Abstract
Quantum dots (QDs) are luminescent semiconductor nanocrystals that are widely used as fluorescent probes in biomedical applications, including cellular imaging and tumor tracking. Cell-penetrating peptides (CPPs), also called protein transduction domains (PTDs), are short basic peptides that permeate cell membranes and are able to deliver a variety of macromolecule cargoes, such as DNAs, RNAs, proteins, and nanomaterials. Here we review strategies to couple QDs to CPPs, by either covalent linkages or noncovalent interactions, to provide a tool to study intracellular delivery. This facilitated transport of QDs by CPPs into cells is both simple and efficient. Accordingly, CPP-QD nanoparticles are likely to be of broad utility in biological research and advance the development of medical and pharmaceutical therapeutics.
Keywords: Arginine-Rich, Cell-Penetrating Peptide, Cellular Internalization, Protein Transduction Domain, Quantum Dot
INTRODUCTION
Nanomaterials (materials with at least one dimension in the range of 1–100 nm) have unique physical and chemical properties because of their small size. An increase in the use of nanomaterials in bioscience and biomedical research parallels developments in nanotechnology and the use of nanomaterials in manufacturing processes. Colloidal seminconductor nanocrystals, quantum dots (QDs), have unique photophysical properties which make them attractive candidates for imaging applications.1, 2 Notably, the conducting characteristics of QDs are closely related to the size and shape of the individual crystals.1-7 In general, the smaller the crystal, the larger the band gap (i.e., the difference in energy between the highest valence band and the lowest conduction band). Thus, more energy is needed to excite the dot, and more energy is released when the crystal returns to its resting state. The higher frequency of light emitted after excitation of the dot as the crystal size grows smaller results in a color shift from red to blue in the light emission. Advantages of QDs over traditional dyes and proteins (such as green fluorescent proteins) include photostability, high quantum yield, narrow emission peak, exceptional resistance to degradation, and broad size-dependent photoluminescence.8 Therefore, QDs have the potential to revolutionize medical, diagnostic, and basic research applications.1-4
QDs would seen to be particularly well suited for the visualization of cellular processes, as they have potential to allow long-term and multicolor labeling of fixed and live cells for biomedical applications. Several examples follow:
An important initial use of QDs has been as stable fluorescent markers for cancer diagnosis and treatment. Wu et al. used QDs linked to streptavidin and antibody to label the cancer marker Her2 on the surface of human SK-BR-3 breast cancer cells.9
Type II QDs emit light within the near-infrared spectrum and have a potential surgical utility by providing optical guidance that can result in reduction of cancer metastases.10
QD fluorescence can also be used for sentinel lymph node mapping and removal, providing accurate staging and therapeutic planning.10, 11
QD properties such as multiplexing potential, photostability, and inorganic nature make them useful in drug discovery applications. For example, QDs allow simultaneous monitoring of multiple drug candidates over extended time periods in cell culture, thereby saving time and cost.12
QDs can be used for time-released medical treatment. Lai et al. used surface-modified CdS QDs as chemically removable caps to retain drug molecules and neurotransmitters inside mesoporous silica nanospheres.13 The drug is retained inside the CdS QD cap until released by disulfide bond reducing reagents.14
Major constraints of QDs use derive from their insolubility and aggregation in most aqueous solvents as well as the leaching of heavy metals from their cores. Surface coating with functional groups can improve homogenous suspension, reduce aggregation, attenuate toxicity, and allow for conjugation of biologically active molecules, antibodies, nanogels or receptors.7, 15-17 A second major constraint involves our limited ability to deliver QDs and their associated cargoes to specific target sites inside the cell. This emphasizes the importance of a solid understanding of the intracellular dynamics and kinetics of QDs, including their mechanisms of uptake and intracellular delivery, to the development of successful application in biomedical and basic research.
Proposed mechanisms for the cellular internalization of QDs can be generally grouped into three categories: passive, facilitated and active delivery.1 Passive delivery of QDs is nonspecific and relies on electrostatic interactions between QD surface and cell membrane by endocytosis. The functional shell coating on QD surface is usually necessary for this type of transport. However, this additional modification tends to enlarge the sizes of QD and increase the difficulty of delivery across the plasma membrane.18 Active delivery of QDs involves physical manipulations, such as microinjection and electroporation. This delivery method may bring a certain degree of injury to cells and decrease delivering efficiencies.1 Finally, facilitated delivery of QDs can be achieved by peptides (such as cell-penetrating peptides, CPPs), proteins, polymers/lipids, drugs or small molecules.
The plasma membrane represents a formidable challenge for the delivery of materials; its function is to protect cells from exogenous molecules and to maintain the osmotic balance. CPPs, also known as protein transduction domains (PTDs), are short peptides containing significant amounts of basic amino acids that can permeate cell membrane. CPPs were originally derived from the Tat protein of the human immunodeficiency virus type 1.19, 20 CPPs do not require receptors or energy-dependent pathway to penetrate the membrane.21 While most recognized CPPs are derived from naturally-occurring proteins, a small number of CPP sequences have been artificially constructed. The cellular internalization of polyarginine is more efficient than that of polylysine, polyhistidine, polyornithine, and other synthetic CPPs.22 Moreover, the highest internalization efficiency is achieved using octa-arginine or nona-arginine (R9) among peptides with various chain lengths of arginine-rich CPPs.23
As a sequence capable of crossing the plasma membrane, CPPs are an attractive tool for delivering molecules (including QDs) into cells. Penetration of the plasma membrane by CPPs is not dependent on linkage with other molecules,24 and cargoes up to 200 nm in diameter can be transported across the plasma membrane by this method.25 For example, our laboratory has shown that arginine-rich CPPs can deliver proteins,26-33 DNAs,34, 35 RNAs,36 and QDs37 into cells. CPPs can be linked to these cargoes either covalently26, 27 or noncovalently.28-31, 34-37 Moreover, we have recently shown that arginine-rich CPPs can simultaneously deliver covalently- and noncovalently-bound molecules into cells.32, 33 Their ability of CPPs to transport a wide variety of cargoes into cells, along with the fact that they show little cytotoxic,38 makes arginine-rich CPPs promising candidates for safe and efficient drug carriers.
The following sections review 1) linking methods for QDs and CPPs and 2) cellular uptake mechanisms for arginine-rich CPP/QD complexes. Finally, obstacles and challenges for the further development of these carrier systems are discussed.
2. COVALENT LINKAGES BETWEEN CPPS AND QDS
QDs are effective fluorophores for in vivo imaging, intracellular labeling, and clinical applications. Thus, the ability of QDs to achieve intracellular delivery is of utmost importance. CPP-mediated intracellular delivery has received a great deal of interest and is likely to be applicable to deliver QDs. Complexing hydrophilic arginine-rich CPPs with water-insoluble QDs can increase the solubility and consequently the efficiency of delivery.22 In this section, we discuss the use of CPPs to increase cellular uptake of QDs.
2.1. Sulfosuccinimidylsuberyl Linkage
Bis(sulfosuccinimidyl)suberate (BS3) is a homobifunctional reagent that contains an amine-reactive N-hydroxysulfosuccinimide (NHS) ester at each end of spacer arm (Thermo Scientific, Pierce Biotechnology, Rockford, IL). NHS esters react with primary amines to form stable amide bonds. Recently, BS3 crosslinker was shown to conjugate amine-coated QDs with both arginine-rich CPPs39 and PTDs of Tat protein40 (Table 1). Moreover, a HA2 sequence from the influenza hemagglutinin protein can be incorporated to form HA2-Tat-QD complexes that can escape from intracellular vesicles upon acidification in cells.40
Table I.
Summary of linkages between CPPs and QDs.
| Linkage manners | CPPs | Target cells or tissues | References |
|---|---|---|---|
| Covalent linkages | |||
| Sulfosuccinimidylsuberyl linkage | R8 and R12 | HeLa cells | 39 |
| Sulfosuccinimidylsuberyl linkage | Cysteine-containing PTDs of Tat and Tat-HA2 | Rat neonatal fibroblasts and myocytes | 40 |
| Carbodiimide conjugation | PTD of Tat | QGY and MCF7 cells | 41 |
| Carbodiimide conjugation | PTD of Tat-derived peptide (GRKKRRQRRR) | hTERT-BJ1 fibroblast | 42 |
| Carbodiimide conjugation | PTD of Tat | CHO-K1 cells | 44 |
| Thio-amine coupling | Cysteine-containing PTD of Tat | Mesenchymal stem cells | 45, 46 |
| Thio-amine coupling | R11KC (RRRRRRRRRRRKC) | Vero cells | 47 |
| Thio-amine coupling | Cysteine-containing PTD of Tat | HepG2 cells | 48 |
| Thio-amine coupling |
Cysteine-containing PTD of Tat |
Brain tissues of rat |
49 |
| Noncovalent interactions | |||
| Biotin-streptavidin interaction | PTD of Tat | HeLa cells | 50 |
| Biotin-streptavidin interaction | CPP (YARVRRRGPRR) | MDA-MB-435 cells | 51 |
| Biotin-streptavidin interaction | PTD of Tat | A549 and HeLa cells | 52, 53 |
| Biotin-streptavidin interaction | CPP (H8WLA-Aib-SGRs), where Aib is α-aminoisobutyric acid | HEK 293T/17 and COS-1 cells | 54 |
| Biotin-streptavidin interaction | POD (GGG(ARKKAAKA)4) | HER 911 cells | 55 |
| Biotin-streptavidin interaction | R8 | BS-C-1 cells | 56 |
| Biotin-streptavidin interaction | R9 and cysteine-containing R9 | Swiss 3T3, HeLa and MG63 cells | 57, 58 |
| Electrostatic interaction | SR9 (R9) | A549 cells | 37 |
| Electrostatic interaction | Cysteine-containing PTD of Tat | HepG2 cells | 48 |
| Metal-affinity interaction | CPP (H8WLA-Aib-SGR8) | HEK 293T/17 and COS-1 cells | 60, 61 |
2.2. Carbodiimide Conjugation
To enhance intracellular delivery of QDs in liver and breast cancer cells, PTDs of Tat protein were coupled with QDs by 1-ethyl-3-(3-dimethylamino-propyl)-carbodiimide hydrochloride (EDC) crosslinking agent.41 EDC is a crosslinker that is often used to couple carboxyl groups to primary amines in diverse applications. This reaction is performed at a specific ratio of QD, CPP, and EDC in borate buffer for four hours at room temperature.41
Alternatively, a non-natural amino acid, tiopronin (N-2-mercaptopropionylglycine), can be used as a capping agent on the QD surface.42, 43 Tiopronin is used to treat cystinuria and rheumatold arthritis. It contains a thiol group that can attach to QDs and a free terminally carboxylic acid that provides a site for subsequent derivatization. QD-tiopronin can then couple with PTD of Tat protein in the presence of EDC.2, 42
Another coupling method involves the use of block copolymers to form various kinds of micelles with QDs.44 PTDs of Tat protein can then be crosslinked with QDs by EDC/sulfo-NHS. The resultant small spherical micelles (10 nm) are internalized by Chinese hamster ovary cells more rapidly than larger cylindrical micelles (20–30 nm diameter by >200 nm). Interestingly, the spherical micelles (polymer-QD-PTD) can exit the cell at a rate proportional to the amount of CPP loading.
2.3. Thio-Amine Coupling
Amine-encapsulated QDs have been conjugated with cysteine-containing PTDs of Tat protein using sulfosuccinimidyl-4-(N-maleimidomethyl)cyclohexane-1-carboxylate (Sulfo-SMCC) reagent.45 Sulfo-SMCC is a coupling linker that contains a NHS ester at one end that can react with a primary amine on the QD. The other end of Sulfo-SMCC consists of a maleimide group that can react with a thiol moiety in a cysteine-containing PTD, forming thioether bond. PTD-conjugated QDs can enter mesenchymal stem cells efficiently.45, 46 The distribution of stem cells thus labeled is observed primarily in the liver, lung, and spleen of nude mice.
Arginine-rich CPPs were conjugated to QDs by a two-step reaction.47 Initially, QDs are conjugated with cysteine by EDC. After removal of free cysteine by a Nap-5 column, arginine-rich lysine-cysteine-containing CPPs were secondarily crosslinked with Cys-QD using sulfo-SMCC reagent. Arginine-rich CPP-QD conjugates were delivered into the nuclear compartment of cells. This study reveals that QDs coupled with organelle-targeting signal peptides can be directed to a specific subcellular compartment.
Similar to Sulfo-SMCC, succinimidyl-[(N-maleimidopropionamido)tetraethylene glycol] ester (NHS-PEO4-MAL) is a heterobifunctional amine- and sulfhydryl-reactive crosslinker that has been recently used to conjugate cysteine-containing PTDs of Tat protein to silica-and polyacrylate-coated QDs.48 The silica and polyacrylate coatings provide multiple primary and secondary amines on the QD surface. Then, cysteine-containing PTDs are coupled with amine-coated QDs by NHS-PEO4-MAL agent. These PTD-QD nanoparticles are localized in both perinuclear regions and lysosomes after cell entry.
Cysteine-containing PTDs of Tat protein have been crosslinked to QDs using N-succinimidyl-3-(2-pyridyldithio)propionate (SPDP) to provide intra-arterial delivery to rat brain.49 QD is coated with an amine-functionalized silica layer. SPDP is a heterobifunctional crosslinker that contains an amine-reactive NHS ester at one end. The other end of SPDP is a pyridyl disulfide group that reacts with sulfhydryls to form a reversible disulfide bond (Thermo Scientific). The PTDs were necessary to deliver these conjugated QDs through the blood-brain-barrier (BBB) and into brain tissue.
3. NONCOVALENT INTERACTIONS BETWEEN CPPS AND QDS
CPP-functionalized QDs can be prepared by either covalent linkage or noncovalent interactions. Covalent coupling methods tend to produce larger nanoparticles (10–50 nm) with greater colloidal stability.48 In contrast, noncovalent approaches are simple and produce smaller nanoparticles (< 10 nm); however, the weak binding between peptides and QDs results in poor colloidal stability.47 Three commonly used noncovalent interactions are described below.
3.1. Biotin-Streptavidin Interaction
Coupling CPPs to QDs by biotin-streptavidin conjugation is the most popular approach to facilitated intracellular delivery of QDs.50-58 This method is easily customizable, requires minimal conjugation reactions, and requires only commercially available streptavidin-conjugated QDs.57 Biotinylated CPPs are conjugated with streptavidin-coated QDs at an empirically determined appropriate ratio for one hour at room temperature.53 Then cells are incubated with CPP-QD conjugates for one hour. The uniformity of cell labeling by the CPP-QD conjugation can be evaluated by flow cytometry, whereas intracellular localization can be characterized by fluorescent or confocal microscope. Efficient intracellular delivery of QDs depends on the presence of CPPs.54
3.2. Electrostatic Interactions
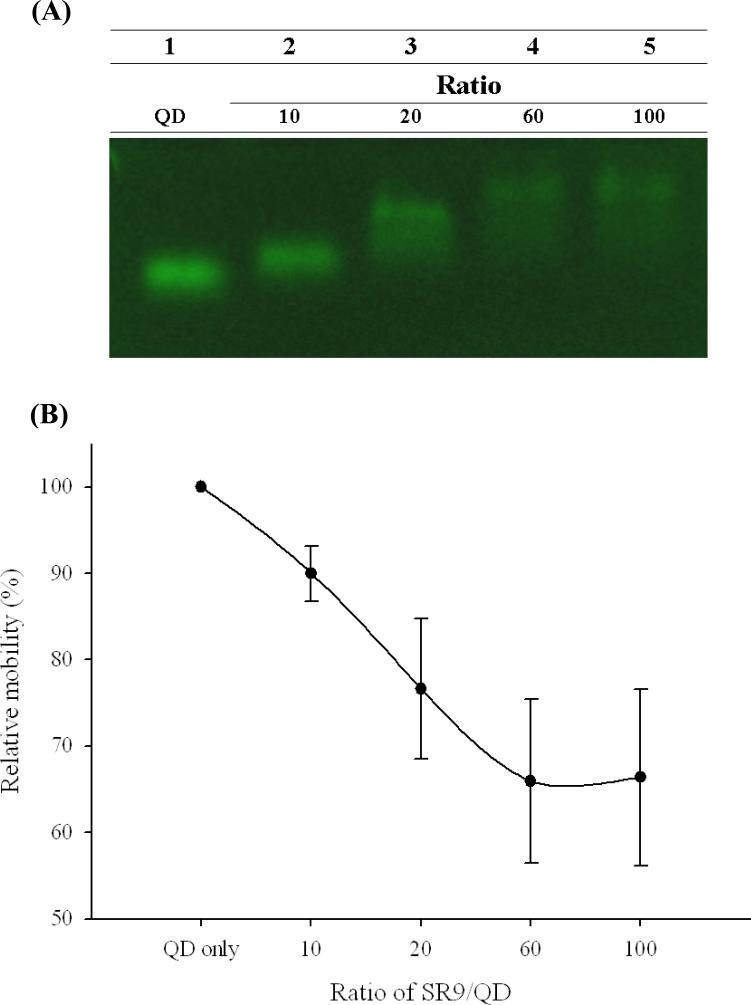
Our laboratory has recently demonstrated that synthetic nona-arginine (SR9) peptides (arginine-rich CPPs) interact with carboxyl-functionalized green QDs to form relatively stable noncovalent complexes in vitro.37 Agarose-based gel retardation demonstrated that SR9 peptides and carboxylated QDs form stable complexes (Fig. 1A); gel mobility of QDs decreased as the concentration of SR9 increased. The greatest retardation of the SR9/QD complex mobility occurred at SR9/QD molecular ratio of 60 (Fig. 1B). Higher ratios did not further diminish complex mobility. These results indicate that SR9 interacts with QDs to form stable noncovalent complexes.
Fig. 1.
Gel retardation assay of noncovalent SR9/QD complexes. (A) Gel retardation showing interactions between SR9 peptides and QDs. Different amounts of SR9 were mixed with QDs at molecular ratios of 0 (QD only), 10, 20, 60, and 100, respectively. After the incubation with agitation for one hour, SR9 and QDs mixtures were analyzed by electrophoresis on a 0.5% agarose gel. QD fluorescence was visualized with excitation at 488 nm. (B) Relative mobility shift of SR9/QD complexes in electrophoresis. Relative mobility percentage of QDs (y-axis) was plotted against various ratios between SR9 and QDs (x-axis).
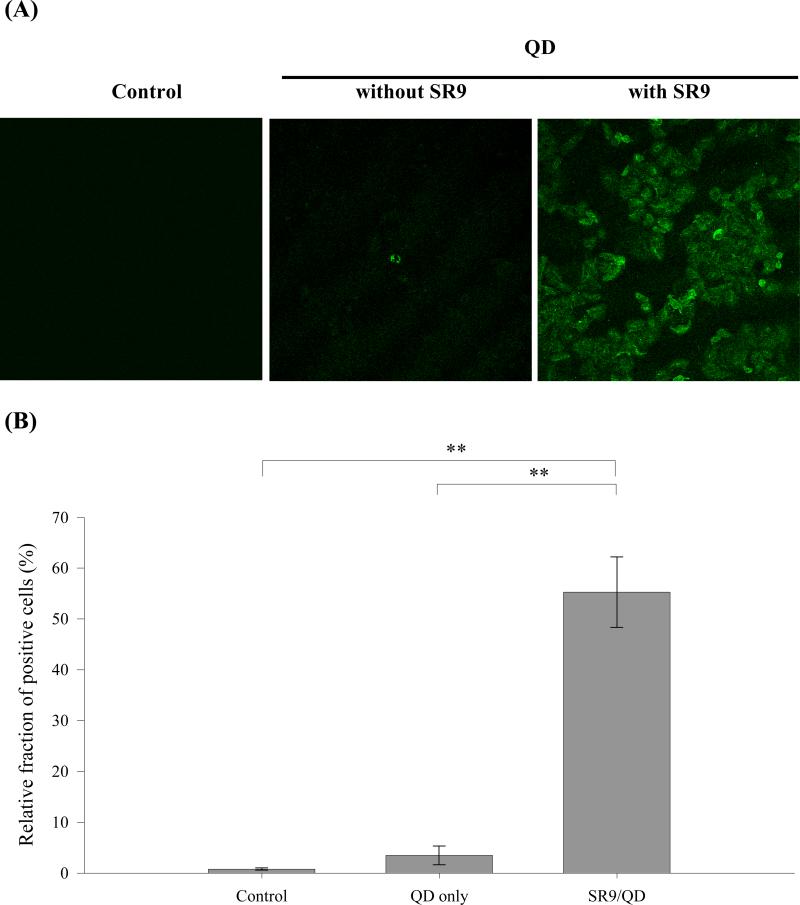
To determine the rate and efficiency of SR9/QD complexes uptake, human lung cancer cells (A549) were exposed to QDs or noncovalently associated CPP/QD complexes, and then analyzed by confocal microscopy (Fig. 2A) and flow cytometry (Fig. 2B). Control cells emitted no fluorescence under confocal microscopy (left panel in Fig. 2A), and only a very small fraction of the control cell population (0.80 ± 0.24%) displayed positive fluorescent signal under flow cytometry (left panel in Fig. 2B). Only 3.46 ± 1.84% of the cell population displayed green fluorescence when cells were treated with QDs only for one hour (middle panels in Fig. 2A and B). In contrast, 55.29 ± 6.94% of the cell population exhibited green fluorescence when cells were treated with SR9/QD complexes for one hour (right panels in Fig. 2A and B). This demonstrates that noncovalent association with arginine-rich CPPs can increase the rate and efficiency of QD uptake in living cells.
Fig. 2.
Confocal microscopy of cellular uptake of SR9/QD complexes. (A) Confocal microscopic images of cells treated with QD or SR9/QD complexes. Human lung carcinoma A549 cells treated with mock as a control, 100 nM of QD (Evident Technologies, Troy, NY), and SR9/QD complexes at a molecular ratio of 60:1 (6 μM of SR9 peptide premixed with 100 nM of QD) for 1 hour were shown on the left, middle, and right, respectively. All images were recorded by the TCS SL confocal microscope system (Leica, Wetzlar, Germany) and shown at a magnification of 200X. (B) Efficiency of cellular uptake of QD or SR9/QD complexes. Cells were treated with different conditions as described above and analyzed by the Cytomics FC500 flow cytometer (Beckman Coulter, Fullerton, CA). Significant differences were shown for P < 0.01 (**).
Electrostatic interactions between cysteine-containing PTDs of Tat protein and QDs can be achieved using a direct ligand-exchange method.48 CPPs containing one additional cysteine residue were chemically synthesized, and QDs are prepared in a reverse micellar system. The sulfhydryl groups should allow electrostatic adsorption to the QD surface when the reverse micellar system is disrupted.59 Partial precipitation of the CPP-QD complex is observed upon longer storage.48 Compared to other covalent CPP-QD conjugates, this noncovalent CPP-QD complex has a lower colloidal stability and is more cytotoxic due to the weak binding of the ligands.
3.3. Metal-Affinity Interactions
Arginine-rich CPPs can noncovalently bind to the surface of QDs surface-capped with dihydrolipoic acid (DHLA) via metal-affinity coordination between a polyhistidine tract present at the peptide's terminus and the QD surface's Zn atoms.1, 60, 61 CPP-mediated QD uptake is dependent on conjugate concentration, while exposure of cells to nonconjugated QDs results in negligible intracellular labeling. Thus the presence or absence of arginine-rich CPPs on the QD surface influences cellular uptake.
4. MECHANISMS OF CPP-ENHANCED CELLULAR INTERNALIZATION OF QDS
QD uptake by cells may occur by several different mechanisms, depending on the surface coating, size and charge of QDs.62 The mechanism of delivery of CPPs and their associated cargoes into cells is incompletely understood. Evidence has been presented for both endocytosis (or more specifically macropinocytosis) and direct membrane translocation of CPPs, although other mechanisms have also been proposed.18, 22, 52, 56
4.1. Macropinocytosis
Endocytosis is a cellular process that delivers macromolecules into the cell in membrane-bound vesicles.63 Recent studies proposed that a specialized form of endocytosis, known as the lipid raft-dependent macropinocytosis, plays an important role in the cellular uptake of CPPs and cargoes.52, 56, 64 Macropinocytosis accompanies the membrane ruffling that is induced in many cell types upon stimulation by growth factors or other signals.63 The signaling cascades that induce macropinocytosis trigger actin-driven formation of membrane protrusions. These membrane protrusions collapse onto and fuse with the plasma membrane to generate large endocytic vesicles, called macropinosomes. Macropinosomes are greater than 0.2 μm in diameter and can be as large as 5 μm.62 However, little is known about the participation of CPPs and cargoes in the fusion process with macropinosomes, or their release into the cytoplasm or nucleus after endosomal escape.
4.2. Direct Membrane Translocation
A direct membrane translocation mechanism for CPPs involving a passive membrane diffusive or destabilization process that does not entail binding to cell surface receptors was initially proposed.25 Many recent studies support a direct pore-opening mechanism for CPP entry.18, 22, 65-69 The direct membrane translocation mechanism is comprised of four steps: 1) CPPs first bind to phosphate groups of phospholipids on the surface of cell membrane; 2) the arrangement of lipids is disrupted as the surface concentration of CPPs increases; 3) side chains of arginines translocate through the distal layer and form a water pore; and 4) a few CPPs translocate by diffusing on the surface of the pore, and finally the transient pore closes.68 The complete translocation of a CPP and closing of the pore occur on a microsecond timescale. Moreover, the radius of the pore varies in size with a maximal diameter of 2.5 nm, and the pore surface is lined up with phosphate groups.68
CPPs use both endocytosis and direct penetration for cellular internalization, but to different extents. Guterstam et al. found that the pathway for cellular uptake of arginine-rich CPPs is dominated by direct membrane translocation, whereas the pathway for cellular delivery of arginine-rich CPP-mediated DNA transport is dominated by endocytosis.22 Jiao et al. reported that direct membrane translocation occurs at low extracellular CPP concentrations, while endocytosis is activated at higher CPP concentrations.66 Reuter et al. found that fluid vesicles are more easily penetrated by CPPs than gel state vesicles, and polyarginine translocates through the membrane more easily than polylysine.67 Ter-Avetisyan et al. reported that the PTD of Tat protein directly penetrates the plasma membrane, and internalization of PTD peptide is independent of endocytosis.65
5. OUTLOOK
Several aspects of QDs and carriers interactions need additional engineering before QDs can be reliably incorporated into biological applications. Delehanty et al. suggest three areas of QDs development that will receive the most attention in the near future: water solubility, cellular delivery, and toxicity.3 Another area for development lies in turning QD emission: owing to quantum confinement effects, the emission of QDs could be potentially tuned from 400 to 2,000 nm by altering particle size.5, 70 Recently, hybrid organic QD light-emitting device (QD-LED) efficiency was improved by the use of different colloidal QDs and a robust QD deposition method.71 Spectrally narrow electroluminescence of these QD-LEDs is tunable over the entire visible spectra (460–650 nm).
QD nanocrystals can be used to target intracellular delivery with the help of CPPs in biological and medical applications.72 Mechanisms of CPPs in intracellular delivery are still one of great challenges for further investigation. While mechanisms involving both endocytosis and direct membrane translocation appear to be involved, many questions remain. The basic amino acids are essential for translocation, and membrane binding is the first step in endocytic uptake. However, there is no consensus regarding the specific endocytic pathway used for the import of CPPs. Moreover, it is difficult to reconcile our ideas with the efficient uptake of the CPP transportan 10, which has no arginine residues.22, 73
Gump et al. recently reported that the binding of PTD of Tat protein to acidic glycosaminoglycans on the cell surface is independent of the CPP-mediated transduction mechanism.74 This has revised the role of heparin sulfate proteoglycans which were suspected to be the receptors of CPP-mediated cellular transduction on the cell surface. Enzymatic removal of proteins from the cell surface completely ablates PTD-mediated transduction. Further study is needed to determine the protein(s) on cell surface required for protein transduction.
Target-specific delivery of QDs to specific organelles in cells is an important goal of CPP-mediated delivery. As far as endocytosis appears to be one of the primary uptake mechanisms for facilitated delivery mediated by CPPs, QDs often aggregate inside living cells trapped in organelles, such as vesicles, endosomes, and lysosomes.1 El-Sayed et al. suggest that escape from the endocytic vesicles is a bottleneck to the efficient delivery of functional macromolecules intracellularly mediated by arginine-rich CPPs.75 After endocytic uptake, the internalized arginine-rich CPPs, either alone or linked to cargoes, must escape from the endocytic vesicles into the cytosol to avoid degradation,54, 75 although arginine-rich CPPs and cargoes have been reported to be able to reach the cell nucleus.47, 50, 76, 77 Several strategies have been proposed to overcome endosomal entrapment, including incorporation of the lysosomotropic agent chloroquine22 or as endosome disruptive peptides, such as HA2 peptide,39, 78, 79 INF7 peptide,75 deca-histidine,80 GALA peptide,81 and Pas peptide, into the transport complex.82
Activatable CPPs (ACPPs) have been recently developed as novel vehicles for payload delivery into cells in vitro and in vivo.83, 84 ACPPs contain three covalently attached parts: arginine-rich CPPs, peptide linkers and polyanionic inhibitory domains. Cleavage of the linkers by specific proteases, such as matrix metalloproteinase-2, dissociates the polyanion, and enables the arginine-rich CPPs to enter cells. In contrast to their CPP counterparts, ACPPs have relatively high target specificity, less toxicity, and are nonadherent and distribute uniformly in normal tissues, nude mice,84 genetic knockouts, primary tumors, and associated metastasis.85
Acknowledgments
We are grateful to Dr. Robert S. Aronstam from the Department of Biological Sciences, Missouri University of Science and Technology, for editing of the manuscript. This work was supported by Award Number R15EB009530 from the National Institute of Biomedical Imaging and Bioengineering (to Y.W.H.) and the National Science Council (NSC 97-2621-B-259-003-MY3) of Taiwan (to H.J.L.).
Abbreviations
- ACPP
activatable cell-penetrating peptide
- BS3
bis(sulfosuccinimidyl)suberate
- CPP
cell-penetrating peptide
- DHLA
dihydrolipoic acid
- EDC
1-ethyl-3-(3-dimethylamino-propyl)-carbodiimide
- LED
light-emitting device
- NHS
N-hydroxysulfosuccinimide
- NHS-PEO4-MAL
succinimidyl-[(N-maleimidopropionamido)tetraethylene glycol] ester
- PTD
protein transduction domain
- QD
quantum dot
- R9
nona-arginine
- SPDP
N-succinimidyl-3-(2-pyridyldithio)propionate
- SR9
synthetic nona-arginine
- Sulfo-SMCC
sulfosuccinimidyl-4-(N-maleimidomethyl)cyclohexane-1-carboxylate
Biography
 Betty Revon Liu received a bachelor's degree in Clinical Laboratory Sciences and Medical Biotechnology from the College of Medicine, National Taiwan University in 2002 and a M.S. in Biotechnology from the National Dong Hwa University in 2007. In 2003, she was a research assistant in Cancer Research Center, National Taiwan University and was devoted to cancer research. She is pursuing her Ph.D. in the Institute of Biotechnology, National Dong Hwa University now. Her Ph.D. research focuses on molecules (peptides or nanomolecules) delivery and molecular cell biology.
Betty Revon Liu received a bachelor's degree in Clinical Laboratory Sciences and Medical Biotechnology from the College of Medicine, National Taiwan University in 2002 and a M.S. in Biotechnology from the National Dong Hwa University in 2007. In 2003, she was a research assistant in Cancer Research Center, National Taiwan University and was devoted to cancer research. She is pursuing her Ph.D. in the Institute of Biotechnology, National Dong Hwa University now. Her Ph.D. research focuses on molecules (peptides or nanomolecules) delivery and molecular cell biology.
 Yue-wern Huang received a B.S. and a M.Sc. in Biology, from National Taiwan Normal University, and a Ph.D. in Zoology, with Professor William H. Karasov, from the University of Wisconsin-Madison in 1998. His Ph.D. research focused on toxicity and mechanisms of polychlorinated biphenyls and Dioxins on amphibians. His postdoctoral work, with Professor Timothy R. Zacharewski at the Department of Biochemistry and Molecular Biology at Michigan State University focused on endocrine disruption in the environment. In 2000 he jointed the Department of Biological Sciences of Missouri University of Science and Technology (M S&T) as a tenure-track Assistant Professor. His research has been focused on 1) identifying endocrine modulators in the environments and their effects on aquatic organisms; 2) elucidating toxicity mechanisms of nanomaterials, particularly metal oxides, and 3) establishing a system to deliver biologically active molecules into cells using quantum dots as imaging molecules and cell-penetrating peptides as carriers. The system will eventually be applicable to in vivo systems.
Yue-wern Huang received a B.S. and a M.Sc. in Biology, from National Taiwan Normal University, and a Ph.D. in Zoology, with Professor William H. Karasov, from the University of Wisconsin-Madison in 1998. His Ph.D. research focused on toxicity and mechanisms of polychlorinated biphenyls and Dioxins on amphibians. His postdoctoral work, with Professor Timothy R. Zacharewski at the Department of Biochemistry and Molecular Biology at Michigan State University focused on endocrine disruption in the environment. In 2000 he jointed the Department of Biological Sciences of Missouri University of Science and Technology (M S&T) as a tenure-track Assistant Professor. His research has been focused on 1) identifying endocrine modulators in the environments and their effects on aquatic organisms; 2) elucidating toxicity mechanisms of nanomaterials, particularly metal oxides, and 3) establishing a system to deliver biologically active molecules into cells using quantum dots as imaging molecules and cell-penetrating peptides as carriers. The system will eventually be applicable to in vivo systems.
 Huey-Jenn Chiang received a B.S. in Chemistry from Tamkang University in 1976. He completed his Ph.D. in Bio-inorganic Chemistry from California Institute of Technology in 1987. He then carried out postdoctoral research at Stanford University and at California Institute of Technology, respectively. From 1994 to 1997, Dr. Chiang was a faculty member in Department of Bioengineering at Tatung University. In 1997, Dr. Chiang moved to National Dong Hwa University and joined the faculties in Department of Life Science and Institute of Biotechnology. His research involves the studies of Lab-on-a-CD, asymmetric photolysis of chiral molecules, electron transfers in native and non-covalently modified DNA, dynamics of pharmaceutical formulations, and cell-penetrating peptides.
Huey-Jenn Chiang received a B.S. in Chemistry from Tamkang University in 1976. He completed his Ph.D. in Bio-inorganic Chemistry from California Institute of Technology in 1987. He then carried out postdoctoral research at Stanford University and at California Institute of Technology, respectively. From 1994 to 1997, Dr. Chiang was a faculty member in Department of Bioengineering at Tatung University. In 1997, Dr. Chiang moved to National Dong Hwa University and joined the faculties in Department of Life Science and Institute of Biotechnology. His research involves the studies of Lab-on-a-CD, asymmetric photolysis of chiral molecules, electron transfers in native and non-covalently modified DNA, dynamics of pharmaceutical formulations, and cell-penetrating peptides.
 Han-Jung Lee received a B.Ed. in Biology from the National Changhua University of Education in 1983 and a M.S. in Molecular Biology from the National Tsing Hua University in 1985 in Taiwan. He completed his Ph.D. in Endocrinology-Reproductive Physiology from the University of Wisconsin, Madison, in 1996. He then moved on to a postdoctoral work at the National Institutes of Health (NIH). Dr. Lee joined the faculty in the Department of Life Science and Institute of Biotechnology in 1998, and moved to the Department of Natural Resources and Environmental Studies in 2009 at the National Dong Hwa University in Taiwan. His research group focuses on the study of arginine-rich intracellular delivery (AID) peptides (cell-penetrating peptides). He currently has projects focused on DNA delivery, biodiversity, and nanotechnology. He is the recipient of The Anderson Fellowship of the Comprehensive Cancer Center from the University of Wisconsin-Madison, Intramural Research Training Award of the NIH, and Faculty Research Awards of the National Dong Hwa University.
Han-Jung Lee received a B.Ed. in Biology from the National Changhua University of Education in 1983 and a M.S. in Molecular Biology from the National Tsing Hua University in 1985 in Taiwan. He completed his Ph.D. in Endocrinology-Reproductive Physiology from the University of Wisconsin, Madison, in 1996. He then moved on to a postdoctoral work at the National Institutes of Health (NIH). Dr. Lee joined the faculty in the Department of Life Science and Institute of Biotechnology in 1998, and moved to the Department of Natural Resources and Environmental Studies in 2009 at the National Dong Hwa University in Taiwan. His research group focuses on the study of arginine-rich intracellular delivery (AID) peptides (cell-penetrating peptides). He currently has projects focused on DNA delivery, biodiversity, and nanotechnology. He is the recipient of The Anderson Fellowship of the Comprehensive Cancer Center from the University of Wisconsin-Madison, Intramural Research Training Award of the NIH, and Faculty Research Awards of the National Dong Hwa University.
References and Notes
- 1.Delehanty JB, Mattoussi H, Medintz IL. Anal. Bioanal. Chem. 2009;393:1091. doi: 10.1007/s00216-008-2410-4. [DOI] [PubMed] [Google Scholar]
- 2.Stewart KM, Horton KL, Kelley SO. Org. Biomol. Chem. 2008;6:2242. doi: 10.1039/b719950c. [DOI] [PubMed] [Google Scholar]
- 3.Delehanty JB, Boeneman K, Bradburne CE, Robertson K, Medintz IL. Expert Opin. Drug Deliv. 2009;6:1091. doi: 10.1517/17425240903167934. [DOI] [PubMed] [Google Scholar]
- 4.Iga AM, Robertson JHP, Winslet MC, Seifalian AM. J. Biomed. Biotechnol. 2007;2007:76087. doi: 10.1155/2007/76087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou M, Ghosh I. Biopolymers. 2007;88:325. doi: 10.1002/bip.20655. [DOI] [PubMed] [Google Scholar]
- 6.Gao X, Yang L, Petros JA, Marshall FF, Simons JW, Nie S. Curr. Opin. Biotechnol. 2005;16:63. doi: 10.1016/j.copbio.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Michalet X, Pinaud FF, Bentolila LA, Tsay JM, Doose S, Li JJ, Sundaresan G, Wu AM, Gambhir SS, Weiss S. Science. 2005;307:538. doi: 10.1126/science.1104274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen F, Gerion D. Nano Lett. 2004;4:1827. [Google Scholar]
- 9.Wu X, Liu H, Liu J, Haley KN, Treadway JA, Larson JP, Ge N, Peale F, Bruchez MP. Nat. Biotechnol. 2003;21:41. doi: 10.1038/nbt764. [DOI] [PubMed] [Google Scholar]
- 10.Soltesz EG, Kim S, Kim SW, Laurence RG, De Grand AM, Parungo CP, Cohn LH, Bawendi MG, Frangioni JV. Ann. Surg. Oncol. 2006;13:386. doi: 10.1245/ASO.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 11.Parungo CP, Ohnishi S, Kim SW, Kim S, Laurence RG, Soltesz EG, Chen FY, Colson YL, Cohn LH, Bawendi MG, Frangioni JV. J. Thorac. Cardiovasc. Surg. 2005;129:844. doi: 10.1016/j.jtcvs.2004.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ozkan M. Drug Discov. Today. 2004;9:1065. doi: 10.1016/S1359-6446(04)03291-X. [DOI] [PubMed] [Google Scholar]
- 13.Lai CY, Trewyn BG, Jeftinija DM, Jeftinija K, Xu S, Jeftinija S, Lin VS. J. Am. Chem. Soc. 2003;125:4451. doi: 10.1021/ja028650l. [DOI] [PubMed] [Google Scholar]
- 14.Alivisatos AP, Gu W, Larabell C. Annu. Rev. Biomed. Eng. 2005;7:55. doi: 10.1146/annurev.bioeng.7.060804.100432. [DOI] [PubMed] [Google Scholar]
- 15.Pathak S, Tolentino R, Nguyen K, D’Amico L, Barron E, Cheng L, Freeman WR, Silva GA. J. Nanosci. Nanotechnol. 2009;9:5047. doi: 10.1166/jnn.2009.gr08. [DOI] [PubMed] [Google Scholar]
- 16.Toita S, Hasegawa U, Koga H, Sekiya I, Muneta T, Akiyoshi K. J. Nanosci. Nanotechnol. 2008;8:2279. doi: 10.1166/jnn.2008.240. [DOI] [PubMed] [Google Scholar]
- 17.Manokaran S, Berg A, Zhang X, Chen W, Srivastava DK. J. Biomed. Nanotechnol. 2008;4:491. doi: 10.1166/jbn.2008.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jablonski AE, Humphries WH, Payne CK. J. Phys. Chem. B. 2009;113:405. doi: 10.1021/jp809956w. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Green M, Loewenstein PM. Cell. 1988;55:1179. doi: 10.1016/0092-8674(88)90262-0. [DOI] [PubMed] [Google Scholar]
- 20.Frankel AD, Pabo CO. Cell. 1988;55:1189. doi: 10.1016/0092-8674(88)90263-2. [DOI] [PubMed] [Google Scholar]
- 21.Suzuki T, Futaki S, Niwa M, Tanaka S, Ueda K, Sugiura Y. J. Biol. Chem. 2002;277:2437. doi: 10.1074/jbc.M110017200. [DOI] [PubMed] [Google Scholar]
- 22.Guterstam P, Madani F, Hirose H, Takeuchi T, Futaki S, El-Andaloussi S, Graslund A, Langel U. Biochim. Biophys. Acta. 2009;1788:2509. doi: 10.1016/j.bbamem.2009.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Futaki S, Suzuki T, Ohashi W, Yagami T, Tanaka S, Ueda K, Sugiura Y. J. Biol. Chem. 2001;276:5836. doi: 10.1074/jbc.M007540200. [DOI] [PubMed] [Google Scholar]
- 24.Fonseca SB, Pereira MP, Kelley SO. Adv. Drug Deliv. Rev. 2009;61:953. doi: 10.1016/j.addr.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 25.Wadia JS, Dowdy SF. Curr. Opin. Biotechnol. 2002;13:52. doi: 10.1016/s0958-1669(02)00284-7. [DOI] [PubMed] [Google Scholar]
- 26.Chang M, Chou JC, Lee HJ. Plant Cell Physiol. 2005;46:482. doi: 10.1093/pcp/pci046. [DOI] [PubMed] [Google Scholar]
- 27.Liu K, Lee HJ, Leong SS, Liu CL, Chou JC. J. Plant Growth Regul. 2007;26:278. [Google Scholar]
- 28.Wang YH, Chen CP, Chan MH, Chang M, Hou YW, Chen HH, Hsu HR, Liu K, Lee HJ. Biochem. Biophys. Res. Commun. 2006;346:758. doi: 10.1016/j.bbrc.2006.05.205. [DOI] [PubMed] [Google Scholar]
- 29.Chang M, Chou JC, Chen CP, Liu BR, Lee HJ. New Phytol. 2007;174:46. doi: 10.1111/j.1469-8137.2007.01977.x. [DOI] [PubMed] [Google Scholar]
- 30.Hou YW, Chan MH, Hsu HR, Liu BR, Chen CP, Chen HH, Lee HJ. Exp. Dermatol. 2007;16:999. doi: 10.1111/j.1600-0625.2007.00622.x. [DOI] [PubMed] [Google Scholar]
- 31.Liu BR, Chou JC, Lee HJ. J. Membrane Biol. 2008;222:1. doi: 10.1007/s00232-008-9096-6. [DOI] [PubMed] [Google Scholar]
- 32.Hu JW, Liu BR, Wu CY, Lu SW, Lee HJ. Peptides. 2009;30:1669. doi: 10.1016/j.peptides.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 33.Lu SW, Hu JW, Liu BR, Lee CY, Li JF, Chou JC, Lee HJ. J. Agric. Food Chem. 2010 doi: 10.1021/jf903039j. in press. [DOI] [PubMed] [Google Scholar]
- 34.Chen CP, Chou JC, Liu BR, Chang M, Lee HJ. FEBS Lett. 2007;581:1891. doi: 10.1016/j.febslet.2007.03.076. [DOI] [PubMed] [Google Scholar]
- 35.Li JF, Huang Y, Chen RL, Lee HJ. Anticancer Res. 2010 in press. [Google Scholar]
- 36.Wang YH, Hou YW, Lee HJ. J. Biochem. Biophys. Methods. 2007;70:579. doi: 10.1016/j.jbbm.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Liu BR, Li JF, Lu SW, Lee HJ, Huang YW, Shannon KB, Aronstam RS. J. Nanosci. Nanotechnol. 2010 doi: 10.1166/jnn.2010.2637. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kilk K, Mahlapuu R, Soomets U, Langel U. Toxicol. 2009;265:87. doi: 10.1016/j.tox.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 39.Takayama K, Tadokoro A, Pujals S, Nakase I, Giralt E, Futaki S. Bioconjug. Chem. 2009;20:249. doi: 10.1021/bc800327f. [DOI] [PubMed] [Google Scholar]
- 40.Koshman YE, Waters SB, Walker LA, Los T, de Tombe P, Goldspink PH, Russell B. J. Mol. Cell. Cardiol. 2008;45:853. doi: 10.1016/j.yjmcc.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xue FL, Chen JY, Guo J, Wang CC, Yang WL, Wang PN, Lu DR. J. Fluoresc. 2007;17:149. doi: 10.1007/s10895-006-0152-2. [DOI] [PubMed] [Google Scholar]
- 42.de la Fuente JM, Fandel M, Berry CC, Riehle M, Cronin L, Aitchison G, Curtis ASG. ChemBioChem. 2005;6:989. doi: 10.1002/cbic.200500071. [DOI] [PubMed] [Google Scholar]
- 43.Lam KM, Chan PH, Wong KY. J. Nanosci. Nanotechnol. 2009;9:2337. doi: 10.1166/jnn.2009.se30. [DOI] [PubMed] [Google Scholar]
- 44.Zhang K, Fang H, Chen Z, Taylor JSA, Wooley KL. Bioconjug. Chem. 2008;19:1880. doi: 10.1021/bc800160b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lei Y, Tang H, Yao L, Yu R, Feng M, Zou B. Bioconjug. Chem. 2008;19:421. doi: 10.1021/bc0700685. [DOI] [PubMed] [Google Scholar]
- 46.Lei Y, Tang H, Feng M, Zou B. J. Nanosci. Nanotechnol. 2009;9:5726. doi: 10.1166/jnn.2009.1258. [DOI] [PubMed] [Google Scholar]
- 47.Hoshino A, Fujioka K, Oku T, Nakamura S, Suga M, Yamaguchi Y, Suzuki K, Yasuhara M, Yamamoto K. Microbiol. Immunol. 2004;48:985. doi: 10.1111/j.1348-0421.2004.tb03621.x. [DOI] [PubMed] [Google Scholar]
- 48.Wei Y, Jana NR, Tan SJ, Ying JY. Bioconjug. Chem. 2009;20:1752. doi: 10.1021/bc8003777. [DOI] [PubMed] [Google Scholar]
- 49.Santra S, Yang H, Stanley JT, Holloway PH, Moudgil BM, Walter G, Mericle RA. Chem. Commun. 2005;25:3144. doi: 10.1039/b503234b. [DOI] [PubMed] [Google Scholar]
- 50.Nitin N, LaConte L, Rhee WJ, Bao G. Ann. Biomed. Eng. 2009;37:2018. doi: 10.1007/s10439-009-9768-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mork H, Bae KH, Ahn CH, Park TG. Langmuir. 2009;25:1645. doi: 10.1021/la803542v. [DOI] [PubMed] [Google Scholar]
- 52.Chen B, Liu Q, Zhang Y, Xu L, Fang X. Langmuir. 2008;24:11866. doi: 10.1021/la802048s. [DOI] [PubMed] [Google Scholar]
- 53.Ruan G, Agrawai A, Marcus AI, Nie S. J. Am. Chem. Soc. 2007;129:14759. doi: 10.1021/ja074936k. [DOI] [PubMed] [Google Scholar]
- 54.Medintz IL, Pons T, Delehanty JB, Susumu K, Brunel FM, Dawson PE, Mattoussi H. Bioconjug. Chem. 2008;19:1785. doi: 10.1021/bc800089r. [DOI] [PubMed] [Google Scholar]
- 55.Johnson LN, Cashman SM, Kumar-Singh R. Mol. Ther. 2008;16:107. doi: 10.1038/sj.mt.6300324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hess GT, Humphries WH, Fay NC, Payne CK. Biochim. Biophs. Acta. 2007;1773:1583. doi: 10.1016/j.bbamcr.2007.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lagerholm BC. Methods Mol. Biol. 2007;374:105. doi: 10.1385/1-59745-369-2:105. [DOI] [PubMed] [Google Scholar]
- 58.Lagerholm BC, Wang M, Ernst LA, Ly DH, Liu H, Bruchez MP, Waggoner AS. Nano Lett. 2004;4:2019. [Google Scholar]
- 59.Derfus AM, Chan WCW, Bhatia SN. Adv. Mater. 2004;16:961. [Google Scholar]
- 60.Delehanty JB, Medintz IL, Pons T, Brunel FM, Dawson PE, Mattoussi H. Bioconjug. Chem. 2006;17:920. doi: 10.1021/bc060044i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sapsford KE, Pons T, Medintz IL, Higashiya S, Brunel FM, Dawson PE, Mattoussi H. J. Phys. Chem. C. 2007;111:11528. [Google Scholar]
- 62.Zhang LW, Monteiro-Riviere NA. Toxicol. Sci. 2009;110:138. doi: 10.1093/toxsci/kfp087. [DOI] [PubMed] [Google Scholar]
- 63.Conner SD, Schmid SL. Nature. 2003;422:37. doi: 10.1038/nature01451. [DOI] [PubMed] [Google Scholar]
- 64.Wadia JS, Stan RV, Dowdy SF. Nat. Med. 2004;10:310. doi: 10.1038/nm996. [DOI] [PubMed] [Google Scholar]
- 65.Ter-Avetisyan G, Tunnemann G, Nowak D, Nitschke M, Herrmann D, Drab M, Cardoso MC. J. Biol. Chem. 2009;284:3370. doi: 10.1074/jbc.M805550200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jiao CY, Delaroche D, Burlina F, Alves ID, Chassaing G, Sagan S. J. Biol. Chem. 2009;284:33957. doi: 10.1074/jbc.M109.056309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reuter M, Schwieger C, Meister A, Karlsson G, Blume A. Biophy. Chem. 2009;144:27. doi: 10.1016/j.bpc.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 68.Herce HD, Garcia AE, Litt J, Kane RS, Martin P, Enrique N, Rebolledo A, Milesi V. Biophy. J. 2009;97:1917. doi: 10.1016/j.bpj.2009.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schmidt N, Mishra A, Lai GH, Wong GC. FEBS Lett. 2010 doi: 10.1016/j.febslet.2009.11.046. in press. [DOI] [PubMed] [Google Scholar]
- 70.Murray CB, Kagan CR, Bawendi MG. Ann. Rev. Mater. Sci. 2000;30:545. [Google Scholar]
- 71.Anikeeva PO, Halpert JE, Bawendi MG, Bulovic V. Nano Lett. 2009;9:2532. doi: 10.1021/nl9002969. [DOI] [PubMed] [Google Scholar]
- 72.Fonseca SB, Pereira MP, Kelley SO. Adv. Drug Deliv. Rev. 2009;61:953. doi: 10.1016/j.addr.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 73.Soomets U, Lindgren M, Gallet X, Hallbrink M, Elmquist A, Balaspiri L, Zorko M, Pooga M, Brasseur R, Langel U. Biochim. Biophy. Acta. 2000;1467:165. doi: 10.1016/s0005-2736(00)00216-9. [DOI] [PubMed] [Google Scholar]
- 74.Gump JM, June RK, Dowdy SF. J. Biol. Chem. 2010;285:1500. doi: 10.1074/jbc.M109.021964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.El-Sayed A, Futaki S, Harashima H. AAPS J. 2009;11:13. doi: 10.1208/s12248-008-9071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vives E, Brodin P, Lebleu B. J. Biol. Chem. 1997;272:16010. doi: 10.1074/jbc.272.25.16010. [DOI] [PubMed] [Google Scholar]
- 77.Melikov K, Chernomordik LV. Cell. Mol. Life Sci. 2005;62:2739. doi: 10.1007/s00018-005-5293-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sugita T, Yoshikawa T, Mukai Y, Yamanada N, Imai S, Nagano K, Yoshida Y, Shibata H, Yoshioka Y, Nakagawa S, Kamada H, Tsunoda S, Tsutsumi Y. Biochem. Biophys. Res. Commun. 2007;363:1027. doi: 10.1016/j.bbrc.2007.09.077. [DOI] [PubMed] [Google Scholar]
- 79.Neundorf I, Rennert R, Hoyer J, Schramm F, Lobner K, Kitanovic I, Wolfl S. Pharmaceuticals. 2009;2:49. doi: 10.3390/ph2020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lo SL, Wang S. Biomaterials. 2008;29:2408. doi: 10.1016/j.biomaterials.2008.01.031. [DOI] [PubMed] [Google Scholar]
- 81.Kobayashi S, Nakase I, Kawabata N, Yu HH, Pujals S;, Imanishi M, Giralt E, Futaki S. Bioconjug. Chem. 2009;20:953. doi: 10.1021/bc800530v. [DOI] [PubMed] [Google Scholar]
- 82.Takayama K, Nakase I, Michiue H, Takeuchi T, Tomizawa K, Matsui H, Futaki S. J. Control. Release. 2009;138:128. doi: 10.1016/j.jconrel.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 83.Jiang T, Olson ES, Nguyen QT, Roy M, Jennings PA, Tsien RY. Proc. Natl. Acad. Sci. USA. 2004;101:17867. doi: 10.1073/pnas.0408191101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aguilera TA, Olson ES, Timmers MM, Jiang T, Tsien RY. Integr. Biol. 2009;1:371. doi: 10.1039/b904878b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Olson ES, Aguilera TA, Jiang T, Ellies LG, Nguyen QT, Wong EH, Gross LA, Tsien RY. Integr. Biol. 2009;1:382. doi: 10.1039/b904890a. [DOI] [PMC free article] [PubMed] [Google Scholar]