Abstract
Purpose:
To determine the number of specimens to be obtained from pulmonary lesions to get the highest possible accuracy in histological work-up.
Materials and methods:
A retrospective evaluation (January 1999 to April 2004) covered 260 patients with thoracic lesions who underwent computer tomography (CT)-guided core-cut biopsy in coaxial technique. All biopsies were performed utilizing a 19 gauge introducer needle and a 20 gauge core-cut biopsy needle. In all, 669 usable biopsies were taken (from 1–5 biopsies in each setting). The specimens were marked sequentially and each biopsy was worked up histologicaly. The biopsy results were correlated to histology after surgery, clinical follow-up or autopsy. The number of biopsies was determined that is necessary to achieve the highest possible accuracy in diagnosing pulmonary lesions.
Results:
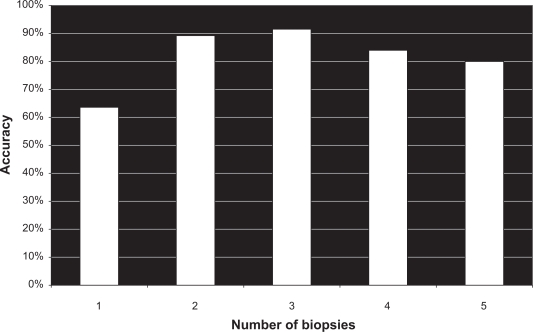
In 591 of 669 biopsies (88.3%), there were correct positive results. The overall accuracy was 87.4%. In 193 of 260 (74.2%) patients, a suspected malignancy was confirmed. In 50 of 260 (19.2%) patients, a benign lesion was correctly diagnosed. Seventeen (6.5%) patients were lost to follow-up. The first, second and third biopsies had cumulative accuracies of 63.6%, 89.2% and 91.5%, respectively (P < 0.02). More biopsies did not show any higher impact on accuracy.
Conclusion:
For the highest possible accuracy in diagnosing pulmonary lesions by CT-guided core-cut biopsy, at least three usable specimens are recommended to be taken.
Keywords: lung biopsy, CT, number of biopsies, thoracic lesions
Introduction
Computed tomography (CT) scan-guided biopsy of thoracic lesions is a widely accepted diagnostic technique.1 Previously, CT scan-guided biopsies were usually performed with fine-needle aspiration and cytological examination to differentiate malignant from benign lesions.2,3 A further development is tissue core biopsy using a cutting needle; this allows histopathological evaluation of the specimen.4 An automated spring-driven cutting needle for tissuecore biopsy has made it easier to obtain satisfactory specimens for histological analysis.5–7 Percutaneous transthoracic biopsy is now more widely performed with helical CT-scanning;2 however, there are other modalities employed for this imaging guided procedure such as fluoroscopy and conventional CT-scanning.1–3
We are unaware of reports in the literature dealing with the number of biopsies in pulmonary lesions required for an accurate histological work up. Therefore, the purpose of our study was to analyse, whether the number of biopsy specimen taken has an impact on diagnostic accuracy at histologic examination.
Materials and Methods
Subjects
From January 1999 to April 2004, 260 patients (mean age of the patients was 64.3 years (range 35–82 years; 158 men and 102 women)) with pulmonary lesions underwent CT-guided core-cut biopsy at our institution. Overall, 669 biopsies were obtained, 1–5 biopsies from each patient at the radiologists’s discretion. None of the patients had severe chronic obstructive disease (COPD), severe emphysema or a coagulopathy. All patients gave written informed consent.
Biopsy Needle
Core-cut biopsy in coaxial technique was performed with a 20-gauge needle (Manan® biopsy needle, Gainsville Florida). The Auto Surecut system (Pro Mag 2.2 Manan®) consists of an outer cutting cannula with a coring point and a trocar with a sharp tip. A closed microsyringe is attached to the outer cutting cannula inside the body of the cutting needle device. The outer cutting cannula is automatically extended to a length of 2.2 cm. At the same time, a vacuum is established in the biopsy canal; the tissue biopsy is obtained by negative pressure at the tip of the outer cannula.
Biopsy Procedure
Before undergoing biopsy all patients had diagnostic helical CT scans (Lightspeed GE, Wisconsin, USA) of the chest with 5 mm slice thickness. These preliminary images were reviewed to plan the level of the needle entry site, patient’s position and the most direct approach for successful biopsy. Patients assumed a supine, prone or lateral position. Experienced interventional radiologists performed all biopsies.
An 19 gauge outer guiding cannula was always used to prevent the flexible 20-gauge needle from deviating into the soft tissue.
Core-cut biopsies were taken with the Auto Surecut system as described previously.
Informed consent was obtained from each patient at least 24 hours before the interventional procedure.
Statistics
All statistical analyses were performed with the statistical software package SPSS version 10.0. The chi square test was applied to analyse dichotomous variables. Statistical significance was considered as P < 0.05.
Results
In 591 of 669 biopsies (88.3%), there were positive results that correlated with and ultimately were confirmed by subsequent surgery, clinical follow-up or autopsy. The accuracy was 87.4%. In 193 of 260 (74.2%) patients, a suspected malignancy was confirmed by surgery. The diagnosis of 13 patients of the surgical group was confirmed additionally by autopsy. In 50 of 260 (19.2%) patients, a benign lesion was correctly diagnosed. They had a follow up period of one year. At the end of one year a CT scan was performed. Seventeen (6.5%) patients were lost to follow-up. The first, second and third biopsies had cumulative accuracies of 63.6%, 89.2% and 91.5%, respectively (P < 0.02) (Fig. 1). In Figures 2 and 3 the number of patients and the number of biopsies that were performed are listed.
Figure 1.
Correlation between number of biopsies and histopathological accuracy of pulmonary nodular lesions. (P < 0.02).
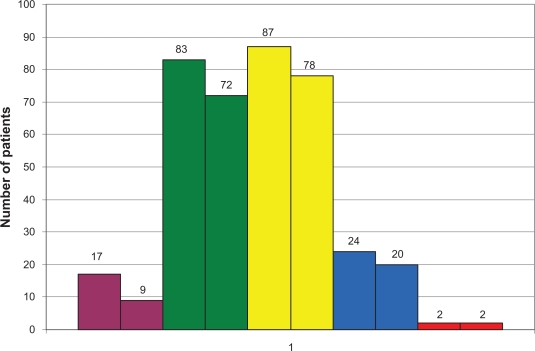
Figure 2.
Number of patients with a histopathological malignancy diagnosed with 1–5 biopsies (first bar) and correct diagnosis after 1–5 biopsies (second bar).
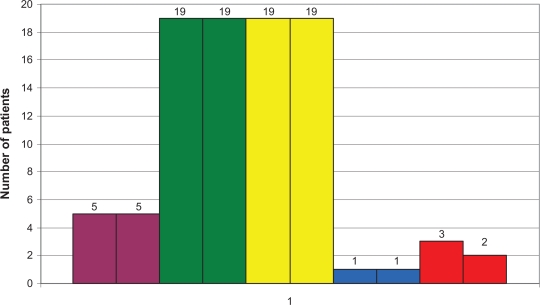
Figure 3.
Number of patients with a histopathological benign diagnosed with 1–5 biopsies (first bar) and correct diagnosis after 1–5 biopsies (second bar).
All histological results are summarized in Figure 3.
The median size of pulmonary nodules was 2.8 cm ± 14.9 (range 0.9–6.3 cm). The median lesion depth was 1.2 cm ± 1.4 (range 0–6 cm). Pneumothorax was the most frequent complication: 87 of 260 patients (33.4%) developed a pneumothorax but only 10 (3.8%) patients required a transthoracal chest tube to evacuate the pneumothorax. The second most frequent complication was haemoptysis in 12 (4.6%) patients, none of whom required any further interventional or surgical treatment (Table 1). Otherwise, there were no serious adverse events.
Table 1.
Histological diagnosis of 260 patients with pulmonary lesions. Specimens obtained by CT-guided core-cut biopsy.
| Histology | |
|---|---|
| Benign | 50 (19.2%) |
| Harmatoma | 7 |
| Wegener’s disease | 2 |
| Sarckoidosis | 2 |
| Amyloidosis | 1 |
| Non-specific* | 38 |
| Lost to follow-up | 0 (0%) |
| Malignant | 193 (74.2%) |
| Adenocarcinoma | 85 |
| Non-small cell | 23 |
| Squamous | 33 |
| Metastasis | 29 |
| Undifferentiated carcinoma | 17 |
| BAC | 5 |
| Lymphoma | 1 |
| Lost to follow-up | 17 (6.5%) |
In the non-specific group no precise diagnosis was obtained by biopsy, but the benign nature of the lesion was confirmed during follow-up period.
Discussion
Percutaneous biopsy of thoracic lesions has become established as an effective and safe procedure. Successful percutaneous needle biopsy of lung lesions has been applied with excellent results and few complications.8–10 The key to these procedures is the imaging guidance, which allows for the safe passage of a needle into the region of interest in the lung. In most settings, percutaneous biopsy is the first approach to diagnosis.
There is little literature dealing with the question of the optimal number of biopsies that should be obtained for the highest possible accuracy, unless a pathologist is on site.
In 669 biopsies, we found that the highest possible accuracy was obtained with three suitable specimens. More biopsies did not have any further impact on diagnostic accuracy. We find it of consequence to obtain three specimens in one setting because the operator uses the same approach via the previously positioned outer cannula. More biopsies do not improve the accuracy in the histopathological work-up. A strong reason for this retrospective result cannot be addressed. One fact we stress is the prefabricated way for the multiple biopsies by the outer cannula. Furthermore we state, that there are different numbers of patients in the different biopsy groups which makes the data less comparable. Statistically, we found a strong indication, that at least three biopsies show the best result in terms of accuracy.
In our cohort, we observed a complication rate in terms of pneumothorax of 33.4%. Twelve patients needed further treatment with a transthoracal chest tube to evacuate the pneumothorax. Our results correlate quite well with the literature, in which the reported frequency of pneumothorax for CT-guided procedures varies from 8% to 64% (Fig. 2).11–15 The median size of our pulmonary nodules was 2.8 cm ± 14.9 (range 0.9–6.3 cm) and the median lesion depth was 1.2 cm ± 1.4 (range 0–6 cm). A lesion size ≤ 2 cm, a lesion depth of 0.1 to 2 cm and less experienced radiologists are given as the strongest parameters predictive of pneumothorax. The highest bleeding risk correlates with a lesion size ≤ 2 cm, a lesion depth of > 2.1 cm and the absence of pleural effusion.16 Finally, for the power of this study it is important to mention the multi—operative specimens obtaining.
The histological results of our cohort also correlate well with those in the literature.17 There is an important advantage to be mentioned in terms of patient’s risks. Obtaining three specimens instead of four or five reduces the risk of bleeding and pneumothorax.
The limits of this study are not only the small patient number. The fact, that there a different numbers of patients in the different study groups makes a reliable statement on the absolute necessary number of core cut biopsies in lung lesions difficult. Therefore we stress the fact to design a lager prospective study with better comparable numbers of patients in the different study groups.
Nevertheless, we find that CT-guided core-cut biopsy of pulmonary nodules is an effective diagnostic tool for diagnosing pulmonary lesions. On the basis of our data a total number of at least three specimens for every CT-guided core-cut biopsy could be recommended on the condition that each core shows a well preserved barrel for histopathological work up. However, further prospective studies with a greater number of patients and a better distribution of the patients between the different biopsy groups will be helpful for the confirmation of this study data.
Table 2.
Synopsis of complication rate in 260 patients undergoing CT-guided core-cut biopsy.
| Complication | |
|---|---|
| Overall | 99 (38.1%) |
| Pneumothorax | 87 (33.4%) |
| Transthoracal chest tube | 10 (3.8%) |
| Haemoptysis | 12 (4.6%) |
Footnotes
Disclosure
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material.
References
- 1.Westcott JL. Percutanous transthoracic needle biopsy. Radiology. 1988;169:593–601. doi: 10.1148/radiology.169.3.3055026. [DOI] [PubMed] [Google Scholar]
- 2.Laurent F, Latrabe V, Vergier B, et al. Percutaneous CT-guided biopsy of the lung: Comparison between aspiration and automated cutting needle using a coaxial technique. Cardiovascular Interventional Radiology. 2000;23:266–72. doi: 10.1007/s002700010067. [DOI] [PubMed] [Google Scholar]
- 3.Westcott JL. Direct percutaneous needle aspiration of localized pulmonary lesions: Results in 422 patients. Radiology. 1980;137:31–5. doi: 10.1148/radiology.137.1.7422857. [DOI] [PubMed] [Google Scholar]
- 4.Greene R, Szyfelbein WM, Isler RJ, et al. Supplementary tissue-core histology from fine-needle transthoracic aspiration biopsy. AJR Am J Roentgenol. 1985;144:787–92. doi: 10.2214/ajr.144.4.787. [DOI] [PubMed] [Google Scholar]
- 5.Klein JS, Salomon G, Stewart EA. Transthoracic needle biopsy with coaxially placed 20-gauge automated cutting needle. Results in 122 patients. Radiology. 1996;198:715–20. doi: 10.1148/radiology.198.3.8628859. [DOI] [PubMed] [Google Scholar]
- 6.Lucidarme O, Howarth N, Finet JF, et al. Intrapulmonary lesions: percutaneous automated biopsy with a detachable, 18-gauge, coaxial cutting needle. Radiology. 1998;207:759–65. doi: 10.1148/radiology.207.3.9609901. [DOI] [PubMed] [Google Scholar]
- 7.Tsukada H, Satou T, Iwashima A, et al. Diagnostic accuarcy of CT-guided automated needle biopsy of lung nodules. AJR Am J Roentgenol. 2000;175:239–43. doi: 10.2214/ajr.175.1.1750239. [DOI] [PubMed] [Google Scholar]
- 8.vanSonnenberg E, Casola G, Ho M, et al. Difficult thoracic lesions: CT-guided biopsy expierence in 150 cases. Radiology. 1988;167:457–61. doi: 10.1148/radiology.167.2.3357956. [DOI] [PubMed] [Google Scholar]
- 9.Goralnik CH, O’Connell DM, Yousef SJ, Haaga JR. CT-guided cutting needle biopsies of selected chest lesions. AJR Am J Roentgenol. 1988;151:903–7. doi: 10.2214/ajr.151.5.903. [DOI] [PubMed] [Google Scholar]
- 10.Wittich GR, Nowels KW, Korn RL, et al. Coaxial transthoracic fine-needle biopsy in patients with a history of malignant lymphoma. Radiology. 1992;183:175–8. doi: 10.1148/radiology.183.1.1549668. [DOI] [PubMed] [Google Scholar]
- 11.Stanley JH, Fish GD, Andriole JG, et al. Lung lesions: cytologic diagnosis by fine-needle biopsy. Radiology. 1987;162:389–91. doi: 10.1148/radiology.162.2.3797651. [DOI] [PubMed] [Google Scholar]
- 12.Li H, Boiselle PM, Shepard JO, Trotman-Dickenson B, McCloud TC. Diagnostic accuracy and safety of CT-guided percutaneous needle aspiration biopsy of the lung: comparison of small and large pulmonary nodules. AJR Am J Roentgenol. 1996;167:105–9. doi: 10.2214/ajr.167.1.8659351. [DOI] [PubMed] [Google Scholar]
- 13.Larscheid RC, Thorpe PE, Scott WJ. Percutaneous transthoracic needle aspiration biopsy: a comprehensive review of its current role in the diagnosis and treatment of lung tumors. Chest. 1998;114:704–9. doi: 10.1378/chest.114.3.704. [DOI] [PubMed] [Google Scholar]
- 14.Larscheid RC, Thorpe PE, Scott WJ. Percutaneous transthoracic needle aspiration biopsy: a comprehensive review of its current role in the diagnosis and treatment of lung tumors. Chest. 1998;114:704–9. doi: 10.1378/chest.114.3.704. [DOI] [PubMed] [Google Scholar]
- 15.Laurent F, Labtrabe V, Vergier B, Michel P. Percutaneous CT-guided biopsy of the lung: comparison between aspiration and automated cutting needles using a coaxial technique. Cardiovasc Intervent Radiol. 2000;23:266–72. doi: 10.1007/s002700010067. [DOI] [PubMed] [Google Scholar]
- 16.Yeow KM, Su IH, Pan KT, et al. Risk Factors of Pneumothorax and Bleeding: Multivariate Analysis of 660 CT-Guided Coaxial Cutting Needle Lung Biopsies. Chest. 2004;126(3):748–54. doi: 10.1378/chest.126.3.748. [DOI] [PubMed] [Google Scholar]
- 17.Baldwin DR, Eaton T, Kolbe J, et al. Management of solitary pulmonary nodules: How do thoracic computed tomography and guided fine needle biopsy influence clinical decisions? Thorax. 2002;57:817–22. doi: 10.1136/thorax.57.9.817. [DOI] [PMC free article] [PubMed] [Google Scholar]