Abstract
Clinical nursing expertise is central to quality patient care. Research on factors that contribute to expertise has focused largely on individual nurse characteristics to the exclusion of contextual factors. To address this, we examined effects of hospital contextual factors and individual nurse education and experience on clinical nursing expertise in a cross-sectional analysis of data from 8,611 registered nurses. In a generalized ordered logistic regression analysis, the composition of the hospital staff, particularly the proportion of nurses with at least a bachelor of science in nursing degree, was associated with significantly greater odds of a nurse reporting a more advanced expertise level. Our findings suggest that, controlling for individual characteristics, the hospital context significantly influences clinical nursing expertise.
Keywords: expertise, nursing, nursing education, experience, nursing practice environment
Clinical nursing expertise is fundamental to quality of care. Research on the foundations of expertise has focused on individual characteris tics—particularly a nurse's years of experience and level of education. Debate continues about the respective contributions of experience and education to expertise. A notable gap in this debate that we examine is the influence of hospital contextual factors on an individual nurse's expertise. These contextual factors include the educational and experience levels of a nurse's coworkers as well as the nursing practice environment.
We capitalized on a large multi-level secondary data set of nurses in hospitals to examine individual nurses and their contexts. We hypothesized that contextual factors affect expertise above and beyond individual factors. Our study contributes evidence about the theoretical relationships between individual and contextual factors and expertise that may guide efforts to improve nurses' expertise.
As background for the study, in this manuscript we first outline the theoretical framework used to structure this investigation and then review the literature related to expertise in nursing. We then outline the relationships between expertise and the three principal concepts examined in this study—experience, education, and the nurse practice environment.
Theoretical Framework
We developed a multi-level framework (Fig. 1) to describe how clinical expertise develops through both individual and organizational factors. Through this framework, derived from the sociology of organizations (Blau, 1960; Shortell & Getzen, 1979), we suggest that the organization provides a context that influences individual outcomes. The organizational context includes the educational and experiential composition of the staff and the nurse practice environment. A contextual approach is particularly useful for understanding organizational phenomena where individuals are nested within larger systems such as nurses within hospitals. In our framework the individual characteristics of the nurse, such as education level and years of experience, influence an individual nurse's clinical expertise. Additionally, the context in which the nurse practices may help to establish a culture of professional nursing that encourages, values, and provides opportunities for the development of clinical nursing expertise.
FIGURE 1.
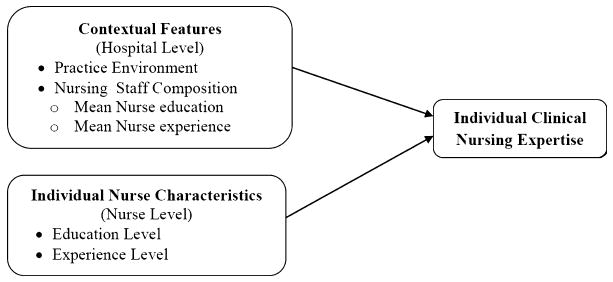
Conceptual framework outlining relationships between individual nurse characteristics, hospital contextual features of nursing and clinical nursing expertise.
Contextual effects have long been of interest in sociological and educational research where, for example, individual student achievement was thought to be influenced by the achievement level of the class and school of a student (Kreft & de Leeuw, 1998). Generally, contextual effects occur when the collective properties of individuals (e.g., nurses) in an organization like a hospital have an effect on an outcome (e.g., expertise) over and above the effect of individual characteristics (Blalock, 1984). Books and Prysby (1988) outlined three potential mechanisms of contextual effects: (a) social interaction with like-minded others, (b) conformity to prevailing norms, and (c) information flow patterns. Although we did not test the specific mechanism, we expected that more educated and experienced staff and a more professional work environment would provide opportunities for ongoing learning and feedback, thereby functioning to promote the development of nurse expertise through these mechanisms.
Contextual effects like those examined in this investigation can be described as compositional or structural (Books & Prysby, 1988). Compositional effects are usually measured as the aggregate mean of an individual phenomenon. In this study, education and experience were examined both as individual-level variables (the education and experience of a nurse) and compositional variables (the mean education and experience for all nurses in a hospital). By contrast, structural variables were derived from individual-level data and represent more complex aggregate measures. In our study, the practice environment was a structural variable derived as a complex measure from nurse ratings of their environment; it was not compositional because it was not an aggregate of nurses' individual characteristics. Based on this framework, we hypothesized that working in a hospital with higher mean levels of education and experience and a more professional practice environment would have a contextual effect on an individual nurse's expertise level even after controlling for the individual nurses' level of education and experience.
Literature Review
Expertise
We defined clinical expertise as a hybrid of practical and theoretical knowledge, based on Benner (1984). Clinically expert nurses are distinguished from their colleagues by their often intuitive ability to efficiently make critical clinical decisions while grasping the whole nature of a situation. Expertise influences nurses' clinical judgment and quality of care and develops when a nurse tests and refines both theoretical and practical knowledge in actual clinical situations (Benner, 1984).
Benner (1984) also detailed the acquisition of nursing expertise and proposed five possible expertise levels: novice, advanced beginner, competent, proficient, and expert. Nurses at the novice stage are still in nursing school. Nurses at the advanced beginner stage use learned procedures and rules to determine what actions are required for the immediate situation. Competent nurses are task-oriented and deliberately structure their work in terms of plans for goal achievement. Competent nurses can respond to many clinical situations but lack the ability to recognize situations in terms of an overall picture. Proficient nurses perceive situations as a whole and have more ability to recognize and respond to changing circumstances. Expert nurses recognize unexpected clinical responses and can alert others to potential problems before they occur. Experts have an intuitive grasp of whole situations and are able to accurately diagnose and respond without wasteful consideration of ineffective possibilities. Because of their superior performance, expert nurses are often consulted by other nurses and relied upon to be preceptors. Although most nurses will progress to the competent level of expertise, many will not become experts (Benner, 1984).
Experience and expertise
Experience and expertise are related but different concepts. We define experience, also based on Benner (1984), as both time in practice and self-reflection that allows preconceived notions and expectations to be confirmed, refined, or disconfirmed in real circumstances. Merely encountering patient conditions and situations is not experience; rather, experience involves nurses reflecting on encountered circumstances to refine their moment-to-moment decision making at an unconscious, intuitive level, (Benner, 1984; Benner & Tanner, 1987; Simmons, Lanuza, Fonteyn, Hicks, & Holm, 2003).
Experience is a necessary but not sufficient condition for expertise and not all experienced nurses are experts (Christensen & Hewitt-Taylor, 2006; Ericsson, Whyte, & Ward, 2007). For example, Benner (1984) noted that a number of years on the job in the same or similar situations may create competence; however, the passage of time and occurrence of events and interactions does not automatically confer expert status. As Benner stated, there is a discontinuity or leap between expertise at the competent level and expertise at the proficient and expert levels. One potential explanation for this discontinuity is that years of experience may provide fluidity and flexibility but not the complex reflexive thinking that has been hypothesized to be an important component of clinical nursing expertise (Bobay, 2004).
Few quantitative studies have been able to capture both the temporal and transactional nature of experience, and these studies have been limited to measuring experience in terms of years in practice. Young, Lehrer, and White (1991) found that nurses with more experience reported performing more complex functions than those with less experience. In a recent study of five hospitals, Bobay, Gentile, and Hagle (2009) found that years of experience were associated with expertise. However, Kovner and Schore (1998) did not find such a relationship.
The majority of the research on how experience contributes to expertise is at the individual nurse level; however, experience has also been assessed as a contextual variable. This latter work has primarily focused on the influence of aggregate experience on patient and nurse outcomes. For example, Aiken, Clarke, Cheung, Sloane, and Silber (2003) assessed the influence of the mean years of experience among nurses on surgical patient mortality in 168 hospitals. They found that the mean experience level was not a significant predictor of mortality. In a study that used the patient care unit as the level of analysis, researchers found that a higher proportion of nurses with ≥ 5 years of experience was associated with fewer medication errors and lower patient fall rates (Blegen, Vaughn, & Goode, 2001). Similarly, Clarke, Rockett, Sloane, and Aiken (2002) examined the effect of the mean nurse experience level at the hospital level on nurse needlestick injuries; they concluded that a low mean experience level was associated with more near-miss needlestick incidents. In another study of nursing outcomes, Kanai-Pak, Aiken, Sloane, and Poghosyan (2008) found that the odds of high burnout, job dissatisfaction and poor-to-fair quality of care were twice as high in hospitals with 50% inexperienced nurses (i.e., nurses with less than 4 years experience) versus those with 20% inexperienced nurses.
Education and expertise
Education influences expertise by providing a theoretical and practical knowledge base that can be tested and refined in actual situations (Dreyfus & Dreyfus, 1996). Didactic learning alone cannot generate clinical expertise, and one distinguishing aspect of nursing education is a focus on clinical learning. Benner (2004) suggested that hands-on learning is at the heart of good clinical judgment. Mentored clinical learning situations in both classrooms and practice sites offer critical opportunities for nurses to apply and integrate theoretical knowledge with actual events (Field, 2004). A sound educational foundation expedites the acquisition of skills through experience (Benner, 1984). Without background knowledge, nurses risk using poor judgment and lack the tools necessary to learn from experience.
Theory and principles enable nurses to ask the right questions to hone in on patient problems to provide safe care and make good clinical decisions. Bonner's (2003) research on nephrology nurses showed expert and non-expert nurses differed based on types of learning opportunities (both formal and informal) rather than years of experience. In a literature review on the relationship between nursing education and practice, Kovner and Schore (1998) reported mixed findings regarding whether and in what ways bachelor of science in nursing (BSN) prepared nurses' skills and abilities differ from those of associate degree and diploma-prepared nurses.
The collective education level of staff may impart a unique contribution to the development of expertise in the clinical setting. Few researchers have focused directly on the aggregate educational composition of the staff with whom a nurse practices as a factor affecting individual clinical nursing expertise. There are, however, examples where researchers have examined the relationship of contextual variables including education at the hospital level, to outcomes. For example, Aiken et al. (2003) found that the proportion of BSN-prepared nurses in a hospital was associated with lower surgical patient mortality and failure to rescue. In the same study, mean years of experience in a hospital was not associated with outcomes and did not alter the relationship between education and outcomes. Aiken et al. (2003) hypothesized that the effect of education was due, in part, to better critical thinking and clinical judgment skills associated with BSN preparation. Estabrooks, Midodzi, Cummings, Ricker, and Giovannetti (2005) also found that the proportion of BSN-prepared nurses in a hospital was associated with lower patient mortality. In a report on two studies, Blegen et al. (2001) found no association between the nursing unit's proportion of BSN-prepared nurses and patient falls and mixed-results for the association with medication errors.
Nurse practice environment and expertise
Many expert nurses leave hospital practice due to negative working conditions (Orsolini-Hain & Malone, 2007). The nurse practice environment may offer a modifiable avenue through which nurse managers and administrators can cultivate nursing expertise and attract and retain nurse experts. Benner (1984) noted that the most skilled clinical nursing performance can be attained in a supportive environment where clinical learning with colleagues from all levels of expertise takes place. Organizations that facilitate a professional nursing practice environment foster clinical autonomy, support the continued education and advancement of nurses, increase the opportunity for shared experience and knowledge with physician colleagues, and provide support for professional decision making and action (Lake & Friese, 2006). In one study of the nurse practice environment and expertise, researchers surveyed 103 nurses in two military hospitals (Foley, Kee, Minick, Harvey, & Jennings, 2002). The investigators measured the practice environment with the Revised Nursing Work Index (NWI-R; Aiken & Patrician, 2000). Expertise was measured by the Manifestation of Early Recognition instrument, a 16-item scale based on the concepts of clinical expertise (Minick, 2003). The results indicated significant, positive although modest correlations between nursing expertise and two of the three reported NWI-R subscales: control over practice and collaborative relationships between nurses and physicians.
Overall, our understanding of the relationship between contextual factors and expertise is limited. Thus, we examined the effects of both hospital contextual factors and individual nurse education and experience on clinical nursing expertise. We hypothesized that contextual factors would affect expertise over and above individual factors.
Methods
We conducted a secondary analysis of cross-sectional data from a 1999 statewide survey of registered nurses (RNs) in Pennsylvania (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002) to explore the relationship between individual nurse characteristics and hospital contextual factors and their association with nursing expertise. The sample for this analysis included acute care staff nurses (n = 9,445) working in Pennsylvania acute care hospitals (n = 182). To obtain stable and reliable estimates, data were limited to hospitals with survey data from at least 15 staff nurses (Lake & Friese, 2006). The average number of respondents per hospital was 86 (range 15–225). Nurse responses were aggregated to calculate the measure of the nurse practice environment and also to create hospital-level measures of education and experience, using the mean as a measure of central tendency. Institutional review board approval for research with human subjects was obtained for the studies that generated these data (Aiken et al., 2002).
Measures
The measures of the variables of interest, including the outcome of individual nurse expertise, independent variables at the nurse level, independent variables at the hospital level, and additional descriptive variables are described below.
Outcome
The dependent variable was nurse-reported level of expertise. Based on Benner's (1984) work, the survey asked nurses to identify their level of expertise as one of the following: Advanced Beginner, Competent, Proficient, or Expert. The responses to this item were categorized as a four-category ordered variable. Nurses at the novice stage are generally still in nursing school and were not included in our study. In unpublished work by one of the authors (Lake, 2002a), nurses' self-reported expertise was strongly correlated with assessments by colleagues and supervisors.
Content validity questions were developed based on two characteristics that Benner (1984) suggested identify expert nurses: (a) how frequently the nurse was selected as a preceptor; and (b) how often the nurse was consulted by other nurses for clinical judgment. The response categories were Never, Rarely, Occasionally, and Frequently.
Independent Variables: Individual Nurse Measures
Education
Nurses reported their highest nursing education degree as diploma, associate's degree (ADN), BSN degree, or master of science in nursing (MSN) degree. The categories were collapsed into less than a BSN (equal to zero) or BSN or higher (equal to one) for analysis. We chose to dichotomize education by BSN status to reflect the importance of the BSN in policy recommendations (American Association of Colleges of Nursing, 2000; Benner, Sutphen, Leonard, Day, & Shulman, 2010). To ensure that there were not different relationships between diploma or ADN level of education and expertise, we estimated alternative models with each category of education and obtained equivalent findings.
Experience
Individual-level nurse experience was analyzed on a continuous scale of years. The data for this variable were drawn from responses to the survey question, “How many years have you worked as an RN?”
Independent Variables: Contextual Measures
Mean education
Mean education was calculated as the group mean of a binary (zero/one) variable indicating an individual nurse's having a BSN degree or higher. This variable was equivalent to the proportion of RNs in each hospital with a BSN degree or higher.
Mean experience
Mean nurse experience in each hospital was measured by calculating the mean of the years of experience among the nurses practicing in each hospital. The data for this variable were drawn from responses to the survey question, “How many years have you worked as an RN?”
Nurse practice environment
The Practice Environment Scale of the Nursing Work Index (PES-NWI) was used to measure the professional nursing practice environment of each hospital (Lake, 2002b). The PES-NWI was adopted by the National Quality Forum (2004) as a national voluntary consensus standard for nursing-sensitive care.
The PES-NWI consists of 31 items in five subscales that characterize the domains of professional nursing practice environments (Lake, 2007). All five subscales were used in this study. The nurses rated each item on a scale of 1 (strongly disagree) to 4 (strongly agree) to indicate whether the feature was “present in the current job.” The subscales are: (a) Nurse Participation in Hospital Affairs; (b) Staffing and Resource Adequacy; (c) Nursing Foundations for Quality of Care; (d) Nurse Manager Ability, Leadership, and Support of Nurses; and (e) Collegial Nurse/Physician Relations. The subscale score was the average of the subscale item responses. The potential score ranged from 1 to 4 with higher scores indicating more agreement that the subscale items were present in the current job. With a theoretical midpoint of 2.5, values above 2.5 indicated general agreement that the characteristics measured by the scales were present; values below 2.5 indicated disagreement. Agreement that characteristics were present was interpreted to indicate a favorable assessment of a domain of the practice environment as measured by the subscale. Hospitals were sorted into a three-level classification (“favorable,” “mixed,” and “unfavorable”) according to how many subscales were assessed favorably by their nurses (Lake & Friese, 2006). Hospitals rated favorably on 0 or 1 subscale were classified as unfavorable, on 2 or 3 as mixed, and on 4 or 5 as favorable. The three-level categorization has been favored for use in research (Aiken, Clarke, Sloane, Lake, & Cheney, 2008; Aiken et al., 2010; Friese, Lake, Aiken, Silber, & Sochalski, 2008; Kutney-Lee et al., 2009; Patrician, Shang, & Lake, 2010). We estimated alternative models with the continuous form of the variable and obtained equivalent findings.
The subscales exhibited high reliability at the individual and hospital levels. Internal consistency at the individual level was high (α ≥ .80) for all subscales in our sample. All hospital-level subscale measures were highly internally consistent (α = .86–.93).
Analysis
Nurse characteristics were explored in descriptive and bivariate analyses. For the purposes of regression modeling, the individual nurse variables were centered on the grand mean—the mean for all the nurses in the sample was subtracted from each individual nurse's score for both the education and experience variables. Centering the individual-level variables and expressing them as a deviation from the grand mean removed correlation and concern with multi-collinearity (Kreft & de Leeuw, 1998). Using the grand-mean-centered variables allowed for an assessment of a within-group effect. We then interpreted within-group effects, which represented the expected difference in log-odds of being in the next highest category of expertise between two nurses working in the same hospital who differ by one unit in an individual-level independent variable (education or experience). Analyzing the hospital-level group means for education and experience allowed for interpretation of a contextual effect. The contextual effect was interpreted as the difference in expertise between two nurses who have the same experience and education but who work in hospitals differing by one unit mean experience or one unit mean education. In other words, these contextual effects explained the association between expertise and the educational and experiential composition of the nursing staff with whom a nurse practiced.
We conducted robust, generalized ordered logistic regression to evaluate the association of nurse and hospital contextual factors with a four-category measure of individual nurses' expertise. Robust regression allows for the analysis of data clustered at an organizational level, such as nurses in hospitals, while addressing error variance arising from intraclass correlation of the data (Huber, 1967; Lake, 2006; White, 1980).
Ordered logistic regression is appropriate with an ordered categorical-dependent variable such as our nurse expertise variable ranging from Advanced Beginner to Expert. An advantage of the generalized ordered logistic model, unlike the ordered logistic model, is that it is not limited by the parallel regression assumption (Williams, 2006). That is, it does not constrain the parameter estimates to be constant across each of the four expertise groups. An assessment of the Brandt test (Long & Freese, 2006) suggested that the parallel slopes assumption would be inappropriate for our data.
We considered and tested both robust and hierarchical linear regression as modeling approaches. The robust versus hierarchical linear models yielded roughly equivalent results in terms of significance and direction of effects. We chose ordered general robust regression because it handled the general problem of correlated observations while still accurately modeling the ordered nature of the dependent variable without being limited by the parallel regression assumption. All presented analyses were conducted using Stata (Version 10).
The generalized ordered logistic model was fitted,
where each Yij was the probability that an individual nurse i was in the kth category out of the M = 4 potential categories of expertise, Xij1 was the grand-centered deviation (Xij1 − X̄.1) of individual nurse experience, Xij2 was the grand-centered deviation (Xij2− X̄.11) of the dummy variable for having a BSN degree or higher, X̄.j1 was the hospital mean of nurse experience, X̄.j2 was the hospital proportion with BSN degree or higher, Zj was the vector of the dummy variables for hospital practice environment category (favorable, mixed, with unfavorable as the reference category). The model predicted the probability of being in the next highest category of expertise. Positive coefficients indicated that higher values on the explanatory variable made it more likely that the respondent would be in a higher category of expertise than the current one. Negative coefficients indicated that higher values on the explanatory variable increased the likelihood of being in the current or a lower category.
Results
The data were cleaned and the final data set (n = 8,611) contained no missing data on the analytic variables. The nurse respondents were 94% female with an average age of 39 years. The respondents reported an average of 13.2 years nursing experience. Thirty-eight percent of the nurses held a BSN degree.
The mean hospital-level nursing experience was 13.6 years. The higher hospital-level mean as compared to the overall mean indicates that nurse experience is not evenly distributed across hospitals. RNs comprised 74% of the licensed nursing staff in the hospitals. Most hospitals (66%) were classified as having mixed practice environments, 21% were classified as having unfavorable environments, and 13% were classified as having favorable environments.
Details of nurses' self-reported level of expertise are displayed in Table 1. The majority of nurses (58%) rated themselves as Proficient, followed in descending proportional order by Competent (20%), Expert (16%), and Advanced Beginner (6%). Nurses' categorization of themselves into the four categories of expertise was correlated with the validation questions of “how frequently a nurse was selected as preceptor” (rs = .34, p < .001) and “how frequently a nurse was consulted by other nurses for clinical judgment on a difficult clinical problem” (rs = .42, p < .001).
Table 1. Nurses' Self-Reported Level of Clinical Nursing Expertise (n= 8,611).
| Level of Expertise | ||||||||
|---|---|---|---|---|---|---|---|---|
| Adv. Beginner | Competent | Proficient | Expert | |||||
| n | % | n | % | n | % | n | % | |
| Totala (%) | 489 | 6 | 1,727 | 20 | 5,028 | 58 | 1,367 | 16 |
| Selected to be preceptorb (%) | ||||||||
| Never | 389 | 80 | 651 | 38 | 905 | 18 | 18 | 13 |
| Rarely | 64 | 13 | 460 | 27 | 1,240 | 25 | 244 | 18 |
| Occasionally | 36 | 7 | 505 | 29 | 2,084 | 41 | 524 | 38 |
| Frequently | 0 | 0 | 111 | 6 | 799 | 16 | 415 | 30 |
| Nurses come to you for your clinical judgmentb (%) | ||||||||
| Never | 61 | 12 | 25 | 1 | 18 | <1 | 2 | <1 |
| Rarely | 144 | 29 | 192 | 11 | 133 | 3 | 26 | 2 |
| Occasionally | 257 | 53 | 1,187 | 69 | 2,593 | 52 | 303 | 22 |
| Frequently | 27 | 6 | 323 | 19 | 2,284 | 45 | 1,036 | 76 |
Note. All numbers are expressed as percentages.
Row total = 100%.
Column total = 100%.
Table 2 displays the distribution of expertise across levels of individual nurse education. Spearman's rank-order correlations demonstrate a weak but significant association between nurse's highest degree (diploma, ADN, BSN, or MSN) and expertise classification (rs = .03, p < .001). Nurses with an MSN reported the highest level of expertise, followed in descending order by Diploma, BSN, and ADN nurses. The high level of expertise reported by Diploma nurses suggests an experience effect as Diploma nurses had an average of 17.7 years of experience, just behind those with an MSN (M = 18.9). Nurses with a BSN had an average of 10.9 years of nursing experience, and ADN-prepared nurses had the least experience (M = 9.5). Individual nurse years of experience were significantly positively correlated with expertise (rs = .48, p < .001).
Table 2. Associations Between Nurse Education Level and Nurse Expertise (n= 8,611).
| Reported Expertise | n | % |
|---|---|---|
| Diploma | 2,997 | 35 |
| Advanced Beginner | 97 | 3 |
| Competent | 556 | 19 |
| Proficient | 1,835 | 61 |
| Expert | 509 | 17 |
| ADN | 2,348 | 27 |
| Advanced Beginner | 160 | 7 |
| Competent | 583 | 25 |
| Proficient | 1,357 | 58 |
| Expert | 248 | 11 |
| BSN | 3,074 | 36 |
| Advanced Beginner | 231 | 8 |
| Competent | 578 | 19 |
| Proficient | 1,769 | 58 |
| Expert | 496 | 16 |
| MSN | 192 | 2 |
| Advanced Beginner | 1 | 1 |
| Competent | 10 | 5 |
| Proficient | 67 | 35 |
| Expert | 114 | 59 |
Note. ADN, Associate's Degree in Nursing; BSN, Bachelor of Science Degree in Nursing; MSN, Master of Science Degree in Nursing.
Table 3 displays the generalized ordered logistic regression coefficients and corresponding odds ratios indicating the effects of nurse characteristics and organizational contextual effects on individual nurse expertise. The coefficients represent the change in log-odds of being in the next highest category of expertise related to one unit change in the predictor or independent variable with other variables held at their mean. The odds ratios indicate the odds of being in the next highest category of expertise related to one unit change in the predictor or independent variable with other variables held at their mean.
Table 3. Effects of Individual Nurse Characteristics and Hospital Contextual Factors on Reporting Higher Level of Expertise (n= 8,611).
| Advanced Beginner vs. Competent, Proficient, and Expert | Advanced Beginner & Competent vs. Proficient and Expert | Advanced Beginner, Competent, and Proficient vs. Expert | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | Odds Ratio | 95% CI | β | SE | Odds Ratio | 95% CI | β | SE | Odds Ratio | 95% CI | |
| Individual-level nurse variables | ||||||||||||
| Experience | 0.63** | 0.05 | 1.89 | 1.71−2.08 | 0.14** | 0.01 | 1.16 | 1.14−1.17 | 0.11** | 0.00 | 1.11 | 1.10−1.12 |
| Education | 0.00 | 0.09 | 1.00 | .84−1.19 | 0.18** | 0.06 | 1.20 | 1.08−1.34 | 0.31** | 0.07 | 1.36 | 1.17−1.57 |
| Hospital-level variables | ||||||||||||
| Mean experience (contextual effect) | −0.01 | 0.02 | .99 | .95−1.04 | −0.02 | 0.01 | 0.98 | .96−1.00 | −0.02 | 0.02 | .98 | .95−1.01 |
| Mean education (contextual effect) | 0.33 | 0.37 | 1.40 | .67−2.89 | 0.83** | 0.22 | 2.29 | 1.49−3.50 | 2.32** | 0.29 | 10.21 | 5.79−18.00 |
| Favorable practice environment | −0.06 | 0.23 | .95 | .61−1.47 | 0.02 | 0.14 | 1.02 | .78−1.35 | −0.28* | 0.12 | .76 | .60−.97 |
| Mixed practice environment | −0.08 | 0.19 | .93 | .63−1.35 | 0.01 | 0.12 | 1.01 | .80−1.28 | −0.04 | 0.11 | .96 | .77−1.18 |
| Intercept | 7.88 | 0.65 | 1.33 | 0.24 | −2.36 | 0.33 | ||||||
p < .05.
p < .001.
At the lower end of expertise (Advanced Beginner vs. all higher categories), the odds of being in a category higher than Advanced Beginner were 1.89 times greater for each additional year of individual nurse experience. However, the effect of individual experience diminishes at the higher end of expertise. Although still significant, the odds of being in the Expert category versus the lower categories were only 1.11 times greater for each additional year of individual nurse experience holding the other variables at their mean. The contextual effect of the mean level of experience at the hospital was not significant at any level.
Education was significant at both the individual and hospital levels. Nurses with a BSN were more likely to report higher expertise levels. Similarly, there was a contextual effect of education. Nurses practicing in hospitals with a higher proportion of BSN nurses were more likely to report higher levels of expertise. This effect was more pronounced at more advanced levels of expertise, as evidenced by the non-significant findings for the Advanced Beginner versus Competent, Proficient, and Expert level but highly significant findings at higher levels (e.g., Advanced Beginner and Competent vs. Proficient and Expert; and Advanced Beginner, Competent, and Proficient, vs. Expert). The practice environment was not significantly associated with clinical nursing expertise.
The contextual effect of a higher proportion of BSN-educated colleagues implies that altering the educational composition of the staff has implications for an individual nurse's level of expertise. As shown in Table 4, if the proportion of BSN-prepared nurses in a hospital increased from 25% to 65%, the predicted probability of an average nurse in an average hospital reporting being an expert increased from .10 to .16.
Table 4. Estimated Probabilities of an Individual Nurse in an Average Hospital Being an Expert by % of Nursing Staff With Education of BSN or More (n= 8,611).
| Education, % With BSN or More | Overall Probabilitya |
|---|---|
| 25 | .10 |
| 35 | .12 |
| 45 | .13 |
| 55 | .15 |
| 65 | .16 |
Note. BSN, bachelor of science in nursing degree.
All probabilities in the overall column are associated with the proportion of nurses with a BSN or more education holding all other variables at their mean.
Discussion
The study provides the first multi-level, multi-hospital evidence showing that the composition of a hospital's staff, particularly the aggregate level of education, contributes to clinical nurse expertise independent of individual education and experience level. Our findings also confirm the evidence from prior, smaller-scale studies showing that individual nurse level of education and years experience are related to clinical nursing expertise (Bobay et al., 2009; Bonner, 2003).
Unexpectedly, we did not find support for our hypothesized association between a professional practice environment as measured by the PES-NWI and nursing expertise. This is surprising in light of the considerable literature suggesting the importance of the professional nurse practice environment measured by the PES-NWI on patient outcomes (Aiken et al., 2008; Friese et al., 2008; Kutney-Lee et al., 2009; Vahey, Aiken, Sloane, Clarke, & Vargas, 2004). Given that the hospital sample demonstrated sufficient variation in practice environments, we do not attribute the lack of association to restricted range of the independent variable.
One potential explanation for the finding of no association between the practice environment and expertise is that the PES-NWI may not capture all facets of the practice environment relevant to the development of clinical nursing expertise. The American Association of Colleges of Nursing (AACN) has specified eight Hallmarks of the Professional Practice Environment (2002), which are a comprehensive set of characteristics that permit “nurses to practice to their full potential” (p. 298). In a review of measures of the practice environment, Lake (2007) identified that although the PES-NWI was best instrument across criteria of theoretical relevance, ease of use, and dissemination, the measure does not cover all eight of the AACN hallmarks. The PES-NWI should be supplemented with four domains—autonomy, recognition/advancement of nurse preparation and expertise, professional development, and supportive relationships with peers—to cover the full spectrum of practice environment measurement. Recognition/advancement of nurse preparation and expertise is one potential domain where the PES-NWI may not assess how the practice environment advances clinical nursing expertise. The missing domain of professional development and supportive relationships with peers may also contain important factors associated with precepting and peer feedback that may enhance expertise.
As a possible alternative to the PES-NWI, a hospital's American Nurses Credentialing Center Magnet Recognition Program status could be used as an overarching contextual factor; however, none of the hospitals in our sample had achieved formal Magnet recognition at the time of data collection. We note that Foley et al. (2002) detected a significant association between the practice environment and expertise in nurse-level bivariate analyses. A key difference between that study and ours may be that both Foley et al.'s independent and dependent variables were a nurse's own ratings of the practice environment and expertise, introducing the potential for correlation due to the same source (i.e., the nurse). In our study, the independent variable (practice environment) was a structural contextual variable measured at the hospital level, and the dependent variable (expertise) was the nurse's own individual rating.
Our study also did not find a contextual effect of hospital experience. Although this seems reasonable given research showing no link between aggregate experience and patient outcomes (Aiken et al., 2003), one limitation may be our one-dimensional measure of experience as a number of years. Benner (1984) noted that experience depends not only on the passage of time but also on the availability of actual situations through which a nurse can refine, elaborate, or disconfirm knowledge. A limitation of our study that is also common throughout the literature is the use of a measure of experience based solely on time.
Our findings may inform nurse executive strategies for shaping the composition of their staff to maximize the expertise of individual nurses. Executives can favor individual characteristics (a BSN or more experience) through recruitment or retention and advancement. Clinical advancement programs based on expertise and the use of expert nurses as clinical preceptors and educators may also augment the overall expertise within a hospital (Moore, 2008). Hospital executives can institute policies favoring hiring of experienced nurses or nurses with a BSN through salary structures that differentiate based on these factors. They can also support completion of the BSN among existing nursing staff by providing tuition reimbursement.
We have shown that although an individual nurse's education level and years experience both influence his or her level of expertise, gains in the probability of an individual nurse being an expert can also be achieved through having a more educated nursing staff overall. To ensure that there is an adequate pool of nurses for hospitals to draw from, particularly to replace retiring experienced nurses, federal policy changes should be directed at preparing BSN-prepared nurses. Expanding the pool of available BSN nurses could be promoted through increasing nursing school program capacity (including faculty), tuition support, targeting of underrepresented groups, and promoting pathways to a BSN for RNs and licensed practical nurses (LPNs).
The current study had notable limitations. The cross-sectional design cannot establish causal relationships. The dependent variable of expertise is self-reported by nurses; although we provide some evidence of content validity, methods of measuring expertise other than self-report should be considered in future research. Our data only represent Pennsylvania nurses and hospitals and the findings may have limited generalizability. The data are from 1999 and some of the variables may have shifted over time. However, data from the National Sample Survey of Registered Nurses show that the percentage of RNs in the US with a BSN as their highest educational preparation has been relatively stable (32.7% in 2000 to 34.2% in 2004; U.S. Department of Health and Human Services, 2006). Additionally, although experience has increased somewhat, the increase is consistent with the aging of the nursing workforce nationally.
Our findings highlight important issues for nurse researchers going forward. Alternatives to self-reported expertise, such as peer or manager assessments, should be explored. Multidimensional measures that assess factors such as care coordination, clinical assessment and management, or relationships with patients may help to develop a more robust conceptualization of nurse expertise. Future research might consider individual trajectories of expertise and identify mechanisms influencing expertise longitudinally. A related research endeavor would develop a more nuanced measure of experience that might capture time as well as the nature of the clinical situations to which the nurse is exposed.
Future researchers should also examine the relationship between expertise and patient outcomes. Factors theoretically related to expertise have been associated with patient outcomes. For example, researchers have found the proportion of staff nurses with a BSN degree (Aiken et al., 2003; Estabrooks et al., 2005; Tourangeau et al., 2007), nurse experience (Blegen et al., 2001; Kendall-Gallagher & Blegen, 2009), and the nursing practice environment (Aiken et al., 2008; Friese et al., 2008) to be significant predictors of patient outcomes. One pathway through which these factors may affect outcomes is the expertise level of nurses. Evidence illuminating this pathway will help complete the causal chain from nurse characteristics and environments to patient outcomes. This evidence can then guide the development of interventions to improve both expertise and outcomes. Clarifying the relationship between patient outcomes and clinical nursing expertise would also enlighten the current state of nursing science on factors such as staffing which largely treat RNs as equivalent in expertise, that is, a nurse is a nurse.
This investigation provides the first multi-hospital study of nursing expertise and its relationship to individual-level education and experience as well as hospital contextual characteristics. Our study did not identify the ideal nurse staffing composition to maximize expertise because ideal staffing is unique to each hospital. Our findings suggest, however, that both individual level and hospital contextual factors have important effects on expertise and must be considered when making human resource decisions.
Acknowledgments
This study was supported by the National Institute of Nursing Research (T32-NR-007104; P30-NR-005043; R01-NR-004513; Aiken, PI; and K01-NR00166; Lake, PI) and the Agency for Healthcare Research and Quality (K08--HS-017551; McHugh, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute for Nursing Research or the Agency for Healthcare Research and Quality. The authors thank the anonymous reviewers, Associate Editor, and Editor for their thoughtful reviews of and suggestions for this manuscript as well as Robert Lucero PhD, MPH, RN for his contributions to early drafts of this manuscript.
References
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. Journal of Nursing Administration. 2008;38:223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Patrician PA. Measuring organizational traits of hospitals: The Revised Nursing Work Index. Nursing Research. 2000;49:146–153. doi: 10.1097/00006199-200005000-00006. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Sloane DM, Cimiotti JP, Clarke SP, Flynn L, Seago JA, et al. Implications of the California Nurse Staffing Mandate for Other States. Health Services Research. 2010 doi: 10.1111/j.1475-6773.2010.01114.x. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Association of Colleges of Nursing. The baccalaureate degree in nursing as minimal preparation for professional practice. 2000 December 12; doi: 10.1053/jpnu.2001.26300. Retrieved April 21, 2010, from http://www.aacn.nche.edu/Publications/positions/baccmin.htm. [DOI] [PubMed]
- American Association of Colleges of Nursing. Hallmarks of the professional nursing practice environment. Journal of Professional Nursing. 2002;18:295–304. doi: 10.1053/jpnu.2002.129231. [DOI] [PubMed] [Google Scholar]
- Benner P. From novice to expert: Excellence and power in clinical nursing practice. Menlo Park, CA: Addison-Wesley; 1984. [Google Scholar]
- Benner P. Using the Dreyfus Model of Skill Acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. The Bulletin of Science, Technology and Society. 2004;24:188–199. [Google Scholar]
- Benner P, Sutphen M, Leonard V, Day L, Shulman LS. Educating nurses: A call for radical transformation. San Francisco: Jossey-Bass; 2010. [Google Scholar]
- Benner P, Tanner C. Clinical judgment: How expert nurses use intuition. American Journal of Nursing. 1987;87:23–31. [PubMed] [Google Scholar]
- Blalock HM. Contextual-effects models: Theoretical and methodological issues. Annual Review of Sociology. 1984;10:353–372. [Google Scholar]
- Blau PM. Structural effects. American Sociological Review. 1960;25:178–193. [Google Scholar]
- Blegen MA, Vaughn TE, Goode CJ. Nurse experience and education: Effect on quality of care. Journal of Nursing Administration. 2001;31:33–39. doi: 10.1097/00005110-200101000-00007. [DOI] [PubMed] [Google Scholar]
- Bobay KL. Does experience really matter? Nursing Science Quarterly. 2004;17:313–316. doi: 10.1177/0894318404269369. [DOI] [PubMed] [Google Scholar]
- Bobay K, Gentile DL, Hagle ME. The relationship of nurses' professional characteristics to levels of clinical nursing expertise. Applied Nursing Research. 2009;22:48–53. doi: 10.1016/j.apnr.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Bonner A. Recognition of expertise: An important concept in the acquisition of nephrology nursing expertise. Nursing & Health Sciences. 2003;5:123–131. doi: 10.1046/j.1442-2018.2003.00143.x. [DOI] [PubMed] [Google Scholar]
- Books J, Prysby C. Studying contextual effects on political behavior: A research inventory and agenda. American Politics Quarterly. 1988;16:211–238. [Google Scholar]
- Christensen M, Hewitt-Taylor J. From expert to tasks, expert nursing practice redefined? Journal of Clinical Nursing. 2006;15:1531–1539. doi: 10.1111/j.1365-2702.2006.01601.x. [DOI] [PubMed] [Google Scholar]
- Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. American Journal of Infection Control. 2002;30:207–216. doi: 10.1067/mic.2002.123392. [DOI] [PubMed] [Google Scholar]
- Dreyfus HL, Dreyfus SE. The relationship of theory and practice in the acquisition of skill. In: Benner PA, Tanner CA, Chesla CA, editors. Expertise in nursing practice: Caring, clinical judgment, and ethics. New York: Springer; 1996. [Google Scholar]
- Ericsson KA, Whyte J, Ward P. Expert performance in nursing: Reviewing research on expertise in nursing within the framework of the expert-performance approach. Advances in Nursing Science. 2007;30:E58–E71. doi: 10.1097/00012272-200701000-00014. [DOI] [PubMed] [Google Scholar]
- Estabrooks CA, Midodzi WK, Cummings GG, Ricker KL, Giovannetti P. The impact of hospital nursing characteristics on 30-day mortality. Nursing Research. 2005;54:74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- Field DE. Moving from novice to expert—The value of learning in clinical practice: A literature review. Nurse Education Today. 2004;24:560–565. doi: 10.1016/j.nedt.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Foley BJ, Kee CC, Minick P, Harvey SS, Jennings BM. Characteristics of nurses and hospital work environments that foster satisfaction and clinical expertise. Journal of Nursing Administration. 2002;32:273–282. doi: 10.1097/00005110-200205000-00007. [DOI] [PubMed] [Google Scholar]
- Friese CR, Lake ET, Aiken LH, Silber JH, Sochalski J. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Services Research. 2008;43:1145–1163. doi: 10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber PJ. The behavior of maximum likelihood estimates under non-standard conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability; Berkeley, CA: University of California Press; 1967. pp. 221–233. [Google Scholar]
- Kanai-Pak M, Aiken LH, Sloane DM, Poghosyan L. Poor work environments and nurse inexperience are associated with burnout, job dissatisfaction and quality deficits in Japanese hospitals. Journal of Clinical Nursing. 2008;17:3324–3329. doi: 10.1111/j.1365-2702.2008.02639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Gallagher D, Blegen MA. Competence and certification of Registered Nurses and safety of patients in intensive care units. American Journal of Critical Care. 2009;18:106–113. doi: 10.4037/ajcc2009487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovner CT, Schore J. Differentiated levels of nursing work force demand. Journal of Professional Nursing. 1998;14:242–253. doi: 10.1016/s8755-7223(98)80065-3. [DOI] [PubMed] [Google Scholar]
- Kreft IGG, de Leeuw J. Introducing multilevel modeling. London: Sage; 1998. [Google Scholar]
- Kutney-Lee A, McHugh MD, Sloane DM, Cimiotti JP, Flynn L, Neff DF, et al. Nursing: A key to patient satisfaction. Health Affairs. 2009;28:w669–w677. doi: 10.1377/hlthaff.28.4.w669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET. Development of survey measures of clinical nursing expertise. Paper presented at the 14th Annual Scientific Session of the Eastern Nursing Research Society.2002a. [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Research in Nursing & Health. 2002b;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lake ET. Multilevel models in health outcomes research. Part II: Statistical and analytic issues. Applied Nursing Research. 2006;19:113–115. doi: 10.1016/j.apnr.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Lake ET. The nursing practice environment: Measurement and evidence. Medical Care Research and Review. 2007;64:104S–122S. doi: 10.1177/1077558707299253. [DOI] [PubMed] [Google Scholar]
- Lake ET, Friese CR. Variations in nursing practice environments: Relation to staffing and hospital characteristics. Nursing Research. 2006;55:1–9. doi: 10.1097/00006199-200601000-00001. [DOI] [PubMed] [Google Scholar]
- Long JS, Freese J. Regression models for categorical dependent variables using Stata. 2nd. College Station, TX: Stata Press; 2006. [Google Scholar]
- Minick P. Manifestations of early recognition: A measure of nursing expertise. In: Strickl OI, DiIorio C, editors. Measurement of nursing outcomes. New York: Springer; 2003. pp. 294–303. [Google Scholar]
- Moore ML. Preceptorships: Hidden benefits to the organization. Journal for Nurses in Staff Development. 2008;24:E9–E15. doi: 10.1097/01.NND.0000300859.29503.ae. [DOI] [PubMed] [Google Scholar]
- National Quality Forum. National Voluntary Consensus Standards for Nursing-Sensitive Care: An initial performance measure set—A consensus report (No NQFCR-08-04) Washington, DC: 2004. [Google Scholar]
- Orsolini-Hain L, Malone RE. Examining the impending gap in clinical nursing expertise. Policy, Politics, & Nursing Practice. 2007;8:158–169. doi: 10.1177/1527154407309050. [DOI] [PubMed] [Google Scholar]
- Patrician PA, Shang J, Lake ET. Organizational determinants of work outcomes and quality care ratings among Army Medical Department registered nurses. Research in Nursing and Health. 2010;33:99–110. doi: 10.1002/nur.20370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortell SM, Getzen TE. Measuring hospital medical staff organizational structure. Health Services Research. 1979;14:97–110. [PMC free article] [PubMed] [Google Scholar]
- Simmons B, Lanuza D, Fonteyn M, Hicks F, Holm K. Clinical reasoning in experienced nurses. Western Journal of Nursing Research. 2003;25:701–719. doi: 10.1177/0193945903253092. [DOI] [PubMed] [Google Scholar]
- Tourangeau AE, Doran DM, McGillis Hall L, O'Brien Pallas L, Pringle D, Tu JV, et al. Impact of hospital nursing care on 30-day mortality for acute medical patients. Journal of Advanced Nursing. 2007;57:32–44. doi: 10.1111/j.1365-2648.2006.04084.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The registered nurse population: Findings from the March 2004 National Sample Survey of Registered Nurses. Washington, DC: Health Resources and Services Administration, Bureau of Health Professions; 2006. [Google Scholar]
- Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Medical Care. 2004;42:II57–II66. doi: 10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–838. [Google Scholar]
- Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. The Stata Journal. 2006;6:58–82. [Google Scholar]
- Young WB, Lehrer EL, White WD. The effect of education on the practice of nursing. Image: The Journal of Nursing Scholarship. 1991;23:105–108. doi: 10.1111/j.1547-5069.1991.tb00652.x. [DOI] [PubMed] [Google Scholar]


