Abstract
Non-steroidal anti-inflammatory drugs (NSAIDs) constitute a family of drugs, which taken as a group, represents one of the most frequently prescribed around the world. Thus, not surprisingly NSAIDs, along with anti-infectious agents, list on the top for causes of Drug-Induced Liver Injury (DILI). The incidence of liver disease induced by NSAIDs reported in clinical studies is fairly uniform ranging from 0.29/100 000 [95% confidence interval (CI): 0.17-051] to 9/100 000 (95% CI: 6-15). However, compared with these results, a higher risk of liver-related hospitalizations was reported (3-23 per 100 000 patients). NSAIDs exhibit a broad spectrum of liver damage ranging from asymptomatic, transient, hyper-transaminasemia to fulminant hepatic failure. However, under-reporting of asymptomatic, mild cases, as well as of those with transient liver-tests alteration, in conjunction with reports non-compliant with pharmacovigilance criteria to ascertain DILI and flawed epidemiological studies, jeopardize the chance to ascertain the actual risk of NSAIDs hepatotoxicity. Several NSAIDs, namely bromfenac, ibufenac and benoxaprofen, have been withdrawn from the market due to hepatotoxicity; others like nimesulide were never marketed in some countries and withdrawn in others. Indeed, the controversy concerning the actual risk of severe liver disease persists within NSAIDs research. The present work intends (1) to provide a critical analysis of the dissimilar results currently available in the literature concerning the epidemiology of NSAIDS hepatotoxicity; and (2) to review the risk of hepatotoxicity for each one of the most commonly employed compounds of the NSAIDs family, based on past and recently published data.
Keywords: Non-steroidal anti-inflammatory drugs, Side effects, Fulminant hepatic failure, Cholestasis, Liver damage, Liver injury, Hepatitis, Hepatotoxicity
INTRODUCTION
Non-steroidal anti-inflammatory drugs (NSAIDs) are consumed massively worldwide and, along with antimicrobial agents, are the most frequent causes of drug-induced liver injury (DILI)[1-3]. Indeed, roughly 10% of total drug-induced hepatotoxicity is NSAIDs related. Recent data from England indicates that the relative frequency of NSAIDs prescription has changed, i.e. a 4% decline in the consumption of diclofenac and a parallel 5% increase in the use of naproxen are probably due to an increase in the awareness of both gastrointestinal and cardiovascular serious adverse events[4]. The current policy concerning the use of NSAIDs recommends that patients take “the lowest effective dose for the shortest duration” needed to control symptoms. In this particular setting evidence indicates that naproxen is associated with a lower thrombotic risk than coxibs, and that ibuprofen has a good thrombotic safety profile for daily doses of up to 1200 mg[5]. Noticeably, 6% of the US population consumes at least one of these products in a month. Information regarding ibuprofen indicates that 24% is sold as over the counter medication[6].
The paradox is that even when it has been known historically and widely accepted that the use of these NSAIDs is associated with a low rate of hepatic adverse events, it is severe liver damage that is the main adverse event through which these drugs are eventually withdrawn from the market[7]. On the other hand, 50% of fulminant hepatic failure (FHF) in the USA is due to hepatotoxicity[8]. Antimicrobial drugs are the most often involved[9].
Hepatotoxicity is more frequently encountered in post-marketing studies or even after, once the drug has already been launched due to the fact that premarketing recruits a relatively low number of patients, frequently insufficient to fully judge the true incidence of hepatotoxicity[10]. One of the most representative examples of this situation is that of bromfenac-related severe liver damage. Bromfenac was withdrawn from the market in 1998 as a result of multiple reports of FHF within the year of its approval (1 case for every 10 000 exposed individuals)[11,12]. Frequent severe liver damage associated with nimesulide had also been reported[13]. Although nimesulide is currently approved in 50 countries worldwide, national health authorities of several countries have withdrawn nimesulide from the market and others have never approved it[14-16]. EMEA (European Medicines Evaluation Agency) currently recommends a restricted length of treatment (15 d) and a maximal drug dosage (100 mg/d) for nimesulide therapy, which in addition should be avoided in children.
Interestingly, NSAIDs-induced hepatotoxicity may be associated with liver injury six to nine times more frequently in patients who are taking other potentially hepatotoxic medications concomitantly. (i.e. amoxicillin-clavulanic acid, proton pump inhibitor, phenobarbitol, isoniazid)[17,18].
According to a recent study, hepatic steatosis and metabolic syndrome might predispose to an NSAIDs-induced liver toxicity[19], a similar situation to that already proven for methotrexate and halothane.
Finally, chronic alcohol abuse during treatment with paracetamol was associated with an increase in liver injury induced by acetaminophen including those patients who were taking doses not higher than 4 g daily[20].
Our attempt in the present work is two-fold (1) to analyze the clinical impact regarding severity of NSAIDs hepatotoxicity based on a critical analysis of the conflicting epidemiological approaches currently available in the literature; and (2) to review the individual expected risk of hepatotoxicity for NSAIDs most commonly employed in clinical practice based on past and recently published data.
EPIDEMIOLOGY
Epidemiological studies evaluating severe NSAID liver toxicity take into consideration hospitalization and death of the exposed population. One important pitfall to demonstrate the risk of liver damage induced by NSAIDs resides in the epidemiological study design.
Generally speaking, the strengths of randomized control trials (RCT) are the close patient follow up, the comparison with a control group and an accepted design in order to prove specific therapeutic actions. However, RCT frequently represent just a sample of the general population seldom truly representative, particularly as evidence of the incidence of hepatotoxicity[6]. In addition, trials frequently fail to be informative concerning populations under 18 years of age because this group of individuals is usually underrepresented when not openly excluded[21]. On the other hand, data regarding incidence of liver toxicity from cohort, case-control studies and trials are not free from bias. Environmental factors, alcohol abuse, viral infections and metabolic factors coexist with DILI constituting confounding factors. Likewise, retrospective studies have important drawbacks such as researcher unawareness of concurrent drug intake other than the study drug. Other important limiting factors affect both pre- and post-marketing hepatotoxicity studies. Among these is the fact that mild and reversible cases are underreported. The other frequent source of error is the lack of a reliable “denominator” (defined as the number of patients potentially exposed) for calculations. We may also consider an additional source of underestimation of hepatotoxicity which is the report lag - the delay between the occurrence of adverse events and case communication. The latter should be taken into account when the alert is associated with severe liver damage. The incidence of liver disease induced by NSAIDs reported in most studies is fairly uniform ranging from 1 to 9 cases per 100 000 persons exposed[21,22]. In spite of these results, epidemiologists analyzing the real risk of liver disease induced by different NSAIDs usually face difficulties, such as different study designs, different populations (ethnic groups, age and sex) and adjustment variable control methods that add complexity to the data analysis.
Traversa and co-workers analyzed a retrospective study from 1997 through 2001 in a region of Italy (850 000 inhabitants). About 2 million prescriptions corresponding to NSAIDs-treated patients through a 5-year period follow-up were analyzed[23].
One of the main conclusions drawn from this study is that the risk of NSAIDs induced hepatotoxicity is very small (if the number of prescriptions is taken as the denominator, the incidence of liver injury was 1.7 per 100 000 exposed individuals). In contrast, a higher rate of hepatotoxicity was observed among people older than 75 years old (5.7-fold increased risk of liver disease when compared with people under 45 years). Interestingly, it was observed that nimesulide showed both a slightly higher incidence of liver damage and a higher hospitalization rate than that observed with the other NSAIDs (33 per 100 000 patient-years vs 22 per 100 000 patient-years respectively). The authors were unable to find severe liver damage and deaths related to NSAIDs. While the positive features of this study were the high number of patients enrolled and the extended follow-up, the major limitations were that the database monitoring system neither included the reason for prescription nor NSAIDs doses.
In contrast, a case-control study that included prescriptions of all market-approved NSAIDs highlighted diclofenac as the only drug associated with an increased risk of liver damage (95% confidence interval: 1.9-8.8)[24]. Laine and co-workers recently reported the largest prospective, randomized double-blind study comprising four times more patients than the largest previous trials. They evaluated the incidence of diclofenac-induced hepatotoxicity in 17 289 patients, showing that patients who suffered diclofenac-associated adverse drugs reactions seldom required hospital admission (23/100 000 patients). They also observed that symptoms of diclofenac-related liver disease developed either early or late after starting drug therapy[25]. The conclusions were: a low rate of occurrence of diclofenac-related admissions, and a very low rate of diclofenac-associated FHF. Indeed, only one patient required liver hospitalization for every 132 patients with aminotransferase > 3 × upper limit of normal (ULN).
Rostom and co-workers investigated bibliographic databases MEDLINE and EMBASE and public FDA archives in order to identify randomized controlled trials of diclofenac, naproxen, ibuprofen, celecoxib, rofecoxib, valdecoxib, or meloxicam in adults with osteoarthritis or rheumatoid arthritis. The authors analyzed aminotransferase elevations > 3 ULN, liver-related drug discontinuation, serious hepatic adverse events, liver-related hospitalizations, and liver-related deaths[21]. After analyzing 65 database articles and 67 FDA submitted studies, they concluded that diclofenac and rofecoxib had a higher level of transaminases both compared with placebo and with the other studied NSAIDs. Interestingly, none of these studies had a high rate of serious hepatic adverse events, hospitalizations or death.
The authors found only 1 hospital admission (naproxen) observed among 37 671 patients included in studies reporting hospitalization. This very low hospitalization rate represents 3 per 100 000 patients (0.5-15 per 100 000 patients). One patient died due to naproxen liver toxicity among 51 942 patients consuming NSAIDs, which in turn also represents a low death rate: 2 per 100 000 patients (0.3-11 per 100 000 patients).
These results are in concordance with those reported by Rubenstein and Laine who also analyzed several epidemiologic studies designed to determine the incidence and risk of serious liver-related NSAIDs toxicity[26]. Seven studies met the inclusion criteria proposed by the authors. They observed an incidence of liver toxicity associated with hospital admission ranging from 3.1-23.4/100 000 patient-years related to current use of NSAIDs, with an excess risk compared with past NSAIDs users of 4.8-8.6/100 000 patient-years of exposure. Moreover, these researchers documented zero mortality associated with NSAIDs when cumulative exposure of liver damage was analyzed in 396 392 patients/year.
Most of the information regarding the incidence and relative risk of hepatotoxicity associated with NSAIDs comes from cohort or case control studies and usually shows a low incidence of hepatotoxicity (Table 1).
Table 1.
Results of population-based studies showing liver toxicity induced by non-steroidal anti-inflammatory drugs
| Authors | Study design | Incidence rate of hepatotoxicity (ALT ≥ 3 ULN) per 100 000 patient-years (95% CI) |
| García Rodríguez et al[22], 1992 | Retrospective cohort study, cross over design | 9/100 000 (6-15) |
| Traversa et al[23], 2003 | Retrospective cohort | 1.4/100 000 (1.0-2.1) |
| de Abajo et al[24], 2004 | Retrospective population-based case-control study | 2.4/100 000 (2.0-2.8) |
| Rubenstein et al[26], 2004 | Systematic review (hospitalization or death) | 3.1 to 23.4/100 000 |
| Rostom et al[21], 2005 | Systematic review | 0.29/100 000 (0.17-0.51) |
| Laine et al[25], 2009 | Long-term prospective trial | 2.1/100 000 (1.9-2.3) |
ALT: Alanine transaminase; ULN: Upper limit of normal; CI: Confidence interval.
Great efforts have been made to identify those clinical factors predictive of severe liver damage induced by drugs. Several years ago the FDA along with Representatives of Pharmaceutical Research and Manufacturers of America (PhRMA) and the American Association for the Study of Liver Disease (AASLD) constituted a working group to study how to minimize the risk of hepatotoxicity[27]. Despite valuable effort, expert consensus could not be achieved concerning: (1) biochemical markers of liver injury to applied used in pre-marketing studies; and (2) clinical parameters able to predict severe liver injury. Yet today we still continue using transaminases level higher than three times the ULN as a marker of significant hepatocellular injury[28].
CHARACTERISTICS OF NSAIDS INDUCED LIVER TOXICITY
The discovery of aspirin in 1946 followed by that of phenylbutazone was the beginning of the NSAIDs era. However, not until 1960 was indomethacin marketed. On the other hand, during the 1950s, ibuprofen was the second drug (along with aspirin) approved to be sold as over the counter medication. Interestingly, most of these substances were employed during the 60s, before the prostaglandin era.
The NSAIDs chemical classification recognizes four major groups of molecules: (1) carboxylic acids; (2) oxicams carboxamides; (3) sulphonanilides diaryl-substituted; and (4) pyrazole/furanones[29]. From the clinical stand point NSAIDs induced hepatotoxicity is associated with different patterns of clinical presentation, several mechanisms of liver damage and various pathological patterns.
We will only describe below the clinical characteristics of several NSAIDs that may be associated with a potential liver injury (Table 2).
Table 2.
Liver-related hepatotoxicity induced by non-steroidal anti-inflammatory drugs
| Drug | Pattern of liver damage | Proposed mechanism | Incidence |
| Aspirin | Acute and chronic hepatitis | Dose dependent | Low |
| Reye’s syndrome | > with high dose | ||
| Diclofenac | Acute and chronic hepatitis | Metabolic | Low |
| Mixed damage and pure cholestasis | Immunologic | ||
| Sulindac | Acute hepatitis and mixed injury | Hypersensivity | Moderate |
| Ibuprofen | Acute hepatitis, ductopenia | Metabolic | Low |
| Naproxen | Cholestatic, mixed damage | Metabolic | Low |
| Coxibs | Acute hepatitis, mixed damage | Probably metabolic | Low |
| Oxicams | Acute hepatitis, massive and submassive necrosis, cholestasis and ductopenia | Metabolic | Low |
| Nimesulide | Acute hepatitis, pure cholestasis | Probably metabolic | Moderate |
Acetaminophen was not taken into account because most cases of liver damage are due to suicide attempts but a minority of cases are accidental and related to use of paracetamol as a therapeutic prescription. Acetaminophen-induced hepatotoxicity should be described separately and not within this topic.
ASPIRIN
Although liver toxicity induced by aspirin is considered to be dose-dependent, there is evidence that rheumatic patients may have predisposing conditions that may increase individual risk of liver damage. Hypoalbuminemia in patients with systemic lupus erythematosus and juvenile rheumatoid arthritis are two well documented risk factors for increased susceptibility to liver injury[30,31]. In addition, studies in rats have shown that aspirin hepatotoxicity is more common in animals with experimentally-induced rheumatoid arthritis compared to that observed in those without arthritis[32]. The clinical presentation of liver toxicity is often anicteric (jaundice at less than 5%) and transaminase levels correlate with serum salicylate levels (> 25 mg/100 mL)[33]. Focal nonspecific necrosis, hepatocellular degeneration and hydropic changes are commonly seen in liver histology[34]. Aspirin can also produce a mitochondrial dysfunction pattern that may lead to a liver free fatty acid accumulation and subsequently develop into a severe metabolic disorder associated with hepatic massive micro-steatosis. This syndrome, known as Reye’s Syndrome, is characterized by metabolic acidosis, hepatic encephalopathy, hypoglycemia, coagulopathy and azotemia. Reye’s disease induced by aspirin is a rarity since aspirin is currently avoided in pediatric patients and replaced by ibuprofen and paracetamol.
A recent experimental study in rats suggests that salicylic acid could trigger mitochondrial dysfunction causing a marked fall in intracellular ATP which in turn leads to a lethal hepatocellular injury mediated by a lipid peroxidation mechanism[35].
DICLOFENAC
Diclofenac is the most widely used NSAID in the world[36,37]. The vast majority of data related to hepatic reactions comes from retrospective studies. There were no more than 60 cases of diclofenac hepatotoxicity reported in the literature until Banks and co-workers in 1995 reported their analysis of 180 cases referred to FDA from 1988 through 1991. The authors observed evidence of liver disease in 85% of the patients within the first 6 mo after drug intake. Interestingly, a higher latency (after 6 mo) was observed in 12% of cases[38]. The long latency period observed in a large number of cases in addition to the absence of hypersensibility support a metabolic mechanism of hepatotoxicity. Jaundice was a very common sign present in 90 out of 120 patients. A total of 7 jaundiced patients died as a result of liver disease. In this analysis liver function tests (LFTs) showed a mixed (hepatocellular and cholestatic) pattern in 66% of cases, cholestatic in 8% and indeterminate in the remainder of the group. In contrast to Jick’s point of view which suggests that hepatotoxicity induced by diclofenac is an uncommon event[39], the study by Banks proposed for the first time that diclofenac is a much more common cause of liver damage than so far suspected[38]. This concept was reinforced in a recent report from Laine who conducted the longest and largest liver-related diclofenac study so far ever reported [Multinational Etoricoxib and Diclofenac Arthritis Long-Term (MEDAL) program][25]. They conducted a prospective, randomized and double-blind study analyzing the frequency of diclofenac induced liver reactions in 17 289 patients. The authors randomized only those osteoarthritis or rheumatoid arthritis patients over 50 years of age who were going to receive diclofenac therapy (150 mg daily) or etoricoxib (60 or 90 mg daily). They also excluded cases with previous liver disease or more than 14 weekly alcohol drinks. Hypertransaminasemia > 3 × ULN was observed in over 3% of arthritic patients with a regular intake of diclofenac. It is interesting to point out that alanine transaminase (ALT) values higher than 10 × ULN were only identified in 0.5% of cases[25]. The incidence of diclofenac liver-related hospitalizations in this study was 16 per 100 000 patient-years. Through these results, the authors provide evidence that diclofenac is a very safe drug. The small number of related hospitalizations (0.023%), and Hy’s cases (transaminases > × 3 ULN and bilirubin > 2 ULN or a fatal outcome or liver transplantation) (0.012%) are the strongest evidence showing that diclofenac bears a low liver toxicity rate.
These data are in concordance with those observed by Traversa and co-workers showing ibuprofen and naproxen also displayed a low hepatotoxicity rate. However, in this latter study nimesulide had a higher hospitalization rate when compared with a past control cohort (33 per 100 000 patient-years)[23]. In a systematic analysis of several randomized studies, Rostom and co-workers also found a very low frequency of hospital admissions due to NSAIDs related-liver disease in 4261 patients (3 per 100 000 patient) and 0% when diclofenac was evaluated separately[21].
Diclofenac is a typical example of the combination of factors resulting in hepatotoxicity (e.g. drug metabolism, reactive metabolite formation and clearance) determining the actual development and the severity of liver damage. Moreover, diclofenac might produce liver injury through either metabolic idiosyncrasy or an immunological mechanism generated by drug adduct formation[8].
SULINDAC
Sulindac (SLD) is associated with an increased incidence of liver toxicity and serious hepatic reactions (5-10 times) when compared with other NSAIDs. Besides its recognized anti-inflammatory mechanism through the inhibition of cyclooxygenase (COX 1 and 2), SLD became very popular due to its antiapoptotic effect in colonic polyposis treatment[40]. SLD induced hepatotoxicity was more frequently encountered among people over 50 years old. Regarding the mechanism of hepatotoxicity, SLD associated DILI is one other example of a combination of factors as judged by the conflicting results present in the literature. Indeed, in a series of 91 documented cases reported to FDA a predominantly cholestatic pattern was present in 43% while hepatocellular-related changes were found in 25% of patients[41]. Moreover, a hypersensitivity mechanism of liver injury was present in 60% of cases. Zou et al[42] recently reported an interesting pilot study showing that co-treatment of SLD and lipopolysaccharide (LPS) caused liver injury in rats. In this context they also found a selectively clotting system activation and fibrinolytic system inhibition in rats treated with SLD/LPS. These changes were also associated with tisular hypoxia and fibrin clot deposit in the hepatic sinusoids[42]. Researchers suggest that these results may be extrapolated to humans with the disease. Furthermore, they hypothesize that hypoxia in the frame of the SLD/LPS association may underlie the idiosyncratic model where the sulfide metabolite probably plays a central role.
Another experimental study carried out by the same authors shows that tumor necrosis factor (TNF)-α augmented the cytotoxicity of SLD sulfide in primary hepatocytes and HepG2 cells. These results suggest that TNF-α can enhance SLD sulfide-induced hepatotoxicity, thereby contributing to liver injury in SLD/LPS-cotreated rats[43].
Regrettably the current coexistence of conflicting and heterogeneous results precludes us from reaching valid conclusions regarding SLD DILI.
IBUPROFEN
Ibuprofen has a recognized anti-inflammatory, analgesic and antipyretic property and is one of the most commonly NSAIDs used worldwide. It is characterized by a high safety profile and very low liver toxicity incidence. Along with paracetamol and aspirin, ibuprofen has become one of the largest ever selling over the counter drugs. It was first introduced to the UK market in 1969 and due to the low rate of gastrointestinal adverse events, it has ever since almost replaced aspirin, indometacin and phenylbutazone in arthritic patients[44]. A scarce number of hepatotoxicity reports involving ibuprofen were published, associated to both hepatocellular and cholestatic liver damage. Indeed, one of the latter cases was linked to vanishing bile duct syndrome[45,46]. It has also been suggested that ibuprofen may increase the risk of liver injury when administered to patients with chronic hepatitis C. An ibuprofen associated increase of transaminases > 5 × UNL was recently reported in three patients with chronic hepatitis C, eventually confirmed by re-challenge[47].
Traversa et al[23] in their cohort study that recruited thousands of patients receiving various NSAIDs confirmed that ibuprofen has a very low liver toxicity rate: Only two patients showed ibuprofen-associated liver injury (out of 126 cases that had NSAIDs). Despite the massive use of this drug worldwide, a low rate of ibuprofen liver toxicity along with a low incidence of gastrointestinal, renal and cardiovascular serious events characterizes the safety profile. This is probably based on the fact ibuprofen has a short plasma half life and does not form pathological metabolites.The absence of reports including ibuprofen induced liver injury in several studies and meta-analyses, strongly suggests that ibuprofen is an unlikely cause of liver disease[48-50].
COXIBS
Coxibs are NSAIDs designed to selectively inhibit COX-2. Lately, this group of drugs has been gaining worldwide popularity due to a much better gastrointestinal safety profile when compared with nonselective NSAIDs[25]. However, NSAIDs-induced cardiovascular adverse events have generated significant controversy[51,52]. Due to increased risk of myocardial infarction and arterial hypertension, rofecoxib was removed from the market by Merck in 2004[53]. Valdecoxib was also voluntarily discontinued by manufacturer Bextra, Pfizer Canada Inc and by FDA in 2005 because of severe allergic skin lesions including cases of Stevens-Johnson syndrome and also because of an increased risk of heart and stroke attack[54]. On the other hand, celecoxib continues to be marketed in many countries. Laine and coworkers recently published a comprehensive evaluation of the literature up to 2007 analyzing controlled trials, meta-analyses and reviews related to the safety profile of selective inhibitors of COX-2 in patients with osteoarthritis (OA)[55]. Their results are truly encouraging and show that coxibs have a therapeutic efficacy comparable to other NSAIDs and higher than that of acetaminophen. This was observed when patients with OA were treated for moderate to severe degree of pain. Through meta-analysis the authors documented that coxibs have a 74% lower risk of gastro-duodenal ulcer complications. In contrast, they found a double risk of myocardial infarction vs placebo and naproxen treated patients. There were no significant differences in cardiovascular risk between coxibs compared with non-naproxen NSAIDs. Despite these encouraging results, FDA reported an alert related to the increase of cardiovascular risk induced by coxibs.
Coxib-induced liver injury is an uncommon event and the annual reported incidence of hepatotoxicity is 1 in 100 000 exposed persons[56]. A long term study evaluating the safety profile of celecoxib in arthritics patients (Celecoxib Long-term Arthritis Safety Study-CLASS) found increased transaminase level in 0.6 % patients[57].
A rise of transaminase level was also reported and associated with rofecoxib (2%) and with higher doses of lumiracoxib (3%). In this study, a higher frequency of clinical hepatitis was found in patients receiving 400 mg of lumiracoxib when compared with ibuprofen and naproxen treated patients[58]. In another survey, lumiracoxib was linked to severe hepatocellular necrosis[59]. Health authorities from United Kingdom subsequently removed it from the market. Scottish authorities reported 20 cases of severe liver disease probably associated with lumiracoxib. FHF was documented in 14 out of 20 patients (two patients died and three patients needed liver transplantation). In addition, recent postmarketing reports from Australia of severe hepatic reactions with lumiracoxib at doses of at least 200 mg (two patients died and 2 underwent liver transplantation) led also to its withdrawal from the market in that country[60].
On the other hand, rofecoxib was associated with a low rate of hepatic reactions and an increase of ALT ≥ 3 × UNL was documented in 1.8/100 000 exposed persons[55], but despite this excellent safety profile, Yan and colleagues reported two well-documented cases of cholestatic hepatitis induced by rofecoxib[61]. The first patient showed a high level of alkaline phosphatase (APH) associated with hepatocellular injury in zone 1 whereas in the other case a significant increase in ALT associated with a minimum increase of APH was documented. In this latter patient mild liver damage in both acinar zones 1 and 3 was described. In contrast, four other published cases of rofecoxib induced liver toxicity were characterized by predominant cholestatic presentation[62,63].
To our knowledge no case of etoricoxib severe hepatotoxicity has ever been published. However, transaminase elevation (3 × ULN) has been reported in 1% of patients treated with etoricoxib for up to one year[21,64].The mechanism of liver damage induced by coxibs has not yet been completely elucidated. Kung and co-workers recently suggested that the bioactivation of lumiracoxib and its metabolite [4’-hydroxylumiracoxib (M5)] may produce GSH depletion, covalent binding to proteins and oxidative stress, that in turn may lead to liver injury[65].
Nevertheless, hepatotoxicity caused by non-selective NSAIDs has been more extensively studied. Furthermore, mitochondrial injury, cholestasis and oxidative stress induced by a reactive metabolite formation constitute the most conspicuous molecular reported disorders. An attractive hypothesis suggests that NSAIDs inhibition of COX-2, might cause liver damage through a prostaglandin (PGs) pathway. Regarding this concept the authors proposed that the inhibition of PGE2 could down regulate the antiapoptotic mitochondrial protein Bcl-2, which protects against bile acid induced apoptosis[66].
OXICAMS
Oxicams induced hepatotoxicity is an uncommon clinical situation. Piroxicam induced severe hepatocellular necrosis was the most frequent reported clinical pattern[35,67,68]. Uneventful recovery, death and need of liver transplantation have all been reported[69,70]. On the other hand, a clinical and histological pattern of hepatocellular plus cholestatic (mixed) injury was also associated with piroxicam in one single case. LFTs normalization was observed in this patient within 4 mo after starting the clinical disease[71], Interestingly, a case of severe intrahepatic cholestasis linked to a long period of piroxicam intake, was originally described 20 years ago[72].
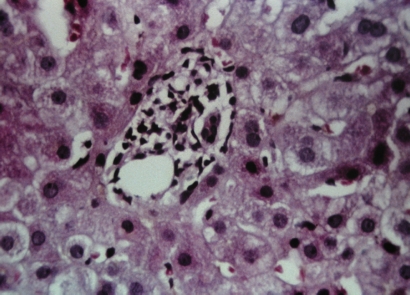
Only two patients with piroxicam-induced liver toxicity were admitted to our liver unit during the last three decades (unpublished data). The first patient was a 44-year-old woman with clinical and histological evidence of submassive necrosis. The patient developed ascites and liver failure after 28 d of drug intake and uneventfully recovered without liver transplantation in 95 d from clinical onset. The other case was a 42-year-old man admitted with clinical and biochemical manifestations of severe cholestasis after piroxicam treatment as the single medication for 58 d. Liver histology showed a typical hepato-canalicular cholestasis associated with ductopenia (Figure 1). This latter case progressively evolved to prolonged cholestasis with asthenia, anorexia and intolerable itching. He underwent corticosteroids therapy for 30 d. We were able to document a complete biochemical recovery 120 d from the clinical onset.
Figure 1.
Piroxicam induced hepato-canalicular cholestasis associated with ductopenia (notice absence of bile duct in the portal tract).
Other oxicam derivatives were also occasionally implicated in cases of acute cholestatic hepatitis included isoxicam and droxicam[73].
The mechanism of oxicams-induced hepatotoxicity appears to be idiosyncratic and dose independent. Due to the absence of immunoallergic features in most of the reported cases, it is very difficult to support an immune-mediated mechanism of liver injury[74].
NIMESULIDE
Nimesulide has analgesic, anti-inflammatory and anti-pyretic activity due to potent inhibitory effects on the COX-2 enzymes. Nimesulide bears a good gastro-intestinal tolerance. The mechanism of action has been attributed to a unique chemical structure of the sulphonanilides class of NSAIDs[75].
Our group in Argentina reported the first observation linking nimesulide with liver toxicity in 1997[76]. Since then, a steady flow of reports confirmed severe forms of hepatotoxicity, to the point that national health authorities of several countries withdrew nimesulide from the market[77-88]. Despite this, nimesulide commercialization is still maintained in several European countries, although the EMEA reports recommend a length of therapy restricted to 15 d and maximal dosage of 100 mg/d[13]. Controversy regarding nimesulide persists due to the fact that clinical series reports and epidemiological trials continue to involve nimesulide in severe liver damage[19,89,90]. On the other hand, health institutions conclude that nimesulide-induced-liver injury is statistically comparable to that of the remainder of the NSAIDs[91,92].
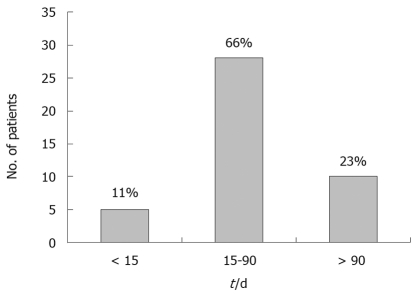
In our institution, 5 out of 30 cases (17%) had severe liver injury[93]. In 2009 our series included 43 well documented cases of nimesulide-induced liver damage associated to a wide clinical and histological spectrum of hepatotoxicity[94]. To our knowledge this constitutes the largest series of nimesulide hepatotoxicity ever reported. The main clinical symptoms at presentation are jaundice (70%), malaise (65%) and pruritus (50%). Interestingly, two thirds of patients start liver toxicity 15 to 90 d after drug intake. Relevant to drug safety, in only 11% latency was shorter than 15 d (Figure 2). On the other hand, normalization exceeded 90 d in 27% of cases[94]. In cholestatic liver injury, normalization of alkaline phosphatase serum level usually takes more time than transaminases (i.e. more than 1 year)[95].
Figure 2.
Latency (time from nimesulide intake to clinical onset) in 43 patients.
Nine patients in our series developed severe liver disease and FHF was observed in 6 cases. In agreement with the recent publication by Walker et al[96], this subpopulation was composed predominantly of females older than 50 years. Two patients died before liver transplant due to multiorgan failure, while a 9-year-old girl successfully underwent orthotopic liver transplantation.
We observed a wide range of variations of ALT/aspartate transaminase level in concordance with Bjarnason who analyzed 33 case reports documenting an elevation of ALT of at least 2-fold in 100%, and a 5-fold elevation in 89% of patients[97].
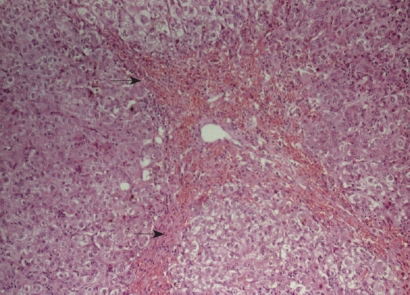
Nimesulide hepatotoxicity shows a wide spectrum of liver damage including acute hepatitis, cholestasis, mixed forms, massive and submassive hepatic necrosis. We found hepatocellular necrosis (Figure 3) in 64%, cholestatic hepatitis in 27% and pure cholestasis in 9 %[94].
Figure 3.
Acute hepatitis induced by nimesulide (hepatocellular collapsed areas are shown with arrows).
The mechanism of nimesulide induced hepatotoxicity remains unknown. It has been suggested that it could be due to the formation of a reactive metabolite. On the other hand, individual genetic variations in drug metabolism have also been proposed.
Acknowledging the true impact of nimesulide on the liver is not an easy task. Despite the proliferation of reports describing nimesulide-induced severe liver injury (mainly Argentina, Ireland and Finland), the epidemiological studies have almost unanimously concluded that severe hepatotoxicity is of low incidence determining a positive risk-benefit-ratio. Inquiring about nimesulide intake should be incorporated into standard anamnesis of liver disease, especially when acute liver damage is being investigated.
Addendum
Other than the previously analyzed drugs, indomethacin, naproxen, meloxican, tenoxican and etodoloc have also been associated with various hepatic reactions[73].
CONCLUSION
Aspirin was the first discovered NSAID. Dose dependent liver injury is accepted as the prevalent mechanism. Liver toxicity rate is very low currently since aspirin has been replaced by paracetamol and ibuprofen in pediatric patients and in various rheumatic diseases.
Diclofenac is probably the most used NSAID in rheumatology. Severe liver reactions and diclofenac hospitalization rate are uncommon. An increase in ALT levels of 3-10 × ULN is observed in 3% of cases.
Sulindac induced hepatotoxicity was documented more than fifty years ago. Liver damage occurrence was reported to be 5-10 times higher than that of other NSAIDs. A hypersensivity mechanism of liver injury was the most prevalent liver reaction.
Ibuprofen has the highest liver safety profile among NSAIDs and showed no severe liver injury in larger studies. Along with paracetamol and aspirin, it is considered one of the most common over the counter NSAIDs sold in the world.
Coxibs have currently replaced several NSAIDs due to safer GI profile. However, the high rate of cardiovascular events associated to rofecoxib is the main drawback related to drug marketing. Despite liver damage being a rare clinical situation, lumiracoxib has been discontinued in several countries due to severe hepatotoxicity.
Oxicams are associated with a well-documented hepatic safety profile. Uncommonly, piroxicam may cause severe hepatocellular damage. The clinical and histological pattern may be mixed or associated to clinical and biochemical prolonged cholestasis with or without ductopenia. Isoxicam and droxicam were only linked to liver toxicity in sporadic reports. The mechanism of liver damage appears to be an idiosyncratic one.
Nimesulide was removed from the market in several countries due to severe liver damage described in clinical series, but various epidemiological surveys do not document these findings. EMEA recommends that nimesulide should only be used for short periods at daily doses not higher than 200 mg/d in adults.
In summary, neither documenting the possibility of the causative role of a drug when confronting liver damage in an individual patient nor determining the true incidence of NSAIDs induced hepatotoxicity in the general population, are easy tasks. Rigorous data collecting, caution and clinical commitment are required when judging potential hepatotoxicity. The clinician always needs to critically evaluate the possibility whether other factors may play a role in the actual findings.
Despite the shortage of well-designed epidemiological studies, there is evidence showing that most of the NSAIDs are safe drugs with low risk of liver injury (mostly ranging from 0.29-3.1/100 000 exposed individuals when recent based-population studies were analyzed).
Both sulindac and nimesulide have been linked to a higher frequency of liver damage. NSAIDs induced liver injury which might potentially lead to a fatal outcome or need liver transplantation. As in other forms of DILI, jaundice entails poor prognosis with 25% of jaundiced patients developing severe liver disease. Drugs with an increased risk of liver damage should undergo close LFTs monitoring in order to prompt drug withdrawal to avoid severe hepatotoxicity.
Acknowledgments
I would like to thank Professor Luis Colombato for his support and for reviewing this manuscript and to Professor Miguel Bruguera for his counsel and advice.
Footnotes
Peer reviewer: Dr. Christoph Reichel, Priv.-Doz., Head, the Gastroenterological Rehabilitation Center Bad Brückenau, Clinic Hartwald, German Pension Insurance Federal Office, Schlüchterner Str. 4, 97769 Bad Brückenau, Germany
S- Editor Wang JL L- Editor O'Neill M E- Editor Lin YP
References
- 1.Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, García-Ruiz E, García-Muñoz B, González-Grande R, Pizarro A, Durán JA, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology. 2005;129:512–521. doi: 10.1016/j.gastro.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Bjornsson E. Review article: drug-induced liver injury in clinical practice. Aliment Pharmacol Ther. 2010;32:3–13. doi: 10.1111/j.1365-2036.2010.04320.x. [DOI] [PubMed] [Google Scholar]
- 3.Hussaini SH, Farrington EA. Idiosyncratic drug-induced liver injury: an overview. Expert Opin Drug Saf. 2007;6:673–684. doi: 10.1517/14740338.6.6.673. [DOI] [PubMed] [Google Scholar]
- 4.Fosbøl EL, Gislason GH, Jacobsen S, Folke F, Hansen ML, Schramm TK, Sørensen R, Rasmussen JN, Andersen SS, Abildstrom SZ, et al. Risk of myocardial infarction and death associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs) among healthy individuals: a nationwide cohort study. Clin Pharmacol Ther. 2009;85:190–197. doi: 10.1038/clpt.2008.204. [DOI] [PubMed] [Google Scholar]
- 5.Drug Safety Update. Volume 2, Issue 7, February 2009. [Google Scholar]
- 6.Goldkind L, Laine L. A systematic review of NSAIDs withdrawn from the market due to hepatotoxicity: lessons learned from the bromfenac experience. Pharmacoepidemiol Drug Saf. 2006;15:213–220. doi: 10.1002/pds.1207. [DOI] [PubMed] [Google Scholar]
- 7.Aithal GP, Day CP. Nonsteroidal anti-inflammatory drug-induced hepatotoxicity. Clin Liver Dis. 2007;11:563–575, vi-vii. doi: 10.1016/j.cld.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Watkins PB, Seligman PJ, Pears JS, Avigan MI, Senior JR. Using controlled clinical trials to learn more about acute drug-induced liver injury. Hepatology. 2008;48:1680–1689. doi: 10.1002/hep.22633. [DOI] [PubMed] [Google Scholar]
- 9.Reuben A, Koch DG, Lee WM. Acute liver failure secondary to drug induced liver injury: causes and consequences (Abstract) Hepatology. 2009;50 Suppl:347A. [Google Scholar]
- 10.Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:474–485. doi: 10.1056/NEJMra021844. [DOI] [PubMed] [Google Scholar]
- 11.Rabkin JM, Smith MJ, Orloff SL, Corless CL, Stenzel P, Olyaei AJ. Fatal fulminant hepatitis associated with bromfenac use. Ann Pharmacother. 1999;33:945–947. doi: 10.1345/aph.18364. [DOI] [PubMed] [Google Scholar]
- 12.Hunter EB, Johnston PE, Tanner G, Pinson CW, Awad JA. Bromfenac (Duract)-associated hepatic failure requiring liver transplantation. Am J Gastroenterol. 1999;94:2299–2301. doi: 10.1111/j.1572-0241.1999.01321.x. [DOI] [PubMed] [Google Scholar]
- 13.EMEA: European Medicines Agency. European Medicines Agency recommends restricted use of nimesulide-containing medicinal products (on-line) Available from: http://www.emea.europa.eu/pdfs/general/direct/pr/43260407en.pdf.
- 14.ANMAT Administración Nacional de Medicamentos Alimentos y Tecnología Medica Disposición 4087/03 (on-line) Argentina Acceso: 15/08/2009. Available from: http://www.anmat.gov.ar.
- 15.Nota informativa de la Agencia Española del Medicamento sobre Nimesulida. 2002. Available from: http://www.osanet.euskadi.net/contenidos/informacion/notas_seg_cevime/eu_1676/adjuntos/02-05-06nimesulida.pdf.
- 16.WHO Pharmaceuticals Newsletter 2002, No. 04. Available from: http://apps.who.int/medicinedocs/fr/d/Js4943e/3.1.html.
- 17.García Rodríguez LA, Williams R, Derby LE, Dean AD, Jick H. Acute liver injury associated with nonsteroidal anti-inflammatory drugs and the role of risk factors. Arch Intern Med. 1994;154:311–316. doi: 10.1001/archinte.1994.00420030117012. [DOI] [PubMed] [Google Scholar]
- 18.Pérez Gutthann S, García Rodríguez LA. The increased risk of hospitalizations for acute liver injury in a population with exposure to multiple drugs. Epidemiology. 1993;4:496–501. [PubMed] [Google Scholar]
- 19.Licata A, Calvaruso V, Cappello M, Craxì A, Almasio PL. Clinical course and outcomes of drug-induced liver injury: nimesulide as the first implicated medication. Dig Liver Dis. 2010;42:143–148. doi: 10.1016/j.dld.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 20.Verma S, Kaplowitz N. Diagnosis, management and prevention of drug-induced liver injury. Gut. 2009;58:1555–1564. doi: 10.1136/gut.2008.163675. [DOI] [PubMed] [Google Scholar]
- 21.Rostom A, Goldkind L, Laine L. Nonsteroidal anti-inflammatory drugs and hepatic toxicity: a systematic review of randomized controlled trials in arthritis patients. Clin Gastroenterol Hepatol. 2005;3:489–498. doi: 10.1016/s1542-3565(04)00777-3. [DOI] [PubMed] [Google Scholar]
- 22.García Rodríguez LA, Pérez Gutthann S, Walker AM, Lueck L. The role of non-steroidal anti-inflammatory drugs in acute liver injury. BMJ. 1992;305:865–868. doi: 10.1136/bmj.305.6858.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Traversa G, Bianchi C, Da Cas R, Abraha I, Menniti-Ippolito F, Venegoni M. Cohort study of hepatotoxicity associated with nimesulide and other non-steroidal anti-inflammatory drugs. BMJ. 2003;327:18–22. doi: 10.1136/bmj.327.7405.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Abajo FJ, Montero D, Madurga M, GarcÃa RodrÃguez LA. Acute and clinically relevant drug-induced liver injury: a population based case-control study. Br J Clin Pharmacol. 2004;58:71–80. doi: 10.1111/j.1365-2125.2004.02133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laine L, Goldkind L, Curtis SP, Connors LG, Yanqiong Z, Cannon CP. How common is diclofenac-associated liver injury? Analysis of 17,289 arthritis patients in a long-term prospective clinical trial. Am J Gastroenterol. 2009;104:356–362. doi: 10.1038/ajg.2008.149. [DOI] [PubMed] [Google Scholar]
- 26.Rubenstein JH, Laine L. Systematic review: the hepatotoxicity of non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2004;20:373–380. doi: 10.1111/j.1365-2036.2004.02092.x. [DOI] [PubMed] [Google Scholar]
- 27.FDA Working Group. PhRMA/FDA/AASLD. Drug-induced hepatotoxicity: white paper, postmarketing considerations. PhRMA/FDA/AASLD: 2000; 1-29. Accessed October 29, 2008. Available from: http://www.fda.gov/cder/livertox/postmarket.pdf. [Google Scholar]
- 28.FDA Working Group. Guidance for Industry Drug-Induced Liver Injury: Premarketing Clinical Evaluation. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER), July 2009. [Google Scholar]
- 29.Rainsford KD. Anti-inflammatory drugs in the 21st century. Subcell Biochem. 2007;42:3–27. doi: 10.1007/1-4020-5688-5_1. [DOI] [PubMed] [Google Scholar]
- 30.Zimmerman HJ. Editorial: Aspirin-induced hepatic injury. Ann Intern Med. 1974;80:103–105. doi: 10.7326/0003-4819-80-1-103. [DOI] [PubMed] [Google Scholar]
- 31.Russell AS, Sturge RA, Smith MA. Serum transaminases during salicylate therapy. Br Med J. 1971;2:428–429. doi: 10.1136/bmj.2.5759.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rainsford KD. Side-effects and toxicology of the salicylates. In: Rainsford KD, ed , editors. Aspirin and Related Drugs. Boca Raton, Florida: CRC Press; 2004. pp. 367–554. [Google Scholar]
- 33.Teoh NC, Farrell GC. Hepatotoxicity associated with non-steroidal anti-inflammatory drugs. Clin Liver Dis. 2003;7:401–413. doi: 10.1016/s1089-3261(03)00022-9. [DOI] [PubMed] [Google Scholar]
- 34.Zimmerman HJ. Effects of aspirin and acetaminophen on the liver. Arch Intern Med. 1981;141:333–342. doi: 10.1001/archinte.141.3.333. [DOI] [PubMed] [Google Scholar]
- 35.Doi H, Horie T. Salicylic acid-induced hepatotoxicity triggered by oxidative stress. Chem Biol Interact. 2010;183:363–368. doi: 10.1016/j.cbi.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 36.Cannon CP, Curtis SP, Bolognese JA, Laine L. Clinical trial design and patient demographics of the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) study program: cardiovascular outcomes with etoricoxib versus diclofenac in patients with osteoarthritis and rheumatoid arthritis. Am Heart J. 2006;152:237–245. doi: 10.1016/j.ahj.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 37.Cannon CP, Curtis SP, FitzGerald GA, Krum H, Kaur A, Bolognese JA, Reicin AS, Bombardier C, Weinblatt ME, van der Heijde D, et al. Cardiovascular outcomes with etoricoxib and diclofenac in patients with osteoarthritis and rheumatoid arthritis in the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) programme: a randomised comparison. Lancet. 2006;368:1771–1781. doi: 10.1016/S0140-6736(06)69666-9. [DOI] [PubMed] [Google Scholar]
- 38.Banks AT, Zimmerman HJ, Ishak KG, Harter JG. Diclofenac-associated hepatotoxicity: analysis of 180 cases reported to the Food and Drug Administration as adverse reactions. Hepatology. 1995;22:820–827. [PubMed] [Google Scholar]
- 39.Jick H, Derby LE, García Rodríguez LA, Jick SS, Dean AD. Liver disease associated with diclofenac, naproxen, and piroxicam. Pharmacotherapy. 1992;12:207–212. [PubMed] [Google Scholar]
- 40.Guldenschuh I, Hurlimann R, Muller A, Ammann R, Mullhaupt B, Dobbie Z, Zala GF, Flury R, Seelentag W, Roth J, et al. Relationship between APC genotype, polyp distribution, and oral sulindac treatment in the colon and rectum of patients with familial adenomatous polyposis. Dis Colon Rectum. 2001;44:1090–1097; discussion 1097-1099. doi: 10.1007/BF02234627. [DOI] [PubMed] [Google Scholar]
- 41.Tarazi EM, Harter JG, Zimmerman HJ, Ishak KG, Eaton RA. Sulindac-associated hepatic injury: analysis of 91 cases reported to the Food and Drug Administration. Gastroenterology. 1993;104:569–574. doi: 10.1016/0016-5085(93)90428-f. [DOI] [PubMed] [Google Scholar]
- 42.Zou W, Devi SS, Sparkenbaugh E, Younis HS, Roth RA, Ganey PE. Hepatotoxic interaction of sulindac with lipopolysaccharide: role of the hemostatic system. Toxicol Sci. 2009;108:184–193. doi: 10.1093/toxsci/kfn259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zou W, Beggs KM, Sparkenbaugh EM, Jones AD, Younis HS, Roth RA, Ganey PE. Sulindac metabolism and synergy with tumor necrosis factor-alpha in a drug-inflammation interaction model of idiosyncratic liver injury. J Pharmacol Exp Ther. 2009;331:114–121. doi: 10.1124/jpet.109.156331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rainsford KD. Ibuprofen: pharmacology, efficacy and safety. Inflammopharmacology. 2009;17:275–342. doi: 10.1007/s10787-009-0016-x. [DOI] [PubMed] [Google Scholar]
- 45.Alam I, Ferrell LD, Bass NM. Vanishing bile duct syndrome temporally associated with ibuprofen use. Am J Gastroenterol. 1996;91:1626–1630. [PubMed] [Google Scholar]
- 46.Laurent S, Rahier J, Geubel AP, Lerut J, Horsmans Y. Subfulminant hepatitis requiring liver transplantation following ibuprofen overdose. Liver. 2000;20:93–94. doi: 10.1034/j.1600-0676.2000.020001093.x. [DOI] [PubMed] [Google Scholar]
- 47.Riley TR 3rd, Smith JP. Ibuprofen-induced hepatotoxicity in patients with chronic hepatitis C: a case series. Am J Gastroenterol. 1998;93:1563–1565. doi: 10.1111/j.1572-0241.1998.00484.x. [DOI] [PubMed] [Google Scholar]
- 48.Boureau F, Schneid H, Zeghari N, Wall R, Bourgeois P. The IPSO study: ibuprofen, paracetamol study in osteoarthritis. A randomised comparative clinical study comparing the efficacy and safety of ibuprofen and paracetamol analgesic treatment of osteoarthritis of the knee or hip. Ann Rheum Dis. 2004;63:1028–1034. doi: 10.1136/ard.2003.011403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Doyle G, Furey S, Berlin R, Cooper S, Jayawardena S, Ashraf E, Baird L. Gastrointestinal safety and tolerance of ibuprofen at maximum over-the-counter dose. Aliment Pharmacol Ther. 1999;13:897–906. doi: 10.1046/j.1365-2036.1999.00539.x. [DOI] [PubMed] [Google Scholar]
- 50.Kellstein DE, Waksman JA, Furey SA, Binstok G, Cooper SA. The safety profile of nonprescription ibuprofen in multiple-dose use: a meta-analysis. J Clin Pharmacol. 1999;39:520–532. [PubMed] [Google Scholar]
- 51.Bombardier C, Laine L, Reicin A, Shapiro D, Burgos-Vargas R, Davis B, Day R, Ferraz MB, Hawkey CJ, Hochberg MC, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343:1520–1528, 2 p following 1528. doi: 10.1056/NEJM200011233432103. [DOI] [PubMed] [Google Scholar]
- 52.Bessone F. Non-steroidal anti-inflammatory drugs do not protect against coronary heart disease among people at high risk. Evid base Cardiovasc Med. 2002;6:62. [Google Scholar]
- 53.Rainsford KD. Introduction - The coxib controversies. Inflammopharmacology. 2005;13:331–341. doi: 10.1163/156856005774415628. [DOI] [PubMed] [Google Scholar]
- 54.FDA Requests Voluntarily Withdrawal of Valdecoxib (Bextra®) from US Markets. Available from: http://google2.fda.gov/search?q=cox+2&client=FDAgov&site=FDAgov&lr=&proxystylesheet=FDAgov&output=xml_no_dtd&getfields=*&x=17&y=14.
- 55.Laine L, White WB, Rostom A, Hochberg M. COX-2 selective inhibitors in the treatment of osteoarthritis. Semin Arthritis Rheum. 2008;38:165–187. doi: 10.1016/j.semarthrit.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 56.Boelsterli UA. Mechanisms of NSAID-induced hepatotoxicity: focus on nimesulide. Drug Saf. 2002;25:633–648. doi: 10.2165/00002018-200225090-00003. [DOI] [PubMed] [Google Scholar]
- 57.Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, Makuch R, Eisen G, Agrawal NM, Stenson WF, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: A randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA. 2000;284:1247–1255. doi: 10.1001/jama.284.10.1247. [DOI] [PubMed] [Google Scholar]
- 58.Schnitzer TJ, Burmester GR, Mysler E, Hochberg MC, Doherty M, Ehrsam E, Gitton X, Krammer G, Mellein B, Matchaba P, et al. Comparison of lumiracoxib with naproxen and ibuprofen in the Therapeutic Arthritis Research and Gastrointestinal Event Trial (TARGET), reduction in ulcer complications: randomised controlled trial. Lancet. 2004;364:665–674. doi: 10.1016/S0140-6736(04)16893-1. [DOI] [PubMed] [Google Scholar]
- 59.Medicines and Healthcare products Regulatory Authority. Lumiracoxib (Prexige): suspension of marketing authorisation. 2007. Accessed January 25, 2008. Available from: http://www.mhra.gov.uk/onlineservices/medicines/druganalysisprints/index.htm.
- 60.Techman A. Novartis Withdraws Lumiracoxib (Prexige®) in Australia in Response to Decision From Therapeutic Goods Administration to Cancel Registration. CIAOMed. August 14, 2007. Available from: http://www.mskreports.com/search_results.cfm?searchterm=cox-2. [Google Scholar]
- 61.Yan B, Leung Y, Urbanski SJ, Myers RP. Rofecoxib-induced hepatotoxicity: a forgotten complication of the coxibs. Can J Gastroenterol. 2006;20:351–355. doi: 10.1155/2006/356434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huster D, Schubert C, Berr F, Mössner J, Caca K. Rofecoxib-induced cholestatic hepatitis: treatment with molecular adsorbent recycling system (MARS) J Hepatol. 2002;37:413–414. doi: 10.1016/s0168-8278(02)00177-0. [DOI] [PubMed] [Google Scholar]
- 63.Papachristou GI, Demetris AJ, Rabinovitz M. Acute cholestatic hepatitis associated with long-term use of rofecoxib. Dig Dis Sci. 2004;49:459–461. doi: 10.1023/b:ddas.0000020503.92146.8b. [DOI] [PubMed] [Google Scholar]
- 64.Baraf HS, Fuentealba C, Greenwald M, Brzezicki J, O'Brien K, Soffer B, Polis A, Bird S, Kaur A, Curtis SP. Gastrointestinal side effects of etoricoxib in patients with osteoarthritis: results of the Etoricoxib versus Diclofenac Sodium Gastrointestinal Tolerability and Effectiveness (EDGE) trial. J Rheumatol. 2007;34:408–420. [PubMed] [Google Scholar]
- 65.Kang P, Dalvie D, Smith E, Renner M. Bioactivation of lumiracoxib by peroxidases and human liver microsomes: identification of multiple quinone imine intermediates and GSH adducts. Chem Res Toxicol. 2009;22:106–117. doi: 10.1021/tx8002356. [DOI] [PubMed] [Google Scholar]
- 66.Souto EO, Miyoshi H, Dubois RN, Gores GJ. Kupffer cell-derived cyclooxygenase-2 regulates hepatocyte Bcl-2 expression in choledocho-venous fistula rats. Am J Physiol Gastrointest Liver Physiol. 2001;280:G805–G811. doi: 10.1152/ajpgi.2001.280.5.G805. [DOI] [PubMed] [Google Scholar]
- 67.Farrell GC. Drug-induced liver disease. Edinburgh: Churchill Livingstone; 1994. [Google Scholar]
- 68.Lee SM, O'Brien CJ, Williams R, Whitaker S, Gould SR. Subacute hepatic necrosis induced by piroxicam. Br Med J (Clin Res Ed) 1986;293:540–541. doi: 10.1136/bmj.293.6546.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Planas R, De León R, Quer JC, Barranco C, Bruguera M, Gassull MA. Fatal submassive necrosis of the liver associated with piroxicam. Am J Gastroenterol. 1990;85:468–470. [PubMed] [Google Scholar]
- 70.Paterson D, Kerlin P, Walker N, Lynch S, Strong R. Piroxicam induced submassive necrosis of the liver. Gut. 1992;33:1436–1438. doi: 10.1136/gut.33.10.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Poniachik J, Guerrero J, Calderón P, Smok G, Morales A, Muñoz G, Venegas M. [Cholestatic hepatitis associated with piroxicam use. Case report] Rev Med Chil. 1998;126:548–552. [PubMed] [Google Scholar]
- 72.Hepps KS, Maliha GM, Estrada R, Goodgame RW. Severe cholestatic jaundice associated with piroxicam. Gastroenterology. 1991;101:1737–1740. doi: 10.1016/0016-5085(91)90417-j. [DOI] [PubMed] [Google Scholar]
- 73.Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs, antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002;22:169–183. doi: 10.1055/s-2002-30102. [DOI] [PubMed] [Google Scholar]
- 74.Caballeria E, Masso RM, Arago JV, Sanchis A. Piroxicam hepatotoxicity. Am J Gastroenterol. 1990;85:898–899. [PubMed] [Google Scholar]
- 75.Bennett A. Nimesulide: a well-established cyclo-oxygenase-2inhibitor with many other pharmacological properties relevantto inflammatory disease. In: Vane JR, Botting RM, eds , editors. Therapeutic roles of selective COX-2 inhibitors. London: William Harvey Press; 2001. pp. 524–540. [Google Scholar]
- 76.Bessone F, Fay F, Vorobioff J, Passamonti ME, Godoy A, Tanno H. Nimesulide hepatotoxicity: Evidence from six cases. Hepatology. 1997;26:483A. [Google Scholar]
- 77.Grignola JC, Arias L, Rondan M, Sola L, Bagnulo H. Hepatoxicity associated to nimesulide [Revision of five cases] Arch Med Int. 1998;20:13–18. [Google Scholar]
- 78.Selig J, Liberek C, Kondo Oestreicher M, Desmeules J, Stoller R. Nimesulide hepatotoxicity. Poster presented at the 6th Annual Meeting of the European Society of Pharmacovigilance - Budapest, September 28-29, 1998. [Google Scholar]
- 79.Romero Gómez M, Nevado Santos M, Fobelo MJ, Castro Fernández M. [Nimesulide acute hepatitis: description of 3 cases] Med Clin (Barc) 1999;113:357–358. [PubMed] [Google Scholar]
- 80.Ozgür O, Hacihasanoğlu A, Karti SS, Ovali E. Nimesulide-induced fulminant hepatitis. Turk J Gastroenterol. 2003;14:208–210. [PubMed] [Google Scholar]
- 81.Lewin S. Post-marketing surveillance of nimesulide suspension. Indian Pediatr. 2002;39:890–891; author reply 891-892. [PubMed] [Google Scholar]
- 82.Andrade RJ, Lucena MI, Fernández MC, González M. Fatal hepatitis associated with nimesulide. J Hepatol. 2000;32:174. doi: 10.1016/s0168-8278(00)80208-1. [DOI] [PubMed] [Google Scholar]
- 83.Pérez-Moreno J, Llerena Guerrero RM, Puertas Montenegro M, Jiménez Arjona MJ. [Nimesulide toxic hepatitis in pregnancy] Gastroenterol Hepatol. 2000;23:498–499. [PubMed] [Google Scholar]
- 84.Papaioannides D, Korantzopoulos P, Athanassiou E, Sinapidis D. Nimesulide-induced acute hepatotoxicity. Indian J Gastroenterol. 2003;22:239. [PubMed] [Google Scholar]
- 85.Tejos S, Torrejón N, Reyes H, Meneses M. [Bleeding gastric ulcers and acute hepatitis: 2 simultaneous adverse reactions due to nimesulide in a case] Rev Med Chil. 2000;128:1349–1353. [PubMed] [Google Scholar]
- 86.Dourakis SP, Sevastianos VA, Petraki K, Hadziyannis SJ. Nimesulide induced acute icteric hepatitis. Iatriki. 2001;79:275–278. [Google Scholar]
- 87.Rodrigo L, de Francisco R, Pérez-Pariente JM, Cadahia V, Tojo R, Rodriguez M, Lucena MI, Andrade RJ. Nimesulide-induced severe hemolytic anemia and acute liver failure leading to liver transplantation. Scand J Gastroenterol. 2002;37:1341–1343. doi: 10.1080/003655202761020650. [DOI] [PubMed] [Google Scholar]
- 88.Stadlmann S, Zoller H, Vogel W, Offner FA. COX-2 inhibitor (nimesulide) induced acute liver failure. Virchows Arch. 2002;440:553–555. doi: 10.1007/s00428-002-0612-2. [DOI] [PubMed] [Google Scholar]
- 89.Polimeni G, Salvo F, Cutroneo P, Morreale I, Patrizio Caputi A. Adverse reactions induced by NSAIDs and antibacterials: analysis of spontaneous reports from the Sicilian regional database. Drug Saf. 2006;29:449–459. doi: 10.2165/00002018-200629050-00006. [DOI] [PubMed] [Google Scholar]
- 90.Maciá MA, Carvajal A, del Pozo JG, Vera E, del Pino A. Hepatotoxicity associated with nimesulide: data from the Spanish Pharmacovigilance System. Clin Pharmacol Ther. 2002;72:596–597. [PubMed] [Google Scholar]
- 91.Press Release: European Medicines Evaluation Agency (EMEA) states that nimesulide is safe and effective. 2003. Accessed September 16, 2004. Available from: http://www.mahalo.com/nimesulide. [Google Scholar]
- 92.Conforti A, Leone R, Moretti U, Mozzo F, Velo G. Adverse drug reactions related to the use of NSAIDs with a focus on nimesulide: results of spontaneous reporting from a Northern Italian area. Drug Saf. 2001;24:1081–1090. doi: 10.2165/00002018-200124140-00006. [DOI] [PubMed] [Google Scholar]
- 93.Bessone F, Colombato L, Pasamonti ME, Godoy A, Vorobioff J, Tanno H. Nimesulide: clinical and histological evidences of severe hepatotoxicity. J Hepatol. 2001;34(Suppl 1):46. [Google Scholar]
- 94.Bessone F, Colombato L, Fassio E, Reggiardo MV, Vorobioff J, Tanno H. The spectrum of nimesulide-induced-hepatotoxicity. An overview. Anti-Inflamm & Anti-Allergy Agents Med Chem. 2010;9:355–365. [Google Scholar]
- 95.Bessone F, Tanno H. [Hepatotoxicity induced by non-steroidal anti-inflammatory drugs] Gastroenterol Hepatol. 2000;23:200–205. [PubMed] [Google Scholar]
- 96.Walker SL, Kennedy F, Niamh N, McCormick PA. Nimesulide associated fulminant hepatic failure. Pharmacoepidemiol Drug Saf. 2008;17:1108–1112. doi: 10.1002/pds.1665. [DOI] [PubMed] [Google Scholar]
- 97.Bjarnason I, Bissoli F, Conforti A, Maiden L, Moore N, Moretti U, Rainsford KD, Takeuchi K, Velo GP. Adverse reactions and their mechanisms from nimesulide. In: Rainsford KD, ed , editors. Nimesulide - Actions and Uses. Basel Switzerland: Birkhäuser Verlag; 2005. pp. 315–341. [Google Scholar]