Abstract
Background
Nonspecific spinal pain (NSP), comprising back and/or neck pain, is one of the leading disorders behind long-term sick-listing, including disability pensions. Early interventions to prevent long-term sick-listing require the identification of patients at risk. The aim of this study was to compare living conditions associated with long-term sick-listing for NSP in patients with nonacute NSP, with a nonpatient population-based sample. Nonacute NSP is pain that leads to full-time sick-listing >3 weeks.
Methods
One hundred and twenty-five patients with nonacute NSP, 2000–2004, were included in a randomized controlled trial in Stockholm County with the objective of comparing cognitive–behavioral rehabilitation with traditional primary care. For these patients, a cross-sectional study was carried out with baseline data. Living conditions were compared between the patients and 338 nonpatients by logistic regression. The conditions from univariate analyses were included in a multivariate analysis. The nonsignificant variables were excluded sequentially to yield a model comprising only the significant factors (P < 0.05). The results are shown as odds ratios (OR) with 95% confidence intervals.
Results
In the univariate analyses, 13 of the 18 living conditions had higher odds for the patients with a dominance of physical work strains and Indication of alcohol over-consumption, odds ratio (OR) 14.8 (95% confidence interval [CI] 3.2–67.6). Five conditions qualified for the multivariate model: High physical workload, OR 13.7 (CI 5.9–32.2); Hectic work tempo, OR 8.4 (CI 2.5–28.3); Blue-collar job, OR 4.5 (CI 1.8–11.4); Obesity, OR 3.5 (CI 1.2–10.2); and Low education, OR 2.7 (CI 1.1–6.8).
Conclusions
As most of the living conditions have previously been insufficiently studied, our findings might contribute a wider knowledge of risk factors for long-term sick-listing for NSP. As the cross-sectional design makes causal conclusions impossible, our study should be complemented by prospective research.
Keywords: nonspecific spinal pain, back pain, neck pain, long-term sick-listing, populationbased sample, cross-sectional study
Introduction
Since the late 1990s, the industrial world, particularly Sweden, has seen a substantial growth of sick-listing, especially on a long-term basis, including disability pensions. In 2007, despite a slight decrease since 2004, 11% of Swedes of working age were sick-listed versus 6% in comparable countries.1 Up to and including 2004, musculoskeletal disorders, dominated by spinal pain, comprising back and/or neck pain, formed the largest diagnostic group behind disability pensions in Sweden. Following international trends, it was outflanked from 2005 by mental disorders.2 Nevertheless, despite this relative decrease, recent data indicate a continued increase in the total cost to society of spinal pain.3 The vast majority of cases concern nonspecific spinal pain (NSP) and present a task for primary care.4
Clinical guidelines emphasize the necessity of early intervention to prevent long-term sick-listing caused by NSP,4 requiring the identification of patients at risk. Socioeconomic and medical factors are associated both with the onset of acute NSP and the progression to nonacute NSP.5–8 Acute and nonacute NSP is pain that leads to full-time sick-listing for ≤3 weeks and >3 weeks, respectively.9 However, research within the area has been seriously limited with, eg, an under-representation of women.10
Sweden has a unique tradition of keeping population statistics, going back as far as 1749.11 Since 1975 extensive annual surveys of living conditions, including life-style, have been conducted on large random samples representing Sweden as a whole as well as local districts.12 This provides an exceptional opportunity for epidemiological research. However, we have found no previous study in which primarycare patients with nonacute NSP were compared with a population-based sample.
The aim of this study was to compare living conditions associated with long-term sick-listing for NSP in patients with nonacute NSP, with a nonpatient population-based sample.
Methods
The study was approved by the local ethics committee at Karolinska University Hospital, Huddinge, Sweden.
Setting and source population
The study area was the Southern part of Stockholm County, including 5 urban districts (Enskede-Årsta-Vantör, Farsta, Älvsjö, Skarpnäck, and Hägersten-Liljeholmen) and 4 semi-urban districts (Huddinge, Nynäshamn, Tyresö, and Haninge). The number of inhabitants (31 December 2001) in the county totalled about 1,830,000, of whom 1,100,100 were of the same age as the patients studied (18–59 years). The study area had about 467,000 inhabitants, of whom 281,000 were aged 18 to 59 years and constituted the source population. A detailed description of the distribution of the inhabitants between the districts is shown in Table 1.
Table 1.
Distribution of inhabitants and patients between the study districts (ranking by the number of patients)
| Districts (inhabitants; total 467,298a) | Inhabitants aged 18–59 years (%) |
Patients (%) |
||
|---|---|---|---|---|
| Frequency | Cumulative frequency | Frequency | Cumulative frequency | |
| Huddinge (85,700) | 50,430 (18.0) | 50,430 (18.0) | 37 (29.6) | 37 (29.6) |
| Nynäshamn (24,332) | 13,523 (4.8) | 63,953 (22.8) | 36 (28.8) | 73 (58.4) |
| Tyresö (39,434) | 22,454 (8.0) | 86,407 (30.8) | 26 (20.8) | 99 (79.2) |
| Enskede-Årsta-Vantör (80,984) | 49,562 (17.7)b | 135,969 (48.5) | 11 (8.8) | 110 (88.0) |
| Haninge (70,432) | 42,487 (15.1) | 178,456 (63.6) | 5 (4.0) | 115 (92.0) |
| Farsta (45,597) | 26,211 (9.3)b | 204,667 (72.9) | 3 (2.4) | 118 (94.4) |
| Älvsjö (20,786) | 11,861 (4.2)b | 216,528 (77.2) | 3 (2.4) | 121 (96.8) |
| Skarpnäck (40,060) | 24,979 (8.9)b | 241,507 (86.1) | 3 (2.4) | 124 (99.2) |
| Hägersten-Liljeholmen (59,973) | 39,118 (13.9)b | 280,625 (100.0) | 1 (0.8) | 125 (100.0) |
Notes: 31 December 2001;
For age group 20–64 years (data for age group 18–59 years were not available).
Patients
One hundred and twenty-five patients with nonacute NSP, between August 2000 and January 2004, were included in a randomized controlled trial, which was described in detail in a previous study.13 The patients were allocated to a multidisciplinary, cognitive–behavioral program at a rehabilitation center or continued with traditional primary care. The rehabilitation center opened in 1991 and was situated in Haninge, geographically near the middle of the study area.
The criteria for inclusion were: 1) Vocationally active, up to and including 59 years of age. 2) Sick-listed full-time for spinal pain for at least 6 weeks (42 days) and for at most 2 years (730 days). 3) Able to fill in forms. The criteria for exclusion were: 1) Temporary disability pension, or disability pension being paid or in preparation. 2) A primary need for action by a hospital specialist (eg, operation for intravertebral slipped disc). 3) Pregnancy and diseases (other than spinal pain) that would probably make rehabilitation impracticable (eg, advanced pulmonary disease). 4) Whiplash associated disorders as a primary obstacle to working. 5) Previous rehabilitation at the rehabilitation center. 6) Other multidisciplinary rehabilitation ongoing or planned.
The patients living in the study area were recruited by 41 family doctors at 13 primary-care health centers. Twelve of the centers engaged >1 family doctor, and 1 center was a 1-doctor clinic. To ensure that all the study patients, including those who were allocated to continued primary care, received a high minimum level of treatment, only permanently employed or long-term substitute doctors were engaged. The rehabilitation center was well known to the family doctors, as they had been referring patients to it for several years. The recruitment of the patients was nonsystematic, ie, dependent on the motivation and available time of the family doctor. Before randomization, the study patients met a research assistant in the health center and completed a questionnaire of baseline characteristics. A detailed description of the distribution of included patients between the family doctors is shown in Table 2, and of the distribution of the patients between the districts in Table 1. One of the 125 patients failed to complete the questionnaire and was excluded. The remaining 124 patients were included in this study.
Table 2.
Distribution of patients (n = 125) between the recruiting family doctors (n = 41) (ranking by the number of patients)
| Family doctors (%) |
Patients (%) |
||
|---|---|---|---|
| Frequency | Cumulative frequency | Frequency | Cumulative frequency |
| 1 (2.4) | 1 (2.4) | 17 (13.6) | 17 (13.6) |
| 1 (2.4) | 2 (4.9) | 16 (12.8) | 33 (26.4) |
| 1 (2.4) | 3 (7.3) | 10 (8.0) | 43 (34.4) |
| 1 (2.4) | 4 (9.8) | 8 (6.4) | 51 (40.8) |
| 1 (2.4) | 5 (12.2) | 7 (5.6) | 58 (46.4) |
| 1 (2.4) | 6 (14.6) | 5 (4.0) | 63 (50.4) |
| 4 (9.8) | 10 (24.4) | 4 (3.2) | 79 (63.2) |
| 5 (12.2) | 15 (36.6) | 3 (2.4) | 94 (75.2) |
| 5 (12.2) | 20 (48.8) | 2 (1.6) | 104 (83.2) |
| 21 (51.2) | 41 (100.0) | 1 (0.8) | 125 (100.0) |
Nonpatients
From a nationwide sample, a simple, random, local sample of 338 nonpatients was selected as a comparison group to the patients:
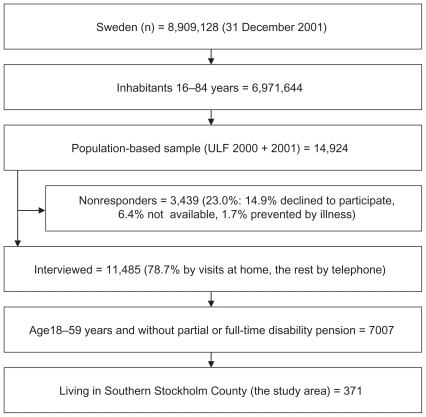
Statistics Sweden, a governmental authority, conducts The Survey of Living Conditions annually (In Swedish: Undersökningarna av levnadsförhållanden [ULF]).12,14 To reach an acceptable power, 2 years of ULF data, 2000 + 2001, were combined. Most of the patients (81/124) were recruited during that period. A flowchart of ULF is shown in Figure 1.
Figure 1.
Flowchart of the ULF (Undersökningarna av levnadsförhållanden) surveys 2000 + 2001.
ULF 2000 + 2001 was a simple, random sample of 7465 and 7459 individuals respectively, aged 16 to 84 years. They were invited to participate in an interview in their homes. Nonresponders and those who declared that they did not want to be visited were offered a telephone interview. From the interviewed individuals we selected subjects of the same age as the patients except for those with partial or total disability pensions. This resulted in a nationwide sample, of which 371 individuals were living in the home districts of the patients. By exclusion of the vocationally inactive and the full-time sick-listed subjects, a comparison group of 338 nonpatients was achieved.
Living conditions associated with long-term sick-listing for NSP
The cross-sectional design made conclusions about causes and effects impossible. For example, anxiety, depression and low physical activity could be both explanatory and responding variables for nonacute NSP.6,7 We therefore limited our analyses to living conditions that could reasonably be supposed to have existed before the start of the current sick-listing and excluded comparisons of, eg, mental distress, pain and exercise habits.
For a majority (10 out of 18) of the living conditions, the questions in the patient questionnaire and the ULF questionnaire were identical or nearly identical. For 8 living conditions, we made modifications so they were reasonably comparable. The nonidentical questions in the study and ULF, and our modifications of them, are shown in Table 3.
Table 3.
Nonidentical questions in the questionnaires of the randomized controlled trial and the ULF (Undersökningarna av levnadsförhållanden) surveys
| Living condition | The wording of the questions is shown in italics |
|
|---|---|---|
| The randomized controlled trial | ULFa | |
| High physical workload |
State work conditions that you regularly (not occasionally) have been or are exposed to. For each alternative, Yes/No: Lifting heavy things or greater muscular efforts? |
Does your work require lifting heavy things? Yes/No. (If Yes:) Are lifting heavy things required: Daily – Some time every week – More seldom (Question 124). Specification: We considered “daily” as equivalent to “regularly”. |
| Monotonous work moments |
Monotonous work movements? |
For each alternative, Yes/No: Does your work include very frequent and monotonous movements? |
| Difficult work postures | Difficult work postures (bent, twisted, locked, etc.)? | In your work, are you forced to be bent, twisted or in other ways to adopt unsuitable working postures? |
| Vibrations in work | Vibrations?47 | Are you exposed to powerful shaking or vibrations in your work? (Question 123) |
| Hectic work tempo | For each alternative, Yes, often – Yes, sometimes – No, seldom – No, practically never, 1–4: Does your work require that you work very fast? Specification:Hectic work tempo<3. |
Is your work hectic? Yes/No. For each alternative, No possibilities – Very many possibilities, 0–10: |
| Low decision latitude |
Do you have the freedom to decide … how your work should be performed? … what is to be done in your work21 Specification: Low decision latitude ≥2 in both questions. |
What possibilities do you think you have to … decide how your daily work should be performed? … influence decisions of the general direction of your work? (Question 128 b+d) Specification: Low decision latitude = <5 in both questions. |
| Indication of alcohol over-consumption |
How often do you on one and the same occasion drink half a bottle of strong spirits (bottle = 75 cl) or 2 bottles of wine or 6 tins of strong beer (= 8 bottles of 33 cl) or 12 bottles of medium-strong beer? Almost every day (at least 5 days weekly) – 3–4 times weekly – 1–2 times weekly – 2–3 times monthly – Once monthly – 1–6 times yearly – Never, 1–735 Specification: 1–4 = increased tolerance, which indicates alcohol over-consumption. This cut-off point, ie, a frequency of binge drinking of at least 2–3 times monthly, is based on a personal communication (Anders Romelsjö, 27 August 2007). |
Roughly, how often during the last 12 months have you drunk any alcoholic drinks, ie, wine, strong beer or strong spirits? Daily or almost daily (at least 5 days weekly) – 2–4 times weekly – Once weekly – 2–3 times monthly – Once monthly – 6–11 times yearly – More seldom – Never, 1–8 (Question 64 e). Roughly, how many glasses do you usually drink at those occasions? One glass could be 1 glass of wine, 1 bottle or tin of strong beer, 1 snapsbor drink: number of glasses (Question 64 f). Specification: 1–4 in question 64 e + >8 glasses in question 64 f indicate increased tolerance. |
| Comorbidity |
Except your back/neck/shoulder pain – do you have any other, current diseases? Yes/No. (If Yes:) What disease/s?: …………………………………………... |
Do you have any prolonged disease, trouble after an accident, any handicap or other frailty? Yes/No. (If Yes:) Note every trouble or disease as precisely as possible: …………..…………………………………… (Question 42–43) |
Note: The complete ULF questionnaire: http://www.scb.se/statistik/LE/LE0101/_dokument/ULF_2001.pdf
Snaps is Swedish for a little glass (often 4–6 centiliters) of pure liquor, eg, vodka.
Questions on alcohol consumption were put only to the ULF subjects of 2001, of whom 169 belonged to the nonpatients. Questions on work conditions were put exclusively to the 325 nonpatients in employment. The questions on the other living conditions were put to all nonpatients.
The 18 living conditions associated with long-term sick-listing for NSP are shown in Table 4. The rationale of the choice of conditions is shown as references in the table.
Table 4.
Living conditions – univariate analyses
| Patients (n =124) | Nonpatients (n =338) | Odds ratio | P value | |
|---|---|---|---|---|
| Woman20,48–50 | 68 (54.8 [46.0–63.7]) | 161 (47.6 [42.3–53.0]) | 1.3 [0.9–2.0] | NS |
| Older age (= ≥ 45 years)17,18 | 57 (46.0 [37.1–54.9]) | 107 (31.7 [26.7–3.6]) | 1.8 [1.2 –2.8] | 0.006 |
| Immigrant (= born outside Sweden)51 | 34 (27.4 [19.5–35.4]) | 43 (12.7 [9.2–16.3]) | 2.6 [1.6–4.4] | <0.001 |
| Single life (= living alone without children)52 | 22 (17.7 [10.9–24.6]) | 101 (29.9 [25.0–34.8]) | 0.5 [0.3–0.9] | 0.02 |
| Living with children at home52 | 69 (55.7 [46.8–64.5]) | 167 (49.4 [44.1–54.8]) | 1.3 [0.9–2.0] | NS |
| Low education (= at most junior high school)53 | 44 (35.5 [26.9–44.0]) | 41 (12.1 [8.6–15.6]) | 3.8 [2.3–6.3] | <0.001 |
| Unemployed54 | 29 (23.4 [15.8–30.9]) | 13 (3.9 [1.8–5.9]) | 8.2 [4.0–16.5] | <0.001 |
| Blue-collar joba,b,5,47 | 83 (87.4 [80.6–94.2]) | 108 (33.2 [28.1–38.4]) | 15.0 [7.7–29.1] | <0.001 |
| Physical work strainsa,47 | ||||
| High physical workload17–20 | 79 (83.2 [75.5–90.8]) | 51/325 (15.7 [11.7–19.7]) | 30.4 [15.9–58.3] | <0.001 |
| Monotonous work moments19 | 61 (64.2 [54.4–74.0]) | 134/324 (41.4 [36.0–46.7]) | 2.7 [1.7–4.3] | <0.001 |
| Difficult work postures19 | 76 (80.0 [71.8–88.2]) | 107/324 (33.0 [27.9–38.2]) | 9.0 [5.1–15.9] | <0.001 |
| Vibrations in work55 | 35 (36.8 [27.0–46.7]) | 15/324 (4.6 [2.3–6.9]) | 18.6 [8.7–39.9] | <0.001 |
| Psychosocial work strainsa,56 | ||||
| Hectic work tempo26 | 88 (92.6 [87.3–98.0]) | 239/324 (73.8 [68.9–78.6]) | 4.5 [2.0–10.1] | <0.001 |
| Low decision latitude19 | 30 (31.6 [22.1–41.1]) | 42/321 (13.1 [9.4–16.8]) | 3.2 [1.8–5.5] | <0.001 |
| Smoking (daily + not daily)17 | 49 (39.5 [30.8–48.2]) | 118/336 (35.1 [30.0–40.2]) | 1.2 [0.8–1.8] | NS |
| Indication of alcohol over-consumptionc,37 | 17 (13.7 [7.6–19.8]) | 2/164 (1.2 [−0.0–2.9]) | 14.8 [3.2–67.6] | 0.001 |
| Obesity (= BMI ≥ 3038)43 | 30 (24.2 [16.6–31.8]) | 23/332 (6.9 [4.2–9.7]) | 4.3 [2.3–7.7] | <0.001 |
| Comorbidityd,57 | 45 (36.3 [27.7–44.9]) | 105 (31.1 [26.1–36.0]) | 1.1 [0.7–1.7] | NS |
Notes: One hundred and twenty-four patients with nonacute nonspecific spinal pain (NSP) compared with 338 nonpatients by logistic regression, adjusted for gender and age. If not otherwise stated, results are shown as number (in case of missing data, the total number is also shown) with percentage in parenthesis; 95% confidence intervals within brackets.
For the subjects in employment: 95/124 patients and 325/338 nonpatients;
According to Socio-Economic Classification (In Swedish “Socioekonomisk indelning (SEI)”) [http://www.scb.se/statistik/LE/LE0101/_dokument/SEIstandard.pdf]. Modification: the subjects in the group “Entrepreneur” were included or not in Blue-collar job starting from their probable level of education;
The alcohol questions were put to 169/338 nonpatients;
Any other prolonged disease except NSP and obesity.
Outcome measure
The outcome measure was the outcome variable of logistic regression, being either a patient or a nonpatient.
Statistics
The patients were compared with the nonpatients by applying logistic regression. Stata, version 10.1 was used to analyze the data.15
We first estimated the distribution of the living conditions for the patients and the nonpatients. The results are shown as proportions (means) with 95% confidence intervals (CI). Differences between the patients and the nonpatients were evaluated by univariate-logistic regression, adjusted for gender and age.16 Two age classes were defined: Old age ≥45 years and Young age ≤44 years. The outcome (dependent) variable was the sample class, ie, patient or nonpatient. The predictive (independent) variable was the living condition. The results are presented with odds ratios (OR), 95% CI and P values.
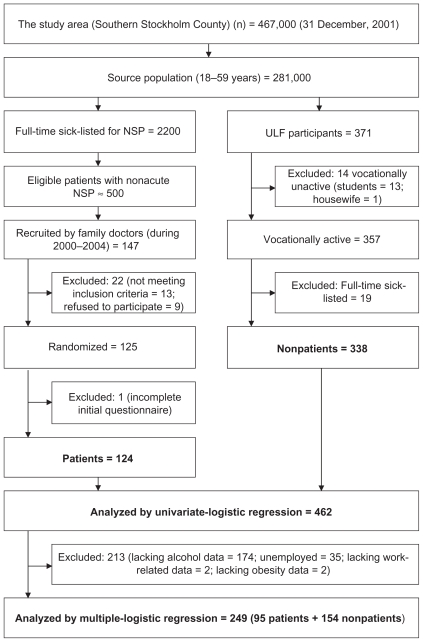
Several of the living conditions could be expected to intercorrelate, eg, Immigrant and Low education, and Blue-collar job and High physical workload. To find the most discriminative living conditions we used multiple-logistic regression, adjusted for gender and age, with the sample class as the outcome variable and the living conditions as the explanatory variables. A prerequisite for multiple-logistic regression is the same number of respondents for the different variables,16 so subjects with missing data were excluded from the multivariate analysis (Figure 2). This left 249 subjects (95 patients and 154 nonpatients) for multiple-logistic regression analysis. We first explored univariate analyses. The variables with a P value of at most 0.10 are presented with OR, P values and 95% CI. They were included in a multiple model, from which the variables with P values of 0.05 or higher were excluded stepwise to yield a model comprising only variables with P values < 0.05. The final multivariate model is presented with OR, P values, 95% CI, a goodness-of-fit test by Hosmer–Lemeshow, the percentage of correctly predicted patients, and the area under the ROC (receiver operating characteristic) curve.16
Figure 2.
Flowchart of the study.
Abbreviations: NSP, nonspecific spinal pain; ULF, Undersökningarna av levnadsförhållanden.
Results
A flowchart of the study is shown in Figure 2.
Eligible subjects in the source population
From ULF data, we estimated a point prevalence of individuals with full-time sick-listing for NSP to 0.8% or 2200 subjects. As these data included both short- and long-term sick-listing, we had to estimate the proportion of nonacute NSP, ie, the individuals with sick-listing >3 weeks. Previous research indicates an initial high recovery speed: starting from full-time sick-listing for NSP, ~90% of the individuals have returned to work after 12 weeks, and the rate clearly levels off thereafter.9 We estimated the point prevalence in the source population of nonacute NSP to be ~0.2% or ~500 individuals. We have no data for the prevalence over time.
Patients
A majority of the patients were recruited by a minority of the doctors: 15 doctors (36.6%) recruited in all 94 patients (75.2%). Twenty-one doctors recruited only 1 patient each (Table 2). Ninety-nine patients (79.2%) were living in 3 of the 9 districts, this number of inhabitants corresponding to 30.8% of the total number of inhabitants in the study area (Table 1).
The mean age of the 124 patients was 42.6 (range 18–59) years. The proportion of Old age was significantly higher than among the nonpatients (Table 4). Females predominated slightly. The current sick-listing period at baseline was m 170.9 (range 43–721) days.
Nonpatients
The mean age of the 338 nonpatients was 39.3 (range 19–59) years. Males predominated slightly. However, the difference in gender distribution versus the patients was nonsignificant (Table 4).
Outcome
In the univariate analyses, 13 of the 18 conditions had higher odds for the patients with a dominance of physical and psychosocial work strains, and Indication of alcohol over-consumption (OR 14.8); only 1 condition, Single life (OR 0.5), had lower odds (Table 4).
Five conditions qualified for the final multivariate model: High physical workload (OR 13.7), Hectic work tempo (OR 8.4), Blue-collar job (OR 4.5), Obesity (OR 3.5), and Low education (OR 2.7) (Table 5). The proportion of correctly classified subjects was high (85.5%) and the area under ROC curve was large (0.92; the maximum would be 1.0).
Table 5.
Living conditions – multivariate analysis
| Odds ratio | P value | 95% confidence interval | |
|---|---|---|---|
| High physical workload | 13.7 | <0.001 | 5.9–32.2 |
| Hectic work tempo | 8.4 | 0.001 | 2.5–28.3 |
| Blue-collar job | 4.5 | 0.003 | 1.8–11.4 |
| Obesity | 3.5 | 0.02 | 1.2–10.2 |
| Low education | 2.7 | 0.04 | 1.1–6.8 |
| Goodness-of-fit: | |||
| Hosmer–Lemeshow | 0.57 | ||
| Correctly classified | 85.5% | ||
| Area under ROC | 0.92 | ||
Notes: Ninety-five patients with nonacute nonspecific spinal pain compared with 154 nonpatients by logistic regression. Ranking by odds ratios.
Abbreviation: ROC, receiver operating characteristic.
Discussion
Living conditions associated with long-term sick-listing in primary-care patients with nonacute NSP were compared with a local sample of nonpatients. In the univariate analyses, the patients had higher odds for 13 of the 18 conditions. In the multivariate analysis, 5 conditions qualified, indicating work strains, lower social class, and life-style.
Work strains
High physical workload and Hectic work tempo were the two outstanding living conditions in the model. The association of High physical workload with NSP has been pinpointed in many studies.17–20 Job strain, ie, high demands, including among other items a high work tempo, and low control,21 has been associated with disabling NSP in several studies.22–25 Hectic work tempo as a single risk factor, however, is far less clear. In a review of risk factors for NSP, insufficient evidence was found for high work pace.26 Despite occasional studies that indicate a relationship between high work tempo and a longer time to return to work,27 a recent review of psychosocial predictors of failure to return to work in NSP showed strong evidence for the recovery expectations of the patients, while stress/psychological strain were non-predictive. 28 This is also in line with our newly published prospective study, in which High self prediction qualified as a predictor of stable return to work, while work-related variables did not.29
Indicators of lower social class
Blue collar job and Low education are closely associated and might be looked upon as different aspects of belonging to a lower social class.5 Low education limits the chances of getting a white-collar job, which explains the great dominance of work strains in the model and the fairly low degree of variance for Blue collar job and Low education in themselves. There is conflicting evidence in previous research of a relationship between NSP and lower social class. A possible association is probably a matter of social disadvantage, although it is not clear which aspects of the disadvantage are important.5 In our prediction study, there were indications that Low education, though a nonpredictor, may have qualified as a predictor with a longer follow-up than the 2 years of that study.29 Blue-collar job, however, was a clear nonpredictor. With a prevalence of 87.4% of the patients versus 33.2% of the nonpatients, it is logical that such a great difference qualifies for a multivariate analysis with the sample class as outcome variable. The prediction study, however, exclusively involved patients with return to work/nonreturn to work as the outcome. A variable of such overwhelming frequency might be nondiscriminative, although it has a powerful effect on sick-listing. There is a lack of conclusive studies on the possible association between sick-listing for NSP and social class, according to a large 2004 review.10 Our research might contribute to the elucidation of this complex issue.
Life-style
While the prevalence of Smoking was nonsignificantly higher in the patients, the prevalences of Indication of alcohol over-consumption and Obesity were remarkably higher.
Smoking as a nonpredictor of disabling NSP was indicated in a cross-national, prospective study from 2000, including about 2000 subjects.19 However, associations between smoking and NSP have been found in several other studies. A 1999 review indicated smoking as a weak risk indicator but not a cause of NSP, and signs of causality were evident only in the study with the largest sample, >30,000 subjects.30 In a 2000 review, a possible association between NSP and cigarette smoking was suggested, but the lack of prospective studies was emphasized.31 In a recent meta-analysis of both cross-sectional and prospective studies, current as well as former smoking was associated with NSP, though the association was fairly modest.32 The nonsignificance of Smoking in this study and in our prediction study might therefore be due to the small sample size.
More or less hidden alcohol abuse constitutes one of the greatest public health problems, with substantial social and clinical implications. Large population studies have shown that 10% to 15% of all men and approximately 5% of all women suffer from chronic alcohol dependency33 and quite recent primary-care research indicates a continued increase of those proportions.34 Among the subjects with chronic alcohol dependency about one-quarter are in a phase of active abuse.33 This should correspond to around 2% to 2.5% of the nonpatients of our study, which was approximately confirmed by the ULF data. The patients had a substantially higher prevalence, and we have found nothing equivalent in any other study of NSP. The reason could be our use of one single binge-drinking question (Table 3),35 which might decrease the risk for under-estimation of alcohol abuse in questionnaires that ask for total intake. We have found no previous study of NSP where this question has been used. However, in the multivariate context, the alcohol issue was eliminated by other closely correlated variables. For example, 15 of the 16 subjects in the multivariate analysis with Indication of alcohol over-consumption had a Blue-collar job. One study showed that alcohol over-consumption was not a risk factor for long-term sick-listing for NSP,36 but this was contradicted by an other study.37 In our prediction study, Indication of alcohol over-consumption did not predict sick-listing during a 2-year follow-up.29 Though these conflicting results motivate further research, this cross-sectional study might contribute in pinpointing the comparatively higher prevalence of abuse problems among those patients.
During recent decades the prevalence of obesity has increased remarkably but with a certain international variation. For example, while the prevalence in the USA has increased to a full 20%,38 it doubled in Sweden from the years 1980/81 to 2004/5 from 5% to 10% in both women and men.39 Comorbidities with obesity include diabetes, cardiovascular diseases, pain in general, and NSP in particular.40 In our study, the prevalence of Obesity in the nonpatients during the years 2000/01 corresponded well with the 7% in 1996/97 concerning all Swedes 16 to 84 years,39 while among the patients it was more than 3-fold higher. Obesity remained significant in the multivariate model, though with a decreased OR, probably influenced by Low education, which is a risk factor for obesity. 41 According to a 2000 review, obesity should be considered a possible weak risk indicator, but with insufficient data to assess whether it causes spinal pain.42 In a prospective study from 2002, obesity was a risk factor for the transition from acute to nonacute NSP, though with low OR (1.7).20 However, in a large 2004 review on predictors for nonacute NSP, there was insufficient evidence for obesity as a risk factor.10 A quite recent, very large, cross-sectional population-based study from Norway indicated associations between obesity and NSP and commented that further studies were needed to determine whether the association was causal.43 Our prediction study, however, found no impact of Obesity on sick-listing.29 Obesity was found in 24.2% of the patients versus 6.9% of the nonpatients. In line with the paragraph above, such a difference might qualify for a model with the sample class as outcome variable, but be eliminated in an analysis with return to work/nonreturn to work as outcome. It therefore remains unclear whether, how, and why obesity and NSP are correlated.40 Furthermore, the clinical relevance of that association, if any, is obscure. Recently, however, a reduction of musculoskeletal pain was reported in a study of a weight-reduction program, at least on a short-term basis, which might be of future clinical interest in the treatment of disabling NSP.44
To sum up: the patients were distinguished by higher odds of obesity, higher odds of indication of alcohol abuse that vanished in the multivariate analysis, and nonsignificant differences on smoking. Prospective research, including our prediction study, has yielded conflicting results. Therefore, the causal associations between smoking, alcohol abuse, and obesity, and sick-listing for NSP, if any, are small.
Study strengths
One of the strengths of our study was the good representation of women.
As in the ULF surveys, the patient questionnaires were completed under the supervision of an assistant during an interview with the patient in the recruiting health center. This might have contributed to the high quality of the patient data, and increased the comparability between the patients and the nonpatients.
The design of the nationwide ULF also allows local comparisons to be made. The responding rates of the ULF in 2000 and 2001 were practically 80%. These high-quality data for the comparison group were a strength.
Another strength of the study was the excellent model fit. The number of variables in the multivariate model was by a wide margin within the upper limit, which is suggested in previous research.45
Study limitations
The sample of 124 patients was a very low proportion of the eligible subjects and the inclusion procedure was prolonged and nonsystematic. These limitations are discussed in detail in our predictor study.29 A closely related limitation was the geographical imbalance in the recruitment; however, the greatest number of recruited patients were living in the district with the greatest number of inhabitants (Huddinge) (Table 1).
A limitation was the nonprospective design. However, this study might contribute to a more detailed cross-sectional picture of the patients with nonacute NSP, which is also of value in the planning of prospective research, eg, our predictor study.29
External validity
To what extent might the results be generalized beyond the samples of patients and nonpatients studied and be applied to other subjects (population validity) or settings (ecological validity)? As the rehabilitation center and the family doctors engaged were very well established, the 124 patients might be reasonably representative of the everyday primary care in the study area, comprising a comparably large part of Stockholm County. The 338 nonpatients in the study were generally comparable with nonpatients in the nation. The only significant (P < 0.05) differences from the national sample of 7007subjects were a higher prevalence of Immigrant (12.7% vs 10.5%), Unemployed (3.9% vs 8.4%), Blue-collar job (33.3% vs 39.2%), Heavy physical workload (15.7% vs 35.3%), and Vibrations in work (4.6% vs 8.6%). According to a large cross-national study, including primary care in 14 countries in 5 continents, the dominating pain problem was nonacute spinal pain; and despite certain variations, the cross-national manifestations of spinal pain were surprisingly equivalent.46 Therefore, given that the study samples are reasonably representative of Swedish primary care, the external validity might also be satisfactory from a non-Swedish perspective.
Clinical implications
Standing alone, the cross-sectional design of this study limits its clinical implications. However, together with prospective studies, it might increase the knowledge of what distinguishes patients with nonacute, nonspecific spinal pain. Though this knowledge in no way includes unambiguous management options, it might help family doctors, supervisors in the work place, handling officers of the Social Insurance Agency, and so on, to identify subjects at risk.
Conclusions
The living conditions associated with long-term sick-listing of 124 patients with nonacute nonspecific spinal pain were compared with 338 nonpatients by applying logistic regression. In the univariate analyses, 13 of the 18 conditions had higher odds for the patients with a dominance of physical work strains and Indication of alcohol over-consumption (OR 14.8). Five conditions qualified for the multivariate analysis: High physical workload (OR 13.7), Hectic work tempo (OR 8.4), Blue-collar job (OR 4.5), Obesity (OR 3.5), and Low education (OR 2.7). As most of those living conditions have hitherto been insufficiently studied, our findings might help extend our knowledge of what distinguishes the individuals at risk for long-term sick-listing due to NSP. As the cross-sectional design makes causal conclusions impossible, our study should be complemented by prospective research.
Acknowledgment
This study was supported by grants from the Stockholm County Social Insurance Agency, Stockholm County Council, Ministry of Health and Social Affairs, Vårdal Foundation, Cardionics, and Pharmacia (now part of Pfizer).
Footnotes
Authors’ contributions
OL was the main investigator and carried out the study, performed the analysis, and drafted the manuscript. SEJ contributed to the statistical analysis. LES, as supervisor of OL, participated in all phases of the study. All authors read and approved the final manuscript.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Oecd.org [homepage on the Internet] Key trends and outcomes. Sickness, Disability and Work. Keeping on track in the economic downturn. OECD, Directorate for employment, labour and social affairs; Background paper: High-Level Forum; Stockholm. 2009 May 14–15; [Accessed 2010 Oct 8]. pp. 11–16. http://www.oecd.org/dataoecd/42/15/42699911.pdf. [Google Scholar]
- 2.Forsakringskassan.se [homepage on the Internet] Newly awarded disability pensions. Distribution between counties and diagnoses, 2006 [In Swedish; Nybeviljade sjukersättningar/aktivitetsersättningar. Fördelning på län och diagnos, 2006] Social Insurance in Sweden. [Accessed 2010 Oct 8];Statistics. 2007 7 [In Swedish; Försäkringskassan. Statistik 2007:7]. [ http://statistik.forsakringskassan.se/rfvexcel/statpub/Statistik_2007-02.pdf] [Google Scholar]
- 3.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. Comprehensive review of epidemiology, scope, and impact of spinal pain. [Accessed 2010 Oct 8];Pain Physician. 2009 12(4) [about 36 p.]. [ http://www.painphysicianjournal.com/2009/july/2009;12;E35-E70.pdf] [PubMed] [Google Scholar]
- 4.Waddell G, van Tulder M. Clinical guidelines. In: Waddell G, editor. Back Pain Revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2004. pp. 283–322. [Google Scholar]
- 5.Waddell G, Waddell H. A review of social influences on neck and back pain and disability. In: Nachemson A, Jonson E, editors. Neck and Back Pain. The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia: Lippincott Williams & Williams; 2000. pp. 13–55. [Google Scholar]
- 6.Linton SJ. Psychological risk factors for neck and back pain. In: Nachemson A, Jonson E, editors. The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia: Lippincott Williams & Williams; 2000. pp. 57–78. [Google Scholar]
- 7.Nachemson A, Vingård E. Influences of individual factors and smoking on neck and low back pain. In: Nachemson A, Jonson E, editors. The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia: Lippincott Williams & Williams; 2000. pp. 79–95. [Google Scholar]
- 8.Vingård E, Nachemson A. Work-related influences on neck and low back pain. In: Nachemson A, Jonson E, editors. The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia: Lippincott Williams & Williams; 2000. pp. 97–126. [Google Scholar]
- 9.Waddell G. The biopsychosocial model. In: Waddell G, editor. Back Pain Revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2004. pp. 265–282. [Google Scholar]
- 10.Hansson T, Jensen I. Sickness absence due to back and neck disorders. In: Alexanderson K, Norlund A, editors. Sickness Absence – Causes, Consequences, and Physicians’ Sickness-Certification Practice. [Google Scholar]; Scand J Public Health. 2004;63 (Suppl):S109–S151. [Google Scholar]
- 11.Unorg [homepage on the Internet] Brief history and other relevant background information Country Profile of Sweden. United Nations Statistical Division. [Accessed 2010 Oct 8]. [ http://unstats.un.org/unsd/dnss/docViewer.aspx?docID=666#start]
- 12.Scb.se [homepage on the Internet] Living conditions. Appendix 16. The Swedish Survey of Living Conditions. Design and methods. Official Statistics of Sweden. Statistics Sweden. [Accessed 2010 Oct 8]. [ http://www.scb.se/statistik/LE/LE0101/_dokument/Appendix_16.PDF]
- 13.Lindell O, Johansson SE, Strender LE. Subacute and chronic, non-specific back and neck pain: cognitive-behavioural rehabilitation versus primary care. A randomized controlled trial. [Accessed 2010 Oct 8];BMC Musculoskelet Disord. 2008 9:172. doi: 10.1186/1471-2474-9-172. [about 17 p.]. [ http://www.ncbi.nlm.nih.gov/pubmed/19116007] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scb.se [homepage on the Internet] Supplement to appendix 16. Statistics Sweden. [Accessed 2010 Oct 8]. [ http://www.scb.se/statistik/LE/LE0101/Supplement16.pdf]
- 15.StataCorp. Stata Statistical Software: Release 9. College Station TX: StataCorp LP; 2005. [Google Scholar]
- 16.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: John Wiley & Sons; 2000. [Google Scholar]
- 17.Krause N, Dasinger LK, Deegan LJ, Rudolph L, Brand RJ. Psycho-social job factors and return-to-work after compensated low back injury: a disability phase-specific analysis. Am J Ind Med. 2001;40(4):374–392. doi: 10.1002/ajim.1112. [DOI] [PubMed] [Google Scholar]
- 18.Dasinger LK, Krause N, Deegan LJ, Brand RJ, Rudolph L. Physical workplace factors and return to work after compensated low back injury: a disability phase-specific analysis. J Occup Environ Med. 2000;42(3):323–333. doi: 10.1097/00043764-200003000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Hansson TH, Hansson EK. The effects of common medical interventions on pain, back function, and work resumption in patients with chronic low back pain: A prospective 2-year cohort study in six countries. Spine. 2000;25(23):3055–3064. doi: 10.1097/00007632-200012010-00013. [DOI] [PubMed] [Google Scholar]
- 20.Fransen M, Woodward M, Norton R, Coggan C, Dawe M, Sheridan N. Risk factors associated with the transition from acute to chronic occupational back pain. Spine. 2002;27(1):92–98. doi: 10.1097/00007632-200201010-00022. [DOI] [PubMed] [Google Scholar]
- 21.Theorell T, Karasek RA, Eneroth P. Job strain variations in relation to plasma testosterone fluctuations in working men – a longitudinal study. J Intern Med. 1990;227(1):31–36. doi: 10.1111/j.1365-2796.1990.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 22.Rugulies R, Krause N. Job strain, iso-strain, and the incidence of low back and neck injuries. A 7.5-year prospective study of San Francisco transit operators. Soc Sci Med. 2005;61(1):27–39. doi: 10.1016/j.socscimed.2004.11.042. [DOI] [PubMed] [Google Scholar]
- 23.IJzelenberg W, Burdorf A. Risk factors for musculoskeletal symptoms and ensuing health care use and sick leave. Spine. 2005;30(13):1550–1556. doi: 10.1097/01.brs.0000167533.83154.28. [DOI] [PubMed] [Google Scholar]
- 24.Ghaffari M, Alipour A, Farshad AA, Jensen I, Josephson M, Vingard E. Effect of psychosocial factors on low back pain in industrial workers. Occup Med (Lond) 2008;58(5):341–347. doi: 10.1093/occmed/kqn006. [DOI] [PubMed] [Google Scholar]
- 25.Harcombe H, McBride D, Derrett S, Gray A. Physical and psychosocial risk factors for musculoskeletal disorders in New Zealand nurses, postal workers and office workers. Inj Prev. 2010;16(2):96–100. doi: 10.1136/ip.2009.021766. [DOI] [PubMed] [Google Scholar]
- 26.Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25(16):2114–2125. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- 27.van der Weide WE, Verbeek JH, Sallé HJ, van Dijk FJ. Prognostic factors for chronic disability from acute low-back pain in occupational health care. Scand J Work Environ Health. 1999;25(1):50–56. doi: 10.5271/sjweh.383. [DOI] [PubMed] [Google Scholar]
- 28.Iles RA, Davidson M, Taylor NF. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: a systematic review. Occup Environ Med. 2008;65(8):507–517. doi: 10.1136/oem.2007.036046. [DOI] [PubMed] [Google Scholar]
- 29.Lindell O, Johansson SE, Strender LE. Predictors of stable return-to-work in non-acute, non-specific spinal pain: low total prior sick-listing, high self prediction and young age. A two-year prospective cohort study. [Accessed 2010 Oct 8];BMC Fam Pract. 2010 11(53) doi: 10.1186/1471-2296-11-53. [about 12 p.]. [ http://www.ncbi.nlm.nih.gov/pubmed/20646286] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leboeuf-Yde C. Smoking and low back pain. A systematic literature review of 41 journal articles reporting 47 epidemiologic studies. Spine. 1999;24(14):1463–1470. doi: 10.1097/00007632-199907150-00012. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg MS, Scott SC, Mayo NE. A review of the association between cigarette smoking and the development of nonspecific back pain and related outcomes. Spine. 2000;25(8):995–1014. doi: 10.1097/00007632-200004150-00016. [DOI] [PubMed] [Google Scholar]
- 32.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. [Accessed 2010 Oct 8];Am J Med. 2010 123(1) doi: 10.1016/j.amjmed.2009.05.028. [about 29 p]. [ http://www.sciencedirect.com/science?_ob=MImg&_imagekey=B6TDC-4Y0T775-N-1&_cdi=5195&_user=3285060&_pii=S000293430900713X&_origin=search&_coverDate=01%2F31%2F2010&_sk=998769998&view=c&wchp=dGLzVtb-zSkzk&md5=7582f0241d1b0042e2b3e6972ac94462&ie=/sdarticle.pdf] [DOI] [PubMed] [Google Scholar]
- 33.Berglund M. Treatment of alcohol and drug abuse – an evidence-based review [In Swedish; Behandling av alkohol- och narkotikaproblem – en evidensbaserad kunskapssammanställning] The Swedish Council on Technology Assessment in Health Care; Stockholm: 2001. [Accessed 2010 Oct 8]. Summary and conclusions [In Swedish; Sammanfattning och slutsatser] pp. 11–28. Summary in English: [ http://www.sbu.se/upload/Publikationer/Content0/1/alcoholdrug_2001/drugslut.html] [Google Scholar]
- 34.Zivin K, Pfeiffer PN, Szymanski BR, et al. Initiation of Primary Care-Mental Health Integration programs in the VA Health System: associations with psychiatric diagnoses in primary care. Med Care. 2010;48(9):843–851. doi: 10.1097/MLR.0b013e3181e5792b. [DOI] [PubMed] [Google Scholar]
- 35.Romelsjö A, Leifman H, Nyström S. A comparative study of two methods for the measurement of alcohol consumption in the general population. Int J Epidemiol. 1995;24(5):929–936. doi: 10.1093/ije/24.5.929. [DOI] [PubMed] [Google Scholar]
- 36.Holmberg SA, Thelin AG. Primary care consultation, hospital admission, sick leave and disability pension owing to neck and low back pain: a 12-year prospective cohort study in a rural population. [Accessed 2010 Oct 8];BMC Musculoskelet Disord. 2006 7(66) doi: 10.1186/1471-2474-7-66. [about 8 p.]. [ http://www.biomedcentral.com/content/pdf/1471-2474-7-66.pdf] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129(3):332–342. doi: 10.1016/j.pain.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 38.Kjellström T. Obesity – problems and interventions [In Swedish; Fetma – problem och åtgärder] The Swedish Council on Technology Assessment in Health Care. Report number: 160; Stockholm: 2002. [Accessed 2010 Oct 8]. Summary and conclusions [In Swedish: Sammanfattning och slutsatser] pp. 6–24. Summary in English: [ http://www.sbu.se/en/Published/Yellow/Obesity---problems-and-interventions/] [Google Scholar]
- 39.Norberg M, Danielsson M. The report of public health 2009 [In Swedish; Folhälsorapporten 2009] The Swedish National Institute of Public Health; Stockholm: 2009. [Accessed 2010 Oct 8]. Overweight, cardiovascular diseases and diabetes [In Swedish; Övervikt, hjärt-och kärlsjukdomar och diabetes] pp. 201–242. [ http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8495/2009-126-71_200912671.pdf] [Google Scholar]
- 40.Janke EA, Collins A, Kozak AT. Overview of the relationship between pain and obesity: What do we know? Where do we go next? J Rehabil Res Dev. 2007;44(2):245–262. doi: 10.1682/jrrd.2006.06.0060. [DOI] [PubMed] [Google Scholar]
- 41.Rissanen AM, Heliövaara M, Knekt P, Reunanen A, Aromaa A. Determinants of weight gain and overweight in adult Finns. Eur J Clin Nutr. 1991;45(9):419–430. [PubMed] [Google Scholar]
- 42.Leboeuf-Yde C. Body weight and low back pain. A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine. 2000;25(2):226–237. doi: 10.1097/00007632-200001150-00015. [DOI] [PubMed] [Google Scholar]
- 43.Heuch I, Hagen K, Heuch I, Nygaard Ø, Zwart JA. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine. 2010;35(7):764–768. doi: 10.1097/BRS.0b013e3181ba1531. [DOI] [PubMed] [Google Scholar]
- 44.Kotowski SE, Davis KG. Influence of weight loss on musculoskeletal pain: Potential short-term relevance. Work. 2010;36(3):295–304. doi: 10.3233/WOR-2010-1031. [DOI] [PubMed] [Google Scholar]
- 45.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 46.Gureje O, Simon GE, von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92(1–2):195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 47.Linton SJ. Risk factors for neck and back pain in a working population in Sweden. Work Stress. 1990;4(1):41–49. [Google Scholar]
- 48.Hagen KB, Holte HH, Tambs K, Bjerkedal T. Socioeconomic factors and disability retirement from back pain: a 1983–1993 population-based prospective study in Norway. Spine. 2000;25(19):2480–2487. doi: 10.1097/00007632-200010010-00010. [DOI] [PubMed] [Google Scholar]
- 49.Karlsson N, Borg K, Carstensen J, Hensing G, Alexanderson K. Risk of disability pension in relation to gender and age in a Swedish county; a 12-year population based, prospective cohort study. Work. 2006;27(2):173–179. [PubMed] [Google Scholar]
- 50.Du Bois M, Szpalski M, Donceel P. Patients at risk for long-term sick leave because of low back pain. Spine. 2009;9(5):350–359. doi: 10.1016/j.spinee.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 51.Borg K, Hensing G, Alexandersson K. Predictive factors for disability pension – an 11-year follow up of young persons on sick leave due to neck, shoulder or back diagnoses. Scand J Public Health. 2001;29(2):104–112. [PubMed] [Google Scholar]
- 52.Mastekaasa A. Parenthood, gender and sickness absence. Soc Sci Med. 2000;50(12):1827–1842. doi: 10.1016/s0277-9536(99)00420-7. [DOI] [PubMed] [Google Scholar]
- 53.Åstrand NE, Isacsson SO. Back pain, back abnormalities, and competing medical, psychological, and social factors as predictors of sick leave, early retirement, unemployment, labour turnover and mortality: a 22 year follow up of male employees in a Swedish pulp and paper company. Br J Ind Med. 1988;45(6):387–395. doi: 10.1136/oem.45.6.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Selander J, Marnetoft SU, Bergroth A, Ekholm J. Return to work following vocational rehabilitation for neck, back and shoulder problems: risk factors reviewed. Disabil Rehabil. 2002;24(14):704–712. doi: 10.1080/09638280210124284. [DOI] [PubMed] [Google Scholar]
- 55.Tornqvist EW, Kilbom A, Vingård E, et al. The influence on seeking care because of neck and shoulder disorders from work-related exposures. Epidemiology. 2001;12(5):537–545. doi: 10.1097/00001648-200109000-00013. [DOI] [PubMed] [Google Scholar]
- 56.Theorell T, Perski A, Åkerstedt T. Changes in job strain in relation to changes in psychological state: a longitudinal study. Scand J Work Environ Health. 1988;14(3):189–196. doi: 10.5271/sjweh.1932. [DOI] [PubMed] [Google Scholar]
- 57.Nordin M, Hiebert R, Pietrek M, Alexander M, Crane M, Lewis S. Association of comorbidity and outcome in episodes of nonspecific low back pain in occupational populations. J Occup Environ Med. 2002;44(7):677–684. doi: 10.1097/00043764-200207000-00015. [DOI] [PubMed] [Google Scholar]