Abstract
Although cardiovascular disease (CVD) has always been perceived as a pathology regarding essentially males, incidence and death from cardiovascular events dramatically increase after menopause in women. Obviously, while many aspects of CVD are similar in both sexes, it is now clear that there are significant differences as well. Exploration of these gender-related differences in CVD might provide a basis for the development of new strategies in the management of patients with CVD from a gender point of view. In particular, a growing amount of data suggested the possible major role of oxidative stress in female patients and the possibility to integrate this new biomarker in future study evaluating CVD risk in women.
Keywords: Cardiovascular, Risk factors, Menopause, Gender, Women, Oxidative stress
INTRODUCTION
It is well known that coronary heart disease (CHD) represents the main cause of mortality and morbidity for men but also for women over age 50 years[1]. However, it has been essentially conceived as a “man’s disease”, and the influence of gender on CHD has been misunderstood and underestimated. Really, mortality due to CHD has not decreased in women as it has in men in the last 20 years, with most women dying suddenly from cardiovascular disease (CVD) without previous symptoms, but with a high prevalence of risk factors for CHD[2].
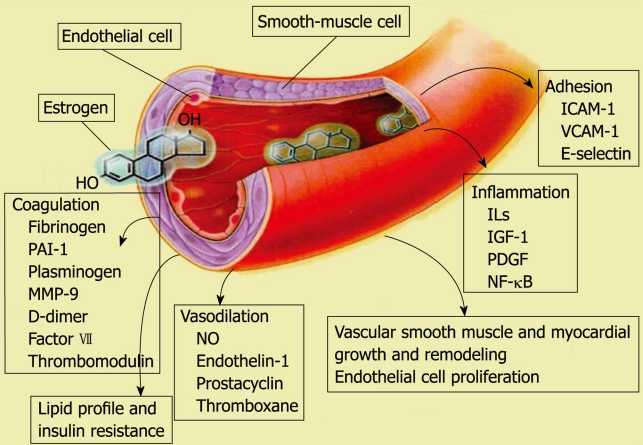
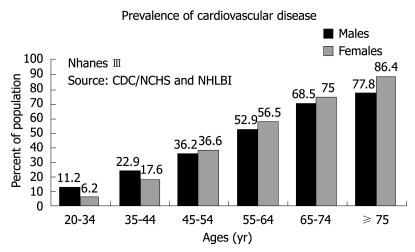
Generally, the risk for women is misperceived because of the strong conviction that females are “protected” against CVD. This conviction rises from the fact that women are effectively at lower risk of cardiovascular events with respect to men during their first decades of life, being protected by estrogen action in their premenopausal life (Figure 1). However, the onset of menopause marks a crucial point in the woman with important implications also for the cardiovascular system. It is well known that the incidence of CVD is significantly higher in postmenopausal women when compared to those in the same age range who are still fertile[3]. To note, life expectancy for women is greatly increased, and women spend up to one third of their life in their menopause status. Thus, according to the increased possibility of experiencing cardiovascular events, which rapidly rises after the menopause, the advantage gap for women becomes progressively smaller until it is overcome by that of men in advanced age (Figure 2)[2,4].
Figure 1.
Multiple effects of estrogen on the cardiovascular system. Available from: URL: http://www.ehealthspan.com.
Figure 2.
Prevalence of cardiovascular disease in males and females during their lifespan. From: Nhanes III: 1999-2002. Source: Center for Disease Control (CDC)/National Center for Health Statistics (NCHS), National Heart, Lung and Blood Institute (NHLBI).
Aspects related to pathogenesis, clinical presentation and outcome of the CHD have not been as extensively studied in women as in men. For a long time, the percentage of women included in CVD trials was always too low[5]. Consequently, most current indications for the prevention, diagnosis and therapy are deduced from cohort trials essentially conducted in men, and often result in inappropriate treatment.
However, the deepening of these issues is of particular interest because much evidence indicated that elderly women have even higher mortality and morbidity than men after cardiovascular events. Interestingly, some recent trials on the prevalence of normal or nonobstructive coronary arteries by gender assessed by early angiography after an acute coronary event showed a 20% or greater excess of normal or nonobstructive arteries in women vs men[6]. The women with nonobstructive coronary artery disease appeared to have an even higher rate of subsequent adverse events, as indicated by the Women’s Ischemia Syndrome Evaluation study[7].
Obviously, if many aspects of CVD are similar in both men and women, some differences concerning physiopathology, risk profile, symptoms, age of onset and response to medical treatments are emerging[8]. These differences demonstrate the need of more attention by physicians to address gender disparities[9]. Thus, new insights into women’s cardiovascular physiopathology are essential in order to assess more accurately and target more specific prevention strategies to reduce CHD risk in female subjects, as well as in men.
GENDER DIFFERENCES AND CARDIOVASCULAR RISK FACTORS
The studies focused on the possible gender-related role of different cardiovascular (CV) risk factors, have shown important differences (Table 1)[8]. Naturally, hormonal status represents a specific and unique risk factor for women. Moreover, in addition to traditional risk factors, cardio-metabolic risk is an important determinant in women[10]. It is known from examining the lipid profile that total cholesterol, triglycerides, low-density lipoprotein (LDL) and lipoprotein [Lp(a)] increase sharply within 6 mo of menopause onset, while high-density lipoprotein (HDL) gradually declines[10]. However, HDL-C is always significantly higher in women than in men; this may be considered a gender-specific protective factor[10]. Nonetheless, it has been determined that low HDL-C, rather than high total and LDL-C, represented a more important predictor of CHD in women[10].
Table 1.
Risk factors for cardiovascular disease in men and women
| Risk factor | Men | Women |
| Total cholesterol | +++ | +++ |
| LDL | +++ | +++ |
| HDL | ++ | +++ |
| Triglycerides | + | ++ |
| Apo A-I | +++ | +++ |
| Apo B | +++ | +++ |
| Apo (a) | ++ | +(+) |
| Smoking | ++ | ++(+) |
| Diabetes | ++ | +++ |
| Body mass index | ++ | ++ |
| WHR | +++ | +++ |
| Hypertension | ++ | ++ |
| Family history | ++ | ++(+) |
| Hormones | +++ | |
| Homocysteine | + | + |
| Fibrinogen | ++ | ++ |
| Inflammation (PCR) | + | ++ |
| Psychosocial factors | + | + |
Modified from Ref. 8.
Other gender-related differences emerged in a meta-analysis of 17 studies (including 46 000 men and 11 000 women), which indicated elevated triglycerides as a greater predictor of CV events for women than for men, even after adjustment for HDL-C and other risk factors[11]. Moreover, high levels of Lp(a)were associated with increased CV risk, particularly in women with high levels of LDL-C[12].
Among the inflammatory biomarkers, the addition of C-reactive protein to the Framingham risk score improved the global CV risk prediction in women, especially in those at low-to-intermediate risk[13].
THE ROLE OF OXIDATIVE STRESS FOR CV RISK IN WOMEN
Many risk factors that promote CVD have been identified, including hypertension, hypercholesterolemia, diabetes, decreased estrogen in post-menopausal women, increased homocysteine, and cigarette smoking[14]. A mechanism common to all these risk factors is the elevation of the oxidative stress status[15]. In particular, oxidative stress phenomena occur during the progressive step that characterizes an atherosclerotic lesion from the onset, during its development until the events that induce clinical manifestation of the CVD[15]. Consequently, oxidative stress biomarkers have been found by us and others to be associated with the presence and severity of the CVD, and to the presence and number of risk factors[16,17]. However, few studies evaluating the risk of CVD in women also included markers of oxidative stress[18].
It is known that young women during their fertile life are at lower risk of cardiovascular events compared with men, being protected by estrogen action and that oxidative stress is generally higher in men than in premenopausal women[19,20]. However, after menopause the risk of experiencing cardiovascular events rapidly rises in women, in conjunction with a parallel increase in oxidative stress biomarkers[19,21,22]. Recent data showed higher levels of biomarkers of inflammation and higher oxidative stress levels in elderly women than in elderly men[23]. Oxidative stress has been found elevated in post-menopausal women when compared to pre-menopausal women, and recent data has shown that oxidative stress plays a major role in different conditions which often accompany menopause, such as hot flashes and osteoporosis[24-26]. Moreover, although oxidative stress results are lower in females compared to males during the first decades of life, this difference decreases until the age range which corresponds to the onset of menopause for women, while for elderly people the tendency is even inverted[27].
Although many in vitro data showed the antioxidant properties of estradiol, the role of hormone replacement therapy (HRT) on oxidative stress levels remains still to be demonstrated[28]. However, most of the studies suggested possible beneficial effects or lack of adverse consequences of different doses and formulations of estradiol on the oxidative status in postmenopausal women treated with HRT[29,30]. Nonetheless, future studies are needed in this field to better clarify the role of different HRT regimens and doses on the oxidative stress balance.
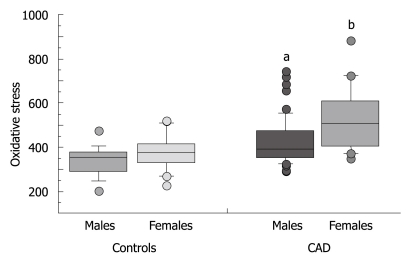
Interestingly, data conducted in patients with neurodegenerative disease showed that female patients presented with higher levels of oxidative stress compared to affected males, suggesting a higher susceptibility to oxidative injury in such female subjects[31,32]. However, there is a dearth of reliable information on oxidative stress in women in the field of CVD[18]. We have recently evaluated whether gender-related differences in oxidative stress levels in aged patients with coronary artery disease (CAD) exist. Data obtained showed a higher oxidative stress status in elderly women with respect to men, whereas elevated oxidative stress levels represented the only strong independent risk factor for CAD in elderly women (Figure 3)[33]. At the moment, molecular mechanisms for the overwhelming gender disparity concerning oxidative stress in CAD are unknown, but they are probably related to hormonal status and likely associated with the loss of estrogen-dependent antioxidant effects[34,35]. Nonetheless, the estimation and correction of levels of oxidative stress might represent a crucial issue in elderly female patients.
Figure 3.
Levels of an oxidative stress biomarker by coronary artery disease (CAD) and gender. Modified from: Vassalle C, Maffei S, Boni C, Zucchelli GC. Gender-related differences in oxidative stress levels among elderly patients with coronary artery disease. Fertil Steril 2008; 89: 608-613. aP < 0.05 vs males; bP < 0.001 vs both control groups (males and females).
With regard to antioxidant vitamin supplementation to prevent CVD, actual guidelines did not recommend its use although folic acid supplementation is advised for high-risk women with high levels of homocysteine[36,37]. Moreover, two recent trials (Norwegian Vitamin and Heart Outcomes Prevention Evaluation 2) have demonstrated the lack of efficacy of combined supplementation of folic acid and vitamins B12 and B6 in preventing CVD[38,39]. Conversely, data from the Women’s Health Study suggested that vitamin E failed to provide benefits for either major CV events or myocardial infarction except in women > 65 years of age, where it significantly reduced the risk of major CV events[40].
CONCLUSION
Emerging data have suggested significant gender-based differences in CVD. In particular, menopausal status appears to enhance the development of CVD through several unfavourable changes in metabolism and hemodynamic parameters. Exploration of these aspects of CVD will provide a basis for clinical strategies directed to improve the outcome for women and consequently lead to the discovery and adaptation of different approaches to prevention, diagnosis and management of CVD in women when appropriate.
In particular, recent data on the role of oxidative stress suggested that the estimation of oxidative stress, central to cardiovascular physiopathology, could represent a useful biomarker for cardiovascular risk estimation particularly relevant in elderly female subjects.
Footnotes
Peer reviewers: Antigone Lazou, Professor of Physiology, Lab of Animal Physiology, Sch of Biology, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece; Veselin Mitrovic, MD, Professor, Department of Cardiology, Kerckhoff-Klinik GmbH, Benekestrasse 2-8, 61231 Bad Nauheim, Germany
S- Editor Wang JL L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Stramba-Badiale M, Fox KM, Priori SG, Collins P, Daly C, Graham I, Jonsson B, Schenck-Gustafsson K, Tendera M. Cardiovascular diseases in women: a statement from the policy conference of the European Society of Cardiology. Eur Heart J. 2006;27:994–1005. doi: 10.1093/eurheartj/ehi819. [DOI] [PubMed] [Google Scholar]
- 2.Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O'Donnell C, Kittner S, et al. Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 3.Gordon T, Kannel WB, Hjortland MC, McNamara PM. Menopause and coronary heart disease. The Framingham Study. Ann Intern Med. 1978;89:157–161. doi: 10.7326/0003-4819-89-2-157. [DOI] [PubMed] [Google Scholar]
- 4.Oparil S. Arthur C. Corcoran Memorial Lecture. Hormones and vasoprotection. Hypertension. 1999;33:170–176. doi: 10.1161/01.hyp.33.1.170. [DOI] [PubMed] [Google Scholar]
- 5.Harris DJ, Douglas PS. Enrollment of women in cardiovascular clinical trials funded by the National Heart, Lung, and Blood Institute. N Engl J Med. 2000;343:475–480. doi: 10.1056/NEJM200008173430706. [DOI] [PubMed] [Google Scholar]
- 6.Anderson RD, Pepine CJ. Gender differences in the treatment for acute myocardial infarction: bias or biology? Circulation. 2007;115:823–826. doi: 10.1161/CIRCULATIONAHA.106.685859. [DOI] [PubMed] [Google Scholar]
- 7.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Pepine CJ, Mankad S, Sharaf BL, et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study: Part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47:S21–S29. doi: 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 8.Roeters van Lennep JE, Westerveld HT, Erkelens DW, van der Wall EE. Risk factors for coronary heart disease: implications of gender. Cardiovasc Res. 2002;53:538–549. doi: 10.1016/s0008-6363(01)00388-1. [DOI] [PubMed] [Google Scholar]
- 9.Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Fabunmi RP, Kwan J, Mills T, Simpson SL. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 10.Rosano GM, Maffei S, Andreassi MG, Vitale C, Vassalle C, Gambacciani M, Stramba-Badiale M, Mercuro G. Hormone replacement therapy and cardioprotection: a new dawn? A statement of the Study Group on Cardiovascular Disease in Women of the Italian Society of Cardiology on hormone replacement therapy in postmenopausal women. J Cardiovasc Med (Hagerstown) 2009;10:85–92. doi: 10.2459/JCM.0b013e328313e979. [DOI] [PubMed] [Google Scholar]
- 11.Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996;3:213–219. [PubMed] [Google Scholar]
- 12.Suk Danik J, Rifai N, Buring JE, Ridker PM. Lipoprotein(a), measured with an assay independent of apolipoprotein(a) isoform size, and risk of future cardiovascular events among initially healthy women. JAMA. 2006;296:1363–1370. doi: 10.1001/jama.296.11.1363. [DOI] [PubMed] [Google Scholar]
- 13.Cook NR, Buring JE, Ridker PM. The effect of including C-reactive protein in cardiovascular risk prediction models for women. Ann Intern Med. 2006;145:21–29. doi: 10.7326/0003-4819-145-1-200607040-00128. [DOI] [PubMed] [Google Scholar]
- 14.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, Ganiats TG, Gomes AS, Gornik HL, Gracia C, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481–501. doi: 10.1161/CIRCULATIONAHA.107.181546. [DOI] [PubMed] [Google Scholar]
- 15.Fearon IM, Faux SP. Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol. 2009;47:372–381. doi: 10.1016/j.yjmcc.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Vassalle C, Petrozzi L, Botto N, Andreassi MG, Zucchelli GC. Oxidative stress and its association with coronary artery disease and different atherogenic risk factors. J Intern Med. 2004;256:308–315. doi: 10.1111/j.1365-2796.2004.01373.x. [DOI] [PubMed] [Google Scholar]
- 17.Schwedhelm E, Bartling A, Lenzen H, Tsikas D, Maas R, Brümmer J, Gutzki FM, Berger J, Frölich JC, Böger RH. Urinary 8-iso-prostaglandin F2alpha as a risk marker in patients with coronary heart disease: a matched case-control study. Circulation. 2004;109:843–848. doi: 10.1161/01.CIR.0000116761.93647.30. [DOI] [PubMed] [Google Scholar]
- 18.Quyyumi AA. Women and ischemic heart disease: pathophysiologic implications from the Women's Ischemia Syndrome Evaluation (WISE) Study and future research steps. J Am Coll Cardiol. 2006;47:S66–S71. doi: 10.1016/j.jacc.2004.11.075. [DOI] [PubMed] [Google Scholar]
- 19.Baker L, Meldrum KK, Wang M, Sankula R, Vanam R, Raiesdana A, Tsai B, Hile K, Brown JW, Meldrum DR. The role of estrogen in cardiovascular disease. J Surg Res. 2003;115:325–344. doi: 10.1016/s0022-4804(03)00215-4. [DOI] [PubMed] [Google Scholar]
- 20.Rossouw JE. Hormones, genetic factors, and gender differences in cardiovascular disease. Cardiovasc Res. 2002;53:550–557. doi: 10.1016/s0008-6363(01)00478-3. [DOI] [PubMed] [Google Scholar]
- 21.Gebara OC, Mittleman MA, Sutherland P, Lipinska I, Matheney T, Xu P, Welty FK, Wilson PW, Levy D, Muller JE. Association between increased estrogen status and increased fibrinolytic potential in the Framingham Offspring Study. Circulation. 1995;91:1952–1958. doi: 10.1161/01.cir.91.7.1952. [DOI] [PubMed] [Google Scholar]
- 22.Gierach GL, Johnson BD, Bairey Merz CN, Kelsey SF, Bittner V, Olson MB, Shaw LJ, Mankad S, Pepine CJ, Reis SE, et al. Hypertension, menopause, and coronary artery disease risk in the Women's Ischemia Syndrome Evaluation (WISE) Study. J Am Coll Cardiol. 2006;47:S50–S58. doi: 10.1016/j.jacc.2005.02.099. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal A, Lourenço EV, Gupta S, La Cava A. Gender-Based Differences in Leptinemia in Healthy Aging, Non-obese Individuals Associate with Increased Marker of Oxidative Stress. Int J Clin Exp Med. 2008;1:305–309. [PMC free article] [PubMed] [Google Scholar]
- 24.Leal M, Díaz J, Serrano E, Abellán J, Carbonell LF. Hormone replacement therapy for oxidative stress in postmenopausal women with hot flushes. Obstet Gynecol. 2000;95:804–809. doi: 10.1016/s0029-7844(00)00822-x. [DOI] [PubMed] [Google Scholar]
- 25.Altindag O, Erel O, Soran N, Celik H, Selek S. Total oxidative/anti-oxidative status and relation to bone mineral density in osteoporosis. Rheumatol Int. 2008;28:317–321. doi: 10.1007/s00296-007-0452-0. [DOI] [PubMed] [Google Scholar]
- 26.Grassi F, Tell G, Robbie-Ryan M, Gao Y, Terauchi M, Yang X, Romanello M, Jones DP, Weitzmann MN, Pacifici R. Oxidative stress causes bone loss in estrogen-deficient mice through enhanced bone marrow dendritic cell activation. Proc Natl Acad Sci USA. 2007;104:15087–15092. doi: 10.1073/pnas.0703610104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miquel J, Ramirez-Boscá A, Soler A, Díez A, Carrión-Gutiérrez MA, Díaz-Alperi J, Quintanilla-Ripoll E, Bernd A, Quintanilla-Almagro E. Increase with age of serum lipid peroxides: implications for the prevention of atherosclerosis. Mech Ageing Dev. 1998;100:17–24. doi: 10.1016/s0047-6374(97)00118-8. [DOI] [PubMed] [Google Scholar]
- 28.Strehlow K, Rotter S, Wassmann S, Adam O, Grohé C, Laufs K, Böhm M, Nickenig G. Modulation of antioxidant enzyme expression and function by estrogen. Circ Res. 2003;93:170–177. doi: 10.1161/01.RES.0000082334.17947.11. [DOI] [PubMed] [Google Scholar]
- 29.Maffei S, Mercuri A, Prontera C, Zucchelli GC, Vassalle C. Vasoactive biomarkers and oxidative stress in healthy recently postmenopausal women treated with hormone replacement therapy. Climacteric. 2006;9:452–458. doi: 10.1080/13697130601014752. [DOI] [PubMed] [Google Scholar]
- 30.Unfer TC, Conterato GM, da Silva JC, Duarte MM, Emanuelli T. Influence of hormone replacement therapy on blood antioxidant enzymes in menopausal women. Clin Chim Acta. 2006;369:73–77. doi: 10.1016/j.cca.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Kikuchi A, Takeda A, Onodera H, Kimpara T, Hisanaga K, Sato N, Nunomura A, Castellani RJ, Perry G, Smith MA, et al. Systemic increase of oxidative nucleic acid damage in Parkinson's disease and multiple system atrophy. Neurobiol Dis. 2002;9:244–248. doi: 10.1006/nbdi.2002.0466. [DOI] [PubMed] [Google Scholar]
- 32.Schuessel K, Leutner S, Cairns NJ, Müller WE, Eckert A. Impact of gender on upregulation of antioxidant defence mechanisms in Alzheimer's disease brain. J Neural Transm. 2004;111:1167–1182. doi: 10.1007/s00702-004-0156-5. [DOI] [PubMed] [Google Scholar]
- 33.Vassalle C, Maffei S, Boni C, Zucchelli GC. Gender-related differences in oxidative stress levels among elderly patients with coronary artery disease. Fertil Steril. 2008;89:608–613. doi: 10.1016/j.fertnstert.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 34.Shwaery GT, Vita JA, Keaney JF Jr. Antioxidant protection of LDL by physiologic concentrations of estrogens is specific for 17-beta-estradiol. Atherosclerosis. 1998;138:255–262. doi: 10.1016/s0021-9150(98)00020-3. [DOI] [PubMed] [Google Scholar]
- 35.Huang M, Li J, Teoh H, Man RY. Low concentrations of 17beta-estradiol reduce oxidative modification of low-density lipoproteins in the presence of vitamin C and vitamin E. Free Radic Biol Med. 1999;27:438–441. doi: 10.1016/s0891-5849(99)00086-6. [DOI] [PubMed] [Google Scholar]
- 36.Davey Smith G, Ebrahim S. Folate supplementation and cardiovascular disease. Lancet. 2005;366:1679–1681. doi: 10.1016/S0140-6736(05)67676-3. [DOI] [PubMed] [Google Scholar]
- 37.Bazzano LA, Reynolds K, Holder KN, He J. Effect of folic acid supplementation on risk of cardiovascular diseases: a meta-analysis of randomized controlled trials. JAMA. 2006;296:2720–2726. doi: 10.1001/jama.296.22.2720. [DOI] [PubMed] [Google Scholar]
- 38.Bønaa KH, Njølstad I, Ueland PM, Schirmer H, Tverdal A, Steigen T, Wang H, Nordrehaug JE, Arnesen E, Rasmussen K. Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006;354:1578–1588. doi: 10.1056/NEJMoa055227. [DOI] [PubMed] [Google Scholar]
- 39.Lonn E, Yusuf S, Arnold MJ, Sheridan P, Pogue J, Micks M, McQueen MJ, Probstfield J, Fodor G, Held C, et al. Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med. 2006;354:1567–1577. doi: 10.1056/NEJMoa060900. [DOI] [PubMed] [Google Scholar]
- 40.Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women's Health Study: a randomized controlled trial. JAMA. 2005;294:56–65. doi: 10.1001/jama.294.1.56. [DOI] [PubMed] [Google Scholar]