Abstract
Nontraumatic intramural duodenal hematoma (IDH) is rare disease and it is generally related to coagulation abnormalities. Reports of nontraumatic IDH associated with pancreatic disease are relatively rare, and various conditions including acute or chronic pancreatitis are thought to be associated with nontraumatic IDH. However, the association between IDH and acute pancreatitis remains unknown. We report the case of a 45-year-old man who presented with vomiting and right hypochondrial pain. He had no medical history, but was a heavy drinker. The diagnosis of IDH was established by computed tomography, ultrasonography and endoscopy, and it was complicated by acute pancreatitis. The lesions resolved with conservative management. We discuss this case in the context of previously reported cases of IDH concomitant with acute pancreatitis. In our patient, acute pancreatitis occurred concurrently with hematoma, probably due to obstruction of the duodenal papilla, or compression of the pancreas caused by the hematoma. The present analysis of the published cases of IDH with acute pancreatitis provides some information on the pathogenesis of IDH and its relationship with acute pancreatitis.
Keywords: Intramural duodenal hematoma, Acute pancreatitis, Computed tomography, Ultrasonography, Jaundice
INTRODUCTION
Intramural duodenal hematoma (IDH) is a rare disease in which there is hematoma formation within the wall of duodenum, and was first reported at autopsy in 1838 by MacLauchlan[1]. IDH occurs mainly in children, secondary to blunt abdominal trauma[2], and in adults, abdominal trauma accounts for > 70% of cases[3]. Nontraumatic IDH is particularly associated with coagulation abnormalities, including anticoagulant therapy, hemophilia, and Von Willebrand disease[4]. Recently, there have been a few reported cases of IDH occurring after duodenal biopsy or injection therapy for bleeding peptic ulcer during upper gastrointestinal fiberscopy (GF)[5,6].
Reports of nontraumatic IDH associated with pancreatic diseases are relatively rare, and various pancreatic conditions, including acute or chronic pancreatitis, pancreatic tumors, and ectopic pancreas are thought to be associated with nontraumatic IDH[7]. However, the association between IDH and acute pancreatitis remains unknown. Recently, we encountered a case of IDH complicated by acute pancreatitis. In this paper, we discuss this case in the context of previously reported cases of IDH concomitant with acute pancreatitis.
CASE REPORT
A 45-year-old man was admitted to our hospital with chief complaints of postprandial vomiting and right hypochondrial pain of 1 d duration. He had no medical or family history of note, but was a heavy drinker who consumed > 2 L of beer every day. Physical examination on admission revealed a palpable epigastric mass with tenderness over the epigastric region and right flank.
On initial laboratory evaluation, hemoglobin was 12.5 g/dL, white blood cell count 14 000/μL (normal: 4000-9000/μL), C-reactive protein 1.1 mg/dL (normal: 0.0-0.2 mg/dL), serum amylase 1150 IU/L (normal: 24-137 IU/L), and total bilirubin 3.2 mg/dL (normal: 0.1-1.0 mg/dL).
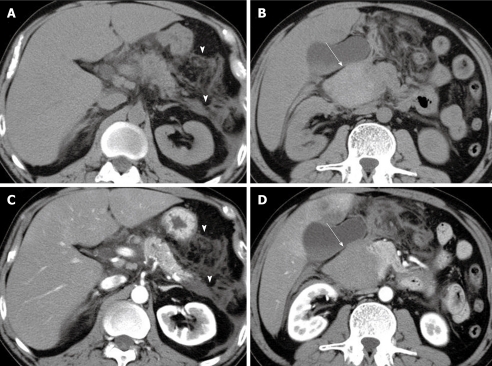
Contrast-enhanced abdominal computed tomography (CT) revealed mild pancreatic enlargement with an increased density of peripancreatic dirty fat tissue and fluid collection. A slightly hyperdense, spindle-shaped mass, 65 mm in maximum diameter was also present, mainly along the descending part of the duodenum, which showed no contrast enhancement in the arterial and equilibrium phases (Figure 1).
Figure 1.
Abdominal computed tomography revealed an increased density of peripancreatic dirty fat tissue and fluid collection (arrowheads), without (A) and with (C) contrast. Unenhanced computed tomography (B) revealed a slightly hyperdense, spindle-shaped mass, 65 mm in maximum diameter, mainly along the descending part of the duodenum (arrow). This mass showed no contrast enhancement in the arterial phase (arrow) (D).
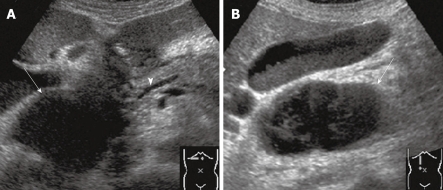
Abdominal ultrasonography (US) showed a 65 mm × 45 mm heterogeneous mass at the level of the pancreatic head, with a slightly dilated main pancreatic duct and peripancreatic fluid collection (Figure 2). Doppler US revealed no internal blood flow signal in the mass. Contrast-enhanced US with Sonazoid (Daiichi-Sankyo, Tokyo, Japan) showed no flow of contrast medium into the mass in any phase.
Figure 2.
Abdominal ultrasonography showed a 65 mm × 45 mm heterogeneous mass at the level of the pancreatic head (arrows) (A and B), with a slightly dilated main pancreatic duct (arrowhead) and peripancreatic fluid collection (A).
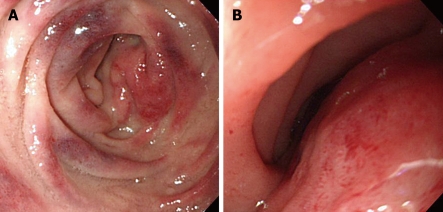
GF showed that the mucosa of the duodenal bulb and the descending part was reddish and edematous, and the mucosa of the distal portion of the latter was elevated like a relatively soft submucosal tumor (Figure 3). Endoscopic US revealed a homogeneous, hypoechoic tumor.
Figure 3.
Gastrointestinal fiberscopy showed the reddish and edematous mucosa in the descending part of the duodenum (A) and luminal narrowing was observed (B).
These findings led to a diagnosis of IDH complicated by acute pancreatitis. During his hospital stay, the patient showed no enlargement of the hematoma or worsening of the clinical symptoms, and was started on conservative treatment. Thereafter, the symptoms and laboratory data gradually improved, with no progression of anemia. After the clinical symptoms and laboratory data had stabilized on day 25 in hospital, abdominal angiography was performed, which showed that the gastroduodenal artery and pancreatic arterial arcade had no irregularities. Aortic angiography showed no abnormalities of the renal or jejunal arteries. The patient’s subsequent course was uneventful, and he was discharged 30 d after admission.
DISCUSSION
Most often, IDH develops after blunt abdominal trauma, which results from child abuse in children younger than 15 years of age in over 60% of cases[2]. In adults, nontraumatic IDH due to anticoagulant therapy or blood abnormalities is common, and cases of iatrogenic IDH due to duodenal biopsy or endoscopic retrograde cholangiopancreatography have recently been reported[5,8]. Compared with traumatic IDH, which usually occurs at the subserosal layer of the duodenum, nontraumatic IDH is mostly underneath the duodenal mucosa or submucosa[9]. Thus, nontraumatic IDH causes intestinal stenosis, often initially presenting with abdominal pain and vomiting, and sometimes causing symptoms of dehydration with severe vomiting and jaundice due to biliary stenosis. Laboratory data show progressive anemia and an increased inflammatory response. Gastrointestinal tract radiography has long been the gold standard diagnostic procedure for IDH, which is characterized by a thread-like lumen and the “coil spring sign” of the duodenum[10]. Diniz-Santos et al[11] have noted that CT is useful in that it facilitates not only the diagnosis of IDH, but also differentiation from other diseases, and judgment regarding the presence or absence of perforation. However, they have reported that CT exposes patients to high levels of radiation, which makes it unsuitable for follow-up during therapy, and that magnetic resonance imaging and abdominal US are effective for follow-up. In the present case, the patient visited our hospital with chief complaints of abdominal pain and vomiting, and exhibited elevated levels of released pancreatic enzymes and hepatobiliary enzymes. These and contrast-enhanced CT findings led to a diagnosis of IDH complicated by acute pancreatitis.
Reports of nontraumatic IDH associated with pancreatic diseases are relatively rare. Although various pancreatic conditions, such as acute pancreatitis, are believed to be associated with IDH, the nature of the association remains unknown. A PubMed search from 1980 onward using the key words IDH and acute pancreatitis yielded 32 cases reported in the English literature (Table 1)[5-7,9,11-33]. We reviewed the association between IDH and acute pancreatitis for these cases.
Table 1.
Characteristics of patients with intramural duodenal hematoma associated with acute pancreatitis
| No. | Ref. | Yr | Age (yr)/sex | Underlying disease | Heavy drinker | AMY (IU/L) | Cause of IDH | Therapy | Type |
| 1 | van Spreeuwel et al[12] | 1981 | 45/M | CP | Yes | 136 | ACP | Ope | C |
| 2 | Patel et al[13] | 1982 | 48/M | CP | Yes | - | ERCP | Ope | A |
| 3 | Fingerhut et al[14] | 1983 | 47/M | CP | Yes | - | ACP | Con | C |
| 4 | Giraud et al[15] | 1986 | 40/M | CP | Yes | 3175 | ACP | Con | C |
| 5 | Glassman et al[16] | 1988 | 18/M | Hemophilia A | - | 3000 | Hemophilia A | Con | A |
| 6 | Zinelis et al[17] | 1989 | 23/M | Malabsorption synd. | No | 1410 | DB | Con | A |
| 7 | Sadry et al[6] | 1990 | -/F | Breast cancer | - | 2940 | Injection therapy | Con | A |
| 8 | Archer et al[18] | 1991 | 35/M | CP | Yes | 195 | ACP | Ope | C |
| 9 | Szajewska et al[19] | 1993 | 5/F | None | - | 1200 | DB | Ope | A |
| 10 | Karjoo et al[20] | 1994 | 14/F | RD | - | 1164 | DB | Con | A |
| 11 | Rohrer et al[21] | 1994 | 51/M | Hepatic cirrhosis | Yes | - | DB | Con | A |
| 12 | 1994 | 61/M | Renal failure | - | - | DB | Con | A | |
| 13 | 1994 | 22/M | HELLP synd. | - | - | DB | Con | A | |
| 14 | Lipson et al[22] | 1996 | 15/M | Leukemia | - | 1948 | DB | Con | A |
| 15 | 1996 | 32/F | Leukemia | - | 299 | DB | Con | A | |
| 16 | 1996 | 11/M | Leukemia | - | 403 | DB | Con | A | |
| 17 | Guzman et al[23] | 1998 | 13/M | ASD | - | 2236 | DB | Con | A |
| 18 | 1998 | 13/F | None | - | 522 | DB | Con | A | |
| 19 | Worynski et al[24] | 1998 | 23/M | Leukemia | No | - | DB | Con | A |
| 20 | Fesenmyer et al[25] | 1998 | 71/M | CP | No | 377 | ACP | Con | C |
| 21 | Bellens et al[26] | 1999 | 40/M | CP | Yes | 98 | ACP | Ope | C |
| 22 | Bodnár et al[27] | 2000 | 33/M | None | No | 2375 | AP | Con | B |
| 23 | Dugernier et al[28] | 2002 | 32/M | - | - | - | AP | - | B |
| 24 | Dubois et al[7] | 2003 | 51/M | CP | Yes | 573 | ACP | Con | C |
| 25 | Sgouros et al[29] | 2004 | 32/M | Noonan synd. | No | - | DB | Con | A |
| 26 | Diniz-Santos et al[11] | 2006 | 6/M | None | - | 527 | DB | Con | A |
| 27 | Borsaru et al[30] | 2007 | 10/F | None | - | - | DB | Con | A |
| 28 | Ma et al[9] | 2008 | 32/M | CP | Yes | 758 | ACP | Ope | C |
| 29 | Chen et al[31] | 2008 | 17/M | Hodgkin disease | - | - | DB | Con | A |
| 30 | Fukunaga et al[32] | 2009 | 49/M | None | Yes | 1374 | AP | Ope | B |
| 31 | Antoniou et al[5] | 2009 | 5/M | None | - | 334 | DB | Con | A |
| 32 | Abdel Samie et al[33] | 2009 | 80/F | Af | No | - | Anticoagulation | Con | A |
| 33 | Present case | 2010 | 45/M | None | Yes | 1150 | None | Con | A |
IDH: Intramural duodenal hematoma; -: Not reported; CP: Chronic pancreatitis; RD: Von Reckling hausen’s disease; ASD: Atrial septal defect; ACP: Acute exacerbation of chronic pancreatitis; ERCP: Endoscopic retrograde cholangiopancreatography; DB: Duodenal biopsy; AP: Acute pancreatitis; Ope: Operation; Con: Conservative therapy; AMY: Amylase; synd.: Syndrome.
As a result, IDH complicated with pancreatitis could be broadly classified into the following three types: (A) acute pancreatitis due to duodenal papilla obstruction by hematoma; (B) hematoma formation due to vascular disruption by pancreatic enzymes released during acute pancreatitis; and (C) hematoma formation due to vascular disruption by pancreatic enzymes released during chronic pancreatitis, or its acute exacerbation. In type A, hematoma formation through some cause precedes the development of obstructive acute pancreatitis as a complication. As described above, nontraumatic IDH often develops in the duodenal mucosa or submucosa[9], and impaired pancreatic enzyme secretion due to obstruction of the duodenal papilla is believed to cause acute pancreatitis. In recent years, duodenal biopsy in children as well as young and adult patients with underlying diseases such as leukemia and hemophilia has often been implicated as a cause of hematoma formation. In particular, the vicinity of the duodenal papilla has a rich submucosal vascular supply of the pancreatic arcade, and the descending part of the duodenum is not fixed to the retroperitoneum; therefore, it has been noted that the separation of the mucosa from the underlying immobile submucosa during biopsy might cause tearing of the submucosal vessels, which can lead to the formation of hematoma[19]. This makes it necessary to perform duodenal biopsies carefully, and avoid, as much as possible, the vicinity of the duodenal papilla in children or patients with underlying diseases. On the other hand, in types B and C IDH, pancreatitis results in hematoma formation. Vascular abnormalities, such as duodenal or pancreatic artery pseudoaneurysm, have been demonstrated by abdominal angiography in chronic pancreatitis patients[7], which suggests that vascular disruption leads to hematoma formation.
In patients with type A IDH, imaging often shows dilatation of the bile and main pancreatic ducts, which can aid in the classification of the relationship between IDH and acute pancreatitis. However, in any type of IDH with acute pancreatitis, it is often difficult to differentiate obstructive acute pancreatitis due to IDH from IDH due to acute pancreatitis or the acute exacerbation of chronic pancreatitis, by imaging findings alone. Indeed, there have been reported cases that were difficult to classify.
In patients with type A IDH with obstructive acute pancreatitis, abdominal pain and severe vomiting occur almost simultaneously; in particular, in many biopsied patients, these symptoms can appear relatively shortly after biopsy. This suggests that the rapid formation of an intramural hematoma causes duodenal stenosis with vomiting, and is complicated immediately thereafter by obstructive acute pancreatitis. On the other hand, patients with type B or C IDH preceded by acute pancreatitis or acute exacerbation of chronic pancreatitis often complain only of abdominal pain, and some may complain of mild vomiting or nausea. Moreover, the progression of symptoms is slow in the majority of these patients. We consider that detailed analysis of the findings of various imaging modalities and the clinical course of IDH could lead to a better understanding of the relationship between IDH and acute pancreatitis.
In our case, the patient had no history of underlying diseases or chronic pancreatitis, and had no vascular abnormalities on abdominal angiography. These findings along with his clinical course were consistent with type A IDH. This is the first reported case of type A IDH in which the patient had no underlying diseases, such as coagulation abnormalities, or history of duodenal biopsy. However, as in about one-third of the reported patients, this patient was a heavy drinker. Therefore, the absence of evidence of chronic pancreatitis on different imaging modalities does not exclude the possibility of a causal relationship between IDH and heavy drinking.
Nontraumatic IDH cannot be differentiated from pancreatic cancer, therefore, some patients have been treated by surgical resection in the past[7,12]. However, recent advances in diagnostic imaging techniques have increased the number of patients who show a favorable clinical course after conservative treatment, including US-guided aspiration with endoscopic balloon dilatation of the narrowed duodenal lumen[34,35]. However, some patients with underlying diseases are complicated by severe acute obstructive pancreatitis with an unfavorable outcome[6,31]. We consider that a rapid diagnosis based on the clinical course and findings of different imaging techniques, mainly including US and CT, as well as the time-lapse observation of the hematoma leads to the selection of an appropriate treatment approach.
In conclusion, we encountered a patient with nontraumatic IDH complicated by acute pancreatitis. Despite the few reported cases of IDH with acute pancreatitis, the relationship between the diseases remains unknown. The present analysis of the published cases of IDH with acute pancreatitis provides some information on the pathogenesis of IDH and its relationship with acute pancreatitis.
Footnotes
Peer reviewer: Filippo Cademartiri, MD, PhD, Departmento of Radiology - c/o Piastra Tecnica - Piano 0, Azienda Ospedaliero-Universitaria di Parma, Via Gramsci, 14 - 43100 Parma, Italy
S- Editor Cheng JX L- Editor Kerr C E- Editor Zheng XM
References
- 1.M’Lauchlan J. False aneurysm tumour occupying nearly the whole of the duodenum. Lancet. 1838;2:203–205. [Google Scholar]
- 2.Hayashi K, Futagawa S, Kozaki S, Hirao K, Hombo Z. Ultrasound and CT diagnosis of intramural duodenal hematoma. Pediatr Radiol. 1988;18:167–168. doi: 10.1007/BF02387565. [DOI] [PubMed] [Google Scholar]
- 3.Jewett TC Jr, Caldarola V, Karp MP, Allen JE, Cooney DR. Intramural hematoma of the duodenum. Arch Surg. 1988;123:54–58. doi: 10.1001/archsurg.1988.01400250064011. [DOI] [PubMed] [Google Scholar]
- 4.Aston JK. Computed tomography of obstructive jaundice secondary to duodenal hematoma. J Comput Tomogr. 1986;10:171–173. doi: 10.1016/0149-936x(86)90071-8. [DOI] [PubMed] [Google Scholar]
- 5.Antoniou D, Zarifi M, Gentimi F, Christopoulos-Geroulanos G. Sonographic diagnosis and monitoring of an intramural duodenal hematoma following upper endoscopic biopsy in a child. J Clin Ultrasound. 2009;37:534–538. doi: 10.1002/jcu.20629. [DOI] [PubMed] [Google Scholar]
- 6.Sadry F, Hauser H. Fatal pancreatitis secondary to iatrogenic intramural duodenal hematoma: a case report and review of the literature. Gastrointest Radiol. 1990;15:296–298. doi: 10.1007/BF01888801. [DOI] [PubMed] [Google Scholar]
- 7.Dubois J, Guy F, Porcheron J. A pancreatic-induced intramural duodenal hematoma: a case report and literature review. Hepatogastroenterology. 2003;50:1689–1692. [PubMed] [Google Scholar]
- 8.Kiely PE, Karr GF, O'Shea M. Massive intramural duodenal haemorrhage complications E R C P. Ir J Med Sci. 1982;151:223–224. doi: 10.1007/BF02940186. [DOI] [PubMed] [Google Scholar]
- 9.Ma JK, Ng KK, Poon RT, Fan ST. Pancreatic-induced intramural duodenal haematoma. Asian J Surg. 2008;31:83–86. doi: 10.1016/S1015-9584(08)60063-9. [DOI] [PubMed] [Google Scholar]
- 10.Jones WR, Hardin WJ, Davis JT, Hardy JD. Intramural hematoma of the duodenum: a review of the literature and case report. Ann Surg. 1971;173:534–544. doi: 10.1097/00000658-197104000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diniz-Santos DR, de Andrade Cairo RC, Braga H, Araújo-Neto C, Paes IB, Silva LR. Duodenal hematoma following endoscopic duodenal biopsy: a case report and review of the existing literature. Can J Gastroenterol. 2006;20:39–42. doi: 10.1155/2006/391702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Spreeuwel JP, van Gorp LH, Bast TJ, Nadorp JH. Intramural hematoma of the duodenum in a patient with chronic pancreatitis. Endoscopy. 1981;13:246–248. doi: 10.1055/s-2007-1021697. [DOI] [PubMed] [Google Scholar]
- 13.Patel R, Shaps J. Intramural duodenal hematoma--a complication of ERCP. Gastrointest Endosc. 1982;28:218–219. doi: 10.1016/s0016-5107(82)73074-3. [DOI] [PubMed] [Google Scholar]
- 14.Fingerhut A, Rouffet F, Eugène C, Fendler JP, Hillion D, Ronat R. Nontraumatic intramural hematoma of the duodenum. Report of 4 cases and review of the literature. Digestion. 1983;26:231–235. doi: 10.1159/000198895. [DOI] [PubMed] [Google Scholar]
- 15.Giraud RM, Berzin S, Shein DM. Acute relapsing pancreatitis complicated by ruptured intramural duodenal haematoma. J R Coll Surg Edinb. 1986;31:247–249. [PubMed] [Google Scholar]
- 16.Glassman MS, Rodrigues R, Bussel J, Spivak W, Hilgartner M. Acute obstructive pancreatitis secondary to a duodenal hematoma. J Pediatr Gastroenterol Nutr. 1988;7:619–621. doi: 10.1097/00005176-198807000-00024. [DOI] [PubMed] [Google Scholar]
- 17.Zinelis SA, Hershenson LM, Ennis MF, Boller M, Ismail-Beigi F. Intramural duodenal hematoma following upper gastrointestinal endoscopic biopsy. Dig Dis Sci. 1989;34:289–291. doi: 10.1007/BF01536064. [DOI] [PubMed] [Google Scholar]
- 18.Archer S, Levitt S, Drury P. Duodenal necrosis and intramural haematoma complicating acute pancreatitis. Aust N Z J Surg. 1991;61:542–544. doi: 10.1111/j.1445-2197.1991.tb00286.x. [DOI] [PubMed] [Google Scholar]
- 19.Szajewska H, Albrecht P, Ziolkowski J, Kubica W. Intramural duodenal hematoma: an unusual complication of duodenal biopsy sampling. J Pediatr Gastroenterol Nutr. 1993;16:331–333. [PubMed] [Google Scholar]
- 20.Karjoo M, Luisiri A, Silberstein M, Kane RE. Duodenal hematoma and acute pancreatitis after upper gastrointestinal endoscopy. Gastrointest Endosc. 1994;40:493–495. doi: 10.1016/s0016-5107(94)70219-5. [DOI] [PubMed] [Google Scholar]
- 21.Rohrer B, Schreiner J, Lehnert P, Waldner H, Heldwein W. Gastrointestinal intramural hematoma, a complication of endoscopic injection methods for bleeding peptic ulcers: a case series. Endoscopy. 1994;26:617–621. doi: 10.1055/s-2007-1009050. [DOI] [PubMed] [Google Scholar]
- 22.Lipson SA, Perr HA, Koerper MA, Ostroff JW, Snyder JD, Goldstein RB. Intramural duodenal hematoma after endoscopic biopsy in leukemic patients. Gastrointest Endosc. 1996;44:620–623. doi: 10.1016/s0016-5107(96)70024-x. [DOI] [PubMed] [Google Scholar]
- 23.Guzman C, Bousvaros A, Buonomo C, Nurko S. Intraduodenal hematoma complicating intestinal biopsy: case reports and review of the literature. Am J Gastroenterol. 1998;93:2547–2550. doi: 10.1111/j.1572-0241.1998.00716.x. [DOI] [PubMed] [Google Scholar]
- 24.Worynski A, Zimmerman M, Herrmann RP, Forbes GM. Intramural duodenal haematoma following endoscopic biopsy in a bone marrow transplant patient. Aust N Z J Med. 1998;28:843–844. doi: 10.1111/j.1445-5994.1998.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 25.Fesenmyer ME, Nelson DB. Intramural duodenal hematoma due to pancreatitis. J Clin Gastroenterol. 1998;26:350–352. doi: 10.1097/00004836-199806000-00033. [DOI] [PubMed] [Google Scholar]
- 26.Bellens L, Van Hee R, Vanderstighelen Y, Vanderputte S. Intramural duodenal hematoma of pancreatic origin. Hepatogastroenterology. 1999;46:930–932. [PubMed] [Google Scholar]
- 27.Bodnár Z, Várvölgyi C, Tóth J, Sápy P, Kakuk G. Intramural duodenal hematoma complicating acute necrotizing pancreatitis. Gastrointest Endosc. 2000;52:791–793. doi: 10.1067/mge.2000.109587. [DOI] [PubMed] [Google Scholar]
- 28.Dugernier TL, Breuskin FM. Duodenal air dissection secondary to intramural hematoma in necrotizing pancreatitis. Endoscopy. 2002;34:1024. doi: 10.1055/s-2002-35833. [DOI] [PubMed] [Google Scholar]
- 29.Sgouros SN, Karamanolis G, Papadopoulou E, Papageorgiou G, Stefanides G, Nastos H, Mantides A. Postbiopsy intramural hematoma of the duodenum in an adult with Noonan's syndrome. J Gastroenterol Hepatol. 2004;19:1217–1219. doi: 10.1111/j.1440-1746.2004.02931.x. [DOI] [PubMed] [Google Scholar]
- 30.Borsaru AD, Nandurkar D. Intramural duodenal haematoma presenting as a complication after endoscopic biopsy. Australas Radiol. 2007;51:378–380. doi: 10.1111/j.1440-1673.2007.01692.x. [DOI] [PubMed] [Google Scholar]
- 31.Chen PS, Cheng HC, Sheu BS. Diffuse intramural duodenal hematoma complicated by lethal necrotizing pancreatitis after endoscopic duodenal biopsy. Endoscopy. 2008;40 Suppl 2:E143. doi: 10.1055/s-2007-995736. [DOI] [PubMed] [Google Scholar]
- 32.Fukunaga N, Ishikawa M, Yamamura Y, Ichimori T, Sakata A. Spontaneous intramural duodenal hematoma complicating acute pancreatitis. Surgery. 2009:Epub ahead of print. doi: 10.1016/j.surg.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 33.Abdel Samie A, Sun R, Theilmann L. A rare cause of obstructive jaundice. Gastroenterology. 2009;137:40, 394. doi: 10.1053/j.gastro.2008.12.063. [DOI] [PubMed] [Google Scholar]
- 34.Maemura T, Yamaguchi Y, Yukioka T, Matsuda H, Shimazaki S. Laparoscopic drainage of an intramural duodenal hematoma. J Gastroenterol. 1999;34:119–122. doi: 10.1007/s005350050226. [DOI] [PubMed] [Google Scholar]
- 35.Aizawa K, Tokuyama H, Yonezawa T, Doi M, Matsuzono Y, Matumoto M, Uragami K, Nishioka S, Yataka I. A case of traumatic intramural hematoma of the duodenum effectively treated with ultrasonically guided aspiration drainage and endoscopic balloon catheter dilation. Gastroenterol Jpn. 1991;26:218–223. doi: 10.1007/BF02811084. [DOI] [PubMed] [Google Scholar]