Abstract
Malignancies of the gallbladder, including neuroendocrine tumors, are uncommon, mostly found incidentally after cholecystectomy and are frequently asymptomatic in the early stages, but highly fatal. Limited data is available on adrenocorticotropic hormone (ACTH)-producing neuroendocrine tumors specifically originating from the gallbladder. We report the clinical and radiographic findings, which included positron emission tomography and computed tomography, of a patient with a gallbladder mass who presented with Cushing’s syndrome. Subsequently, a diagnosis of ACTH-producing large cell neuroendocrine carcinoma of the gallbladder was made. Despite being rare and having a poor prognosis, hormone-producing neuroendocrine tumors should be part of the differential diagnosis in the approach of patients with Cushing’s syndrome.
Keywords: Adrenocorticotropic hormone, Cushing’s syndrome, Neuroendocrine, Carcinoma, Gallbladder
INTRODUCTION
Malignant carcinoma of the gallbladder is the fifth most common malignancy of the gastrointestinal tract, with an incidence of approximately 1.2 cases per 100 000 of the population per year in the United States. Histologically, 70% to 90% of cases are adenocarcinomas. Neuroendocrine tumors can also arise de novo in the gallbladder, as they can in every organ[1,2]. However, they are rare, representing only 0.5% of all gallbladder tumors[3] and 0.2% of all gastrointestinal carcinoids[4].
We report a case of an adrenocorticotropic hormone (ACTH)-producing gallbladder neuroendocrine tumor. We have also undertaken a comprehensive search for published cases of neuroendocrine tumors of the gallbladder, with special emphasis of ACTH-production, and present the results.
CASE REPORT
A 65 year old Filipino woman with past medical history of hypertension, hyperlipidemia, and diabetes mellitus presented to the hospital with three months progressive generalized weakness and anorexia. On physical examination, she displayed proximal muscle weakness, hirsutism, a moon face and a buffalo hump. She was admitted to the medical intensive care unit for severe hypokalemia of 1.8 mmol/L with U-waves on electrocardiogram.
The clinical signs, history of hypertension and diabetes mellitus, and the laboratory finding of severe hypokalemia raised the suspicion of Cushing’s syndrome. Additional tests revealed a high serum ACTH level of 224 pg/mL on presentation that was not suppressed (20 pg/mL) by administration of high-dose dexamethasone intravenously.
A CT scan of the brain, chest, abdomen, and pelvis revealed a large mass within the gallbladder. A PET/CT scan to look for metastases showed the gallbladder (Figure 1A) as the only site of malignancy. Bilateral enlarged and moderately hypermetabolic adrenal glands were also noted (Figure 1B) and appeared to represent adrenal hyperplasia stimulated by the ectopically produced ACTH. The pituitary gland was normal.
Figure 1.
F-18 Fluorodeoxyglucose PET/CT Findings in ACTH-producing gallbladder carcinoma. A: PET image shows a rounded, diffusely hypermetabolic mass in the gallbladder fossa (arrow), and bilaterally hypermetabolic adrenal glands (arrowheads); B: CT image shows a corresponding tissue-density mass within the body of the gallbladder (arrow) and bilaterally prominent adrenal glands (arrowheads).
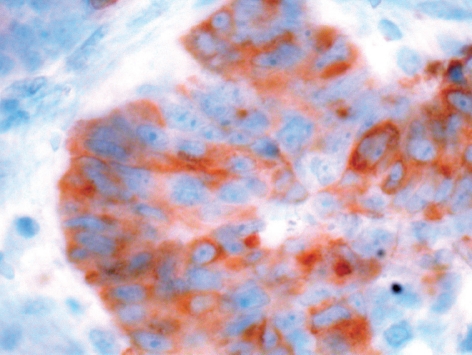
The patient underwent definitive treatment: a cholecystectomy and wedge-shaped liver resection were performed. Perioperatively, stress dose steroids were given and then reduced after surgery. Immunohistochemical analysis of the gallbladder tumor revealed expression of chromogranin and synaptophysin consistent with a neuroendocrine tumor. ACTH-stain of the tumor cells was positive (Figure 2). Normalization of the serum ACTH level postoperatively to 9 pg/mL suggested the tumor to be the source of ectopic ACTH-production. Chemotherapy was offered because of the risk of metastases, but the patient declined to undergo this. Two months later, she returned to the hospital with hepatic metastases with again elevated ACTH level of 647 pg/mL. Arterial embolization as palliative treatment was performed. The patient eventually died with active metastatic disease.
Figure 2.
ACTH-stain of the tumor cells.
DISCUSSION
The National Cancer Institute predicted 9520 new cases of gallbladder carcinoma and 3340 deaths from this in the US in 2008. Adenocarcinoma is the most common gallbladder malignancy. A minority of gallbladder tumors may exhibit carcinoid features. While carcinoids are well-differentiated, large cell neuroendocrine carcinomas are more poorly differentiated, and carry a more serious prognosis.
The most common symptoms of gallbladder cancer are right upper quadrant or abdominal pain, anorexia, nausea and vomiting, thus frequently mimicking cholelithiasis or cholecystitis. Often, the disease is asymptomatic early on, leading many patients ultimately to present with advanced-stage disease. It has been shown that with increased use of CT and other imaging techniques, a preoperative diagnosis may be reached in 75% to 88% of cases[5].
In general, treatment and prognosis of gallbladder cancer depends on the disease stage at the time of diagnosis. Surgery is the only potentially curative treatment for gallbladder cancer, but only 10% to 30% of patients are eligible for such potentially curative resection. Five-year survival rates range from 5% to 12%. The poor prognosis associated with gallbladder cancer is related to the difficulty of diagnosis except at an advanced stage of the disease, which is due, in turn, to both the anatomic position of the gallbladder, and the relatively low specificity of the symptoms.
Coates et al[6] mentioned that a wide variety of tissue can produce ACTH, and that Cushing’s syndrome caused by “non-endocrine” organs has been known since 1928. Most of the tumors causing Cushing’s syndrome are derived from cells of the diffuse neuroendocrine system. Hormone production outside the usual tissue of origin accounted for between 12% and 25% of cases of Cushing’s syndrome, in which small cell carcinomas were the most commonly recognized tumors.
They described one feature of these highly malignant tumors as exhibiting high levels of hormone secretion and high serum levels of ACTH, with, as a consequence,low storage of hormones in the tumor cells. Only one of their 18 patients with tumors causing Cushing’s syndrome had a tumor derived from the gall bladder, which was a highly aggressive atypical carcinoid. The patient died only one month after presentation.
We identified a highly aggressive ACTH-producing gall bladder tumor with positive immunocytochemical stain of the tumor cells in our patient.
The first two cases of large cell neuroendocrine carcinoma of the gallbladder were reported in 2000[2]. Both cases were found incidentally after cholecystectomy. In contrast to our patient, neither of these patients had Cushing’s syndrome or other evidence of an ACTH-producing tumor. A single case report in 1975 described an ACTH-secreting anaplastic adenocarcinoma of the gallbladder in a patient with Cushingoid symptoms. Histology reported a fibrous, poorly differentiated anaplastic adenocarcinoma of the gallbladder[7]. Large cell neuroendocrine tumors can also occur in other parts of the body, including the lungs[1], the stomach[8], the urinary bladder[9,10] and the uterine cervix[11]. In general, it represents an aggressive tumor type and has a poor prognosis, similar to that of small cell carcinoma. It is therapeutically relevant to recognize large cell neuroendocrine carcinomas, since the chemotherapeutic agents used to treat such tumors differ from those used in adenocarcinomas[2].
In conclusion, neuroendocrine tumors can theoretically develop and present de novo in any organ of the body. They are often found incidentally unless they are hormone-producing. ACTH-producing neuroendocrine carcinomas located specifically in the gallbladder are rare in the literature. In the case of our patient, the findings on PET/CT support this diagnosis, showing malignant activity within the gallbladder, as well as abnormal functional activity in the adrenal glands as a consequence of Cushing’s syndrome. Cushing’s syndrome can therefore be a sign of the presence of a hormone-producing neuroendocrine tumor. Although rapid growth and poor prognosis can be features of those tumors , with the help of modern immunocytochemical and radiographically techniques, earlier detection might be possible.
Acknowledgments
The authors greatly appreciate the support of Dr. J Harlan-Meyer, endocrinology, Dr. Steven Nishida, general surgery, and Dr. Thomas Namiki, pathology. We thank Dr. Dominic Chow, MPH, for his constructive advice.
Footnotes
Peer reviewer: Robert John Lovat Fraser, Associate Professor, Investigations and Procedures Unit, Repatriation General Hospital, Daw Park 5041, Australia
S- Editor Li LF L- Editor Herholdt A E- Editor Lin YP
References
- 1.Travis WD, Linnoila RI, Tsokos MG, Hitchcock CL, Cutler GB Jr, Nieman L, Chrousos G, Pass H, Doppman J. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15:529–553. doi: 10.1097/00000478-199106000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Papotti M, Cassoni P, Sapino A, Passarino G, Krueger JE, Albores-Saavedra J. Large cell neuroendocrine carcinoma of the gallbladder: report of two cases. Am J Surg Pathol. 2000;24:1424–1428. doi: 10.1097/00000478-200010000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Albores-Saavedra J, Henson DE. Tumours of the gallbladder and extrahepatic bile ducts. In: Atlas of tumor pathology, 2nd series, fascicle 22., editors. Armed Forces Institute of Pathology. 2nd Series, fascicle 22. Washington, DC: Armed Forced Institute of Pathology; 1986. [Google Scholar]
- 4.Jun SR, Lee JM, Han JK, Choi BI. High-grade neuroendocrine carcinomas of the gallbladder and bile duct: Report of four cases with pathological correlation. J Comput Assist Tomogr. 2006;30:604–609. doi: 10.1097/00004728-200607000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Chijiiwa K, Sumiyoshi K, Nakayama F. Impact of recent advances in hepatobiliary imaging techniques on the preoperative diagnosis of carcinoma of the gallbladder. World J Surg. 1991;15:322–327. doi: 10.1007/BF01658723. [DOI] [PubMed] [Google Scholar]
- 6.Coates PJ, Doniach I, Howlett TA, Rees LH, Besser GM. Immunocytochemical study of 18 tumours causing ectopic Cushing's syndrome. J Clin Pathol. 1986;39:955–960. doi: 10.1136/jcp.39.9.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spence RW, Burns-Cox CJ. ACTH-secreting 'apudoma' of gallbladder. Gut. 1975;16:473–476. doi: 10.1136/gut.16.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsui K, Jin XM, Kitagawa M, Miwa A. Clinicopathologic features of neuroendocrine carcinomas of the stomach: appraisal of small cell and large cell variants. Arch Pathol Lab Med. 1998;122:1010–1017. [PubMed] [Google Scholar]
- 9.Abenoza P, Manivel C, Sibley RK. Adenocarcinoma with neuroendocrine differentiation of the urinary bladder. Clinicopathologic, immunohistochemical, and ultrastructural study. Arch Pathol Lab Med. 1986;110:1062–1066. [PubMed] [Google Scholar]
- 10.Hailemariam S, Gaspert A, Komminoth P, Tamboli P, Amin M. Primary, pure, large-cell neuroendocrine carcinoma of the urinary bladder. Mod Pathol. 1998;11:1016–1020. [PubMed] [Google Scholar]
- 11.Gilks CB, Young RH, Gersell DJ, Clement PB. Large cell neuroendocrine [corrected] carcinoma of the uterine cervix: a clinicopathologic study of 12 cases. Am J Surg Pathol. 1997;21:905–914. doi: 10.1097/00000478-199708000-00004. [DOI] [PubMed] [Google Scholar]