Abstract
Hepatocellular carcinoma (HCC) is one of most common malignancies in the world. Systemic treatments for HCC, particularly for advanced stages, are limited by the drug resistance phenomenon which ultimately leads to therapy failure. Recent studies have indicated an association between drug resistance and the existence of the cancer stem cells (CSCs) as tumor initiating cells. The CSCs are resistant to conventional chemotherapies and might be related to the mechanisms of the ATP Binding Cassette (ABC) transporters and alterations in the CSCs signaling pathways. Therefore, to contribute to the development of new HCC treatments, further information on the characterization of CSCs, the modulation of the ABC transporters expression and function and the signaling pathway involved in the self renewal, initiation and maintenance of the cancer are required. The combination of transporters modulators/inhibitors with molecular targeted therapies may be a potent strategy to block the tumoral progression. This review summarizes the association of CSCs, drug resistance, ABC transporters activities and changes in signaling pathways as a guide for future molecular therapy for HCC.
Keywords: Hepatocellular carcinoma, Liver, Cancer stem cells, Drug resistance, Hepatocellular carcinoma therapy
INTRODUCTION
Primary liver cancer is the fifth most common neoplasm in the world and the third most common cause of cancer-related death[1]. Approximately more than 500 000 new cases are diagnosed per year[2]. Hepatocellular carcinoma (HCC) accounts for 85% to 90% of primary liver cancers[3]. Several major risk factors for HCC are known, the main ones are liver cirrhosis due to viral infections hepatitis B virus (HBV) or/and hepatitis C virus (HCV), excessive alcohol consumption, aflatoxin B and vinyl-chloride monomer[4], obesity-related disease and familial-related disorders such as primary hemochromatosis[5]. In Asia and Africa, as much as 70% of HCC is caused by the HBV infection, while in Europe and North America 50%-70% is caused by HCV infection[2,6]. HCC without liver cirrhosis is also found although the annual HCC incidence is much lower than HCC with cirrhosis[7] indicating that chronic necro-inflammation is a key element of the occurrence of disease[8].
Until now, main treatments for HCC are surgical intervention (liver resection and liver transplantation) and local radiofrequency ablation. These approaches are curative only for localized small liver tumors, preferably in early stage (monofocal) when patients have a good life expectancy. In contrast, potential treatments for more advanced stages of HCC are more difficult. For HCC patients who cannot have any surgical intervention, survival has not significantly increased in the past 30 years[9].
Systemic treatment for more advanced stages of HCC is given as another option, although there are many limitations and the prognosis of unresectable HCC remains poor. Many chemotherapeutic agents have been tested but the response rate is still low, ranging between 10% and 15%[10]. Significant toxicity and decrease of the efficiency of the drugs also become limitations.
One of the most studied chemotherapeutic agents for cancer treatment for over 30 years is doxorubicin. A report from a phase III trial in unresectable HCC patients compared the administration of doxorubicin as single-agent therapy and combination regimen therapy PIAF [cisplatin/interferon/doxorubicin (Adriamycin)/5-fluoruacil (5-FU)]. Although patients on PIAF showed a higher overall response rate (20.9%) than patients on doxorubicin alone (10.9%), the difference was not significant[11]. Since both single and combination therapies showed serious toxicity and an overall disappointing survival rate, the use of this systemic treatment should be carefully considered.
CANCER STEM CELLS
Stem cells are non-specialized cells which have potential capabilities to self-renew, differentiate into multiple cell types and proliferate extensively. They serve as the source of all cells types and have the capacity to divide without limit to replace damaged cells or generate new cells and tissues. These unique characteristics offer valuable advantages in regenerative medicine, tissue engineering and biotechnology applications[12]. Many studies demonstrate that stem/progenitor cells derived from several organs can replenish and express molecular characteristic and biological functions of adult cells. This benefit provides the basis for attempts for stem cell therapy in various diseases.
On the other hand, if some mutations alter the genetic properties of the stem cells, they can become tumorigenic and may initiate cancer (Figure 1). These so-called cancer stem cells (CSCs) still possess the whole capacity as normal stem cells to proliferate and develop heterogeneous lineages of cancer cells that comprise the tumor[13]. CSCs are suggested to be one of the main players in the initial growth and maintenance of cancer. Evidences of CSCs were observed in the hematopoietic system[14-18] as well as in solid tumors breast[19], brain[20,21], prostate[22,23], gastric[24], lung[25], colon[26,27] and liver[28-32,41]. Many cancers are composed of heterogeneous lineages of stem cells, progenitor cells, less differentiated cells and differentiated cancer cells. Cancer is compiled by various types of cells, at different stages of differentiation and with different functions.
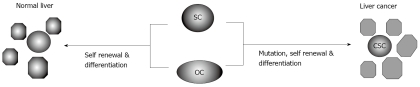
Figure 1.
The liver cancer initiation hypothesis based on CSCs theory. The hepatic stem cells (SC) and oval progenitor (OC) cells have specific capacities to self renew and differentiate into multiple hepatic lineages. Mutations in SC and/or OC may modify the cells genetic property and switch the normal SC into CSCs leading to tumor initiation.
Current studies on several cancer types have revealed that CSCs are resistant to chemotherapy and radiotherapy. In chronic myeloid leukemia (CML), cells expressing CD34 remained viable in a quiescent state even in the presence of tyrosine kinase inhibitor STI571, a common drug for CML[33]. In HCC, purified cells expressing CD133 isolated from human cell line and xenograft mouse model survived chemotherapeutic agents doxorubicin and fluorouracil in a higher percentage compared to most tumor cells without CD133 phenotype[34]. Studies in glioblastoma demonstrated that CD133-positive cells were also resistant to radiotherapy. They were enriched after radiation and preferentially activated the DNA damage checkpoint and repaired radiation-induced DNA damage more efficiently than CD133-negative cells[35]. This mechanism is suggested to be a defense system of the cells.
Because CSCs are important in the initiation and maintenance of the cancer, their resistance to anticancer drugs is an obstacle for the total eradication of cancer. Conventional chemotherapies may recognize and kill most of bulk (differentiated) tumor cells but spare the CSCs. Therefore, to achieve a complete response in cancer therapy, it is crucial to target the CSCs first to eradicate the source of the cancer and then the more differentiated tumor cells.
CANCER STEM CELLS IN HCC
The common normal hepatic stem/progenitor cells candidates are proposed to be localized at the junction of the bile ducts and hepatic cords, known as canal of Hering[36]. The origin of stem cells in the liver has been a subject of discussion as to whether they are real resident hepatic stem cells or derived from bone marrow stem cells migrated to the liver. Different studies report that the progenitor cells population share phenotypic markers between common hematopoietic stem cells with the real hepatic markers.
A population of progenitor cells from adult liver identified as human liver stem cells (HLSCs) was reported. These cells expressed the mesenchymal stem cell markers CD29, CD73, CD44 and CD90 (Thy-1), but not hematopoietic stem cells markers CD34, CD117 (c-kit) and CD133 (Prominin-1). The HLSCs had multipotent capacities for hepatocytes, osteogenic, adipogenic and endothelial differentiation in vitro. In vivo, HLSCs contributed to mouse liver regeneration[37]. In contrast, the multipotent progenitor cells population originating from fetal liver expressed CD117 and CD34 markers. These cells had the capacity to differentiate to liver and mesenchymal cell lineages and replenish functional hepatocyes in vivo[38,39]. Interestingly, a study performed in a rat liver injury model characterized two distinct liver progenitor subpopulations of hematopoietic and hepatic origins. The hepatic (oval) progenitor cells population needed hepatic niche to proliferate in vitro while hematopoietic stem cells had a limited capacity to replicate and differentiate to hepatic lineage[40].
In HCC, surface marker CD133 is one of the most studied markers of the CSCs. CD133 was also identified as a CSCs marker in human leukemia, brain tumor, prostate cancer and laryngeal tumor. In the liver, CD133+ cells possess higher proliferative output, greater capacity to form colonies and greater ability to induce tumor in vivo compared with CD133- cells[28,31,41]. Together with aldehyde dehydrogenase (ALDH), a hierarchical organization characterizing the tumorigenic hepatic CSCs population CD133+ALDH+ > CD133+ALDH- > CD133-ALDH- was reported[42]. ALDH has been identified to be highly expressed in embryonic tissue as well as in adult stem cells[43]. Reactivated CD133+ cells were frequently present in HCC and increased CD133 expression corresponded with higher stage tumors and indicated a poor prognosis for patients[44].
Other studies have proposed surface marker CD90 (Thy-1) since CD90+ cells, but not CD90- cells, from HCC cell lines could induce tumor growth in vivo, and the number of injected cells paralleled with tumorigenicity. The detection of CD45-CD90+ cells in either tumor or blood was proposed to be a highly sensitive and specific circulating marker for the diagnosis of liver cancer[29,45].
A gene expression study showed molecular signature of hepatic progenitor cells including the presence of stem markers such as cytokeratin 19 (K19) and c-kit (CD117) in EpCAM+ HCC while EpCAM- HCC displayed features of mature hepatocytes. This result proposed EpCAM as one of the stem cells markers. The EpCAM+ cells also showed Wnt/β-catenin signaling activation[46]. The cells with EpCAM and alpha fetoprotein (AFP) co-expression had the capabilities to self-renew, differentiate and initiate highly invasive HCC in mice[47]. In human hepatic adenoma and focal nodular hyperplasia, distinct cytokeratin 7 (K7) and K19, together with neuronal cell adhesion molecule expression, suggested different subsets of hepatic progenitor cells[48].
Tumorigenesis consists of a multisteps process from normal to cancerous cells. Wide variations in the HCC prognosis among individuals imply that HCC may have different phenotypes. A genomic study using oligonucleotide microarrays revealed 2 subtypes of HCC with different prognosis. Individuals in subtype sharing a gene expression pattern with fetal hepatoblast had a poor prognosis compared to another subtype which shared pattern with adult hepatocytes. This hepatoblast subtype may arise from bipotent progenitor cells. These cells highly expressed the K7 and K19 markers for early hepatoblast and mature hepatic progenitor cells[49,50]. K7 and K19 were also associated as a predictor of postoperative recurrence due to increased invasiveness[51,52].
However, the heterogeneity and hierarchy of liver cancer remain elusive and the characteristic of the hepatic CSCs is still unclear. Although several biological markers have been proposed to identify the hepatic CSCs, supporting data are contradictory and no agreement has been reached. In addition, the markers between normal stem cells and CSCs markers might overlap. The CSCs characterizations which distinguish them from normal stem cells will be significantly important.
ABC TRANSPORTERS AND DRUG RESISTANCE
The ATP Binding Cassette (ABC) transporters are one of the largest families of membrane transport proteins. These proteins utilize a pair ATP (Adenosine-5’-triphosphate) molecule to export specific compounds or to flip them from inner to outer leafs of the membranes[53]. Thus, they are responsible for translocations of various substrates such as metal ions, sugars, peptides, proteins, amino acids and a large number of hydrophobic compounds and metabolites across the membrane barrier[54]. In humans, there are 49 members of ABC transporters gene which are classified into seven subfamilies based on the sequence homology and ATP-binding proteins[55], as described in Table 1.
Table 1.
Human ABC transporter genes and proteins conferred drug resistance
| Official symbol | Alternative name | Members | Proteins associated with drug resistance | Resistant drugs |
| ABCA | 13 (ABCA1 to ABCA13) | ABCA2 | Mitoxantrone | |
| ABCB | MDR | 11 (ABCB1 to ABCB11) | ABCB1 (MDR1/PGP) | Doxorubicin, colchicine, etoposide, paclitaxel, cisplatin, methotrexate, daunorubicin, camptothecin |
| ABCB11 (BSEP) | 5-fluorouracil, paclitaxel | |||
| ABCC | MRP | 13 (ABCC1 to ABCC13) | ABCC1 (MRP1) | Doxorubicin, daunorubicin, methotrexate, colchicine |
| ABCC2 (MRP2) | Doxorubicin, cisplatin, etoposide | |||
| ABCC3 (MRP3) | Methotrexate, etoposide | |||
| ABCC6 (MRP6) | Etoposide | |||
| ABCC10 (MRP7) | Vinorelbine, paclitaxel, docetaxel | |||
| ABCC11 (MRP8) | 5-fluorouracil, tamoxifen, paclitaxel | |||
| ABCD | ALD | 4 (ABCD1 to ABCD4) | ||
| ABCE | OABP | 1 (ABCE1) | ||
| ABCF | GCN20 | 3 (ABCF1 to ABCF3) | ||
| ABCG | White | 5 (ABCG1, ABCG2, ABCG4, ABCG5, ABCG8) | ABCG2 (BCRP) | Mitoxantrone, topotecan, doxorubicin, daunorubicin, cisplatin, etoposide |
The ABC genes are composed either as full transporters containing two transmembrane domains (TM) and two nucleotide binding folds (NBF) domains or as half transporters containing one of each TM and NBF[56]. While NBFs are responsible for the binding and hydrolysis of ATP creating the motional force, TM builds the translocation pathway for compound translocation[57].
The main role of the ABC transporters is to protect the cells from accumulation of toxic compounds since these proteins have the capacity to export drugs and decrease the cell sensitivity to drugs. This explains the close association between ABC transporters proteins and drug resistance (Table 1). Extensive reviews on the molecular basis of the multidrug transport by ABC transporters are available[57].
Many normal stem cells and cancer cells express high level of specific ABC transporters[58]. Some ABC transporters such as multidrug resistance 1 (ABCB1/MDR1/PGY1), multidrug resistance-associated protein-1 (ABCC1/MRP1), multidrug resistance-associated protein-3 (ABCC3/MRP3) and breast cancer resistance protein (ABCG2/BCRP/MXR) were found in hepatic progenitor cells and hepatocytes in severe liver diseases[59,60]. ABCB1 was expressed primarily in the liver and blood brain barrier and supposed to be involved in cell protection[54]. ABCB1 over expression in drug resistant cells has been studied for more than 20 years[61]. This protein has broad substrates specificity and mediates resistance to a wide variety of drugs such as doxorubicin, colchicines, vinblastine and many more. In HCC, the expression of ABCB1 is variable, being either high or low expressed, or even not expressed. A study showed that ABCB1 over-expression was associated with HCC aggressiveness and reduction of survival, and ABCB1 was proposed as a prognostic marker after surgical resection in patients[62]. In contrast, another study showed that ABCB1 was less expressed in HCC than non tumorous tissue and not related with a more aggressive tumor phenotype and survival[63]. Since ABCB1 expression is closely associated with histological cellular differentiation[64], this could be the reason of the divergent expression among individuals with different HCC phenotypes. Another explanation might be the presence of the polymorphisms of ABCB1. The association between HCC recurrence-free and 2677A carrier (carrying at least one variant A allele) was significant compared to other polymorphisms on ABCB1 nucleotide sequences[65].
The role of ABCC1 is to serve as primary transporters for compounds conjugated to glutathione, glucuronate and sulfate conjugated and cytotoxic drugs, indicating its importance in defending cells from oxidative stress. The transporters ABCC2 and ABCC3 had overlapping substrate specificities with ABCC1 but different distribution in the tissue[66]. Rat liver progenitor cells expressed high levels of active ABCC1 and ABCC3[67]. ABCC1 expression was higher in HCC with poor survival and hepatoblast subtype of HCC and correlated with K19 expression[50,68]. Together with ABCC3 and ABCG2, they co-localized with K7/K19, markers for hepatic progenitor cells in the tumor[68].
ABCG2 was first identified in human breast carcinoma cells. This protein is expressed in many normal tissues such as placenta, brain, prostate, small intestine, testis and liver. The spectrum of anticancer drugs transported by ABCG2 included mitoxantrone, camptothecin-derived and indolocarbazole topoisomerase I inhibitors, methotrexate and flavopiridol[69]. ABCG2 was one of the chemosensitivity determinants of irinotecan hydrochloride (CPT-11), an effective anticancer drug[70]. The study of ABCG2 expression in a variety of solid tumors demonstrated its presence in 40% of tumors with different degrees of positivity[71]. The ABCG2 expression is assumed to be correlated with stem cells and CSCs. ABCG2 expression in the progenitor cells/reactive ductules could contribute to the resistance to cytotoxic agents and xenotoxins[60].
SIDE POPULATIONS OF STEM CELLS
The isolation of side population (SP) rich on stem cells was first developed to purify the hematopoietic stem cells from the murine bone marrow cells following the Hoechst 33342 efflux activity by FACS[72]. This population was composed of primitive and progenitor hematopoietic cells subpopulations, one of which expressed stem cell markers Sca+ and CD34− as the most primitive[73]. SP cells were visualized as “dull cells” with low or negative fluorescence in dot plot due to the unique feature of SP cells capability to pump out the dye out of the cells. The activity of SP cells in exporting many types of substrates including dyes and drugs is assumed to have close association with the drug resistance.
The purified SP cells had been obtained from many solid tumors, including isolation of stem/progenitor cells from cancer originating from prostate[74], pancreas[75], stomach[76] and liver[30]. These studies confirmed the existence of a distinct hierarchy in malignancies and many SP cells obtained from different cancers demonstrated tumor initiating potentials. For example, SP from pancreatic cancer cell line had high capacity of the epithelial to mesenchymal transition (EMT), invasion and metastasis[75].
In humans, SP cells derived from an adult normal liver had the capacity to generate hepatocyte-like cells in vitro, irrespective to their CD45 marker status[77]. In the murine model, SP cells isolated from liver had potential to generate various liver cells such as mature hepatocytes and bile duct epithelium. As much as 75% of these SP cells expressed CD45+ but the highest efflux activity was found in CD45- cells. Moreover, both CD45+ and CD45- SP cells expressed CD34, CD117, Sca-1 and CD90[78].
A study using murine models demonstrated that bone marrow cells from MDR1A/1B-/- mice contained a normal number of SP cells, indicating that MDR1A/1B was not required for SP phenotype. By contrast, a significant reduction of SP cells in bone marrow and skeletal muscle was observed in BCRP1-/- mice, suggesting BCRP1 as molecular phenotype of SP[79,80].
In HCC, the SP population has also been reported. SP cells, sorted from HCC cell lines HCCLM3, MHCC97-H, MHCC97-L and Hep3B harboured CSCs-like, might be related to the metastatic potentials and therapeutic-resistance[81]. The SP from cell lines PLC/PRF/5 (0.80%) and HuH7 (0.25%) showed high proliferations, anti-apoptotic properties and capabilities to initiate tumor formation in non-obese diabetes/severe combined immunodeficiency (NOD/SCID) mice[30]. Further studies on ABCG2 expression in these cell lines showed that the sorted ABCG2+ cells generated both ABCG2+ and ABCG2- cells while ABCG2- cells only gave ABCG2- cells. Additionally, GATA6, an essential factor of earliest phase of hepatic development, was intensely expressed in ABCG2+ cells and C/EBPβ, a factor for late phase of liver development, was expressed more in ABCG2- cells[82]. Using a 2-acetylaminofluorene partial hepatectomy (AAF/PH) rat model, it has been demonstrated that hepatic oval cells of non-parenchymal cells had the side population phenotype defined by expression of ABCG2/BCRP1[83].
A study by Hu et al[84] showed that ABCG2 expression significantly influenced the levels of drug efflux from HCC cell lines. The SP cells were importantly involved in the drug efflux-related chemotherapy resistance and the SP analysis was found to be an efficient method to evaluate the functional activity of ABCG2.
However, since ABCG2 is also expressed in other normal tissues[69], ABCG2 is perhaps not the best single marker to identify stem cells. The molecular phenotype markers of stem cells from various tissues obtained by SP technique were diverse. In human bone marrow, ABCG2 co-expression with CD34 and CD133 was found to be very low or undetectable and the use of single marker ABCG2 only harbored little colony forming potential[85]. In human liver, SP cells with CD45+ phenotype could generate hepatocytes similar to their CD45- counterpart[77].
Furthermore, the characterization and definition of SP stem cells has several limitations. The SP population is usually very low and further characterization will be inadequate. Hoechst dye is toxic to the cells and the efflux is a biological process that may affect the results. High variations found in different studies might be caused by different ways of tissue dissociation, cells counting, dye concentration, staining condition and stringency in selection of SP cells. These parameters dramatically affected the viability, homogeneity and the apparent yield of SP cells[86].
ABC TRANSPORTER INHIBITORS
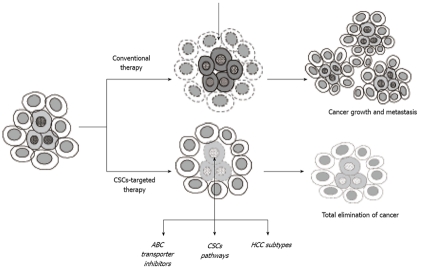
As mentioned previously, one of the most important appearances of the CSCs is their resistance to standard chemotherapies. The combination of chemotherapy drugs and specific inhibitors targeting ABC transporters could be a potential strategy to kill both tumor cells and the CSCs[87]. This approach focuses on killing the CSCs as the main source of the tumor by sensitizing the cells to drugs and inhibiting the drugs efflux from the cells. Total eradication of the tumor will prevent the reoccurrence of cancer (Figure 2).
Figure 2.
The CSCs-targeted therapy strategy. Conventional therapies affecting mainly the differentiated cells might not be sufficient to eradicate total tumor. In the CSCs-targeted therapy, chemotherapeutic agents is specially designed to target the CSCs. This strategy may primary block the main source and consistently inhibit the growth of tumor. Some factors such as CSCs pathways, tumor subtypes and drugs transporters inhibitions should be considered to increase the efficiency and safety of the treatment.
Experimental and clinical studies focused on increasing the sensitivity of cancer cells to anticancer drugs are ongoing. Several compounds have been introduced to block ABCB1, ABCC1 and ABCG2 in HCC, including the use of modulators and monoclonal antibodies, as listed in Table 2. Combination therapies between modulators and antibody against transporter proteins have also been explored. For example, the synergistic effect of bromocriptine and tumor necrosis factor-alpha reversed the cancer growth in nude mouse ABCB1 model of liver neoplasm[88]. Drug delivery system is also becoming a subject of interest. The use of liposome-encapsulated drugs administered through the hepatic artery[89] and adenoviral delivery of ABC transporters nucleic acid constructs are proposed to be an efficient and safe system[90,91].
Table 2.
Several potential inhibitors and targeted agents of growth factor receptors, signaling pathways and ABC transporters in liver cancer
| Targets | Agents | Ref. | |
| ABC transporters | ABCB1/MDR1 | Verapamil, cyclosporine, GF120918, PSC833, GG918, biricodar | [146-149] |
| ABCC1/MRP1 | Cyclosporine, biricodar | [146,149] | |
| ABCG2/BCRP | FTC, Kol43, GF120918, novobiocin, naringenin | [69,70,147,150,151] | |
| Growth factor receptors and signaling pathways | VEGF receptors | Sorafenib, sunitinib, bevacizumab | [139,142-145] |
| EGF receptors | Erlotinib, gefitinib, cetuximab | [120-126] | |
| IGF receptors | IMC-A12 | [132-134] | |
| Hedgehog pathway | Cyclopamine, anti-Rab23, SHH neutralizing antibodies | [107,108] | |
| Wnt/ β-catenin | Anti-Wnt antibody, AKT1 inhibitor | [34] | |
| Notch | TW-37 | [136] |
VEGF: Vascular endothelial growth factor; IGF: Insulin growth factor; EGF: Epidermal growth factor; ABC: ATP binding cassette.
Nevertheless, serious cell toxicity of the inhibitors requires careful consideration due to drug sensitization and accumulation[92]. Combination regimens therapy containing optimum concentration of anticancer drugs and inhibitors with a better targeting system will be useful for the success of the therapy.
SIGNALING PATHWAYS
Another way to approach potential HCC treatment with minimal systemic toxicity is to target the essential CSCs pathways. Several signals pathways coordinate together in the development and differentiation of stem cells in a complex network which has not been fully described. New therapeutic strategies targeting signaling pathways which are involved in the self renewal of CSCs and block differentiated cancer cells have been suggested[93]. These therapies aim to modulate important steps of the networks such as growth factors, growth factor receptors or kinase involved in the cell cycle, cellular survival, angiogenesis, and metastasis.
The transforming growth factor beta (TGF-β) family proteins are responsible for controlling cell proliferation, differentiation and other functions. These proteins are involved in regulating the biology of embryonic stem cells and tumor suppression and help the selection of cell fate and the progression of differentiation[94]. However, a recent study showed that TGF-β signaling network is a dynamic process in which different signals function in parallel to induce different early genes[95]. Moreover, the role of TGF-β in early events of differentiation depended on the cell types. The bone morphogenetic protein (BMP), a member of TGF-β family, induced differentiation of mesenchymal cells into chondroblast or osteoblast phenotypes in vitro. The activin/TGF-β provided competence for chondroblast differentiation at early stages, while TGF-β inhibited osteoblast maturation at late stages in the differentiation pathway[96]. In fetal murine hepatoblasts, the TGF-β signaling pathway members were significantly up-regulated during ductular differentiation in vitro but not during hepatocyte differentiation[97]. The inhibition of activin/TGF-β signaling by the Onecut transcription factors HNF-6 and OC-2 allowed normal hepatocyte differentiation[98].
Cell fate decisions in the liver were suggested to be also related with the role of microRNAs, in which miR-23b clusters miRNAs repressed bile duct gene expression by down-regulating Smads[99]. Interestingly, TGF-β treatment induced dedifferentiation of fetal rat hepatocytes to liver stem cell-like phenotype, suggesting that TGF-β might play an essential role in the transdifferentiation process[100].
TGF-β family members may also have implications in the maintenance of somatic stem cells and cancer stem cells. During carcinogenesis, the TGF-β signaling play important roles in inducing EMT by up-regulating the expression of Snail transcription factor family members[101]. A recent study demonstrated that TGF-β pathway was deregulated in human HCC. Both normal tissues and HCC specimens contained progenitor/stem cells which express signal transducer and activator of transcription 3 (STAT3), ornithine carbamoyl-transferase 4 (OCT4) and NANOG. The signaling proteins TGFBR2 (TGF-β receptor 2) and embryonic liver fodrin (ELF) which were prominently found in the normal tissues, were absent in HCC tissues suggesting that the change in TGF-β pathway may induce HCC trough interruption of differentiation by hepatic progenitor/stem cells. STAT3/OCT4 stem cells with disrupted TGF-β signaling were likely cancer progenitor cells and modulation on stem cell renewal factor may reduce tumor construction[102].
A functional link between IL-6, a major stem cell signaling pathway and TGF-β pathway has been revealed. Gene expression analysis of HCC in ELF+/- mice showed that HCC could arise from an IL-6-driven transformed stem cell with inactivated TGF-β signaling[102,103]. Additionally, the absence of inter-α-trypsin inhibitor-4 (ITIH4), an IL-6 target and a biomarker of foregut cancer, appeared to decrease the expression of IL-6/STAT3. The tumor size of ELF+/-/ITIH4-/- mouse was smaller than ELF-/- mouse[102].
The Hedgehog (HH) signaling pathway is one of the key controllers in cell development. HH pathway is most active during embryogenesis and may be involved in the regulation of adult stem cells, mainly in maintenance and self renewal[104]. The disregulation in HH pathway has been proposed to be a component in stem cell activation in cancers and therefore represents an attractive agent for cancer therapy[105]. Cyclopamine, a steroid-like compound against smoothened (SMO) in the HH pathway, was found to significantly down regulate the SHH, SUFU, PTCH, GLI2 and GLI3 on prostate cancer cells DU-145[106]. In HCC, HH pathway was over expressed in cancer tissues compared with non-cancer tissues and linked with histological differentiation and portal venous invasion. Cyclopamine was reported to block HH signaling pathway also in HCC[107,108] by inducing the reduction of DNA synthesis and inhibiting cell growth, thus causing a significant reduction in HCC invasiveness and motility of HCC cells[107]. The new inhibitor HhAntag691 (GDC-0449) has entered clinical trials for a variety of solid tumors. This molecule inhibits both HH signaling and ABC transporters ABCG2 and ABCB1[109,110]. The SHH neutralizing antibodies were reported to decrease the expression of HH target genes, inhibit cell growth and result in apoptosis[108].
The Wnt signaling pathway consists of a large network of proteins involved in embryogenesis and cancer. The Wnt proteins were assumed to act as stem cells growth factor and maintain the proliferation of stem cells[111]. The Wnt signaling may crosstalk with TGF-β signaling and regulate the mesenchymal stem cells proliferation[101].
Active Wnt/β-catenin signaling pathway was shown to occur preferentially in liver progenitor cells and to be closely related with drug resistance[112]. An activation of Akt signaling and impaired expression of phosphatase and tensin homolog (PTEN) has been reported in about 40% of human HCC[113]. AKT1 inhibitor treatment to CD133+ HCC cells significantly reduced the expression of survival protein[34]. A study from the SP population demonstrated that the Akt signaling inhibition attenuated the drug efflux and increased drug efficacy[84].
PTEN is one of the most frequently mutated tumor suppressors in cancer[114]. Decreased PTEN expression was correlated with HCC progression, high AFP levels, p53 over expression and poor prognosis[113]. Chemoresistance to interferon-alpha/5-FU combination therapy for HCC was induced by Wnt/β-catenin signaling pathway[115]. The PTEN-Akt pathway activated stem cells by helping control nuclear localization of the Wnt/β-catenin[116]. Data obtained from gene expression analysis showed that the activation of Wnt/β-catenin pathway led to enrichment of the proposed progenitor cells EpCAM+ population. The RNA interference-based blockage of EpCAM, Wnt/β-catenin target attenuated the activities of the cells[47,117].
Epidermal growth factor (EGF) is a single strand polypeptide involved in regulation of a wide variety of physiological and pathological processes including embryogenesis, growth, tissue repair, regeneration and neoplasia. EGF works by binding with the EGF receptor (EGFR). Microarray analysis on liver-specific non-mutated β-catenin over expressing transgenic mice demonstrated increase levels of activated EGFR and Stat3. The EGFR inhibition decreased liver size and seemed to be a direct target of the pathway[118]. EGFR was found to be over expressed in HCC and associated with tumor aggressiveness and poor prognosis[119].
Several agents targeting EGFR are currently under development. In phase II clinical trials, erlotinib, an oral receptor tyrosine kinase inhibitor specific for the EGFR/HER1, has been evaluated and is reported to give progression-free survival in advanced HCC with median overall survival 10 to 13 mo[120,121]. In experimental models with mouse and human HCC cells, gefitinib, another EGFR inhibitor for lung cancer treatment, inhibited the growth of HCC and its combination with cisplatin enhanced inhibitory effect[122,123]. In the cirrhotic rat model, the number of HCC nodules was reduced after gefitinib administration and EGFR was activated lower in the diseased and tumoral tissues[124]. Cetuximab, a chimeric monoclonal antibody against EGFR, is also under investigation. A phase II clinical study of cetuximab in advanced HCC demonstrated that although cetuximab was tolerable in terms of toxicity, it had no antitumor activity[125]. However, even though cetuximab seemed to have no effect as single agent, combination of cetuximab and gemcitabine plus oxaliplatin in advanced stages HCC patients appeared to be active and to have a manageable toxicity[126].
Transforming growth factor-α (TGF-α), one of the most important ligands for EGFR, was commonly over-expressed in HCC[127]. In HCC, serum TGF-α levels were found to be closely related to severity of liver dysfunction, and hepatic expression of TGF-α and EGFR correlated with proliferation of normal and neoplastic hepatocytes[128]. A recent study reported that TGF-α interacted with MYC oncogene. The expression of MYC and TGF-α in liver progenitor cells resulted in enhanced cell proliferation in culture and the generation of poorly differentiated tumors after inoculation into nude mice. However, further study using the apoptosis-deficient mutants T58A and S71F showed that T58A allele had an increased ability to interact with TGF-α in promoting cell proliferation and tumorigenesis, while the interactions between S71F allele and the TGF-α had opposite effects[129].
Current study is also focused on the insulin growth factor (IGF) which is involved in the hepatogenesis. Alteration of IGF and its receptor was associated with tumor stages, reduced survival, development of metastasis and dedifferentiation[130]. A study on human hepatoma cell lines showed that the IGF2/IGF1-R activation triggered proliferative and survival signals through EGFR-dependent and -independent mechanisms. The IGF2/IGF-1R survival pathway may contribute to gefitinib resistance in these cells[131]. Currently, monoclonal antibody inhibits IGF1-R is under clinical phase II study for HCC[132-134].
The Notch signaling pathway is involved in the development of many organs and has important role in keeping the balance of cell proliferation, differentiation and apoptosis. The activation of Notch signaling in mouse hepatoblast resulted in inhibition of hepatic differentiation and induction of several cholangiocytic characteristics, suggesting that Notch signaling plays a key role in the differentiation of hepatoblast[135].
Alteration disturbed Notch might induce tumorigenesis and changes in the expression of Notch receptors were found in many malignant tumors including HCC. In pancreatic cancer, antitumor drug TW-37, a small-molecule inhibitor of Bcl-2 family proteins, inhibited cell growth and induced apoptosis. It has been suggested that the activity of TW-37 was mediated through a novel pathway involving inactivation of Notch-1 and Jagged-1[136]. In adult human liver, the expression and localization of Notch receptors has been observed to be altered during liver damage[137]. The over-expression of Notch1 using cDNA encoding its constitutively active form was able to inhibit the growth of HCC cells in vitro and in vivo[138].
The angiogenesis pathway also has become an effective target of current pharmacologic strategies[139]. The vascular endothelial growth factor (VEGF) expression was closely related with vascularity of HCC compared with a non-cancer specimen[140] and associated with the invasion and metastasis[141]. Several VEGF signaling inhibitors might be promising therapeutic agents for HCC. Sorafenib, a multi-tyrosine kinase inhibitor including VEGFR-2 and VEGFR-3 targeting, was demonstrated to prolong median survival and time to progression by nearly 3 months in patients with advanced HCC in a large phase III trial[142]. Another inhibitor on a phase II clinical trial, sunitinib, has demonstrated tolerability and efficacy in patients with advanced HCC[143]. Bevacizumab, a recombinant monoclonal antibody against VEGF has been used as single or combination therapy agent[144,145]. Combination of bevacizumab and erlotinib in advanced HCC patients showed significant anti-tumor activity[145]. Still, further evaluation is needed to avoid the negative side effects of the agents.
CONCLUSION
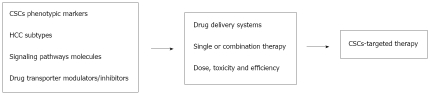
The existence of CSCs in HCC has been supported by a growing body of evidence from basic and clinical research. However, until now the CSCs characteristics in HCC are still unsettled and CSCs signaling pathways network is not fully described. More information of CSCs uniqueness and activation would be one of the main keys in understanding the initiation and development of cancer. Furthermore, to achieve a better strategy for a total elimination of HCC, several biological and clinical aspects should be considered for an effective CSCs-targeted therapy (Figure 3). First, characterization and identification of the CSCs phenotypes which distinguish them from normal stem cells will be important. Specific CSCs-targeted therapies which recognize only CSCs and not normal stem cells will greatly increase the efficiency while avoiding the ‘wrong’ target. Therefore, further investigations on signaling pathways involved in CSCs-induced tumor will be a potent means in finding the best target of therapies. Second, understanding of the biological properties of CSCs that makes them resistant to treatments will help to decrease drug resistance and increase drug sensitivity. Application of ABC transporters inhibitors and combination therapies of drugs and inhibitors may enhance treatment efficacy and at the same time decrease drug toxicity. Third, drug design and administration to obtain a correct delivery target in the diseased tissue will greatly improve toxic effect where needed and remove toxicity where this is harmful. And fourth, the analysis of HCC prognostic subtypes might form a basis to decide a better personalized approach to the patients. Combining all data together, more studies on HCC and hepatic CSCs are needed to have a better view of the mechanism underlying HCC and to find potent novel molecular therapies in the future.
Figure 3.
A collaborative approach to target the CSCs. The hepatic CSCs identifications and their functional significances, including multidrugs resistance behavior and aberrant signaling pathways should be clearly identified. Together with CSCs markers, clinical aspects such as drug delivery system, single or combination therapy, drug dose and toxicity will support the potential of therapy. Both biological and clinical considerations will be potent means to improve the safety and efficiency of CSCs-targeted therapy.
Acknowledgments
The authors thank a fellowship of the Italian Ministry of Foreign Affairs of the Istituto Italiano di Cultura, Jakarta, Indonesia for their help.
Footnotes
Supported by a Grant from the Italian Liver Foundation
Peer reviewers: Yi-Tao Ding, Professor, Department of Hepatobiliary Surgery, The Affiliated Drum Tower Hospital, School of Medicine, Nanjing University, Nanjing 210008, Jiangsu Province, China; Isabel Fabregat Romero, PhD, Laboratori de Oncologia Molecular, Institut de Investigació Biomèdica de Bellvitge, Gran via de Hospitalet, Barcelona 08907, Spain; Wen-Dong Huang, PhD, Department of Gene Regulation and Drug Discovery, Beckman Research Institute of City of Hope, Duarte, CA 91010, United States
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–156. doi: 10.1002/ijc.1440. [DOI] [PubMed] [Google Scholar]
- 2.Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 4.Mastrangelo G, Fedeli U, Fadda E, Valentini F, Agnesi R, Magarotto G, Marchì T, Buda A, Pinzani M, Martines D. Increased risk of hepatocellular carcinoma and liver cirrhosis in vinyl chloride workers: synergistic effect of occupational exposure with alcohol intake. Environ Health Perspect. 2004;112:1188–1192. doi: 10.1289/ehp.6972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niederau C, Fischer R, Sonnenberg A, Stremmel W, Trampisch HJ, Strohmeyer G. Survival and causes of death in cirrhotic and in noncirrhotic patients with primary hemochromatosis. N Engl J Med. 1985;313:1256–1262. doi: 10.1056/NEJM198511143132004. [DOI] [PubMed] [Google Scholar]
- 6.Bosch FX, Ribes J, Borràs J. Epidemiology of primary liver cancer. Semin Liver Dis. 1999;19:271–285. doi: 10.1055/s-2007-1007117. [DOI] [PubMed] [Google Scholar]
- 7.Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet. 1981;2:1129–1133. doi: 10.1016/s0140-6736(81)90585-7. [DOI] [PubMed] [Google Scholar]
- 8.Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127:S35–S50. doi: 10.1053/j.gastro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Blum HE. Hepatocellular carcinoma: therapy and prevention. World J Gastroenterol. 2005;11:7391–7400. doi: 10.3748/wjg.v11.i47.7391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abou-Alfa GK, Huitzil-Melendez FD, O’Reilly EM, Saltz LB. Current management of advanced hepatocellular carcinoma. Gastrointest Cancer Res. 2008;2:64–70. [PMC free article] [PubMed] [Google Scholar]
- 11.Yeo W, Mok TS, Zee B, Leung TW, Lai PB, Lau WY, Koh J, Mo FK, Yu SC, Chan AT, et al. A randomized phase III study of doxorubicin versus cisplatin/interferon alpha-2b/doxorubicin/fluorouracil (PIAF) combination chemotherapy for unresectable hepatocellular carcinoma. J Natl Cancer Inst. 2005;97:1532–1538. doi: 10.1093/jnci/dji315. [DOI] [PubMed] [Google Scholar]
- 12.Mimeault M, Hauke R, Mehta PP, Batra SK. Recent advances in cancer stem/progenitor cell research: therapeutic implications for overcoming resistance to the most aggressive cancers. J Cell Mol Med. 2007;11:981–1011. doi: 10.1111/j.1582-4934.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarke MF, Dick JE, Dirks PB, Eaves CJ, Jamieson CH, Jones DL, Visvader J, Weissman IL, Wahl GM. Cancer stem cells--perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer Res. 2006;66:9339–9344. doi: 10.1158/0008-5472.CAN-06-3126. [DOI] [PubMed] [Google Scholar]
- 14.Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, Minden M, Paterson B, Caligiuri MA, Dick JE. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994;367:645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 15.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3:730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 16.Holyoake TL, Jiang X, Drummond MW, Eaves AC, Eaves CJ. Elucidating critical mechanisms of deregulated stem cell turnover in the chronic phase of chronic myeloid leukemia. Leukemia. 2002;16:549–558. doi: 10.1038/sj.leu.2402444. [DOI] [PubMed] [Google Scholar]
- 17.Cox CV, Evely RS, Oakhill A, Pamphilon DH, Goulden NJ, Blair A. Characterization of acute lymphoblastic leukemia progenitor cells. Blood. 2004;104:2919–2925. doi: 10.1182/blood-2004-03-0901. [DOI] [PubMed] [Google Scholar]
- 18.Cobaleda C, Gutiérrez-Cianca N, Pérez-Losada J, Flores T, García-Sanz R, González M, Sánchez-García I. A primitive hematopoietic cell is the target for the leukemic transformation in human philadelphia-positive acute lymphoblastic leukemia. Blood. 2000;95:1007–1013. [PubMed] [Google Scholar]
- 19.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983–3938. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 21.Hemmati HD, Nakano I, Lazareff JA, Masterman-Smith M, Geschwind DH, Bronner-Fraser M, Kornblum HI. Cancerous stem cells can arise from pediatric brain tumors. Proc Natl Acad Sci USA. 2003;100:15178–15183. doi: 10.1073/pnas.2036535100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patrawala L, Calhoun T, Schneider-Broussard R, Li H, Bhatia B, Tang S, Reilly JG, Chandra D, Zhou J, Claypool K, et al. Highly purified CD44+ prostate cancer cells from xenograft human tumors are enriched in tumorigenic and metastatic progenitor cells. Oncogene. 2006;25:1696–1708. doi: 10.1038/sj.onc.1209327. [DOI] [PubMed] [Google Scholar]
- 23.Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res. 2005;65:10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 24.Houghton J, Stoicov C, Nomura S, Rogers AB, Carlson J, Li H, Cai X, Fox JG, Goldenring JR, Wang TC. Gastric cancer originating from bone marrow-derived cells. Science. 2004;306:1568–1571. doi: 10.1126/science.1099513. [DOI] [PubMed] [Google Scholar]
- 25.Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S, Crowley D, Bronson RT, Jacks T. Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell. 2005;121:823–835. doi: 10.1016/j.cell.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 26.O’Brien CA, Pollett A, Gallinger S, Dick JE. A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature. 2007;445:106–110. doi: 10.1038/nature05372. [DOI] [PubMed] [Google Scholar]
- 27.Ricci-Vitiani L, Lombardi DG, Pilozzi E, Biffoni M, Todaro M, Peschle C, De Maria R. Identification and expansion of human colon-cancer-initiating cells. Nature. 2007;445:111–115. doi: 10.1038/nature05384. [DOI] [PubMed] [Google Scholar]
- 28.Ma S, Chan KW, Hu L, Lee TK, Wo JY, Ng IO, Zheng BJ, Guan XY. Identification and characterization of tumorigenic liver cancer stem/progenitor cells. Gastroenterology. 2007;132:2542–2556. doi: 10.1053/j.gastro.2007.04.025. [DOI] [PubMed] [Google Scholar]
- 29.Yang ZF, Ngai P, Ho DW, Yu WC, Ng MN, Lau CK, Li ML, Tam KH, Lam CT, Poon RT, et al. Identification of local and circulating cancer stem cells in human liver cancer. Hepatology. 2008;47:919–928. doi: 10.1002/hep.22082. [DOI] [PubMed] [Google Scholar]
- 30.Chiba T, Kita K, Zheng YW, Yokosuka O, Saisho H, Iwama A, Nakauchi H, Taniguchi H. Side population purified from hepatocellular carcinoma cells harbors cancer stem cell-like properties. Hepatology. 2006;44:240–251. doi: 10.1002/hep.21227. [DOI] [PubMed] [Google Scholar]
- 31.Suetsugu A, Nagaki M, Aoki H, Motohashi T, Kunisada T, Moriwaki H. Characterization of CD133+ hepatocellular carcinoma cells as cancer stem/progenitor cells. Biochem Biophys Res Commun. 2006;351:820–824. doi: 10.1016/j.bbrc.2006.10.128. [DOI] [PubMed] [Google Scholar]
- 32.Zen Y, Fujii T, Yoshikawa S, Takamura H, Tani T, Ohta T, Nakanuma Y. Histological and culture studies with respect to ABCG2 expression support the existence of a cancer cell hierarchy in human hepatocellular carcinoma. Am J Pathol. 2007;170:1750–1762. doi: 10.2353/ajpath.2007.060798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graham SM, Jørgensen HG, Allan E, Pearson C, Alcorn MJ, Richmond L, Holyoake TL. Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood. 2002;99:319–325. doi: 10.1182/blood.v99.1.319. [DOI] [PubMed] [Google Scholar]
- 34.Ma S, Lee TK, Zheng BJ, Chan KW, Guan XY. CD133+ HCC cancer stem cells confer chemoresistance by preferential expression of the Akt/PKB survival pathway. Oncogene. 2008;27:1749–1758. doi: 10.1038/sj.onc.1210811. [DOI] [PubMed] [Google Scholar]
- 35.Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, Dewhirst MW, Bigner DD, Rich JN. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444:756–760. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 36.Sell S. The hepatocyte: heterogeneity and plasticity of liver cells. Int J Biochem Cell Biol. 2003;35:267–271. doi: 10.1016/s1357-2725(02)00182-6. [DOI] [PubMed] [Google Scholar]
- 37.Herrera MB, Bruno S, Buttiglieri S, Tetta C, Gatti S, Deregibus MC, Bussolati B, Camussi G. Isolation and characterization of a stem cell population from adult human liver. Stem Cells. 2006;24:2840–2850. doi: 10.1634/stemcells.2006-0114. [DOI] [PubMed] [Google Scholar]
- 38.Nowak G, Ericzon BG, Nava S, Jaksch M, Westgren M, Sumitran-Holgersson S. Identification of expandable human hepatic progenitors which differentiate into mature hepatic cells in vivo. Gut. 2005;54:972–979. doi: 10.1136/gut.2005.064477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dan YY, Riehle KJ, Lazaro C, Teoh N, Haque J, Campbell JS, Fausto N. Isolation of multipotent progenitor cells from human fetal liver capable of differentiating into liver and mesenchymal lineages. Proc Natl Acad Sci USA. 2006;103:9912–9917. doi: 10.1073/pnas.0603824103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corcelle V, Stieger B, Gjinovci A, Wollheim CB, Gauthier BR. Characterization of two distinct liver progenitor cell subpopulations of hematopoietic and hepatic origins. Exp Cell Res. 2006;312:2826–2836. doi: 10.1016/j.yexcr.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 41.Yin S, Li J, Hu C, Chen X, Yao M, Yan M, Jiang G, Ge C, Xie H, Wan D, et al. CD133 positive hepatocellular carcinoma cells possess high capacity for tumorigenicity. Int J Cancer. 2007;120:1444–1450. doi: 10.1002/ijc.22476. [DOI] [PubMed] [Google Scholar]
- 42.Ma S, Chan KW, Lee TK, Tang KH, Wo JY, Zheng BJ, Guan XY. Aldehyde dehydrogenase discriminates the CD133 liver cancer stem cell populations. Mol Cancer Res. 2008;6:1146–1153. doi: 10.1158/1541-7786.MCR-08-0035. [DOI] [PubMed] [Google Scholar]
- 43.Moreb JS. Aldehyde dehydrogenase as a marker for stem cells. Curr Stem Cell Res Ther. 2008;3:237–246. doi: 10.2174/157488808786734006. [DOI] [PubMed] [Google Scholar]
- 44.Song W, Li H, Tao K, Li R, Song Z, Zhao Q, Zhang F, Dou K. Expression and clinical significance of the stem cell marker CD133 in hepatocellular carcinoma. Int J Clin Pract. 2008;62:1212–1218. doi: 10.1111/j.1742-1241.2008.01777.x. [DOI] [PubMed] [Google Scholar]
- 45.Yang ZF, Ho DW, Ng MN, Lau CK, Yu WC, Ngai P, Chu PW, Lam CT, Poon RT, Fan ST. Significance of CD90+ cancer stem cells in human liver cancer. Cancer Cell. 2008;13:153–166. doi: 10.1016/j.ccr.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 46.Yamashita T, Forgues M, Wang W, Kim JW, Ye Q, Jia H, Budhu A, Zanetti KA, Chen Y, Qin LX, et al. EpCAM and alpha-fetoprotein expression defines novel prognostic subtypes of hepatocellular carcinoma. Cancer Res. 2008;68:1451–1461. doi: 10.1158/0008-5472.CAN-07-6013. [DOI] [PubMed] [Google Scholar]
- 47.Yamashita T, Ji J, Budhu A, Forgues M, Yang W, Wang HY, Jia H, Ye Q, Qin LX, Wauthier E, et al. EpCAM-positive hepatocellular carcinoma cells are tumor-initiating cells with stem/progenitor cell features. Gastroenterology. 2009;136:1012–1024. doi: 10.1053/j.gastro.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iyer A, Robert ME, Bifulco CB, Salem RR, Jain D. Different cytokeratin and neuronal cell adhesion molecule staining patterns in focal nodular hyperplasia and hepatic adenoma and their significance. Hum Pathol. 2008;39:1370–1377. doi: 10.1016/j.humpath.2008.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee JS, Heo J, Libbrecht L, Chu IS, Kaposi-Novak P, Calvisi DF, Mikaelyan A, Roberts LR, Demetris AJ, Sun Z, et al. A novel prognostic subtype of human hepatocellular carcinoma derived from hepatic progenitor cells. Nat Med. 2006;12:410–416. doi: 10.1038/nm1377. [DOI] [PubMed] [Google Scholar]
- 50.Lee JS, Chu IS, Heo J, Calvisi DF, Sun Z, Roskams T, Durnez A, Demetris AJ, Thorgeirsson SS. Classification and prediction of survival in hepatocellular carcinoma by gene expression profiling. Hepatology. 2004;40:667–676. doi: 10.1002/hep.20375. [DOI] [PubMed] [Google Scholar]
- 51.Uenishi T, Kubo S, Yamamoto T, Shuto T, Ogawa M, Tanaka H, Tanaka S, Kaneda K, Hirohashi K. Cytokeratin 19 expression in hepatocellular carcinoma predicts early postoperative recurrence. Cancer Sci. 2003;94:851–857. doi: 10.1111/j.1349-7006.2003.tb01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Durnez A, Verslype C, Nevens F, Fevery J, Aerts R, Pirenne J, Lesaffre E, Libbrecht L, Desmet V, Roskams T. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology. 2006;49:138–151. doi: 10.1111/j.1365-2559.2006.02468.x. [DOI] [PubMed] [Google Scholar]
- 53.Higgins CF. ABC transporters: from microorganisms to man. Annu Rev Cell Biol. 1992;8:67–113. doi: 10.1146/annurev.cb.08.110192.000435. [DOI] [PubMed] [Google Scholar]
- 54.Dean M, Hamon Y, Chimini G. The human ATP-binding cassette (ABC) transporter superfamily. J Lipid Res. 2001;42:1007–1017. [PubMed] [Google Scholar]
- 55.Dean M, Rzhetsky A, Allikmets R. The human ATP-binding cassette (ABC) transporter superfamily. Genome Res. 2001;11:1156–1166. doi: 10.1101/gr.184901. [DOI] [PubMed] [Google Scholar]
- 56.Hyde SC, Emsley P, Hartshorn MJ, Mimmack MM, Gileadi U, Pearce SR, Gallagher MP, Gill DR, Hubbard RE, Higgins CF. Structural model of ATP-binding proteins associated with cystic fibrosis, multidrug resistance and bacterial transport. Nature. 1990;346:362–365. doi: 10.1038/346362a0. [DOI] [PubMed] [Google Scholar]
- 57.Seeger MA, van Veen HW. Molecular basis of multidrug transport by ABC transporters. Biochim Biophys Acta. 2009;1794:725–737. doi: 10.1016/j.bbapap.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 58.Dean M. ABC transporters, drug resistance, and cancer stem cells. J Mammary Gland Biol Neoplasia. 2009;14:3–9. doi: 10.1007/s10911-009-9109-9. [DOI] [PubMed] [Google Scholar]
- 59.Ros JE, Libbrecht L, Geuken M, Jansen PL, Roskams TA. High expression of MDR1, MRP1, and MRP3 in the hepatic progenitor cell compartment and hepatocytes in severe human liver disease. J Pathol. 2003;200:553–560. doi: 10.1002/path.1379. [DOI] [PubMed] [Google Scholar]
- 60.Vander Borght S, Libbrecht L, Katoonizadeh A, van Pelt J, Cassiman D, Nevens F, Van Lommel A, Petersen BE, Fevery J, Jansen PL, et al. Breast cancer resistance protein (BCRP/ABCG2) is expressed by progenitor cells/reactive ductules and hepatocytes and its expression pattern is influenced by disease etiology and species type: possible functional consequences. J Histochem Cytochem. 2006;54:1051–1059. doi: 10.1369/jhc.5A6912.2006. [DOI] [PubMed] [Google Scholar]
- 61.Shen DW, Fojo A, Chin JE, Roninson IB, Richert N, Pastan I, Gottesman MM. Human multidrug-resistant cell lines: increased mdr1 expression can precede gene amplification. Science. 1986;232:643–645. doi: 10.1126/science.3457471. [DOI] [PubMed] [Google Scholar]
- 62.Kato A, Miyazaki M, Ambiru S, Yoshitomi H, Ito H, Nakagawa K, Shimizu H, Yokosuka O, Nakajima N. Multidrug resistance gene (MDR-1) expression as a useful prognostic factor in patients with human hepatocellular carcinoma after surgical resection. J Surg Oncol. 2001;78:110–115. doi: 10.1002/jso.1129. [DOI] [PubMed] [Google Scholar]
- 63.Ng IO, Liu CL, Fan ST, Ng M. Expression of P-glycoprotein in hepatocellular carcinoma. A determinant of chemotherapy response. Am J Clin Pathol. 2000;113:355–363. doi: 10.1309/AC1M-4TY4-U0TN-EN7T. [DOI] [PubMed] [Google Scholar]
- 64.Lage H. ABC-transporters: implications on drug resistance from microorganisms to human cancers. Int J Antimicrob Agents. 2003;22:188–199. doi: 10.1016/s0924-8579(03)00203-6. [DOI] [PubMed] [Google Scholar]
- 65.Wu L, Xu X, Shen J, Xie H, Yu S, Liang T, Wang W, Shen Y, Zhang M, Zheng S. MDR1 gene polymorphisms and risk of recurrence in patients with hepatocellular carcinoma after liver transplantation. J Surg Oncol. 2007;96:62–68. doi: 10.1002/jso.20774. [DOI] [PubMed] [Google Scholar]
- 66.Leslie EM, Deeley RG, Cole SP. Toxicological relevance of the multidrug resistance protein 1, MRP1 (ABCC1) and related transporters. Toxicology. 2001;167:3–23. doi: 10.1016/s0300-483x(01)00454-1. [DOI] [PubMed] [Google Scholar]
- 67.Ros JE, Roskams TA, Geuken M, Havinga R, Splinter PL, Petersen BE, LaRusso NF, van der Kolk DM, Kuipers F, Faber KN, et al. ATP binding cassette transporter gene expression in rat liver progenitor cells. Gut. 2003;52:1060–1067. doi: 10.1136/gut.52.7.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vander Borght S, Komuta M, Libbrecht L, Katoonizadeh A, Aerts R, Dymarkowski S, Verslype C, Nevens F, Roskams T. Expression of multidrug resistance-associated protein 1 in hepatocellular carcinoma is associated with a more aggressive tumour phenotype and may reflect a progenitor cell origin. Liver Int. 2008;28:1370–1380. doi: 10.1111/j.1478-3231.2008.01889.x. [DOI] [PubMed] [Google Scholar]
- 69.Doyle LA, Ross DD. Multidrug resistance mediated by the breast cancer resistance protein BCRP (ABCG2) Oncogene. 2003;22:7340–7358. doi: 10.1038/sj.onc.1206938. [DOI] [PubMed] [Google Scholar]
- 70.Takahata T, Ookawa K, Suto K, Tanaka M, Yano H, Nakashima O, Kojiro M, Tamura Y, Tateishi T, Sakata Y, et al. Chemosensitivity determinants of irinotecan hydrochloride in hepatocellular carcinoma cell lines. Basic Clin Pharmacol Toxicol. 2008;102:399–407. doi: 10.1111/j.1742-7843.2007.00199.x. [DOI] [PubMed] [Google Scholar]
- 71.Diestra JE, Scheffer GL, Català I, Maliepaard M, Schellens JH, Scheper RJ, Germà-Lluch JR, Izquierdo MA. Frequent expression of the multi-drug resistance-associated protein BCRP/MXR/ABCP/ABCG2 in human tumours detected by the BXP-21 monoclonal antibody in paraffin-embedded material. J Pathol. 2002;198:213–219. doi: 10.1002/path.1203. [DOI] [PubMed] [Google Scholar]
- 72.Goodell MA, Brose K, Paradis G, Conner AS, Mulligan RC. Isolation and functional properties of murine hematopoietic stem cells that are replicating in vivo. J Exp Med. 1996;183:1797–1806. doi: 10.1084/jem.183.4.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parmar K, Sauk-Schubert C, Burdick D, Handley M, Mauch P. Sca+CD34- murine side population cells are highly enriched for primitive stem cells. Exp Hematol. 2003;31:244–250. doi: 10.1016/s0301-472x(02)01074-3. [DOI] [PubMed] [Google Scholar]
- 74.Santamaria-Martínez A, Barquinero J, Barbosa-Desongles A, Hurtado A, Pinós T, Seoane J, Poupon MF, Morote J, Reventós J, Munell F. Identification of multipotent mesenchymal stromal cells in the reactive stroma of a prostate cancer xenograft by side population analysis. Exp Cell Res. 2009;315:3004–3013. doi: 10.1016/j.yexcr.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 75.Kabashima A, Higuchi H, Takaishi H, Matsuzaki Y, Suzuki S, Izumiya M, Iizuka H, Sakai G, Hozawa S, Azuma T, et al. Side population of pancreatic cancer cells predominates in TGF-beta-mediated epithelial to mesenchymal transition and invasion. Int J Cancer. 2009;124:2771–2779. doi: 10.1002/ijc.24349. [DOI] [PubMed] [Google Scholar]
- 76.Fukuda K, Saikawa Y, Ohashi M, Kumagai K, Kitajima M, Okano H, Matsuzaki Y, Kitagawa Y. Tumor initiating potential of side population cells in human gastric cancer. Int J Oncol. 2009;34:1201–1207. [PubMed] [Google Scholar]
- 77.Hussain SZ, Strom SC, Kirby MR, Burns S, Langemeijer S, Ueda T, Hsieh M, Tisdale JF. Side population cells derived from adult human liver generate hepatocyte-like cells in vitro. Dig Dis Sci. 2005;50:1755–1763. doi: 10.1007/s10620-005-2933-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wulf GG, Luo KL, Jackson KA, Brenner MK, Goodell MA. Cells of the hepatic side population contribute to liver regeneration and can be replenished with bone marrow stem cells. Haematologica. 2003;88:368–378. [PubMed] [Google Scholar]
- 79.Zhou S, Morris JJ, Barnes Y, Lan L, Schuetz JD, Sorrentino BP. Bcrp1 gene expression is required for normal numbers of side population stem cells in mice, and confers relative protection to mitoxantrone in hematopoietic cells in vivo. Proc Natl Acad Sci USA. 2002;99:12339–12344. doi: 10.1073/pnas.192276999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou S, Schuetz JD, Bunting KD, Colapietro AM, Sampath J, Morris JJ, Lagutina I, Grosveld GC, Osawa M, Nakauchi H, et al. The ABC transporter Bcrp1/ABCG2 is expressed in a wide variety of stem cells and is a molecular determinant of the side-population phenotype. Nat Med. 2001;7:1028–1034. doi: 10.1038/nm0901-1028. [DOI] [PubMed] [Google Scholar]
- 81.Shi GM, Xu Y, Fan J, Zhou J, Yang XR, Qiu SJ, Liao Y, Wu WZ, Ji Y, Ke AW, et al. Identification of side population cells in human hepatocellular carcinoma cell lines with stepwise metastatic potentials. J Cancer Res Clin Oncol. 2008;134:1155–1163. doi: 10.1007/s00432-008-0407-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zen Y, Fujii T, Yoshikawa S, Takamura H, Tani T, Ohta T, Nakanuma Y. Histological and culture studies with respect to ABCG2 expression support the existence of a cancer cell hierarchy in human hepatocellular carcinoma. Am J Pathol. 2007;170:1750–1762. doi: 10.2353/ajpath.2007.060798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shimano K, Satake M, Okaya A, Kitanaka J, Kitanaka N, Takemura M, Sakagami M, Terada N, Tsujimura T. Hepatic oval cells have the side population phenotype defined by expression of ATP-binding cassette transporter ABCG2/BCRP1. Am J Pathol. 2003;163:3–9. doi: 10.1016/S0002-9440(10)63624-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hu C, Li H, Li J, Zhu Z, Yin S, Hao X, Yao M, Zheng S, Gu J. Analysis of ABCG2 expression and side population identifies intrinsic drug efflux in the HCC cell line MHCC-97L and its modulation by Akt signaling. Carcinogenesis. 2008;29:2289–2297. doi: 10.1093/carcin/bgn223. [DOI] [PubMed] [Google Scholar]
- 85.Naylor CS, Jaworska E, Branson K, Embleton MJ, Chopra R. Side population/ABCG2-positive cells represent a heterogeneous group of haemopoietic cells: implications for the use of adult stem cells in transplantation and plasticity protocols. Bone Marrow Transplant. 2005;35:353–360. doi: 10.1038/sj.bmt.1704762. [DOI] [PubMed] [Google Scholar]
- 86.Montanaro F, Liadaki K, Schienda J, Flint A, Gussoni E, Kunkel LM. Demystifying SP cell purification: viability, yield, and phenotype are defined by isolation parameters. Exp Cell Res. 2004;298:144–154. doi: 10.1016/j.yexcr.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 87.Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–284. doi: 10.1038/nrc1590. [DOI] [PubMed] [Google Scholar]
- 88.Ding L, Chen XP, Zhang ZW, Guan J, Zhang WG, Wang HP, Wang ZH, Li CL. Synergistic effect of bromocriptine and tumor necrosis factor-alpha on reversing hepatocellular carcinoma multidrug resistance in nude mouse MDR1 model of liver neoplasm. World J Gastroenterol. 2005;11:5621–5626. doi: 10.3748/wjg.v11.i36.5621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sun DS, Chen JH, Ling R, Yao Q, Wang L, Ma Z, Li Y. Treatment of hepatoma with liposome-encapsulated adriamycin administered into hepatic artery of rats. World J Gastroenterol. 2006;12:4741–4744. doi: 10.3748/wjg.v12.i29.4741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huesker M, Folmer Y, Schneider M, Fulda C, Blum HE, Hafkemeyer P. Reversal of drug resistance of hepatocellular carcinoma cells by adenoviral delivery of anti-MDR1 ribozymes. Hepatology. 2002;36:874–884. doi: 10.1053/jhep.2002.35619. [DOI] [PubMed] [Google Scholar]
- 91.Folmer Y, Schneider M, Blum HE, Hafkemeyer P. Reversal of drug resistance of hepatocellular carcinoma cells by adenoviral delivery of anti-ABCC2 antisense constructs. Cancer Gene Ther. 2007;14:875–884. doi: 10.1038/sj.cgt.7701082. [DOI] [PubMed] [Google Scholar]
- 92.Henrich CJ, Bokesch HR, Dean M, Bates SE, Robey RW, Goncharova EI, Wilson JA, McMahon JB. A high-throughput cell-based assay for inhibitors of ABCG2 activity. J Biomol Screen. 2006;11:176–183. doi: 10.1177/1087057105284576. [DOI] [PubMed] [Google Scholar]
- 93.Klonisch T, Wiechec E, Hombach-Klonisch S, Ande SR, Wesselborg S, Schulze-Osthoff K, Los M. Cancer stem cell markers in common cancers - therapeutic implications. Trends Mol Med. 2008;14:450–460. doi: 10.1016/j.molmed.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 94.Mishra L, Derynck R, Mishra B. Transforming growth factor-beta signaling in stem cells and cancer. Science. 2005;310:68–71. doi: 10.1126/science.1118389. [DOI] [PubMed] [Google Scholar]
- 95.Wandzioch E, Zaret KS. Dynamic signaling network for the specification of embryonic pancreas and liver progenitors. Science. 2009;324:1707–1710. doi: 10.1126/science.1174497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Maeda S, Hayashi M, Komiya S, Imamura T, Miyazono K. Endogenous TGF-beta signaling suppresses maturation of osteoblastic mesenchymal cells. EMBO J. 2004;23:552–563. doi: 10.1038/sj.emboj.7600067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ader T, Norel R, Levoci L, Rogler LE. Transcriptional profiling implicates TGFbeta/BMP and Notch signaling pathways in ductular differentiation of fetal murine hepatoblasts. Mech Dev. 2006;123:177–194. doi: 10.1016/j.mod.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 98.Clotman F, Jacquemin P, Plumb-Rudewiez N, Pierreux CE, Van der Smissen P, Dietz HC, Courtoy PJ, Rousseau GG, Lemaigre FP. Control of liver cell fate decision by a gradient of TGF beta signaling modulated by Onecut transcription factors. Genes Dev. 2005;19:1849–1854. doi: 10.1101/gad.340305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rogler CE, Levoci L, Ader T, Massimi A, Tchaikovskaya T, Norel R, Rogler LE. MicroRNA-23b cluster microRNAs regulate transforming growth factor-beta/bone morphogenetic protein signaling and liver stem cell differentiation by targeting Smads. Hepatology. 2009;50:575–584. doi: 10.1002/hep.22982. [DOI] [PubMed] [Google Scholar]
- 100.del Castillo G, Alvarez-Barrientos A, Carmona-Cuenca I, Fernández M, Sánchez A, Fabregat I. Isolation and characterization of a putative liver progenitor population after treatment of fetal rat hepatocytes with TGF-beta. J Cell Physiol. 2008;215:846–855. doi: 10.1002/jcp.21370. [DOI] [PubMed] [Google Scholar]
- 101.Watabe T, Miyazono K. Roles of TGF-beta family signaling in stem cell renewal and differentiation. Cell Res. 2009;19:103–115. doi: 10.1038/cr.2008.323. [DOI] [PubMed] [Google Scholar]
- 102.Amin R, Mishra L. Liver stem cells and tgf-Beta in hepatic carcinogenesis. Gastrointest Cancer Res. 2008;2:S27–S30. [PMC free article] [PubMed] [Google Scholar]
- 103.Tang Y, Kitisin K, Jogunoori W, Li C, Deng CX, Mueller SC, Ressom HW, Rashid A, He AR, Mendelson JS, et al. Progenitor/stem cells give rise to liver cancer due to aberrant TGF-beta and IL-6 signaling. Proc Natl Acad Sci USA. 2008;105:2445–2450. doi: 10.1073/pnas.0705395105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Beachy PA, Karhadkar SS, Berman DM. Tissue repair and stem cell renewal in carcinogenesis. Nature. 2004;432:324–331. doi: 10.1038/nature03100. [DOI] [PubMed] [Google Scholar]
- 105.Dean M. Cancer stem cells: redefining the paradigm of cancer treatment strategies. Mol Interv. 2006;6:140–148. doi: 10.1124/mi.6.3.5. [DOI] [PubMed] [Google Scholar]
- 106.Lou H, Dean M. Targeted therapy for cancer stem cells: the patched pathway and ABC transporters. Oncogene. 2007;26:1357–1360. doi: 10.1038/sj.onc.1210200. [DOI] [PubMed] [Google Scholar]
- 107.Cheng WT, Xu K, Tian DY, Zhang ZG, Liu LJ, Chen Y. Role of Hedgehog signaling pathway in proliferation and invasiveness of hepatocellular carcinoma cells. Int J Oncol. 2009;34:829–836. doi: 10.3892/ijo_00000209. [DOI] [PubMed] [Google Scholar]
- 108.Huang S, He J, Zhang X, Bian Y, Yang L, Xie G, Zhang K, Tang W, Stelter AA, Wang Q, et al. Activation of the hedgehog pathway in human hepatocellular carcinomas. Carcinogenesis. 2006;27:1334–1340. doi: 10.1093/carcin/bgi378. [DOI] [PubMed] [Google Scholar]
- 109.Zhang Y, Laterra J, Pomper MG. Hedgehog pathway inhibitor HhAntag691 is a potent inhibitor of ABCG2/BCRP and ABCB1/Pgp. Neoplasia. 2009;11:96–101. doi: 10.1593/neo.81264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Romer JT, Kimura H, Magdaleno S, Sasai K, Fuller C, Baines H, Connelly M, Stewart CF, Gould S, Rubin LL, et al. Suppression of the Shh pathway using a small molecule inhibitor eliminates medulloblastoma in Ptc1(+/-)p53(-/-) mice. Cancer Cell. 2004;6:229–240. doi: 10.1016/j.ccr.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 111.Willert K, Brown JD, Danenberg E, Duncan AW, Weissman IL, Reya T, Yates JR 3rd, Nusse R. Wnt proteins are lipid-modified and can act as stem cell growth factors. Nature. 2003;423:448–452. doi: 10.1038/nature01611. [DOI] [PubMed] [Google Scholar]
- 112.Yang W, Yan HX, Chen L, Liu Q, He YQ, Yu LX, Zhang SH, Huang DD, Tang L, Kong XN, et al. Wnt/beta-catenin signaling contributes to activation of normal and tumorigenic liver progenitor cells. Cancer Res. 2008;68:4287–4295. doi: 10.1158/0008-5472.CAN-07-6691. [DOI] [PubMed] [Google Scholar]
- 113.Hu TH, Huang CC, Lin PR, Chang HW, Ger LP, Lin YW, Changchien CS, Lee CM, Tai MH. Expression and prognostic role of tumor suppressor gene PTEN/MMAC1/TEP1 in hepatocellular carcinoma. Cancer. 2003;97:1929–1940. doi: 10.1002/cncr.11266. [DOI] [PubMed] [Google Scholar]
- 114.Ali IU, Schriml LM, Dean M. Mutational spectra of PTEN/MMAC1 gene: a tumor suppressor with lipid phosphatase activity. J Natl Cancer Inst. 1999;91:1922–1932. doi: 10.1093/jnci/91.22.1922. [DOI] [PubMed] [Google Scholar]
- 115.Noda T, Nagano H, Takemasa I, Yoshioka S, Murakami M, Wada H, Kobayashi S, Marubashi S, Takeda Y, Dono K, et al. Activation of Wnt/beta-catenin signalling pathway induces chemoresistance to interferon-alpha/5-fluorouracil combination therapy for hepatocellular carcinoma. Br J Cancer. 2009;100:1647–1658. doi: 10.1038/sj.bjc.6605064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.He XC, Yin T, Grindley JC, Tian Q, Sato T, Tao WA, Dirisina R, Porter-Westpfahl KS, Hembree M, Johnson T, et al. PTEN-deficient intestinal stem cells initiate intestinal polyposis. Nat Genet. 2007;39:189–198. doi: 10.1038/ng1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yamashita T, Budhu A, Forgues M, Wang XW. Activation of hepatic stem cell marker EpCAM by Wnt-beta-catenin signaling in hepatocellular carcinoma. Cancer Res. 2007;67:10831–10839. doi: 10.1158/0008-5472.CAN-07-0908. [DOI] [PubMed] [Google Scholar]
- 118.Tan X, Apte U, Micsenyi A, Kotsagrelos E, Luo JH, Ranganathan S, Monga DK, Bell A, Michalopoulos GK, Monga SP. Epidermal growth factor receptor: a novel target of the Wnt/beta-catenin pathway in liver. Gastroenterology. 2005;129:285–302. doi: 10.1053/j.gastro.2005.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wu BW, Wu Y, Wang JL, Lin JS, Yuan SY, Li A, Cui WR. Study on the mechanism of epidermal growth factor-induced proliferation of hepatoma cells. World J Gastroenterol. 2003;9:271–275. doi: 10.3748/wjg.v9.i2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Philip PA, Mahoney MR, Allmer C, Thomas J, Pitot HC, Kim G, Donehower RC, Fitch T, Picus J, Erlichman C. Phase II study of Erlotinib (OSI-774) in patients with advanced hepatocellular cancer. J Clin Oncol. 2005;23:6657–6663. doi: 10.1200/JCO.2005.14.696. [DOI] [PubMed] [Google Scholar]
- 121.Thomas MB, Chadha R, Glover K, Wang X, Morris J, Brown T, Rashid A, Dancey J, Abbruzzese JL. Phase 2 study of erlotinib in patients with unresectable hepatocellular carcinoma. Cancer. 2007;110:1059–1067. doi: 10.1002/cncr.22886. [DOI] [PubMed] [Google Scholar]
- 122.Zhu BD, Yuan SJ, Zhao QC, Li X, Li Y, Lu QY. Antitumor effect of Gefitinib, an epidermal growth factor receptor tyrosine kinase inhibitor, combined with cytotoxic agent on murine hepatocellular carcinoma. World J Gastroenterol. 2005;11:1382–1386. doi: 10.3748/wjg.v11.i9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Höpfner M, Sutter AP, Huether A, Schuppan D, Zeitz M, Scherübl H. Targeting the epidermal growth factor receptor by gefitinib for treatment of hepatocellular carcinoma. J Hepatol. 2004;41:1008–1016. doi: 10.1016/j.jhep.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 124.Schiffer E, Housset C, Cacheux W, Wendum D, Desbois-Mouthon C, Rey C, Clergue F, Poupon R, Barbu V, Rosmorduc O. Gefitinib, an EGFR inhibitor, prevents hepatocellular carcinoma development in the rat liver with cirrhosis. Hepatology. 2005;41:307–314. doi: 10.1002/hep.20538. [DOI] [PubMed] [Google Scholar]
- 125.Zhu AX, Stuart K, Blaszkowsky LS, Muzikansky A, Reitberg DP, Clark JW, Enzinger PC, Bhargava P, Meyerhardt JA, Horgan K, et al. Phase 2 study of cetuximab in patients with advanced hepatocellular carcinoma. Cancer. 2007;110:581–589. doi: 10.1002/cncr.22829. [DOI] [PubMed] [Google Scholar]
- 126.Asnacios A, Fartoux L, Romano O, Tesmoingt C, Louafi S S, Mansoubakht T, Artru P, Poynard T, Rosmorduc O, Hebbar M, et al. Gemcitabine plus oxaliplatin (GEMOX) combined with cetuximab in patients with progressive advanced stage hepatocellular carcinoma: results of a multicenter phase 2 study. Cancer. 2008;112:2733–2739. doi: 10.1002/cncr.23489. [DOI] [PubMed] [Google Scholar]
- 127.Laird AD, Brown PI, Fausto N. Inhibition of tumor growth in liver epithelial cells transfected with a transforming growth factor alpha antisense gene. Cancer Res. 1994;54:4224–4232. [PubMed] [Google Scholar]
- 128.Harada K, Shiota G, Kawasaki H. Transforming growth factor-alpha and epidermal growth factor receptor in chronic liver disease and hepatocellular carcinoma. Liver. 1999;19:318–325. doi: 10.1111/j.1478-3231.1999.tb00056.x. [DOI] [PubMed] [Google Scholar]
- 129.Cheung RS, Brooling JT, Johnson MM, Riehle KJ, Campbell JS, Fausto N. Interactions between MYC and transforming growth factor alpha alter the growth and tumorigenicity of liver progenitor cells. Carcinogenesis. 2007;28:2624–2631. doi: 10.1093/carcin/bgm184. [DOI] [PubMed] [Google Scholar]
- 130.Scharf JG, Braulke T. The role of the IGF axis in hepatocarcinogenesis. Horm Metab Res. 2003;35:685–693. doi: 10.1055/s-2004-814151. [DOI] [PubMed] [Google Scholar]
- 131.Desbois-Mouthon C, Cacheux W, Blivet-Van Eggelpoël MJ, Barbu V, Fartoux L, Poupon R, Housset C, Rosmorduc O. Impact of IGF-1R/EGFR cross-talks on hepatoma cell sensitivity to gefitinib. Int J Cancer. 2006;119:2557–2566. doi: 10.1002/ijc.22221. [DOI] [PubMed] [Google Scholar]
- 132.Feng Y, Zhu Z, Xiao X, Choudhry V, Barrett JC, Dimitrov DS. Novel human monoclonal antibodies to insulin-like growth factor (IGF)-II that potently inhibit the IGF receptor type I signal transduction function. Mol Cancer Ther. 2006;5:114–120. doi: 10.1158/1535-7163.MCT-05-0252. [DOI] [PubMed] [Google Scholar]
- 133.Tanaka S, Arii S. Molecularly targeted therapy for hepatocellular carcinoma. Cancer Sci. 2009;100:1–8. doi: 10.1111/j.1349-7006.2008.01006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lu D, Zhang H, Koo H, Tonra J, Balderes P, Prewett M, Corcoran E, Mangalampalli V, Bassi R, Anselma D, et al. A fully human recombinant IgG-like bispecific antibody to both the epidermal growth factor receptor and the insulin-like growth factor receptor for enhanced antitumor activity. J Biol Chem. 2005;280:19665–19672. doi: 10.1074/jbc.M500815200. [DOI] [PubMed] [Google Scholar]
- 135.Tanimizu N, Miyajima A. Notch signaling controls hepatoblast differentiation by altering the expression of liver-enriched transcription factors. J Cell Sci. 2004;117:3165–3174. doi: 10.1242/jcs.01169. [DOI] [PubMed] [Google Scholar]
- 136.Wang Z, Azmi AS, Ahmad A, Banerjee S, Wang S, Sarkar FH, Mohammad RM. TW-37, a small-molecule inhibitor of Bcl-2, inhibits cell growth and induces apoptosis in pancreatic cancer: involvement of Notch-1 signaling pathway. Cancer Res. 2009;69:2757–2765. doi: 10.1158/0008-5472.CAN-08-3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nijjar SS, Crosby HA, Wallace L, Hubscher SG, Strain AJ. Notch receptor expression in adult human liver: a possible role in bile duct formation and hepatic neovascularization. Hepatology. 2001;34:1184–1192. doi: 10.1053/jhep.2001.29399. [DOI] [PubMed] [Google Scholar]
- 138.Qi R, An H, Yu Y, Zhang M, Liu S, Xu H, Guo Z, Cheng T, Cao X. Notch1 signaling inhibits growth of human hepatocellular carcinoma through induction of cell cycle arrest and apoptosis. Cancer Res. 2003;63:8323–8329. [PubMed] [Google Scholar]
- 139.Finn RS, Zhu AX. Targeting angiogenesis in hepatocellular carcinoma: focus on VEGF and bevacizumab. Expert Rev Anticancer Ther. 2009;9:503–509. doi: 10.1586/era.09.6. [DOI] [PubMed] [Google Scholar]
- 140.Mise M, Arii S, Higashituji H, Furutani M, Niwano M, Harada T, Ishigami S, Toda Y, Nakayama H, Fukumoto M, et al. Clinical significance of vascular endothelial growth factor and basic fibroblast growth factor gene expression in liver tumor. Hepatology. 1996;23:455–464. doi: 10.1053/jhep.1996.v23.pm0008617424. [DOI] [PubMed] [Google Scholar]
- 141.Li XM, Tang ZY, Zhou G, Lui YK, Ye SL. Significance of vascular endothelial growth factor mRNA expression in invasion and metastasis of hepatocellular carcinoma. J Exp Clin Cancer Res. 1998;17:13–17. [PubMed] [Google Scholar]
- 142.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 143.Faivre S, Demetri G, Sargent W, Raymond E. Molecular basis for sunitinib efficacy and future clinical development. Nat Rev Drug Discov. 2007;6:734–745. doi: 10.1038/nrd2380. [DOI] [PubMed] [Google Scholar]
- 144.Siegel AB, Cohen EI, Ocean A, Lehrer D, Goldenberg A, Knox JJ, Chen H, Clark-Garvey S, Weinberg A, Mandeli J, et al. Phase II trial evaluating the clinical and biologic effects of bevacizumab in unresectable hepatocellular carcinoma. J Clin Oncol. 2008;26:2992–2998. doi: 10.1200/JCO.2007.15.9947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Thomas MB, Morris JS, Chadha R, Iwasaki M, Kaur H, Lin E, Kaseb A, Glover K, Davila M, Abbruzzese J. Phase II trial of the combination of bevacizumab and erlotinib in patients who have advanced hepatocellular carcinoma. J Clin Oncol. 2009;27:843–850. doi: 10.1200/JCO.2008.18.3301. [DOI] [PubMed] [Google Scholar]
- 146.Shiraga K, Sakaguchi K, Senoh T, Ohta T, Ogawa S, Sawayama T, Mouri H, Fujiwara A, Tsuji T. Modulation of doxorubicin sensitivity by cyclosporine A in hepatocellular carcinoma cells and their doxorubicin-resistant sublines. J Gastroenterol Hepatol. 2001;16:460–466. doi: 10.1046/j.1440-1746.2001.02457.x. [DOI] [PubMed] [Google Scholar]
- 147.de Bruin M, Miyake K, Litman T, Robey R, Bates SE. Reversal of resistance by GF120918 in cell lines expressing the ABC half-transporter, MXR. Cancer Lett. 1999;146:117–126. doi: 10.1016/s0304-3835(99)00182-2. [DOI] [PubMed] [Google Scholar]
- 148.Warmann S, Göhring G, Teichmann B, Geerlings H, Fuchs J. MDR1 modulators improve the chemotherapy response of human hepatoblastoma to doxorubicin in vitro. J Pediatr Surg. 2002;37:1579–1584. doi: 10.1053/jpsu.2002.36188. [DOI] [PubMed] [Google Scholar]
- 149.Bramwell VH, Morris D, Ernst DS, Hings I, Blackstein M, Venner PM, Ette EI, Harding MW, Waxman A, Demetri GD. Safety and efficacy of the multidrug-resistance inhibitor biricodar (VX-710) with concurrent doxorubicin in patients with anthracycline-resistant advanced soft tissue sarcoma. Clin Cancer Res. 2002;8:383–393. [PubMed] [Google Scholar]
- 150.Allen JD, van Loevezijn A, Lakhai JM, van der Valk M, van Tellingen O, Reid G, Schellens JH, Koomen GJ, Schinkel AH. Potent and specific inhibition of the breast cancer resistance protein multidrug transporter in vitro and in mouse intestine by a novel analogue of fumitremorgin C. Mol Cancer Ther. 2002;1:417–425. [PubMed] [Google Scholar]
- 151.Shiozawa K, Oka M, Soda H, Yoshikawa M, Ikegami Y, Tsurutani J, Nakatomi K, Nakamura Y, Doi S, Kitazaki T, et al. Reversal of breast cancer resistance protein (BCRP/ABCG2)-mediated drug resistance by novobiocin, a coumermycin antibiotic. Int J Cancer. 2004;108:146–151. doi: 10.1002/ijc.11528. [DOI] [PubMed] [Google Scholar]