Abstract
Despite the assumption that health care providers work synergistically in practice, professions have tended to be more exclusive than inclusive when it comes to educating students in a collaborative approach to interdisciplinary evidence-based practice (EBP). This article explores the state of academic and clinical training regarding interdisciplinary EBP, describes efforts to foster interdisciplinary EBP, and suggests strategies to accelerate the translation of EBP across disciplines. Moving from silos to synergy in interdisciplinary EBP will require a paradigm shift. Changes can be leveraged professionally and politically using national initiatives currently in place on improving quality and health care reform.
An exponentially expanding evidence base, complex patient needs and health systems, and lack of preparation to work in interdisciplinary teams have stymied the ability of health care providers to deliver high quality care.1 Evidence suggests that teams of people from different disciplines who work together can improve work processes and patient care outcomes. 2, 3 Multiple disciplines are invariably involved in solving complex patient problems, making knowledge sharing across the disciplines foundational to effective care. 4 To narrow the gap between knowledge generation and knowledge translation, providers from all disciplines must be able to collaborate effectively. 5
Recommendations by the Institute of Medicine (IOM) focus on the need for systematic reviews to guide practice, skills to translate evidence into practice, and interdisciplinary education. The IOM has endorsed the need to promote rigorous systematic reviews and development of clinical practice guidelines as a health care priority.6 The preferred future includes health care providers who are educated to deliver patient-centered care in interprofessional teams proficient in EBP, quality improvement, and informatics solutions. 1 In addition, interdisciplinary continuing education (CE) should focus health care team members on the shared goal of improving patient outcomes. 7 The IOM suggests a national interprofessional institute to develop and monitor the financing, regulation, and evaluation of continuing education. 7 Providing a common educational base in both CE and the academic curriculum is a good first step in enhancing interdisciplinary EBP efforts.
The terms multidisciplinary, interdisciplinary, and transdisciplinary are often used to describe the contribution of multiple disciplines, but actually describes a continuum of involvement of disciplines. 8 Multidisciplinarity represents the basic efforts of multiple disciplines working together to solve a problem without challenging disciplinary boundaries. 8 Interdisciplinarity, the focus of this paper, is defined as the coordinated and coherent linkages between disciplines resulting in reciprocal interactions that overlap disciplinary boundaries, generating new common methods, knowledge, or perspectives8. Transdisciplinarity is the most advanced level, and includes scientist, nonscientist, and other stakeholders who go beyond or transcend the disciplinary boundaries through role release and expansion. 8 In this paper, the terms “interprofessional” and “interdisciplinary” will be used interchangeably, based on the term used in the related reference. The purpose of this article is to explore the state of academic and clinical training regarding interdisciplinary EBP, describe interdisciplinary efforts to foster EBP, and suggest strategies to accelerate the translation of EBP across disciplines.
Interdisciplinary Education Initiatives
Movement toward interdisciplinary education is already under way, being driven by the same inevitability that drives interdisciplinary research. The reality is that different professions are trained to address different parts of a patient’s health needs. Bringing the professions together to each do what they uniquely do well does more for the patient than having only one profession involved. For this reason, the Health Resources and Services Administration (HRSA), as well as the World Health Organization (WHO), have launched initiatives to improve interdisciplinary health care.
HRSA has established an Advisory Committee on Interdisciplinary, Community-Based Linkages to advise and provide recommendations to the Secretary and Congress on advancing the cause of interprofessional education. Some of the recommendations they are considering include establishing a National Center of Excellence, improving alignment in accreditation requirements, engaging accreditation agencies in facilitating interprofessional approaches in the health care professions, convening a summit of the major health care profession accreditation agencies to compare guidelines and standards and to discuss opportunities for facilitating interprofessional approaches to education. 9
There are also international efforts to advance interprofessional education. Based on the evidence that interprofessional education enhances collaborative practice, and collaborative practice results in better outcomes for patients, WHO has developed a Framework for Action on Interprofessional Education and Collaborative Practice. 10 The action agenda includes: developing supportive management practices; changing the culture and attitudes of health care workers; identifying and supporting champions; revising curricula; and enacting legislation to eliminate barriers to collaborative practice. 10
Interdisciplinary EBP Education
Despite some successes in educating the different disciplines collaboratively 11, the degree of interdisciplinary education at present is insufficient and sporadic. Within the nursing curriculum, the content for teamwork is present, but the evidence for education of disciplines together is sparse. In a survey of its member schools, the American Association of Colleges of Nursing (AACN) found high levels of teamwork and collaboration (82%) and EBP (73%) threaded throughout the curriculum. 12
There is some indication however, that other disciplines are encountering barriers to interprofessional education. Leaders at seven academic health centers report that implementation of interdisciplinary education in dentistry is difficult because of curricular demands (crowded curriculum would require that interprofessional education replace content instead of being added on), lack of support from both faculty and administration to develop and integrate new courses and experiences, and financial constraints. 13 The group suggested specific areas for incorporating interprofessional coursework, including ethics, communication skills, evidence-based practice, and informatics use. 13 It will be important to have clinical and didactic experiences, since both may improve short-term learners’ knowledge and attitudes about interdisciplinary care. 14
When considering nursing’s readiness to engage in interdisciplinary EBP, faculty development needs need to be addressed. In the AACN survey, 52% of respondents cited faculty experience with EBP as an area in which they had only intermediate/some comfort and 11% stated they believed faculty were novices in or uncomfortable with the EBP content. 12 When asked about their satisfaction with students’ initial competencies in EBP, respondents reported an overall score of 3.7 on a scale of 1-5.12 Comparable data about teamwork and EBP is not available for other health professions.
Including EBP in interprofessional education makes sense since the process and methodology for systematic review, generation of practice recommendations, and translation are a shared science. The need to develop clinical guidelines may help focus some of these interdisciplinary efforts. 15 For example, interdisciplinary teams could conduct an evidence review based on a common question, and translate recommendations in a clinical setting as a practicum experience.
The evidence reviewed indicates a gap between actual and required skills, knowledge, and abilities in EBP for both faculty members and graduating nurses. There are, however, some models of interdisciplinary EBP initiatives that can inform the way forward.
Examples of Interdisciplinary EBP
There are three examples of interdisciplinary in EBP that can serve as case studies to inform future efforts. Two are knowledge synthesizers: the Cochrane Collaboration 17 and U. S. Preventive Services Task Force (USPSTF). 16 The third is an interdisciplinary group that includes the authors, which has developed and implemented an interdisciplinary conceptual model, process, and educational resources: Evidence Based Behavioral Practice (EBBP). 18 EBBP’s work is intended to provide training and resources for all professions that enhances the translation of evidence to practice. These three examples will be described.
Cochrane Collaboration and U. S. Preventive Services Task Force: Evidence synthesizers
The Cochrane Collaboration and USPSTF are part of the EBP infrastructure that synthesizes research into usable recommendations. Both entities have helped pave the way toward interdisciplinary EBP by engaging multiple disciplines. The review teams include physicians, nurses, psychologists, and other professional representatives. Team members use standard methodological approaches. Graduate education for all disciplines should prepare health professionals to be knowledge utilizers of systematic reviews. At the doctoral level, graduates should be prepared to serve on teams that generate systematic reviews.
The Cochrane Collaboration
The Cochrane Collaboration was formed in 1993 to inform health care decisions by creating systematic reviews related to prevention, treatment, rehabilitation interventions, or testing. 17 To date, more than 28,000 people from more than 100 countries have contributed to The Cochrane Collaboration’s more than 4,000 systematic reviews. 20 The process for question generation, search strategies, evidence review, critical appraisal processes, rating, and grading of evidence considering bias and random error is specified by experts at The Cochrane Collaboration with the goal of producing reliable recommendations. 17 A handbook describing the process is publically available. 21
U. S. Preventive Services Task Force (USPSTF)
The USPSTF is an interdisciplinary panel of primary care experts that extrapolates from systematic reviews for the utility to preventive services and develops guidelines. 16 The reviews that the USPSTF considers are conducted by evidence-based practice centers (EPCs), and both the USPSTF and the EPCs are funded through the Agency for Healthcare Research and Quality (AHRQ). After analyzing the EPCs’ systematic reviews, the USPSTF makes recommendations about which preventive services should be included in primary care. 16 The question generation, evidence review, synthesis, and recommendations follow established procedures. Results are widely distributed and publically available in a Guide to Clinical Preventive Services. 19 An EPC’s systematic review followed by analysis and formulation of guidelines recommendations by USPSTF are links in a chain that can result in evidence-based practice policy. As an example, the recent Patient Affordability and Protection Act now requires that all preventive services designated by the USPSTF as having A or B level evidence must be covered without co-pays by large insurers.
The USPSTF synthesizes and disseminates evidence and is a source to guide standards of preventive care – but it does not focus on interdisciplinary adoption of evidence. As a standard of practice in primary and community care, educators use USPSTF recommendations to teach nurses best clinical practices.
Evidence Based Behavioral Practice (EBBP)
In 2006, the National Institutes of Health (NIH) Office of Behavioral and Social Science Research (OBSSR) commissioned the second author to undertake a project to harmonize the EBP approach to behavioral health interventions and support communication and collaboration across health disciplines. The resulting interprofessional Council for Training in Evidence-Based Behavioral Practice and its scientific and practitioner advisory boards include EBP experts from medicine, nursing, psychology, social work, public health, and library sciences (www.ebbp.org). The group collaborated to create a trans-disciplinary model of EBP. 18
The EBBP model, process, and resources are discussed here because they are purposely interdisciplinary and have been implemented successfully in both academic and practice settings. Each discipline represented in the Council brought its own profession-specific perspectives, language, and resource base to the development of the model, process, and competencies for health care providers. 22 The Council implements objectives of the EBBP project with input from a Scientific Advisory Board and expert consultants.
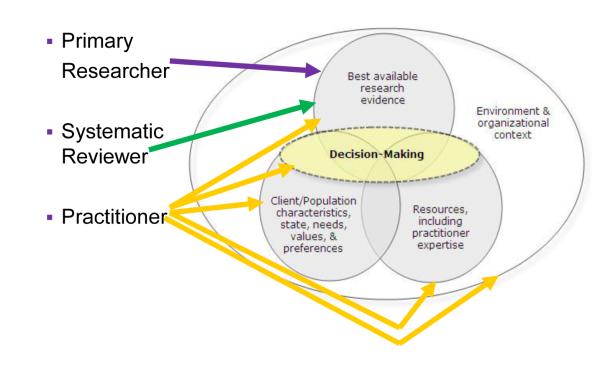
The EBBP conceptual model (see Figure 1) uses an ecological framework as its foundation, and reflects shared decision-making among the practitioner, patient, and other affected stakeholders. 18 This ecological framework posits that in order to promote change, one must influence multiple levels that include interpersonal, organizational, community, and public policy. The model was developed after review of existing EBP conceptual models from each discipline that represent how evidence-based decisions are made in practice. Details of the development of the conceptual model are published elsewhere. 18
Figure 1. The Trans-disciplinary Model of Evidence-based Practice (EBP) and Health Professionals’ Roles in EBP.
Source for Model: Satterfield, J. et al. 18
Figure 1 uses the EBBP conceptual model to illustrate the role of clinicians, evidence synthesizers, and researchers in evidence-based decision making in the EBBP model. Primary researchers generate evidence for practice. Those that conduct systematic review synthesize evidence for practice (e.g., Cochrane) and those that generate recommendations use systematic reviews (e.g., USPSTF). Health care practitioners incorporate all components of the model, including the best available research evidence (i.e., research studies and systematic reviews), patient characteristics (condition, needs, values, and preferences), resources (i.e., provider expertise) into health care decisions within a specific environment and organizational context. 18
Clinical decisions are based on the best available research evidence (randomized controlled trials, quasi-experimental and non-experimental or systematic reviews of research) practitioner expertise, patient (client)/population characteristics/ needs, values, and preferences, within a specific organizational context). 18, 23 Decision-making is the core concept that ties the other three together, and all action transpires within an organizational context.
In addition to a conceptual model, EBP entails a five-step process to synthesize research evidence by all the professions delivering care as a team: 1) Ask, 2) Acquire, 3) Appraise, 4) Apply, and 5) Analyze and Adjust. 23 Table 1 describes the interprofessional provider competencies developed to clearly define the requisite provider skills and knowledge competencies necessary to implement the model and improve overall care. 24
Table 1.
Skills and Competencies for Evidence-based Behavioral Practice
| Skills | Competencies |
|---|---|
| Expertise | Performing the evidence-based practice process, assessment, communication/collaboration, and engagement/ intervention. |
| EBP process | Formulating answerable practical questions, acquiring and appraising relevant evidence, applying the evidence through shared decision-making that integrates patient characteristics and resource considerations, analyzing outcomes, and adjusting as appropriate. |
| Assessment | Appraisal of care recipients as well as appraising one’s level of expertise to implement and evaluate the outcome of a needed health procedure. |
| Communication and collaboration |
Convey information clearly and listen, observe, and adjust to achieve understanding and agreement on a course of action. |
| Engagement and intervention |
Proficiency at motivating interest, constructive involvement, and positive change from stakeholders who may be affected by health decisions. |
The EBBP website (www.ebbp.org) includes tools to help educators teach EBP and disseminate information about concepts and methods used in EBP. 25 Learning materials are also available to help providers acquire skills to perform the EBP process. Since its launch November 2008, EBBP’s website has attracted 20,775 visits (13,096 unique visitors) from 111 countries.
Five training modules are publically available to educators who teach graduate level EBP courses and can be used by any health professions educator. The modules include the EBP process, search for evidence, systematic review, randomized controlled trials, and critical appraisal of research methods. The intended audience is interprofessional and includes both researchers and practitioners. These interactive EBBP learning modules have been incorporated into graduate and post-graduate training of health professionals in the U. S., Canada, and Australia. According to the registration database, physicians, nurses, social workers, psychologists, and public health workers have all completed the modules. Comparison of pre- and post-test scores shows significant improvements in attitudes, skills, and knowledge about EBP. Qualitative evaluations have been favorable, with 80% indicating that the modules met or exceeded their expectations.
Evaluation of the model, process and tools has not focused on assessment of actual skills learned and implemented to date. Three Council members are conducting a randomized controlled trial funded by Robert Wood Johnson Foundation in 10 acute care hospitals to test the effect of the EBBP model and process on nurse evidence adoption, knowledge and skills. An important next step for the Council is to develop an implementation resource or tool kit to assist organizations in the implementation of evidence in practice settings.
Council members have also embarked on training and education initiatives for each discipline. Specific efforts to date have focused on psychology (Society of Behavioral Medicine) and medicine (Society of General Internal Medicine), with future continuing education planned for nursing, public health, and social work. Continuing education (CE) is important in parallel to academic infusion. Continuing education credit is available online on the EBBP website through the APA Office of Continuing Education in Psychology, Accreditation Council for Continuing Medical Education (ACCME), the American Nurses Credentialing Center (ANCC).
EBBP, Cochrane, and the USPSTF are all examples of interdisciplinary models with associated processes that support evidence-based shared decision-making on interprofessional health care teams. The steps in EBP go beyond asking a question and acquiring and appraising evidence. A major activity of interdisciplinary practice is in the application and evaluation of evidence in the practice setting. With few exceptions, however, the level of interdisciplinary activity is far too low within academic and clinical settings. What will it take to accelerate such activities?
Strategies to Leverage Nursing Engagement in Interdisciplinary EBP
Increasing engagement in interdisciplinary EBP will require a new way of “doing business,” with major shifts in philosophy within disciplines. Paradigm shifts occur through changed circumstances, making the old ways incommensurate with the new. 26 This shift is not unattainable—it’s already happening. Changes will need to be leveraged both professionally and politically within the framework of national initiatives currently in place.
Nursing Faculty
The first step will need to focus on interdisciplinary education. Academic nursing will need to fully engage and align strategically with local, national, and global efforts. Nursing faculty can support the transition to interdisciplinary EBP by taking action locally, at the state level, and nationally. At the local level, faculty should: 1) evaluate the interdisciplinary EBP curriculum; 2) assess the extent to which there are interdisciplinary practice and research teams within the academic setting; and 3) determine if there are opportunities to improve relationships on campus.
The curriculum review may indicate that changes need to be made, with accompanying faculty development in knowledge, skills, and attitudes. Faculty will need to work within their academic settings to identify courses that can be offered to interdisciplinary students. A good place to start with interprofessional coursework is ethics, communication skills, evidence-based practice, and informatics use. 13
A faculty development plan will need to be implemented. Faculty development can be accomplished through mentorship or co-teaching classes with EBP experts, or formal education. The learning objectives, outcomes, and competencies expected for each discipline will need to be standardized before implementing an interdisciplinary curriculum. Teaching strategies can be selected by the interdisciplinary faculty to include small group case studies, attending meetings with an interdisciplinary audience, broadening subscriptions and required reading in interdisciplinary journals, and engaging in policy activities. 27
The EBBP model can serve as a framework for curriculum: research evidence, patient preferences, resources, context, and decision making. Research evidence includes the EBP process: asking an important question; searching for evidence; critical appraisal of evidence design and quality; synthesis of evidence quality, quantity, and consistency; practice recommendations; translation; and evaluation. Patient preferences content should include how to incorporate evidence with patient characteristics, values, and beliefs. Resources should include content on assessment of provider expertise and available options for care of the patient. Context should include the influences of the organization’s policies and procedures) and state or federal laws and regulations on decision making. Decision should include the incorporation of research evidence, patient preferences, resources, and context on the choice of health care treatment for the patient and use of decision making tools for providers and patients.
At the state level, faculty can partner with other disciplines for specific initiatives, plan state-level training in EBP with other disciplines, and incorporate expectations for interdisciplinary practice in state policies. Faculty members should seek appointments to state committees through their university or professional associations to represent the perspectives, contributions, and value added by nursing in addressing common health care needs.
At the national level, faculty should be engaged in interdisciplinary national guideline formulation, assuring that the nursing perspective is represented. For example, faculty should consider membership on a Cochran workgroup appropriate for their expertise or volunteering for evidence synthesis initiatives or guideline formulation. This is an excellent way to bring students into interdisciplinary training experiences. It will be important for faculty to stay current with the recommendations that emerge from the HRSA and WHO initiatives on interdisciplinary education.
Clinicians
Clinicians also have a role in promoting interdisciplinary EBP. At the local level, clinicians will need to develop skills in EBP so that they can enable its spread throughout the nursing department or practice. Clinicians in all settings (acute, long term, primary care) will need to be prepared to serve on interdisciplinary teams that review evidence for practice and recommend practice changes that are incorporated into policies. One strategy is to partner with academic institutions so that teams can benefit from both practice expertise and methodological expertise.
Leaders (both nursing and other disciplines) in clinical settings will need to set the expectation that EBP initiatives are interdisciplinary. Recommendations from WHO on interdisciplinary practice can guide specific strategies to improve supportive management practices, focusing on culture changes that embrace interdisciplinary EBP. 10 Identifying and supporting champions will begin to prepare the organization for the change. 10 Assessment of the environment and creating strategies to eliminate barriers to collaborative practice will enhance success. 10
At the national level, clinicians will need to be represented on interdisciplinary initiatives for guideline translation. Nurses are well prepared to construct plans that enable adoption of evidence in practice, having firsthand experience on health care processes and the roles of each discipline in system implementation. Translation of evidence to practice is an area where clinical nurses can excel.
Researchers
Researchers will need to test models of interdisciplinary EBP, develop metrics to represent high quality interdisciplinary efforts, and evaluate outcomes in clinical settings. As interdisciplinary EBP gains momentum, interventions that promote shared decision making among disciplines will need to be evaluated in terms of the benefits (quality care for patients) and cost effectiveness. 28 A careful assessment of shared decision making models can reveal under what circumstances (i.e., patients and setting) interdisciplinary EBP is effective, and under what circumstances there are no quality or cost benefits. Important patient outcomes will require evaluation as interdisciplinary teams apply evidence. Electronic records will need to capture standard process and outcome measures representative of interdisciplinary EBP.
If interdisciplinary EBP becomes a standard, metrics will need to be developed to describe when it is or is not present. These metrics will go beyond the count of disciplines involved, to better capture the full engagement of all team members instead of summarizing each member’s unique contribution individually. Changes in pay for performance will need to shift from individual providers to interdisciplinary groups responsible for the care of patients and populations.
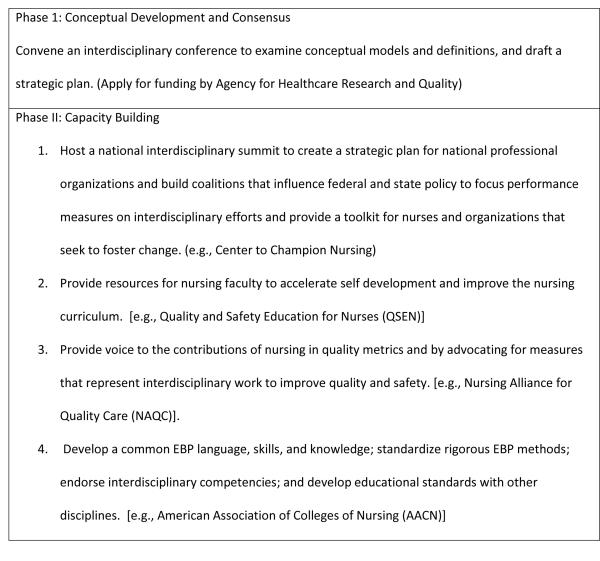
Moving Interdisciplinary Education Forward: The Big Picture
To move interdisciplinary EBP forward, current recommendations from interdisciplinary groups can be applied to nursing. The first phase consists of conceptual development and consensus. The second phase then moves to capacity building.
Conceptual Development and Consensus
Conceptual development is the fundamental first step in advancing interdisciplinary EBP. 9 A consensus conference should be held with health care professional association leaders, policy makers, and quality metric developers. The conference goal should be to attain consensus on three-year goals and draft a business plan with objectives, timelines, responsibilities, and tactics. Grant funding should be sought through AHRQ to support the conference. The deliverable from the conference would be a consensus document or white paper to guide capacity building for the next three to five years.
Capacity Building
After conceptual development and consensus, capacity building for interdisciplinarity in EBP can begin. Academic curricula will need to be revised to incorporate interdisciplinary EBP. Legislation will be needed to eliminate barriers to collaborative practice. 10 Accreditation requirements will need to be aligned with interdisciplinary EBP. 9 Financial incentives, such as pay for performance, academic and practice standards, and quality and safety metrics will need to reinforce interdisciplinary efforts instead of individual providers.
Fortunately, nursing has initiatives in place that are well positioned to leverage nursing’s engagement. These include the Center to Champion Nursing in America, Quality and Safety Education in Nursing, Nursing Alliance for Quality Care, and AACN. Each will be briefly described in terms of their role in fostering interdisciplinary EBP.
Center to Champion Nursing in America
The Center is a consumer-driven initiative intended to enable nursing’s positive impact on health care, which is supported by AARP, the AARP Foundation, and the Robert Wood Johnson Foundation. Among its goals is to enhance the influence of nurses in high levels of health care, policy, business, and community decision making. 29 Center strategies include building coalitions, hosting national summits and forums, technical assistance for grassroots efforts, and acting as an information resource. 29 Potential strategies related to interdisciplinary EBP include hosting a national summit to create a strategic plan for national professional organizations, build coalitions that influence federal and state policy to focus performance measures on interdisciplinary efforts, and provide a toolkit for nurses and organizations that seek to foster change.
Quality and Safety Education for Nurses (QSEN)
Quality and Safety Education for Nurses (QSEN), funded by the Robert Wood Johnson Foundation (RWJF), prepares nurses with the knowledge, skills, and attitudes for health care quality and safety improvements in the workplace setting. 30 There are resources for undergraduate and graduate curricula and training available for faculty. Teamwork and collaboration are already a core component, making the QSEN model an ideal resource for nursing faculty to accelerate self development and improve the nursing curriculum.
Nursing Alliance for Quality Care (NAQC)
NAQC is a partnership of nursing organizations, consumers, and stakeholder to foster high quality, safe, consumer-centered care. 31 A primary goal is to ensure that policy makers recognize the contributions of nursing. NAQC can play a role in promoting interdisciplinarity by providing voice to the contributions of nursing in quality metrics and by advocating for measures that represent trans-disciplinary work to improve quality and safety.
American Association of Colleges of Nursing (AACN)
As leaders in quality standards for nursing education, AACN has a major role in developing a common EBP language, skills, and knowledge; rigorous EBP methods; interdisciplinary competencies; and educational standards. Standardized interdisciplinary skills, knowledge, and attitudes incorporated into academic outcome standards will go a long way to prepare teams to approach common problems effectively. Standards will then be incorporated into the nursing curriculum to include strong EBP methods for decision making in clinical and academic arenas.
An issue for nursing is the multiple entry level degrees (associate, bachelors or master’s) with a corresponding different emphasis on EBP and related skills and competency. Nurses from all educational backgrounds will be required to work on teams in the local setting. The high proportion of associate degree nurses in some settings will require that linkages be forged with academic and professional organizations to provide evidence, resources, and consultation to assist with local decision making. AACN can also work to foster networks for nurses to gain access to mentors who can work with them to develop needed skills or link them to experts that can work on their behalf.
Challenges and Opportunities
As health care providers move toward interdisciplinary EBP, nursing will encounter resistance and challenges. Many suggestions for increasing interdisciplinary efforts already exist, but they are not well received, embraced, or adopted. The challenge is that the professions need to learn to communicate, understand each others’ language, ideally develop a shared language, and learn to coordinate their actions as a team. As we move forward, power differentials typically encountered in organizational life will proliferate, requiring support from national and organizational leadership to set expectations for the various disciplines to work together.
If patient centered care is a real goal, and better outcomes result from interdisciplinary practice, then the only rational choice is for multiple disciplines to work together. We will need to deal with the challenges and construct a plan to include who or how will we pay for this work. If a national priority for all health care professions is to promote rigorous systematic review and the development of clinical practice guidelines to improve health care 6, then all health care providers will need to be fully engaged in the synthesis and translation of evidence to practice to make these goals a reality. Efforts must be accelerated at both the macro and micro level to enable interdisciplinarity in both the knowledge synthesis and knowledge translation.
Conclusion
Despite the philosophy that we can do more together than separately, health care professions have tended to be more exclusive than inclusive when it comes to educating in a collaborative approach to interdisciplinary EBP interdisciplinary EBP. Interdisciplinary EBP is still in its infancy, with many single discipline efforts, models, and resources. Interprofessional collaboration is foundational for improved patient care. Provider and system attributes affect the success of interdisciplinary collaboration. Consequently, engaging multiple disciplines in EBP becomes critically important.
Although all health professions share a common focus on patient care, the disciplines are rooted in different professional training backgrounds and hold distinct professional perspectives. This would suggest that the academic preparation of our health care work force offers an ideal arena in which to infuse a harmonized approach to evidence-based practice. Further progress will require efforts by nurses in academia, practice, and research.
To achieve the vision for interdisciplinary EBP, both conceptual development and capacity building need to occur. Further representation on evidence synthesis groups such as the USPSTF and Cochrane Collaboration will be important. Using interdisciplinary models and resources such as EBBP will help faculty build skills and to construct an interdisciplinary curriculum. Nursing will need to accelerate efforts to engage both professionally and politically, to leverage a shift from silos to synergy in interdisciplinary EBP.
Figure 2.
Initial Strategies to Accelerate Interdisciplinary EBP
Acknowledgments
Preparation of this paper was supported in part by an award from the National Institutes of Health, Office of Behavioral and Social Sciences Research (N01-LM-6-3512) to Dr. Spring to support the development of Resources for Training in Evidence-based Behavioral Practice. The views expressed are solely the responsibility of the authors and do not necessarily reflect the official views of their employers or sponsors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Robin P. Newhouse, Department of Organizational Systems and Adult Health, University of Maryland School of Nursing, Baltimore, MD.
Dr. Bonnie Spring, Department of Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL.
References
- 1.Committee on the Health Professions Education Summit . Health professions education: A bridge to quality. National Academy of Sciences; Washington, D.C.: 2003. [Google Scholar]
- 2.Barrett J, Curran V, Glynn L, Goodwin M. CHSRF Synthesis: Interprofessional collaboration and quality primary healthcare. Canadian Health Services Research Foundation; Ottawa, Ontario: 2007. [Google Scholar]
- 3.Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: Effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009 Jul 8;(3) doi: 10.1002/14651858.CD000072.pub2. (3):CD000072. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell R, Parker V, Giles M, White N. Toward realizing the potential of diversity in composition of interprofessional health care teams: An examination of the cognitive and psychosocial dynamics of interprofessional collaboration. Med Care Res Rev. 2009 Jul 15; doi: 10.1177/1077558709338478. [DOI] [PubMed] [Google Scholar]
- 5.Davis D, Evans M, Jadad A, Perrier L, Rath D, Ryan D, et al. The case for knowledge translation: Shortening the journey from evidence to effect. BMJ. 2003 Jul 5;327(7405):33–5. doi: 10.1136/bmj.327.7405.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee on Reviewing Evidence to Identify Highly Effective Clinical Services, Board on Health Care Services . Knowing what works in health care: A roadmap for the nation. The National Academies Press; Washington, D.C.: [Google Scholar]
- 7.Institute, Committee on Planning a Continuing Health Professional Education, Medicine Io . Redesigning continuing education in the health professions. National Academies Press; [PubMed] [Google Scholar]
- 8.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006 Dec;29(6):351–64. [PubMed] [Google Scholar]
- 9.Advisory committee on interdisciplinary, community-based linkages January 2009 meeting minutes [homepage on the Internet] U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; Rockville, M.D.: [cited 8/21/2010]. 2009. Available from: http://bhpr.hrsa.gov/interdisciplinary/acicbl/0809minutes.htm. [Google Scholar]
- 10.WHO ∣ framework for action on interprofessional education and collaborative practice [homepage on the Internet] World Health Organization, Department of Human Resources for Health; Geneva, Switzerland: [cited 8/21/2010]. 2010. Available from: http://www.who.int/hrh/resources/framework_action/en/index.html. [Google Scholar]
- 11.Gaboury I, Bujold M, Boon H, Moher D. Interprofessional collaboration within canadian integrative healthcare clinics: Key components. Soc Sci Med. 2009 Sep;69(5):707–15. doi: 10.1016/j.socscimed.2009.05.048. [DOI] [PubMed] [Google Scholar]
- 12.Smith EL, Cronenwett L, Sherwood G. Current assessments of quality and safety education in nursing. Nurs Outlook. 2007 May-Jun;55(3):132–7. doi: 10.1016/j.outlook.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 13.Rafter ME, Pesun IJ, Herren M, Linfante JC, Mina M, Wu CD, et al. A preliminary survey of interprofessional education. J Dent Educ. 2006 Apr;70(4):417–27. [PubMed] [Google Scholar]
- 14.Remington TL, Foulk MA, Williams BC. Evaluation of evidence for interprofessional education. Am J Pharm Educ. 2006 Jun 15;70(3):66. doi: 10.5688/aj700366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craven MA, Bland R. Better practices in collaborative mental health care: An analysis of the evidence base. 2006. Report No.: 51. [PubMed]
- 16.About the USPSTF [homepage on the Internet] U.S. Preventive Services Task Force; Rockville, M.D.: [cited 8/21/2010]. 2010. Available from: http://www.uspreventiveservicestaskforce.org/about.htm. [Google Scholar]
- 17.Cochrane reviews ∣ the cochrane collaboration [homepage on the Internet] The Cochrane Collaboration; Freiburg Germany: [cited 8/21/2010]. 2010. Available from: http://www.cochrane.org/cochrane-reviews. [Google Scholar]
- 18.Satterfield JM, Spring B, Brownson RC, Mullen EJ, Newhouse RP, Walker BB, et al. Toward a transdisciplinary model of evidence-based practice. Milbank Q. 2009 Jun;87(2):368–90. doi: 10.1111/j.1468-0009.2009.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guide to clinical preventive services, 2009. Agency for Healthcare Research and Quality; Rockville, MD: Sep, 2009. Report No.: AHRQ Publication No. 09-IP006. [Google Scholar]
- 20.The Cochrane Collaboration ∣ working together to provide the best evidence for health care [homepage on the Internet] The Cochrane Collaboration; Freiburg Germany: [cited 8/21/2010]. 2010. Available from: http://www.cochrane.org/ [Google Scholar]
- 21.The Cochrane Collaboration . In: Cochrane handbook for systematic reviews of interventions version 5.0.2. Higgins JPT, Green S, editors. Wiley-Blackwell; Chichester, England: Sep, 2009. c2008.; 2009. [Google Scholar]
- 22.Newhouse RP. Evidence-based behavioral practice: An exemplar of interprofessional collaboration. J Nurs Adm. 2008 Oct;38(10):414–6. doi: 10.1097/01.NNA.0000338157.48471.1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steps for evidence-based behavioral practice [homepage on the Internet] Northwestern University; Chicago, Il: Available from: http://www.ebbp.org/steps.html. [Google Scholar]
- 24.Spring B, Walker B, Satterfield J, Newhouse R, Brownson R, Hitchcock K, et al. Foundations for quality: Competencies for interprofessional evidence-based practice. In press.
- 25.Evidence based behavorial practice [homepage on the Internet] Northwestern University; Chicago, IL: Available from: http://www.ebbp.org/index.html. [Google Scholar]
- 26.Kuhn TS. The structure of scientific revolutions. University of Chicago Press; Chicago: 1962. [Google Scholar]
- 27.Barnsteiner JH, Disch JM, Hall L, Mayer D, Moore SM. Promoting interprofessional education. Nurs Outlook. 2007 May-Jun;55(3):144–50. doi: 10.1016/j.outlook.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Légaré F, Ratté S, Stacey D, Kryworuchko J, Gravel K, Graham ID, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database of Systematic Reviews. 2010;(5) doi: 10.1002/14651858.CD006732.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Center to Champion Nursing in America [homepage on the Internet] Center to Champion Nursing in America; Washington, D.C.: [cited 8/21/2010]. 2009. Available from: http://championnursing.org/. [Google Scholar]
- 30.Project overview ∣ QSEN - quality & safety education for nurses [homepage on the Internet] Quality and Safety Education for Nurses (QSEN); Chapel Hill, N.C.: [cited 8/21/2010]. 2010. Available from: http://www.qsen.org/overview.php. [Google Scholar]
- 31.George Washington University, Nursing Alliance for Quality Care [homepage on the Internet] Department of Nursing Education, George Washington University Medical Center; Washington, D.C.: [cited 8/21/2010]. 2010. Available from: http://www.gwumc.edu/healthsci/departments/nursing/naqc/index.html. [Google Scholar]