Abstract
A 17-year-old female presented with rectal bleeding from an ulcerated sigmoid mass in 1994. Initial pathological evaluation revealed a rare clear cell neoplasm of the colon, possibly originating from kidneys, adrenals, lung or a gynecologic source as a metastatic lesion. Extensive imaging studies were negative, and over the next 15 years, she remained well with no recurrence. The original resected neoplasm was reviewed and re-classified as a perivascular epithelioid cell neoplasm (PEComa). Although the long-term natural history of PEComas requires definition, increased clinical and pathological awareness should lead to increased recognition of an apparently rare type of colonic neoplasm that likely occurs more often than is currently appreciated.
Keywords: Perivascular epithelioid cell neoplasm, Carcinoid tumor, Colonic adenocarcinoma, Clear cell tumor
INTRODUCTION
Clear cell tumors were historically described as benign and malignant neoplasms consisting of cells with clear cytoplasm characteristic of kidneys and adrenal glands[1]. Later, it was appreciated that these clear cell neoplasms might develop in a variety of other sites in addition to the kidneys, including tissues originating from the developing mullerian ductal system[2]: ovaries, extra-ovarian endometriosis, uterine cervix, upper vagina or lower genital tract. Detailed pathological descriptions of clear cell tumors in the lung were also reported (clear cell “sugar tumors”)[3]. Finally, cytoplasmic clearing was detected in other neoplasms (e.g. myoepithelial neoplasia in major salivary glands, squamous cell carcinoma, chordomas), and focally in neoplastic epithelium of colorectal adenomas, likely reflecting cytoplasmic glycogen or lipid[4].
Clear cell tumor in the colon was initially reported in 1964 by Hellstrom and Fisher because the neoplastic clear cells resembled the physaliferous (clear) cells of chordomas[5]. Since then, these colonic tumors have been described, largely in males and usually on the left side of the colon[2]. In 1988, the Canadian experience in these clear cell tumors emphasized their rarity being limited to a single report of 4 cases accessed from the National Canadian Tumor Reference Centre in Ottawa[1]. Some cases have also appeared in the literature described as metastatic clear cell carcinomas with a focus from other organs, including renal or ovarian sites[6]. Rarely, concomitant renal and colonic clear cell carcinomas were also noted[7]. Due to the limited number of reported cases, however, the natural history and long-term prognosis of this colonic neoplasm has not been determined.
In 1992, Bonetti et al[8] analyzed the the shared pathological features of angiolipomas and clear cell “sugar” tumors of the lung: In 2002, the World Health Organization officially recognized this family of neoplasms derived from these distinctive cells as perivascular epithelioid cell neoplasms (PEComas)[9]. The family included: adenomyoepithelioma (AML), lymphangioleiomyomatosis (LAM), clear cell sugar tumor of the lung, clear cell myomelanocytic tumor of the falciform ligament and generic PEComas in a variety of sites, including the uterus, soft tissue, and rarely the intestinal tract[10-15]. An association was also described between tuberous sclerosis, AML and LAM[16].
The present report describes the pathological and histochemical features of a clear cell neoplasm of the colon, later re-classified as a PEComa, and notes an entirely benign clinical course extending over more than a decade with detailed clinical and endoscopic monitoring after a localized colonic resection.
CASE REPORT
A 33-year-old female was referred in 2009 for colonoscopic evaluation because of a past history of a resected sigmoid neoplasm in 1994. Her colonoscopy was normal with a well-healed anastomosis. Because of her age, however, her clinical history and the pathology of her previously resected tumor were re-evaluated. In addition, as part of this review, added pathological studies on the original stored paraffin blocks were done.
Clinical background
At the age of 17 years, she presented with an emergent rectal bleeding event and a hemoglobin of 90 g/L. Endoscopic evaluation showed an ulcerated polypoid lesion in the sigmoid colon suggestive of a possible carcinoid tumor. No transfusions were given. A sigmoid resection was performed for a tumor estimated to have a diameter of 4-6 cm showing features of a “clear cell” tumor of the colon. Later clinical evaluation and blood tests were normal. In particular, there was no evidence for tuberous sclerosis or other disorders. Computed tomography scanning of her chest, abdomen and pelvis were done to exclude metastatic disease from other possible primary clear cell neoplasms (e.g. renal cell or adrenal cell carcinoma) and the scanning was normal. Subsequent colonoscopies in 1997, 2000, 2003 and 2006 showed a well-healed anastomosis, but no other findings.
Pathological studies
Pathological review confirmed an unusual clear cell tumor composed of discrete rounded collections of clear cells in a fine vascular stroma with centrally placed low-grade nuclei (Figures 1 and 2). The mitotic rate was low. The tumor was well delimited but was unencapsulated. Intramucosal invasion was present but there was no invasion of the muscularis propria. There were no nodal metastases. The tumor appeared to arise in the submucosa of the colon and extended to the mucosal surface with ulceration. Initial pathological differential diagnosis were: metastatic clear cell carcinoma of the kidney or adrenal gland; clear cell variant of a primary colorectal carcinoma or carcinoid tumor; a paraganglioma variant; a clear cell variant of a smooth muscle tumor or gastrointestinal stromal tumor.
Figure 1.
Perivascular epithelioid cell neoplasm (PEComa). A: PEComa in sigmoid colon site (HE, × 12.5); B: PEComa in sigmoid colon showing mucosal ulceration (HE, × 12.5); C: PEComa with individual cell nests invading mucosa (HE, × 100).
Figure 2.
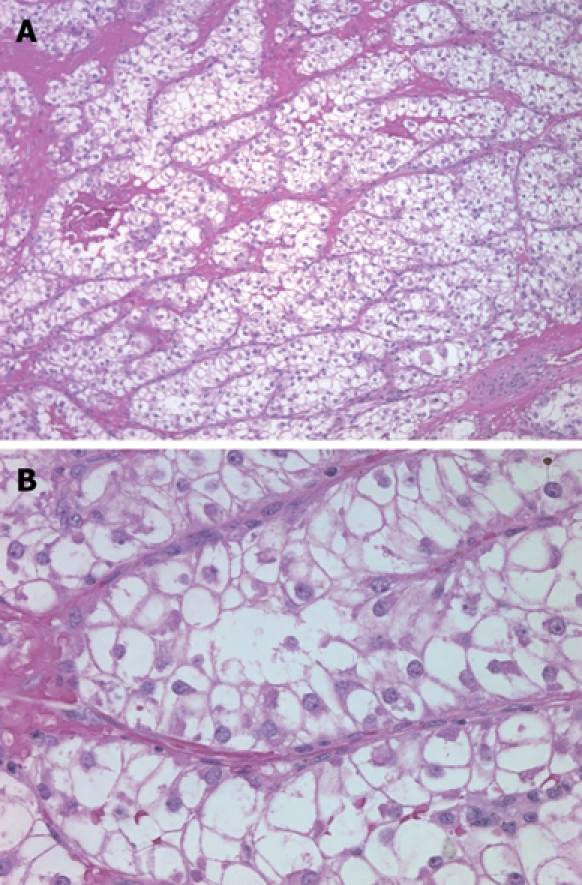
PEComa tumor body. A: PEComa tumor body with intervening delicate capillary network (HE, × 100); B: PEComa, tumor body (HE, × 400).
Special studies
The previous paraffin blocks from the resected tumor were recovered, reviewed and added special studies were done. All neuroendocrine markers that were initially negative were repeated and were again negative. These included neuron-specific enolase, synaptophysin, chromogranin and CD-56. Initial electron microscopy was not repeated, however, this did not reveal evidence of melanosomes or intercellular junctions and a cell of origin could not be defined. Histochemical staining for neurosecretory granules was negative by argyrophil and Fontessa-Masson methods, and the cells were also negative for mucin (mucicarmine). The cells were negative using a multimolecular weight pan-keratin cocktail antibody and did not express cytokeratin-7 or cytokeratin-20. Cells did not express c-kit (CD-117), desmin, smooth muscle actin, muscle specific actin, CD-34 or vimentin. The tumor cells were negative for S-100, but were strongly positive for HMB-45 (Figure 3). Based on this re-evaluation of the original stored tissue blocks, the colonic neoplasm was re-classified as a PEComa of the colorectum, or PEComa.
Figure 3.
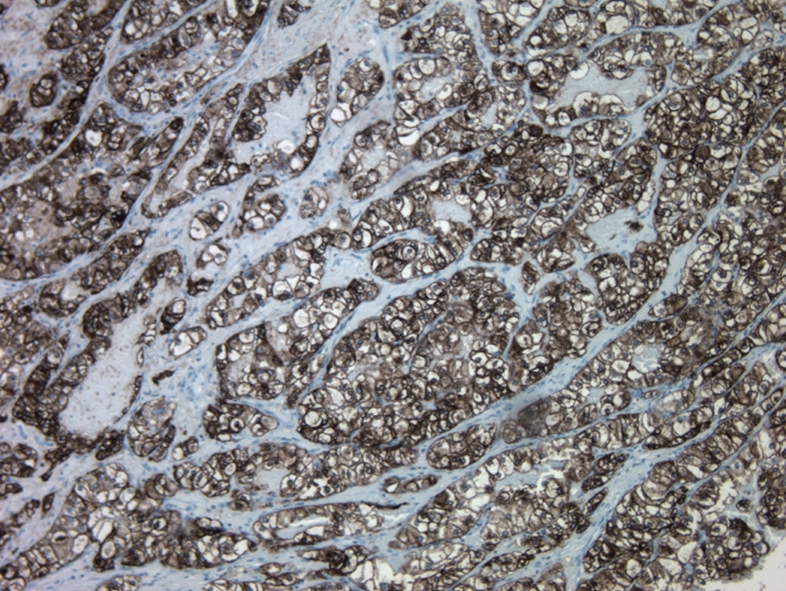
PEComa with HMB-45 antibody strongly stained cytoplasm of neoplastic cells (HMB-45, × 100).
DISCUSSION
PEComas are rare tumors characterized by myomelanocytic differentiation. To date, the precursor lesion or cell of origin has not been identified. Intestinal PEComas, and specifically, colonic PEComas have been rarely described in only a few case reports that detail the morphologic and immunohistochemical features[16-23]. The precise incidence of these neoplasms is not known, but some have estimated these to occur in less than 0.1% of colon neoplasms[4]. In part, this low rate currently reflects different factors that may result in increased recognition in the future. As in the present case, earlier evaluation of some clear cell tumors may not have been conclusive, or the pathological studies may not have permitted final classification. Likely, an increased awareness among gastroenterologists and pathologists will result in increased recognition in the intestinal tract as these are likely to occur more often than is currently recognized.
The biological behavior of the PEComa family is still not very well understood. Clinically benign, but concomitant nodal involvement with angiomyolipomas may have represented multifocal, rather than metastatic disease[6,7]. Histologic criteria indicative of malignancy in PEComas have not been proven, in part, because information on the long-term natural history of intestinal lesions has not been reported. It does appear, however, that non-gastrointestinal PEComas with definite evidence of malignant behavior are usually large (over 5 cm), contain areas of coagulative necrosis and also have a high mitotic rate. Other important criteria that have been suggested include: an infiltrative tumor border, high nuclear grade and cellularity, and vascular invasion. For intestinal lesions, the reported length of follow-up has been usually short (as with most case reports) and the outcome data are very limited. In a recent review[23], the longest duration of follow-up for a colonic PEComa was 24 mo. In the present case, the PEComa (initially defined as a clear cell tumor of the sigmoid colon) appeared to be completely resected. However, added imaging studies were performed to ensure that another primary site (e.g. kidney, lung) was not evident and further endoscopic follow-up has confirmed an entirely benign clinical course with no recurrence over a period of more than 15 years. Added histopathological studies with larger numbers of cases will be needed to further define the long- term natural history of this disorder.
Footnotes
Peer reviewer: Nadia Peparini, MD, PhD, Department of General Surgery “Francesco Durante”, La Sapienza University, Viale del Policlinico,155, Rome 00161, Italy
S- Editor Wang JL L- Editor Ma JY E- Editor Zheng XM
References
- 1.Jewell LD, Barr JR, McCaughey WT, Nguyen GK, Owen DA. Clear-cell epithelial neoplasms of the large intestine. Arch Pathol Lab Med. 1988;112:197–199. [PubMed] [Google Scholar]
- 2.Soga K, Konishi H, Tatsumi N, Konishi C, Nakano K, Wakabayashi N, Mitsufuji S, Kataoka K, Okanoue T, Mukaisho K, et al. Clear cell adenocarcinoma of the colon: a case report and review of literature. World J Gastroenterol. 2008;14:1137–1140. doi: 10.3748/wjg.14.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaffey MJ, Mills SE, Zarbo RJ, Weiss LM, Gown AM. Clear cell tumor of the lung. Immunohistochemical and ultrastructural evidence of melanogenesis. Am J Surg Pathol. 1991;15:644–653. doi: 10.1097/00000478-199107000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Domoto H, Terahata S, Senoh A, Sato K, Aida S, Tamai S. Clear cell change in colorectal adenomas: its incidence and histological characteristics. Histopathology. 1999;34:250–256. doi: 10.1046/j.1365-2559.1999.00598.x. [DOI] [PubMed] [Google Scholar]
- 5.Hellstrom HR, Fisher ER. Physaliferous variant of carcinoma of colon. Cancer. 1964;17:259–263. doi: 10.1002/1097-0142(196402)17:2<259::aid-cncr2820170217>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 6.Medina Pérez M, Valero Puerta JA, Valpuesta Fernández I, Pérez Fernández D, Sánchez González M. [Renal carcinoma with intranuclear inclusions associated with colon carcinoma] Arch Esp Urol. 2000;53:79–81. [PubMed] [Google Scholar]
- 7.D'Amato A, Nigri G, Pronio A, Montesani C, Ferrazza G, Rusignolo A, Solinas S, Ribotta G. [The use of autotransfusion in general surgery] Ann Ital Chir. 2000;71:643–647; discussion 647-648. [PubMed] [Google Scholar]
- 8.Bonetti F, Pea M, Martignoni G, Zamboni G. PEC and sugar. Am J Surg Pathol. 1992;16:307–308. doi: 10.1097/00000478-199203000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Folpe AL. Neoplasms with perivascular epithelioid cell differentiation (PEComas) In: Fletcher CDM, Unni KK, Mertens F, editors. World Health Organization classification of tumors. Pathology and genetics of tumors of soft tissue and bone. Lyon: IARC Press; 2002. pp. 221–222. [Google Scholar]
- 10.Fröhlich T, Brands A, Thon WF, Weskott HP, Ostertag H. Angiomyolipoma of the kidney and lymph nodes. World J Urol. 1999;17:123–125. doi: 10.1007/s003450050117. [DOI] [PubMed] [Google Scholar]
- 11.Prasad ML, Keating JP, Teoh HH, McCarthy SW, Battifora H, Wasef E, Rosai J. Pleomorphic Angiomyolipoma of Digestive Tract: A Heretofore Unrecognized Entity. Int J Surg Pathol. 2000;8:67–72. doi: 10.1177/106689690000800112. [DOI] [PubMed] [Google Scholar]
- 12.Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol. 2005;29:1558–1575. doi: 10.1097/01.pas.0000173232.22117.37. [DOI] [PubMed] [Google Scholar]
- 13.Ferry JA, Malt RA, Young RH. Renal angiomyolipoma with sarcomatous transformation and pulmonary metastases. Am J Surg Pathol. 1991;15:1083–1088. doi: 10.1097/00000478-199111000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Cibas ES, Goss GA, Kulke MH, Demetri GD, Fletcher CD. Malignant epithelioid angiomyolipoma ('sarcoma ex angiomyolipoma') of the kidney: a case report and review of the literature. Am J Surg Pathol. 2001;25:121–126. doi: 10.1097/00000478-200101000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Hornick JL, Fletcher CD. PEComa: what do we know so far? Histopathology. 2006;48:75–82. doi: 10.1111/j.1365-2559.2005.02316.x. [DOI] [PubMed] [Google Scholar]
- 16.Baek JH, Chung MG, Jung DH, Oh JH. Perivascular epithelioid cell tumor (PEComa) in the transverse colon of an adolescent: a case report. Tumori. 2007;93:106–108. doi: 10.1177/030089160709300120. [DOI] [PubMed] [Google Scholar]
- 17.Birkhaeuser F, Ackermann C, Flueckiger T, Guenin MO, Kern B, Tondelli P, Peterli R. First description of a PEComa (perivascular epithelioid cell tumor) of the colon: report of a case and review of the literature. Dis Colon Rectum. 2004;47:1734–1737. doi: 10.1007/s10350-004-0637-5. [DOI] [PubMed] [Google Scholar]
- 18.Bonetti F, Martignoni G, Colato C, Manfrin E, Gambacorta M, Faleri M, Bacchi C, Sin VC, Wong NL, Coady M, et al. Abdominopelvic sarcoma of perivascular epithelioid cells. Report of four cases in young women, one with tuberous sclerosis. Mod Pathol. 2001;14:563–568. doi: 10.1038/modpathol.3880351. [DOI] [PubMed] [Google Scholar]
- 19.Evert M, Wardelmann E, Nestler G, Schulz HU, Roessner A, Röcken C. Abdominopelvic perivascular epithelioid cell sarcoma (malignant PEComa) mimicking gastrointestinal stromal tumour of the rectum. Histopathology. 2005;46:115–117. doi: 10.1111/j.1365-2559.2005.01991.x. [DOI] [PubMed] [Google Scholar]
- 20.Pisharody U, Craver RD, Brown RF, Gardner R, Schmidt-Sommerfeld E. Metastatic perivascular epithelioid cell tumor of the colon in a child. J Pediatr Gastroenterol Nutr. 2008;46:598–601. doi: 10.1097/MPG.0b013e318148b65c. [DOI] [PubMed] [Google Scholar]
- 21.Tazelaar HD, Batts KP, Srigley JR. Primary extrapulmonary sugar tumor (PEST): a report of four cases. Mod Pathol. 2001;14:615–622. doi: 10.1038/modpathol.3880360. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto H, Oda Y, Yao T, Oiwa T, Kobayashi C, Tamiya S, Kawaguchi K, Hino O, Tsuneyoshi M. Malignant perivascular epithelioid cell tumor of the colon: report of a case with molecular analysis. Pathol Int. 2006;56:46–50. doi: 10.1111/j.1440-1827.2006.01917.x. [DOI] [PubMed] [Google Scholar]
- 23.Ryan P, Nguyen VH, Gholoum S, Carpineta L, Abish S, Ahmed NN, Laberge JM, Riddell RH. Polypoid PEComa in the rectum of a 15-year-old girl: case report and review of PEComa in the gastrointestinal tract. Am J Surg Pathol. 2009;33:475–482. doi: 10.1097/PAS.0b013e31819003d1. [DOI] [PubMed] [Google Scholar]



