Abstract
Human herpes virus 6 (HHV-6) infects > 95% of humans. Primary infection which occurs mostly during the first 2 years of life in the form of roseola infantum, non-specific febrile illness, or an asymptomatic illness, results in latency. Reactivation of latent HHV-6 is common after liver transplantation. Since the majority of human beings harbor the latent virus, HHV-6 infections after liver transplantation are most probably caused by endogenous reactivation or superinfection. In a minority of cases, primary HHV-6 infection may occur when an HHV-6-seronegative individual receives a liver allograft from an HHV-6-seropositive donor. The vast majority of HHV-6 infections after liver transplantation are asymptomatic. Only in a minority of cases, when HHV-6 causes a febrile illness associated with rash and myelosuppression, hepatitis, gastroenteritis, pneumonitis, and encephalitis after liver transplantation. In addition, HHV-6 has been implicated in a variety of indirect effects, such as allograft rejection and increased predisposition to and severity of other infections, including cytomegalovirus, hepatitis C virus, and opportunistic fungi. Because of the uncommon nature of the clinical illnesses directly attributed to HHV-6, there is currently no recommended HHV-6-specific approach prevention after liver transplantation. Asymptomatic HHV-6 infection does not require antiviral treatment, while treatment of established HHV-6 disease is treated with intravenous ganciclovir, foscarnet, or cidofovir and this should be complemented by a reduction in immunosuppression.
Keywords: Human herpes virus 6, Opportunistic infections, Liver transplantation, Antivirals
INTRODUCTION
Human herpes virus 6 (HHV-6), a member of the β-Herpesviridae subfamily, was first isolated from human peripheral blood lymphocytes in 1986[1]. It was initially considered an orphan virus, because it was not associated with any human illness until two years after its discovery, when HHV-6 was implicated as the etiologic agent of a common childhood febrile illness known as roseola infantum (also termed exanthem subitum or sixth disease)[2].
Primary infection with HHV-6 occurs most commonly during the first two years of life, and the peak incidence occurs between 6 and 12 mo after birth[3]. By two years, more than 90% of humans have been infected with the virus, as indicated by the presence of a positive HHV-6 IgG antibody[3]. Primary HHV-6 infections may present as an asymptomatic illness or as a febrile syndrome, later accompanied by a maculopapular rash (exanthem subitum)[3]. Primary HHV-6 infection has also been associated with otitis, gastrointestinal symptoms, respiratory distress, seizures, and, more rarely, with encephalitis or hepatitis in children[3-5].
There are two variants of HHV-6, designated variant A and variant B (HHV-6A and HHV-6B), respectively[6,7]. The two subtypes share certain biological properties and a high level of sequence homology, but are clearly two distinct viruses, both virologically and epidemiologically[8,9]. HHV-6B is implicated in the majority of primary HHV-6 infections during the first two years of life. Since HHV-6B replicates in the salivary glands, the mechanism of transmission between humans is thought to be via salivary secretions[10]. On the other hand, HHV-6A seems to be more neurotropic and it has been implicated mainly in neurologic diseases, especially in patients with HIV infection[11-13]. The age of acquisition of HHV-6A remains undetermined, and, unlike HHV-6B, it does not seem to replicate in salivary glands, and its primary mode of transmission is currently not known.
LATENCY AND CHROMOSOMAL INTEGRATION
HHV-6 is a lymphotropic virus that replicates in CD4+ T-lymphocytes[14], and by using the CD46 molecule as its cellular receptor[15], it may also infect other cell types, such as monocytes and macrophages, astrocytes, fibroblasts, and cells of endothelial or epithelial origin[16-20]. HHV-6 infects various organs, including the brain, salivary glands, tonsils, lungs, kidneys and liver[14,21-29]. Primary HHV-6 infection results in the establishment of latent infection, with the virus being located primarily located in mononuclear cells. During latency, HHV-6 genome is harbored mainly as a separate circular DNA inside various cells, such as lymphocytes and monocytes[16]. Indeed, in one study, HHV-6 DNA sequences were detected in peripheral blood mononuclear cells in as many as 90% of the subjects being studied, thus implying the ubiquitous nature of the virus[30].
In the minority of HHV-6 infected individuals, instead of existing as a separate circular DNA, the virus becomes integrated into the host chromosome[31,32]. This is known as a chromosomally-integrated HHV-6 infection. Both HHV-6A and HHV-6B variants have the ability to be integrated into the chromosome. The incidence of chromosomally-integrated HHV-6 infection is not exactly known, although a recent study of blood donors from the United Kingdom estimated an incidence between 0.2%-1%[31]. Because the virus can be found in germ lines, it has also been suggested that chromosomally-integrated HHV-6 may be transmitted from mother to child (i.e. vertical transmission)[32,33]. However, this has not been confirmed by other investigators[34]. Individuals with chromosomally-integrated HHV-6 infection have a characteristic persistently high level of HHV-6 DNA in the blood, serum, and hair follicles, usually millions of genomic copies, but without causing clinical illness[35]. The high level of HHV-6 DNA in the blood and other body fluids in individuals with chromosomally-integrated HHV-6 infection is thought to be due to cellular proliferation and lysis, and not as a result of viral replication. However, in a few individuals with chromosomally-integrated HHV-6, some degree of viral replication may also occur[33]. Many believe that chromosomally-integrated HHV-6 infection is not clinically significant, although there are a few studies reporting on its association with an increased risk of lymphoproliferative diseases[36,37].
MECHANISMS OF HHV-6 INFECTION AFTER LIVER TRANSPLANT
Latent HHV-6 serves as the reservoir for endogenous viral reactivation after transplantation, or as a potential vector of transmission to susceptible individuals via the transplanted organ itself. Given the high seroprevalence of HHV-6 in adults, which is estimated at over 90%-95%, most active infections after liver transplantation are thought to originate from reactivation of the endogenous latent virus. However, primary HHV-6 infection may occur in previously non-infected individuals, and this scenario is more commonly observed in pediatric transplant recipients who are under 2 years of age, who may not have been infected with the virus, and who may in turn have received an organ transplant from an HHV-6 positive donor[38]. Some of the primary HHV-6 infections, which were presumably of donor origin, have resulted in fatal primary HHV-6 diseases[39,40]. Viral reactivation may also occur in the transplanted allograft to cause HHV-6 superinfection in a previously-infected individual[41]. In a minority of cases, primary HHV-6 infection may occur when a transplant patient acquires the virus through blood products, or through natural transmission (e.g. exposure to oropharyngeal secretions).
EPIDEMIOLOGY OF HHV-6 AFTER LIVER TRANSPLANTATION
The reported incidence of HHV-6 infection after liver transplantation ranges widely, between 14% to 82%[42-44]. These estimates vary depending on the population being studied (adults versus children), the use of anti-CMV prophylaxis (ganciclovir products are active against HHV-6 and may suppress its reactivation)[45], the severity of pharmacologic immunosuppression, and the sensitivity of the laboratory methods used for the diagnosis[46]. HHV-6 infections typically occur during the first 2-8 wk after liver transplantation, when the level of immunosuppression is at its most intense. However, HHV-6 infections occurring as early as 10 d, and as late as 5 years, after liver transplantation have been reported[47].
While subclinical HHV-6 infection may be common, the reported incidence of HHV-6-associated clinical disease is rare. HHV-6B accounts for the majority of documented infections and disease in transplant recipients. The epidemiology of HHV-6A after liver transplantation is less well-defined, although it has certainly been reported to cause clinical disease, including those that have resulted in fatal outcomes[39,40].
The risk factors for HHV-6 infections and disease after liver transplantation are not completely defined. Since most infections after liver transplantation probably represent reactivation of latent viruses, it is reasonable to assume that the intensity of pharmacologic immunosuppression may be a risk factor, potentially through prolonged suppression of HHV-6 specific memory responses. Indeed, factors that have been associated with HHV-6 reactivation after liver transplantation are acute allograft rejection and the result of receiving high doses of corticosteroids[47,48]. Certain immunosuppressive agents, including muromunab-CD3 (OKT3), an investigational anti-CD3 monoclonal antibody (BC3), and alemtuzumab have been associated with active HHV-6 infection after transplantation[49,50]. The presence of active HHV-6 infection during acute liver failure has also been reported as a risk factor for the development of hepatic allograft infection after liver transplantation[51].
CLINICAL SYNDROMES ASSOCIATED WITH HHV-6 INFECTION AFTER LIVER TRANSPLANTATION
The vast majority of HHV-6 reactivations and infections after liver transplantation are asymptomatic[47,52-54]. Only in a minority of cases do they cause clinical disease. Nonetheless, there have been a myriad of clinical syndromes associated with HHV-6 infection after liver transplantation, and these have been classified either as direct or indirect effects. The direct clinical manifestations due to HHV-6 include a febrile illness with or without rash, myelosuppression, hepatitis, pneumonitis, gastrointestinal disease, and neurological diseases[47,54-56]. These overt clinical diseases that have been directly attributed to HHV-6 have been estimated to occur in less than 1% of liver transplant patients[57,58]. The indirect effects attributed to HHV-6 are presumed to be consequences of virus-induced immunomodulation and include the exacerbation of cytomegalovirus (CMV) disease, an increased severity of hepatitis C virus (HCV) recurrence, an increased risk of other opportunistic infections, allograft dysfunction, and acute cellular rejection (Table 1)[45,47,53,54,58-62].
Table 1.
Clinical syndromes attributed to human herpes virus 6 after liver transplantation
| Direct effects | Indirect effects |
| Fever | Increased incidence and severity of cytomegalovirus disease |
| Rash | Earlier and more severe recurrence of hepatitis C virus |
| Myelosuppression | Higher incidence of fungal infections |
| Pneumonitis | Higher incidence of other opportunistic infections |
| Hepatitis | Higher incidence of allograft rejection |
| Gastritis and colitis | Higher incidence of allograft failure |
| Neurologic illness | Higher all-cause mortality |
Direct HHV-6 effects
Fever and rash: The most frequently reported clinical presentation of HHV-6 infection after liver transplantation is a febrile illness, frequently associated with myelosuppression and rash[48,54,63]. This clinical presentation of HHV-6 infection mimics the syndrome classically attributed to CMV, and it could thus possibly be misdiagnosed as a CMV syndrome[64]. In a retrospective study of 200 liver transplant recipients, two patients (1%) presented with a febrile illness and, after excluding all other pathogens and etiologies for the fever, HHV-6 was implicated as the causative agent[54]. In a second study involving 67 living-donor liver transplant recipients, five patients with HHV-6 viremia or DNAemia had unexplained fever at the time of infection, and this was accompanied by elevations in serum aminotransferase levels[65]. In a prospective study on 51 adult liver transplant recipients who were frequently monitored for HHV-6, eleven patients developed HHV-6B antigenemia at 7-280 d after transplantation[66], including four patients with HHV-6 associated fever or abdominal pain[66]. Skin rash or myelosuppression were not recorded in any of these patients. In some cases, co-infections between HHV-6 and CMV have been observed[64,67]. However, the contribution of HHV-6 to the clinical illness when CMV is present is debated. In a large study of liver and other solid organ transplant recipients with CMV disease, the presence of concomitant HHV-6 was not significantly associated with more severe clinical symptoms or higher CMV viral load[45,68].
Hepatitis: HHV-6 may infect the liver and cause allograft dysfunction in liver transplant recipients[47]. Clinically, HHV-6 infection of the liver has presented with elevated aminotransferases, allograft dysfunction, acute rejection, and lymphocytic infiltration of the graft (Figure 1A)[47,54]. In one study of 51 liver transplant recipients, there was significant graft dysfunction observed in eight out of 11 patients with HHV-6 antigenemia, and in three of these patients, HHV-6 antigens were detected in their liver biopsy specimens (5.9%)[66,67]. In another study, which was a retrospective review of 121 patients, HHV-6 infection was thought to be the etiologic agent of liver allograft infection after liver transplantation in eight (6.7%) cases[47], shown by serology and immunostaining of HHV-6 antigens in liver biopsy specimens (Figure 1B). HHV-6 antigens were detected in all six available liver biopsy specimens. Histologic examination of biopsy specimens demonstrated acute rejection in 5 of the 8 patients, and 3 patients had portal lymphocyte infiltration[47]. In a study involving 67 living-donor liver transplant patients, the five patients with HHV-6 viremia or HHV-6 DNAemia had elevated aminotransferase levels that accompanied the febrile illness during the time of HHV-6 infection[65]. Another study showed that nine of 18 patients who had pre-transplant hepatic HHV-6B infection developed intra-allograft HHV-6B infection after liver transplantation[51], while another report documented donor-transmitted HHV-6A superinfection in an HHV-6B infected liver transplant recipient, which manifested itself as syncytial giant cell hepatitis[41].
Figure 1.
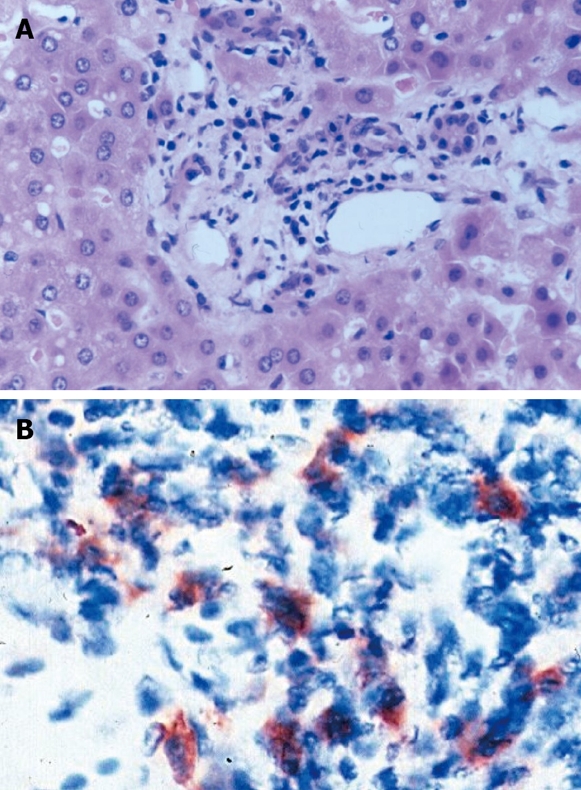
The histological findings associated with intragraft human herpes virus 6 infection. A: Portal area with mild lymphocyte dominated inflammatory infiltrate (H&E staining, original magnification × 400); B: Human herpes virus 6 positive cells in the portal area demonstrated by immunohistochemistry (original magnification × 1000). From Härmä et al. Transplantation 2006; 81: 367-372 with permission[52].
Gastrointestinal disease: HHV-6 infection may manifest with symptoms of gastroenteritis and colitis, and this may or may not be accompanied by detectable HHV-6 viremia[69]. One study evaluated the presence of HHV-6 in the gastroduodenal mucosa of 90 liver transplant recipients who were undergoing gastroscopic examination for dyspeptic symptoms. HHV-6-positive cells were found in the biopsy specimens from 21 (23%) of the liver transplant recipients (Figure 2)[70]. Fifteen of the transplant recipients with positive HHV-6 findings in the gastroduodenal mucosa were also found to have HHV-6 antigenemia. The histopathological findings were, however, nonspecific, and included very mild inflammatory changes[70].
Figure 2.
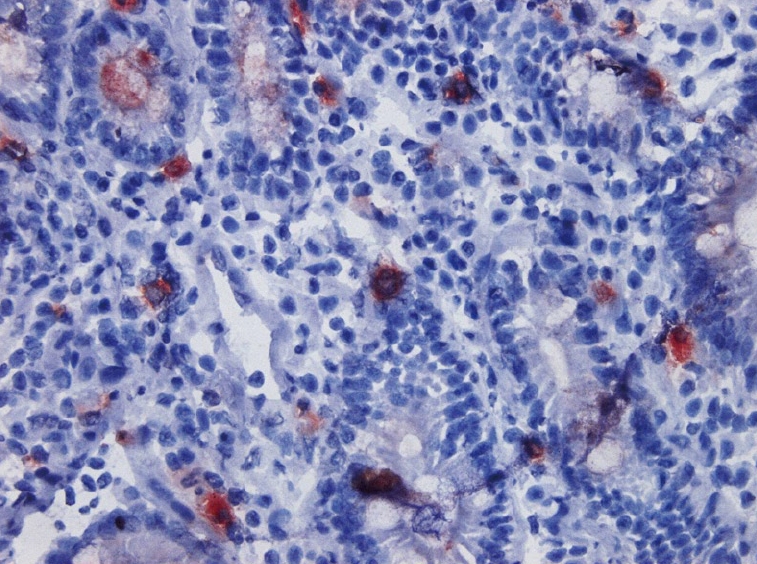
Human herpesvirus-6 positive cells in the gastroduodenal mucosa demonstrated by immunohistochemistry (original magnification × 400). (Courtesy of Dr. Johanna Arola, University of Helsinki, Finland).
Bone marrow suppression: Suppression of the blood cell lines is one of the more common manifestations of HHV-6 infection. In one report, four liver transplant recipients developed HHV-6 associated myelosuppression at a median of 50 d (range 17-90 d) after transplantation. While all the cell lineages were affected, leukopenia was the most common presentation[55].
Pneumonia: HHV-6 may infect the lungs to cause pneumonitis, often in association with other abnormalities such as bone marrow suppression. In one of the four patients with myelosuppression, concomitant interstitial HHV-6 pneumonitis was observed, as documented by positive HHV-6 immunostaining of the lung biopsy specimen[55].
Encephalitis: The vast majority of clinical reports of HHV-6 encephalitis have described its occurrence in allogeneic bone marrow transplant recipients, although HHV-6 has been reported to cause encephalitis in liver transplant recipients[56,71]. Encephalitis typically occurs within 4-6 wk after transplantation and is characterized by confusion, loss of short-term memory, and seizures. Patients will often have normal cerebrospinal fluid profiles, although elevated cerebrospinal fluid protein may be observed. Brain imaging may be abnormal, with hallmark abnormalities found in the medial temporal lobes. In one report, central nervous system complications such as mental status changes of unidentified etiology were more likely to occur in liver transplant recipients who had developed HHV-6 infection[62]. However, another report found no significant association between HHV-6 infection and neurological illnesses[54]. These contradictory results may be due to the differences in neurotropism between HHV-6 variants, with HHV-6A as the neurotropic variant.
Indirect HHV-6 effects
CMV disease: Many studies have described the association among the β-herpes viruses that results in a predisposition to develop CMV disease after liver transplantation. In one study, concurrent HHV-6 antigenemia was detected in 50% of 42 liver transplant patients with active CMV infection[67]. In another study, concurrent CMV and HHV-6 infections were detected in 16 of 19 liver transplant patients at a mean of 11 d (range 6 to 24 d) after transplantation[60]. Since HHV-6 had been detected prior to CMV in most cases, there was a suggestion that HHV-6, through its immunomodulating property, enhanced the reactivation of CMV[60]. Indeed, another study demonstrated that liver transplant recipients with primary HHV-6 seroconversion were more likely to develop symptomatic CMV disease than those who did not have HHV-6 seroconversion[59]. This finding was again demonstrated in a prospective study which revealed that liver transplant recipients who developed CMV disease also had detectable HHV6 DNA in the blood[43]. However, this association between HHV-6 and CMV was not observed in a large cohort of solid organ transplant recipients who received oral ganciclovir and valganciclovir prophylaxis, and which revealed that the incidence of CMV disease was not significantly different between those who did and those who did not develop HHV-6 DNAemia[45]. Alternatively, the presence of HHV-6 may serve as a marker of an over-immunosuppressed state and hence the predisposition to develop other infections, such as CMV.
HCV disease progression: Liver transplant patients with HCV-induced liver cirrhosis were more likely to have HHV-6 infection[65]. Conversely, HHV-6 may be associated with early fibrosis due to HCV recurrence after liver transplantation[58,61], thereby creating a bidirectional relationship. A prospective study reported that HCV-positive patients who developed HHV-6 viremia after liver transplantation had an earlier recurrence and a higher fibrosis score upon hepatitis C recurrence when compared to patients without HHV6 viremia[61]. In another analysis of 60 liver transplant recipients with chronic hepatitis C, HHV-6 infection was associated with more severe hepatitis and higher fibrosis scores[58]. In contrast, a study of 93 HCV-infected liver transplant recipients showed no association between HHV-6 and the incidence and severity of hepatitis C recurrence after transplantation[72].
Fungal and other opportunistic infections: Possibly due to its immune modulating properties, HHV-6 may influence other opportunistic infections after liver transplantation. One study of 200 liver transplant recipients demonstrated the impact of HHV-6 infection on opportunistic infections, including CMV, Epstein Barr virus-related post transplant lymphoproliferative disease, varicella zoster virus, invasive fungal infections, and mycobacterial disease. In a multivariate analysis, HHV-6 was found to be a significant risk factor for the occurrence of these opportunistic infections[54]. In another study, HHV-6 infection was independently associated with the occurrence of invasive fungal infections in a cohort of 80 liver transplant recipients[62]. Likewise, in a study of 247 patients, the incidence of invasive fungal infection was twice as high in patients with HHV-6 seroconversion compared to those without HHV-6 seroconversion[54]. It was further demonstrated that HHV-6 infection was an independent predictor of invasive fungal infections during the first 90 d after liver transplantation[54].
Allograft rejection and function: HHV-6 may cause graft dysfunction and may be associated with rejection[47,53,54]. Local HHV-6 infection of the allograft was associated with increased expression of adhesion molecules on vascular endothelial cells and infiltrating leukocytes, and this could lead to local inflammation and graft damage, leading to dysfunction and rejection[73]. In liver biopsies, there was mild to moderate lymphocyte infiltration associated with HHV-6 infection. HHV-6 significantly increased the vascular expression of ICAM-1 and VCAM-1, and the number of graft-infiltrating lymphocytes positive for LFA-1, VLA-4 and class II antigens[73]. In an analysis of liver transplant recipients who developed allograft rejection, HHV-6 infection was the only factor significantly associated with rejection beyond 30 d after liver transplantation[54]. Another study further supported the independent association between HHV-6 and biopsy-proven acute allograft rejection after liver transplantation[53].
Mortality: A higher all-cause mortality rate after liver transplantation has been reported in patients with HHV-6 infection[62]. This concurs with data from heart-lung[74] and bone marrow transplantation[75]. In another study, all-cause mortality at the last follow-up in liver transplant recipients with HHV-6 reactivation was significantly higher than for those patients without viral reactivation[65].
DIAGNOSIS OF HHV-6 INFECTION
Identification of clinically-relevant HHV-6 infection is hampered by the ubiquitous nature of latent infection[46]. The diagnostic tests that are available for the detection of HHV-6 infection include serology, culture, antigenemia, immunohistochemistry, and nucleic acid amplification assays[76]. In general, serology has inadequate sensitivity and specificity in identifying acute infection in immunocompromised transplant patients, who have impaired ability to mount an effective immune response[46,76]. Moreover, the high HHV-6 seroprevalence rates in adults further limits the potential utility of serology in detecting clinically relevant infections. Culture techniques, on the other hand, are very laborious and are not helpful in real-time management of patients[46,76].
Methods exploiting direct viral detection, such as the detection of nucleic acids by polymerase chain reaction (PCR) or antigenemia, are preferred for the detection of HHV-6 after liver transplantation[46,76]. HHV-6 antigenemia can be detected on mononuclear cells of a whole blood sample by using specific monoclonal antibodies and immunostaining[66]. This technique indicates the presence of an active infection and enables differentiation between HHV-6A and HHV-6B infections. However, it is labor-intensive, semi-quantitative, and it is not widely available for clinical use. This same technique and specific antibodies can be used to demonstrate HHV-6 infection in tissue specimens[47,66].
Molecular assays that detect and amplify HHV-6 nucleic acid are currently the most common laboratory methods for the detection of HHV-6 infection after transplantation. Both quantitative and qualitative methods have been developed to detect HHV-6 DNA in the blood and other clinical samples[77-80]. In addition to blood samples, HHV-6 detection by PCR can also be performed on biopsy and tissue specimens[81]. These assays, depending on the primers used, may differentiate between variants of HHV-6A and HHV-6B as a result of base-differences[77]. PCR testing has some limitations, especially the qualitative assays, which are mainly due to the inability of most assays to distinguish latent from replicating viruses. To address this, the use of serum samples has been suggested, since the virus is cell-associated, and the detection of free viral particles in cell-free serum would be more indicative of active HHV-6 infection[77]. However, this is not the case for whole blood specimens where latent HHV-6 may be present and amplified from leukocytes.
The use of quantitative PCR assays may be helpful in distinguishing replicating from latent HHV-6, with the premise that high HHV-6 levels or increasing viral levels over time would indicate true HHV-6 replication[78]. In the interpretation of HHV-6 viral loads, however, one should take into consideration the rare presence of chromosomally-integrated HHV-6 infections[35,37]. While chromosomally-integrated HHV-6 is rare[31,32], this possibility should be considered when interpreting HHV-6 results in the liver transplant population, in order to avoid unnecessary treatment[82]. Chromosomally-integrated HHV-6 infections are usually detected in high millions of copies of genomic DNA. Detecting HHV-6 by PCR of hair follicles samples also indicates chromosomally-integrated HHV-6[31,32]. The detection of HHV-6 RNA by real-time reverse transcriptase PCR assay, on the other hand, would indicate the presence of an actively replicating virus[83].
Because of the low rate of clinical HHV-6-associated disease and the relatively high rate of subclinical HHV-6 reactivations, it is generally not recommended to perform routine monitoring for HHV-6 after liver transplantation[46]. However, when clinically indicated, such as in certain clinical scenarios including encephalitis, hepatitis or liver allograft dysfunction, these molecular assays may be helpful in confirming a clinical suspicion of HHV-6 infection[11]. In addition, demonstration of HHV-6-specific antigens by immunostaining in the biopsy specimens may be useful in the diagnosis of HHV-6 hepatitis or gastrointestinal infection[47,66,70].
PREVENTION AND TREATMENT OF HHV-6 INFECTIONS
There are no randomized clinical trials that have been conducted of an antiviral drug for the prevention and treatment of HHV 6 disease in humans. As a result, there is currently no antiviral drug that is FDA-approved for clinical use in HHV-6 infection. In the absence of specific antiviral drug therapies, HHV-6-associated diseases have been managed clinically with broad-spectrum anti-herpes drugs such as foscarnet and ganciclovir, and less commonly cidofovir[84]. The clinical use of these drugs has been based mainly on in vitro data and several anecdotal case series and reports[84]. In vitro, HHV-6 is sensitive to achievable concentrations of ganciclovir, foscarnet, and cidofovir[85,86]. Generally, once the anti-herpetic drugs become activated after a series of phosphorylation, they act by inhibiting viral DNA polymerase. However, in vitro data suggests that the ability of HHV-6 pU69 protein kinase to phosphorylate ganciclovir is about 10 fold less when compared to its phosphorylation of CMV[87], suggesting potentially lower efficacy against HHV-6. In addition, the HHV-6A and HHV-6B variants have been demonstrated by different studies to have varying susceptibilities to ganciclovir (although this could potentially be due to the type of cell cultures and viral strains)[85,86]. The HHV-6 variants are resistant to acyclovir and penciclovir[85,86].
The majority of HHV-6 infections are subclinical and transient, and treatment of asymptomatic viral reactivation is not recommended[46]. However, treatment directed against HHV-6 should be initiated in the setting of HHV-6 encephalitis, and should also be considered for other clinical syndromes attributable to HHV-6[46]. The International Herpes Management Forum recommends that HHV-6 infection be considered in the differential diagnosis of encephalitis, particularly in immunocompromised patients[88]. The forum goes on to recommend ganciclovir and foscarnet either alone or in combination as first line therapy for treatment of HHV-6-related central nervous system illness[88]. While studies in order to define precise dosing and duration recommendations have not (yet) been performed, dosing typical for CMV disease is often used. In the setting of HHV-6 encephalitis, some clinicians base duration of therapy on a minimum course of 3-4 wk, and factor in the patient’s clinical course and viral levels over time to define the ultimate course[88]. It should be recognized, however, that active viral replication in brain tissue may persist even after levels in blood and cerebrospinal fluid have resolved[89].
As in the treatment of most cases of opportunistic infections, strong consideration should be given to reducing the degree of pharmacologic immunosuppression when treating HHV-6 disease. This will allow the immune system to develop (among HHV-6-seronegative recipients) or recover (among seropositive recipients) sufficient HHV-6 specific immunity needed for adequate control of infection. Although there is no direct evidence to support this strategy, it is assumed that the degree of immunosuppression is a risk factor that could have led to HHV-6 reactivation and clinical disease.
Indirect evidence suggests that anti-CMV prophylaxis with ganciclovir-containing regimens has been associated with a lower rate and degree of HHV-6 detection[45,90,91]. However, these observations were contradicted by other studies that demonstrated that ganciclovir treatment of CMV disease was not as effective against HHV-6 co-infections[68,92]; these differences in antiviral efficacy may be due to several factors, including viral strains (with HHV-6B considered as the less susceptible variant) and the degree of immunosuppression. Currently, there is insufficient evidence to recommend the routine use of antiviral prophylaxis or preemptive therapy for HHV-6 infection. And since the majority of HHV-6 infections after liver transplantation are subclinical, antiviral prophylaxis or preemptive therapy are currently of questionable benefit.
CONCLUSION
Subclinical HHV-6 infection in liver transplant recipients is common, while clinical HHV-6 disease is rare. Nonetheless, some of the reported HHV-6-associated diseases have led to serious complications and even mortality. The immunomodulatory effect of HHV-6, particularly its interaction with other viruses, and its effect on allograft survival in liver transplant recipients is very intriguing, and needs to be further elucidated. Hence, a better understanding of the impact of HHV-6 in liver transplant recipients is needed. However, this goal is hampered by the challenges in clinical diagnosis, due to the lack of standardized diagnostic methodologies. Although currently available antivirals have been used for treating severe cases of HHV-6 infections, well-controlled clinical studies that support their clinical use are still lacking.
Footnotes
Peer reviewers: Shinichi Ueno, MD, PhD, Department of Surgical Oncology and Digestive Surgery, Field of Oncology, Course of Advanced Therapeutics, Kagoshima University Graduate School of Medicine and Dental Sciences, 8-35-1 Sakuragaoka, Kagoshima 890, Japan; Pierluigi Toniutto, Professor, Internal Medicine, Medical Liver Transplant Unit, University of Udine, P. zale S.M. della Misericordia 1, Udine 33100, Italy
S- Editor Zhang HN L- Editor Herholdt A E- Editor Liu N
References
- 1.Salahuddin SZ, Ablashi DV, Markham PD, Josephs SF, Sturzenegger S, Kaplan M, Halligan G, Biberfeld P, Wong-Staal F, Kramarsky B. Isolation of a new virus, HBLV, in patients with lymphoproliferative disorders. Science. 1986;234:596–601. doi: 10.1126/science.2876520. [DOI] [PubMed] [Google Scholar]
- 2.Yamanishi K, Okuno T, Shiraki K, Takahashi M, Kondo T, Asano Y, Kurata T. Identification of human herpesvirus-6 as a causal agent for exanthem subitum. Lancet. 1988;1:1065–1067. doi: 10.1016/s0140-6736(88)91893-4. [DOI] [PubMed] [Google Scholar]
- 3.Zerr DM, Meier AS, Selke SS, Frenkel LM, Huang ML, Wald A, Rhoads MP, Nguy L, Bornemann R, Morrow RA, et al. A population-based study of primary human herpesvirus 6 infection. N Engl J Med. 2005;352:768–776. doi: 10.1056/NEJMoa042207. [DOI] [PubMed] [Google Scholar]
- 4.Pruksananonda P, Hall CB, Insel RA, McIntyre K, Pellett PE, Long CE, Schnabel KC, Pincus PH, Stamey FR, Dambaugh TR. Primary human herpesvirus 6 infection in young children. N Engl J Med. 1992;326:1445–1450. doi: 10.1056/NEJM199205283262201. [DOI] [PubMed] [Google Scholar]
- 5.Hall CB, Long CE, Schnabel KC, Caserta MT, McIntyre KM, Costanzo MA, Knott A, Dewhurst S, Insel RA, Epstein LG. Human herpesvirus-6 infection in children. A prospective study of complications and reactivation. N Engl J Med. 1994;331:432–438. doi: 10.1056/NEJM199408183310703. [DOI] [PubMed] [Google Scholar]
- 6.Ablashi DV, Balachandran N, Josephs SF, Hung CL, Krueger GR, Kramarsky B, Salahuddin SZ, Gallo RC. Genomic polymorphism, growth properties, and immunologic variations in human herpesvirus-6 isolates. Virology. 1991;184:545–552. doi: 10.1016/0042-6822(91)90424-a. [DOI] [PubMed] [Google Scholar]
- 7.Schirmer EC, Wyatt LS, Yamanishi K, Rodriguez WJ, Frenkel N. Differentiation between two distinct classes of viruses now classified as human herpesvirus 6. Proc Natl Acad Sci USA. 1991;88:5922–5926. doi: 10.1073/pnas.88.13.5922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindquester GJ, O’Brian JJ, Anton ED, Greenamoyer CA, Pellett PE, Dambaugh TR. Genetic content of a 20.9 kb segment of human herpesvirus 6B strain Z29 spanning the homologs of human herpesvirus 6A genes U40-57 and containing the origin of DNA replication. Arch Virol. 1997;142:103–123. doi: 10.1007/s007050050062. [DOI] [PubMed] [Google Scholar]
- 9.Gompels UA, Nicholas J, Lawrence G, Jones M, Thomson BJ, Martin ME, Efstathiou S, Craxton M, Macaulay HA. The DNA sequence of human herpesvirus-6: structure, coding content, and genome evolution. Virology. 1995;209:29–51. doi: 10.1006/viro.1995.1228. [DOI] [PubMed] [Google Scholar]
- 10.Levy JA, Ferro F, Greenspan D, Lennette ET. Frequent isolation of HHV-6 from saliva and high seroprevalence of the virus in the population. Lancet. 1990;335:1047–1050. doi: 10.1016/0140-6736(90)92628-u. [DOI] [PubMed] [Google Scholar]
- 11.Dewhurst S, McIntyre K, Schnabel K, Hall CB. Human herpesvirus 6 (HHV-6) variant B accounts for the majority of symptomatic primary HHV-6 infections in a population of U.S. infants. J Clin Microbiol. 1993;31:416–418. doi: 10.1128/jcm.31.2.416-418.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Razonable RR, Fanning C, Brown RA, Espy MJ, Rivero A, Wilson J, Kremers W, Smith TF, Paya CV. Selective reactivation of human herpesvirus 6 variant a occurs in critically ill immunocompetent hosts. J Infect Dis. 2002;185:110–113. doi: 10.1086/324772. [DOI] [PubMed] [Google Scholar]
- 13.Knox KK, Harrington DP, Carrigan DR. Fulminant human herpesvirus six encephalitis in a human immunodeficiency virus-infected infant. J Med Virol. 1995;45:288–292. doi: 10.1002/jmv.1890450309. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi K, Sonoda S, Higashi K, Kondo T, Takahashi H, Takahashi M, Yamanishi K. Predominant CD4 T-lymphocyte tropism of human herpesvirus 6-related virus. J Virol. 1989;63:3161–3163. doi: 10.1128/jvi.63.7.3161-3163.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santoro F, Kennedy PE, Locatelli G, Malnati MS, Berger EA, Lusso P. CD46 is a cellular receptor for human herpesvirus 6. Cell. 1999;99:817–827. doi: 10.1016/s0092-8674(00)81678-5. [DOI] [PubMed] [Google Scholar]
- 16.Kondo K, Kondo T, Okuno T, Takahashi M, Yamanishi K. Latent human herpesvirus 6 infection of human monocytes/macrophages. J Gen Virol. 1991;72(Pt 6):1401–1408. doi: 10.1099/0022-1317-72-6-1401. [DOI] [PubMed] [Google Scholar]
- 17.He J, McCarthy M, Zhou Y, Chandran B, Wood C. Infection of primary human fetal astrocytes by human herpesvirus 6. J Virol. 1996;70:1296–1300. doi: 10.1128/jvi.70.2.1296-1300.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caruso A, Rotola A, Comar M, Favilli F, Galvan M, Tosetti M, Campello C, Caselli E, Alessandri G, Grassi M, et al. HHV-6 infects human aortic and heart microvascular endothelial cells, increasing their ability to secrete proinflammatory chemokines. J Med Virol. 2002;67:528–533. doi: 10.1002/jmv.10133. [DOI] [PubMed] [Google Scholar]
- 19.Chen M, Popescu N, Woodworth C, Berneman Z, Corbellino M, Lusso P, Ablashi DV, DiPaolo JA. Human herpesvirus 6 infects cervical epithelial cells and transactivates human papillomavirus gene expression. J Virol. 1994;68:1173–1178. doi: 10.1128/jvi.68.2.1173-1178.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luka J, Okano M, Thiele G. Isolation of human herpesvirus-6 from clinical specimens using human fibroblast cultures. J Clin Lab Anal. 1990;4:483–486. doi: 10.1002/jcla.1860040617. [DOI] [PubMed] [Google Scholar]
- 21.Luppi M, Barozzi P, Maiorana A, Marasca R, Torelli G. Human herpesvirus 6 infection in normal human brain tissue. J Infect Dis. 1994;169:943–944. doi: 10.1093/infdis/169.4.943. [DOI] [PubMed] [Google Scholar]
- 22.Luppi M, Barozzi P, Marasca R, Torelli G. Integration of human herpesvirus-6 (HHV-6) genome in chromosome 17 in two lymphoma patients. Leukemia. 1994;8 Suppl 1:S41–S45. [PubMed] [Google Scholar]
- 23.Fox JD, Briggs M, Ward PA, Tedder RS. Human herpesvirus 6 in salivary glands. Lancet. 1990;336:590–593. doi: 10.1016/0140-6736(90)93392-3. [DOI] [PubMed] [Google Scholar]
- 24.Roush KS, Domiati-Saad RK, Margraf LR, Krisher K, Scheuermann RH, Rogers BB, Dawson DB. Prevalence and cellular reservoir of latent human herpesvirus 6 in tonsillar lymphoid tissue. Am J Clin Pathol. 2001;116:648–654. doi: 10.1309/Y2HH-B1CK-0F5L-U7B8. [DOI] [PubMed] [Google Scholar]
- 25.Hammerling JA, Lambrecht RS, Kehl KS, Carrigan DR. Prevalence of human herpesvirus 6 in lung tissue from children with pneumonitis. J Clin Pathol. 1996;49:802–804. doi: 10.1136/jcp.49.10.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gupta M, Diaz-Mitoma F, Feber J, Shaw L, Forget C, Filler G. Tissue HHV6 and 7 determination in pediatric solid organ recipients--a pilot study. Pediatr Transplant. 2003;7:458–463. doi: 10.1046/j.1399-3046.2003.00099.x. [DOI] [PubMed] [Google Scholar]
- 27.Ozaki Y, Tajiri H, Tanaka-Taya K, Mushiake S, Kimoto A, Yamanishi K, Okada S. Frequent detection of the human herpesvirus 6-specific genomes in the livers of children with various liver diseases. J Clin Microbiol. 2001;39:2173–2177. doi: 10.1128/JCM.39.6.2173-2177.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grivel JC, Santoro F, Chen S, Fagá G, Malnati MS, Ito Y, Margolis L, Lusso P. Pathogenic effects of human herpesvirus 6 in human lymphoid tissue ex vivo. J Virol. 2003;77:8280–8289. doi: 10.1128/JVI.77.15.8280-8289.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lusso P, Malnati MS, Garzino-Demo A, Crowley RW, Long EO, Gallo RC. Infection of natural killer cells by human herpesvirus 6. Nature. 1993;362:458–462. doi: 10.1038/362458a0. [DOI] [PubMed] [Google Scholar]
- 30.Luppi M, Barozzi P, Morris C, Maiorana A, Garber R, Bonacorsi G, Donelli A, Marasca R, Tabilio A, Torelli G. Human herpesvirus 6 latently infects early bone marrow progenitors in vivo. J Virol. 1999;73:754–759. doi: 10.1128/jvi.73.1.754-759.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leong HN, Tuke PW, Tedder RS, Khanom AB, Eglin RP, Atkinson CE, Ward KN, Griffiths PD, Clark DA. The prevalence of chromosomally integrated human herpesvirus 6 genomes in the blood of UK blood donors. J Med Virol. 2007;79:45–51. doi: 10.1002/jmv.20760. [DOI] [PubMed] [Google Scholar]
- 32.Tanaka-Taya K, Sashihara J, Kurahashi H, Amo K, Miyagawa H, Kondo K, Okada S, Yamanishi K. Human herpesvirus 6 (HHV-6) is transmitted from parent to child in an integrated form and characterization of cases with chromosomally integrated HHV-6 DNA. J Med Virol. 2004;73:465–473. doi: 10.1002/jmv.20113. [DOI] [PubMed] [Google Scholar]
- 33.Hall CB, Caserta MT, Schnabel K, Shelley LM, Marino AS, Carnahan JA, Yoo C, Lofthus GK, McDermott MP. Chromosomal integration of human herpesvirus 6 is the major mode of congenital human herpesvirus 6 infection. Pediatrics. 2008;122:513–520. doi: 10.1542/peds.2007-2838. [DOI] [PubMed] [Google Scholar]
- 34.Luppi M, Barozzi P, Bosco R, Vallerini D, Potenza L, Forghieri F, Torelli G. Human herpesvirus 6 latency characterized by high viral load: chromosomal integration in many, but not all, cells. J Infect Dis. 2006;194:1020–1021; author reply 1021-1023. doi: 10.1086/506952. [DOI] [PubMed] [Google Scholar]
- 35.Ward KN, Leong HN, Nacheva EP, Howard J, Atkinson CE, Davies NW, Griffiths PD, Clark DA. Human herpesvirus 6 chromosomal integration in immunocompetent patients results in high levels of viral DNA in blood, sera, and hair follicles. J Clin Microbiol. 2006;44:1571–1574. doi: 10.1128/JCM.44.4.1571-1574.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bandobashi K, Daibata M, Kamioka M, Tanaka Y, Kubonishi I, Taguchi H, Ohtsuki Y, Miyoshi I. Human herpesvirus 6 (HHV-6)-positive Burkitt’s lymphoma: establishment of a novel cell line infected with HHV-6. Blood. 1997;90:1200–1207. [PubMed] [Google Scholar]
- 37.Daibata M, Taguchi T, Kamioka M, Kubonishi I, Taguchi H, Miyoshi I. Identification of integrated human herpesvirus 6 DNA in early pre-B cell acute lymphoblastic leukemia. Leukemia. 1998;12:1002–1004. doi: 10.1038/sj.leu.2401036. [DOI] [PubMed] [Google Scholar]
- 38.Feldstein AE, Razonable RR, Boyce TG, Freese DK, El-Youssef M, Perrault J, Paya CV, Ishitani MB. Prevalence and clinical significance of human herpesviruses 6 and 7 active infection in pediatric liver transplant patients. Pediatr Transplant. 2003;7:125–129. doi: 10.1034/j.1399-3046.2003.00028.x. [DOI] [PubMed] [Google Scholar]
- 39.Rossi C, Delforge ML, Jacobs F, Wissing M, Pradier O, Remmelink M, Byl B, Thys JP, Liesnard C. Fatal primary infection due to human herpesvirus 6 variant A in a renal transplant recipient. Transplantation. 2001;71:288–292. doi: 10.1097/00007890-200101270-00021. [DOI] [PubMed] [Google Scholar]
- 40.Revest M, Camus C, D’Halluin PN, Cha S, Compagnon P, Boudjema K, Colimon R, Thomas R. Fatal human herpes virus 6 primary infection after liver transplantation. Transplantation. 2007;83:1404–1405. doi: 10.1097/01.tp.0000261705.78595.98. [DOI] [PubMed] [Google Scholar]
- 41.Potenza L, Luppi M, Barozzi P, Rossi G, Cocchi S, Codeluppi M, Pecorari M, Masetti M, Di Benedetto F, Gennari W, et al. HHV-6A in syncytial giant-cell hepatitis. N Engl J Med. 2008;359:593–602. doi: 10.1056/NEJMoa074479. [DOI] [PubMed] [Google Scholar]
- 42.Dockrell DH, Paya CV. Human herpesvirus-6 and -7 in transplantation. Rev Med Virol. 2001;11:23–36. doi: 10.1002/rmv.299. [DOI] [PubMed] [Google Scholar]
- 43.Mendez JC, Dockrell DH, Espy MJ, Smith TF, Wilson JA, Harmsen WS, Ilstrup D, Paya CV. Human beta-herpesvirus interactions in solid organ transplant recipients. J Infect Dis. 2001;183:179–184. doi: 10.1086/317929. [DOI] [PubMed] [Google Scholar]
- 44.Emery VC. Human herpesviruses 6 and 7 in solid organ transplant recipients. Clin Infect Dis. 2001;32:1357–1360. doi: 10.1086/320000. [DOI] [PubMed] [Google Scholar]
- 45.Razonable RR, Brown RA, Humar A, Covington E, Alecock E, Paya CV. Herpesvirus infections in solid organ transplant patients at high risk of primary cytomegalovirus disease. J Infect Dis. 2005;192:1331–1339. doi: 10.1086/466529. [DOI] [PubMed] [Google Scholar]
- 46.Razonable RR, Zerr DM. HHV-6, HHV-7 and HHV-8 in solid organ transplant recipients. Am J Transplant. 2009;9 Suppl 4:S97–S100. doi: 10.1111/j.1600-6143.2009.02899_1.x. [DOI] [PubMed] [Google Scholar]
- 47.Lautenschlager I, Höckerstedt K, Linnavuori K, Taskinen E. Human herpesvirus-6 infection after liver transplantation. Clin Infect Dis. 1998;26:702–707. doi: 10.1086/514592. [DOI] [PubMed] [Google Scholar]
- 48.Singh N, Carrigan DR, Gayowski T, Singh J, Marino IR. Variant B human herpesvirus-6 associated febrile dermatosis with thrombocytopenia and encephalopathy in a liver transplant recipient. Transplantation. 1995;60:1355–1357. [PubMed] [Google Scholar]
- 49.Jacobs U, Ferber J, Klehr HU. Severe allograft dysfunction after OKT3-induced human herpes virus-6 reactivation. Transplant Proc. 1994;26:3121. [PubMed] [Google Scholar]
- 50.Peleg AY, Husain S, Kwak EJ, Silveira FP, Ndirangu M, Tran J, Shutt KA, Shapiro R, Thai N, Abu-Elmagd K, et al. Opportunistic infections in 547 organ transplant recipients receiving alemtuzumab, a humanized monoclonal CD-52 antibody. Clin Infect Dis. 2007;44:204–212. doi: 10.1086/510388. [DOI] [PubMed] [Google Scholar]
- 51.Härmä M, Höckerstedt K, Krogerus L, Lautenschlager I. Pretransplant human herpesvirus 6 infection of patients with acute liver failure is a risk factor for posttransplant human herpesvirus 6 infection of the liver. Transplantation. 2006;81:367–372. doi: 10.1097/01.tp.0000195771.83614.0b. [DOI] [PubMed] [Google Scholar]
- 52.Schmidt CA, Wilbron F, Weiss K, Brinkmann V, Oettle H, Lohmann R, Langrehr JM, Neuhaus P, Siegert W. A prospective study of human herpesvirus type 6 detected by polymerase chain reaction after liver transplantation. Transplantation. 1996;61:662–664. doi: 10.1097/00007890-199602270-00027. [DOI] [PubMed] [Google Scholar]
- 53.Griffiths PD, Ait-Khaled M, Bearcroft CP, Clark DA, Quaglia A, Davies SE, Burroughs AK, Rolles K, Kidd IM, Knight SN, et al. Human herpesviruses 6 and 7 as potential pathogens after liver transplant: prospective comparison with the effect of cytomegalovirus. J Med Virol. 1999;59:496–501. doi: 10.1002/(sici)1096-9071(199912)59:4<496::aid-jmv12>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 54.Humar A, Kumar D, Caliendo AM, Moussa G, Ashi-Sulaiman A, Levy G, Mazzulli T. Clinical impact of human herpesvirus 6 infection after liver transplantation. Transplantation. 2002;73:599–604. doi: 10.1097/00007890-200202270-00021. [DOI] [PubMed] [Google Scholar]
- 55.Singh N, Carrigan DR, Gayowski T, Marino IR. Human herpesvirus-6 infection in liver transplant recipients: documentation of pathogenicity. Transplantation. 1997;64:674–678. doi: 10.1097/00007890-199709150-00002. [DOI] [PubMed] [Google Scholar]
- 56.Montejo M, Ramon Fernandez J, Testillano M, Valdivieso A, Aguirrebengoa K, Varas C, Olaizola A, De Urbina JO. Encephalitis caused by human herpesvirus-6 in a liver transplant recipient. Eur Neurol. 2002;48:234–235. doi: 10.1159/000066172. [DOI] [PubMed] [Google Scholar]
- 57.Cervera C, Marcos MA, Linares L, Roig E, Benito N, Pumarola T, Moreno A. A prospective survey of human herpesvirus-6 primary infection in solid organ transplant recipients. Transplantation. 2006;82:979–982. doi: 10.1097/01.tp.0000229938.12722.ee. [DOI] [PubMed] [Google Scholar]
- 58.Humar A, Kumar D, Raboud J, Caliendo AM, Moussa G, Levy G, Mazzulli T. Interactions between cytomegalovirus, human herpesvirus-6, and the recurrence of hepatitis C after liver transplantation. Am J Transplant. 2002;2:461–466. doi: 10.1034/j.1600-6143.2002.20511.x. [DOI] [PubMed] [Google Scholar]
- 59.Dockrell DH, Mendez JC, Jones M, Harmsen WS, Ilstrup DM, Smith TF, Wiesner RH, Krom RA, Paya CV. Human herpesvirus 6 seronegativity before transplantation predicts the occurrence of fungal infection in liver transplant recipients. Transplantation. 1999;67:399–403. doi: 10.1097/00007890-199902150-00010. [DOI] [PubMed] [Google Scholar]
- 60.Härmä M, Höckerstedt K, Lyytikäinen O, Lautenschlager I. HHV-6 and HHV-7 antigenemia related to CMV infection after liver transplantation. J Med Virol. 2006;78:800–805. doi: 10.1002/jmv.20626. [DOI] [PubMed] [Google Scholar]
- 61.Singh N, Husain S, Carrigan DR, Knox KK, Weck KE, Wagener MM, Gayowski T. Impact of human herpesvirus-6 on the frequency and severity of recurrent hepatitis C virus hepatitis in liver transplant recipients. Clin Transplant. 2002;16:92–96. doi: 10.1034/j.1399-0012.2002.1o096.x. [DOI] [PubMed] [Google Scholar]
- 62.Rogers J, Rohal S, Carrigan DR, Kusne S, Knox KK, Gayowski T, Wagener MM, Fung JJ, Singh N. Human herpesvirus-6 in liver transplant recipients: role in pathogenesis of fungal infections, neurologic complications, and outcome. Transplantation. 2000;69:2566–2573. doi: 10.1097/00007890-200006270-00016. [DOI] [PubMed] [Google Scholar]
- 63.Chang FY, Singh N, Gayowski T, Wagener MM, Marino IR. Fever in liver transplant recipients: changing spectrum of etiologic agents. Clin Infect Dis. 1998;26:59–65. doi: 10.1086/516265. [DOI] [PubMed] [Google Scholar]
- 64.Razonable RR, Rivero A, Brown RA, Hart GD, Espy MJ, van Cruijsen H, Wilson J, Groettum C, Kremers W, Smith TF, et al. Detection of simultaneous beta-herpesvirus infections in clinical syndromes due to defined cytomegalovirus infection. Clin Transplant. 2003;17:114–120. doi: 10.1034/j.1399-0012.2003.02104.x. [DOI] [PubMed] [Google Scholar]
- 65.Ohashi M, Sugata K, Ihira M, Asano Y, Egawa H, Takada Y, Uemoto S, Yoshikawa T. Human herpesvirus 6 infection in adult living related liver transplant recipients. Liver Transpl. 2008;14:100–109. doi: 10.1002/lt.21304. [DOI] [PubMed] [Google Scholar]
- 66.Lautenschlager I, Linnavuori K, Höckerstedt K. Human herpesvirus-6 antigenemia after liver transplantation. Transplantation. 2000;69:2561–2566. doi: 10.1097/00007890-200006270-00015. [DOI] [PubMed] [Google Scholar]
- 67.Lautenschlager I, Linnavuori K, Lappalainen M, Suni J, Höckerstedt K. HHV-6 reactivation is often associated with CMV infection in liver transplant patients. Transpl Int. 2000;13 Suppl 1:S351–S353. doi: 10.1007/s001470050359. [DOI] [PubMed] [Google Scholar]
- 68.Humar A, Asberg A, Kumar D, Hartmann A, Moussa G, Jardine A, Rollag H, Mouas H, Gahlemann CG, Pescovitz MD. An assessment of herpesvirus co-infections in patients with CMV disease: correlation with clinical and virologic outcomes. Am J Transplant. 2009;9:374–381. doi: 10.1111/j.1600-6143.2008.02501.x. [DOI] [PubMed] [Google Scholar]
- 69.Lamoth F, Jayet PY, Aubert JD, Rotman S, Mottet C, Sahli R, Lautenschlager I, Pascual M, Meylan P. Case report: human herpesvirus 6 reactivation associated with colitis in a lung transplant recipient. J Med Virol. 2008;80:1804–1807. doi: 10.1002/jmv.21268. [DOI] [PubMed] [Google Scholar]
- 70.Halme L, Arola J, Höckerstedt K, Lautenschlager I. Human herpesvirus 6 infection of the gastroduodenal mucosa. Clin Infect Dis. 2008;46:434–439. doi: 10.1086/525264. [DOI] [PubMed] [Google Scholar]
- 71.Singh N, Paterson DL. Encephalitis caused by human herpesvirus-6 in transplant recipients: relevance of a novel neurotropic virus. Transplantation. 2000;69:2474–2479. doi: 10.1097/00007890-200006270-00002. [DOI] [PubMed] [Google Scholar]
- 72.Razonable RR, Burak KW, van Cruijsen H, Brown RA, Charlton MR, Smith TF, Espy MJ, Kremers W, Wilson JA, Groettum C, et al. The pathogenesis of hepatitis C virus is influenced by cytomegalovirus. Clin Infect Dis. 2002;35:974–981. doi: 10.1086/342911. [DOI] [PubMed] [Google Scholar]
- 73.Lautenschlager I, Härmä M, Höckerstedt K, Linnavuori K, Loginov R, Taskinen E. Human herpesvirus-6 infection is associated with adhesion molecule induction and lymphocyte infiltration in liver allografts. J Hepatol. 2002;37:648–654. doi: 10.1016/s0168-8278(02)00246-5. [DOI] [PubMed] [Google Scholar]
- 74.Jacobs F, Knoop C, Brancart F, Gilot P, Mélot C, Byl B, Delforge ML, Estenne M, Liesnard C. Human herpesvirus-6 infection after lung and heart-lung transplantation: a prospective longitudinal study. Transplantation. 2003;75:1996–2001. doi: 10.1097/01.TP.0000058809.42027.66. [DOI] [PubMed] [Google Scholar]
- 75.Zerr DM, Corey L, Kim HW, Huang ML, Nguy L, Boeckh M. Clinical outcomes of human herpesvirus 6 reactivation after hematopoietic stem cell transplantation. Clin Infect Dis. 2005;40:932–940. doi: 10.1086/428060. [DOI] [PubMed] [Google Scholar]
- 76.Abdel Massih RC, Razonable RR. Human herpesvirus 6 infections after liver transplantation. World J Gastroenterol. 2009;15:2561–2569. doi: 10.3748/wjg.15.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gautheret-Dejean A, Manichanh C, Thien-Ah-Koon F, Fillet AM, Mangeney N, Vidaud M, Dhedin N, Vernant JP, Agut H. Development of a real-time polymerase chain reaction assay for the diagnosis of human herpesvirus-6 infection and application to bone marrow transplant patients. J Virol Methods. 2002;100:27–35. doi: 10.1016/s0166-0934(01)00390-1. [DOI] [PubMed] [Google Scholar]
- 78.Alvarez-Lafuente R, De las Heras V, Bartolomé M, Picazo JJ, Arroyo R. Relapsing-remitting multiple sclerosis and human herpesvirus 6 active infection. Arch Neurol. 2004;61:1523–1527. doi: 10.1001/archneur.61.10.1523. [DOI] [PubMed] [Google Scholar]
- 79.Zhen Z, Bradel-Tretheway B, Sumagin S, Bidlack JM, Dewhurst S. The human herpesvirus 6 G protein-coupled receptor homolog U51 positively regulates virus replication and enhances cell-cell fusion in vitro. J Virol. 2005;79:11914–11924. doi: 10.1128/JVI.79.18.11914-11924.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Secchiero P, Carrigan DR, Asano Y, Benedetti L, Crowley RW, Komaroff AL, Gallo RC, Lusso P. Detection of human herpesvirus 6 in plasma of children with primary infection and immunosuppressed patients by polymerase chain reaction. J Infect Dis. 1995;171:273–280. doi: 10.1093/infdis/171.2.273. [DOI] [PubMed] [Google Scholar]
- 81.Clark DA, Ait-Khaled M, Wheeler AC, Kidd IM, McLaughlin JE, Johnson MA, Griffiths PD, Emery VC. Quantification of human herpesvirus 6 in immunocompetent persons and post-mortem tissues from AIDS patients by PCR. J Gen Virol. 1996;77(Pt 9):2271–2275. doi: 10.1099/0022-1317-77-9-2271. [DOI] [PubMed] [Google Scholar]
- 82.Clark DA, Nacheva EP, Leong HN, Brazma D, Li YT, Tsao EH, Buyck HC, Atkinson CE, Lawson HM, Potter MN, et al. Transmission of integrated human herpesvirus 6 through stem cell transplantation: implications for laboratory diagnosis. J Infect Dis. 2006;193:912–916. doi: 10.1086/500838. [DOI] [PubMed] [Google Scholar]
- 83.Pradeau K, Bordessoule D, Szelag JC, Rolle F, Ferrat P, Le Meur Y, Turlure P, Denis F, Ranger-Rogez S. A reverse transcription-nested PCR assay for HHV-6 mRNA early transcript detection after transplantation. J Virol Methods. 2006;134:41–47. doi: 10.1016/j.jviromet.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 84.De Bolle L, Naesens L, De Clercq E. Update on human herpesvirus 6 biology, clinical features, and therapy. Clin Microbiol Rev. 2005;18:217–245. doi: 10.1128/CMR.18.1.217-245.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yoshida M, Yamada M, Tsukazaki T, Chatterjee S, Lakeman FD, Nii S, Whitley RJ. Comparison of antiviral compounds against human herpesvirus 6 and 7. Antiviral Res. 1998;40:73–84. doi: 10.1016/s0166-3542(98)00049-7. [DOI] [PubMed] [Google Scholar]
- 86.De Clercq E, Naesens L, De Bolle L, Schols D, Zhang Y, Neyts J. Antiviral agents active against human herpesviruses HHV-6, HHV-7 and HHV-8. Rev Med Virol. 2001;11:381–395. doi: 10.1002/rmv.336. [DOI] [PubMed] [Google Scholar]
- 87.De Bolle L, Michel D, Mertens T, Manichanh C, Agut H, De Clercq E, Naesens L. Role of the human herpesvirus 6 u69-encoded kinase in the phosphorylation of ganciclovir. Mol Pharmacol. 2002;62:714–721. doi: 10.1124/mol.62.3.714. [DOI] [PubMed] [Google Scholar]
- 88.Dewhurst S. Human herpesvirus type 6 and human herpesvirus type 7 infections of the central nervous system. Herpes. 2004;11 Suppl 2:105A–111A. [PubMed] [Google Scholar]
- 89.Fotheringham J, Akhyani N, Vortmeyer A, Donati D, Williams E, Oh U, Bishop M, Barrett J, Gea-Banacloche J, Jacobson S. Detection of active human herpesvirus-6 infection in the brain: correlation with polymerase chain reaction detection in cerebrospinal fluid. J Infect Dis. 2007;195:450–454. doi: 10.1086/510757. [DOI] [PubMed] [Google Scholar]
- 90.Rapaport D, Engelhard D, Tagger G, Or R, Frenkel N. Antiviral prophylaxis may prevent human herpesvirus-6 reactivation in bone marrow transplant recipients. Transpl Infect Dis. 2002;4:10–16. doi: 10.1034/j.1399-3062.2002.040101.x. [DOI] [PubMed] [Google Scholar]
- 91.Tokimasa S, Hara J, Osugi Y, Ohta H, Matsuda Y, Fujisaki H, Sawada A, Kim JY, Sashihara J, Amou K, et al. Ganciclovir is effective for prophylaxis and treatment of human herpesvirus-6 in allogeneic stem cell transplantation. Bone Marrow Transplant. 2002;29:595–598. doi: 10.1038/sj.bmt.1703423. [DOI] [PubMed] [Google Scholar]
- 92.Lautenschlager I, Lappalainen M, Linnavuori K, Suni J, Höckerstedt K. CMV infection is usually associated with concurrent HHV-6 and HHV-7 antigenemia in liver transplant patients. J Clin Virol. 2002;25 Suppl 2:S57–S61. doi: 10.1016/s1386-6532(02)00101-4. [DOI] [PubMed] [Google Scholar]


