Abstract
Several conventional methods of bariatric surgery and some novel gastrointestinal surgical procedures induce long-term remission of type 2 diabetes mellitus (T2DM). In addition, these procedures dramatically improve other metabolic conditions, including hyperlipidemia and hypertension, in patients with and without obesity. Several studies have provided evidence that these metabolic effects are not simply the results of drastic weight loss and decreased caloric intake but might be attributable in part to endocrine changes that result from surgical manipulation of the gastrointestinal tract. In this Review, we provide an overview of the clinical evidence that demonstrate the effects of such interventions—termed metabolic surgery—on T2DM and discuss the implications for future research. In light of the evidence presented here, we speculate that the gastrointestinal tract might have a role in the pathophysiology of T2DM and obesity.
INTRODUCTION
Several conventional and novel methods of bariatric surgery—termed metabolic surgeries — induce long-term remission of type 2 diabetes mellitus (T2DM) and dramatically improve other metabolic abnormalities, such as hyperlipidemia and hypertension, independent of the patients’ weight.1–4 Some previous studies demonstrated that these metabolic effects are not only attributable to drastic weight loss and diminished caloric intake,1,5,6 but also to endocrine changes that result from surgical manipulation of the gastrointestinal tract. Here, we evaluate the clinical evidence that demonstrate the effects of metabolic surgery on T2DM and discuss the implications for future research.
BARIATRIC SURGERY
Surgical techniques
Bariatric surgical procedures have traditionally been divided into three categories: restrictive, malabsorbitive, or mixed surgery. This classification is made on the assumption that bariatric surgery controls only food intake and/or nutrient absorption. According to this conventional view, restrictive surgical procedures, such as laparoscopic adjustable gastric banding (LAGB) or vertical banded gastroplasty (VBG), induce early satiety during meals by decreasing the volume of the stomach (Figures 1a and 1b). Malabsorbitive procedures (Figures 1c and 1d), such as bilio–pancreatic diversion (BPD), divert bile into the terminal segment of the ileum so that bile and food are only mixed in the final 50–100 cm of the small bowel, thereby drastically reducing nutrient absorption. Mixed procedures, such as Roux-en-Y gastric bypass (RYGB), involves restriction of the stomach and bypass of the small bowel, which is, however, shortened much less than it is in BPD (Figure 1e). Other novel procedures, such as duodenal–jejunal bypass (DJB), ileal interposition and sleeve gastrectomy are becoming increasingly popular owing to their ability to cause dramatic weight loss and/or substantial improvement of glycemic regulation among both obese and nonobese patients (Figure 2). Nevertheless, RYGB, LGB and BPD remain the most widely used treatments for morbid obesity.1
Figure 1.
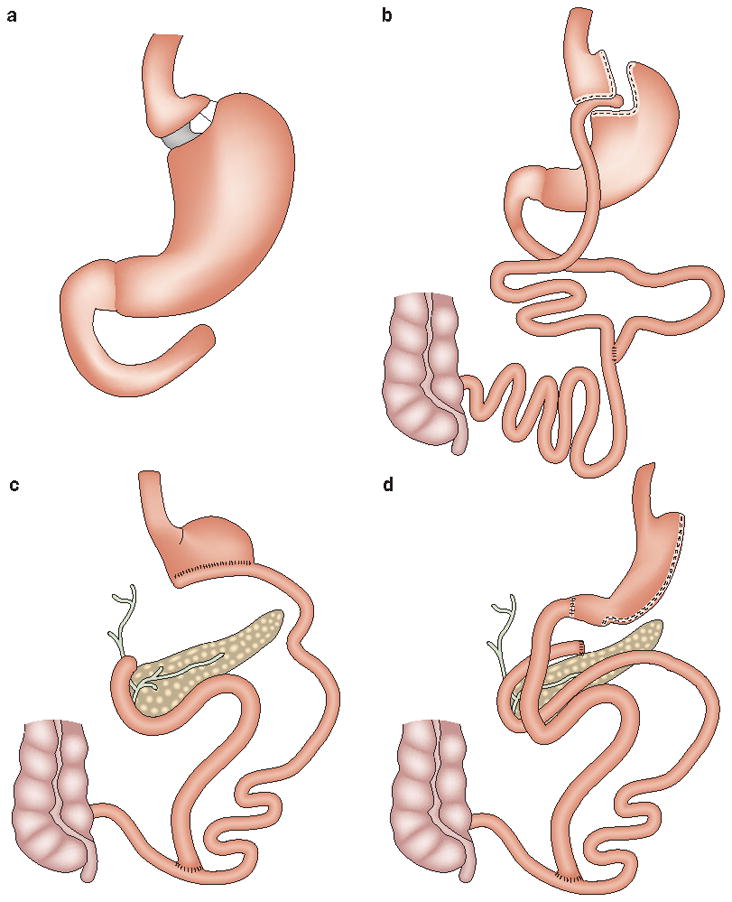
Conventional bariatric operations. a During laparoscopic adjustable gastric banding, the upper part of the stomach is encircled by a saline-filled tube. The extent of restriction can be adjusted by injecting/withdrawing saline solution to/from the tube. b During Roux-en-Y gastric bypass, a surgical stapler is used to create a small, vertical gastric pouch. The upper pouch, which is completely separated from the gastric remnant, is anastomosed to the jejunum, whereas the excluded biliary limb is anastomosed to the alimentary limb. After surgery, ingested food bypasses about 95% of the stomach, the entire duodenum and a portion of the jejunum, but bile and nutrients mix in the distal jejunum and can be absorbed through the remaining portion of the small bowel. Biliopancreatic diversion involves a horizontal resection (c) or a vertical resection (d, also known as ‘sleeve gastrectomy’ or ‘duodenal switch’). The reduced stomach is anastomosed to the distal 250 cm of the small intestine. The excluded small intestine, which carries the bile and pancreatic secretions, is connected to the alimentary limb. Bile and nutrients mix in a short segment of small bowel, the only site where fat and starches are absorbed; noncaloric nutrients are absorbed in the alimentary limb.
Figure 2.
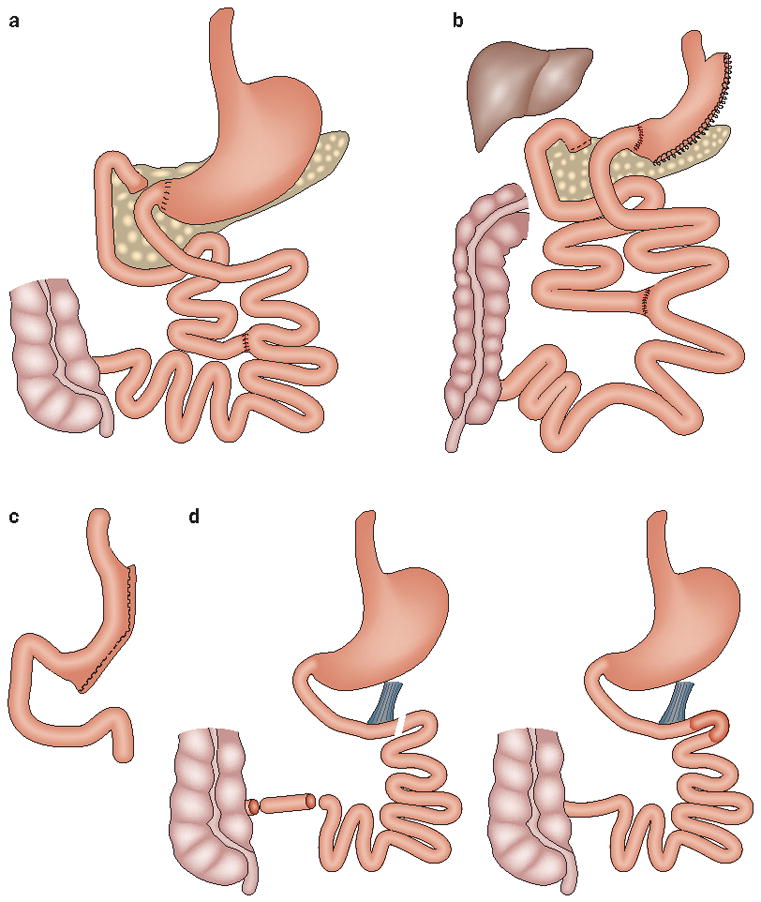
Novel methods of metabolic surgery. a Duodenal–jejunal bypass consists of a stomach-preserving bypass of a short segment of proximal small intestine (similar to that bypassed in a standard Roux-en-Y gastric bypass). Some variants of this procedure preserve the pylorus. This procedure might be associated with a sleeve resection of the stomach, which reduces the risk of marginal ulcerations and increases weight loss (b). Long-term data about the efficacy of this procedure are not yet available. c Sleeve gastrectomy not only reduces the capacity of the stomach but also eliminates the ghrelin-rich gastric fundus, which might contribute to the beneficial effects of the procedure. Sleeve gastrectomy has been also shown to improve type 2 diabetes mellitus in patients with severe obesity. The efficacy of the procedure in the long-term needs to be further investigated. d During ileal interposition, a small segment of ileum (with its intact vascular and nervous supplies) is surgically interposed into the proximal small intestine, which increases its exposure to ingested nutrients. Ileal interposition can be performed alone or in association with sleeve gastrectomy and duodenal exclusion. The procedure requires three anastomoses (gastric bypass operations include two). The long-term effects of this procedure are unknown.
Clinical outcomes of conventional procedures
Traditional methods of bariatric surgery are associated with high rates of remission of T2DM, as demonstrated by a meta-analysis of 136 studies that included a total of 22,094 patients who underwent bariatric surgery as a treatment for morbid obesity.1 Although most of the studies were retrospective and lacked long-term follow-up (duration of follow-up was 1–3 years), the results were still ]impressive: the mean ratios of patients with resolution of T2DM after LAGB, VBG, RYGB and BPD were 48%, 68%, 84%, and 98%, respectively (Table 1).
Table 1.
Effects of various types of bariatric surgery on comorbidities.
| Improvement | Rates of improvement (%) after surgery | ||
|---|---|---|---|
| LAGB | RYGB | BPD | |
| Resolution of T2DM | 48 | 84 | 98 |
| Resolution of hypertension | 43 | 68 | 83 |
| Improvement of hyperlipidemia | 59 | 97 | 99 |
| Excess weight loss | 47 | 62 | 70 |
Abbreviations: BPD, biliopancreatic diversion; LAGB, laparoscopic adjustable gastric banding; RYGB, Roux-en-Y gastric bypass; T2DM, type 2 diabetes mellitus. Permission needed from the American Medical Association © Buchwald, H. et al. (2004) JAMA 292, 1724–1737.
The multicenter, prospective, controlled Swedish Obese Subjects (SOS) study compared the effects of bariatric surgery (LAGB: n = 156; VBG: n = 451; RYGB: n = 34) with those of nonsurgical weight-loss treatment patients with obesity. Bariatric surgery resulted in a 16.1% mean weight loss at 10 years after surgery (RYGB: 25.0 kg; LAGB: 13.2 kg; VBG: 16.5 kg), compared with a small weight gain observed in the control group. Fasting glycemia tended to increase during the study in the control group (18.7% at 10 years), whereas a substantial decrease in fasting glycemia was detected in surgically treated patients at 2 years (13.6%) and 10 years (2.5% overall decrease, ranging from 0.8% for gastric banding and 10% for gastric bypass). Furthermore, at 10 years, the relative risk of incident T2DM was three times lower, and the rates of recovery from T2DM were three times greater, for patients who underwent surgery than for individuals in the control group.
Some studies evaluated the procedure-specific effects on T2DM, including a randomized, controlled trial in which 60 patients with BMI values of 30–40 kg/m2 received either standard therapy (medical and/or behavioral) or LAGB plus standard therapy.7 2 years after surgery, remission of T2DM (defined as having a fasting glucose level below 7 mmol/l and HbA1C <6.2% without the use of pharmacotherapy) was seen in 73% of patients who underwent surgery and standard therapy versus 13% of patients who received standard therapy alone. Two large case-series studies8,9 that included patients with T2DM or impaired glucose tolerance documented normalization of HbA1C levels after RYGB without antidiabetic medication in 89% and 82% of patients, respectively. A retrospective study on the effect of BPD in 243 patients with T2DM showed normalization of glycemia in 97% of patients at 10 years after surgery.10 SG has also been shown to dramatically improve symptoms of T2DM, at least in the short term, as reported in a 12-month, prospective study in which 84.6% of patients achieved complete remission of T2DM.11 However, a gradient of efficacy seems to exist among the various surgical procedures in the rates of normalization of glycemia achieved without pharmacological intervention, as demonstrated by a study of 72 patients with T2DM who underwent one of three bariatric surgeries over a 30-month period in a single institution.12 After a mean duration of follow-up of 13 months, patients who underwent LAGB experienced a mean of 17% decrease of glycemic levels, whereas those who underwent SG or RYGB experienced decreases of 33% and 69%, respectively.
Improvement of T2DM after gastrointestinal surgery has also been reported in patients with relatively mild forms of obesity and in nonobese individuals. In a randomized, controlled trial, 80 patients with a BMI of 30–35 kg/m2 were treated with either a strict medical regimen that included a very low calorie diet, lifestyle modification, and pharmacotherapy, or LAGB.4 At baseline, 38% of patients in each group had been diagnosed with the metabolic syndrome; 2 years after surgery, metabolic syndrome was prevalent in 24% of nonsurgically treated patients but in only 3% of those treated with surgery. Another research group reported remarkable reduction of fasting plasma glucose levels in a prospective series of 37 patients with BMI <35 kg/m2 who underwent laparoscopic RYGB.2
A prospective study evaluated the effects of gastric bypass surgery in 44 patients with T2DM and BMI <35 kg/m2 as compared with 157 patients with BMI >35 kg/m2.3 After 4 years of postoperative follow-up, 90% of patients with BMI <35 kg/m2 and 98% of patients with BMI >35 kg/m2 experienced normalization of glycemia. The investigators concluded that 77% of those with a BMI <35 kg/m2 achieved the targets determined by the American Diabetes Association, namely HbA1C level <7.0%, LDL-cholesterol level <2.59 mmol/l and triglyceride level <1.695 mmol/l. In this study, 2.2% of patients experienced major complications (one fatality), and 6.2% of patients experienced minor complications. A prospective pilot study that used BPD as a primary treatment for T2DM in five patients with T2DM and nonmorbid obesity (BMI 27–33 kg/m2) documented dramatic reductions of hyperglycemia and improvements in insulin sensitivity as early as 1 month after surgery.13 Remission of T2DM after BPD in patients with nonmorbid obesity was reported in two other studies.14,15
Cohen and colleagues16 reported the first two patients who underwent duodenal–jejunal bypass (DJB) for T2DM; these patients had BMIs of 29 kg/m2 and 30 kg/m2, respectively. After surgery, the patients’ HbA1C levels normalized within 3 months, and stabilized after 9 months at 5–6% (from 8–9% preoperatively). Importantly, neither patient lost weight, which suggests that surgery evoked weight-independent antidiabetic mechanisms. In another study, marked reductions were observed in fasting glycemic levels and HbA1C levels after laparoscopic DJB, and 18 out of 20 patients with BMI <30 kg/m2 discontinued antidiabetic medications.17 Another study found a decrease in antidiabetic medication requirements after DJB but only modest improvements of HbA1C levels (from 9.4 to 8.5%) and blood glucose levels (from 11.60 mmol/l to 8.55 mmol/l).18 Ileal interposition alone or in combination with SG among 60 patients with T2DM and BMI 24–34 kg/m2 resulted in adequate glycemic control in 87% of patients at a mean follow-up of 7.4 months.19,20
Endoluminal duodenal–jejunal sleeve (ELS) is a flexible plastic sleeve that excludes the proximal intestine from alimentary flow, analogous to the surgical bypass in a standard RYGB or DJB. The device can be implanted endoscopically without disrupting bowel continuity or creating surgical anastomoses and has been reported to improve glucose homeostasis in both animal and human studies.21,22
Nonglycemic metabolic effects
In addition to substantially improving hyperglycemia, bariatric surgery might ameliorate several other metabolic symptoms, including hyperlipidemia and hypertension. Results of a meta-analysis1 showed marked decreases in levels of total cholesterol, LDL-cholesterol and triglycerides after bariatric procedures. Approximately 70% of patients experienced an improvement in hyperlipidemia, whereas 79% of patients experienced improvement or resolution of hypertension.1 Surgical improvement of hyperlipidemia and hypertension has also been reported in patients with BMI <35 kg/m2.2,3,15 These findings indicate that bariatric or metabolic surgery offers health benefits other than just weight loss and glycemic control. Several clinical investigations have demonstrated that bariatric operations improve long-term survival in patients with severe obesity, both with and without T2DM, when compared with matched control individual who do not undergo surgery: bariatric surgery is associated with decreases in mortality ranging from 33% to 89%.23–28 In a large case–control study, 7,925 patients underwent RYGB whereas 7,925 matched controls did not undergo surgery of any kind. After a mean follow-up of 8.4 years, surgery reduced overall mortality by 40%, cardiovascular mortality by 56%, cancer mortality by 60% and diabetes-related mortality by 92%.29 In the Swedish Obese Subjects study, patients in the surgical group experienced a 24% nonadjusted decrease in overall mortality compared with matched controls; the most prominent decreases were observed in cancer-related and cardiovascular mortality (38.0% and 20.5%, respectively).30
Safety
The frequent misconception that bariatric surgery is associated with markedly elevated rates of complications and mortality is not supported by the available data. A meta-analysis of 361 studies that included a total of 85,048 patients showed an overall mortality of 0.28% within 30 days after surgery, and a mortality of 0.35% between 30 days and 2 years after surgery.31 Several other studies reported surgical mortality of 0.25%–0.50%.32–35 The Longitudinal Assessment of Bariatric Surgery consortium conducted a multicenter, prospective observationalstudy of 30-day outcomes in patients who underwentbariatric surgery at 10 clinical sites in the US between 2005 and 2007.36 The30-day death rate among patients who underwent RYGB or LAGB was0.3%, and in total 4.1% of patients experienced at least one major adverseevent.36 Of note, mortality rates associated with bariatric surgery are equivalent with those of several common abdominal surgeries, such as laparoscopic cholecystectomy, which has a mortality rate of 0.3–0.6% in the US.37
Another study, which analyzed the data of more than 9,500 patients who underwent bariatric surgery at 652 hospitals in the US, showed an impressive 21% decline in 6-month, risk-adjusted complication rates.38 The study also found that inpatient complication rates fell from 24% to 15%, despite inclusion of a high percentage of elderly and ailing operative patients. These data demonstrate that over the past several years, morbidity and mortality associated with bariatric surgery have steadily declined. Such improvements have been largely attributed to the widespread use of minimally invasive laparoscopic techniques, in addition to other factors,39,40 such as implementation of centers of excellence and greater experience with the procedures.
CONTROL OF T2DM BY METABOLIC SURGERY
Effects on glucose and insulin homeostasis
Several studies suggest that RYGB and BPD might improve T2DM by enhancing insulin sensitivity41 and/or by improving β-cell function. The beneficial effect of gastric bypass surgery on β-cell function is supported by two observations. One is represented by the increasing rate of reported hyperinsulinemic hypoglycemia in patients who have undergone RYGB,42 which suggests that the postoperative milieu after RYGB, at least in some cases, can overstimulate the function and possibly the growth of β cells. Further support derives from the observation that gastric bypass surgery can also restore acute β-cell response to glucose, which suggests that the defect in glucose-induced insulin secretion, which is typical of T2DM, is a reversible abnormality.43
Gastric bypass surgery also consistently improves oral glucose tolerance, both in animals and humans. A study where oral glucose tolerance tests were performed in nine obese women with T2DM before and 1 month after RYGB and in 10 matched women after a diet-induced, equivalent weight loss (10 kg) showed a dramatic improvement of oral glucose tolerance and an increase in the levels of glucagon-like peptide-1 (GLP-1) and in the overall incretin-related effect after RYGB, but not in the control group.44
Weight-independent antidiabetic effects
Increasing evidence suggests that certain types of surgical manipulations of the gastrointestinal tract ameliorate T2DM by mechanisms other than weight loss and diminished caloric intake. A direct role of surgical manipulation of the gastrointestinal tract on diabetes mellitus was suggested by an experiment in nonobese diabetic rats (Goto-Kakizaki strain) that underwent DJB surgery.45 These rats experienced substantially greater improvement of glucose homeostasis than matched control rats that had undergone sham operation, diet restriction or therapy with insulin-sensitizing drugs.45 Similar findings have been reported in other studies that used in the same animal model46–48 as well as in rodent models of diet-induced insulin resistance,49,50 and numerous cases of glycemic improvement have been reported in humans following experimental gastrointestinal procedures that cause little to no weight loss.16,17 Additional evidence of weight-independent mechanisms of T2DM control derives from observations that bypass surgical procedures induce higher rates of T2DMD remission than restrictive forms of bariatric surgery or nonsurgical interventions, despite equivalent weight loss, consistent with the study discussed above that compared the results of RYGB and dieting.44
In a randomized, controlled trial that compared SG and gastric bypass, greater rates of T2DM remission were found among patients treated with gastric bypass than among those treated with SG, despite equivalent weight loss in both groups. Similar results were found in studies that compared LAGB and RYGB.51,52 These observations suggest that manipulation of the gastrointestinal anatomy by bypass surgery directly influences metabolic pathways, which ultimately results in the improvement of glucose homeostasis and body-weight regulation. Consequently, weight loss and T2DM control might be considered two separate outcomes of gastrointestinal surgery, which means that improvement of glycemia is not necessarily secondary to weight loss.
Possible neuroendocrine mechanisms
Gastrointestinal bypass procedures connect two otherwise separated segments of the gastrointestinal tract, thereby allowing nutrients to reach the distal portion of the small intestine more rapidly than usual and bypassing the contact of nutrients with much of the stomach, the entire duodenum and part of the jejunum. Two major hypotheses exist for improvement of glycemia following gastrointestinal surgery. According to the ‘lower intestinal hypothesis’53 (also known as ‘distal’ or ‘foregut’ hypothesis54), the rapid delivery of nutrients to the lower intestine increases stimulation of L-cells, which results in increased secretion of hormones that enhance insulin release and/or insulin action (for example, GLP-1), and a subsequent decrease in blood glucose levels. According to the ‘upper intestinal hypothesis’53 (also defined as ‘proximal’ of ‘hindgut’ hypothesis54), gastrointestinal bypass reduces the secretion of upper gastrointestinal factors that decrease insulin secretion and/or promote insulin resistance. Reduction of the amount of these putative anti-insulin factors (or anti-incretins) would increase insulin action, and so improve symptoms of T2DM. Although the proximal and distal hypotheses are often conceptualized in terms of the release of hormones, they are also compatible with the theory that altered nutrient flow triggers neural signaling rather than hormone release.
The distal and proximal hypotheses are often presented as mutually exclusive. Although such presentation might be convenient for didactic purposes, no reported data precludes the possibility that the distal and proximal mechanisms both contribute to the efficacy of gastric bypass procedures. For example, the exclusion of the proximal bowel per se might cause changes in levels of distal gut hormones as proximal signals are involved in the regulation of L-cells secretory functions.55
A number of gastrointestinal hormonal changes have been reported to occur following gastric surgery, consistent with the hypotheses that alterations in gastrointestinal anatomy affect endocrine functioning of the gut. For example, RYGB induces substantial hormonal changes, even before weight loss takes places.56 Increased levels of peptide YY and GLP-144,57–60 have been consistently reported in several animal and human studies. RYGB also seems to alter secretion of ghrelin61 and GIP.56,62 These hormones are all involved in the regulation of energy homeostasis via their effects on peripheral organs, as well as the brain. Although the exact molecular mechanisms that underlie the improvements in metabolism following gastric bypass surgery are not known, these findings establish that changes in gastrointestinal anatomy have profound effects on the gastrointestinal tract’s control of metabolism. Furthermore, as a number of gastrointestinal hormones and neural signals are produced at various sites of the gastrointestinal tract, different surgical methods might activate distinct mechanisms of action.
RATIONALE FOR A PARADIGM SHIFT
The evidence provided here supports the need for a conceptual shift in the way gastrointestinal surgery should be regarded. Currently, the term ‘bariatric’ (which originates from the Greek word for ‘weight’ [baros]) reflects the perceived notion that gastrointestinal surgery is used to primarily induce weight loss. However, strong evidence shows that bariatric surgery not only induces dramatic weight loss but also improves symptoms of T2DM, hypertension and hyperlipidemia, and, as noted above, the metabolic improvements often precede substantial weight loss. On the basis of this evidence, the term ‘metabolic’ surgery seems more appropriate as it refers to the effects of gastrointestinal surgery on the metabolic syndrome as a whole, while also capturing the metabolic nature of its mechanisms of action.
Need for revision of BMI-based criteria
A patient’s BMI is used as the primary eligibility criterion for surgical treatment of severe obesity. According to the guidelines of the National Institutes of Health (NIH),63 only patients with a BMI >40 kg/m2 or with a BMI >35 kg/m2 accompanied by comorbidities, such as T2DM, are eligible for gastrointestinal surgery. Although this approach is convenient, BMI does not accurately predict the diabetes-related risk of morbidity and mortality. Moreover, no evidence suggests that specific BMI cut-off values can serve as predictors of successful metabolic control after gastrointestinal surgery. As described above, several studies have successfully demonstrated that gastrointestinal surgery can be a life-saving procedure for individuals with severe obesity. Such surgery also seems to dramatically improve hyperlipidemia, hypertension and hyperglycemia in nonobese individuals, thereby providing a plausible therapeutic alternative to reducing cardiovascular risk in selected patients. Therefore, we consider it inappropriate that BMI continues to be used by clinicians and insurance companies as the sole criterion to determine patients’ eligibility for surgical treatment of T2DM and the metabolic syndrome.
Intestinal factors that contribute to T2DM
The gastrointestinal tract is not commonly considered in discussions of the etiology of insulin resistance and T2DM. Attention is usually focused on the liver, muscle, adipose tissue and the pancreatic β cells, which are the major peripheral organs and tissues involved in the control of whole-body energy homeostasis. In the following discussion, we provide a number of reasons why the gastrointestinal tract should be included in these considerations.
The gastrointestinal tract is the first organ to receive information about the nutrient load of a meal and, as an endocrine organ, it transmits this information via hormonal secretion and direct neural signaling to peripheral tissues, as well as the brain, thereby modulating the control of metabolism. As a consequence, the gastrointestinal tract has a major role in the integration of nutrients with metabolic responses and changes in its anatomy can, predictably, have profound effects in the control of metabolism. In fact, the effects of surgical manipulation of the intestine on T2DM, independent of weight-loss, are consistent with the hypothesis that the gastrointestinal tract has a physiological role in glucose homeostasis and might also have a role in abnormalities of glucose homeostasis, such as insulin resistance and T2DM. Dysfunction of the gastrointestinal tract could provide a potential explanation for the link between excess nutrition and the development of insulin resistance and T2DM. The passage of excess nutrients in general or an increase in the passage of specific nutrients through the gastrointestinal tract could trigger intestinal neuroendocrine dysfunction, possibly owing to an overstimulation (see the discussion below on anti-incretin theory). Consistent with the role of excessive nutrient stimulation, all forms of restriction of nutrient passage throughout the intestine invariably result in improvement of T2DM, and the data suggest a positive correlation between the decrease of nutrient stimulation (‘intestinal rest’) and the degree of improvement of T2DM (that is, diet, restrictive surgery and gastric bypass surgery are associated with relatively small, medium and relatively great improvement, respectively) (Figure 3).
Figure 3.
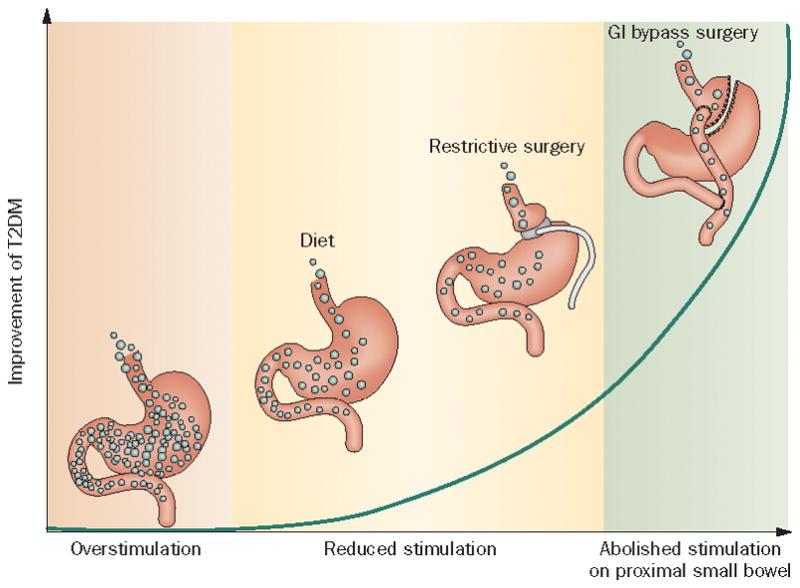
Intestinal factors that contribute to the pathophysiology of T2DM. A dysfunctional intestinal signal is posited to be involved in the pathophysiology of T2DM. According to this hypothesis, overstimulation of the gastrointestinal tract (by overeating and/or the presence of chemical or biological stimuli in modern diets) could lead to insulin resistance, obesity and T2DM, whereas all forms of restriction of nutrients’ transit could improve these conditions. Indeed, diet might improve T2DM not just because of a restriction of caloric intake, but owing to the reduced stimulation of abnormal intestinal mechanisms. Likewise, restrictive surgery could improve T2DM by reducing the nutrient load even further. Bypass operations, which completely and indefinitely inactivate a large part of the intestine, reduce nutrient-related stimuli more than any other approach and are the most effective ways of improving T2DM, obesity and insulin resistance syndrome. Abbreviation: T2DM, type 2 diabetes mellitus.
The epidemic growth of the incidence of T2DM suggests that environmental or infectious agents contribute to the development of this disease. Although considering the rising incidences of obesity and T2DM from the perspective of an infectious epidemic is highly speculative, this approach is supported by some studies.64 We would like to point out that the gastrointestinal tract is the organ that is first exposed to food-borne toxins or infectious agents, and as it is involved in the control of metabolism, such insults could have profound metabolic effects. Notably, the microbiota of the gut can affect the control of energy metabolism, and, therefore, changes in the microbiota might contribute to the epidemic of obesity and T2DM.65 Future studies are required to unravel the potential role and contributions of infectious agents, environmental toxins and changes in the gut microbiota on the rise of these abnormalites.
The anti-incretin hypothesis
As discussed above, a variety of arguments suggest that the gastrointestinal tract is involved in the development of T2DM and is a potential target for the treatment of this disease. Nevertheless, we do not understand the role of the gastrointestinal tract at a mechanistic level. Although a number of possible mechanisms are known, here we discuss only the ‘anti-incretin’ hypothesis, which could explain both the effects of gastrointestinal surgery on T2DM and the role of the gastrointestinal tract in the physiology and pathophysiology of glucose homeostasis. Incretins include gut hormones, such as GLP-1 and gastrointestinal peptide, whose secretion is triggered by the passage of nutrients through the small bowel. These hormones increase glucose-stimulated insulin secretion by pancreatic β cells and also affect gastric emptying, nitrite influx and β-cell prolifereation (via anti-apoptotic effects).66 The ‘anti-incretin’ theory posits the existence of nutritionally-stimulated, gastrointestinal, neuroendocrine signals that antagonize the effects of incretins.67 A normal, physiologic balance between incretins and ‘anti-incretins’ would ensure normal excursions of blood glucose and proper β-cell function. The anti-incretin theory suggests that an increase or untimely production of the anti-incretin signal could disrupt the incretin–anti-incretin homeostatic mechanism and ultimately affect the functions of a number of organs that are involved in the regulation of metabolism (such as β cells, adipose tissue and the brain). This theory predicts that in patients with T2DM, gastrointestinal bypass surgery might prevent the release of excess of anti-incretins, which restores the proper incretin–anti-incretin balance, and eventually results in the improvement of T2DM. A corollary of this hypothesis is that in some patients gastrointestinal bypass surgery results in an underproduction of ‘anti-incretins’, which might cause a shift toward an exaggerated incretin effect, thereby increasing the risk of postprandial hyperinsulinemia and hypoglycemia. We must emphasize, however, that this hypothesis has not been confirmed and putative anti-incretins produced by the gastrointestinal tract have not been identified to date.
An alternative hypothesis regarding the effect of bariatric surgery on insulin sensitivity is that exclusion of portions of the gut reduces the flux of nutrients, and this reduced flux is directly responsible for the beneficial effects associated with surgery. Severe caloric restriction acutely improves insulin resistance, although the underlying mechanism for this effect is not known. This effect could be directly related to the change in the flux of nutrients (that is, independent of any effects on the secretion of known and hypothesized gut hormones). Alternatively, the change in nutrient flux could affect the balance of gut hormones (including hypothetical anti-incretins) and the change in hormone milieu might be responsible for changes in insulin sensitivity. Regardless of the explanation for the effects of altering nutrient flux through the gut, a better understanding of the role of the gut in the control of insulin sensitivity will certainly support the future development of treatments for insulin resistance and T2DM.
CONCLUSIONS
Considering the escalating pandemic of T2DM, clinicians must recognize the need for improved therapeutic options. When behavioral and pharmacological interventions fail to manage T2DM, metabolic surgery offers an effective alternative, with the potential of complete remission of the disease. As the data presented in this article indicate, traditional bariatric or metabolic surgeries are highly safe and effective in patients with severe obesity and T2DM. Furthermore, gastrointestinal bypass techniques improve glucose homeostasis through mechanisms beyond reduced caloric intake and weight loss. Continued research to better understand the weight-independent antidiabetic mechanisms of gastrointestinal surgery and the role of the gastrointestinal tract in the physiology and pathophysiology of glucose homeostasis might lead to important discoveries that can ultimately help identify targets for novel drug development, as well as facilitate the design of interventions that are less invasive than current methods for the treatment of obesity and T2DM.
Key points.
Conventional and novel bariatric surgeries induce long-term remission of type 2 diabetes mellitus (T2DM) and dramatically improve other metabolic conditions, including hyperlipidemia and hypertension
Animal studies and clinical investigations show that the effects of surgery on T2DM might be partly explained by endocrine changes that result from surgical manipulation of the gastrointestinal tract
Current BMI-based criteria for patient selection are not sufficiently inclusive to define indications for surgical treatment and evaluation of the risk profile of patients with T2DM
Randomized, controlled trials that compare surgery with medical treatment should aim to define the role of surgery in the management of T2DM and identify new criteria for selection
Research into the mechanisms of action of metabolic surgery represents an extraordinary opportunity to improve our understanding of the pathophysiology of T2DM and ultimately improve its treatment
Acknowledgments
This work was supported in part by NIH Grants DK52852 (TEM) and DK069982 (TEM).
References
- 1.Buchwald H, et al. Bariatric Surgery: A Systematic review and meta-analysis. JAMA. 2004;292:1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 2.Cohen R, Pinheiro JS, Correa JL, Schiavon CA. Laparoscopic Roux-en-Y gastric bypass for BMI < 35 kg/m(2): a tailored approach. Surg Obes Relat Dis. 2006;2:401–4. doi: 10.1016/j.soard.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Lee WJ, et al. Effect of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI>35 and <35 kg/m2. J Gastrointest Surg. 2008;12:945–52. doi: 10.1007/s11605-007-0319-4. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien PE, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006;144:625–33. doi: 10.7326/0003-4819-144-9-200605020-00005. [DOI] [PubMed] [Google Scholar]
- 5.Suter M, Calmes JM, Romy A, Giusti V. Results of Roux-en-Y gastric bypass in morbidly obese vs. super obese patients: similar body weight loss, correction of comorbidities, and improvement of quality of life. Arch Surg. 2009;144:312–18. doi: 10.1001/archsurg.2009.19. [DOI] [PubMed] [Google Scholar]
- 6.Thaler JP, Cummings DE. Hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009;150:2518–25. doi: 10.1210/en.2009-0367. [DOI] [PubMed] [Google Scholar]
- 7.Dixon JB, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299:316–23. doi: 10.1001/jama.299.3.316. [DOI] [PubMed] [Google Scholar]
- 8.Pories WJ, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–50. doi: 10.1097/00000658-199509000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schauer PR, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238:467–84. doi: 10.1097/01.sla.0000089851.41115.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scopinaro N. Biliopancreatic diversion: mechanisms of action and long-term results. Obes Surg. 2006;16:683–9. doi: 10.1381/096089206777346637. [DOI] [PubMed] [Google Scholar]
- 11.Vidal J, Ibarzabal A, Romero F, et al. Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects. Obes Surg. 2008;18:1077–82. doi: 10.1007/s11695-008-9547-2. [DOI] [PubMed] [Google Scholar]
- 12.Gan SS, Talbot ML, Jorgensen JO. Efficacy of surgery in the management of obesity-related type 2 diabetes mellitus. ANZ J Surg. 2007;77:958–62. doi: 10.1111/j.1445-2197.2007.04290.x. [DOI] [PubMed] [Google Scholar]
- 13.Chiellini C, Rubino F, Castagneto M, Nanni G, Mingrone G. The effect of bilio-pancreatic diversion on type 2 diabetes in patients with BMI <35 kg/m2. Diabetologia. 2009;52:1027–30. doi: 10.1007/s00125-009-1333-8. [DOI] [PubMed] [Google Scholar]
- 14.Noya G, et al. Biliopancreatic diversion preserving the stomach and pylorus in the treatment of hypercholesterolemia and diabetes type II: results in the first 10 cases. Obes Surg. 1998;8:67–72. doi: 10.1381/096089298765555088. [DOI] [PubMed] [Google Scholar]
- 15.Scopinaro N, Marinari GM, Camerini GB, Papadia FS, Adami GF. Specific effects of biliopancreatic diversion on the major components of metabolic syndrome: a long-term follow-up study. Diabetes Care. 2005;28:2406–11. doi: 10.2337/diacare.28.10.2406. [DOI] [PubMed] [Google Scholar]
- 16.Cohen R, Schiavon C, Pinheiro J, Correa J, Rubino F. Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22–34 kg/m2. Surg Obes Relat Dis. 2007;3:195–7. doi: 10.1016/j.soard.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Ramos AC, et al. Laparoscopic duodenal-jejunal exclusion in the treatment of type 2 diabetes mellitus in patients with BMI < 30 kg/m2 (LBMI) Obes Surg. 2009;19:307–312. doi: 10.1007/s11695-008-9759-5. [DOI] [PubMed] [Google Scholar]
- 18.Ferzli GS, Dominique E, Ciaglia M, Bluth MH, Gonzalez A, Fingerhut A. Clinical improvement after duodenojejunal bypass for non obese type 2 diabetes despite minimal improvement in glycemic homeostasis. World J Surg. 2009;33:972–9. doi: 10.1007/s00268-009-9968-7. [DOI] [PubMed] [Google Scholar]
- 19.DePaula AL, et al. Laparoscopic treatment of type 2 diabetes mellitus for patients with a body mass index less than 35. Surg Endosc. 2008;22:706–16. doi: 10.1007/s00464-007-9472-9. [DOI] [PubMed] [Google Scholar]
- 20.DePaula AL, Macedo AL, Mota BR, Schraibman V. Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg Endosc. 2009;23:1313–20. doi: 10.1007/s00464-008-0156-x. [DOI] [PubMed] [Google Scholar]
- 21.Aguirre V, et al. An endoluminal sleeve induces substantial weight loss an d normalizes glucose homeostasis in rats with diet-induced obesity. Obesity. 2008;16:2585–92. doi: 10.1038/oby.2008.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodriguez-Grunert L, et al. First human experience with endoscopically delivered and retrive duodenal-jejunal bypass sleeve. Surg Obes Relat Dis. 2008;4:55–9. doi: 10.1016/j.soard.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 23.MacDonald KG, et al. The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg. 1997;1:213–20. doi: 10.1016/s1091-255x(97)80112-6. [DOI] [PubMed] [Google Scholar]
- 24.Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg. 2004;199:543–51. doi: 10.1016/j.jamcollsurg.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Christou NV, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23. doi: 10.1097/01.sla.0000137343.63376.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sowemimo OA, et al. Natural history of morbid obesity without surgical intervention. Surg Obes Relat Dis. 2007;3:73–7. doi: 10.1016/j.soard.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 27.Peeters A, et al. Substantial intentional weight loss and mortality in the severely obese. Ann Surg. 2007;246:1028–33. doi: 10.1097/SLA.0b013e31814a6929. [DOI] [PubMed] [Google Scholar]
- 28.Perry CD, Hutter MM, Smith DB, Newhouse JP, McNeil BJ. Survival and changes in comorbidities after bariatric surgery. Ann Surg. 2008;247:21–7. doi: 10.1097/SLA.0b013e318142cb4b. [DOI] [PubMed] [Google Scholar]
- 29.Adams TD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61. doi: 10.1056/NEJMoa066603. [DOI] [PubMed] [Google Scholar]
- 30.Sjostrom L, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 31.Buchwald H, Estok R, Fahrbach K, Bane D, Sledge I. Trends in Mortality in Bariatric Surgery: A systematic review and meta-analysis. Surgery. 2007;142:621–32. doi: 10.1016/j.surg.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 32.Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y- 500 patients: technique and results, with 3–60 month follow-up. Obes Surg. 2000;10:233–9. doi: 10.1381/096089200321643511. [DOI] [PubMed] [Google Scholar]
- 33.Morinigo R, et al. GLP-1 and changes in glucose tolerance following gastric bypass surgery in morbidly obese subjects. Obes Surg. 2006;16:1594–601. doi: 10.1381/096089206779319338. [DOI] [PubMed] [Google Scholar]
- 34.Wickremesekera K, Miller G, Naotunne TD, Knowles G, Stubbs RS. Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes Surg. 2005;15:474–81. doi: 10.1381/0960892053723402. [DOI] [PubMed] [Google Scholar]
- 35.Pontiroli AE, et al. Laparoscopic gastric banding prevents type 2 diabetes and arterial hypertension and induces their remission in morbid obesity: a 4-year case-controlled study. Diabetes Care. 2005;28:2703–9. doi: 10.2337/diacare.28.11.2703. [DOI] [PubMed] [Google Scholar]
- 36.LABS Consortium. Perioperative Safety in the Longitudinal Assessment of Bariatric Surgery. NEJM. 2009;361:520–1. [Google Scholar]
- 37.Khuri SF, et al. Comparison of surgical outcomes between teaching and non-teaching hospitals in the Department of Veterans Affairs. Ann Surg. 2001;234:370–82. doi: 10.1097/00000658-200109000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Encinosa WE, Bernard DM, Du D, Steiner CA. Recent Improvements in Bariatric Surgery Outcomes. Medical Care. 2009;47(5):531–5. doi: 10.1097/MLR.0b013e31819434c6. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen NT, Hinojosa M, Fayad C, Varela E, Wilson SE. Use and outcomes of laparoscopic versus open gastric bypass at academic and medical centers. J Am Coll Surg. 2007;205:248–55. doi: 10.1016/j.jamcollsurg.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 40.Han SH, et al. Improved outcomes using a systematic and evidence based approach to the laparoscopic Roux-en-Y gastric bypass in a single academic institution. Am Surg. 2007;73:955–8. [PubMed] [Google Scholar]
- 41.Mari A, et al. Restoration of normal glucose tolerance in severely obese patients after bilio-pancreatic diversion: role of insulin sensitivity and beta cell function. Diabetologia. 2006;49:2136–43. doi: 10.1007/s00125-006-0337-x. [DOI] [PubMed] [Google Scholar]
- 42.Patti ME, et al. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia. 2005;48:2236–40. doi: 10.1007/s00125-005-1933-x. [DOI] [PubMed] [Google Scholar]
- 43.Polyzogopoulou EV, Kalfarentzos F, Vagenakis AG, Alexandrides TK. Restoration of euglycemia and normal acute insulin response to glucose in obese subjects with type 2 diabetes following bariatric surgery. Diabetes. 2003;52:1098–103. doi: 10.2337/diabetes.52.5.1098. [DOI] [PubMed] [Google Scholar]
- 44.LaFerrere B, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008;93:2479–85. doi: 10.1210/jc.2007-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239:1–11. doi: 10.1097/01.sla.0000102989.54824.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kindel TL, Yoder SM, Seeley RJ, D’Alessio DA, Tso P. Duodenal-Jejunal Exclusion Improves Glucose Tolerance in the Diabetic, Goto-Kakizaki Rat by a GLP-1 Receptor-Mediated Mechanism. J Gastrointest Surg. 2009 May 12; doi: 10.1007/s11605-009-0912-9. [DOI] [PubMed] [Google Scholar]
- 47.Pacheco D, et al. The effects of duodenal-jejunal exclusion on hormonal regulation of glucose metabolism in Goto-Kakizaki rats. Am J Surg. 2007;194(2):221– 4. doi: 10.1016/j.amjsurg.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 48.Wang TT, et al. Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann Surg. 2008;247(6):968–75. doi: 10.1097/SLA.0b013e318172504d. [DOI] [PubMed] [Google Scholar]
- 49.Troy S, et al. Intestinal gluconeogenesis is a key factor for early metabolic changes after gastric bypass but not after gastric lap-band in mice. Cell Metab. 2008;8(3):201–11. doi: 10.1016/j.cmet.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 50.Strader AD, Clausen TR, Goodin SZ, Wendt D. Ileal interposition improves glucose tolerance in low dose streptozotocin-treated diabetic and euglycemic rats. Obes Surg. 2009;19(1):96–104. doi: 10.1007/s11695-008-9754-x. [DOI] [PubMed] [Google Scholar]
- 51.Pattou F, et al. Restoration of beta cell function after bariatric surgery in type 2 diabetes patients: A prospective controlled study comparing gastric banding and gastric bypass. Obes Surg. 2007;17:1041–3. [Google Scholar]
- 52.Pattou F, et al. Catering of insulin secretion after a gastric bypass in type 2 diabetes is independent from weight loss and correlated to the increase of GLP. Diabetes Metab. 2008;34:A23. [Google Scholar]
- 53.Cummings DE, Overduin J, Foster-Schubert KE, Carlson MJ. Role of the bypassed proximal intestine in the anti-diabetic effects of bariatric surgery. Surg Obes Relat Dis. 2007:109–15. doi: 10.1016/j.soard.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moo TA, Rubino F. Gastrointestinal surgery as treatment for type 2 diabetes. Current Opinion in Endocrinology Diabetes & Obesity. 2008;15:153–158. doi: 10.1097/MED.0b013e3282f88a0a. [DOI] [PubMed] [Google Scholar]
- 55.Damholt AB, Buchan AM, Kofod H. Glucagon-like-peptide-1 secretion from canine L-cells is increased by glucose-dependent-insulinotropic peptide but unaffected by glucose. Endocrinology. 1998;139:2085–91. doi: 10.1210/endo.139.4.5921. [DOI] [PubMed] [Google Scholar]
- 56.Rubino F, et al. The early effect of the Roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004;2:236–42. doi: 10.1097/01.sla.0000133117.12646.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Le Roux CW, Aylwin SJ, Batterham RL, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243:108–114. doi: 10.1097/01.sla.0000183349.16877.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Le Roux CW, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–785. doi: 10.1097/SLA.0b013e3180caa3e3. [DOI] [PubMed] [Google Scholar]
- 59.Korner J, et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity. 2006;14:1553–1561. doi: 10.1038/oby.2006.179. [DOI] [PubMed] [Google Scholar]
- 60.Korner J, et al. Effects of Roux-en-Y-gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90:359–365. doi: 10.1210/jc.2004-1076. [DOI] [PubMed] [Google Scholar]
- 61.Cummings DE, et al. Plasma ghrelin levels after diet induced weight loss or gastric bypass surgery. NEJM. 2002;346:1623–1630. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 62.Laferrère B, et al. Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care. 2007;30(7):1709–16. doi: 10.2337/dc06-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.NIH Conference–Consensus Development Conference Panel. Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;115:956–961. [PubMed] [Google Scholar]
- 64.Pasarica M, Dhurandhar NV. Infectobesity: obesity of infectious origin. Advances in food and nutrition research. 2007;52:61–102. doi: 10.1016/S1043-4526(06)52002-9. [DOI] [PubMed] [Google Scholar]
- 65.Burcelin R, Luche E, Serino M, Amar J. The gut microbiotica ecology: a new opportunity for the treatment of metabolic diseases? Front Biosci. 2009;14:5107–5117. doi: 10.2741/3589. [DOI] [PubMed] [Google Scholar]
- 66.Lovshin JA, Drucker DJ. Incretin based therapies for type 2 diabetes mellitus. Nat Rev Endocrinol. 2009;5:262–269. doi: 10.1038/nrendo.2009.48. [DOI] [PubMed] [Google Scholar]
- 67.Rubino F. Is type 2 diabetes an operable intestinal disease? Diabetes Care. 2008;3(Supplement 2):S290–296. doi: 10.2337/dc08-s271. [DOI] [PubMed] [Google Scholar]


