Abstract
The advent of minimally invasive surgery and the advances in endoluminal flexible endoscopy have converged to generate a new concept in digestive surgery, whose acronym natural orifice transluminal endoscopic surgery (NOTES), has become a familiar term in the surgical community. NOTES has been performed through the mouth, the bladder, the rectum and the vagina. Of these four approaches, the vagina has gained most popularity for several reasons. It is not only readily accessible and easy to decontaminate but it also provides safe entry and simple closure. The transvaginal approach has been described in the experimental and the clinical setting as an option for cholecystectomy, nephrectomy, splenectomy, segmental gastrectomy, retroperitoneal exploration and bariatric surgery. However, larger series are needed to delineate the exact risks of this approach, and to transcend cultural barriers that impede its wider introduction. Prospective randomized trials will shed light on the definitive role of the vaginal approach in minimal invasive surgery of the future.
Keywords: Transvaginal approach, Cholecystectomy, Nephrectomy, Splenectomy, Segmental gastrectomy, Retroperitoneal exploration, Natural orifice transluminal endoscopic surgery, Bariatric surgery
INTRODUCTION
The advent of minimally invasive surgery and the advances in endoluminal flexible endoscopy have converged to generate a new concept in digestive surgery in which the wall of a hollow organ is trespassed to gain access to the peritoneal cavity. This new approach, whose acronym natural orifice transluminal endoscopic surgery (NOTES) has become a familiar term in the surgical community, aims to reduce the effects and consequences of surgical trauma to a minimum. Since it was first defined by Kalloo et al[1] in 2004, it has attracted tremendous interest from surgeons and flexible endoscopists all around the world[2,3]. NOTES surgery poses many conceptual, physical and technical challenges that were thoroughly assessed in a “white paper” published in 2006[4]. The most complex technical issues related to NOTES are access closure and the risk of microbial contamination. NOTES has been performed through the mouth, urinary bladder, rectum and vagina. Of these four approaches, the vagina has gained most popularity for several reasons. It is not only readily accessible and easy to decontaminate but it also provides safe entry and simple closure[5]. The aim of this paper is to describe the anatomical and technical considerations associated with this surgical procedure, and provide an overview of experimental and clinical evidence collected to date.
ANATOMIC BASIS
The transvaginal approach to the peritoneal cavity for diagnostic or therapeutic purposes is not new in the field of gynecology. It was named “ventroscopy” by Ott in 1901, culdoscopy by Decker and Cherry (1944) or colpolaparoscopy by Klaften (1948)[6]. Transvaginal hysterectomy has been performed successfully for many years. In 1998, Tsin[6] described his experience with operative colpolaparoscopy for appendectomies and cholecystectomies. The vagina has also been used for years to retrieve organs such as the spleen or the kidney[7,8] after laparoscopic dissection, so as to avoid a minilaparotomy or trocar site enlargement.
The anatomical basis for the transvaginal approach is the wide posterior fundus of the vagina formed as a result of the anteversion position of the uterus[9]. The vaginal pouch is bounded by the posterior vaginal wall, the sacrouterine ligaments and the anterior rectum wall, and it forms the floor of the Douglas pouch (Figures 1 and 2). The fundus of the vagina is 3-4 cm wide. As it is not adherent to the anterior face of the rectum and has no interposed organ or anatomical structure, it allows direct entry to the peritoneum.
Figure 1.
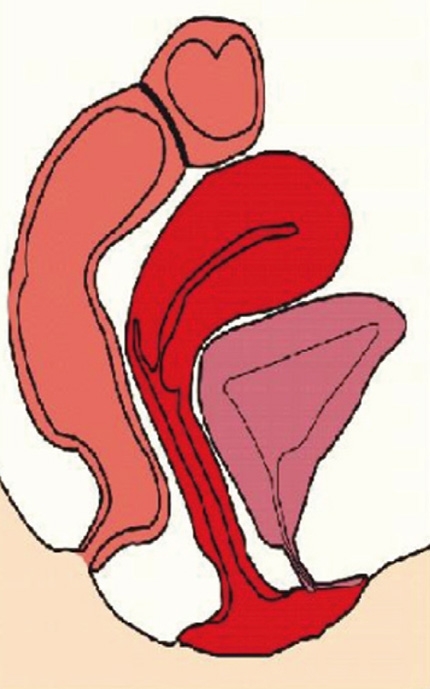
Sagital view of the female pelvis showing the shape and location of the vaginal fundus that delineate the floor of the Douglas pouch.
Figure 2.
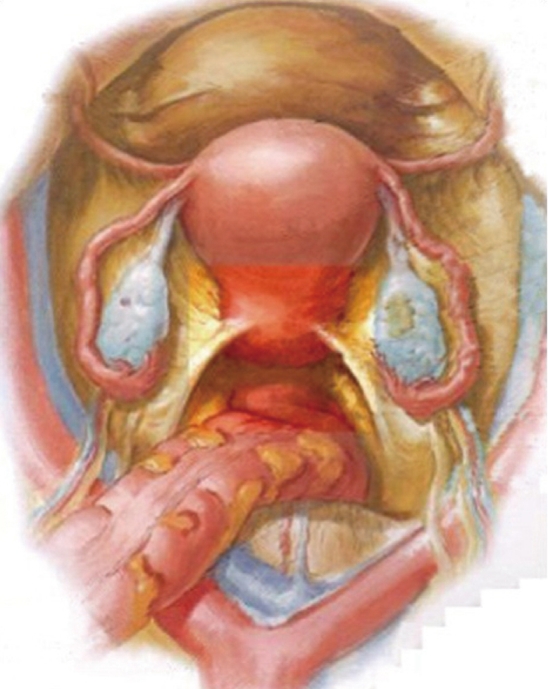
Draft of the deep pelvis and the Douglas pouch showing the free zone for transvaginal access to the peritoneal cavity.
TRANSVAGINAL APPROACH
Technique
Colpotomy is a common, standardized and consolidated approach in gynecology. It is used to remove not only gynecologic lesions but also non-gynecological organs in mini-invasive general surgery. For this procedure, the patient is placed in dorsal decubitus with the legs in stirrups, in the Lloyd-Davies position. Antithrombotic prophylaxis is administered together with a single dose of antibiotic prophylaxis. A nasogastric tube and a Foley catheter are used under general orotracheal anesthesia. A bimanual gynecologic examination is recommendable to rule out masses or adherences. After bladder catheterization, the vagina is decontaminated with betadine. The presence of a gynecologist is recommended when initially gaining experience with the technique. The colpotomy can be performed blindly without transumbilical laparoscopic control, or under laparoscopic control. If entry is blind, the patient is placed in the Trendelenburg position to reduce the risk of injuring the small bowel while gaining access to the abdominal cavity. The posterior fundus is then grasped two cm below the cervix and a sharp or electric scalpel is used to perform a colpotomy to reach the abdominal cavity. This procedure is only applicable for pure NOTES. For safety reasons, entry through the vagina is usually performed under transumbilical laparoscopic control. In this case, after exploratory laparoscopy to rule out adhesions or an impracticable Douglas pouch, entry is gained by sharp dissection or using a conventional laparoscopic trocar (12 mm of diameter), either with or without blades.
Contraindications
There are a number of potential contraindications and when transvaginal surgery is proposed, the patient should be clearly and fully informed and asked to sign a consent form. A preoperative gynecologic examination is recommended. Clinical contraindications are active infections, pregnancy or cervical cancer. Technical difficulties may be encountered in the case of previous gynecologic surgery, gynecologic infections, or previous inflammatory digestive diseases such as inflammatory bowed disease, diverticulitis or appendiceal peritonitis. In such cases a previous laparoscopy should be carried out. The presence of endometriosis should also be ruled out as this could shrink the rectovaginal wall or the Douglas pouch. Another point to consider is the practice of transvaginal surgery in a young nulliparous patient as the impact of transvaginal surgery on fertility is not yet known. A practical safeguard therefore is to offer this surgery only to postmenopausal women or patients who no longer want to have children.
Potential complications
The transvaginal approach appears to be safe. Potential complications with the transvaginal approach would logically resemble those of transvaginal hysterectomy and fertiloscopy. Figures show that there seems to be less pain after transvaginal hysterectomy than after open hysterectomy. Nassif et al[10] found that the incidence of infection after transvaginal hysterectomy was as low as 3.9%, and less than 0.1% after fertiloscopy. Dyspareunia is reported in 2% of cases after the operation and normally improves with time in 81% of cases, leading to an overall incidence around 0.2% at distance from surgery. Rectal injury is estimated to be about 0.2%.
Other complications may arise from postoperative bleeding or chronic infection of the wound. Additional theoretical morbidity may be related to infertility. However, no adverse effects were found in a 12-mo follow up of a combined series of 70 patients who underwent transvaginal cholecystectomy[11,12].
Types of transvaginal NOTES
“Totally”, “Pure” or “True” NOTES refer to procedures performed only with transluminally placed flexible or rigid tools, without laparoscopic assistance to gain access to the abdominal cavity. With currently available instruments these techniques imply a high degree of difficulty and they have been performed in very few cases to date.
The term “Hybrid” NOTES is used to describe procedures that involve any type of transabdominal assistance. Hybrid NOTES can be divided into 2 categories: NOTES-assisted laparoscopy and Lap-assisted NOTES. In the former, most of the operation is conducted using transabdominal instruments while in the second category surgery is mainly transluminal but includes transabdominal assistance[13,14].
Transvaginal NOTES: Current experimental and clinical uses
Cholecystectomy[11-35]: Over a few months, starting in 2007, several groups around the world reported successful performance of transvaginal cholecystectomies performed either fully endoscopically with minimal laparoscopic assistance for retraction and clip application[15-17] or NOTES assisted in which dissection was performed with laparoscopic tools[18,19].
More than 214 cholecystectomies have since then been published using transvaginal NOTES[11-35], Table 1.
Table 1.
Transvaginal NOTES procedures reported to date
| Author | Year | NOTES | NO. of patients | Operation |
| Pugliese | 2009 | Hybrid | 18 | Cholecystectomy |
| DeCarli | 2009 | Hybrid | 12 | Cholecystectomy |
| Gumbs | 2009 | Hybrid (3)/Pure (1) | 4 | Cholecystectomy |
| Zornig | 2009 | Hybrid | 68 | Cholecystectomy |
| Seven | 2009 | Hybrid | 2 | Cholecystectomy |
| Castro-Perez | 2009 | Hybrid | 7 | Cholecystectomy |
| Horgan | 2009 | Hybrid | 9 | Cholecystectomy |
| Horgan | 2009 | Hybrid | 1 | Cholecystectomy |
| Horgan | 2009 | Hybrid | 1 | Appendectomy |
| Targarona | 2009 | Hybrid | 1 | Splenectomy |
| Tabutsadze | 2009 | Hybrid | 2 | Appendectomy |
| Nakajima | 2009 | Hybrid | 2 | Partial Gastrectomy |
| De Sousa | 2009 | Pure | 4 | Cholecystectomy |
| Navarra | 2009 | Hybrid | 6 | Cholecystectomy |
| Noguera | 2009 | Hybrid | 15 | Cholecystectomy |
| Noguera | 2009 | Hybrid | 1 | Liver Resection |
| Palanivelu | 2009 | Hybrid | 6 | Cholecystectomy |
| Cardoso Ramos | 2008 | Hybrid | 4 | Sleeve Gastrectomy |
| Cardoso Ramos | 2008 | Hybrid | 32 | Cholecystectomy |
| Zorrón | 2008 | Pure | 1 | Cancer Diagnostic Staging |
| DeCarli | 2008 | Hybrid | 1 | Cholecystectomy |
| Lacy | 2008 | Hybrid | 1 | Sigmoidectomy |
| Palanivelu | 2008 | Hybrid (2)/Pure (1) | 3 | Appendectomy |
| Branco Filho | 2007 | Hybrid | 1 | Cholecystectomy |
| Dolz | 2007 | Hybrid | 1 | Cholecystectomy |
| Zornig | 2007 | Hybrid | 20 | Cholecystectomy |
| Forgione | 2007 | Hybrid | 3 | Cholecystectomy |
| Marescaux | 2007 | Hybrid | 1 | Cholecystectomy |
| Bessler | 2007 | Hybrid | 1 | Cholecystectomy |
| Zorrón | 2007 | Hybrid | 1 | Cholecystectomy |
NOTES: Natural orifice transluminal endoscopic surgery.
Five cases were carried out using pure NOTES techniques, while the others were hybrid procedures. During the hybrid procedure, the vaginal access is used for visualization and to perform part of the operation by means of endoscopic maneuvers, whilst exposure, clipping and dissection of the gallbladder is done using different technical options, such as transumbilical or transparietal access or by adding additional rigid or articulated instruments through the vagina.
The pure NOTES operations were performed by only two authors. Gumbs et al[34] reported a case in which they performed colpotomy and then introduced a trocar under direct vision into the abdominal cavity. A 15-mm port was then established through the colpotomy, and this was also used to create the pneumoperitoneum. A double channel gastroscope was introduced through the 15-mm port. An extra 5-mm port was placed beside the 15-mm port to allow placement of a reticulating retractor. Calot’s triangle structures were dissected by means of the double channel endoscope. The cystic duct and artery were clipped endoscopically and the gallbladder was removed through the vagina. The colpotomy was then closed with absorbable suture. de Sousa et al[35] published 4 totally NOTES transvaginal cholecystectomies, performing posterior colpotomy under direct visualization. A single channel gastroscope with the insufflation tube attached was inserted through the vagina. A double channel colonoscope was placed next to the gastroscope. One endoscope was used for retraction and insufflation. Calot’s triangle was dissected using endoscopic instruments such as hot-biopsy forceps, polypectomy snare, and endoscopic hook. The cystic duct and artery were clipped endoscopically. The gallbladder was retrieved through the colpotomy which was then closed with absorbable suture. Other authors have performed hybrid procedures, assisted by means of different laparoscopic instruments.
Appendectomy[36-38]: Six appendectomies have been performed using this novel approach. Palanivelu et al[36] reported two hybrid transvaginal NOTES appendectomies and one pure transvaginal NOTES appendectomy. Pneumoperitoneum was achieved by means of a Veress needle in the umbilicus. A 3-mm port was placed through the umbilicus to receive a laparoscope in the first two cases. Colpotomy was made under laparoscopic guidance in the first two patients, and a double channel endoscope was then introduced into the cavity. The left working channel was used to provide traction while the right channel allowed dissection and closure of the appendix base with an endoloop. The specimen was removed through the colpotomy which was then closed with absorbable suture. The operative time was 103.5 min. Two patients complained of postoperative vaginal discomfort, but extra analgesics were not needed. The hospital stay was 48 h. Intraoperative hemorrhage from the appendicular artery was reported but was controlled endoscopically. Tabutsadze et al[37] published two transvaginal NOTES appendectomies and Horgan et al[38] performed one hybrid transvaginal NOTES appendectomy. The operative time averaged 78 min and hospital stay was 24 h. No complications were reported.
Sigmoidectomy and right colectomy[39,40]: A hybrid NOTES transvaginal sigmoidectomy has been reported[39]. A needle scope in the right lower quadrant allowed insufflation with CO2. Colpotomy was made under laparoscopic guidance. A 12 mm port was placed through the colpotomy to insert the flexible endoscope. Two 2-mm ports on the right flank and on the umbilicus were needed for traction. An anal dilator introduced through the rectum improved exposure of the surgical area. The inferior mesenteric pedicle was dissected and then transected with a 45-mm Endo GIA stapler introduced through the vagina. After sigmoid mobilization, a 45-mm Endo GIA stapler was introduced through the vagina and the upper rectum was sectioned. The specimen was extracted through the vagina. The proximal colon section was severed, a purse-string suture was applied, and a circular stapling anvil was inserted into the proximal end of the colon. The proximal colon was then reintroduced into the abdominal cavity. A 31-mm circular stapler was placed transanally to perform the anastomosis. Colpotomy was closed with absorbable suture. Histological diagnosis was adenocarcinoma. The operative time was 150 min. Minimal postoperative pain responded to oral paracetamol and ketoprofene in usual doses. The hospital stay was 96 h and no complications were reported.
A hybrid transvaginal assisted right colectomy has been described by Burghardt in 2008[40].
Cancer diagnostic staging[41]: A totally NOTES transvaginal abdominal exploration was performed to obtain histological diagnosis and tumor staging. Colpotomy was performed under direct vision. A flexible double channel colonoscope was introduced through the vagina and pneumoperitoneum was established through the smallest working channel. Sixteen biopsies were taken. The colpotomy was closed using absorbable suture. The operative time was 105 min, post-surgical analgesia was not required and hospital stay was 48 h. No complications were reported.
Liver resection[42]: A transvaginal hybrid NOTES liver resection was described. Pneumoperitoneum was achieved through a Veress needle in the umbilicus, where a 5-mm trocar was located. A 3-mm trocar was inserted in the right upper quadrant. A 12-mm trocar was placed transvaginally to receive the single channel video gastroscope. The cystic duct and artery were clipped and sectioned. Cholecystectomy was performed with electrocautery. The liver transection required the use of a harmonic scalpel and tissue sealing was achieved with radiofrequency energy. The specimen was inserted into an endobag and extracted transvaginally. The colpotomy was closed with absorbable suture. The histological diagnosis was atypical adenoma. The operative time was 110 min and hospital stay was 48 h. No complications were reported.
Partial gastrectomy[43]: Two transvaginal hybrid NOTES partial gastrectomies have been performed. A pneumoperitoneum was created through the 10 mm port introduced transumbilically. An additional port was needed in the left midabdomen. Colpotomy was carried out through a single puncture with a 12-mm port under laparoscopic vision. A flexible endoscope was introduced through the port in the colpotomy. A second flexible endoscope was advanced transorally into the stomach to determine the localization of the tumor. Once transvaginal gastric mobilization was achieved, the transvaginal endoscope was changed for a linear stapling device which was used to perform a partial gastrectomy, under laparoscopic guidance. The specimen was extracted transvaginally protected in an endobag. The colpotomy was closed with absorbable suture. Analysis of the specimen showed a hemorrhagic lipoma in one case and a gastrointestinal stromal tumor in the other. Operative time was 365 min for the former and 170 min in the latter case. Analgesia was not required. The hospital stay was 120 h in both cases and no complications were observed.
Sleeve gastrectomy[44]: Four transvaginal hybrid NOTES Sleeve Gastrectomies have been reported in the literature so far. Pneumoperitoneum was made through a Veress needle in the umbilicus. A 10-mm port was then inserted and the laparoscope was introduced. Under laparoscopic vision, a 12-mm transvaginal port was placed. A further 5 mm port and a further 2 mm port were placed in the right upper quadrant and in the left upper quadrant, respectively. The stomach was mobilized using a harmonic scalpel and was calibrated with a 36F bougie. Using linear staplers, the sleeve was performed from the mid-antrum to the angle of his. The staple line was then reinforced with suture. The stomach was extracted transvaginally. The colpotomy was closed with absorbable suture and the total operative time was 95 min. One patient required further analgesic treatment on the second postoperative day. Hospital stay was 48 h and no complications were reported.
Splenectomy[45]: Two transvaginal hybrid NOTES splenectomies have been reported so far. Patients were placed in right decubitus with the left leg in stirrups. The table was flexed at the flank. A pneumoperitoneum was made via a Veress needle. A 5-mm port was placed at the anterior axillary line and two 3 mm ports were positioned at the subxyphoid area and the posterior axillary line, respectively. Colpotomy was established in the left vaginal cul-de-sac, and a 15-mm trocar was introduced (Figure 3). This trocar was used for visualization via a colonoscope. Splenic mobilization was achieved through the transabdominal ports using a 5-mm harmonic scalpel. The splenic pedicle was stapled under laparoscopic guidance by using a linear stapler introduced through the vagina. The specimen was extracted transvaginally in an endobag. Colpotomy was closed with absorbable suture. The operative time was 180 min and no complications were reported.
Figure 3.
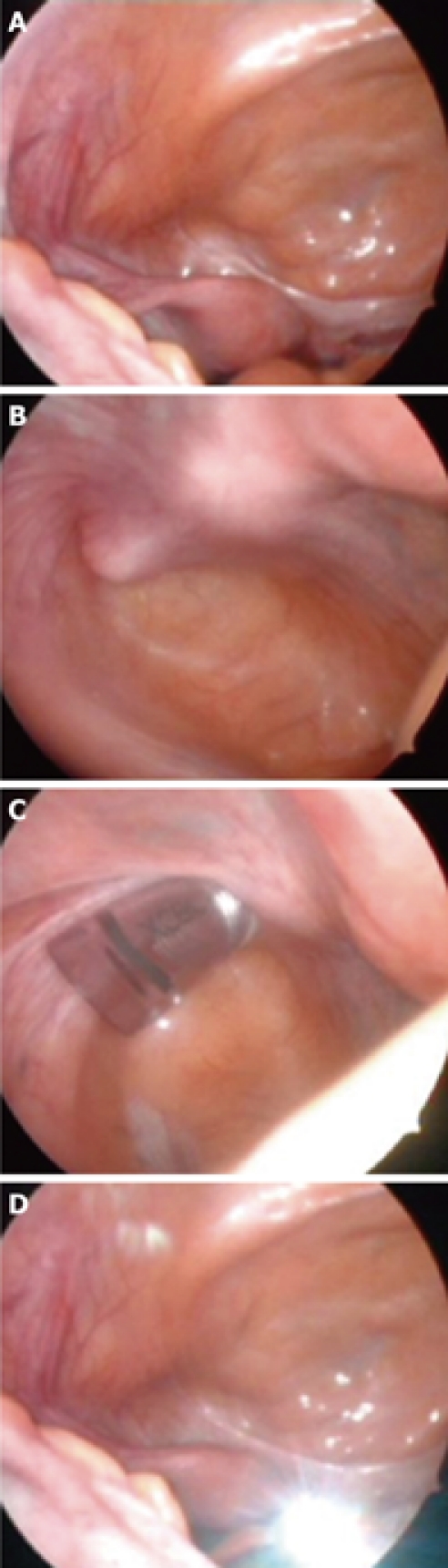
Images corresponding to the transvaginal access to the pelvis with the patient located in full lateral position, used for the transvaginal splenectomy. A: Intraoperative view of the Douglas pouch with the patient placed in full lateratl decubitus; B and C: Insertion of the trocar trough the lateral fundus of the posterior vaginal vault; D: Introduction to the scope ascending to the left hypochondrium.
Urological surgery and retroperitoneal exploration: In an experimental setting, Allemann et al[46-49] approached the retroperitoneal space through the lateral wall of the vagina and this access allowed visualization of the retroperitoneal structures. Removal of the adrenal gland, kidney and pancreatic tail was feasible, and lymph node sampling was also achieved[46-49].
Urological surgery constitutes an emerging area of interest for transvaginal access. Pure NOTES and NOTES-assisted radical nephrectomies have been described and the outcome has been good both in the experimental and the clinical setting[47,50-55].
Other indications: Lomanto et al[56] has recently proposed the experimental possibility of repairing abdominal wall hernias using transvaginal placement and fixation of a mesh.
PERCEPTION OF TRANSVAGINAL NOTES
Several surveys have been conducted to evaluate the perception of surgeons, gynecologists and female patients concerning the procedure[57-61].
From a general point of view, findings show that women accept this procedure if they are assured it is as safe and painless as conventional laparoscopic surgery and will be performed by a surgeon who is skilled in the technique. There are some clearly age-related factors that play an important role in a patient’s decision-making: nulliparous and younger women express concerns regarding sexual function, fertility and cosmesis, whilst postmenopausal women or women who do not want further children are more disposed to accept this type of surgery[58,59].
The surveys found that the major concern for the total group of women was infection. Like women, surgeons and gynecologists are influenced by patient age but their most important concern was the increased risk of procedure-related complications[60,61].
These findings suggest that as more evidence regarding safety emerges, the transvaginal route for NOTES procedures will be better accepted.
CONCLUSION
Current knowledge and experimental and clinical evidence support the potential advantages of the vagina as a NOTES approach. So far, this route represents the most successful and widely accepted among all the other possible NOTES approaches, and this is due mainly to the relative simplicity of access and closure. Larger series are needed to delineate the exact risks of this approach and to overcome cultural barriers to this concept.
Prospective randomized trials will shed light on the definitive role of the vaginal approach in minimal invasive surgery of the future.
Acknowledgments
The authors thank Carolyn Newey for revising the English text.
Footnotes
Peer reviewer: Theodoros E Pavlidis, MD, PhD, Professor, Department of Surgery, University of Thessaloniki, Hippocration Hospital, A Samothraki 23, Thessaloniki 54248, Greece
S- Editor Li LF L- Editor Hughes D E- Editor Yang C
References
- 1.Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 2.Gee DW, Rattner DW. Natural orifice translumenal endoscopic surgery: current status. Adv Surg. 2009;43:1–12. doi: 10.1016/j.yasu.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Targarona EM. [Transgastric endoscopic surgery: technological delirium or potential advance?] Cir Esp. 2006;80:1–2. doi: 10.1016/s0009-739x(06)70907-1. [DOI] [PubMed] [Google Scholar]
- 4.Rattner D, Kalloo A. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 5.Lomanto D, Chua HC, Myat MM, So J, Shabbir A, Ho L. Microbiological contamination during transgastric and transvaginal endoscopic techniques. J Laparoendosc Adv Surg Tech A. 2009;19:465–469. doi: 10.1089/lap.2009.0007. [DOI] [PubMed] [Google Scholar]
- 6.Tsin DA. Culdolaparoscopy: a preliminary report. JSLS. 2001;5:69–71. [PMC free article] [PubMed] [Google Scholar]
- 7.Zornig C, Emmermann A, von Waldenfels HA, Felixmüller C. [Colpotomy for specimen removal in laparoscopic surgery] Chirurg. 1994;65:883–885. [PubMed] [Google Scholar]
- 8.Ghezzi F, Raio L, Mueller MD, Gyr T, Buttarelli M, Franchi M. Vaginal extraction of pelvic masses following operative laparoscopy. Surg Endosc. 2002;16:1691–1296. doi: 10.1007/s00464-002-9043-z. [DOI] [PubMed] [Google Scholar]
- 9.Moran EA, Gostout CJ. Anatomical considerations for natural orifice translumenal endoscopic surgery. Clin Anat. 2009;22:627–632. doi: 10.1002/ca.20816. [DOI] [PubMed] [Google Scholar]
- 10.Nassif J. Transvaginal access. eats.fr. 2008. Available from: http://www.eats.fr/doi-lt01ennassif004.htm. [Google Scholar]
- 11.Zornig C, Mofid H, Siemssen L, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C. Transvaginal NOTES hybrid cholecystectomy: feasibility results in 68 cases with mid-term follow-up. Endoscopy. 2009;41:391–394. doi: 10.1055/s-0029-1214644. [DOI] [PubMed] [Google Scholar]
- 12.Pugliese R, Forgione A, Sansonna F, Ferrari GC, Di Lernia S, Magistro C. Hybrid NOTES transvaginal cholecystectomy: operative and long-term results after 18 cases. Langenbecks Arch Surg. 2010;395:241–245. doi: 10.1007/s00423-009-0528-2. [DOI] [PubMed] [Google Scholar]
- 13.Chamberlain RS, Sakpal SV. A comprehensive review of single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES) techniques for cholecystectomy. J Gastrointest Surg. 2009;13:1733–1740. doi: 10.1007/s11605-009-0902-y. [DOI] [PubMed] [Google Scholar]
- 14.Sodergren MH, Clark J, Athanasiou T, Teare J, Yang GZ, Darzi A. Natural orifice translumenal endoscopic surgery: critical appraisal of applications in clinical practice. Surg Endosc. 2009;23:680–687. doi: 10.1007/s00464-008-0278-1. [DOI] [PubMed] [Google Scholar]
- 15.Zorrón R, Filgueiras M, Maggioni LC, Pombo L, Lopes Carvalho G, Lacerda Oliveira A. NOTES. Transvaginal cholecystectomy: report of the first case. Surg Innov. 2007;14:279–283. doi: 10.1177/1553350607311090. [DOI] [PubMed] [Google Scholar]
- 16.Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142:823–826; discussion 826-827. doi: 10.1001/archsurg.142.9.823. [DOI] [PubMed] [Google Scholar]
- 17.Forgione A, Maggioni D, Sansonna F, Ferrari C, Di Lernia S, Citterio D, Magistro C, Frigerio L, Pugliese R. Transvaginal endoscopic cholecystectomy in human beings: preliminary results. J Laparoendosc Adv Surg Tech A. 2008;18:345–351. doi: 10.1089/lap.2007.0203. [DOI] [PubMed] [Google Scholar]
- 18.Bessler M, Stevens PD, Milone L, Parikh M, Fowler D. Transvaginal laparoscopically assisted endoscopic cholecystectomy: a hybrid approach to natural orifice surgery. Gastrointest Endosc. 2007;66:1243–1245. doi: 10.1016/j.gie.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 19.Zornig C, Mofid H, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C. Scarless cholecystectomy with combined transvaginal and transumbilical approach in a series of 20 patients. Surg Endosc. 2008;22:1427–1429. doi: 10.1007/s00464-008-9891-2. [DOI] [PubMed] [Google Scholar]
- 20.Dolz C, Noguera JF, Martín A, Vilella A, Cuadrado A. [Transvaginal cholecystectomy (NOTES) combined with minilaparoscopy] Rev Esp Enferm Dig. 2007;99:698–702. doi: 10.4321/s1130-01082007001200004. [DOI] [PubMed] [Google Scholar]
- 21.Branco Filho AJ, Noda RW, Kondo W, Kawahara N, Rangel M, Branco AW. Initial experience with hybrid transvaginal cholecystectomy. Gastrointest Endosc. 2007;66:1245–1248. doi: 10.1016/j.gie.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Decarli L, Zorron R, Branco A, Lima FC, Tang M, Pioneer SR, Zanin I Jr, Schulte AA, Bigolin AV, Gagner M. Natural orifice translumenal endoscopic surgery (NOTES) transvaginal cholecystectomy in a morbidly obese patient. Obes Surg. 2008;18:886–889. doi: 10.1007/s11695-008-9523-x. [DOI] [PubMed] [Google Scholar]
- 23.Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc. 2008;22:542–547. doi: 10.1007/s00464-007-9646-5. [DOI] [PubMed] [Google Scholar]
- 24.Ramos AC, Murakami A, Galvão Neto M, Galvão MS, Silva AC, Canseco EG, Moyses Y. NOTES transvaginal video-assisted cholecystectomy: first series. Endoscopy. 2008;40:572–575. doi: 10.1055/s-2008-1077398. [DOI] [PubMed] [Google Scholar]
- 25.Decarli LA, Zorron R, Branco A, Lima FC, Tang M, Pioneer SR, Sanseverino JI, Menguer R, Bigolin AV, Gagner M. New hybrid approach for NOTES transvaginal cholecystectomy: preliminary clinical experience. Surg Innov. 2009;16:181–186. doi: 10.1177/1553350609339375. [DOI] [PubMed] [Google Scholar]
- 26.Palanivelu C, Rajan PS, Rangarajan M, Prasad M, Kalyanakumari V, Parthasarathi R, Senthilnathan P. NOTES: Transvaginal endoscopic cholecystectomy in humans-preliminary report of a case series. Am J Gastroenterol. 2009;104:843–847. doi: 10.1038/ajg.2009.1. [DOI] [PubMed] [Google Scholar]
- 27.Seven R, Barbaros U. Needloscopy-assisted transvaginal cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2009;19:e61–e63. doi: 10.1097/SLE.0b013e31819caa22. [DOI] [PubMed] [Google Scholar]
- 28.Asakuma M, Perretta S, Allemann P, Cahill R, Con SA, Solano C, Pasupathy S, Mutter D, Dallemagne B, Marescaux J. Challenges and lessons learned from NOTES cholecystectomy initial experience: a stepwise approach from the laboratory to clinical application. J Hepatobiliary Pancreat Surg. 2009;16:249–254. doi: 10.1007/s00534-009-0089-3. [DOI] [PubMed] [Google Scholar]
- 29.Navarra G, Rando L, La Malfa G, Bartolotta G, Pracanica G. Hybrid transvaginal cholecystectomy: a novel approach. Am J Surg. 2009;197:e69–e72. doi: 10.1016/j.amjsurg.2008.07.059. [DOI] [PubMed] [Google Scholar]
- 30.Castro-Pérez R, Acosta-González LR, Dopico-Reyes E, Robaina-Arias LE. [MANOS: Transvaginal cholecystectomies: preliminary report] Cir Esp. 2009;85:292–297. doi: 10.1016/j.ciresp.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Noguera J, Dolz C, Cuadrado A, Olea J, Vilella A, Morales R. Hybrid transvaginal cholecystectomy, NOTES, and minilaparoscopy: analysis of a prospective clinical series. Surg Endosc. 2009;23:876–881. doi: 10.1007/s00464-008-0288-z. [DOI] [PubMed] [Google Scholar]
- 32.Horgan S, Mintz Y, Jacobsen GR, Sandler BJ, Cullen JP, Spivack A, Easter DW, Chock A, Savu MK, Ramamoorthy S, et al. Video. NOTES: transvaginal cholecystectomy with assisting articulating instruments. Surg Endosc. 2009;23:1900. doi: 10.1007/s00464-009-0471-x. [DOI] [PubMed] [Google Scholar]
- 33.Sugimoto M, Yasuda H, Koda K, Suzuki M, Yamazaki M, Tezuka T, Kosugi C, Higuchi R, Watayo Y, Yagawa Y, et al. Rendezvous gastrotomy technique using direct percutaneous endoscopic gastrostomy for transgastric cholecystectomy in hybrid natural orifice translumenal endoscopic surgery. J Hepatobiliary Pancreat Surg. 2009;16:758–762. doi: 10.1007/s00534-009-0143-1. [DOI] [PubMed] [Google Scholar]
- 34.Gumbs AA, Fowler D, Milone L, Evanko JC, Ude AO, Stevens P, Bessler M. Transvaginal natural orifice translumenal endoscopic surgery cholecystectomy: early evolution of the technique. Ann Surg. 2009;249:908–912. doi: 10.1097/SLA.0b013e3181a802e2. [DOI] [PubMed] [Google Scholar]
- 35.de Sousa LH, de Sousa JA, de Sousa Filho LH, de Sousa MM, de Sousa VM, de Sousa AP, Zorron R. Totally NOTES (T-NOTES) transvaginal cholecystectomy using two endoscopes: preliminary report. Surg Endosc. 2009;23:2550–2555. doi: 10.1007/s00464-009-0453-z. [DOI] [PubMed] [Google Scholar]
- 36.Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Prasad M. Transvaginal endoscopic appendectomy in humans: a unique approach to NOTES--world's first report. Surg Endosc. 2008;22:1343–1347. doi: 10.1007/s00464-008-9811-5. [DOI] [PubMed] [Google Scholar]
- 37.Tabutsadze T, Kipshidze N. New trend in endoscopic surgery: transvaginal appendectomy NOTES (Natural Orifice Transluminal Endoscopic Surgery) Georgian Med News. 2009:7–10. [PubMed] [Google Scholar]
- 38.Horgan S, Cullen JP, Talamini MA, Mintz Y, Ferreres A, Jacobsen GR, Sandler B, Bosia J, Savides T, Easter DW, et al. Natural orifice surgery: initial clinical experience. Surg Endosc. 2009;23:1512–1518. doi: 10.1007/s00464-009-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lacy AM, Delgado S, Rojas OA, Almenara R, Blasi A, Llach J. MA-NOS radical sigmoidectomy: report of a transvaginal resection in the human. Surg Endosc. 2008;22:1717–1723. doi: 10.1007/s00464-008-9956-2. [DOI] [PubMed] [Google Scholar]
- 40.Burghardt J, Federlein M, Müller V, Benhidjeb T, Elling D, Gellert K. [Minimal invasive transvaginal right hemicolectomy: report of the first complex NOS (natural orifice surgery) bowels operation using a hybrid approach] Zentralbl Chir. 2008;133:574–576. doi: 10.1055/s-2008-1076992. [DOI] [PubMed] [Google Scholar]
- 41.Zorrón R, Soldan M, Filgueiras M, Maggioni LC, Pombo L, Oliveira AL. NOTES: transvaginal for cancer diagnostic staging: preliminary clinical application. Surg Innov. 2008;15:161–165. doi: 10.1177/1553350608320553. [DOI] [PubMed] [Google Scholar]
- 42.Noguera JF, Dolz C, Cuadrado A, Olea JM, Vilella A. Transvaginal liver resection (NOTES) combined with minilaparoscopy. Rev Esp Enferm Dig. 2008;100:411–415. doi: 10.4321/s1130-01082008000700006. [DOI] [PubMed] [Google Scholar]
- 43.Nakajima K, Nishida T, Takahashi T, Souma Y, Hara J, Yamada T, Yoshio T, Tsutsui T, Yokoi T, Mori M, et al. Partial gastrectomy using natural orifice translumenal endoscopic surgery (NOTES) for gastric submucosal tumors: early experience in humans. Surg Endosc. 2009:Epub ahead of print. doi: 10.1007/s00464-009-0474-7. [DOI] [PubMed] [Google Scholar]
- 44.Ramos AC, Zundel N, Neto MG, Maalouf M. Human hybrid NOTES transvaginal sleeve gastrectomy: initial experience. Surg Obes Relat Dis. 2008;4:660–663. doi: 10.1016/j.soard.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 45.Targarona EM, Gomez C, Rovira R, Pernas JC, Balague C, Guarner-Argente C, Sainz S, Trias M. NOTES-assisted transvaginal splenectomy: the next step in the minimally invasive approach to the spleen. Surg Innov. 2009;16:218–222. doi: 10.1177/1553350609345488. [DOI] [PubMed] [Google Scholar]
- 46.Perretta S, Allemann P, Asakuma M, Dallemagne B, Marescaux J. Adrenalectomy using natural orifice translumenal endoscopic surgery (NOTES): a transvaginal retroperitoneal approach. Surg Endosc. 2009;23:1390. doi: 10.1007/s00464-009-0367-9. [DOI] [PubMed] [Google Scholar]
- 47.Perretta S, Allemann P, Asakuma M, Cahill R, Dallemagne B, Marescaux J. Feasibility of right and left transvaginal retroperitoneal nephrectomy: from the porcine to the cadaver model. J Endourol. 2009;23:1887–1892. doi: 10.1089/end.2008.0682. [DOI] [PubMed] [Google Scholar]
- 48.Zacharopoulou C, Nassif J, Allemann P, Dallemagne B, Perretta S, Marescaux J, Wattiez A. Exploration of the retroperitoneum using the transvaginal natural orifice transluminal endoscopic surgery technique. J Minim Invasive Gynecol. 2009;16:198–203. doi: 10.1016/j.jmig.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 49.Allemann P, Perretta S, Asakuma M, Dallemagne B, Mutter D, Marescaux J. Multimedia manuscript. NOTES retroperitoneal transvaginal distal pancreatectomy. Surg Endosc. 2009;23:882–883. doi: 10.1007/s00464-008-0297-y. [DOI] [PubMed] [Google Scholar]
- 50.Kaouk JH, Haber GP, Goel RK, Crouzet S, Brethauer S, Firoozi F, Goldman HB, White WM. Pure Natural Orifice Translumenal Endoscopic Surgery (NOTES) Transvaginal Nephrectomy. Eur Urol. 2009:Epub ahead of print. doi: 10.1016/j.eururo.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 51.Alcaraz A, Peri L, Molina A, Goicoechea I, García E, Izquierdo L, Ribal MJ. Feasibility of transvaginal NOTES-assisted laparoscopic nephrectomy. Eur Urol. 2010;57:233–237. doi: 10.1016/j.eururo.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 52.Kaouk JH, White WM, Goel RK, Brethauer S, Crouzet S, Rackley RR, Moore C, Ingber MS, Haber GP. NOTES transvaginal nephrectomy: first human experience. Urology. 2009;74:5–8. doi: 10.1016/j.urology.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 53.Ribal Caparrós MJ, Peri Cusí L, Molina Cabeza A, García Larrosa A, Carmona F, Alcaraz Asensio A. [First report on hybrid transvaginal nephrectomy for renal cancer] Actas Urol Esp. 2009;33:280–283. doi: 10.1016/s0210-4806(09)74141-5. [DOI] [PubMed] [Google Scholar]
- 54.Aron M, Berger AK, Stein RJ, Kamoi K, Brandina R, Canes D, Sotelo R, Desai MM, Gill IS. Transvaginal nephrectomy with a multichannel laparoscopic port: a cadaver study. BJU Int. 2009;103:1537–1541. doi: 10.1111/j.1464-410X.2009.08612.x. [DOI] [PubMed] [Google Scholar]
- 55.Branco AW, Branco Filho AJ, Kondo W, Noda RW, Kawahara N, Camargo AA, Stunitz LC, Valente J, Rangel M. Hybrid transvaginal nephrectomy. Eur Urol. 2008;53:1290–1294. doi: 10.1016/j.eururo.2007.10.053. [DOI] [PubMed] [Google Scholar]
- 56.Lomanto D, Dhir U, So JB, Cheah WK, Moe MA, Ho KY. Total transvaginal endoscopic abdominal wall hernia repair: a NOTES survival study. Hernia. 2009;13:415–419. doi: 10.1007/s10029-009-0485-2. [DOI] [PubMed] [Google Scholar]
- 57.Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc. 2008;67:854–860. doi: 10.1016/j.gie.2007.09.053. [DOI] [PubMed] [Google Scholar]
- 58.Peterson CY, Ramamoorthy S, Andrews B, Horgan S, Talamini M, Chock A. Women's positive perception of transvaginal NOTES surgery. Surg Endosc. 2009;23:1770–1774. doi: 10.1007/s00464-008-0206-4. [DOI] [PubMed] [Google Scholar]
- 59.Swanstrom LL, Volckmann E, Hungness E, Soper NJ. Patient attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc. 2009;23:1519–1525. doi: 10.1007/s00464-009-0431-5. [DOI] [PubMed] [Google Scholar]
- 60.Volckmann ET, Hungness ES, Soper NJ, Swanstrom LL. Surgeon perceptions of Natural Orifice Translumenal Endoscopic Surgery (NOTES) J Gastrointest Surg. 2009;13:1401–1410. doi: 10.1007/s11605-009-0921-8. [DOI] [PubMed] [Google Scholar]
- 61.Thele F, Zygmunt M, Glitsch A, Heidecke CD, Schreiber A. How do gynecologists feel about transvaginal NOTES surgery? Endoscopy. 2008;40:576–580. doi: 10.1055/s-2008-1077379. [DOI] [PubMed] [Google Scholar]


