Abstract
Background
Incident anxiety and depression are associated separately with cardiac events and mortality in patients after acute coronary syndromes, but the influence of persistent comorbid depression and anxiety on mortality remains unknown. The purpose of this study was to determine the prevalence of comorbid persistent depressive and anxious symptoms in individuals with ischemic heart disease and to evaluate effects on mortality.
Methods
Prospective, longitudinal cohort design in the context of a randomized trial to decrease patient delay in seeking treatment for ischemic heart symptoms (PROMOTION trial) was used, with twelve-month follow-up of 2325 individuals with stable ischemic heart disease. Participants were assessed on enrollment and at three months using the Multiple Adjective Affect Checklist and the Brief Symptom Inventory for depressive and anxious symptoms, respectively.
Results
At three months, 608 individuals (61.7%) reported persistent symptoms of depression, anxiety, or both. Three hundred seventy-nine (42.5%) and 1056 (45.4%) had persistent anxious and depressive symptoms, respectively. Those with persistent, comorbid symptoms had higher mortality compared to others (p = .029). The combined presence of anxious and depressive symptoms contributed significantly to mortality when compared to symptom-free participants (OR 2.35, 95% CI 1.23 – 4.47, p = .010). The presence of persistent depressive symptoms only and persistent anxious symptoms only were not associated with death, when other demographic and clinical variables were considered.
Conclusions
Persistent symptoms of anxiety and depression increased substantially the risk of death in patients with ischemic heart disease. Future research into shared and unique pathways and treatments is needed.
Keywords: anxiety, depression, ischemic heart disease, mortality
Introduction
Depression and anxiety are common in patients with chronic ischemic heart disease (IHD). For depression and anxiety, prevalence rates of 32% and 26%, respectively, have been reported in post-myocardial infarction patients and in stable populations of IHD patients.[1–5] These emotional states are known to persist after a cardiac event, and rates of both have been reported to increase during the first year after a myocardial infarction (MI).[3] In IHD patients, depression has been associated independently with increased mortality and morbidity, including increased cardiac and all-cause mortality and increased non-fatal cardiac events.[6–10] While anxiety is also associated with increased morbidity in IHD, its association with mortality is less certain.[11, 12]
Despite the known deleterious effects of both incident depression and anxiety on cardiac outcomes, the impact of persistent mood disorders has received relatively little attention. Persistent depression has been associated with poor adherence to treatment regimens after MI, but few studies have looked at the effect of persistent depression on cardiac events or mortality. A recent report regarding persistent depression in men with Type 2 diabetes found that persistent depression was associated with lower mortality risk. Evidence regarding the effect of persistent anxiety on cardiac prognosis is also scarce.[12] Both persistent anxiety and depression have been shown to have negative effects on subsequent health-related quality of life.[13]
Anxiety and depression are highly comorbid, both in psychiatric populations and in individuals with chronic medical conditions, including heart disease.[14–16] Although the effect of depression on future cardiac events has been well established, previous reports have not considered the mediating or confounding effect of co-existing anxiety on mortality and morbidity. Anxiety and depression may act synergistically to increase the risk of death or other cardiac events. To date, this possibility has not been systematically investigated. Only a single study has reported that anxiety is more closely related to cardiac events than depression, when both are present in patients with IHD.[17] No investigators have reported the influence of comorbid persistent anxiety and persistent depression on subsequent cardiac events. The purpose of the current study was to determine the prevalence of comorbid persistent depression and anxiety in community dwelling individuals with documented IHD and to evaluate the effect of comorbid persistent depression and anxiety on mortality.
Materials and Methods
Design
As part of a large multicenter clinical trial to reduce prehospital delay in IHD patients experiencing symptoms of acute coronary syndrome (the PROMOTION trial), 3523 patients from seven sites in three countries (United States, Australia, New Zealand) were randomized to received either usual care or a brief teaching intervention delivered by expert nurses and aimed at increasing knowledge of acute coronary event symptoms, along with when and how to seek treatment.[18] This report constitutes an a priori planned analysis of the PROMOTION trial.
Sample
After approval of internal review boards at each site, patients gave informed consent prior to study participation. Patients were eligible for the PROMOTION trial if they had a diagnosis of IHD, confirmed by their physician and/or medical record, and lived independently (i.e., not in an institutional setting). Patients were excluded if they have any of the following: 1) a complicating serious comorbidity (including psychiatric diagnoses of current psychosis or bipolar disorder), 2) untreated malignancy or neurological disorder which impaired cognition, 3) inability to understand spoken English and unable to respond to English language questions on the data collection instruments, and 4) a major and uncorrected hearing loss. To avoid selection bias, individuals with previous histories of mood disorders were not excluded. Of the 3523 patients enrolled in the parent study, 2325 had complete data at all time points and were included in the current report.
Instruments
Two self-report instruments were used to measure depression and anxiety. Depression was measured by the depression subscale of the Multiple Adjective Affect Checklist (MAACL-D), a self-report measure consisting of 132 alphabetically arranged adjectives. Higher scores indicate greater depressive symptoms. The MAACL-D has been used extensively in research and clinical practice and has established reliability and validity, with reported internal consistency reported to be 0.89, .83, and .88.[19, 20] In the current study, the Cronbach’s α coefficients was 0.86. Anxiety was measured using the anxiety subscale of the Brief Symptom Inventory. It consists of 6-items that are rated by the patient on a 5-point scale (0–4) of distress ranging from "not at all" to "extremely". Item scores are summed and the mean obtained. The range of scores is 0 to 4, with higher scores indicating higher levels of anxiety symptoms. Construct, convergent, discriminant, and predictive validity of the Brief Symptom Inventory have been demonstrated in a series of studies.[21] In this study, reliability of the instrument was demonstrated by a Cronbach’s alpha of 0.86. Demographic and clinical data were obtained by self-report and confirmed by medical record review.
Procedure
After giving informed consent, individuals completed the study instruments and were randomized to either the intervention or treatment group of the parent study.[18] At three months, participants repeated the MAACL and the BSI. Those patients who scored higher than reported community norms established for each instrument (BSI > 0.33[21] or MAACL-D >11[19]) both at baseline and at 3 months were considered to have persistent symptoms of anxiety and/or depression. At three, 12, and 24 months, they were queried regarding occurrence of acute coronary events and emergency room visits. Medical records were obtained to confirm all events. Patients were followed for up to a median of 21.6 months. Cardiac and all-cause deaths were verified from medical records and death certificates. Medical records were reviewed by trained researchers unaware of participants’ level of anxiety or depression symptoms.
Analysis
Measures of central tendency were used to describe the sample. Patients identified as consistently having symptoms of both anxiety and depression were compared to all others by t-test for continuous variables and Chi-square for categorical data. The effect of persistent symptoms of both anxiety and depression on all-cause mortality was evaluated using a multivariable Cox regression model. Demographic and clinical variables that were significantly different in individuals with and without persistent anxiety and depression at the ≤ .10 level were included in the model. Demographics (age, gender, education, marital status) and clinical (comorbidities, risk factors, prior cardiac procedures) variables were entered into the model first as separate blocks. Group assignment (intervention or control) in the parent study was entered in an individual block, prior to the entry of a variable coding the presence/absence of persistent anxiety and persistent depression as a final block in the model. Forced entry was used for all variables. Data were analyzed using SPSS 16.0 (Chicago, IL).
Results
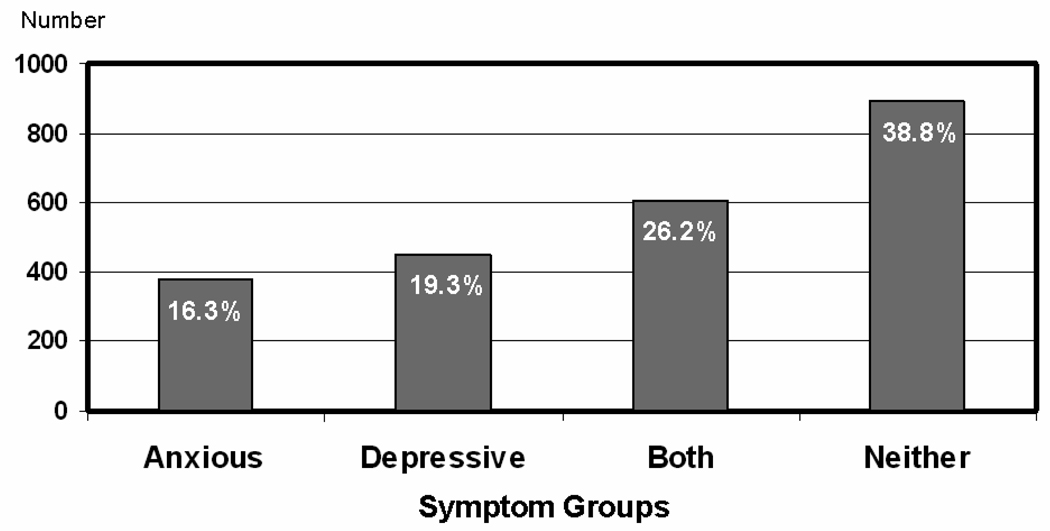
Patients were primarily male (n = 1717, 73.8%) and elderly (67.2 ± 10.7 years). Persistent symptoms of both anxiety and depression were common in the sample. Overall, 1435 individuals (61.7%) reported persistent symptoms of anxiety, depression or both (Figure 1). Considering symptoms of each dysphoria individually, 987 (42.5%) participants had persistent symptoms of anxiety, while 1056 (45.4%) had persistent depressive symptoms. Demographic and clinical characteristics of patients with and without comorbid persistent symptoms of anxiety and depression are summarized in Table 1. Regarding demographic characteristics, patients with both persistent symptoms of both anxiety and depression were more likely to be female and poorer than all others. A higher proportion of women reported the presence of both symptoms than did men (221 [30.6%] vs. 387 [24.2%], p = .001). They were younger (65.8 ± 11.4) than those with either symptoms of anxiety only, symptoms of depression only or neither (67.5 ± 9.77, p = .013). Clinical factors that distinguished individuals with persistent symptoms of both anxiety and depression from all others were: angina (p = .025), myocardial infarction (p = .028), and diabetes (p = .006); current smoking (p = .010), being sedentary (p < .001); and lack of participation in cardiac rehabilitation (p = .010).
Figure 1.
Distribution of Symptom Groups (Anxious, Depressive, Both, Neither)
Table 1.
Demographic and Clinical Characteristics
| Variable | Total Sample (n = 2325) n (%) |
Persistent Anxious and Depressive Symptoms (n = 608) n (%) |
All Others (n = 1717) n (%) |
P |
|---|---|---|---|---|
| Age: | .001 | |||
| < 56 years | 380 (16.3) | 128 (21.1) | 252 (14.7) | |
| 56 – 64.9 years | 524 (22.5) | 143 (23.5) | 381 (22.2) | |
| 65 – 79.9 years | 1178 (50.7) | 274 (45.1) | 904 (52.6) | |
| ≥ 80 years | 243 (10.5) | 63 (10.4) | 180 (10.5) | |
| Female | 723 (31.1) | 221 (36.3) | 502 (29.2) | .001 |
| Married | 1664 (71.6) | 419 (68.9) | 1245 (72.5) | .094 |
| Uninsured or government only | 1178 (50.8) | 318 (52.4) | 289 (47.6) | .370 |
| Not Caucasian | 177 (7.6) | 54 (8.9) | 123 (7.2) | .182 |
| Income in U.S. dollars: | .001 | |||
| < $15K | 515 (22.2) | 169 (27.8) | 346 (20.2) | |
| $15 – 30K | 556 (23.9) | 141 (23.2) | 415 (24.2) | |
| $30 – 45K | 403 (17.3) | 109 (17.9) | 294 (17.1) | |
| $45 – 60K | 327 (14.1) | 66 (10.9) | 261 (15.2) | |
| > $60K | 524 (22.5) | 123 (20.2) | 401 (23.4) | |
| Angina | 1426 (61.3) | 396 (65.1) | 1030 (60.0) | .026 |
| Myocardial infarction | 1288 (55.4) | 360 (59.2) | 928 (54.0) | .029 |
| PTCA | 1121 (48.2) | 308 (50.7) | 813 (47.4) | .171 |
| Stent | 933 (40.4) | 254 (41.9) | 679 (39.8) | .362 |
| Bypass surgery | 1083 (46.6) | 279 (45.9) | 804 (46.8) | .705 |
| Peripheral artery disease | 230 (9.9) | 65 (10.7) | 165 (9.6) | .431 |
| Diabetes | 475 (20.4) | 152 (25.0) | 323 (18.8) | .002 |
| Stroke | 216 (9.3) | 68 (11.2) | 148 (8.6) | .073 |
| Current smoker | 128 (5.5) | 46 (7.6) | 82 (4.8) | .013 |
| Sedentary | 716 (30.8) | 223 (36.7) | 493 (28.7) | <.001 |
| Attended cardiac rehab | 1267 (54.5) | 304 (50.0) | 963 (56.1) | .010 |
| Assigned to experimental group | 1172 (50.4) | 288 (47.4) | 884 (51.5) | .080 |
| Alive at 12 months follow-up | 2262 (97.3) | 585 (96.2) | 1677 (97.7) | .058 |
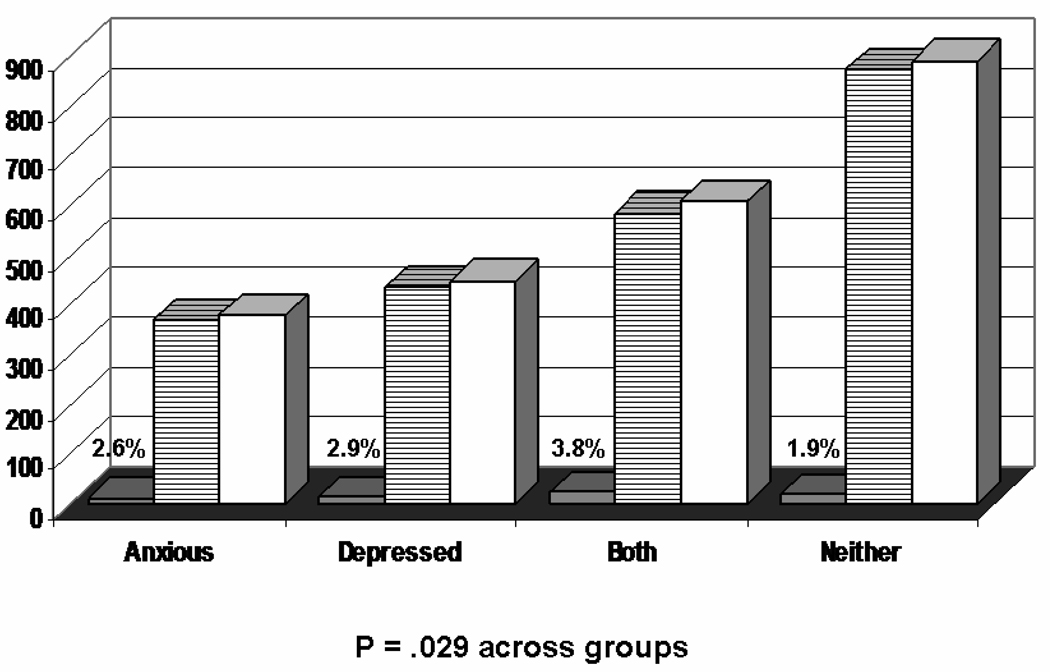
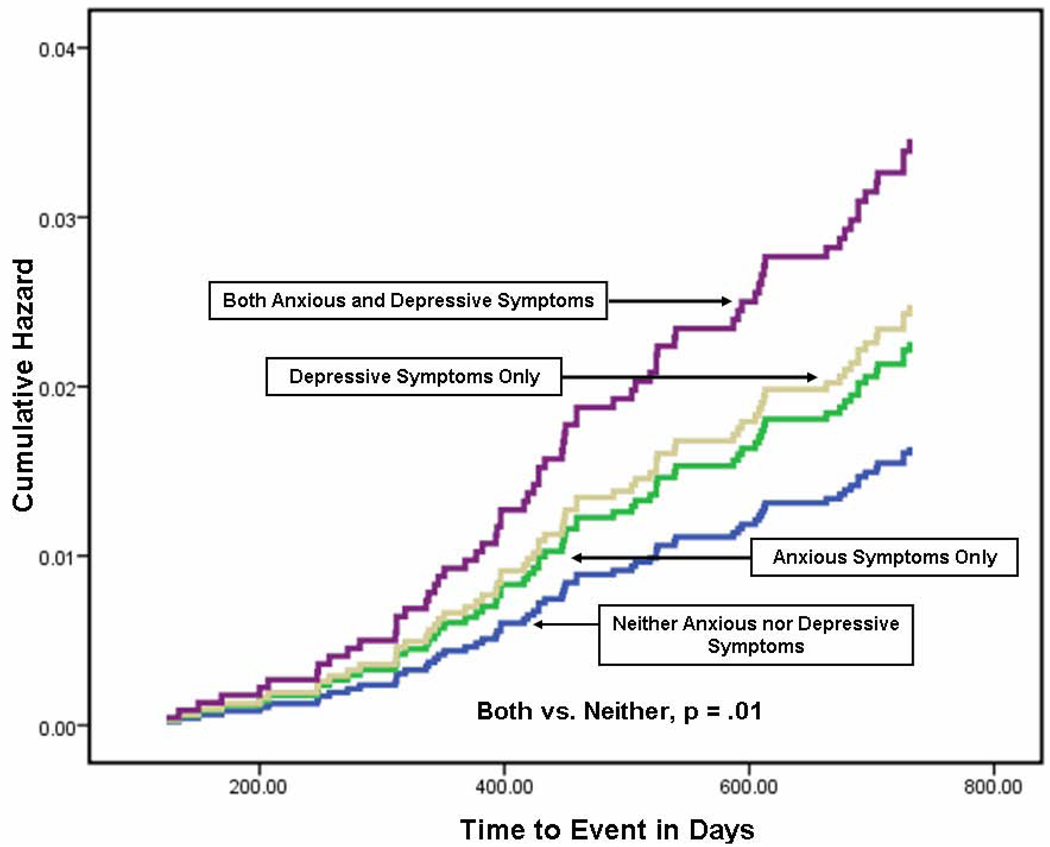
Over the follow-up period, a total of 63 participants died. Twenty-three (36.5%) deaths were attributable to cardiac causes. The frequency of deaths differed across the four groups (p = .029), with the greatest proportion occurring in individuals with both persistent symptoms of both anxiety and depression (Figure 2). Of those with symptoms of both anxiety and depression, 23 of 608 individuals (3.78%) died over 12 months of follow-up, compared to 17 of 890 individuals (1.87%) in the group without symptoms (p = .010, see Figure 3).
Figure 2.
Frequency of Death by Symptom Group (Anxious, Depressive, Both, Neither). Black = deaths; Stripped = survivors; White = total
Figure 3.
Hazard Plot of Symptoms Groups (Anxious, Depressive, Both, Neither) on Morality (N = 2325)
The relationship of anxiety and depression symptom status to mortality when relevant demographic and clinical variables are considered is presented in Table 2. The presence of symptoms of comorbid anxiety and depression, but not the presence of only anxiety symptoms or only depressive symptoms, was significantly associated with mortality (Hazard Ratio = 2.35, 95% confidence interval [CI] 1.23 – 4.47, p = .010). In addition to the presence of comorbid symptoms of anxiety and depression, only age (Harzard Ratio, = 1.08, 95% CI = 1.04 – 1.11, p < .001) and history of myocardial infarction (Hazard Ratio = 1.985, 95% CI 1.14 – 3.45, p = .015) were significant predictors of mortality. For every added year of age, there as an up to 11% increased risk of mortality. Compared to participants who had not had myocardial infarctions, those with a prior history of infarction were 3.5 times more likely to die during the study period. Other factors that were significant when considered alone, such as being female, past medical history, smoking status, activity level, and cardiac rehab attendance, did not contribute independently to mortality risk in the multivariate analysis.
Table 2.
Relationship of Anxious and Depressive Symptoms Status to Mortality when Demographic and Clinical Variables Are Considered
| Adjusted Beta |
Sig. | Hazard Ratio |
95.0% Confidence Interval |
||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age (years) | .074 | .000 | 1.077 | 1.044 | 1.111 |
| Annual income level compared to <$ !5,000: | |||||
| $15,000 – $29,999 | .037 | .920 | 1.037 | .508 | 2.118 |
| $30,000 – $44,999 | −.970 | .071 | .379 | .132 | 1.085 |
| $45,000 – $59,999 | .483 | .271 | 1.621 | .686 | 3.829 |
| ≥ $60,000 | −.076 | .866 | .927 | .383 | 2.243 |
| Not married | −.067 | .841 | .935 | .487 | 1.797 |
| Uninsured | −.196 | .474 | .822 | .482 | 1.404 |
| Female | −.430 | .184 | .651 | .345 | 1.227 |
| History of angina | −.115 | .658 | .892 | .536 | 1.482 |
| History of myocardial infarction | .685 | .015 | 1.985 | 1.143 | 3.446 |
| Diabetic | .258 | .416 | 1.294 | .696 | 2.406 |
| History of stroke | .360 | .308 | 1.434 | .717 | 2.865 |
| Current smoker | −.253 | .731 | .777 | .184 | 3.274 |
| Sedentary | .022 | .935 | 1.023 | .595 | 1.759 |
| No cardiac rehabilitation | −.154 | .561 | .858 | .511 | 1.439 |
| BMI | −.046 | .148 | .955 | .898 | 1.016 |
| Intervention group assignment | .269 | .297 | 1.309 | .789 | 2.172 |
| Anxiety and Depression Symptom status compared to symptom-free: | |||||
| Persistently anxious | .436 | .276 | 1.546 | .706 | 3.389 |
| Persistently depressed | .378 | .316 | 1.459 | .698 | 3.052 |
| Both anxious and depressed persistently | .852 | .010 | 2.345 | 1.230 | 4.468 |
Discussion
Our findings emphasize the ubiquitousness of symptoms of anxiety and depression in community-dwelling adults with IHD. The majority of individuals in our study (61.2%) suffered from significant symptoms of depression, anxiety or both. This is consistent with the reports of other investigators, who confirm that persons with IHD are more likely to experience both anxiety and depression than those without IHD.[22–24] In fact, among individuals with IHD, the odds of developing anxiety and depression are double those of individuals without heart disease, even after adjusting for age and gender. [25] Both anxiety and depression are known to be associated with poorer outcomes in patients with IHD, which underscores the importance of our findings. In fact, the American Heart Association has issued a consensus statement recently endorsing the need for routine depression screening in all patients with IHD.{Lichtman, 2008 741 /id}
This report is one of only a few which have investigated the combined effects of symptoms of both anxiety and depression on cardiac outcomes in those with identified IHD. In evaluating the long-term effects of multiple psychological risk factors, Frasure-Smith and colleagues found that only anxiety and depression (compared to anger, stress and social support) were associated with cardiac mortality.[27] By using a single instrument (the General Health Questionnaire-20) that evaluated psychological distress as a combination of symptoms of depression, anxiety, and dysfunction, they found an association of comorbid anxiety and depression with 5-year cardiac mortality. However, in models adjusted for disease severity, age, and risk factors, only depression conferred an increased risk of cardiac death. In a second report evaluating cardiac mortality plus acute cardiac events, Frasure-Smith et al compared the effect of comorbid anxiety and depression to that of a single diagnosis (anxiety or depression) on occurrence of cardiac events (including mortality, acute coronary syndrome or nonelective revascularization) over two years of follow-up.[28] They found no added effect for the comorbid conditions, compared to single conditions.
Differences in the Frasure-Smith reports compared to our findings may be attributed to how and when IHD sufferers were enrolled, how and when mood disorders were measured, and to the selection of outcome variables. We focused on community-dwelling individuals with IHD, while Frasure-Smith et al enrolled only individuals hospitalized for acute coronary syndrome (ACS). Thus, at enrollment our sample may have been more heterogeneous, but with fewer patients in an acute phase of their cardiac illness. While the Frasure-Smith group included only cardiac mortality and other cardiac-related events, we used a broader category of all-cause mortality, which was more appropriate for our older, community-dwelling sample.[29, 30] Finally, we measured symptoms of anxiety and depression at baseline and again at three months to evaluate persistence of symptoms, while the earlier reports used only baseline assessments.
This study is unique in its focus on the relationship of persistent comorbid symptoms of anxiety and depression to mortality in IHD patients. A few studies have examined separately the persistence of anxiety or depression on outcomes in cardiac or other populations, with equivocal findings. Grace et al reported that persistent anxiety (six months) was associated with a greater number of self-reported recurrent cardiac events, after controlling for IHD severity and smoking, in the first year after ACS.[31] Similarly, Rieckmann et al reported that ACS patients who were persistently depressed (three months) were markedly more likely to be non-adherent to electronically monitored aspirin therapy than nondepressed individuals or those with remitted depression.[32] Conversely, in a large sample of veterans with Type 2 diabetes, Richardson et al reported that even though 10-year all-cause mortality was greater in those with depression, the odds of death decreased more in whites with persistent depression than in blacks.[33] Persistent depression, assessed at 18 month intervals over six years, has been reported to occur more frequently in older women than in older men.[34] While we controlled for gender in our analysis, our sample was too homogeneous to consider racial differences. Race and gender interactions with persistent anxiety and depression require further study.
Our use of all-cause mortality, rather than only cardiac-related mortality, as an outcome measure extends initial evidence that persistent symptoms of depression predict later physical health status in IHD patients.[35] It is likely to also to be a more inclusive measure of adverse outcome and less susceptible to bias in coding. These findings are consistent with previous reports that found incident depression to be an independent predictor of all-cause mortality.[36] Several proposed mechanisms point to the relationship we found between persistently comorbid symptoms of anxiety and depression and all-cause mortality. In addition to the pathways hypothesized above to account for the added effect of comorbid symptoms of anxiety and depression on survival, additional factors may explain why these conditions are related not only to cardiac death, but to all causes of death. First, depression and anxiety may exacerbate other common medical conditions, such as diabetes, stroke, and hypertension, in which depression has been implicated as a predictor of disease-specific mortality.[37, 38] Second, both anxiety and depression may affect cognitive performance and behavior in the course of chronic conditions, thereby increasing disability and mortality.[29, 39] Third, depression appears to have an independent effect (after controlling for chronic conditions) on total life expectancy, particularly in those aged > 70 years, who accounted for 43% of our sample.[30]. Finally, both anxiety and depression are associated with lower quality of life and lower health status, which may in turn, be related to mortality.[40, 41]
Several biobehavioral pathways may account for our findings. Both anxiety and depression may activate stress mechanisms that increase oxygen consumption and potentiate myocardial ischemia.[39] Each condition is believed to activate separate autonomic and adrenal pathways that lead to increased sudden death (anxiety) or increased coaguability and risk of thrombosis (depression).[39, 42–44] In addition, investigators hypothesize that both anxiety and depression may reduce quality of life and contribute to adverse health behaviors, such as inactivity, smoking, and lack of attention to dietary restrictions and medication adherence, which exacerbate atherosclerosis.[43, 44]. Regarding depression, new reports suggest that behavioral, rather than biologic, mediators, may be more important in explaining the its relationship to mortality in cardiac patients.[45] Irrespective of mechanisms, there is compelling evidence that depression and anxiety are linked to cardiac disease; both are highly prevalent, but underrecognized in cardiac patients.{Rumsfeld, 2005 742 /id}
Our study has several limitations. We used self-report instruments to determine the presence of symptoms anxiety and depression, rather than diagnostic interviews or identification of clinical syndromes. However, substantial evidence now supports the belief that symptoms of depression and anxiety alone confer greater risk of poor health outcomes and that clinical depression and depressive symptoms share a large proportion of common variance.[36, 47] Also, use of self-report may have introduced recall bias. We included only subjects in whom we could confirm potential confounding variables, so selection bias may have been possible. However, we found no differences in subjects who were included in the analysis and those who were not. Our sample was largely Caucasian, so we could not consider race or ethnicity as a covariate.
Our findings have implications for both clinical practice and research. Given the extremely common nature of anxious and depressive symptoms found in our study, clinicians must be assess patients periodically for both these conditions. While it is important to identify and treat new depressive or anxious symptoms, it may be even more important to attend to persistent symptoms and to reassess treatment plans if symptoms do not remit over time. Current evidence indicates that psychotherapy combined with pharmacotherapy is often the most effective treatment for clinical depression and anxiety, that treatment is most successful when priority is placed on patient preferences, and that treatment offered in a primary care setting rather than a psychiatric one, may increase adherence.[48, 49] Future research should aim at evaluating strategies to optimize successful screening and treatment, integrate assessment and treatment into clinical practice, and make treatment options more acceptable to IHD patients. In addition, more studies are needed to explicate shared and unique biobehavioral mechanisms that link anxiety and depression to mortality in the context of IHD. Finally, further study is needed to identify subgroups of IHD patients, such as older adults, women, and specific racial or ethnic groups, in whom anxiety, depression or both confer the greatest risk of early death.
Acknowledgements
Funded by National Institutes of Health, National Institute of Nursing Research (R01 NR05323). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health. The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology.[50]
Lynn V. Doering takes responsibility for the integrity of the data and the accuracy of the data analysis. Lynn V. Doering, Kathleen Dracup, Sharon McKinley, Barbara Riegel, Debra K. Moser, Hendrika Meischke, and all contributed to the design of the study. Stephen Paul provided statistical consultation. All authors participated significantly in the conduct of the study and have full access to all of the data in the study.
Other contributions relate to data acquisition:
Beverly Carlson, RN, MS, Sharpe HealthCare, San Diego; Linda Aitken, RN, PhD, Griffith University, Brisbane Australia; Andrea Marshall, RN, PhD, University of Sydney, Sydney, Australia; Patricia Howard, RN, PhD, University of Kentucky; Valerie Rose, BS, University of Washington
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trials Registration: NCT00734760
All authors have no real or potential conflicts of interest, including financial interests and relationships and affiliations relevant to the subject of this manuscript.
Contributor Information
Lynn V. Doering, University of California, Los Angeles Los Angeles, Ca..
Debra K. Moser, University of Kentucky, Lexington, Ca..
Barbara Riegel, University of Pennsylvania, Philadelphia, Pa..
Sharon McKinley, University of Technology, Sydney, Australia.
Patricia Davidson, Curtin University of Technology, Sydney, Australia.
Heather Baker, University of Auckland, Auckland, New Zealand.
Hendrika Meischke, University of Washington, Seattle, Washington.
Kathleen Dracup, University of California, San Francisco, San Francisco, Ca..
Reference List
- 1.Frasure-Smith N, Lesperance F, Juneau M, Talajic M, Bourassa MG. Gender, Depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61(1):26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bankier B, Januzzi JL, Littman AB. The high prevalence of multiple psychiatric disorders in stable outpatients with coronary heart disease. Psychosom Med. 2004;66(5):645–650. doi: 10.1097/01.psy.0000138126.90551.62. [DOI] [PubMed] [Google Scholar]
- 3.Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychology. 2002;7:11–21. doi: 10.1348/135910702169321. [DOI] [PubMed] [Google Scholar]
- 4.Krantz DS, McCeney MK. Effects of psychological and social factors on organic disease: A Critical Assessment of Research on Coronary Heart Disease*. Ann Rev Psychology. 2002;53(1):341–369. doi: 10.1146/annurev.psych.53.100901.135208. [DOI] [PubMed] [Google Scholar]
- 5.Todaro J, Shen B, Raffa S, Tilkemeier P, Niaura R. Prevalence of anxiety disorders in men and women with established coronary heart disease. J Cardiopulm Rehabil Prev. 2007;27(2):89–91. doi: 10.1097/01.HCR.0000265036.24157.e7. [DOI] [PubMed] [Google Scholar]
- 6.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 7.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 8.Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry. 2003;54(3):241–247. doi: 10.1016/s0006-3223(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 9.Empana JP, Jouven X, Lemaitre RN, et al. Clinical depression and risk of out-of-hospital cardiac arrest. Arch Intern Med. 2006;166(2):195–200. doi: 10.1001/archinte.166.2.195. [DOI] [PubMed] [Google Scholar]
- 10.Grace SL, Abbey SE, Kapral MK, Fang J, Nolan RP, Stewart DE. Effect of depression on five-year mortality after an acute coronary syndrome. Am J Cardiol. 2005;96(9):1179–1185. doi: 10.1016/j.amjcard.2005.06.052. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen SS, Denollet J, Spindler H, et al. Anxiety enhances the detrimental effect of depressive symptoms on health status following percutaneous coronary intervention. J Psychosom Res. 2006;61(6):783–789. doi: 10.1016/j.jpsychores.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Shibeshi WA, Young-Xu Y, Blatt CM. Anxiety worsens prognosis in patients with coronary artery disease. J Am Coll Cardiol. 2007;49(20):2021–2027. doi: 10.1016/j.jacc.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Dickens CM, McGowan L, Percival C, et al. Contribution of depression and anxiety to impaired health-related quality of life following first myocardial infarction. Br J Psychiatry. 2006;189(4):367–372. doi: 10.1192/bjp.bp.105.018234. [DOI] [PubMed] [Google Scholar]
- 14.Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc. 2006;106 (5_suppl_2):S9–S14. [PubMed] [Google Scholar]
- 16.Walke LM, Byers AL, Gallo WT, Endrass J, Fried TR. The association of symptoms with health outcomes in chronically ill adults. J Pain Symptom Management. 2007;33(1):58–66. doi: 10.1016/j.jpainsymman.2006.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Strik JJMH, Denollet J, Lousberg R, Honig A. Comparing symptoms of depression and anxiety as predictors of cardiac events and increased health care consumption after myocardial infarction. J Am Coll Cardiol. 2003;42(10):1801–1807. doi: 10.1016/j.jacc.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006;21(3):186–193. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Zuckerman M, Lubin B, Robins s. Validation of the multiple affect adjective checklist in clinical situations. J Consult Clin Psychol. 1965;29(6):594. doi: 10.1037/h0022750. [DOI] [PubMed] [Google Scholar]
- 20.Zuckerman M, Lubin B, Rinck C. Construction of new scales for the multiple affect adjective checklist. J Behav Assess. 1983;5(2):119–129. [Google Scholar]
- 21.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychosom Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 22.Denollet J, Strik JJ, Lousberg R, Honig A. Recognizing increased risk of depressive comorbidity after myocardial infarction: Looking for 4 symptoms of anxiety-depression. Psychother Psychosom. 2006;75(6):346–352. doi: 10.1159/000095440. [DOI] [PubMed] [Google Scholar]
- 23.Rothenbacher D, Hahmann H, Wusten B, Koenig W, Brenner H. Symptoms of anxiety and depression in patients with stable coronary heart disease: prognostic value and consideration of pathogenetic links. Eur J Cardiovasc Prev Rehabil. 2007;14(4):547–554. doi: 10.1097/HJR.0b013e3280142a02. [DOI] [PubMed] [Google Scholar]
- 24.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart Ddsease. Psychosom Med. 2007;69(8):748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 25.Ormel J, Von KM, Burger H, et al. Mental disorders among persons with heart disease - results from World Mental Health surveys. Gen Hosp Psychiatry. 2007;29(4):325–334. doi: 10.1016/j.genhosppsych.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lichtman JH, Bigger JT, Jr, Blumenthal JA, et al. Depression and coronary heart disease: Recommendations for screening, referral, and treatment: A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation. 2008;118(17):1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 27.Frasure-Smith N, Lesperance F. Depression and other psychological risks following myocardial infarction. Arch Gen Psychiatry. 2003;60(6):627–636. doi: 10.1001/archpsyc.60.6.627. [DOI] [PubMed] [Google Scholar]
- 28.Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-Year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry. 2008;65(1):62–71. doi: 10.1001/archgenpsychiatry.2007.4. [DOI] [PubMed] [Google Scholar]
- 29.Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- 30.Reynolds SL, Haley WE, Kozlenki N. The impact of depressive symptoms and chronic diseases on active life expectancy in older Americans. Am Journal Geriatr Psychiatry. 2008;16(5):425–432. doi: 10.1097/JGP.0b013e31816ff32e. [DOI] [PubMed] [Google Scholar]
- 31.Grace SL, Abbey SE, Irvine J, Shnek ZM, Stewart DE. Prospective examination of anxiety persistence and its relationship to cardiac symptoms and recurrent cardiac events. Psychother Psychosom. 2004;73(6):344–352. doi: 10.1159/000080387. [DOI] [PubMed] [Google Scholar]
- 32.Rieckmann N, Kronish IM, Haas D, et al. Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am Heart J. 2006;152(5):922–927. doi: 10.1016/j.ahj.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Richardson LK, Egede LE, Mueller M. Effect of race/ethnicity and persistent recognition of depression on mortality in elderly men With Type 2 Diabetes and depression. Diabetes Care. 2008;31(5):880–881. doi: 10.2337/dc07-2215. [DOI] [PubMed] [Google Scholar]
- 34.Barry LC, Allore HG, Guo Z, Bruce ML, Gill TM. Higher burden of depression among older women: The effect of onset, persistence, and mortality over time. Arch Gen Psychiatry. 2008;65(2):172–178. doi: 10.1001/archgenpsychiatry.2007.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thombs BD, Ziegelstein RC, Stewart DE, Abbey SE, Parakh K, Grace SL. Usefulness of persistent symptoms of depression to predict physical health status 12 months after an acute coronary syndrome. Am J Cardiol. 2008;101(1):15–19. doi: 10.1016/j.amjcard.2007.07.043. [DOI] [PubMed] [Google Scholar]
- 36.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom Med. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 37.Dafer R, Rao M, Shareef A, Sharma A. Poststroke depression. Topics Stroke Rehabilitation. 2008;15(1):13–21. doi: 10.1310/tsr1501-13. [DOI] [PubMed] [Google Scholar]
- 38.Egede LE, Nietert PJ, Zheng D. Depression and all-Cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28(6):1339–1345. doi: 10.2337/diacare.28.6.1339. [DOI] [PubMed] [Google Scholar]
- 39.Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Circulation. 2000;102(15):1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 40.Goyal TM, Idler E, Krause TJ, Contrada RJ. Quality of life following cardiac surgery: Impact of the serverity and course of depressive symptoms. Psychosom Med. 2005;67:759–765. doi: 10.1097/01.psy.0000174046.40566.80. [DOI] [PubMed] [Google Scholar]
- 41.Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111(3):271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 42.Roy-Byrne PP, Davidson KW, Kessler RC, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30(3):208–225. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 43.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 44.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131(2):260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- 45.Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rumsfeld JS, Ho PM. Depression and cardiovascular disease: A call for recognition. Circulation. 2005;111:250–253. doi: 10.1161/01.CIR.0000154573.62822.89. [DOI] [PubMed] [Google Scholar]
- 47.van Melle JP, de JP, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66(6):814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 48.Baldwin DS, Anderson IM, Nutt DJ, et al. Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2005;19(6):567–596. doi: 10.1177/0269881105059253. [DOI] [PubMed] [Google Scholar]
- 49.Wisniewski SR, Fava M, Trivedi MH, et al. Acceptability of second-step treatments to depressed outpatients: a STAR*D report. Am J Psychiatry. 2007;164(5):753–760. doi: 10.1176/ajp.2007.164.5.753. [DOI] [PubMed] [Google Scholar]
- 50.Coats AJ. Ethical authorship and publishing. Int J Cardiol. 2009;131:149–150. doi: 10.1016/j.ijcard.2008.11.048. [DOI] [PubMed] [Google Scholar]