Abstract
Esophageal strictures are a problem frequently encountered by gastroenterologists. Dilation has been the customary treatment for benign esophageal strictures, and dilation techniques have advanced over the years. Depending on their characteristics and the response to treatment, esophageal strictures can be classified into two types: 1, simple (Schatzki rings, webs, peptic injury, and following sclerotherapy) - these are easily amenable to dilation, with a low recurrence rate after initial treatment; and 2, complex (caused by caustic ingestion, radiation injury, anastomotic strictures, and photodynamic therapy) - these are difficult to dilate and are associated with higher recurrence rates. Refractory strictures are those in which it is not possible to relieve the anatomic restriction successfully up to a diameter of 14 mm over five sessions at 2-weekly intervals, due to cicatricial luminal compromise or fibrosis; and recurrent strictures are those in which it is not possible to maintain a satisfactory luminal diameter for 4 wk once the target diameter of 14 mm has been achieved. There are no standard recommendations for the management of refractory strictures. The various techniques used include intralesional steroid injection combined with dilation; endoscopic incisional therapy, with or without dilation; placement of self-expanding metal stents, Polyflex stents, or biodegradable stents; self-bougienage; and endoscopic surgery. This review discusses the indications, technique, results, and complications of the use of intralesional steroid injections combined with dilation and endoscopic incisional therapy with dilation in refractory strictures.
Keywords: Gastrointestinal strictures, Intralesional injection, Triamcinolone, Steroids, Dilation, Endoscopy
INTRODUCTION
Esophageal strictures are a problem frequently encountered by gastroenterologists. Strictures can be subdivided into those with malignant causes and those that are benign. Malignant esophageal strictures are usually due to carcinoma, and in these cases dilation is used only as a supplementary procedure in addition to stent placement, or in order to complete another procedure. Common benign causes include peptic injury, Schatzki rings, esophageal webs, radiation injury, caustic ingestion, and anastomotic strictures[1-3]. Dilation has been the customary treatment for benign esophageal strictures, and dilation techniques have developed from the use of whalebones (reported in the treatment of achalasia) and rigid bougienage in the seventeenth and eighteenth centuries to the present-day use of wire-guided, flexible, polyvinyl bougies (Savary-Gilliard; Wilson-Cook Medical Inc., Winston-Salem, North Carolina, USA) and through-the-scope balloon dilators.
Depending on their characteristics and on the response to treatment, esophageal strictures can be differentiated into two structural types - simple or complex[1]. Simple esophageal strictures are focal, straight, symmetrical, or concentric, with a diameter of > 12 mm (allowing easy passage of a diagnostic upper endoscope), and they are often amenable to treatment with standard techniques such as bougienage or balloon dilation. Common etiologies for simple strictures include Schatzki rings, webs, and peptic injury; they may also develop following sclerotherapy. In these strictures, only one to three dilation sessions are usually required in order to achieve symptomatic relief[1,2], but after initial treatment they may recur in up to 30%-40% of patients during the long-term follow-up[4].
Complex strictures are long (> 2 cm), tortuous, and asymmetrical and are associated with a severely compromised luminal diameter (< 12 mm)[1]. Common causes of benign complex strictures include caustic ingestion, radiation injury, anastomotic strictures, and photodynamic therapy. Some peptic strictures may also be complex in nature. Complex strictures are usually more difficult to treat, requiring some three to eight dilation sessions when conventional bougienage or balloon dilation techniques are used[1,2], and they are associated with higher recurrence rates[3]. In tortuous strictures, fluoroscopic guidance may be needed during dilation therapy[1]. Some complex strictures (e.g. after radiotherapy) may appear completely closed, without an identifiable lumen being visible on endoscopy or contrast esophagography.
REFRACTORY STRICTURES
There is no universally accepted definition for a refractory esophageal stricture, and the numbers of additional dilation sessions required before strictures are categorized as refractory vary in different series[5,6]. A refractory or recurrent stricture is defined as an anatomic restriction resulting from cicatricial luminal compromise or due to fibrosis leading to clinical symptoms of dysphagia in the absence of any endoscopic evidence of inflammation. This may occur either as a result of an inability to successfully resolve the anatomic problem up to a diameter of 14 mm over five sessions at 2-wk intervals (refractory stricture) or due to an inability to maintain a satisfactory luminal diameter for 4 wk once the target diameter of 14 mm has been achieved (recurrent stricture)[7]. There are no standard recommendations for the management of refractory strictures. Intralesional steroid injection combined with dilation[8-13], endoscopic incisional therapy with or without dilation[14-16], and placement of self-expanding metallic stents (SEMS)[17,18], Polyflex stents[19], or biodegradable stents[20], self-bougienage[21], and endoscopic surgery[22,23] have been used in the management of refractory strictures.
INTRALESIONAL STEROID THERAPY
Historical aspects
On the basis of successful injection treatment for dermatologic scars such as keloids and burn scars[24,25], intralesional injection of corticosteroids has been practiced in refractory esophageal strictures of various etiologies for the last 40 years. Although evidence of the effectiveness of corticosteroid injection in benign esophageal strictures was first reported by Ashcraft and Holder[26] in 1969 in an animal model, the technique was used only occasionally during the 1970s and 1980s, primarily with rigid endoscopes in patients under general anesthesia[10,27]. However, during the last decade there has been growing interest in the use of this form of therapy for refractory benign esophageal strictures[8,9,11-13,28,29].
Preparation
Preparation is as for esophageal dilation. Esophageal dilation is routinely performed in an outpatient setting. Patients should fast for 4-6 h before the procedure. Anticoagulant medication should be discontinued[30]. Routine antibiotic coverage is not recommended, and the guidelines for endocarditis prophylaxis should be followed[31]. During the informed consent process, patients should be informed about the risk of perforation and the possible need for surgery should it occur. Although some patients may tolerate dilation with topical anesthesia alone, conscious sedation is generally used[32].
Type and dose of steroids
Most investigators[8-13] have used triamcinolone acetate or acetonide 10 mg/mL, although some have used a concentration of 40 mg/mL[27,28]. The volume of corticosteroid used per injection has varied from 0.5 mL[28] to 2.8 mL[9]. We initially used 10 mg/mL triamcinolone acetate[12], but in a subsequent study we administered 40 mg/mL triamcinolone acetate to a total of 40-100 mg in each session[13]. Ramage et al[28], in a randomized study, standardized the dosage to 0.5 mL aliquots of 20 mg each of 40 mg/mL triamcinolone acetonide.
Ramboer et al[33] used a betamethasone preparation: one 1-mL vial containing 5 mg of betamethasone as a dipropionate suspension diluted into usually 5 mL and sometimes 10 mL of normal saline solution and injected as 0.5-1.0-mL aliquots. Miyashita et al[34] used a total of 8 mg dexamethasone (2 mL) injected endoscopically into four sites (2 mg/0.5 mL per site) at the anastomotic site immediately after dilation. Mendelson and Maloney[10] used hydrocortisone acetate in two of their patients.
There were no differences among the reported studies with regard to the response outcome after using different steroid formulations.
The number of injection sessions in the reported series varies from only one to as many sessions as the number of dilations. Kochhar et al[12,13] used a maximum of four sessions, whereas Rupp et al[35] carried out a maximum of five sessions and Gandhi et al[27] conducted as many as 13 sessions. The number of sessions is an issue that has not yet been settled and requires standardization.
The role of systemic steroids has been a matter of debate, especially in patients with caustic ingestion. In an interesting study, Morikawa et al[36] reported that two children, one with a caustic-induced stricture and the other with an anastomotic stricture, responded to high-dose intravenous methylprednisolone after they had failed to respond to intralesional steroids. However, the follow-up periods for these two patients were only 7 and 8 mo. The authors postulated that high-dose intravenous steroids might deliver the steroid to the stricture segment better than direct injection, as the wall of the stricture appeared to be too thick. They also expected that high-dose steroids given immediately after dilation would suppress the initial inflammation.
However, a meta-analysis of 10 studies[37] concluded that administration of systemic steroids in the management of corrosive ingestion does not prevent the development of strictures and may actually lead to the development of serious adverse effects. In 305 patients treated with corticosteroids, 35.1% developed strictures, whereas 33.3% of the 267 patients who were not treated with corticosteroids developed strictures.
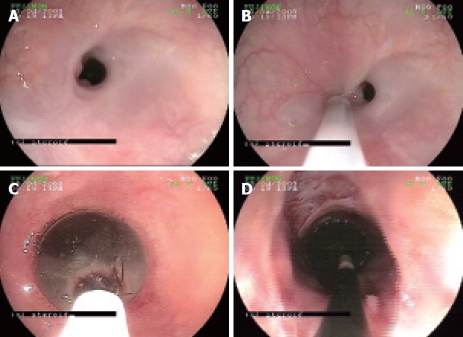
Procedure (Figure 1A-D)
Figure 1.
Endoscopic image of an esophageal stricture and its management. A: A refractory stricture; B: Steroid injection at the proximal edge of the stricture; C: Through-the-scope (TTS) balloon dilation of the stricture; D: The opened stricture after deflation of the TTS balloon.
Triamcinolone is injected intralesionally using a 23-gauge, 5-mm long sclerotherapy injection needle (3MK; Olympus Optical Co., Tokyo, Japan) in aliquots of 0.2-0.8 mL at 10-40 mg/mL, after premedication with intravenous hyoscine N-butylbromide. Injections are commonly given into four quadrants; a total of four to six injections are made at the proximal edge of the stricture and another four to six injections into the strictured segment proper whenever possible. Injections should be given just before dilation whenever possible. In long strictures, injections are first made at the entrance to the stricture, and as the stricture opens they are placed in more distal locations[14]. Kochhar et al[12] suggest that patients with proximal strictures and long strictures should undergo dilation first, followed 2 h later by injections so that the whole length of the stricture can be injected.
Although injections can be made satisfactorily under endoscopic guidance, failures have been noted. Improper localization of the injection has been cited as a probable cause[13]. Bhutani et al[29] have therefore suggested that an endoscopic ultrasound miniprobe should be used to guide the injection into the thickest portion of the esophageal stricture for better results. In their study, one patient with a stricture 4 cm long responded well to steroid injection under ultrasound miniprobe guidance (for 6 mo) after only partially responding (for 12 wk) to steroid injection without ultrasound guidance.
The injection can be repeated if there is no subjective improvement in the dysphagia score or a rapid recurrence of dysphagia is seen. There is no consensus regarding the number of injections to be administered. After each dilation, patients should remain under observation for at least 4 h. After a luminal diameter of 15 mm has been reached, a contrast study may be repeated for documentation (Figure 2).
Figure 2.
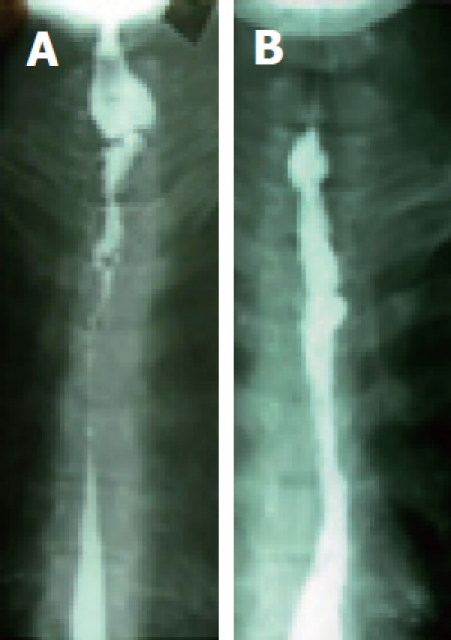
Barium swallow image of a stricture. A: A complex resistant esophageal stricture; B: The opened stricture after intralesional steroid injection and balloon dilation.
Mechanism of action
The exact mechanism by which intralesional steroids enhance the efficacy of dilation is not clear. Intralesional steroid injections have been shown to inhibit stricture formation by interfering with collagen synthesis, fibrosis, and chronic scarring processes[38]. Triamcinolone inhibits the transcription of matrix protein genes, including fibronectin and procollagen. It also reduces the synthesis of α2-macroglobulin, an inhibitor of collagenase activity[24]. It has also been suggested that triamcinolone prevents the cross-linking of collagen that results in scar contracture, so that if the scar is stretched and corticosteroid is injected into it, contracture will presumably not occur[10]. Corticosteroids also decrease the fibrotic healing that appears to occur after dilation[38]. Gandhi et al[27] observed that with corticosteroid injections and dilations, longer corrosive strictures became shorter with time and thus more amenable to nonsurgical treatment.
Assessment of efficacy
In one of the earliest studies, the efficacy of intralesional steroids was tested in an animal model. In canine models of lye-induced esophageal strictures, Ashcraft and Holder[38] and our own group[12,13] confirmed the efficacy of this form of therapy in conjunction with dilation treatment.
The efficacy of steroid injections in humans has traditionally been assessed by studying the need for dilations, the time to dilations, and the number of additional dilations. A periodic dilation index (PDI), calculated as the number of dilations required/duration of time in months, has frequently been used to demonstrate efficacy[12,13].
ESOPHAGEAL STRICTURES
Peptic strictures
As many as 60%-70% of benign esophageal strictures are peptic in origin and result from acid-induced mucosal damage[39]. These patients routinely undergo stricture dilation. However, nearly half of them require subsequent dilation within 1 year, and two-thirds of those requiring repeat dilation within the first year require additional subsequent dilations[40]. Although proton-pump inhibitors may reduce the rate of recurrent stricture formation, a significant proportion of patients require repeated periodic dilation[28]. It is in this group of patients that intralesional steroids have been shown to be useful in reducing the need for repeated dilations. Most of the literature reports on the use of intralesional steroids refer to patients with peptic strictures. Kirsch et al[11] were among the first to demonstrate the usefulness of this form of treatment using fiberoptic endoscopes. They showed a dramatic improvement in two patients with resistant peptic strictures. Lee et al[9] used this therapy in a total of 31 patients, 12 of whom had peptic strictures. All of them showed a reduced need for dilation and an increase in the interval between dilations. Kochhar et al[12] devised an objective parameter for evaluating the response to intralesional steroids, terming the number of dilations required per month the PDI. They studied 14 patients with peptic strictures who required repeated dilation and were given intralesional triamcinolone acetonide (40 mg/mL, dilute 1:1) in aliquots of 0.5 mL in four quadrants around the stricture. The periodic dilation index (number of dilations per month) fell significantly from 0.92 ± 0.44 to 0.42 ± 0.2 over a postdilatation period of 3-12 mo. This was also associated with a significant (P < 0.001) improvement in the dysphagia score (0.28 ± 0.46 vs 1.85 ± 0.36).
Two randomized trials have confirmed the utility of this form of therapy. Altintas et al[41] randomly assigned 21 patients with esophageal strictures who were undergoing bougie dilation either to an intralesional steroid injection group or to a control group. There were six patients with peptic strictures in the study group and four in the control group. The authors injected triamcinolone acetate (40 mg/mL) diluted with 4 mL of saline in four aliquots into the proximal segment of the stricture. The periodic dilation index declined from 0.71 to 0.28 in the study group, which also had a longer symptom-free interval than the control group. Ramage et al[28], in a study including 30 patients with peptic strictures who required repeated dilations, randomly assigned the patients to an intralesional triamcinolone group (40 mg/mL; 0.5 mL in each quadrant) and a sham injection group. During a follow-up period of 1 year, two patients (13%) in the study group and nine patients (60%) in the control group required repeat dilation. Two patients in each group required fundoplication. In another randomized study, published only as an abstract, Rupp et al[35] randomly assigned 43 patients with peptic strictures to an intralesional steroid group and a control group. The PDI was 0.07 in the steroid group in comparison with 0.253 in the control group over 10-13 mo after steroid therapy. Kochhar and Makharia[13] repeated intralesional steroid injections in each session of dilation, with a limit of four injections. Ramage et al[28] and Altintas et al[41] gave steroid injections only once. In all of the studies, steroid injections were combined with bougienage or balloon dilation and all of the patients received proton-pump inhibitors.
Caustic strictures
Caustic-induced strictures are often multiple, tortuous, and more difficult to treat[16]. They are reported to require larger numbers of dilations in comparison with peptic strictures[42]. Most of the early reports on intralesional steroid treatment concerned difficult strictures following caustic ingestion. Mendelson and Maloney[10], using rigid endoscopes, administered two different steroid injections (hydrocortisone and triamcinolone) in five patients with caustic-induced esophageal strictures, with good results in four of the patients. In one patient, they used a hyaluronidase injection along with hydrocortisone acetate. In another study, Gandhi et al[27] carried out 2-13 sessions of intralesional steroid treatment in six infants and children (aged 4 mo-5 years) with caustic-induced strictures and reported a good response in all cases, with 4-11 years of follow-up. Kochhar et al[12] used triamcinolone acetonide (10 mg/mL) in 17 patients with caustic-induced esophageal strictures, 14 of whom had already had repeated dilations, while the other three had not yet undergone dilation. Eleven of the strictures were 3-6 cm long. The periodic dilation index in 14 patients who had previously been receiving dilation treatment declined from 1.67 to 0.32. The mean number of dilations in these patients was 27.9 over a 22-mo period before steroid injections and 3.57 over a period of 10.5 mo after steroid injections. Significantly, three patients did not require any further dilation after the steroid injections. In another study, Kochhar and Makharia[13] reported the use of steroids in 29 patients with caustic-induced esophageal strictures. The periodic dilation index declined from 1.37 (0.5-3.16) before injections to 0.53 (0.1-1.33) after injections. These data confirm the benefit of steroid injections in patients with caustic-induced esophageal strictures, which was also associated with a significant (P < 0.001) improvement in the dysphagia score. There has been one randomized trial comparing triamcinolone injection with saline injection in 14 patients. A larger luminal diameter was achieved in he patients in the steroid group in comparison with those in the control group[43].
Anastomotic strictures
In a study by Catalano et al[44], seven of 15 patients with anastomotic strictures following resection of esophageal carcinoma received triamcinolone injections at the anastomotic site (four quadrants); these patients were classified as having refractory cases following the initial dilation. The symptoms resolved in all of the patients following complete serial dilation. They were all placed on high-dose proton-pump inhibitor treatment following the initial endoscopic dilation. Three stricture recurrences occurred at 2, 4, and 9 mo and were treated successfully by repeat dilation with the use of intralesional steroids. No complications were encountered during therapy. In another study on anastomotic esophageal strictures, Catalano et al[45] found that patients who received steroid injections (triamcinolone 40 mg) along with balloon dilation required fewer dilation sessions (mean 2.7 vs 4.4) and had fewer recurrences (0 vs 2) in comparison with those who received balloon dilation alone. Miyashita et al[34] used injections of dexamethasone (8 mg) around the anastomotic site immediately after balloon dilation in 11 patients with anastomotic strictures following esophagogastrostomy. Endoscopic steroid injection immediately after balloon dilation enhanced the effect of the procedure and significantly reduced the number of treatments needed. Kochhar and Makharia[13] used steroid injections in 19 anastomotic strictures following transhiatal esophagectomy and observed a decline in the periodic dilation index from 1.24 (0.13-2.0) before steroid injections to 0.51 (0-2) after injection therapy. There was a significant increase in the maximum dilation diameter achieved after injection therapy. This was also associated with a significant (P < 0.001) improvement in the dysphagia score (0.63 ± 0.59 vs 2.42 ± 0.5).
Radiation strictures
Radiation-induced strictures are often difficult to treat, due to intense fibrosis. In a study including six patients with radiation stricture, Lee et al[9] injected 28 mg of triamcinolone in each session. The study by Kochhar and Makharia[13] included nine patients with radiation-induced esophageal strictures. The periodic dilation index decreased significantly from 1.32 (0-2) to 0.6 (0-1) (P < 0.02) following use of intralesional triamcinolone injections. This was also associated with a significant (P < 0.001) improvement in the dysphagia score (1.22 ± 0.44 vs 2.44 ± 0.52). Other researchers have also used steroid injections in the treatment of small numbers of patients with radiation-induced strictures[8,41].
Other etiologies
Various reports have included a few patients with strictures of other etiologies who have undergone intralesional steroid treatment. Lee et al[9] described one patient with a sclerotherapy-induced stricture and one with pill-induced esophagitis in their series. Gandhi et al[27] used steroid injections to treat five patients with esophageal atresia, with a good response.
PYLORIC STENOSIS
There have only been a few reports on the use of intralesional steroids in the treatment of pyloric stenosis. Lee et al[9] treated two such patients with injections of 10 mg/mL triamcinolone in two patients, in one case with a peptic etiology and in the other following pyloroplasty. Subsequently, Kochhar et al[46] treated three patients with caustic-induced pyloric stenosis, in two of whom balloon dilation had previously failed. They administered one session of steroid injection each in two patients, while two sessions were given in one patient. All three patients remained well during a follow-up period of up to 3 years and 3 mo.
BILIARY STRICTURES
In a pilot study of eight benign biliary strictures (postoperative, n = 6; primary sclerosing cholangitis, n = 2), Wehrmann et al[47] injected 2 × 10 mg of triamcinolone into the wall of the common bile duct (CBD) at the stricture site using a sclerotherapy needle, along with dilation and placement of a 10-Fr stent. The initial mean diameter of the CBD stenoses was 1.81 mm. The mean serum levels of alkaline phosphatase and bilirubin were 455 U/L and 4.9 mg/dL, respectively. No significant improvement was observed after the initial balloon dilation and stent insertion. However, after local triamcinolone injection and a second dilation and stent insertion, the diameter of the CBD stenosis increased significantly to 3.68 mm (P < 0.01). No adverse affects were noted. Three patients had complete recovery from the CBD stenosis after a third dilation; the remaining five patients were cured after two or three additional balloon dilations with intermittent stent exchanges. Thereafter, no recurrent CBD stenoses were observed during a median follow-up of 12 mo. At the conclusion of the study, the mean serum alkaline phosphatase and bilirubin levels were 195 U/L and 1.2 mg/dL, respectively.
STRICTURES IN CROHN’S DISEASE
Although resection of stenotic or perforated intestinal segments in Crohn’s disease is often unavoidable, surgical remission is only temporary. New lesions are found on endoscopy in more than 70% of patients within a year and 40% become symptomatic within 4 years[48]. Uncontrolled transformation of resident mesenchymal cells into matrix-depositing myofibroblasts is the most likely cause of fibrosis in Crohn’s disease[49], but the underlying molecular mechanisms have not yet been fully explained. As repeated bowel resections may lead to short bowel syndrome, the quest for bowel-conserving strategies during the last 25 years led to the development of both endoscopic and surgical strictureplasty in clinical practice.
Successful endoscopic dilation of anastomotic or intrinsic strictures in patients with Crohn’s disease, using through-the-scope rigid balloons, was first reported in 1981. This procedure is indicated for relatively short (maximum 5 cm), symptomatic, and isolated strictures within the reach of the endoscope in the upper and lower gastrointestinal tract. The immediate success rates vary between 71% and 100%, with symptom recurrence in 13%-100% of patients[33,50-54]. Because of suboptimal long-term outcomes with endoscopic balloon dilation, adjuvant techniques such as intralesional steroid injection have been studied.
In a pilot study of intrastricture steroid injection versus placebo injection after balloon dilation of Crohn’s strictures, East et al[55] noted that a single treatment with intrastricture triamcinolone injection did not reduce the time to redilation after balloon dilation of Crohn’s ileocolonic anastomotic strictures, and there was a trend toward a poorer outcome.
However, Ramboer et al[33] reported a 100% immediate success rate in 13 patients with endoscopic dilation and intramural injection of corticosteroids after the procedure. During a follow-up of 9-73 mo, three patients remained asymptomatic, three required one additional session, and the rest required four or more sessions of dilation with steroid injection. Two operations were carried out during this period, but they were not related to the treated segment itself.
More recently, Singh et al[56] have reported 29 stricture dilations in 17 patients with Crohn’s disease (10 female, seven male) with 20 strictures. Five of the strictures were located in the rectum, two in the sigmoid colon, three at colo-colonic anastomoses, four at ileocolonic anastomoses, one in the ileum, one in the descending colon, one in the cecum, and three in the distal duodenal bulb. The mean follow-up period was 18.8 mo (range 5-50 mo). Technical success was achieved in 28 of the 29 stricture dilations (96.5%). Four-quadrant steroid injections were carried out in 11 strictures. The recurrence rate in this group was 10% and that in the nonsteroid group was 31.3%. Three perforations occurred (all colonic) during the 29 stricture dilations - a complication rate of 10%, with no mortalities.
Lavy[57] described the treatment of 10 patients with colonic strictures attributable to Crohn’s disease who were treated with dilation and injection of triamcinolone. Five of the patients had postoperative strictures. Two patients required additional dilation and injection of steroids after 1 year, while eight patients remained well over a follow up period of 1.5-3 years.
In a retrospective study by Brooker et al[58], 14 patients with Crohn-related strictures underwent a total of 26 dilations, with triamcinolone being injected (median dose 20 mg, range 10-40 mg) in 20 of the procedures. Seven patients (50%) had sustained remission after a single dilation and steroid injection, with a median follow-up period of 16.4 mo (range 13.2-22.0 mo). Four patients (28.5%) required more than one dilation (median three dilations, range two to four) to control their symptoms, with a median follow-up period of 27.8 mo (range 14-32.8 mo). Endoscopic management failed in three patients (21.4%), who were referred for surgery. There were no complications due to dilation or triamcinolone injection.
Recently, Swaminath and Lichtiger[59] have described dilation of a colonic stricture along with injection of infliximab into the distal and medial portions of the strictures in three patients refractory to all medical therapy, including systemic infliximab. Infliximab was effective in treating the strictures in all three patients.
USE IN PEDIATRIC PATIENTS
The safety of intralesional steroids has been documented in a number of studies in pediatric patients, including infants. Zein et al[8] described intralesional steroid injection treatment in seven boys ranging in age from 1-14 years. Three patients had strictures secondary to gastroesophageal reflux; one had a stricture as a complication of radiation therapy to the mediastinum for treatment of lymphoma; one had a stricture at the site of a surgical anastomosis after repair of an esophageal fistula; one had a stricture that developed after lye ingestion; and one was later found at surgery to have a tracheobronchial remnant. Each patient underwent two sessions of intralesional steroid injections, 3-20 d apart, with a 10-mg/mL solution of triamcinolone acetonide. An average of four injections per session were given circumferentially, using 0.2 mL of triamcinolone at each site, before balloon dilation. Only two of the seven patients did not show improvement with the steroid injections; one later had a tracheobronchial remnant diagnosed after a limited esophageal resection, and the other, in whom the stricture was related to lye ingestion, required partial esophagectomy to relieve the symptoms. Similar beneficial effects in pediatric esophageal strictures have been observed by Mendelson and Maloney[10] and Gandhi et al[27].
COMPLICATIONS
There is a theoretical risk that intramural infection might be induced with this form of therapy. Some esophageal strictures are known to be associated with intramural pseudodiverticula, which has been causally linked to Candida albicans[26]. Zein et al[8] observed Candida albicans esophagitis at the site of injection in one patient, and a suspected yeast esophagitis in another. Both were easily treated with an oral antifungal medication. Theoretically, there is a potential for esophageal perforation and mediastinitis or pleural effusion. The only reported esophageal perforation occurred in a series of patients in whom a rigid endoscope was used[10]. Lilly and Bensard[60] reported a significant delay in linear growth in a young boy who had been intermittently treated with intralesional steroids for esophageal stricture between the ages of 5 mo and 2 years. Growth returned to normal after steroid injections were stopped.
CONCLUSION
It has been demonstrated that intralesional steroid injections augment the effect of endoscopic dilation in strictures of varied etiologies and at various sites. As has been recommended in an editorial, intralesional steroid injection therapy should be considered in patients with refractory strictures, especially complex strictures[61]. Triamcinolone acetate/acetonide is the most widely used steroid. The dosage that has been shown to be most effective is 20 mg in each quadrant, to a total of 80 mg. The triamcinolone suspension may need to be diluted for easier injection. The number of sessions of steroid injections that can be carried out has still not yet been determined. Endoscopic ultrasonography may be helpful to improve the targeting of injections.
Footnotes
Peer reviewer: Naoki Muguruma, MD, PhD, Department of Gastroenterology and Oncology, The University of Tokushima Graduate School, 3-18-15, Kuramoto-cho, Tokushima 770-8503, Japan
S- Editor Zhang HN L- Editor Robertson M E- Editor Ma WH
References
- 1.Lew RJ, Kochman ML. A review of endoscopic methods of esophageal dilation. J Clin Gastroenterol. 2002;35:117–126. doi: 10.1097/00004836-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Pereira-Lima JC, Ramires RP, Zamin I Jr, Cassal AP, Marroni CA, Mattos AA. Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol. 1999;94:1497–1501. doi: 10.1111/j.1572-0241.1999.01061.x. [DOI] [PubMed] [Google Scholar]
- 3.Said A, Brust DJ, Gaumnitz EA, Reichelderfer M. Predictors of early recurrence of benign esophageal strictures. Am J Gastroenterol. 2003;98:1252–1256. doi: 10.1111/j.1572-0241.2003.07490.x. [DOI] [PubMed] [Google Scholar]
- 4.Spechler SJ. American gastroenterological association medical position statement on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterology. 1999;117:229–233. doi: 10.1016/s0016-5085(99)70572-x. [DOI] [PubMed] [Google Scholar]
- 5.Hordijk ML, Siersema PD, Tilanus HW, Kuipers EJ. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006;63:157–163. doi: 10.1016/j.gie.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Repici A, Conio M, De Angelis C, Battaglia E, Musso A, Pellicano R, Goss M, Venezia G, Rizzetto M, Saracco G. Temporary placement of an expandable polyester silicone-covered stent for treatment of refractory benign esophageal strictures. Gastrointest Endosc. 2004;60:513–519. doi: 10.1016/s0016-5107(04)01882-6. [DOI] [PubMed] [Google Scholar]
- 7.Kochman ML, McClave SA, Boyce HW. The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc. 2005;62:474–475. doi: 10.1016/j.gie.2005.04.050. [DOI] [PubMed] [Google Scholar]
- 8.Zein NN, Greseth JM, Perrault J. Endoscopic intralesional steroid injections in the management of refractory esophageal strictures. Gastrointest Endosc. 1995;41:596–598. doi: 10.1016/s0016-5107(95)70198-2. [DOI] [PubMed] [Google Scholar]
- 9.Lee M, Kubik CM, Polhamus CD, Brady CE 3rd, Kadakia SC. Preliminary experience with endoscopic intralesional steroid injection therapy for refractory upper gastrointestinal strictures. Gastrointest Endosc. 1995;41:598–601. doi: 10.1016/s0016-5107(95)70199-0. [DOI] [PubMed] [Google Scholar]
- 10.Mendelsohn HJ, Maloney WH. The treatment of benign strictures of the esophagus with cortisone injection. Ann Otol Rhinol Laryngol. 1970;79:900–904. doi: 10.1177/000348947007900504. [DOI] [PubMed] [Google Scholar]
- 11.Kirsch M, Blue M, Desai RK, Sivak MV Jr. Intralesional steroid injections for peptic esophageal strictures. Gastrointest Endosc. 1991;37:180–182. doi: 10.1016/s0016-5107(91)70681-0. [DOI] [PubMed] [Google Scholar]
- 12.Kochhar R, Ray JD, Sriram PV, Kumar S, Singh K. Intralesional steroids augment the effects of endoscopic dilation in corrosive esophageal strictures. Gastrointest Endosc. 1999;49:509–513. doi: 10.1016/s0016-5107(99)70052-0. [DOI] [PubMed] [Google Scholar]
- 13.Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc. 2002;56:829–834. doi: 10.1067/mge.2002.129871. [DOI] [PubMed] [Google Scholar]
- 14.DiSario JA, Pedersen PJ, Bichiş-Canoutas C, Alder SC, Fang JC. Incision of recurrent distal esophageal (Schatzki) ring after dilation. Gastrointest Endosc. 2002;56:244–248. doi: 10.1016/s0016-5107(02)70185-5. [DOI] [PubMed] [Google Scholar]
- 15.Brandimarte G, Tursi A. Endoscopic treatment of benign anastomotic esophageal stenosis with electrocautery. Endoscopy. 2002;34:399–401. doi: 10.1055/s-2002-25293. [DOI] [PubMed] [Google Scholar]
- 16.Hagiwara A, Togawa T, Yamasaki J, Shirasu M, Sakakura C, Yamagishi H. Endoscopic incision and balloon dilatation for cicatricial anastomotic strictures. Hepatogastroenterology. 1999;46:997–999. [PubMed] [Google Scholar]
- 17.Fiorini A, Fleischer D, Valero J, Israeli E, Wengrower D, Goldin E. Self-expandable metal coil stents in the treatment of benign esophageal strictures refractory to conventional therapy: a case series. Gastrointest Endosc. 2000;52:259–262. doi: 10.1067/mge.2000.107709. [DOI] [PubMed] [Google Scholar]
- 18.Song HY, Jung HY, Park SI, Kim SB, Lee DH, Kang SG, Il Min Y. Covered retrievable expandable nitinol stents in patients with benign esophageal strictures: initial experience. Radiology. 2000;217:551–7. doi: 10.1148/radiology.217.2.r00nv03551. [DOI] [PubMed] [Google Scholar]
- 19.Radecke K, Gerken G, Treichel U. Impact of a self-expanding, plastic esophageal stent on various esophageal stenoses, fistulas, and leakages: a single-center experience in 39 patients. Gastrointest Endosc. 2005;61:812–818. doi: 10.1016/s0016-5107(05)00290-7. [DOI] [PubMed] [Google Scholar]
- 20.Fry SW, Fleischer DE. Management of a refractory benign esophageal stricture with a new biodegradable stent. Gastrointest Endosc. 1997;45:179–182. doi: 10.1016/s0016-5107(97)70244-x. [DOI] [PubMed] [Google Scholar]
- 21.Kim CH, Groskreutz JL, Gehrking SJ. Recurrent benign esophageal strictures treated with self-bougienage: report of seven cases. Mayo Clin Proc. 1990;65:799–803. doi: 10.1016/s0025-6196(12)62569-5. [DOI] [PubMed] [Google Scholar]
- 22.Lucktong TA, Morton JM, Shaheen NJ, Farrell TM. Resection of benign esophageal stricture through a minimally invasive endoscopic and transgastric approach. Am Surg. 2002;68:720–723. [PubMed] [Google Scholar]
- 23.Beilstein MC, Kochman ML. Endoscopic incision of a refractory esophageal stricture: novel management with an endoscopic scissors. Gastrointest Endosc. 2005;61:623–625. doi: 10.1016/s0016-5107(04)02787-7. [DOI] [PubMed] [Google Scholar]
- 24.Ketchum LD, Smith J, Robinson DW, Masters FW. The treatment of hypertrophic scar, keloid and scar contracture by triamcinolone acetonide. Plast Reconstr Surg. 1966;38:209–218. doi: 10.1097/00006534-196609000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Kiil J. Keloids treated with topical injections of triamcinolone acetonide (kenalog). Immediate and long-term results. Scand J Plast Reconstr Surg. 1977;11:169–172. doi: 10.3109/02844317709025514. [DOI] [PubMed] [Google Scholar]
- 26.Sabanathan S, Salama FD, Morgan WE. Oesophageal intramural pseudodiverticulosis. Thorax. 1985;40:849–857. doi: 10.1136/thx.40.11.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gandhi RP, Cooper A, Barlow BA. Successful management of esophageal strictures without resection or replacement. J Pediatr Surg. 1989;24:745–749; discussion 749-750. doi: 10.1016/s0022-3468(89)80529-9. [DOI] [PubMed] [Google Scholar]
- 28.Ramage JI Jr, Rumalla A, Baron TH, Pochron NL, Zinsmeister AR, Murray JA, Norton ID, Diehl N, Romero Y. A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol. 2005;100:2419–2425. doi: 10.1111/j.1572-0241.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 29.Bhutani MS, Usman N, Shenoy V, Qarqash A, Singh A, Barde CJ, Gopalswamy N. Endoscopic ultrasound miniprobe-guided steroid injection for treatment of refractory esophageal strictures. Endoscopy. 1997;29:757–759. doi: 10.1055/s-2007-1004304. [DOI] [PubMed] [Google Scholar]
- 30.Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, et al. Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures. Gastrointest Endosc. 2002;55:775–779. doi: 10.1016/s0016-5107(02)70402-1. [DOI] [PubMed] [Google Scholar]
- 31.Hirota WK, Petersen K, Baron TH, Goldstein JL, Jacobson BC, Leighton JA, Mallery JS, Waring JP, Fanelli RD, Wheeler-Harbough J, et al. Guidelines for antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2003;58:475–482. doi: 10.1067/s0016-5107(03)01883-2. [DOI] [PubMed] [Google Scholar]
- 32.Petrini J, Egan JV. Risk management regarding sedation/analgesia. Gastrointest Endosc Clin N Am. 2004;14:401–414. doi: 10.1016/j.giec.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 33.Ramboer C, Verhamme M, Dhondt E, Huys S, Van Eygen K, Vermeire L. Endoscopic treatment of stenosis in recurrent Crohn’s disease with balloon dilation combined with local corticosteroid injection. Gastrointest Endosc. 1995;42:252–255. doi: 10.1016/s0016-5107(95)70101-x. [DOI] [PubMed] [Google Scholar]
- 34.Miyashita M, Onda M, Okawa K, Matsutani T, Yoshiyuki T, Sasajima K, Kyono S, Yamashita K. Endoscopic dexamethasone injection following balloon dilatation of anastomotic stricture after esophagogastrostomy. Am J Surg. 1997;174:442–444. doi: 10.1016/s0002-9610(97)00116-5. [DOI] [PubMed] [Google Scholar]
- 35.Rupp T, Earle D, Ikenberry S, Lumeng L, Lehman G. Randomized trial of Savary dilation with/without intralesional steroids for benign gastroesophageal reflux strictures [abstract] Gastrointest Endosc. 1995;41:357. [Google Scholar]
- 36.Morikawa N, Honna T, Kuroda T, Watanabe K, Tanaka H, Takayasu H, Fujino A, Tanemura H, Matsukubo M. High dose intravenous methylprednisolone resolves esophageal stricture resistant to balloon dilatation with intralesional injection of dexamethasone. Pediatr Surg Int. 2008;24:1161–1164. doi: 10.1007/s00383-008-2224-7. [DOI] [PubMed] [Google Scholar]
- 37.Pelclová D, Navrátil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev. 2005;24:125–129. doi: 10.2165/00139709-200524020-00006. [DOI] [PubMed] [Google Scholar]
- 38.Ashcraft KW, Holder TM. The expeimental treatment of esophageal strictures by intralesional steroid injections. J Thorac Cardiovasc Surg. 1969;58:685–691 passim. [PubMed] [Google Scholar]
- 39.Spechler SJ. AGA technical review on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterology. 1999;117:233–254. doi: 10.1016/s0016-5085(99)70573-1. [DOI] [PubMed] [Google Scholar]
- 40.Patterson DJ, Graham DY, Smith JL, Schwartz JT, Alpert E, Lanza FL, Cain GD. Natural history of benign esophageal stricture treated by dilatation. Gastroenterology. 1983;85:346–350. [PubMed] [Google Scholar]
- 41.Altintas E, Kacar S, Tunc B, Sezgin O, Parlak E, Altiparmak E, Saritas U, Sahin B. Intralesional steroid injection in benign esophageal strictures resistant to bougie dilation. J Gastroenterol Hepatol. 2004;19:1388–1391. doi: 10.1111/j.1440-1746.2004.03491.x. [DOI] [PubMed] [Google Scholar]
- 42.Broor SL, Kumar A, Chari ST, Singal A, Misra SP, Kumar N, Sarin SK, Vij JC. Corrosive oesophageal strictures following acid ingestion: clinical profile and results of endoscopic dilatation. J Gastroenterol Hepatol. 1989;4:55–61. doi: 10.1111/j.1440-1746.1989.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 43.Camargo MA, Lopes LR, Grangeia Tde A, Andreollo NA, Brandalise NA. [Use of corticosteroids after esophageal dilations on patients with corrosive stenosis: prospective, randomized and double-blind study] Rev Assoc Med Bras. 2003;49:286–292. doi: 10.1590/s0104-42302003000300033. [DOI] [PubMed] [Google Scholar]
- 44.Catalano MF, George S, Thomas M, Geenen JE. Endoscopic treatment of anastomotic strictures following resection of esophageal carcinoma: Increased success using submucosal corticosteroid injection (Abstract W1501) Gastrointest Endosc. 2004;59:P241. [Google Scholar]
- 45.Catalano MF, Kaul V, Pezanoski J, Guda N, Geenen JE. Endoscopic treatment of anastomotic strictures following resection of esophageal carcinoma (Abstract S1305) Gastrointest Endosc. 2007;65:AB139. [Google Scholar]
- 46.Kochhar R, Dutta U, Sethy PK, Singh G, Sinha SK, Nagi B, Wig JD, Singh K. Endoscopic balloon dilation in caustic-induced chronic gastric outlet obstruction. Gastrointest Endosc. 2009;69:800–805. doi: 10.1016/j.gie.2008.05.056. [DOI] [PubMed] [Google Scholar]
- 47.Wehrmann T, Schmitt T, Caspary WF, Seifert H. [Local injection of depot corticosteroids in endoscopic therapy of benign bile duct strictures] Z Gastroenterol. 2000;38:235–241. doi: 10.1055/s-2000-14863. [DOI] [PubMed] [Google Scholar]
- 48.Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99:956–963. doi: 10.1016/0016-5085(90)90613-6. [DOI] [PubMed] [Google Scholar]
- 49.Pucilowska JB, Williams KL, Lund PK. Fibrogenesis. IV. Fibrosis and inflammatory bowel disease: cellular mediators and animal models. Am J Physiol Gastrointest Liver Physiol. 2000;279:G653–G659. doi: 10.1152/ajpgi.2000.279.4.G653. [DOI] [PubMed] [Google Scholar]
- 50.Blomberg B, Rolny P, Järnerot G. Endoscopic treatment of anastomotic strictures in Crohn’s disease. Endoscopy. 1991;23:195–198. doi: 10.1055/s-2007-1010654. [DOI] [PubMed] [Google Scholar]
- 51.Couckuyt H, Gevers AM, Coremans G, Hiele M, Rutgeerts P. Efficacy and safety of hydrostatic balloon dilatation of ileocolonic Crohn’s strictures: a prospective longterm analysis. Gut. 1995;36:577–580. doi: 10.1136/gut.36.4.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dear KL, Hunter JO. Colonoscopic hydrostatic balloon dilatation of Crohn’s strictures. J Clin Gastroenterol. 2001;33:315–318. doi: 10.1097/00004836-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Junge U, Züchner H. [Endoscopic balloon dilatation of symptomatic strictures in Crohn‘s disease] Dtsch Med Wochenschr. 1994;119:1377–1382. doi: 10.1055/s-2008-1058848. [DOI] [PubMed] [Google Scholar]
- 54.Thomas-Gibson S, Brooker JC, Hayward CM, Shah SG, Williams CB, Saunders BP. Colonoscopic balloon dilation of Crohn’s strictures: a review of long-term outcomes. Eur J Gastroenterol Hepatol. 2003;15:485–488. doi: 10.1097/01.meg.0000059110.41030.bc. [DOI] [PubMed] [Google Scholar]
- 55.East JE, Brooker JC, Rutter MD, Saunders BP. A pilot study of intrastricture steroid versus placebo injection after balloon dilatation of Crohn’s strictures. Clin Gastroenterol Hepatol. 2007;5:1065–1069. doi: 10.1016/j.cgh.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 56.Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn’s disease strictures. J Clin Gastroenterol. 2005;39:284–290. doi: 10.1097/01.mcg.0000155128.31208.44. [DOI] [PubMed] [Google Scholar]
- 57.Lavy A. Triamcinolone improves outcome in Crohn’s disease strictures. Dis Colon Rectum. 1997;40:184–186. doi: 10.1007/BF02054985. [DOI] [PubMed] [Google Scholar]
- 58.Brooker JC, Beckett CG, Saunders BP, Benson MJ. Long-acting steroid injection after endoscopic dilation of anastomotic Crohn’s strictures may improve the outcome: a retrospective case series. Endoscopy. 2003;35:333–337. doi: 10.1055/s-2003-38145. [DOI] [PubMed] [Google Scholar]
- 59.Swaminath A, Lichtiger S. Dilation of colonic strictures by intralesional injection of infliximab in patients with Crohn’s colitis. Inflamm Bowel Dis. 2008;14:213–216. doi: 10.1002/ibd.20318. [DOI] [PubMed] [Google Scholar]
- 60.Lilly JR, Bensard D. Intralesional steroid injection in the management of esophageal stricture. J Pediatr Surg. 1989;24:1312. doi: 10.1016/s0022-3468(89)80576-7. [DOI] [PubMed] [Google Scholar]
- 61.Shah JN. Benign refractory esophageal strictures: widening the endoscopist’s role. Gastrointest Endosc. 2006;63:164–167. doi: 10.1016/j.gie.2005.08.033. [DOI] [PubMed] [Google Scholar]