Abstract
AIM: To investigate the expression of myeloid differentiation protein-2 (MD-2), MD-2B (a splicing isoform of MD-2 that can block Toll-like receptor 4 (TLR4)/MD-2 LPS-mediated signal transduction) and TLR4 in the liver of acute cholangitis rats.
METHODS: Male Sprague-Dawley rats (SPF level) were randomly divided into four groups: (A) sham-operated group; (B) simple common bile duct ligation group; (C) acute cholangitis group; and (D) acute cholangitis anti-TLR4 intervention group (n = 25 per group). Rat liver tissue samples were used to detect TLR4, MD-2 and MD-2B mRNA expression by fluorescence quantitative PCR in parallel with pathological changes.
RESULTS: In acute cholangitis, liver TLR4 and MD-2 mRNA expression levels at 6, 12, 24, 48 and 72 h were gradually up-regulated but MD-2B mRNA expression gradually down-regulated (P < 0.05). After TLR4 antibody treatment, TLR4 and MD-2 mRNA expression were lower compared with the acute cholangitis group (P < 0.05). However, MD-2B mRNA expression was higher than in the acute cholangitis group (P < 0.05). MD-2 and TLR4 mRNA expressions were positively correlated (r = 0.94981, P < 0.05) and MD-2B mRNA expression was negatively correlated with MD-2 and TLR4 mRNA (r = -0.89031, -0.88997, P < 0.05).
CONCLUSION: In acute cholangitis, MD-2 plays an important role in the process of TLR4- mediated inflammatory response to liver injury while MD-2B plays a negative regulatory role.
Keywords: Acute cholangitis, Toll-like receptor 4, Myeloid differentiation protein-2, Myeloid differentiation protein-2 splicing isoform
INTRODUCTION
In acute cholangitis (AC), a large number of breeding intestinal flora gain access to the bile duct, releasing large amounts of toxins and directly or indirectly triggering excessive inflammation and causing liver damage[1-3]. In recent years, Toll-like receptor 4 (TLR4) has been identified as an important transmembrane signaling system involved in endotoxin-induced inflammation[4-5]. TLR4, as the main receptor for bacterial lipopolysaccharide (LPS), mediates a signal transduction pathway that includes formation of the LPS-LBP-CD14-secreted protein MD-2-TLR4 receptor complex, combination with myeloid differentiation factor 88, phosphorylation of IRAK and activation of a series of cell kinases, collectively controlling the activation of the transcription factor nuclear factor κB (NF-κB) and its biological effects[6-9].
Myeloid differentiation protein-2 (MD-2) is a recently described 160 amino-acid secreted glycoprotein and an important regulatory element in natural immune recognition[10]. Tamai confirmed that MD-2 is involved in synergistic effects of IL-8 production[11]. Research shows that following mutation of MD-2 glycosylation sites, MD-2 can still be expressed at the cell surface and combination with TLR4 is maintained but that TLR4-mediated activation of NF-κB weakens. When two glycosylation sites are simultaneously mutated, MD-2 can no longer promote LPS-induced IL-8 secretion[12]. MD-2 serves as the bridge between TLRs and LPS, playing an important role in the LPS signal transduction[10].
Using RT-PCR, Ohta et al[13] amplified MD-2B, an MD-2 splicing isoform, from mouse spleen and bone marrow cells. NF-κB instruction analysis suggests that HEK 293 cells cotransfected with equal amounts of MD-2 and MD-2B have a slower NF-κB up-regulation and weakened activity. When 8 fold more MD-2B than MD-2 was transfected, NF-κB activity was reduced to similar levels observed in cells transfected with the TLR4 and MD-2 without LPS stimulation. These results suggest that MD-2B can dose-dependently block TLR4/MD-2/LPS-mediated NF-κB signal transduction.
In the present study, real-time quantitative PCR was used to quantitatively detect TLR4, MD-2 and MD-2B mRNA expression in the liver during acute cholangitis. Data were used to study the interrelationship between MD-2, its splicing isoform (MD-2B) and TLR4 and establish the role of MD-2 and MD-2B in the TLR4-mediated inflammatory signaling pathway.
MATERIALS AND METHODS
Experimental strain
E. coli type Oll1B4 was provided by the Chinese drugs biological preparations examination institute. Bacteria were vaccinated on blood plates, incubated at 37°C for 24 h before experiment, eluted with the aseptic physiological saline to a density of 5 × 105 CFU/mL and preserved at 4°C until use.
Animal grouping and model preparation
The Guangdong Medical College hospital ethical committee approved the research protocol and the use of animals in this study was in accordance with the statement.
100 SPF level SD male rats weighing between 220-250 g were obtained from the institutional animal experimentation center (production license SCXK Guangdong 2004-0008, animal quality certification 2007A034) and were stochastically divided into 4 groups (n = 25 per group): a sham-operation (Group A), a control group (Group B), an acute cholangitis group (Group C) and an acute cholangitis anti-TLR4 intervention group (Group D).
The sham group (Group A) received operations simply to free the common bile duct and the control group had only a simple choledoch ligation (Group B). Rat choledoch dissociation was performed using a surgery microscope with the dissociated choledoch dual ligated with No. 1 silk thread at a length of approximately 1 cm. The acute cholangitis (Group C) was induced by injection of 0.2 mL E. coli suspension into the end near the ligation with a No. 4 silk scalp acupuncture needle followed by 1 mL physiological saline. The acute cholangitis anti-TLR4 intervention group (Group D) received an injection of anti-TLR4 monoclonal antibody 1 mL (2.5 g, diluted 1:200). Each group of rats received abdominal wall sutures layer by layer. After surgery rats were individually housed and had unconfined drinking and eating. Rats from each group were serially killed at 6, 12, 24, 48 and 72 h after surgery and then liver tissue was collected for pathological examination and real-time quantitative PCR.
Detection of TLR4, MD-2 and MD-2B mRNA expression
TLR4, MD-2 and MD-2B mRNA expression was detected in rat liver tissue using real-time PCR at various time points. The purity of isolated total RNA was verified by electrophoresis on 1% agarose gels (Figure 1). Templates from RNA reverse transcription were amplified in 10 μL 5 × quantitative PCR buffer, 1 μL upstream primer F (10 pmol/μL), 1 μL downstream primer R (10 pmol/μL), 1 μL probe (10 pmol/μL), 1 μL Taq enzyme (5 U/μL), 1 μL dNTPs (10 mmol), 5 μL, cDNA and 32 μL ddH2O using an ABI7000 completely automatic fluorescence quota PCR meter.
Figure 1.
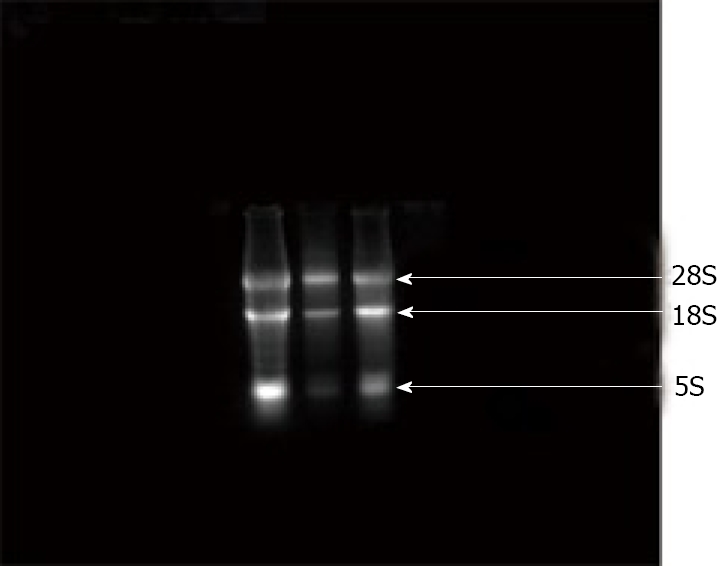
RNA electrophoretograms. There are three visible bands with 28s and 18s, 5s, showing no pollution in the DNA, no degradation with RNA which indicates the purity of RNA is higher.
After amplification, data were adjusted according to the start value, stop value and threshold value of the baseline, the standard curves under the Std curve window was adjusted to optimal (the correlation value to be situated between 0.97 and -1, with the correlation value |r|) and finally, unknown specimen values B were obtained under the Reporter window by auto-calculating analysis (Qty). Considering the difference of total RNA density from each sample, the final computed results were calculated according to the following formula: A (copy counts/ug total RNA) = [B (copy counts/μL cDNA)]/(OD260 × 5/6). Masculine specimen RNA was reverse transcribed as templet.
PCR amplification was performed using a PE9600PCR meter and the primers used for PCR are shown in Table 1.
Table 1.
Primers used for real-time PCR
| Forward | Reverse | |
| MD-2 (130 bp) | 5'-AAATCCCTATTTCAATTAGTTCTGAACC-3' | 5'-GAGTTGATATTGATGAACAGGTTGAAAT-3' |
| MD-2B (93 bp) | 5'-AAATCCCTATTTCAATTAGTTCTGAACC-3' | 5'-GCTTCGGCAATTTTGGAATG-3' |
| TLR4 (117 bp) | 5'-GATTGCTCAGACATGGCAGTTTC-3' | 5'-CTGCTAAGAAGGCGATACAATTCG-3' |
| GAPDH (97 bp) | 5'-CCGAGGGCCCACTAAAGG-3' | 5'-GCTGTTGAAGTCACAGGAGACAA-3' |
The amplification conditions were 2 min at 93°C, 40 cycles of 1 min at 93°C, 1 min at 55°C, 1 min at 72°C and finally 7 min at 72°C for extension. PCR products were electrophoresed in 2% low melting point agarose gel and under UVA objective zones were removed, recycled and purified with the recycling reagent box (QIA quick Gel Extraction Kit). Determination of OD 260/280 > 1.8 indicated the purity of the samples. Concentration (copy/μL) was calculated using the OD260 value and fragment length and then samples were gradient diluted to a positive quantitative standard gradient sample. Dual-distilled sterile water was employed as fluorescence-negative control standard sample.
Analysis and data processing
MD-2, MD-2B, TLR4 RNA copy number ratios were calculated using the formula: copy number ratio = copies/ug total RNA/GAPDH (internal parameters) copies/ug total RNA.
The data obtained were analyzed using SPSS 10.0 to perform completely stochastic variance comparison analyses among groups. Results were considered significant when P < 0.05. A q test was used for individual comparisons. The relevance of the various indexes was calculated using Pearson correlation analyses with statistical significance accepted when P < 0.05.
RESULTS
Change in liver tissue expression of TLR4 mRNA
In Group A, liver TLR4 mRNA expression was detected at all time points examined. TLR4 mRNA expression in Group B rats started to increase 12 h after surgery and by 72 h had increased significantly (P < 0.05). In Group C, TLR4 mRNA had increased by 12 h after surgery and this increased expression extended through 72 h. At the 12 h time point, TLR4 mRNA levels were significantly higher in Group C than in Group B (P < 0.05). In Group D, TLR4 mRNA expression declined 6 h after surgery with levels that were significantly different from those in Group C at corresponding time points (P < 0.05) (Table 2).
Table 2.
TLR4 expression in rat liver tissue (mean ± SE) (copy ratio 104)
| 6 h | 12 h | 24 h | 48 h | 72 h | |
| Group A | 4.32 ± 0.721 | 4.17 ± 0.708 | 4.40 ± 0.435 | 4.36 ± 0.396 | 4.48 ± 0.504 |
| Group B | 3.96 ± 0.051 | 4.90 ± 0.075a | 8.52 ± 0.023a | 11.11 ± 0.029a | 12.90 ± 0.042a |
| Group C | 3.87 ± 0.031 | 5.23 ± 0.033ac | 9.87 ± 0.025ac | 13.70 ± 0.115ac | 19.70 ± 0.123ac |
| Group D | 0.16 ± 0.003e | 0.17 ± 0.002e | 0.22 ± 0.002e | 0.58 ± 0.001e | 0.77 ± 0.006e |
P < 0.05 vs the same group at different time points;
P < 0.05 vs group B at the same time;
P < 0.05 vs group C at the same time.
Change in liver tissue expression of MD-2 mRNA
In Group A, MD-2 mRNA expression was detected in liver tissue at different time points. MD-2 mRNA expression of Group B rats started to rise at 12 h after surgery and by 72 h had risen significantly (P < 0.05). In Group C, MD-2 mRNA expression was also present within 12 h and expression continued through 72 h. At 12 h, expression in Group C was significantly different than that of Group B (P < 0.05). MD-2 mRNA expression declined in Group D rats from 6 h after surgery onwards and was significantly different from Group C at the 6 h time point (P < 0.05) (Table 3).
Table 3.
MD-2 expression in rat liver tissue (mean ± SE) (copy ratio 103)
| 6h | 12h | 24h | 48h | 72h | |
| Group A | 1.16 ± 0.042 | 1.17 ± 0.057 | 1.14 ± 0.016 | 1.16 ± 0.028 | 1.17 ± 0.048 |
| Group B | 1.15 ± 0.015 | 2.11 ± 0.042a | 3.29 ± 0.034a | 15.41 ± 0.267a | 21.97 ± 0.271a |
| Group C | 1.17 ± 0.028 | 4.10 ± 0.054ac | 12.27 ± 0.078ac | 21.158 ± 0.185ac | 30.21 ± 0.342ac |
| Group D | 0.33 ± 0.017e | 0.40 ± 0.061e | 1.15 ± 0.025e | 3.61 ± 0.089e | 4.58 ± 0.034e |
P < 0.05 vs the same group at different time points;
P < 0.05 vs group B at the same time;
P < 0.05 vs group C at the same time.
Change in liver tissue expression of MD-2B mRNA
In Group A, liver MD-2mB RNA expression was detected at all time points. MD-2 mRNA expression in Group B rats started to decline at 12 h after surgery and continued a gradual decline through 72 h. By 72 h, MD-2mB RNA expression had significantly declined (P < 0.05). Group C MD-2 mRNA expression also declined starting at 12 h and was significantly different from Group B at the 12 h time point (P < 0.05). In Group D, liver MD-2 mRNA expression increased starting at the 6 h time point compared with corresponding time point in Group C and was significantly different (P < 0.05) (Table 4).
Table 4.
MD-2B expression in rat liver tissue (mean ± SE) (copy ratio 102)
| 6h | 12h | 24h | 48h | 72h | |
| Group A | 2.35 ± 0.013 | 2.38 ± 0.013 | 2.35 ± 0.012 | 2.35 ± 0.012 | 2.35 ± 0.010 |
| Group B | 2.47 ± 0.021 | 1.32 ± 0.035a | 0.98 ± 0.006a | 0.71 ± 0.006a | 0.48 ± 0.002a |
| Group C | 2.47 ± 0.021 | 1.42 ± 0.015ac | 0.26 ± 0.002ac | 0.09 ± 0.001ac | 0.07 ± 0.003ac |
| Group D | 6.03 ± 0.015e | 4.50 ± 0.017e | 3.85 ± 0.015e | 3.62 ± 0.015e | 2.39 ± 0.022e |
P < 0.05 vs the same group at different time points;
P < 0.05 vs group B at the same time;
P < 0.05 vs group C at the same time.
Correlation analysis between TLR4 mRNA and MD-2, MD-2B mRNA
In rats with acute cholangitis, expression of MD-2 mRNA and TLR4 mRNA was positively correlated (r = 0.94981, P < 0.05) while MD-2 mRNA and MD-2B mRNA were negatively correlated (r = -0.89031, P < 0.05). TLR4 mRNA and MD-2B mRNA were also negatively correlated (r = -0.88997, P < 0.05).
DISCUSSION
In acute cholangitis, bacterial translocation from the intestinal tract and enterogenic endotoxemia may occur. Miyaso[14] investigated the relationship between LPS, the signaling molecule TLR4 and liver damage during obstructive icterus endotoxemia. These observations revealed that LPS-induced liver damage was time dependent and involved TLR4 signaling. The present results show that in the livers of rats with acute cholangitis, TLR4 mRNA expression increased significantly 12 h after induction, continued to increase even higher as inflammation developed in the first 72 h and showed a clear positive correlation with the degree of inflammation. This high level of TLR4 expression suggests that it is closely related to liver damage in acute cholangitis. As TLR4 is an essential component of inflammatory pathways, over expression of TLR4 mRNA during acute cholangitis may result in an excessive inflammatory response leading to liver damage.
Some research has indicated that synergistic up-regulation of other proteins may be necessary for enhancement of TLR-mediated immune responses[15]. MD-2 is a newly discovered, soluble secretary protein which binds to the extracellular region of TLR4. Upon binding, MD-2 enhances TLR4 reactivity to LPS, strengthens the subsequent signal transduction intensity and facilitates LPS-mediating signaling through the NF-κB pathway. Other reports showing that treatment with LPS causes a dose-dependent increase in MD-2 expression[16] and that MD-2 gene knockout mice do not respond to LPS and can survive LPS-induced shock[17], support the concept that extracellular MD-2 directly binds to LPS and unites it with the TLR4 external functional region. Thus MD-2 is indispensable in TLR4-mediated LPS signal transduction[18-19].
MD-2 mRNA expression was up-regulated in the livers of rats with acute cholangitis and its expression increased as inflammation developed in 72 h, suggesting that MD-2 was also an essential media element in the associated inflammatory pathways. The positive correlation between MD-2 and TLR4 during inflammation medium may result from their roles as essential components of LPS complexes[10] and is critical during the occurrence and development of acute cholangitis. Anti-TLR4 group rats showed lower expression of both MD-2 and TLR4 mRNA compared with rats in the sham-operation group, control group and acute cholangitis group at corresponding time points (P < 0.05). These observations were mainly due to the inhibition of normal TLR4 expression by anti-TLR4 and the resultant inhibition of MD-2. When anti-TLR4 bound to TLR4, it is likely that it also suppressed MD-2 that was bound to TLR4 and inhibited MD-2 expression and function. These observations suggest that in acute cholangitis, MD-2 mediates the LPS inflammatory pathway collaboratively with TLR4 through protein-protein interaction[20].
Selective slicing has been the subject of intensive research in the recent years, particularly since the human genome project was completed and may potentially contribute to the discovery and development of new medical treatments, drug targets and diagnosis markers[21-23]. Many key signaling molecules and downstream effector molecules in the TLR4 signaling pathway including MD-2, TRL4, MyD88, IRAK and IκB produce selective splicing isoforms[24-29]. Interestingly, most of these isoforms play a negative role in regulating TLR4 pathway. In acute cholangitis, liver MD-2B decreases to levels that are lower than that in the normal state which is opposite to the observed up-regulation of the inflammatory mediators MD-2 and TLR4. These data suggest that MD-2B plays an inhibitory role in the inflammation process and that MD-2B expression increases as the expression of MD-2 and TLR4 are reduced. Thus, in acute cholangitis, MD-2B is also involved in the inflammatory process by inhibiting MD-2, TLR4 or MD-2 and TLR4 complex. However, the underlying inhibitory mechanism and the exact functioning location of MD-2B need further investigation.
Ohta et al[13] identified MD-2B as an MD-2 splicing isoform and showed that it had a negatively regulatory function during TLR4-mediated LPS signal transduction, reducing cell and tissue damage caused by inflammatory reactions[30-32]. The experiments reported here show that in rats, the liver normally expresses only a small but consistent amount of MD-2B mRNA. In rats with induced, acute cholangitis, MD-2 mRNA expression started to decline 12 h after surgery (P < 0.05). However, in rats treated with anti-TLR4, MD-2 mRNA expression rose after 6 h as compared with its expression in other groups at the same time point (P < 0.05). This up-regulation may be due to the combination of anti-TLR4 with the TLR4 extracellular region which partially blocks the combination of CD14 and MD-2 and subsequently leads to the enhanced expression of the MD-2B, the splicing isoforms of MD-2.
COMMENTS
Background
TLR4 as the main receptor for lipopolysaccharide (LPS) activates transcription factor NF-κB which controls gene expression in various ways to produce biological effects. Myeloid differentiation protein-2 (MD-2) is the bridge between the Toll-like receptor (TLR) and LPS, playing an important role in the lipopolysaccharide signal transduction. MD-2B is an editing isomer of MD-2 extracted from the mouse spleen cells and bone marrow cells. It can block dose-dependent toll-like receptor 4 (TLR4)/MD-2 LPS-mediated signal transduction. The study focused on the expressions of MD-2 and its editing isomers (MD-2B) in acute cholangitis and its mutual relations to TLR4.
Research frontiers
TLR4 has been identified as an important transmembrane signaling system involved in endotoxin-induced inflammation. MD-2 serves as the bridge between TLRs and LPS, playing an important role in the LPS signal transduction. MD-2B can dose-dependently block TLR4/MD-2/LPS-mediated NF-κB signal transduction. In the present study, data were used to study the interrelationship between MD-2, its editing isomers (MD-2B) and TLR4 and establish the role of MD-2 and MD-2B in the TLR4-mediated inflammatory signaling pathway.
Innovations and breakthroughs
In acute cholangitis, MD-2 plays an important role in the process of TLR4-mediated inflammatory response to liver injury while MD-2B plays a negative regulatory role.
Applications
This may potentially contribute to the discovery and development of new medical treatments, drug targets and diagnosis markers. They may offer early diagnosis for severe acute cholangitis.
Peer review
This paper describes an interesting and novel experiment that provides confirmatory evidence of the role of MD-2 in the process of TLR4- mediated inflammatory response to liver injury, while MD-2B plays a negative regulatory role.
Footnotes
Supported by the Medical Technology Research Foundation of Guangdong Province, No. A2008475
Peer reviewers: Xun-Di Xu, MD, PhD, Department of Gastroenterological Surgery, Xiangya Second Hospital, Central South University, Renmin Zhong Road 139, Changsha 410011, Hunan Province, China; Pierce KH Chow, MD, PhD, Professor, Department of General Surgery, Singapore General Hospital, Singapore 169608, Singapore
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
References
- 1.Wu SD, Yu H, Sun JM. Bacteriological and electron microscopic examination of primary intrahepatic stones. Hepatobiliary Pancreat Dis Int. 2006;5:228–231. [PubMed] [Google Scholar]
- 2.Zhang WZ, Chen YS, Wang JW, Chen XR. Early diagnosis and treatment of severe acute cholangitis. World J Gastroenterol. 2002;8:150–152. doi: 10.3748/wjg.v8.i1.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinsky MR. Pathophysiology of sepsis and multiple organ failure: pro- versus anti-inflammatory aspects. Contrib Nephrol. 2004;144:31–43. doi: 10.1159/000078875. [DOI] [PubMed] [Google Scholar]
- 4.Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 5.Beutler B, Poltorak A. Sepsis and evolution of the innate immune response. Crit Care Med. 2001;29:S2–S6; discussion S6-S7. doi: 10.1097/00003246-200107001-00002. [DOI] [PubMed] [Google Scholar]
- 6.Yu H, Wu SD. Activation of TLR-4 and liver injury via NF-kappa B in rat with acute cholangitis. Hepatobiliary Pancreat Dis Int. 2008;7:185–191. [PubMed] [Google Scholar]
- 7.Zhang G, Ghosh S. Molecular mechanisms of NF-kappaB activation induced by bacterial lipopolysaccharide through Toll-like receptors. J Endotoxin Res. 2000;6:453–457. doi: 10.1179/096805100101532414. [DOI] [PubMed] [Google Scholar]
- 8.Bäckhed F, Hornef M. Toll-like receptor 4-mediated signaling by epithelial surfaces: necessity or threat? Microbes Infect. 2003;5:951–959. doi: 10.1016/s1286-4579(03)00189-8. [DOI] [PubMed] [Google Scholar]
- 9.Tsung A, McCoy SL, Klune JR, Geller DA, Billiar TR, Hefeneider SH. A novel inhibitory peptide of Toll-like receptor signaling limits lipopolysaccharide-induced production of inflammatory mediators and enhances survival in mice. Shock. 2007;27:364–369. doi: 10.1097/01.shk.0000239773.95280.2c. [DOI] [PubMed] [Google Scholar]
- 10.Fitzgerald KA, Rowe DC, Golenbock DT. Endotoxin recognition and signal transduction by the TLR4/MD2-complex. Microbes Infect. 2004;6:1361–1367. doi: 10.1016/j.micinf.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Tamai R, Sugawara S, Takeuchi O, Akira S, Takada H. Synergistic effects of lipopolysaccharide and interferon-gamma in inducing interleukin-8 production in human monocytic THP-1 cells is accompanied by up-regulation of CD14, Toll-like receptor 4, MD-2 and MyD88 expression. J Endotoxin Res. 2003;9:145–153. doi: 10.1179/096805103125001540. [DOI] [PubMed] [Google Scholar]
- 12.Ohnishi T, Muroi M, Tanamoto K. N-linked glycosylations at Asn(26) and Asn(114) of human MD-2 are required for toll-like receptor 4-mediated activation of NF-kappaB by lipopolysaccharide. J Immunol. 2001;167:3354–3359. doi: 10.4049/jimmunol.167.6.3354. [DOI] [PubMed] [Google Scholar]
- 13.Ohta S, Bahrun U, Tanaka M, Kimoto M. Identification of a novel isoform of MD-2 that downregulates lipopolysaccharide signaling. Biochem Biophys Res Commun. 2004;323:1103–1108. doi: 10.1016/j.bbrc.2004.08.203. [DOI] [PubMed] [Google Scholar]
- 14.Miyaso H, Morimoto Y, Ozaki M, Haga S, Shinoura S, Choda Y, Iwagaki H, Tanaka N. Obstructive jaundice increases sensitivity to lipopolysaccharide via TLR4 upregulation: possible involvement in gut-derived hepatocyte growth factor-protection of hepatocytes. J Gastroenterol Hepatol. 2005;20:1859–1866. doi: 10.1111/j.1440-1746.2005.03953.x. [DOI] [PubMed] [Google Scholar]
- 15.Faure E, Equils O, Sieling PA, Thomas L, Zhang FX, Kirschning CJ, Polentarutti N, Muzio M, Arditi M. Bacterial lipopolysaccharide activates NF-kappaB through toll-like receptor 4 (TLR-4) in cultured human dermal endothelial cells. Differential expression of TLR-4 and TLR-2 in endothelial cells. J Biol Chem. 2000;275:11058–11063. doi: 10.1074/jbc.275.15.11058. [DOI] [PubMed] [Google Scholar]
- 16.Miyake K. Endotoxin recognition molecules, Toll-like receptor 4-MD-2. Semin Immunol. 2004;16:11–16. doi: 10.1016/j.smim.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Nagai Y, Akashi S, Nagafuku M, Ogata M, Iwakura Y, Akira S, Kitamura T, Kosugi A, Kimoto M, Miyake K. Essential role of MD-2 in LPS responsiveness and TLR4 distribution. Nat Immunol. 2002;3:667–672. doi: 10.1038/ni809. [DOI] [PubMed] [Google Scholar]
- 18.Yang H, Young DW, Gusovsky F, Chow JC. Cellular events mediated by lipopolysaccharide-stimulated toll-like receptor 4. MD-2 is required for activation of mitogen-activated protein kinases and Elk-1. J Biol Chem. 2000;275:20861–20866. doi: 10.1074/jbc.M002896200. [DOI] [PubMed] [Google Scholar]
- 19.Akashi S, Shimazu R, Ogata H, Nagai Y, Takeda K, Kimoto M, Miyake K. Cutting edge: cell surface expression and lipopolysaccharide signaling via the toll-like receptor 4-MD-2 complex on mouse peritoneal macrophages. J Immunol. 2000;164:3471–3475. doi: 10.4049/jimmunol.164.7.3471. [DOI] [PubMed] [Google Scholar]
- 20.Mancek M, Pristovsek P, Jerala R. Identification of LPS-binding peptide fragment of MD-2, a toll-receptor accessory protein. Biochem Biophys Res Commun. 2002;292:880–885. doi: 10.1006/bbrc.2002.6748. [DOI] [PubMed] [Google Scholar]
- 21.Modrek B, Lee C. A genomic view of alternative splicing. Nat Genet. 2002;30:13–19. doi: 10.1038/ng0102-13. [DOI] [PubMed] [Google Scholar]
- 22.Flouriot G, Brand H, Seraphin B, Gannon F. Natural trans-spliced mRNAs are generated from the human estrogen receptor-alpha (hER alpha) gene. J Biol Chem. 2002;277:26244–26251. doi: 10.1074/jbc.M203513200. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Blanco MA, Baraniak AP, Lasda EL. Alternative splicing in disease and therapy. Nat Biotechnol. 2004;22:535–546. doi: 10.1038/nbt964. [DOI] [PubMed] [Google Scholar]
- 24.Janssens S, Burns K, Tschopp J, Beyaert R. Regulation of interleukin-1- and lipopolysaccharide-induced NF-kappaB activation by alternative splicing of MyD88. Curr Biol. 2002;12:467–471. doi: 10.1016/s0960-9822(02)00712-1. [DOI] [PubMed] [Google Scholar]
- 25.Burns K, Janssens S, Brissoni B, Olivos N, Beyaert R, Tschopp J. Inhibition of interleukin 1 receptor/Toll-like receptor signaling through the alternatively spliced, short form of MyD88 is due to its failure to recruit IRAK-4. J Exp Med. 2003;197:263–268. doi: 10.1084/jem.20021790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janssens S, Burns K, Vercammen E, Tschopp J, Beyaert R. MyD88S, a splice variant of MyD88, differentially modulates NF-kappaB- and AP-1-dependent gene expression. FEBS Lett. 2003;548:103–107. doi: 10.1016/s0014-5793(03)00747-6. [DOI] [PubMed] [Google Scholar]
- 27.Rao N, Nguyen S, Ngo K, Fung-Leung WP. A novel splice variant of interleukin-1 receptor (IL-1R)-associated kinase 1 plays a negative regulatory role in Toll/IL-1R-induced inflammatory signaling. Mol Cell Biol. 2005;25:6521–6532. doi: 10.1128/MCB.25.15.6521-6532.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yanagisawa K, Tago K, Hayakawa M, Ohki M, Iwahana H, Tominaga S. A novel splice variant of mouse interleukin-1-receptor-associated kinase-1 (IRAK-1) activates nuclear factor-kappaB (NF-kappaB) and c-Jun N-terminal kinase (JNK) Biochem J. 2003;370:159–166. doi: 10.1042/BJ20021218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hardy MP, O'Neill LA. The murine IRAK2 gene encodes four alternatively spliced isoforms, two of which are inhibitory. J Biol Chem. 2004;279:27699–27708. doi: 10.1074/jbc.M403068200. [DOI] [PubMed] [Google Scholar]
- 30.Mancek M, Pristovsek P, Jerala R. Identification of LPS-binding peptide fragment of MD-2, a toll-receptor accessory protein. Biochem Biophys Res Commun. 2002;292:880–885. doi: 10.1006/bbrc.2002.6748. [DOI] [PubMed] [Google Scholar]
- 31.Williams DL, Ha T, Li C, Kalbfleisch JH, Schweitzer J, Vogt W, Browder IW. Modulation of tissue Toll-like receptor 2 and 4 during the early phases of polymicrobial sepsis correlates with mortality. Crit Care Med. 2003;31:1808–1818. doi: 10.1097/01.CCM.0000069343.27691.F3. [DOI] [PubMed] [Google Scholar]
- 32.Nattermann J, Du X, Wei Y, Shevchenko D, Beutler B. Endotoxin-mimetic effect of antibodies against Toll-like receptor 4. J Endotoxin Res. 2000;6:257–264. [PubMed] [Google Scholar]


