Abstract
Objective
To evaluate the utility of ultrasound in aiding the diagnosis of giant cell arteritis (GCA), in monitoring the response to corticotherapy, and in detecting early relapses.
Methods
A pilot study, prospective, included 10 patients with suspected GCA. All patients underwent ultrasound examination of both temporal arteries before temporal artery biopsy (TAB), 3 weeks after starting treatment, and 3 months after diagnosis. For this study, the histological findings alone were used to define if patients were suffering from GCA. The findings on ultrasound were compared with the results of biopsy. The best place to perform TAB was observed by ultrasound.
Results
All patients with positive biopsy were detected with ultrasound. No false positives were observed on ultrasound. The results presented give a sensibility, specificity, and positive predictive value of 100% for the use of ultrasound in the diagnosis of GCA. Two relapses were detected early by ultrasound during the follow-up.
Conclusions
This pilot study suggests that eco-doppler may be a useful tool in diagnosis and clinic follow-up in patients with suspected GCA.
Keywords: giant cell arteritis, ultrasound, temporal artery biopsy, optic nerve
Giant cell arteritis (GCA) is an ophthalmological emergency that sometimes poses a diagnostic challenge. Its most serious complication is irreversible visual acuity loss secondary to ischemic optic neuropathy that may become bilateral within a few days or weeks if a prompt diagnosis and treatment are not established.1 Traditionally, histopathological confirmation based on a temporal artery biopsy (TAB) has been regarded as the gold standard. In recent years, non-invasive imaging techniques such as high-resolution color Doppler ultrasound (CDU) have been applied in an attempt to overcome the limitations of TAB,2 which is an invasive technique with complications (0.5%) fundamentally in the form of auriculo-temporal branch damage and skin necrosis, and offers only moderate sensitivity (70%–90%). In effect, 10%–30% of all patients with GCA remain undiagnosed with TAB, due to the involvement of other extracranial branches of the carotid, failure to biopsy the affected trajectory owing to the patchy inflammation of the vessel, or failure to actually biopsy arterial tissue. Temporal artery CDU is able to identify three characteristic ultrasound features: 1) A periluminal hypoechogenic halo reflecting arterial wall edema (Figure 1); 2) Segmental arterial stenosis (Figure 2); 3) Arterial luminal occlusion in severe cases. The most specific finding (85%–100%) is the periluminal halo, though the latter is scantly sensitive when isolatedly compared with the histological findings and clinical criteria. However, the sensitivity increases to 95%–100% on considering all three ultrasound features.3,4
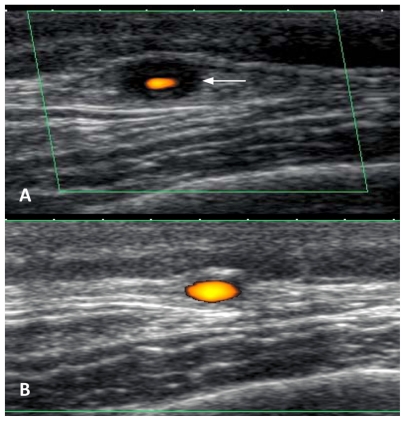
Figure 1.
A) Cross-sectional Doppler ultrasound view of the right temporal artery. The arrow shows the hypoechogenic halo sign. B) Image 3 weeks after treatment, showing disappearance of the halo.
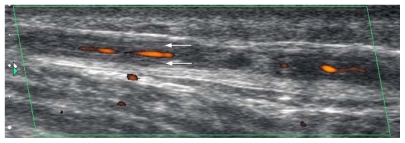
Figure 2.
Longitudinal Doppler ultrasound view. Note the important narrowing of the arterial lumen due to vasculitic edema of the wall, with multiple stenotic areas.
We have begun a prospective pilot study with 10 cases, performing CDU (TOSHIBA APLIO XG, with a PLT-1204BT high-resolution probe at 18 MHz) prior to TAB, after 3 weeks and after 3 months, to evaluate the usefulness of this imaging technique in GCA. The CDU was performed by the same user within the first three days after initial high-dose steroid administration. The TAB was accomplished along the temple, the day after CDU. The study series consisted of 4 males and 6 females, with a mean age of 76.5 years. CDU revealed some compatible sign in 6 cases (halo = 6, stenosis = 5, occlusion = 2) – the biopsy diagnosing GCA in all of them. In the 4 cases with negative CDU findings, the biopsy also proved negative. Two relapses were detected early by ultrasound during the follow-up, with a recurrence of halo sign detected. In our experience, CDU prior to TAB increases the diagnostic yield, because it is able to identify the best biopsy target segment. After starting treatment, the patient response can be evaluated using CDU, based on the course of the ultrasound signs together with the clinical and laboratory test responses. In addition, CDU is able to detect disease relapse.
Thus, CDU may be useful in application to the initial diagnosis and follow-up of patients with GCA, in view of its innocuous nature, reproducibility, and 100% correlation to the TAB findings in our series. Negative result in CDU could be used to spare biopsies. However, at present, we do not believe that CDU (with the risk implied by false-negative findings and user dependance) can fully replace TAB; rather, the two techniques complement each other. Prospective studies involving larger patient samples and longer follow-up, at least 2 years5 are needed to corroborate these findings.
Footnotes
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- 1.Jonasson F, Cullen JF, Elton PA. Temporal arteritis: a 14-year epidemiological, clinical and prognostic study. Scott Med. 1979;24:111–117. doi: 10.1177/003693307902400203. [DOI] [PubMed] [Google Scholar]
- 2.Kawasaky A, Purvin V. Giant cell arteritis: an updated review. Acta Opthalmol. 2009;87:13–32. doi: 10.1111/j.1755-3768.2008.01314.x. [DOI] [PubMed] [Google Scholar]
- 3.Karassa FB, Matsagas MI, Schmidt WA, Ioannidis JP. Meta-analysis test performance of ultrasonography for temporal arteritis. Ann Intern Med. 2009;142:359–369. doi: 10.7326/0003-4819-142-5-200503010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt WA, Möller DE, Gromnica-Ihle E. Color duplex ultrasound of the temporal artery: replacement for biopsy in temporal arteritis. Ophthalmologica. 2002;217:164–165. doi: 10.1159/000068565. [DOI] [PubMed] [Google Scholar]
- 5.Cullen JF, Chan BM, Wong CF, Chew WC. Giant cell (temporal) arteritis in Singapore: an occult case and the rationale of treatment. Singapore Med J. 2010;51:73–77. [PubMed] [Google Scholar]