Abstract
Purpose
The laparoscopic appendectomy has become popular for the treatment of acute appendicitis. A single-incision laparoscopic appendectomy offers better cosmesis. We present the results of single-incision laparoscopic appendectomies in our hospital as initial experience.
Methods
A single-incision laparoscopic appendectomy was performed in 75 patients at The Catholic University of Korea, Bucheon St. Mary's hospital. The operating time, operation type, hospital stay, surgical morbidities, and body mass index were compared.
Results
This retrospective study revealed equal operation times in both the suppurative and the perforated appendicitis group. There was an increase in the hospital stay in the perforated appendicitis group. The postoperative complication rate was 4%, and the median operation time was 58.55 ± 31.79 minutes.
Conclusion
The single-incision laparoscopic appendectomy was easy and safe procedure for treating acute appendicitis. There were no differences in degree of inflammation and body mass index.
Keywords: Laparoscopic surgery, Appendectomy
INTRODUCTION
Acute appendicitis is a common intra-abdominal inflammatory disease which requires emergency surgery, and a surgical appendectomy is the only treatment. Since the introduction of the laparoscopic appendectomy, it has become an alternative method of treatment to an open appendectomy because of less pain, less abdominal scarring, and quick recovery to daily life [1].
The location of the trocar in a laparoscopic appendectomy varies depending on the surgeon's preference. The three trocars (three incisions) were necessary in the past, but a method using a single incision was developed through the accumulation of experience and the development of instruments. The greatest benefit of single-incision laparoscopic surgery is the superior esthetic results after surgery. The single-incision Laparoscopic surgery has been used in nephrectomies [2], adrenalectomies [3], lap-band stomach surgery [4], and surgery for many other diseases. Also, there have been reports about single-incision laparoscopic appendectomy being useful based on precedents [5, 6]. However, there are limitations with surgical equipment and the movement of intra-abdominal equipment. The authors of this report analyzed 75 acute appendicitis cases where a laparoscopic appendectomy with a single incision had been performed and found the method to be feasible.
METHODS
Subject group
From October 2008 to June 2009, 75 patients at The Catholic University of Korea, Bucheon St. Mary's Hospital, who underwent a single-incision laparoscopic appendectomy for acute appendicitis, were retrospectively analyzed. Patients of the subject group had symptoms of appendicitis on physical examination and were diagnosed with appendicitis without abscess formation through abdominal CT or abdomen ultrasonography. Surgery was executed in most of the patients 12 hours after hospitalization. A single-incision appendectomy using laparoscopy was introduced to every patient regardless of the severity of inflammation, and although it was not the standard technique, a laparoscopic appendectomy was executed when the patient agreed to the method. Age, sex, body mass index (BMI), and preoperative white blood cell count were recorded before surgery, and anesthetic period and operation period were recorded during surgery. Surgical method, presence of complications after surgery, usage and amount of analgesics, and postoperative hospitalization period were additionally recorded.
Surgical method
First, third, and fifth finger tips (1 cm) of a surgical glove were cut, and three 5 mm long trocars (Applied Medical, Rancho Santa Margarita, CA, USA) were placed in the holes. The trocars were fixed with a boucle to prevent gas leakage, and single port equipment was ready. A long incision, 1.5-2.0 cm, was made on the patient's umbilicus, the white line was expanded to the left and to the right, the abdominal cavity was reached, and an incision was made. A lanceolate retractor (Alexis®, Applied Medical) was inserted through the incision to expand the incision. Then, a surgical glove was applied on the lanceolate retractor, CO2 gas was injected, abdominal pressure was maintained at 10-14 mmHg, a pneumoperitoneum was created, the operating table was tilted to the left by 30°, and the patient was ready for the operation. Surgery was done by inserting a 5 mm 0° laparoscopic camera through the trocar of the first finger and inserting surgical equipment through the other two trocars. After the location of the appendix had been confirmed, an ultrasonic scalpel (Harmonic Scalpel®, Ethicon Endo-Surgery Inc., Cincinnati, OH, USA) was used to cut the mesoappendix and appendicular artery. Then, the base of the appendix was clipped with an endo-loop, the portion of the appendix directly above the loop was held with the laparoscopic equipment and was incised to make sure there was no pus leak. The surgical globe and appendix was separated from the retractor. The surgical glove was once more covered in order to make a pneumoperitoneum, and the presence of hemorrhage was checked. In cases with perforating appendicitis, pus or abscess in the abdominal cavity was treated using an intra-abdominal drainage tube (Jackson-Pratt drain, 200 mL). During the postoperative period, diet and discharge were decided depending Severity of inflammation, similar to cases involving a normal laparoscopic appendectomy. When the patient expressed pain, a nonsteroidal analgesic (ketorolac tromethamine) was injected through the muscle.
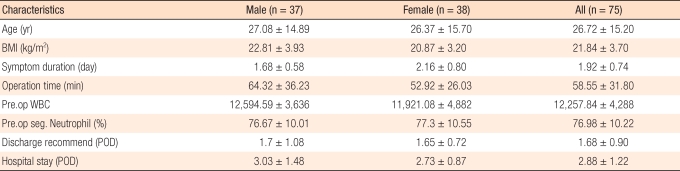
RESULTS
The total number of patients who underwent an appendectomy at The Catholic University of Korea, Bucheon St. Mary's Hospital, was 336. Fifty patients (14.9%) underwent an open appendectomy, and 286 patients (85.1%) underwent a laparoscopic appendectomy. The total number of patients who underwent a single-incision laparoscopic appendectomy was 75 (26.2%); 37 were males and 38 were females. The average BMI of the patients was 21.84 kg/m2, and the average duration of symptoms was 1.92 days. The operation time was defined as the time period from skin incision to suture and showed an average of 58.55 minutes. Discharge was suggested the day after the patient did not show nausea or vomiting after digesting semi-solid diet. In cases with a drainage tube, discharge was suggested after having normal diet and the drainage tube removed. The average suggested discharge was 1.68 days after surgery, and the actual length to patient discharge was 2.88 days (Table 1).
Table 1.
Characteristics of patients
BMI, body mass index; Pre.op, pre-operative; WBC, white blood cell; seg., segment; POD, post-operative day.
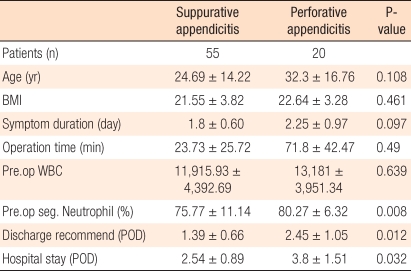
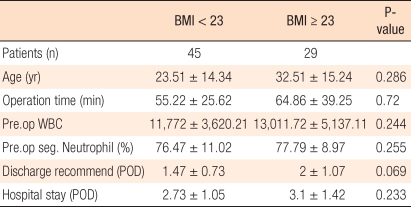
The severity of inflammation in appendicitis was categorized as suppurative or perforating appendicitis based on the biopsy results after the surgery. Among 75 patients, 55 of them had suppurative appendicitis, and 20 of them had perforating appendicitis. From the preoperative hematological test results, segmented neutrophil values were 75.77 in suppurative appendicitis and 80.27 in perforating appendicitis, a noticeable difference. Also, there were significant differences in the suggested day of discharge and the hospitalization period after surgery. There were no significant differences in other factors (Table 2). In addition, there were no significant differences in age, operation time, preoperative white blood cell or segmented neutrophil count, discharge suggestion day, and hospitalization period after dividing the total patient group with BMI 23 as the standard (Table 3).
Table 2.
Perioperative surgical outcomes in relation to inflammation
BMI, body mass index; Pre.op, pre-operative; WBC, white blood cell; seg., segment; POD, post-operative day.
Table 3.
Perioperative surgical outcomes in relation to BMI
BMI, body mass index; Pre.op, pre-operative; WBC, white blood cell; seg., segment; POD, post-operative day.
One out of 75 cases had to switch from a laparoscopic appendectomy to anopen appendectomy. The base of the appendix showed necrosis and suture of the intra-abdominal base failed twice. As a result, the base was sutured after switching to an open appendectomy.
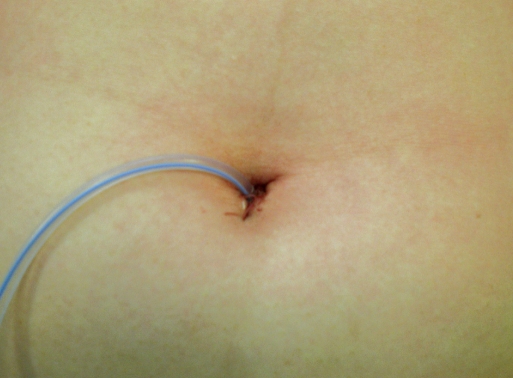
The postoperative wound was treated with a dressing, and it was covered with an umbilical fold (Fig. 1). In cases where a draining tube was installed, the tube was retracted through the wound (Fig. 2). Three out of 75 patients (4%) had postoperative complications. Two cases had a wound infection that was cured after follow-up observation at ambulatory care. One case had an intra-abdominal abscess that was treated with antibiotics.
Fig. 1.
Surgical wound after laparoscopic appendectomy with a single incision.
Fig. 2.
Jackson-Pratt drain was inserted via a single umbilical wound.
Nonsteroidal analgesic (ketrolac tromethamine) was used by injecting it through the muscle. The average number of analgesic injections was 0.64.
DISCUSSION
The purpose of this research was to establish the safety and the benefits, other than the aesthetic value, of a single-incision laparoscopic appendectomy using surgical gloves. Laparoscopic appendicitis has the benefits of small wound, less pain, less wound infection, and quick recovery to daily life. As a result, it is being used as a general treatment for acute appendicitis. Numerous reports on the development and popularization of laparoscopic appendectomy have been published, and much research has been done in order to reduce the number of incisions and the number of trocars for aesthetic values. In the early stages of development, Chouillard et al. [7] reported a appendectomy method of inserting two trocars in a single incision. However, by only using two trocars, it was difficult to approach the appendix and rotating or bending equipment was necessary in order to treat the meso-appendix. Also, Ates et al. [8] presented a method installing two trocars (11 mm and 5 mm), pulling the appendix, inserting a needle forcep from the outside, and suturing the meso-appendix to the abdominal wall. This method, however, has difficulties with pulling the appendix located behind the cecum. In order to resolve these challenges, numerous pieces of equipment have been introduced to enable numerous trocars to be inserted through a single incision. Merchant et al. [9] came out with a method of inserting numerous trocars by using a Gelport, and there is equipment on the market, such as Unix-X™ (Pnavel Systems, Brooklyn, NY, USA) [10], the R-port™ (Advanced Surgical Concepts, Wicklow, Ireland) [11], and the SILS™ Port Multiple Instrument Access Port (Covidien, Mansfield, MA, USA). In this research, these types of equipment could not be used because they were not available on the market at that time. However, similar to recently developed equipment, a method using a surgical glove enabled two trocars, other than the laparoscopic camera, to be inserted. This made it easier to approach the appendix located behind the cecum. In addition, the fact that the other fingers of the glove, those without trocars inserted, could be used when additional equipment was necessary.
In cases with perforating appendicitis, the operation time was increased by intra-abdominal hemorrhage or by an abscess caused by adhesion, and washing and installation of a drainage tube was necessary. However, unlike the results from previous research, there were no significant operation-time difference between suppurative appendicitis and perforating appendicitis. Large gauze and a suction tube were easily inserted through the incision, which made the cleaning process easier.
Fraser et al. [12] reported that the incidence of intra-abdominal abscess was directly proportional to the BMI value in juvenile patients with perforating appendicitis. Also, according to Sadr et al. [13], obese patient with suppurative appendicitis had a greater chance to have complications. This research also analyzed how the BMI value affected the operation time and the hospitalization period. In 1993, the World Health Organization (WHO) defined obesity as a BMI greater than or equal to 30 kg/m2 and overweight as a BMI greater than or equal to 25 kg/m2. In 2004, a research paper reported that a BMI greater than or equal to 23 kg/m2 in Asians was defined as overweight, and the rates of diabetes, cardiovascular diseases, and death were higher in those patients. Accordingly, this research set 23 kg/m2 as the standard value of overweight. Different from other research results, there was no significance in the effects of BMI on the operation time, the hospitalization period, and the complications.
The average operation time was 58.55 ± 31.79 minutes, which was 7.55 to 20.55 minutes longer than the time reported for previous research on a single-incision appendectomy [5-8, 10]. The cause of this increase is thought to be the smallness of the incision, which increased the time to secure single trocar insertion, increased equipment collision, and increased the time to restore the abdominal and muscular cavities.
A single-incision laparoscopic appendectomy is widely practiced in order to minimize scarring. Surgeons skilled in performing an appendectomy were able to execute this method without major complications in all the cases except the ones with an abscess in the abdominal cavity, and postoperative aesthetic benefits were found. In the future, more research and prospective studies comparing a single-incision laparoscopic appendectomy to a regular laparoscopic appendectomy must be done.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Pedersen AG, Petersen OB, Wara P, Ronning H, Qvist N, Laurberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg. 2001;88:200–205. doi: 10.1046/j.1365-2168.2001.01652.x. [DOI] [PubMed] [Google Scholar]
- 2.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–1204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 3.Walz MK, Groeben H, Alesina PF. Single-access retroperitoneoscopic adrenalectomy (SARA) versus conventional retroperitoneoscopic adrenalectomy (CORA): a case-control study. World J Surg. 2010;34:1386–1390. doi: 10.1007/s00268-010-0494-4. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira J, McGill K, Binenbaum S, Forrester G. Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc. 2009;23:1409–1414. doi: 10.1007/s00464-009-0411-9. [DOI] [PubMed] [Google Scholar]
- 5.Kim JW, Park JS, Chang IT, Choi YS, Song HJ, Kim BG. The initial experience with a single incision laparoscopic appendectomy. J Korean Soc Coloproctol. 2009;25:312–317. [Google Scholar]
- 6.Lee YS, Kim JH, Moon EJ, Kim JJ, Lee KH, Oh SJ, et al. Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients. Surg Laparosc Endosc Percutan Tech. 2009;19:493–496. doi: 10.1097/SLE.0b013e3181c15493. [DOI] [PubMed] [Google Scholar]
- 7.Chouillard E, Dache A, Torcivia A, Helmy N, Ruseykin I, Gumbs A. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010;24:1861–1865. doi: 10.1007/s00464-009-0860-1. [DOI] [PubMed] [Google Scholar]
- 8.Ates O, Hakguder G, Olguner M, Akgur FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007;42:1071–1074. doi: 10.1016/j.jpedsurg.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 9.Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS) J Gastrointest Surg. 2009;13:159–162. doi: 10.1007/s11605-008-0737-y. [DOI] [PubMed] [Google Scholar]
- 10.Vidal O, Valentini M, Ginesta C, Marti J, Espert JJ, Benarroch G, et al. Laparoendoscopic single-site surgery appendectomy. Surg Endosc. 2010;24:686–691. doi: 10.1007/s00464-009-0661-6. [DOI] [PubMed] [Google Scholar]
- 11.Rane A, Rao P, Rao P. Clinical evaluation of a novel laparoscopic port (R-PORTTM) in urology and evolution of the single laparoscopic port procedure (SLIPP) and one port umbilical surgery (OPUS) Eur Urol Suppl. 2008;7:193. [Google Scholar]
- 12.Fraser JD, Aguayo P, Sharp SW, Snyder CL, Holcomb GW, 3rd, et al. Physiologic predictors of postoperative abscess in children with perforated appendicitis: subset analysis from a prospective randomized trial. Surgery. 2010;147:729–732. doi: 10.1016/j.surg.2009.10.057. [DOI] [PubMed] [Google Scholar]
- 13.Sadr Azodi O, Lindstrom D, Adami J, Bellocco R, Linder S, Wladis A. Impact of body mass index and tobacco smoking on outcome after open appendicectomy. Br J Surg. 2008;95:751–757. doi: 10.1002/bjs.6079. [DOI] [PubMed] [Google Scholar]