Abstract
The combination of complete cytoreductive surgery and perioperative intraperitoneal chemotherapy provides the only chance for long-term survival for selected patients diagnosed with a variety of peritoneal neoplasms, either primary or secondary to digestive or gynecologic malignancy. Hyperthermic intraperitoneal chemotherapy (HIPEC) delivered in the operating room once the cytoreductive surgical procedure is finalized, constitutes the most common form of administration of perioperative intraperitoneal chemotherapy. This may be complemented in some instances with early postoperative intraperitoneal chemotherapy (EPIC). HIPEC combines the pharmacokinetic advantage inherent to the intracavitary delivery of certain cytotoxic drugs, which results in regional dose intensification, with the direct cytotoxic effect of hyperthermia. Hyperthermia exhibits a selective cell-killing effect in malignant cells by itself, potentiates the cytotoxic effect of certain chemotherapy agents and enhances the tissue penetration of the administered drug. The chemotherapeutic agents employed in HIPEC need to have a cell cycle nonspecific mechanism of action and should ideally show a heat-synergistic cytotoxic effect. Delivery of HIPEC requires an apparatus that heats and circulates the chemotherapeutic solution so that a stable temperature is maintained in the peritoneal cavity during the procedure. An open abdomen (Coliseum) or closed abdomen technique may be used, with no significant differences in efficacy proven to date. Specific technical training and a solid knowledge of regional chemotherapy management are required. Concerns about safety of the procedure for operating room personnel are expected but are manageable if universal precautions and standard chemotherapy handling procedures are used. Different HIPEC drug regimens and dosages are currently in use. A tendency for concurrent intravenous chemotherapy administration (bidirectional chemotherapy, so-called “HIPEC plus”) has been observed in recent years, with the aim to further enhance the cytotoxic potential of HIPEC. Future trials to ascertain the ideal HIPEC regimen in different diseases and to evaluate the efficacy of new drugs or drug combinations in this context are warranted.
Keywords: Hyperthermia, Intracavitary chemotherapy, Peritoneal neoplasms, Peritoneal carcinomatosis, Cytoreductive surgery
INTRODUCTION
Peritoneal dissemination of gastrointestinal (GI) or gynecologic cancers or primary peritoneal neoplasms constitute a difficult challenge for the practicing oncologist given the dismal prognosis associated with these entities and the debilitating effect that they exert on those patients who suffer them. Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy is currently a valid treatment option for selected cases diagnosed with these diseases. Extensive clinical and pharmacological research studies have been conducted and unprecedented therapeutic results have been reported[1-4], bringing peritoneal surface oncology to the forefront of clinical oncology practice and research. Moreover, peritoneal surface malignancy treatment centers have been established around the world.
Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy is a complex therapeutic modality. It includes an aggressive and extensive surgical procedure and the administration of intraperitoneal chemotherapy, either in the intraoperative setting with hyperthermia or/and in the early postoperative setting. In expert hands, the associated morbidity and mortality parallels that of other major oncological surgery[5], but this expertise needs to be gained. Awareness of treatment-related toxicity is important and needs to be factored in the patient selection process.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC) is delivered in the operating room once the cytoreductive surgical procedure is finalized and constitutes the most common form of administration of perioperative intraperitoneal chemotherapy. The acronym HIPEC, coined by the group from the Netherlands Cancer Institute, became the standardized nomenclature for this procedure as a result of the experts’ consensus achieved during the Fourth International Workshop on Peritoneal Surface Malignancy (Madrid, 2004)[6].
In this article, the rationale that supports its use and the methodology employed for the delivery of HIPEC are discussed. Additionally, safety precautions to be observed during the procedure are reviewed.
RATIONALE
The pharmacokinetic advantage of intraperitoneal chemotherapy administration
Following intraperitoneal delivery of cytotoxic drugs, high regional concentrations can be achieved while keeping systemic drug levels low. The concentration differential is in part due to the relatively slow rate of movement of the drug from the peritoneal cavity into the plasma (peritoneal clearance). This pharmacokinetic advantage is explained by the existence of a peritoneal-plasma barrier, which maintains a continuous high concentration gradient of chemotherapeutic drug between the peritoneal cavity and the plasma compartment[7,8], although its exact anatomical nature has not been fully elucidated. Actually, extensive removal of the diseased peritoneum during cytoreductive surgery does not seem to affect the pharmacokinetics of intraperitoneal chemotherapy[9]. An additional advantage to intraperitoneal chemotherapy administration is that the blood drainage of the peritoneal surface occurs via the portal vein to the liver, providing a first-pass (detoxifying) effect and an increased exposure of potential hepatic micrometastases to cytotoxic drugs[10]. Certain drugs are also transported through lymphatics to the systemic circulation and consequently higher drug concentrations in the lymph than in the plasma are achieved.
The area under the concentration-time curve ratio (AUC ratio) of the drugs between the peritoneal cavity and the peripheral blood expresses most adequately the pharmacological advantage of intraperitoneal drug administration. Depending on their molecular weight, their affinity to lipids and first-pass effect and clearance by the liver, the intraperitoneal to plasma drug AUC ratio may exceed 1000, as in the case of placlitaxel. Commonly used agents in GI or gynaecological oncology such as platinum derivatives, 5-FU, taxanes, irinotecan, adriamycin or mitomycin C show this advantage to a different extent.
The pharmacokinetic model that governs this phenomenon goes beyond the classical two-compartment model, with two compartments (plasma and peritoneal cavity in this case) separated by a semipermeable membrane. A three-compartment model that incorporates the tumor-bearing peritoneum as the third compartment, where the drug is also incorporated by tissue penetration, offers a more accurate explanation[11]. This compartment is the actual target of the cytotoxic treatment and can also be reached via systemic administration of the drug via subperitoneal capillaries; this provides the rationale for the recently designed “bidirectional” chemotherapy regimens consisting in the concurrent intraperitoneal and intravenous administration of the drugs.
Tissue penetration
A disadvantage of intracavitary chemotherapy is the limited tissue penetration by the therapeutic agent. Unfortunately, for many agents it is difficult to accurately measure tissue penetration depth and concentration after intraperitoneal administration and, when possible, there is a large inter-individual variation. Nevertheless, the penetration depth of drugs that are intraperitoneally delivered is estimated to be a maximum of 3 to 5 mm[12-17]. These figures are actually considered an overestimation, the reality being in the range from a few cell layers to a few millimeters. This is the reason why an adequate cytoreductive surgery should precede the intraperitoneal delivery of drugs and why 2.5 mm in largest diameter is considered the threshold for residual tumor nodule diameter if a cytoreduction is to be considered optimal (“complete cytoreduction”).
Hyperthermia
There is an abundance of experimental and clinical evidence that indicate that malignant cells are selectively destroyed by hyperthermia in the range of 41 to 43°C. The cellular and molecular basis for this selectivity has been well studied[18-20]. While inhibited RNA synthesis and mitosis arrest are reversible and nonselective results of hyperthermia, an increase in the number of lysosomes and lysosomal enzyme activity are selective effects in malignant cells. These heat-induced lysosomes are more labile in malignant cells and therefore result in increased destructive capacity. Furthermore, the microcirculation in most malignant tumours exhibits a decrease in blood flow or even complete vascular stasis in response to hyperthermia, which is in contrast to an increased flow capacity found in normal tissues[21]. This, in combination with depression or complete inhibition of oxidative metabolism in tumour cells subjected to hyperthermia and unaltered anaerobic glycolysis, leads to accumulation of lactic acid and lower pH in the microenvironment of the malignant cell. This effect is selective for malignant cells and may be due to the increased sensitivity of mitochondrial membranes in malignant cells. The increased acidity then increases the activity of the lysosomes which are increased in number. This results in accelerated cell death of the more fragile malignant cells subjected to hyperthermia[19] as compared to normal cells.
Thermal enhancement of cytotoxicity
The combination of heat and cytotoxic drugs frequently results in an increased cytotoxicity, beyond that predicted for an additive effect. The synergism between both kinds of treatment is dependent on several factors including increased drug uptake in malignant cells which is due to increased membrane permeability and improved membrane transport. There is also evidence that heat may alter cellular metabolism and change drug pharmacokinetics and excretion, both of which can increase the cytotoxicity of certain chemotherapeutic agents[22]. Additional factors include increased drug penetration in tissue, temperature-dependent increases in drug action and inhibition of repair mechanisms. In many cases, this enhancement of activity and penetration depth of drugs is already seen above 39-40°C[16,20,23,24].
The synergism of heat and drugs has been well documented, especially for selected chemotherapeutic agents used during HIPEC. Several agents have been shown to have an apparently improved therapeutic index and efficacy when used with hyperthermia in in vitro and in vivo experimental studies. Generally, the highest thermal enhancement ratios have been observed for alkylating agents such as melphalan, cyclophosphamide and ifosfamide[25]. Thermal enhancement of cytotoxicity has been shown for a variety of drugs, the most questioned today is that of the taxanes.
Uncontrolled hyperthermia may result in acute and late systemic side-effects. Actually central temperature rises during HIPEC. However, in HIPEC the heat is applied locoregionally and hence such an adverse effect of hyperthermia on drugs’ toxicity is not, or in a much lesser extent, to be expected.
Choice of drug and drug dosaging for HIPEC
The choice of the chemotherapeutic drug is very important and certain aspects have to be considered. It is important for the agent to lack severe direct local toxicity after intraperitoneal administration. Moreover, the drug should have a well-established activity against the malignancy treated. Drugs that have to be metabolized systemically into their active form are inappropriate for intraperitoneal use. Whereas in instillation intraperitoneal chemotherapy all categories of active drugs can be used, in HIPEC procedures a direct cytotoxic agent (cell cycle-nonspecific) is needed[22].
Systemic exposure to intraperitoneally administered drugs inevitably occurs to a variable, limited extent and is responsible for their toxicity. In order to make this exposure and the subsequent toxicity predictable, standardized dosaging by body surface area of both the drug and the volume of the carrier solution to be employed are recommended. For the latter, some authors recommend 2 L/m2[26], whereas others propose 1.5 L/m2[27].
TECHNIQUE
HIPEC is delivered once tumor cytoreduction has been concluded and before any digestive reconstruction or diversion is made. The rationale for this timing in relation to GI tract reconstruction has to do with the opportunity of exposing bowel section lines to the chemotherapy solution in an effort to minimize the chance for anastomotic or staple line recurrence. Although this is the classical way to do it, there are some groups that perform anastomoses before the administration of HIPEC with no apparent increase in anastomotic recurrences.
The chemotherapy solution is prepared in the pharmacy department and it is sent to the operating room in a closed light-protected bag with appropriate labeling which is handled with double gloves and the integrity of the bag is checked. Any leak detected results in the bag being returned to the pharmacy department. If the bag is approved there is no risk of direct exposure and it is given to the person responsible for the perfusion, who must check the patient’s name, drug and dose delivered against those prescribed.
Generally speaking, there are two methods for intraperitoneal administration of hyperthermic chemotherapy: open abdomen technique and closed abdomen technique.
The open method is usually performed by the “Coliseum technique”, as described by Sugarbaker[28]. Once the cytoreductive phase has been finalized, a Tenckhoff catheter and four closed suction drains are placed through the abdominal wall and made watertight with a purse string suture at the skin. A different number of temperature probes secured to the skin edge may be used for intraperitoneal temperature monitoring; at least one in the in-flow line and another one at a distance from this point (pelvis) are employed. The skin edges of the abdominal incision are suspended up to a Thompson self-retaining retractor by a running monofilament number 1 suture, in order to create an open space in the abdominal cavity. A plastic sheet is incorporated into this suture to prevent chemotherapy solution splashing from occurring. A slit in the plastic cover is made to allow the surgeon´s double gloved hand access to the abdomen and pelvis. Impervious gown and protection goggles are mandatory. The smoke evacuator is placed under the plastic sheet to clear chemotherapy particles that may be liberated during the procedure. During the 30 min to 90 min of perfusion, all the anatomic structures within the peritoneal cavity are uniformly exposed to heat and chemotherapy by continuous manipulation of the perfusate. A roller pump forces chemotherapy perfusion into the abdomen through the Tenckhoff catheter and pulls it out through the drains, with a flow rate around 1 L/min. A heat exchanger keeps the fluid being infused at 43-45°C so that the intraperitoneal fluid is maintained at 41-43°C. The one-use circuit tubing is commercially available from the HIPEC machine companies or from the cardioplegia industry, and most of them incorporate a reservoir, useful when the chemotherapy solution needs to be quickly extracted from the abdomen for any complication or in cases where the perfusate volume calculated cannot be fully accommodated by the peritoneal cavity capacity. The perfusate is first recirculated between the reservoir and the heat exchanger so that it can be heated to an adequate temperature. At this point, full circulation of the perfusate in and out of the peritoneal cavity is established until a minimum intraperitoneal temperature of 41.5°C is achieved and maintained. The drug is then added to the circuit and the timer for the perfusion is started. In the bidirectional chemotherapy protocols (sometimes referred to as “HIPEC-plus”), the intravenous infusion of the appropriate drugs is started at this time point as well, although some authors advocate doing it 1 h before the initiation of HIPEC.
The main benefit of the Coliseum technique is that heated chemotherapy is adequately distributed throughout the abdominal cavity and there is no pooling of temperature or chemotherapy. One disadvantage of the open technique is heat dissipation that makes it more difficult to initially achieve a hyperthermic state. Another possible disadvantage is the increased exposure of operating room personnel to chemotherapy. As the surgeon is manipulating chemotherapy throughout the perfusion, an increased potential for contact exposure exists. Furthermore, because the abdomen is open during the perfusion, heated chemotherapy could give way to aerosol formation, creating a risk of inhalation exposure. Stuart et al[29] evaluated the safety of operating room personnel during the Coliseum technique. Urine from members of the operating team was assayed for chemotherapy levels. Air below and above the plastic sheet was also analyzed. Finally, sterile gloves commonly used in the operating room were examined for permeability to chemotherapy. All assessments of potential exposures were found to be negative and in compliance with established safety standards.
Side effects from HIPEC appear to be principally related to the magnitude of the surgery[5]. The open technique has theoretical advantages over the closed technique due to improved distribution of heated chemotherapy; however, it has not been definitively proven in a randomized controlled trial.
A variation of the open technique described and mainly used in Japan uses a device called “peritoneal cavity expander” (PCE). The PCE is an acrylic cylinder containing in-flow and out-flow catheters that is secured over the wound. When filled with heated perfusate, the PCE can accommodate the small bowel, allowing it to float freely and be manually manipulated in the perfusate. After HIPEC is completed, the perfusate is drained and the PCE is removed. By using the expander, a more uniform distribution is theoretically achieved compared to a closed technique. The main disadvantage of the PCE technique is the risk of exposure to chemotherapy of the operating room personnel as in Coliseum technique[30]. Fujimura et al[30] reported about PCE-HIPEC use in carcinomatosis from various malignancies with good results. Yonemura et al[31] reported the use of the PCE-HIPEC technique for prophylaxis against recurrence of gastric cancer following resection with 5-year survival of 55% but only a 30% in surgery-only controls. Although there are no studies directly comparing PCE to the coliseum technique or closed technique, the reported results appear to be similar.
In the closed technique catheters and temperature probes are placed in the same fashion but the laparotomy skin edges are sutured watertight so that perfusion is done in a closed circuit. The abdominal wall is manually agitated during the perfusion period in an attempt to promote uniform heat distribution. A larger volume of perfusate is generally needed to establish the circuit compared with the open technique and a higher abdominal pressure is achieved during the perfusion, which may facilitate drug tissue penetration. After perfusion, the abdomen is reopened and the perfusate is evacuated. Appropriate anastomoses are performed and the abdomen is closed in the standard fashion.
A major advantage of the closed technique is the ability to rapidly achieve and maintain hyperthermia as there is minimal heat loss. In addition, there is minimal contact or aerosolized exposure of the operating room staff to the chemotherapy. The only way for exposure is leakage through the surgical wound or catheter wounds. The main disadvantage is the lack of uniform distribution of the chemotherapy. When methylene blue was instilled using closed technique, uneven distribution was observed. Uneven distribution of HIPEC is problematic, because hyperthermia has a narrow therapeutic index. Tumoricidal activity is manifested at 41-43°C; therefore in-flow temperature usually exceeds 45°C[32]. Rats exposed to intraperitoneal temperatures of 45°C suffered significant morbidity and mortality[33]. Therefore, inadequate circulation of heated perfusate leads to pooling and accumulation of heat and chemotherapy in dependent parts of the abdomen. This may result in increased systemic absorption and foci of hyperthermic injury that could contribute to postoperative ileus, bowel perforation, and fistula. On the other hand, certain intraabdominal areas will be undertreated. Cytoreduction and HIPEC closed technique can be performed safely as it has been reported in different centers[34,35]. Morbidity associated with this procedure includes myelosuppression, ileus, and fistula, as in the open technique. Heterogeneous distribution inside the closed abdomen may increase the rate of intra-abdominal complications.
In the last few years, increased interest in HIPEC has led to the commercial development of hyperthermic intraperitoneal perfusion systems. These are compact devices that contain roller pumps, a heating device, a heat exchanger and temperature monitors in a single apparatus. A computer integrates and displays information from the temperature probes, inflow and outflow rates. Several options are commercially available at this time.
The role of the anesthesiologist is crucial during HIPEC, as it is during the whole complex cytoreductive procedure. Specific training is desirable. During the whole lengthy surgical procedure knowledgeable fluid management needs to be carried out, keeping a balance between the use of crystalloids and colloids to achieve adequate central venous pressures and urine output without incurring in fluid overload. The latter is a common undesirable side effect observed after this surgery with consequences that range from acute pulmonary edema to cerebral edema when anesthesiologists not familiarized with this procedure are assigned to these cases. A minimal urine output of 100 cc (desirable 150 cc) every 15 min during the administration of HIPEC is mandatory to avoid renal toxicity derived from the cytotoxic drug employed. The utilization of a low-dose dopamine perfusion is a common measure to achieve this goal. Central temperature is monitored by an esophageal probe and may be expected to rise up to 39°C or more; different cooling measures need to be implemented at this time to avoid sustained central hyperthermia starting by turning off the air heating blankets and moving to the intravenous administration of cold crystalloids or placement of ice packs around the head and neck of the patient.
HIPEC DRUG REGIMENS
Different drug regimens have been employed over the years for HIPEC. Drug choice primarily depends on its known activity against the disease being treated and its suitability for intraoperative administration with hyperthermia (cycle-non-specific method of action, heat-synergized cytotoxicity, non-vesicant). Single drug and drug combination regimens are currently in use. Although different carrier solutions with varying chemical properties have been investigated[36], 1.5% dextrose isotonic peritoneal dialysis solution is the most widely employed. Some groups use regular crystalloids (normal saline or 5% dextrose in water). Heavy molecular weight starch (6% Hetastarch®) is regularly employed as carrier solution for paclitaxel[37].
An important issue regarding toxicity of HIPEC has to do with dosaging. Both the drug dose and the carrier solution volume should be calculated based on body surface area, so that toxicity can be predictable. Perfusate volumes commonly used may be 1.5 L/m2[26] or 2 L/m2[27]. HIPEC regimens using fixed doses (same dose for any patient), drug dosaging by liter of perfusate or by body weight are more prone to find untoward events secondary to unnoticed overdosing of the cytotoxic drug employed. A 33% dose-reduction is recommended for patients over the age of 60, previously exposed to multiple lines of systemic chemotherapy, who needed GM-CSF rescue for febrile neutropenia while on systemic chemotherapy or who have received radiation therapy to bone-marrow bearing regions.
Perioperative intraperitoneal chemotherapy regimens that employ early postoperative intraperitoneal chemotherapy (EPIC) use moderate drug doses for HIPEC, while those that do not employ EPIC use much higher doses for HIPEC. In the last few years, bidirectional HIPEC regimens (concurrent administration of intraperitoneal and intravenous chemotherapy) have gained ground. Elias was first to use intravenous 5-FU and folinic acid prior to HIPEC with oxaliplatin due to the instability of the mix of both drugs[26]. Sugarbaker would later demonstrate that after the intravenous administration of 5-FU in a patient under general anesthesia in an intraperitoneal hyperthermic environment, the drug unexpectedly accumulates in the peritoneal cavity, a true heat-targeting phenomenon[11]. Table 1 lists commonly-used HIPEC regimens.
Table 1.
Common HIPEC regimens currently in use
| Center/Country | HIPEC drug (s) and doses | HIPEC duration | Concomitant intravenous | EPIC | Indication |
| (min) | chemotherapy | ||||
| Washington hospital center/ | Mitomycin C, 15 mg/m2 | 90 | 5-FU, 400 mg/m2 | 5-FU | Appendiceal, and |
| Washington, DC (USA) | Doxorubicin, 15 mg/m2 | LV, 20 mg/m2 | 4 d | colorectal carcinomatosis | |
| Washington hospital center/ | Cisplatin, 50 mg/m2 | 90 | 5-FU, 400 mg/m2 | Taxol | Gastric cancer, peritoneal |
| Washington, DC (USA) | Doxorubicin, 15 mg/m2 | LV, 20 mg/m2 | 4 d | mesothelioma, ovarian | |
| cancer | |||||
| Washington hospital center/ | Oxaliplatin, 130 mg/m2 | 60 | 5-FU, 400 mg/m2 | 5-FU | Appendiceal, and |
| Washington, DC (USA) | LV, 20 mg/m2 | 4 d | colorectal carcinomatosis | ||
| Washington hospital center/ | Melphalan, 50-70 mg/m2 | 60 | No | No | Carcinomatosis with |
| Washington, DC (USA) | incomplete cytoreduction | ||||
| Gustave roussy institute/ | Oxaliplatin, 460 mg/m2 | 30 | 5-FU, 400 mg/m2 | No | Colorectal carcinomatosis |
| Villejuif (France) | LV, 20 mg/m2 | ||||
| National cancer institute/ | Mitomycin C, 35 mg/m2 | 90 | No | No | Appendiceal, and |
| Amsterdam (Netherlands) | colorectal carcinomatosis | ||||
| National cancer institute/ | Cisplatin, 43 mg/L | 90 | No | No | Peritoneal mesothelioma, |
| Milan (Italy) | Doxorubicin ,15.25 mg/L | advanced ovarian cancer | |||
| National cancer institute/ | Mitomycin C, 3.3mg/m2/L | 90 | No | No | Appendiceal, and |
| Milan (Italy) | Cisplatin, 25 mg/m2/L | colorectal carcinomatosis; | |||
| advanced ovarian cancer; | |||||
| peritoneal mesothelioma | |||||
| Centre hospitalo-universitaire | Mitomycin C, | 90 | No | No | Appendiceal, gastric and |
| lyon-sud/Lyon (France) | 10 mg/mL of perfusate | colorectal carcinomatosis | |||
| Centre hospitalo-universitaire | Mitomycin C, 0.5 mg/kg | 90 | No | No | Peritoneal mesothelioma |
| lyon-sud/Lyon (France) | Cisplatin 0.7 mg/kg | ||||
| Centre hospitalo-universitaire | Cisplatin, 20 mg/m2/L | 90 | No | No | Recurrent and |
| lyon-sud/Lyon (France) | chemoresistant stage III | ||||
| ovarian cancer | |||||
| National cancer institute/ | Cisplatin, 250 mg/m2 | 90 | No | 5-FU + Taxol | Peritoneal mesothelioma |
| Bethesda, MD (USA) | 1 d |
L: liter of perfusate; HIPEC: Hyperthermic intraperitoneal chemotherapy; EPIC: Early postoperative intraperitoneal chemotherapy.
GUIDELINES FOR SAFE ADMINISTRATION OF HIPEC
Finally, safety measures in the operating room where HIPEC is to be administered cannot be overemphasized. Although chemotherapy is diluted in the carrier solution and the adverse effects of continuous exposure to low doses of cytotoxic drugs remain unknown, a breach in operating room safety that may unnecessarily expose the staff to hazardous drugs can destroy a HIPEC treatment program. Certain general safety measures must be in effect every tine HIPEC is used in the operating room[38]: (1) At the beginning of the operation the surgical field should be arranged with impervious, disposable sheets and drapes, avoiding the use of any non-disposable fabric cloth; (2) After cytoreduction, all staff not directly involved in the administration of HIPEC should leave the operating room during the administration of the treatment and staff circulation in and out of the room should be kept to a minimum; (3) Signs warning that HIPEC is in progress must be placed at the entrance of the dedicated surgical area; (4) Absorbent towels with impervious back are placed on the floor and all around the surgical table for possible spills; (5) Rigid containers, leak proof for biologically hazardous material and properly labeled with “cytotoxic agents” labels, are placed in the operating room. They should not be more than half full. Chemotherapy contaminated material should be handled as little as possible and with minimal agitation to prevent dissemination into the environment; (6) Protective barrier garments should be worn for all procedures involving preparation, use and disposal of cytotoxic drugs. In the operating room, during HIPEC, all personnel should wear protective disposable impervious gowns and shoe covers, non-permeable powderless latex gloves worn as double gloves and eye wear for possible droplet protection. Potentially contaminated garments must not be worn outside the work area; (7) Universal Precautions for handling biological hazardous materials are implemented and monitored continuously. Any body fluid, blood sample, tissue specimen, laparotomy pads, drapes, gowns or plastic tubing must be handled as biological hazardous material. Body fluids are considered contaminated for 48 h after the last administration of chemotherapy. Labels saying “cytotoxic agent” should be used to mark every sample, specimen, or contaminated trash; (8) Latex powder-free gloves are recommended for all procedures involving cytotoxic drugs. They should be non-permeable and worn as double gloves for direct contact with chemotherapy. In a comparative study, BiogelTM gloves were found to have the lowest permeability to chemotherapy[29]. Gloves should be routinely changed approximately every 30 min when working steadily with cytotoxic agents. Gloves should be changed immediately after overt contamination. Double gloving is recommended for cleaning up of spills. Surgeons in direct contact with chemotherapy should wear the outer glove up to the elbow (Figure 1) (9) High power filtration mask (FFP-3) tightly fit to the face (high filtration of sub-micron particles) may be recommended at some centers; (10) A smoke evacuator should be working continuously under the plastic sheet during the perfusion; (11) Every effort should be done to avoid any spill, but if it happens, the circulating nurse should contain and clean it up immediately. If direct contact with a cytotoxic agent occurs, contaminated clothing should be removed immediately and discarded in a hazardous waste container. Affected skin should be washed immediately with mild, additive-free soap with no dyes or perfumes that may interact with the cytotoxic agent. If the affected area is the eye, it should be flooded immediately with water or isotonic saline for 5 min. The staff member should then report the incident to the occupational health office. The area should be washed three times with water and neutral soap. Then, the area can be cleaned in the routine manner. To clean up a small spill, the personnel should wear the whole protective barrier garments already described. A large spill is defined as a drop of more than 5 g or 5 mL of pure drug. Personnel containing the spill should wear a respirator mask and standard protective clothing. They should take care to avoid creating aerosols when cleaning large spills; (12) During HIPEC and EPIC, chemotherapy is always diluted, never pure, and doses of drugs are in micrograms, so that it is not possible to have a major spill; (13) Cleaning the operating room after HIPEC: personnel should wear the standard protective clothing described. Bactericidal cleaning solutions should not be used to wash contaminated area because they may react with the cytotoxic agents and do not inactivate them. Water with neutral soap is adequate to clean the operating room after HIPEC three consecutive times. Seventy percent isopropyl alcohol is also safe and effective; and (14) Instrument trays are labeled with “cytotoxic agent”. They should be washed three times with water and pure soap before leaving the working area.
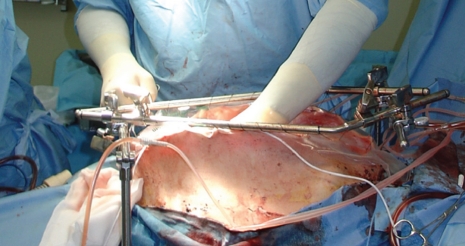
Figure 1.
Administration of HIPEC by the coliseum (open) technique. Constant manipulation of the perfusate ensures a homogeneous distribution of the heated chemotherapy within the peritoneal cavity. Note that elbow-length double gloving, goggles and an impervious gown are used.
Footnotes
Peer reviewer: Akihiko Tsuchida, MD, PhD, Associate Professor, Department of Surgery, Tokyo Medical University, 6-7-1 Nishi-Shinjuku, Shinjuku-ku, Tokyo 160-0023, Japan
S- Editor Li LF L- Editor Roemmele A E- Editor Yang C
References
- 1.Yan TD, Welch L, Black D, Sugarbaker PH. A systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for diffuse malignancy peritoneal mesothelioma. Ann Oncol. 2007;18:827–834. doi: 10.1093/annonc/mdl428. [DOI] [PubMed] [Google Scholar]
- 2.Yan TD, Black D, Savady R, Sugarbaker PH. A systematic review on the efficacy of cytoreductive surgery and perioperative intraperitoneal chemotherapy for pseudomyxoma peritonei. Ann Surg Oncol. 2007;14:484–492. doi: 10.1245/s10434-006-9182-x. [DOI] [PubMed] [Google Scholar]
- 3.Yan TD, Black D, Savady R, Sugarbaker PH. Systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis from colorectal carcinoma. J Clin Oncol. 2006;24:4011–4019. doi: 10.1200/JCO.2006.07.1142. [DOI] [PubMed] [Google Scholar]
- 4.Yonemura Y, Bando E, Kawamura T, Ito H, Endo Y, Miura M, Kiyosaki K, Sasaki T. Cytoreduction and intraperitoneal chemotherapy for carcinomatosis from gastric cancer. Cancer Treat Res. 2007;134:357–373. doi: 10.1007/978-0-387-48993-3_23. [DOI] [PubMed] [Google Scholar]
- 5.Stephens AD, Alderman R, Chang D, Edwards GD, Esquivel J, Sebbag G, Steves MA, Sugarbaker PH. Morbidity and mortality analysis of 200 treatments with cytoreductive surgery and hyperthermic intraoperative intraperitoneal chemotherapy using the coliseum technique. Ann Surg Oncol. 1999;6:790–796. doi: 10.1007/s10434-999-0790-0. [DOI] [PubMed] [Google Scholar]
- 6.González-Moreno S. Peritoneal Surface Oncology: A progress report. Eur J Surg Oncol. 2006;32:593–596. doi: 10.1016/j.ejso.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Jacquet P, Sugarbaker PH. Peritoneal-plasma barrier. Cancer Treat Res. 1996;82:53–63. doi: 10.1007/978-1-4613-1247-5_4. [DOI] [PubMed] [Google Scholar]
- 8.Flessner MF. The transport barrier in intraperitoneal therapy. Am J Physiol Renal Physiol. 2005;288:F433–F442. doi: 10.1152/ajprenal.00313.2004. [DOI] [PubMed] [Google Scholar]
- 9.de Lima Vazquez V, Stuart OA, Mohamed F, Sugarbaker PH. Extent of parietal peritonectomy does not change intraperitoneal chemotherapy pharmacokinetics. Cancer Chemother Pharmacol. 2003;52:108–112. doi: 10.1007/s00280-003-0626-8. [DOI] [PubMed] [Google Scholar]
- 10.Speyer JL, Sugarbaker PH, Collins JM, Dedrick RL, Klecker RW Jr, Myers CE. Portal levels and hepatic clearance of 5-fluorouracil after intraperitoneal administration in humans. Cancer Res. 1981;41:1916–1922. [PubMed] [Google Scholar]
- 11.Van der Speeten K, Stuart OA, Sugarbaker PH. Pharmacokinetics and pharmacodynamics of perioperative cancer chemotherapy in peritoneal surface malignancy. Cancer J. 2009;15:216–224. doi: 10.1097/PPO.0b013e3181a58d95. [DOI] [PubMed] [Google Scholar]
- 12.Ozols RF, Locker GY, Doroshow JH, Grotzinger KR, Myers CE, Young RC. Pharmacokinetics of adriamycin and tissue penetration in murine ovarian cancer. Cancer Res. 1979;39:3209–3214. [PubMed] [Google Scholar]
- 13.El-Kareh AW, Secomb TW. A theoretical model for intraperitoneal delivery of cisplatin and the effect of hyperthermia on drug penetration distance. Neoplasia. 2004;6:117–127. doi: 10.1593/neo.03205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Los G, Verdegaal EM, Mutsaers PH, McVie JG. Penetration of carboplatin and cisplatin into rat peritoneal tumor nodules after intraperitoneal chemotherapy. Cancer Chemother Pharmacol. 1991;28:159–165. doi: 10.1007/BF00685503. [DOI] [PubMed] [Google Scholar]
- 15.Fujimoto S, Takahashi M, Kobayashi K, Nagano K, Kure M, Mutoh T, Ohkubo H. Cytohistologic assessment of antitumor effects of intraperitoneal hyperthermic perfusion with mitomycin C for patients with gastric cancer with peritoneal metastasis. Cancer. 1992;70:2754–2760. doi: 10.1002/1097-0142(19921215)70:12<2754::aid-cncr2820701205>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 16.Panteix G, Guillaumont M, Cherpin L, Cuichard J, Gilly FN, Carry PY, Sayag A, Salle B, Brachet A, Bienvenu J. Study of the pharmacokinetics of mitomycin C in humans during intraperitoneal chemohyperthermia with special mention of the concentration in local tissues. Oncology. 1993;50:366–370. doi: 10.1159/000227211. [DOI] [PubMed] [Google Scholar]
- 17.van de Vaart PJ, van der Vange N, Zoetmulder FA, van Goethem AR, van Tellingen O, ten Bokkel Huinink WW, Beijnen JH, Bartelink H, Begg AC. Intraperitoneal cisplatin with regional hyperthermia in advanced ovarian cancer: pharmacokinetics and cisplatin-DNA adduct formation in patients and ovarian cancer cell lines. Eur J Cancer. 1998;34:148–154. doi: 10.1016/s0959-8049(97)00370-5. [DOI] [PubMed] [Google Scholar]
- 18.Cavaliere R, Ciocatto EC, Giovanella BC, Heidelberger C, Johnson RO, Margottini M, Mondovi B, Moricca G, Rossi-Fanelli A. Selective heat sensitivity of cancer cells. Biochemical and clinical studies. Cancer. 1967;20:1351–1381. doi: 10.1002/1097-0142(196709)20:9<1351::aid-cncr2820200902>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 19.Overgaard J. Effect of hyperthermia on malignant cells in vivo. A review and a hypothesis. Cancer. 1977;39:2637–2646. doi: 10.1002/1097-0142(197706)39:6<2637::aid-cncr2820390650>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 20.Sticca RP, Dach BW. Rationale for hyperthermia with intraoperative intraperitoneal chemotherapy agents. Surg Oncol Clin N Am. 2003;12:689–701. doi: 10.1016/s1055-3207(03)00029-2. [DOI] [PubMed] [Google Scholar]
- 21.Dudar TE, Jain RK. Differential response of normal and tumor microcirculation to hyperthermia. Cancer Res. 1984;44:605–612. [PubMed] [Google Scholar]
- 22.de Bree E, Tsiftsis DD. Principles of perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis. Recent Results Cancer Res. 2007;169:39–51. doi: 10.1007/978-3-540-30760-0_4. [DOI] [PubMed] [Google Scholar]
- 23.Jacquet P, Averbach A, Stuart OA, Chang D, Sugarbaker PH. Hyperthermic intraperitoneal doxorubicin: pharmacokinetics, metabolism, and tissue distribution in a rat model. Cancer Chemother Pharmacol. 1998;41:147–154. doi: 10.1007/s002800050721. [DOI] [PubMed] [Google Scholar]
- 24.Benoit L, Duvillard C, Rat P, Chauffert B. [The effect of intra-abdominal temperature on the tissue and tumor diffusion of intraperitoneal cisplatin in a model of peritoneal carcinomatosis in rats] Chirurgie. 1999;124:375–379. doi: 10.1016/s0001-4001(00)80009-4. [DOI] [PubMed] [Google Scholar]
- 25.Takemoto M, Kuroda M, Urano M, Nishimura Y, Kawasaki S, Kato H, Okumura Y, Akaki S, Kanazawa S, Asaumi J, et al. The effect of various chemotherapeutic agents given with mild hyperthermia on different types of tumours. Int J Hyperthermia. 2003;19:193–203. doi: 10.1080/0265673021000035235. [DOI] [PubMed] [Google Scholar]
- 26.Elias D, Bonnay M, Puizillou JM, Antoun S, Demirdjian S, El OA, Pignon JP, Drouard-Troalen L, Ouellet JF, Ducreux M. Heated intra-operative intraperitoneal oxaliplatin after complete resection of peritoneal carcinomatosis: pharmacokinetics and tissue distribution. Ann Oncol. 2002;13:267–272. doi: 10.1093/annonc/mdf019. [DOI] [PubMed] [Google Scholar]
- 27.Sugarbaker PH, Mora JT, Carmignani P, Stuart OA, Yoo D. Update on chemotherapeutic agents utilized for perioperative intraperitoneal chemotherapy. Oncologist. 2005;10:112–122. doi: 10.1634/theoncologist.10-2-112. [DOI] [PubMed] [Google Scholar]
- 28.Sugarbaker PH. Technical Handbook for the Integration of Cytoreductive Surgery and Perioperative Intraperitoneal Chemotherapy into the Surgical Management of Gastrointestinal and Gynecologic Malignancy. 4th edition. Grand Rapids, Michigan: Ludann Company; 2005. [Google Scholar]
- 29.Stuart OA, Stephens AD, Welch L, Sugarbaker PH. Safety monitoring of the coliseum technique for heated intraoperative intraperitoneal chemotherapy with mitomycin C. Ann Surg Oncol. 2002;9:186–191. doi: 10.1007/BF02557372. [DOI] [PubMed] [Google Scholar]
- 30.Fujimura T, Yonemura Y, Fujita H, Michiwa Y, Kawamura T, Nojima N, Sato T, Fushida S, Nishimura G, Miwa K, et al. Chemohyperthermic peritoneal perfusion for peritoneal dissemination in various intra-abdominal malignancies. Int Surg. 1999;84:60–66. [PubMed] [Google Scholar]
- 31.Yonemura Y, Ninomiya I, Kaji M, Sugiyama K, Fujimura K, Sawa T, Katayama K, Tanaka S, Hirono Y, Miwa K. Prophylaxis with intraoperative chemohyperthermia against peritoneal recurrence of serosal invasion-positive gastric cancer. World J Surg. 1995;19:450–454; discussion 455. doi: 10.1007/BF00299188. [DOI] [PubMed] [Google Scholar]
- 32.Elias D, Detroz B, Debaene B, Damia E, Leclercq B, Rougier P, Lasser P. Treatment of peritoneal carcinomatosis by intraperitoneal chemo-hyperthermia: reliable and unreliable concepts. Hepatogastroenterology. 1994;41:207–213. [PubMed] [Google Scholar]
- 33.Fumagalli U, Trabucchi E, Soligo M, Rosati R, Rebuffat C, Tonelli C, Montorsi M. Effects of intraperitoneal chemotherapy on anastomotic healing in the rat. J Surg Res. 1991;50:82–87. doi: 10.1016/0022-4804(91)90014-d. [DOI] [PubMed] [Google Scholar]
- 34.Loggie BW, Fleming RA, McQuellon RP, Russell GB, Geisinger KR. Cytoreductive surgery with intraperitoneal hyperthermic chemotherapy for disseminated peritoneal cancer of gastrointestinal origin. Am Surg. 2000;66:561–568. [PubMed] [Google Scholar]
- 35.Fujimoto S, Takahashi M, Kobayashi K, Kasanuki J, Ohkubo H. Heated intraperitoneal mitomycin C infusion treatment for patients with gastric cancer and peritoneal metastasis. Cancer Treat Res. 1996;81:239–245. doi: 10.1007/978-1-4613-1245-1_20. [DOI] [PubMed] [Google Scholar]
- 36.Mohamed F, Sugarbaker PH. Carrier solutions for intraperitoneal chemotherapy. Surg Oncol Clin N Am. 2003;12:813–824. doi: 10.1016/s1055-3207(03)00039-5. [DOI] [PubMed] [Google Scholar]
- 37.Mohamed F, Sugarbaker PH. Intraperitoneal taxanes. Surg Oncol Clin N Am. 2003;12:825–833. doi: 10.1016/s1055-3207(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 38.González-Bayón L, González-Moreno S, Ortega-Pérez G. Safety considerations for operating room personnel during hyperthermic intraoperative intraperitoneal chemotherapy perfusion. Eur J Surg Oncol. 2006;32:619–624. doi: 10.1016/j.ejso.2006.03.019. [DOI] [PubMed] [Google Scholar]