoma, which was thought to be unresectable after staging [28]. A curative resection was performed after PDT in all patients; 83% were recurrence free after 1 year, and 5-year survival was 71%. No relevant PDT side effects occurred except for a minor intraoperative phototoxicity in one patient.
Assessment of response to PDT
Evaluating the therapeutic effects of PDT in patients with CC presents a number of challenges. Ortner et al. [21] evaluated the therapeutic effect of PDT in cases of advanced bile duct cancer by comparing the tumor length before and after PDT using the "mother-baby" cholangioscopic technique; however, it has been argued that their assessment was not objective. Although the authors [7] reported reduced serum bilirubin levels after PDT, plastic biliary endoprostheses were inserted in all patients following the PDT procedure, making it difficult to assess the direct effect of PDT for reducing serum bilirubin. However, the PDT group might have benefited, largely, from the number of endoscopic retrograde cholangiopancreatography sessions. For this reason, we do not consider serum bilirubin level to be an objective parameter for assessing a PDT response. Ductal CCs characteristically spread along or within the intrahepatic bile ducts, making it difficult to define the response to PDT based on changes in the tumor mass by computed tomography (CT). Similarly, it may be difficult to obtain objective results when the response to PDT is evaluated based solely on the extent of reopening of an occluded bile duct segment, as has been done in some studies [29]. We assess the thickness of a tumor mass before and after PDT treatment, measuring the thickest part of the tumor before the treatment and every month thereafter [23]. The mean thickness of the bile duct masses, as measured by intraductal ultrasonography, decreased from 8.7 ± 3.7 mm before PDT to 7.1 ± 2.0 mm at 1 month (p = 0.176), to 7.1 ± 2.4 mm (p = 0.157) at 2 months, and declined significantly to 5.8 ± 2.0 mm (p = 0.046) 3 months after PDT.
Some investigators have found that serum interleukin (IL)-6 levels correlate with tumor burden in murine cancer models [33,34], although this remains to be demonstrated clinically. Goydos et al. [34] reported that serum IL-6 levels are correlated with tumor burden as measured by CT in patients with CC; 2 weeks after tumor resection in three of 15 patients, IL-6 levels had dropped to undetectable levels in two patients and dropped by almost 10-fold in a third patient. Our results demonstrated, similarly, that IL-6 was significantly reduced (38.2 ± 9.9 pg/mL; p = 0.008) 1 month after PDT, as compared with the pretreatment level (282.1 ± 121.8 pg/mL); tumor thickness also decreased following PDT. In contrast, IL-6 levels did not change 1 month after endoscopic retrograde biliary drainage [35].
CONCLUSION
Patients with unresectable CC have a very short life expectancy. PDT is the first palliative treatment option that has shown efficacy in two randomized prospective studies. PDT improves survival, jaundice, quality of life, is well tolerated, and can be repeated without losing efficacy. PDT seems to be a promising therapeutic approach for nonresectable CC. PDT combines treating cholestasis with reducing tumor growth; therefore, it should be considered as standard care for palliation of CC. If results are confirmed, new photosensitizers with greater penetration depth and shorter photosensitivity should be used, or better drug targeting or combination therapies should be implemented to induce additional tumor necrosis. As PDT treatment is not available in all centers, patients should be referred to a specialized center that conducts PDT. It is still unknown whether radiotherapy and/or chemotherapy further improve the fate of PDT patients. It is now necessary to confirm these data in an extended randomized multicenter study, as PDT for recurrent tumors after surgery and neoadjuvant PDT remains experimental.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Oleinick NL, Evans HH. The photobiology of photodynamic therapy: cellular targets and mechanisms. Radiat Res. 1998;150(5 Suppl):S146–S156. [PubMed] [Google Scholar]
- 2.Wang KK. Current status of photodynamic therapy of Barrett's esophagus. Gastrointest Endosc. 1999;49(3 Pt 2):S20–S23. doi: 10.1016/s0016-5107(99)70520-1. [DOI] [PubMed] [Google Scholar]
- 3.Dougherty TJ. An update on photodynamic therapy applications. J Clin Laser Med Surg. 2002;20:3–7. doi: 10.1089/104454702753474931. [DOI] [PubMed] [Google Scholar]
- 4.Rea DJ, Munoz-Juarez M, Farnell MB, et al. Major hepatic resection for hilar cholangiocarcinoma: analysis of 46 patients. Arch Surg. 2004;139:514–523. doi: 10.1001/archsurg.139.5.514. [DOI] [PubMed] [Google Scholar]
- 5.Jarnagin WR, Fong Y, DeMatteo RP, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–517. doi: 10.1097/00000658-200110000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zoepf T, Jakobs R, Arnold JC, Apel D, Riemann JF. Palliation of nonresectable bile duct cancer: improved survival after photodynamic therapy. Am J Gastroenterol. 2005;100:2426–2430. doi: 10.1111/j.1572-0241.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- 7.Ortner ME, Caca K, Berr F, et al. Successful photodynamic therapy for nonresectable cholangiocarcinoma: a randomized prospective study. Gastroenterology. 2003;125:1355–1363. doi: 10.1016/j.gastro.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Kremer B, Henne-Bruns D, Vogel I, Grimm H, Soehendra N. Impact of staging on treatment of biliary carcinoma. Endoscopy. 1993;25:92–99. doi: 10.1055/s-2007-1009131. [DOI] [PubMed] [Google Scholar]
- 9.Burke EC, Jarnagin WR, Hochwald SN, Pisters PW, Fong Y, Blumgart LH. Hilar Cholangiocarcinoma: patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system. Ann Surg. 1998;228:385–394. doi: 10.1097/00000658-199809000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luman W, Cull A, Palmer KR. Quality of life in patients stented for malignant biliary obstructions. Eur J Gastroenterol Hepatol. 1997;9:481–484. doi: 10.1097/00042737-199705000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994;344:1655–1660. doi: 10.1016/s0140-6736(94)90455-3. [DOI] [PubMed] [Google Scholar]
- 12.Polydorou AA, Cairns SR, Dowsett JF, et al. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut. 1991;32:685–689. doi: 10.1136/gut.32.6.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ducreux M, Liguory C, Lefebvre JF, et al. Management of malignant hilar biliary obstruction by endoscopy. Results and prognostic factors. Dig Dis Sci. 1992;37:778–783. doi: 10.1007/BF01296439. [DOI] [PubMed] [Google Scholar]
- 14.Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc. 1998;47:354–362. doi: 10.1016/s0016-5107(98)70218-4. [DOI] [PubMed] [Google Scholar]
- 15.Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet. 1992;340:1488–1492. doi: 10.1016/0140-6736(92)92752-2. [DOI] [PubMed] [Google Scholar]
- 16.Bowling TE, Galbraith SM, Hatfield AR, Solano J, Spittle MF. A retrospective comparison of endoscopic stenting alone with stenting and radiotherapy in non-resectable cholangiocarcinoma. Gut. 1996;39:852–855. doi: 10.1136/gut.39.6.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Molt P, Hopfan S, Watson RC, Botet JF, Brennan MF. Intraluminal radiation therapy in the management of malignant biliary obstruction. Cancer. 1986;57:536–544. doi: 10.1002/1097-0142(19860201)57:3<536::aid-cncr2820570322>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 18.Pahernik SA, Dellian M, Berr F, Tannapfel A, Wittekind C, Goetz AE. Distribution and pharmacokinetics of Photofrin in human bile duct cancer. J Photochem Photobiol B. 1998;47:58–62. doi: 10.1016/s1011-1344(98)00203-6. [DOI] [PubMed] [Google Scholar]
- 19.Weishaupt KR, Gomer CJ, Dougherty TJ. Identification of singlet oxygen as the cytotoxic agent in photoinactivation of a murine tumor. Cancer Res. 1976;36(7 Pt 1):2326–2329. [PubMed] [Google Scholar]
- 20.Henderson BW, Donovan JM. Release of prostaglandin E2 from cells by photodynamic treatment in vitro. Cancer Res. 1989;49(24 Pt 1):6896–6900. [PubMed] [Google Scholar]
- 21.Ortner MA, Liebetruth J, Schreiber S, et al. Photodynamic therapy of nonresectable cholangiocarcinoma. Gastroenterology. 1998;114:536–542. doi: 10.1016/s0016-5085(98)70537-2. [DOI] [PubMed] [Google Scholar]
- 22.Rumalla A, Baron TH, Wang KK, Gores GJ, Stadheim LM, de Groen PC. Endoscopic application of photodynamic therapy for cholangiocarcinoma. Gastrointest Endosc. 2001;53:500–504. doi: 10.1067/mge.2001.113386. [DOI] [PubMed] [Google Scholar]
- 23.Shim CS, Cheon YK, Cha SW, et al. Prospective study of the effectiveness of percutaneous transhepatic photodynamic therapy for advanced bile duct cancer and the role of intraductal ultrasonography in response assessment. Endoscopy. 2005;37:425–433. doi: 10.1055/s-2005-861294. [DOI] [PubMed] [Google Scholar]
- 24.Wong M, Wang KK, Alexander Gl, et al. Cholorin E6 and hematophorphyrin derivative (HPD) on photodynamic therapy of a human cholangiocarcinoma model [abstract] Gastroenterology. 1996;110:595. [Google Scholar]
- 25.McCaughan JS, Jr, Mertens BF, Cho C, Barabash RD, Payton HW. Photodynamic therapy to treat tumors of the extrahepatic biliary ducts. A case report. Arch Surg. 1991;126:111–113. doi: 10.1001/archsurg.1991.01410250119022. [DOI] [PubMed] [Google Scholar]
- 26.Wong Kee Song LM, Wang KK, Zinsmeister AR. Mono-L-aspartyl chlorin e6 (NPe6) and hematoporphyrin derivative (HpD) in photodynamic therapy administered to a human cholangiocarcinoma model. Cancer. 1998;82:421–427. [PubMed] [Google Scholar]
- 27.Cheon YK, Kim YS, Cho YD, et al. Experimental interstitial photodynamic therapy of the Morris 7777 hepatoma in the rat. Korean J Med. 2004;66:397–403. [Google Scholar]
- 28.Wiedmann M, Caca K, Berr F, et al. Neoadjuvant photodynamic therapy as a new approach to treating hilar cholangiocarcinoma: a phase II pilot study. Cancer. 2003;97:2783–2790. doi: 10.1002/cncr.11401. [DOI] [PubMed] [Google Scholar]
- 29.Berr F, Wiedmann M, Tannapfel A, et al. Photodynamic therapy for advanced bile duct cancer: evidence for improved palliation and extended survival. Hepatology. 2000;31:291–298. doi: 10.1002/hep.510310205. [DOI] [PubMed] [Google Scholar]
- 30.Wiedmann M, Berr F, Schiefke I, et al. Photodynamic therapy in patients with non-resectable hilar cholangiocarcinoma: 5-year follow-up of a prospective phase II study. Gastrointest Endosc. 2004;60:68–75. doi: 10.1016/s0016-5107(04)01288-x. [DOI] [PubMed] [Google Scholar]
- 31.Cheon YK, Cho YD, Baek SH, et al. Comparison of survival of advanced hilar cholangiocarcinoma after biliary drainage alone versus photodynamic therapy with external drainage. Korean J Gastroenterol. 2004;44:280–287. [PubMed] [Google Scholar]
- 32.Nanashima A, Yamaguchi H, Shibasaki S, et al. Adjuvant photodynamic therapy for bile duct carcinoma after surgery: a preliminary study. J Gastroenterol. 2004;39:1095–1101. doi: 10.1007/s00535-004-1449-z. [DOI] [PubMed] [Google Scholar]
- 33.Utsumi K, Takai Y, Tada T, Ohzeki S, Fujiwara H, Hamaoka T. Enhanced production of IL-6 in tumor-bearing mice and determination of cells responsible for its augmented production. J Immunol. 1990;145:397–403. [PubMed] [Google Scholar]
- 34.Goydos JS, Brumfield AM, Frezza E, Booth A, Lotze MT, Carty SE. Marked elevation of serum interleukin-6 in patients with cholangiocarcinoma: validation of utility as a clinical marker. Ann Surg. 1998;227:398–404. doi: 10.1097/00000658-199803000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheon YK, Cho YD, Moon JH, et al. Diagnostic utility of interleukin-6 (IL-6) for primary bile duct cancer and changes in serum IL-6 levels following photodynamic therapy. Am J Gastroenterol. 2007;102:2164–2170. doi: 10.1111/j.1572-0241.2007.01403.x. [DOI] [PubMed] [Google Scholar]