Abstract
Radiation therapy has a major role in the management of breast cancers. However, there is no consensus on how to irradiate and on volume definitions, and there are strong differences in strategies according to different centers and physicians. New treatment protocols and techniques have been used with the principal purpose of decreasing lung and heart toxicity and adapting radiation treatment to patients’ anatomy. There is evidence that indicates internal mammary chain radiotherapy should be used carefully and that high quality techniques should be used for decreasing the dose delivered to the heart. This review of the literature presents the state of the art on breast cancer radiotherapy, with special focus on the indications, techniques, and potential toxicity.
Keywords: Cardiac toxicity, Ejection fraction, Breast cancer, Radiotherapy, Chemotherapy, Herceptin
INTRODUCTION
Adjuvant radiotherapy to the breast plays a significant role in preventing local failure in women with tumorectomy for early stage breast cancer, as well as postmastectomy chest wall irradiation. Following surgery for early breast cancer, breast irradiation decreases the rate of in-breast local recurrence significantly, which has been demonstrated by randomized trials[1]. Results of a meta analysis showed that there were more cardio related deaths in the group of irradiated patients compared with non irradiated patients[2,3], however, in this period old techniques and treatment modalities were used[2]. On the other hand, with new advances in tumor control and long term survival, breast cancer patients have enough time to develop long term complications[3,4]. In some cases, the principal cause of complications is the anti cancer treatment, in others, there is no direct relationship between heart disease and the use of chemotherapy, radiotherapy and/or targeted treatment. Cardiac toxicity represents a multifactorial process with extreme complexity and direct relationship with patients’ anatomy, habits, co morbidities, and risk factors. Also, received treatment, such as anthracycline-based chemotherapy or capecitabine, radiation therapy, hormonal therapy, target treatments such as trastuzumab, can affect cardiac toxicity. Drug-related cardiac toxicity in patients treated with high-dose chemotherapy has been well described for some drugs[4-6]. For others, such as targeted treatment with trastuzumab, studies are beginning[7-9]. The question is how to decrease radiation induced cardiac toxicity using modern techniques of radiotherapy and how we can elucidate predictive factors in some patients indicating they are at risk to develop this kind of toxicity.
BREAST IRRADIATION AFTER BREAST CONSERVING SURGERY
Breast conserving radiotherapy uses tangential fields. Any other beam incidence would lead to useless irradiation of the underlying lung and heart[10]. The possibilities and the limits of commonly used techniques for irradiation of breast with two tangential fields in supine position have been discussed in recent years[11-13]. The volume of irradiated lung, heart, and contralateral breast, must be considered. Treatment-related complications include cardiovascular morbidity that can translate into an increased risk of mortality in the long term[11] and chronic radiation-induced pneumonitis. The early and late complications of radiation are directly related to the patient’s anatomy, total dose delivered, fractionation scheme, and radiation technique.
It can be difficult to understand and represent doses received by organs at risk (OAR) (Table 1). An example is given with the French recommendations, showing there is no clear explanation for which parts of the heart can withstand these doses, for example, coronary arteries or the muscle. Every type of treatment is associated with a different kind of toxicity, and more details are needed to report the doses received by different OAR. For example, concerning lung irradiation, there is a question whether suggested doses should be designated to patients with only breast irradiation or breast and lymph node area radiation.
Table 1.
Doses to organs at risk (OAR) according to recommendations of the French Society of Radiation Oncology
| Lung | V20 < 15%, V30 < 10% |
| Heart | < 35 Gy |
| Liver | V30 < 50% |
| Spinal cord | < 45 Gy |
| Esophagus | Maximum 40 Gy in 15 cm |
| Larynx | < 20% |
| Thyroid | Must be protected |
| Brachial plexus | < 55 Gy |
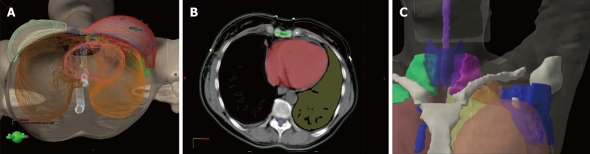
According to some authors, large, pendulous breasts are, in some cases, a contraindication for breast conservation because cosmetic results have been unsatisfactory with increased fibrosis and retraction[12,13]. A number of institutions have reported the use of different techniques to improve the dose distribution within the breast, decrease acute toxicities, decrease the dose to normal tissues and improve the daily reproducibility of women with large breasts[14-21]. Two simple techniques have already been shown to be safe: breast irradiation in a prone position, which is a technique developed in MSCCC, New York, USA, and an isocentric lateral decubitus position founded in the Institute Curie, Paris, France[18-20]. These two techniques were created to prevent lung and heart irradiation. Example of left side breast cancer treated in a lateral decubitus position is given in Figure 1. This treatment is perfectly adapted for breast irradiation only in the elderly, in cases of patients with lung and/or heart co-morbidities, smokers, patients with pendulous breasts, patients treated with chemotherapy, and other specific cases[22]. The limit is that these two techniques are created and adapted to only breast irradiation.
Figure 1.
Patient’s position and dosimetry of patient treated in a lateral position.
For teams without facilities for using the previously described techniques, new developments are also available[21]. Wedges cannot compensate for the change in breast shape in the cranio-caudal direction. A field reduction is necessary at the breast fold to avoid overdosage and treatment complications in this area. Dose uniformity throughout the whole breast volume can be achieved by using MLC sub-fields that are shaped to the successive isodoses found in the dose distribution[23].
The definition of tumor bed “boost” volume is currently also well defined in numerous papers (Figure 2). New techniques such as pre- and post-operative CT scan image registration are used.
Figure 2.

3D reconstruction of boost volume PTV (green) = GTV (red) + CTV clips (yellow), the breast delineation (pink lines) and the relationship between breast volume and boost volume with the cardiac structure[24].
CHEST WALL IRRADIATION AFTER MASTECTOMY AND LYMPH NODE AREAS, INDICATIONS AND NEW TECHNIQUES OF IRRADIATION
The benefit of adjuvant radiotherapy to the chest wall has been controversial for many years. Published data have shown that radiotherapy regimens produced moderate but definite reductions, not only in breast cancer mortality, but also in overall mortality[1,25-29]. The benefit of postmastectomy radiotherapy, independently of the effects of systemic treatment, was shown also in studies of the Danish Breast Cancer Cooperative Group and the British Columbia study[25-31]. However, the first meta-analysis report did not find any advantage in overall survival over 10 and 20 years[2]. One explanation is the increase of non-breast cancer deaths, particularly cardiac disease in relation to older irradiation techniques[2].
Two opposed tangential photon beams is a common technique for postmastectomy radiotherapy to the chest wall[10]. Electron-beam radiotherapy of the chest wall is also used routinely[32-38]. It has been shown that this technique yielded similar loco-regional control, disease free survival and overall survival rates as standard photon beam irradiation[37]. Postmastectomy electron beam chest wall irradiation is well tolerated with low rates of early toxicity events. New developments could continue to improve the previously existing techniques with better dose distribution and decrease of the doses to lung and heart. This is a clinical step towards conformal electron therapy[38,39].
The importance of adjuvant treatment of regional lymph nodes (LN) in N-positive patients, especially with more than 3 involved axillary LN, has already been shown[1]. However, there is no consensus for the adjuvant treatment of internal mammary chain (IMC) and supra and infra clavicular LN, with strong differences in strategies according to centers and physicians. Indications for IMC radiotherapy are debated, since this treatment significantly increases the dose delivered to the heart and leads to potential technical difficulties. Although these data warrant confirmation by the EORTC prospective trial, there is evidence that the indications for IMC radiotherapy should be carefully considered and that high quality techniques should be used for decreasing the dose delivered to the heart. Previously published techniques using electron beams has already been shown to be safe[38].
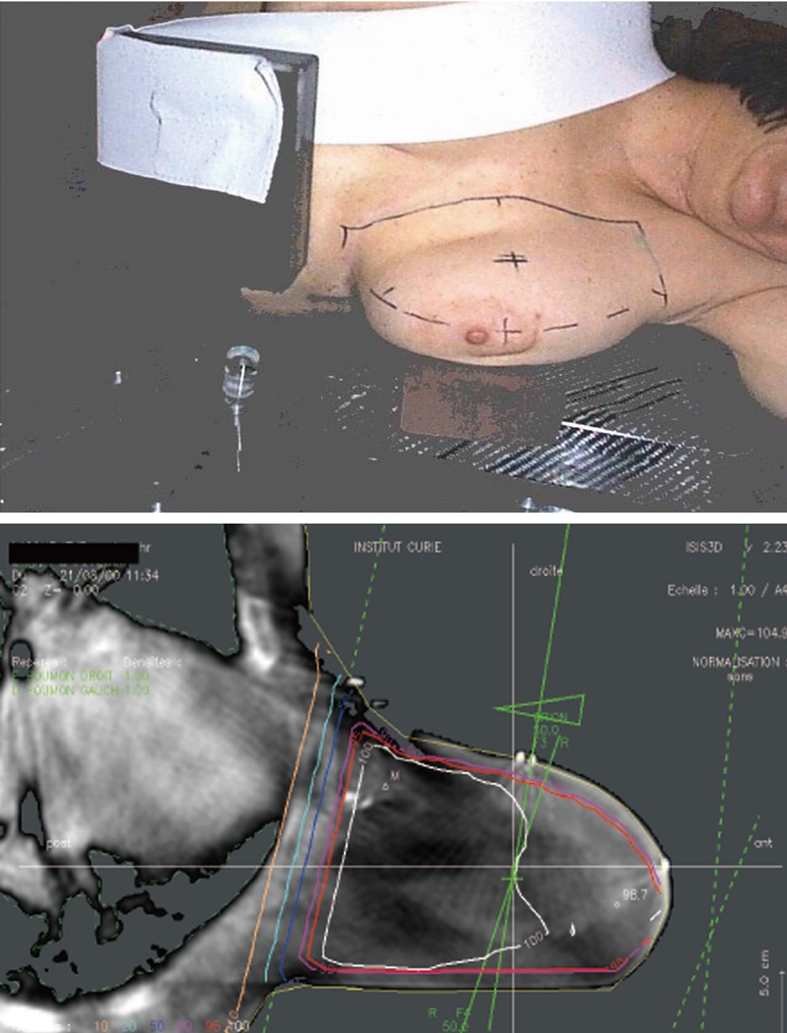
Another revolution in radiotherapy over the last few years is the development of less toxic techniques of irradiation of LN after careful delineation and adaption to the patients’ anatomy[24,40-45] using high performing radiotherapy. Conformal radiotherapy requires definition of target volumes by anatomical limits based on delineation from CT images. Some authors have proposed anatomically based landmarks, specific for breast cancer radiotherapy, to delineate all regional LN[40-43]. Simplified rules of delineation have been developed in our department to delineate lymph node areas before conformal radiotherapy treatment, using easy to find anatomical structures (Table 2 and Figure 3).
Table 2.
Simplified rules delineate the lymph node areas before conformal radiotherapy treatment
| Supra clavicular region: contouring of the supraclavicular region is guided by the origin of the internal mammary artery |
| Cranial: Thyroid cartilage |
| Caudal: Clavicular head |
| Medial (med): Trachea |
| Posterior (post)-lateral (lat): Anterior scalene muscle |
| Post-med: Carotid artery |
| Infra clavicular region: The infraclavicular region corresponds to lymphatic drainage between axillary vertex and the superior limit of the axillary LN dissection (LND) |
| Cranial: Pectoralis minor |
| Caudal: Sternoclavicular joint |
| Lat: Pectoralis minor (medial side) |
| Med: Clavicle |
| Ant: Pectoralis major |
| Post: Axillary artery |
| Internal mammary chain: The lymph nodes of the IMC are located within the anterior interspaces; they are located either medially or laterally to the vessels and are concentrated in the upper three interspaces |
| Ant: Ant. part of the vascular area |
| Post: The pleura |
| Med: Medial limit of the vascular area |
| Lat: Lateral limit of the vascular area |
| Caudal: Superior side of the 4th rib |
| Cranial: Inferior limit of supra clavicular area |
| Rotter LN or intra pectoral node: situated between: pectoralis major and pectoralis minor at the 2nd intercostal space |
| Axilla |
| Ant: Pectoralis major & pectoralis minor |
| Post: Subscapularis, teres major and latissimus dorsi |
| Med: Seratus anterior |
| Lat: 5 mm backward the skin |
| Caudal: 4th and 5th ribs |
| Cranial: Inferior limit of infraclavicular volume or “first clip” after |
| sentinel lymph node procedure |
Figure 3.
3D reconstruction of defined target volumes and the organs of risk. A: The left breast is shown in red, heart in pink, lungs in brown and yellow, thyroid in blue, spinal cord in white; B: Process of practical delineation of breast, lymph nodes and organs of risk; C: 3D reconstruction of defined target LN volumes (supra clavicular LN: fuschia, infra clavicular LN: ochre, axilla: dark blue, internal mammary chain: blue, Rotter LN, white) and thyroid (dark blue) as organ of risk.
CARDIAC TOXICITY RELATED TO CHEMOTHERAPY, TARGETED TREATMENTS, HORMONAL THERAPY
Other adjuvant treatments for breast cancer have been shown to be cardiotoxic. The principal chemotherapy in treatment of breast cancer is still anthracycline-based chemotherapy and the toxicity of this chemotherapy is well known and documented[4-6]. The principal example comes from assessment of cardiac status in long-term survivors of pediatric malignancies who received chemotherapy, including anthracyclines. Steinherz et al[6] have studied 201 patients who had received a total anthracycline dose of 200 mg/m2 to 1275 mg/m2 (median, 450 mg/m2), and 51 patients had mediastinal radiotherapy. The overall incidence and severity of abnormal systolic cardiac function were determined for the entire cohort. Risk factors of total anthracycline dose, mediastinal radiotherapy, age during treatment, and length of follow-up were examined. Twenty-three percent (47/201) of the cohort had abnormal cardiac function on noninvasive testing at long-term follow-up. Correlation between total cumulative dose, length of follow-up, and mediastinal irradiation with incidence of abnormalities was significant. Fifty-six patients were followed up for 10 years or more (median, 12 years), with a median anthracycline dose of 495 mg/m2. Thirty-eight percent (21/56) of these patients, compared with 18% (26/145) of patients evaluated after less than 10 years, had abnormal findings. Sixty-three percent of patients followed up for 10 years or more after receiving 500 mg/m2 or more of anthracyclines had abnormal findings. Nine of 201 patients had late symptoms, including cardiac failure and dysrhythmia, and three patients died suddenly. Microscopic examination of the myocardium on biopsy and autopsy revealed fibrosis. This study illustrates the importance of evaluation of all received treatments and not only one isolated treatment modality.
Other treatments, such as capecitabine, cyclophosphamide, trastuzumab, have also shown cardiac toxicity. Provided that the technique is adapted, the acute skin and heart toxicities of the concomitant administration of trastuzumab-RT appeared satisfactory[8].
PATIENTS’ CO MORBIDITIES
Currently, patients at high risk for cardiac toxicity from usual chemotherapy are evaluated by an anesthesiologist before their surgical procedure and are also evaluated by their oncologist with test results from ejection fraction, electrocardiogram and anamnesis of history of cardiac disease.
There is a trend towards cardiac toxicity in patients with a past history of low ejection fraction, although seemingly poor cardiac risk patients may fare well with high doses of chemotherapy if carefully selected with the aid of a thorough cardiac evaluation with electrocardiogram and cardiac ultrasound. Currently, in our department, in the case of concomitant systemic treatment and radiotherapy, left ventricular ejection fractions, assessed at baseline, before start of RT, after completion of RT and then every 4-6 mo with either echocardiography or multiple gated acquisition scanning, were considered normal if ≥ 50% or stated so by the cardiologist.
At the same time, other risk factors, such as obesity, known cardiac and vascular dysfunction and smoking history must be evaluated.
CONCLUSION
Improvements in breast cancer radiotherapy in the last few years have been spectacular. This fact probably will result in decreasing the side effects of radiation treatment and will improve the quality of life of treated patients with lower rates of side effects. At the same time, the evaluation of long term side effects of new systemic treatments, such as chemotherapy, new targeted drugs, and hormonal treatments, is needed.
Acknowledgments
To all on the team of breast cancer radiotherapy (Fourquet A, Fournier-Bidoz N, Campana F, Bollet M, Dendale R, Castro Pena P, Peurien D, Lelievre H, Stilhart A, Brunet Y).
Footnotes
Peer reviewers: Cem Onal, MD, Department of Radiation Oncology, Adana Research and Treatment Centre, Baskent University Medical Faculty, 01120 Yuregir, Adana, Turkey; Ioannis Valais, PhD, Department of Medical Instrument Technology, Technological Educational Institution of Athens, Ag Spyridonos & Dimitsanis, Egaleo, Athens, 12210, Greece; Ragab Hani Donkol, Professor, Radiology Department, Aseer Central Hospital, 34 Abha, Saudi Arabia; Wellington P Martins, PhD, Departamento de Ginecologia e, Obstetrícia da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, Avenida dos Bandeirantes 3900, 8º andar, Ribeirão Preto, São Paulo 14049-900, Brazil
S- Editor Cheng JX L- Editor Lutze M E- Editor Zheng XM
References
- 1.Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, Godwin J, Gray R, Hicks C, James S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366:2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 2.Darby S. The Early Breast Cancer Trialists¡¯ Collaborative Group (EBCTCG): Late complications of radiation therapy, ESTRO Course: Multidisciplinary management of breast cancer. Lisbon, 2009. [Google Scholar]
- 3.Darby SC, McGale P, Taylor CW, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005;6:557–565. doi: 10.1016/S1470-2045(05)70251-5. [DOI] [PubMed] [Google Scholar]
- 4.Brockstein BE, Smiley C, Al-Sadir J, Williams SF. Cardiac and pulmonary toxicity in patients undergoing high-dose chemotherapy for lymphoma and breast cancer: prognostic factors. Bone Marrow Transplant. 2000;25:885–894. doi: 10.1038/sj.bmt.1702234. [DOI] [PubMed] [Google Scholar]
- 5.Gianni L, Norton L, Wolmark N, Suter TM, Bonadonna G, Hortobagyi GN. Role of anthracyclines in the treatment of early breast cancer. J Clin Oncol. 2009;27:4798–4808. doi: 10.1200/JCO.2008.21.4791. [DOI] [PubMed] [Google Scholar]
- 6.Steinherz LJ, Steinherz PG, Tan CT, Heller G, Murphy ML. Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA. 1991;266:1672–1677. [PubMed] [Google Scholar]
- 7.Alm El-Din MA, Bellon JR, Strom EA, Bourgier C, Jagsi R, Niemierko A, Marsiglia H, Pierce L, Buchholz TA, Taghian AG. Radiation treatments may contribute to the development of cardiac dysfunction in breast cancer patients yreated with chemotherapy and trastuzumab. Int J Radiat Oncol Biol Phys. 2008;72:S89–S90. [Google Scholar]
- 8.Kirova YM, Caussa L, Granger B, Savignoni A, Dendale R, Campana F, Tournat H, Pierga JY, Fourquet A, Bollet MA. [Monocentric evaluation of the skin and cardiac toxicities of the concomitant administration of trastuzumab and radiotherapy] Cancer Radiother. 2009;13:276–280. doi: 10.1016/j.canrad.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Bellon JR, Gover MT, Burstein HJ, Harris JR, Harris LN. Concurrent trastuzumab and radiation therapy (RT) in the adjuvant treatment of breast cancer. Int J Radiat Oncol Biol Phys. 2005;63:S55–S56. [Google Scholar]
- 10.Halperin EC, Perez CA, Brady LW, Wazer DE. Principles and practice of radiation oncology. Lippincott Williams & Wilkins. 2008. [Google Scholar]
- 11.Krasin M, McCall A, King S, Olson M, Emami B. Evaluation of a standard breast tangent technique: a dose-volume analysis of tangential irradiation using three-dimensional tools. Int J Radiat Oncol Biol Phys. 2000;47:327–333. doi: 10.1016/s0360-3016(00)00449-1. [DOI] [PubMed] [Google Scholar]
- 12.Leonardi MC, Brambilla MG, Zurrida S, Intra M, Frasson A, Severi G, Robertson C, Orecchia R. Analysis of irradiated lung and heart volumes using virtual simulation in postoperative treatment of stage I breast carcinoma. Tumori. 2003;89:60–67. doi: 10.1177/030089160308900113. [DOI] [PubMed] [Google Scholar]
- 13.Lu XQ, Sullivan S, Eggleston T, Holupka E, Bellerive M, Abner A, Lamb CC, Lee A, Stevenson MA, Recht A. A three-field breast treatment technique with precise geometric matching using multileaf collimator-equipped linear accelerators. Int J Radiat Oncol Biol Phys. 2003;55:1420–1431. doi: 10.1016/s0360-3016(02)04514-5. [DOI] [PubMed] [Google Scholar]
- 14.Harris JR, Levene MB, Svensson G, Hellman S. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979;5:257–261. doi: 10.1016/0360-3016(79)90729-6. [DOI] [PubMed] [Google Scholar]
- 15.Prosnitz LR, Goldenberg IS, Harris JR, Hellman S, Danoff BF, Kramer S, Wallner PE, Brady LW. Radiotherapy for carcinoma of the breast instead of mastectomy. An update. Front Radiat Ther Oncol. 1983;17:69–75. doi: 10.1159/000407279. [DOI] [PubMed] [Google Scholar]
- 16.Cross MA, Elson HR, Aron BS. Breast conservation radiation therapy technique for women with large breasts. Int J Radiat Oncol Biol Phys. 1989;17:199–203. doi: 10.1016/0360-3016(89)90389-1. [DOI] [PubMed] [Google Scholar]
- 17.Mazonakis M, Varveris H, Damilakis J, Theoharopoulos N, Gourtsoyiannis N. Radiation dose to conceptus resulting from tangential breast irradiation. Int J Radiat Oncol Biol Phys. 2003;55:386–391. doi: 10.1016/s0360-3016(02)04206-2. [DOI] [PubMed] [Google Scholar]
- 18.Grann A, McCormick B, Chabner ES, Gollamudi SV, Schupak KD, Mychalczak BR, Heerdt AS, Merchant TE, Hunt MA. Prone breast radiotherapy in early-stage breast cancer: a preliminary analysis. Int J Radiat Oncol Biol Phys. 2000;47:319–325. doi: 10.1016/s0360-3016(00)00448-x. [DOI] [PubMed] [Google Scholar]
- 19.Merchant TE, McCormick B. Prone position breast irradiation. Int J Radiat Oncol Biol Phys. 1994;30:197–203. doi: 10.1016/0360-3016(94)90535-5. [DOI] [PubMed] [Google Scholar]
- 20.Campana F, Kirova YM, Rosenwald JC, Dendale R, Vilcoq JR, Dreyfus H, Fourquet A. Breast radiotherapy in the lateral decubitus position: A technique to prevent lung and heart irradiation. Int J Radiat Oncol Biol Phys. 2005;61:1348–1354. doi: 10.1016/j.ijrobp.2004.08.051. [DOI] [PubMed] [Google Scholar]
- 21.Fournier-Bidoz N, Kirova Y, Campana F, El Barouky J, Zefkili S, Dendale R, Bollet MA, Mazal A, Fourquet A. Technique alternatives for breast radiation oncology: Conventional radiation therapy to tomotherapy. J Med Phys. 2009;34:149–152. doi: 10.4103/0971-6203.54849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bollet MA, Campana F, Kirova YM, Dendale R, Saliou MG, Rosenwald JC, Fourquet A. Breast radiotherapy in women with pectus excavatum (funnel chest): is the lateral decubitus technique an answer? A dosimetric study. Br J Radiol. 2006;79:785–790. doi: 10.1259/bjr/23839243. [DOI] [PubMed] [Google Scholar]
- 23.Vicini FA, Sharpe M, Kestin L, Martinez A, Mitchell CK, Wallace MF, Matter R, Wong J. Optimizing breast cancer treatment efficacy with intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2002;54:1336–1344. doi: 10.1016/s0360-3016(02)03746-x. [DOI] [PubMed] [Google Scholar]
- 24.Kirova YM, Fournier-Bidoz N, Servois V, Laki F, Pollet GA, Salmon R, Thomas A, Dendale R, Bollet MA, Campana F, et al. How to boost the breast tumor bed? A multidisciplinary approach in eight steps. Int J Radiat Oncol Biol Phys. 2008;72:494–500. doi: 10.1016/j.ijrobp.2007.12.059. [DOI] [PubMed] [Google Scholar]
- 25.Gebski V, Lagleva M, Keech A, Simes J, Langlands AO. Survival effects of postmastectomy adjuvant radiation therapy using biologically equivalent doses: a clinical perspective. J Natl Cancer Inst. 2006;98:26–38. doi: 10.1093/jnci/djj002. [DOI] [PubMed] [Google Scholar]
- 26.Overgaard M, Hansen PS, Overgaard J, Rose C, Andersson M, Bach F, Kjaer M, Gadeberg CC, Mouridsen HT, Jensen MB, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337:949–955. doi: 10.1056/NEJM199710023371401. [DOI] [PubMed] [Google Scholar]
- 27.Overgaard M, Jensen MB, Overgaard J, Hansen PS, Rose C, Andersson M, Kamby C, Kjaer M, Gadeberg CC, Rasmussen BB, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999;353:1641–1648. doi: 10.1016/S0140-6736(98)09201-0. [DOI] [PubMed] [Google Scholar]
- 28.Ragaz J, Jackson SM, Le N, Plenderleith IH, Spinelli JJ, Basco VE, Wilson KS, Knowling MA, Coppin CM, Paradis M, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337:956–962. doi: 10.1056/NEJM199710023371402. [DOI] [PubMed] [Google Scholar]
- 29.Cuzick J, Stewart H, Rutqvist L, Houghton J, Edwards R, Redmond C, Peto R, Baum M, Fisher B, Host H. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994;12:447–453. doi: 10.1200/JCO.1994.12.3.447. [DOI] [PubMed] [Google Scholar]
- 30.Pierce LJ. The use of radiotherapy after mastectomy: a review of the literature. J Clin Oncol. 2005;23:1706–1717. doi: 10.1200/JCO.2005.08.109. [DOI] [PubMed] [Google Scholar]
- 31.Recht A, Edge SB, Solin LJ, Robinson DS, Estabrook A, Fine RE, Fleming GF, Formenti S, Hudis C, Kirshner JJ, et al. Postmastectomy radiotherapy: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol. 2001;19:1539–1569. doi: 10.1200/JCO.2001.19.5.1539. [DOI] [PubMed] [Google Scholar]
- 32.Gaffney DK, Prows J, Leavitt DD, Egger MJ, Morgan JG, Stewart JR. Electron arc irradiation of the postmastectomy chest wall: clinical results. Radiother Oncol. 1997;42:17–24. doi: 10.1016/s0167-8140(96)01860-9. [DOI] [PubMed] [Google Scholar]
- 33.Gaffney DK, Leavitt DD, Tsodikov A, Smith L, Watson G, Patton G, Gibbs FA, Stewart JR. Electron arc irradiation of the postmastectomy chest wall with CT treatment planning: 20-year experience. Int J Radiat Oncol Biol Phys. 2001;51:994–1001. doi: 10.1016/s0360-3016(01)01726-6. [DOI] [PubMed] [Google Scholar]
- 34.Magee B, Ribeiro GG, Williams P, Swindell R. Use of an electron beam for post-mastectomy radiotherapy: 5-year follow-up of 500 cases. Clin Oncol (R Coll Radiol) 1991;3:310–314. doi: 10.1016/s0936-6555(05)80581-3. [DOI] [PubMed] [Google Scholar]
- 35.Hehr T, Budach W, Paulsen F, Gromoll C, Christ G, Bamberg M. Evaluation of predictive factors for local tumour control after electron-beam-rotation irradiation of the chest wall in locally advanced breast cancer. Radiother Oncol. 1999;50:283–289. doi: 10.1016/s0167-8140(99)00016-x. [DOI] [PubMed] [Google Scholar]
- 36.Feigenberg SJ, Price Mendenhall N, Benda RK, Morris CG. Postmastectomy radiotherapy: patterns of recurrence and long-term disease control using electrons. Int J Radiat Oncol Biol Phys. 2003;56:716–725. doi: 10.1016/s0360-3016(03)00112-3. [DOI] [PubMed] [Google Scholar]
- 37.Gez E, Assaf N, Bar-Deroma R, Rosenblatt E, Kuten A. Postmastectomy electron-beam chest-wall irradiation in women with breast cancer. Int J Radiat Oncol Biol Phys. 2004;60:1190–1194. doi: 10.1016/j.ijrobp.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 38.Kirova YM, Campana F, Fournier-Bidoz N, Stilhart A, Dendale R, Bollet MA, Fourquet A. Postmastectomy electron beam chest wall irradiation in women with breast cancer: a clinical step toward conformal electron therapy. Int J Radiat Oncol Biol Phys. 2007;69:1139–1144. doi: 10.1016/j.ijrobp.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 39.Campana F, Kirova YM, Zervoudis S, Assi H, Fournier-Bidoz N, Dendale R, Iatrakis G, Bollet M, Kvrgins G, Peitsidis P, et al. Postmastectomy electron-beam chest wall irradiation in women with breast cancer: early and late complications. Gyneco Ro. 2007;3:170–173. [Google Scholar]
- 40.Kirova YM, Castro Pena P, Dendale R, Servois V, Bollet MA, Fournier-Bidoz N, Campana F, Fourquet A. Simplified rules for everyday delineation of lymph node areas for breast cancer radiotherapy. Br J Radiol. 2009:Epub ahead of print. doi: 10.1259/bjr/28834220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kirova YM, Castro Pena P, Dendale R, Campana F, Bollet MA, Fournier-Bidoz N, Fourquet A. [Definition of nodal volumes in breast cancer treatment and segmentation guidelines] J Radiol. 2009;90:747–751. doi: 10.1016/s0221-0363(09)74733-x. [DOI] [PubMed] [Google Scholar]
- 42.Kirova YM, Servois V, Campana F, Dendale R, Bollet MA, Laki F, Fournier-Bidoz N, Fourquet A. CT-scan based localization of the internal mammary chain and supra clavicular nodes for breast cancer radiation therapy planning. Radiother Oncol. 2006;79:310–315. doi: 10.1016/j.radonc.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 43.Madu CN, Quint DJ, Normolle DP, Marsh RB, Wang EY, Pierce LJ. Definition of the supraclavicular and infraclavicular nodes: implications for three-dimensional CT-based conformal radiation therapy. Radiology. 2001;221:333–339. doi: 10.1148/radiol.2212010247. [DOI] [PubMed] [Google Scholar]
- 44.Martinez-Monge R, Fernandes PS, Gupta N, Gahbauer R. Cross-sectional nodal atlas: a tool for the definition of clinical target volumes in three-dimensional radiation therapy planning. Radiology. 1999;211:815–828. doi: 10.1148/radiology.211.3.r99jn40815. [DOI] [PubMed] [Google Scholar]
- 45.Castro Pena P, Kirova YM, Campana F, Dendale R, Bollet MA, Fournier-Bidoz N, Fourquet A. Anatomical, clinical and radiological delineation of target volumes in breast cancer radiotherapy planning: individual variability, questions and answers. Br J Radiol. 2009;82:595–599. doi: 10.1259/bjr/96865511. [DOI] [PubMed] [Google Scholar]