Abstract
The purpose of this study was to determine the characteristics of primary diffuse large B-cell lymphoma (DLBCL) of the lacrimal sac. A 77-year-old man had epiphora of the right eye for three years. After visiting five clinics and hospitals, he was referred to our hospital, and the preoperative magnetic resonance imaging findings suggested a lacrimal sac mass. Dacryocysteography showed an obstruction of the right nasolacrimal duct, so we performed dacryocystectomy. After a histopathologic examination of the specimen, the patient was diagnosed with a DLBCL. Positron emission tomography scanning excluded metastases, and the final diagnosis was made of a primary DLBCL of the right lacrimal sac. He underwent radiotherapy with 30.6 Gray in total to the right lacrimal sac. After radiotherapy, no recurrence has been observed anywhere in his body for one year. Although a malignant lymphoma of the lacrimal sac is rare, clinicians should consider a primary malignant lymphoma in the differential diagnosis in patients with chronic dacryocystitis.
Keywords: lacrimal sac, diffuse large B-cell lymphoma, radiotherapy, dacryocystectomy, Japanese
Introduction
Primary malignant lymphoma of the lacrimal sac is rare but potentially life-threatening. In Europe, extranodal marginal zone B-cell lymphomas of the mucosa-associated lymphoid tissue (MALT lymphoma) and diffuse large B-cell lymphoma (DLBCL) are major malignant lymphomas of the lacrimal sac.1 However, it is not clear what the characteristics of a major malignant lymphoma of the lacrimal sac are in Japan because there are only a small number of cases reported.2–8
We have examined a patient with primary DLBCL of the lacrimal sac and reviewed Japanese patients with primary malignant lymphoma of the lacrimal sac to compare the characteristics of Japanese patients with those of Caucasian patients.
Case report
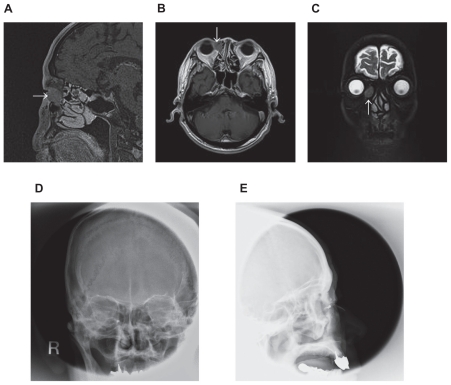
A 77-year-old man had epiphora of the right eye of three years’ duration and had visited three private clinics. His symptoms did not improve with the prescribed medical treatments, and he had noted a painless stiffness in the right lacrimal area six months earlier. After a visit to a fourth private clinic, he was referred to the Sannoh Medical Center for a magnetic resonance imaging (MRI) examination. The MRI findings (Figure 1A–C) suggested a lacrimal sac mass, and he was referred to Chiba University Hospital.
Figure 1.
Preoperative MRI and dacryocysteographic findings in a 77-year-old patient. Both magnetic resonance imaging examinations of T1 images (A, B) and T2 image (C) show a low or isointensity mass in the right lacrimal sac without invasion of surrounding tissues, which is consistent with histopathologic examination; the adjacent epithelium was not invaded by lymphoma cells. Dacryocysteography shows an obstruction of the right nasolacrimal duct (D, E).
At the first examination, his visual acuities were 0.9 OD and 1.0 OS. The intraocular pressures were within the normal range, and the fundi of both eyes were normal. The right lacrimal duct was blocked. The painless stiffness in the right lacrimal sac area was palpable, but the stiffness had not increased for six months. We performed dacryocysteography, and an obstruction of the right nasolacrimal duct was confirmed (Figure 1D–E).
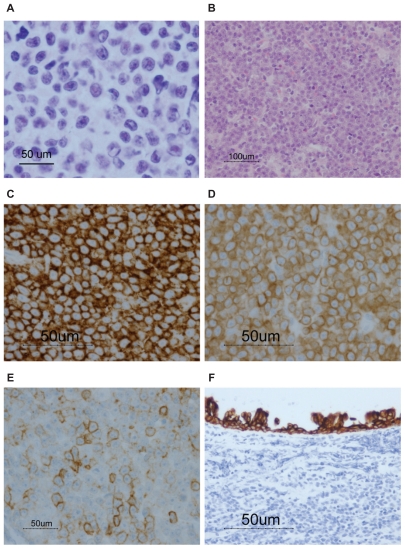
We planned to perform dacryocystorhinostomy with a rapid pathologic examination during the operation. This examination showed evidence of a malignant lymphoma (Figure 2A). Thus, we changed the surgical method from dacryocystorhinostomy to dacryocystectomy. Hisopathologic examination of the resected specimen revealed diffuse proliferation of atypical lymphocytes with prominent nucleoli. There was no lymphoepithelial lesion. Immunohistochemically, the atypical lymphocytes were positive for CD20 (L26), CD79a, and CD10, and negative for CD3, CD45RO (UCHL-1), CD5, and cyclin D1 (Figure 2B–F). A final diagnosis of DLBCL was made from these findings. Postoperative positron emission tomography scanning excluded metastases throughout the body. Thus, the final diagnosis of his mass was a primary DLBCL of the right lacrimal sac.
Figure 2.
Representative histopathologic findings of frozen section (A) and histopathologic findings in the surgical specimen of the right lacrimal sac tumor (B–F). Diffuse proliferation of atypical lymphoid cells can be seen. Atypical nuclei with prominent nuclei are present, which suggest a malignant tumor including malignant lymphoma A. Hematoxylin and eosin staining showed large lymphoid cells with high-density nuclei (B). Immunostaining with L26 C and CD79a (D) are strongly positive, and CD10 (E) is weakly positive on the membrane of lymphoid cells. The adjacent epithelium was not invaded by lymphoma cells (cytokeratin, CAM5.2, (F)).
He underwent radiotherapy with 30.6 Gray in total to the right lacrimal sac. After the radiotherapy, no recurrence has been observed anywhere in his body for one year.
Discussion
The first report of a primary malignant lymphoma of the lacrimal sac in Japan was a case of non-Hodgkin’s B-cell lymphoma in 1997.2 The patient had had epiphora for one year followed by a painless swelling of the lacrimal area for three months. Although a precise classification was not reported, it may have been a DLBCL.2 In the second case of B-cell lymphoma, the patient had epiphora and discharge, and was treated for chronic dacryocystitis for 9–10 months.6 The correct diagnosis may have also been DLBCL.6 Our case is the third documented case of primary DLBCL of the lacrimal sac in Japan, and our patient had also been treated as chronic dacryocystitis for three years.
Merkonidis et al reported that of 1294 biopsies of the lacrimal sac walls obtained during dacryocystorhinostomy in seven studies, only one (0.08%) specimen was found to be a malignant lymphoma.9 Earlier studies reported that of 15 primary lacrimal sac lymphomas, 33% were DLBCL and MALT lymphomas, and 13.3% were transitional MALT lymphomas. 1 Therefore, MALT lymphoma was to be considered in the differential diagnosis of the mass in our patient. We ruled out MALT lymphoma by the histologic features and immunohistologic results, including absence of lymphoepithelial lesion that is common in MALT lymphoma and weak expression of CD10 that is incompatible with MALT lymphoma.
Clinical data for Japanese patients with primary lacrimal sac lymphoma are presented in Tables 1 and 2. It is not clear what the pathognomic signs of major malignant lymphoma of the lacrimal sac in Japan are because there are only seven reported cases. A recent study reported five (5.2%) malignant lymphomas of the lacrimal sac of all primary lacrimal sac tumors in Chinese patients.10 All of the malignant lymphomas of the lacrimal sac in the Chinese patients were diagnosed as MALT lymphoma.10 In addition, only one case of malignant lymphoma of the lacrimal sac has been reported in Malaysia.11 The final diagnosis of malignant lymphoma in Malaysia was a small non-cleaved B-cell nonHodgkin’s lymphoma.11 Thus, the incidence of malignant lymphoma of the lacrimal sac appears to be lower in the Asian population than in Caucasians. Although MALT lymphomas have lower malignancy rates than any other types of malignant lymphoma, MALT lymphomas are rare in Japanese patients compared with Caucasian patients or Chinese patients.1–10
Table 1.
Characteristics of Japanese patients with malignant lymphoma of the lacrimal sac. There are a small numbers of cases reported in Japan. We identified seven patients with primary lacrimal sac lymphoma, of which two cases were DLBCL,2,6 two were diffuse medium cell type lymphoma with B-cell markers,3,5 one was a MALT lymphoma,7 and one was a primary T-cell malignant lymphoma.8 The first case of a natural killer cell lymphoma of the lacrimal sac was reported by Mori et al.4 Compared with Caucasian patients, primary malignant lymphomas of the lacrimal sac are rare and MALT lymphomas are infrequent in Japanese patients
| Japanese | Caucasians |
|---|---|
| DLBCL 2 | DLBCL 33% |
| MALT 1 | MALT 33% |
| Peripheral T-cell lymphoma 1 | Transitional MALT lymphoma 13.3% |
| NK lymphoma 1 | |
| Medium cell type lymphoma with B-cell markers 2 |
Abbreviations: DLBCL, diffuse large B-cell lymphoma; MALT, mucosa-associated lymphoid tissue; NK, natural killer.
Table 2.
Clinical data for Japanese patients with primary lacrimal sac lymphoma
| Case | Age | Gender | Symptoms | Histology | T/B | Stage | Treatment/dose | Follow-up/duration | Authors |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 70 | F | Epiphora; swelling | DLBCL | B | IE | RT/50Gy CHOP/1 cycle | CR/26 m | Nakamura et al2 |
| 2 | 40 | F | Epiphora; discharge | DLBCL | B | IE | NA | NA | Akizawa et al6 |
| 4 | 55 | M | Swelling | DM | B | IE | RT/40Gy CHOP/NA | CR/21 m | Hino et al3 |
| 5 | 78 | M | Epiphora | DM | T | IE | RT/40Gy CHOP/NA | CR/36 m | Morimoto et al5 |
| 6 | 55 | F | NA | MALT | B | NA | NA | CR/98 m | Takada et al7 |
| 7 | 55 | F | Swelling | NA | NK | IIE | CHOP/6 cycles RT/40Gy | DOD/9 m | Mori et al4 |
| 8 | 77 | M | Epiphora; discharge; swelling | DLBCL | B | IE | RT/30.6Gy | CR/12 m | Current report |
Abbreviations: CHOP, cyclophosphamide, doxorubicin, vincristine, and prednisone; CR, complete remission; DLBCL, diffuse large B-cell lymphoma; DM, diffuse medium; DOD, dead of disease; F, female; Gy, Gray; m, months; M, male; MALT, mucosa-associated lymphoid tissue; NA, not available; NK, natural killer; T/B, T-cell/B-cell; RT, radiotherapy.
Although our case had a chronic course, the prognosis appeared to be good. One reason for this may be that, during the chronic course, MALT lymphomas may be transformed to DLBCL, because some DLBCL in the ocular adnexa may arise from MALT lymphomas.1,7 In general, MALT lymphomas tend to remain in the primary tissue.
In summary, we report a case of primary DLBCL of the lacrimal sac. MALT lymphomas are rare in Japanese patients compared with Caucasian patients or Chinese patients. Clinicians should consider primary malignant lymphoma in the differential diagnosis of patients with chronic dacryocystitis.
Acknowledgment
This study was supported by the Grant-in-Aid for Scientific Research from Ministry of Education, Science, Sports and Culture in Japan.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sjo LD, Ralfkiaer E, Juhl BR, et al. Primary lymphoma of the lacrimal sac: An EORTC Ophthalmic Oncology Task Force study. Br J Ophthalmol. 2006;90:1004–1009. doi: 10.1136/bjo.2006.090589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura K, Uehara S, Omagari J, et al. Primary non-Hodgkin’s lymphoma of the lacrimal sac: A case report and a review of the literature. Cancer. 1997;80:2151–2155. doi: 10.1002/(sici)1097-0142(19971201)80:11<2151::aid-cncr15>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 3.Hino Y, Hatsuda T, Okuzawa M, et al. A case of malignant lymphoma of the lacrimal sac. Kyoto Second Red Cross Hospital Igaku Zasshi. 2001;22:124–128. Japanese. [Google Scholar]
- 4.Mori T, Tokuhira M, Mori S, et al. Primary natural killer cell lymphoma of the lacrimal sac. Ann Hematol. 2001;80:607–610. doi: 10.1007/s002770100368. [DOI] [PubMed] [Google Scholar]
- 5.Morimoto A, Shigemitsu T, Kuno T, et al. A case of primary malignant lymphoma diagnosed by immunohistochemical and molecular biological analysis. Journal of the Eye. 2001;18:547–550. Japanese. [Google Scholar]
- 6.Akizawa Y, Yasuzumi K, Shimada N, et al. A case of primary B cell lymphoma originating from the lacrimal sac. Jpn J Clin Ophthalmol. 2002;56:1702–1706. Japanese. [Google Scholar]
- 7.Takada S, Yoshino T, Taniwaki M, et al. Involvement of the chromosomal translocation t(11;18) in som mucosa-associated lymphoid tissue lymphomas and diffuse large B-cell lymphomas of the ocular adnexa: Evidence from multiplex reverse transcriptase-polymerase chain reaction and fluorescence in situ hybridization on using formalin-fixed, paraffin-embedded specimens. Mod Pathol. 2003;16:445–446. doi: 10.1097/01.MP.0000067421.92575.6E. [DOI] [PubMed] [Google Scholar]
- 8.Tamura M, Tsuji H, Kamata S, et al. Swelling of the lower eyelid as initial manifestation of primary T cell malignant lymphoma of the lacrimal sac. Jpn J Clin Ophthalmol. 2003;57:1061–1066. Japanese. [Google Scholar]
- 9.Merkonidis C, Brewis C, Yung M, et al. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol. 2005;89:1589–1591. doi: 10.1136/bjo.2005.072199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bi YW, Chen RJ, Li XP. Clinical and pathological analysis of primary lacrimal sac tumors. Zhonghua Yan Ke Za Zhi. 2007;43:499–504. Chinese. [PubMed] [Google Scholar]
- 11.Maharajah KR, Hussein A, Mohamad H, At LS. Primary non-Hodgkins lymphoma of the lacrimal sac: Mortality-related epiphora. Orbit. 2009;28:306–308. doi: 10.3109/01676830903044346. [DOI] [PubMed] [Google Scholar]